Key Points
Question
Is the use of artificial intelligence (AI) in radiology practice associated with radiologist burnout?
Findings
In this cross-sectional study, the use of AI was associated with burnout among radiologists, exhibiting a dose-response association. This association was particularly pronounced in radiologists with high workload and those with low AI acceptance.
Meaning
These findings suggest the need for harmonious integration of AI tools with radiologists to effectively mitigate burnout in radiology practice.
This cross-sectional study investigates whether there is an association between artificial intelligence (AI) use in radiology and radiologist burnout in China.
Abstract
IMPORTANCE
Understanding the association of artificial intelligence (AI) with physician burnout is crucial for fostering a collaborative interactive environment between physicians and AI.
OBJECTIVE
To estimate the association between AI use in radiology and radiologist burnout.
DESIGN, SETTING, AND PARTICIPANTS
This cross-sectional study conducted a questionnaire survey between May and October 2023, using the national quality control system of radiology in China. Participants included radiologists from 1143 hospitals. Radiologists reporting regular or consistent AI use were categorized as the AI group. Statistical analysis was performed from October 2023 to May 2024.
EXPOSURE
AI use in radiology practice.
MAIN OUTCOMES AND MEASURES
Burnout was defined by emotional exhaustion (EE) or depersonalization according to the Maslach Burnout Inventory. Workload was assessed based on working hours, number of image interpretations, hospital level, device type, and role in the workflow. AI acceptance was determined via latent class analysis considering AI-related knowledge, attitude, confidence, and intention. Propensity score–based mixed-effect generalized linear logistic regression was used to estimate the associations between AI use and burnout and its components. Interactions of AI use, workload, and AI acceptance were assessed on additive and multiplicative scales.
RESULTS
Among 6726 radiologists included in this study, 2376 (35.3%) were female and 4350 (64.7%) were male; the median (IQR) age was 41 (34-48) years; 3017 were in the AI group (1134 [37.6%] female; median [IQR] age, 40 [33-47] years) and 3709 in the non-AI group (1242 [33.5%] female; median [IQR] age, 42 [34-49] years). The weighted prevalence of burnout was significantly higher in the AI group compared with the non-AI group (40.9% vs 38.6%; P < .001). After adjusting for covariates, AI use was significantly associated with increased odds of burnout (odds ratio [OR], 1.20; 95% CI, 1.10-1.30), primarily driven by its association with EE (OR, 1.21; 95% CI, 1.10-1.34). A dose-response association was observed between the frequency of AI use and burnout (P for trend < .001). The associations were more pronounced among radiologists with high workload and lower AI acceptance. A significant negative interaction was noted between high AI acceptance and AI use.
CONCLUSIONS AND RELEVANCE
In this cross-sectional study of radiologist burnout, frequent AI use was associated with an increased risk of radiologist burnout, particularly among those with high workload or lower AI acceptance. Further longitudinal studies are needed to provide more evidence.
Introduction
Burnout encompasses emotional exhaustion (EE), depersonalization (DP), and a diminished sense of personal accomplishment.1 Physician burnout has emerged as a global issue,2 primarily driven by work overload, conflicts between home and work life, and job dissatisfaction.3,4 A previous systematic review has linked physician burnout to career disengagement, high physician turnover, and reduced quality of patient care.5 Radiologists exhibit higher burnout rates compared with other medical specialists. In Germany, over 75% of radiologists have reported experiencing burnout,6 while approximately 40% of their US counterparts report similar conditions.7,8 A recent analysis estimated that 83% of radiologists exhibit at least 1 symptom of burnout.9 Moreover, elevated burnout levels have been documented across various radiology subspecialties, including interventional, musculoskeletal, pediatric, and breast.10,11,12,13
The integration of artificial intelligence (AI) in radiology practice is becoming increasingly prevalent, promising to alleviate the workload of radiologists.14 However, recent studies have shown mixed outcomes, with nearly half of the respondents indicating that AI either increases or does not significantly impact their workload.15,16 Furthermore, the relationship between AI adoption and radiologist burnout remains unclear, warranting further investigation. This cross-sectional study, based on a nationwide survey in China, investigated the association between AI use and burnout by examining the complex interactions among AI use, professional characteristics, and burnout risk. The aim of this study was to propose several short-term, localized strategies that radiology practices can adopt to enhance workforce capacity and efficiency, thereby alleviating current workload challenges.
Methods
Study Design and Participants
From May 1 to October 31, 2023, we conducted a cross-sectional study to obtain a nationally representative sample of radiologists from secondary and higher hospitals through the National Center for Quality Control of Radiology network. The network operates as a tiered system with sentinel surveillance across all 31 provincial units and Xinjiang Production and Construction Corps in mainland China (eAppendix 1 in Supplement 1). We selected 1143 hospitals and enrolled 1 to 5 radiologists aged 20 to 74 years from each, provided they had worked for at least 1 year before the survey.17 Radiologists who were pregnant or who joined the hospital after the retirement age of 60 years were excluded. Eligible radiologists were invited to anonymously complete a self-administered questionnaire via the electronic platform WJX.cn. A cover letter outlined the survey’s purpose, and the completion of the questionnaire implied consent to participate. The study was approved by the Ethics Committee of the Peking Union Medical College Hospital and adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Measures
The primary outcome was the prevalence of burnout, measured using the Chinese version of the 22-item Maslach Burnout Inventory-Human Services Survey (MBI-HSS). This instrument evaluates burnout across 3 dimensions: EE, DP, and personal accomplishment.1,18 According to the most common scoring criteria,2 burnout was defined as exhibiting at least 1 symptom of EE (≥27) or DP (≥10). In our data, the scale demonstrated a Cronbach α of 0.86 overall, with 0.92 for EE and 0.86 for DP.
We designed the survey questionnaire based on validated scales for AI literacy and adoption.19 The frequency of AI use in radiology was gauged by asking, “How frequently have you employed AI for image interpretation within the past year?” Response options included “Never,” “Infrequently,” “Regularly,” and “Consistently.”20 Radiologists reporting regular or consistent AI use were classified into the AI group, whereas others were classified into the non-AI group.
AI acceptance was evaluated through the Technology Acceptance Model,21 encompassing 4 dimensions: knowledge, confidence, attitude, and intention. Each dimension was categorized into low and high levels based on self-reported classifications and sample sizes. An overall measure of AI acceptance was derived using latent class analysis (eAppendix 2 in Supplement 1). The analysis identified 2 distinct latent classes: low acceptance and high acceptance.
Based on previous studies of risk factors for burnout, we assessed workload, psychological factors of job satisfaction, and personal and professional characteristics. Workload was evaluated through working hours on image interpretation, the volume of image interpretation, device type, role in the reporting workflow, and hospital level. Each factor was assigned 0 points for low workload and 1 point for high workload, resulting in an overall workload score ranging from 0 to 5 (eAppendix 2 in Supplement 1). Radiologists were categorized into 3 classes: low (0-2 points), medium (3 points), and high (4-5 points).
Psychological factors were measured using the Gallup Q12 Employee Engagement scale,22 which assesses perceived control, spiritual rewards, work values, organizational support, and coworker support (eAppendix 3 in Supplement 1), demonstrating a Cronbach α of 0.94 in our data. Additionally, personal and professional characteristics were gathered via a self-designed questionnaire, encompassing age, sex, education level, geographic location, marital status, parental status, and average monthly salary, along with years of full-time experience in radiology and professional title and/or position level.
Statistical Analysis
Continuous variables were summarized as median with IQR, while categorical variables were presented as frequencies. Differences between groups were assessed using the Mann-Whitney U test or χ2 test. Generalized linear regression model was used to examine the association between AI use and burnout, adjusting for personal and professional characteristics, workload score, AI acceptance, and psychological factors. We used random effects by provincial units to account for clustering of the multilayer data. AI use was analyzed as both a categorical and continuous variable to illustrate the dose-response association.
To address nonrandomized group assignments, propensity-score methods were used to mitigate confounding effects. Individual propensities for AI use were estimated using a multivariable logistic regression model, incorporating the same covariates as the explanatory model. Three propensity score–based strategies were implemented (eAppendix 4 in Supplement 1): (1) a model with inverse probability weighting (IPW), estimated using predicted probabilities from the propensity-score model; (2) a model based on matched samples created through the nearest neighbor propensity-score matching; and (3) a model that included the propensity score as an additional covariate. The primary analysis focused on models using the IPW strategy.
Stratified analyses were conducted by demographic status, hospital type, workload score, and AI acceptance. To assess the interaction among workload score, AI acceptance, and AI use on burnout, joint association analyses classified radiologists into subgroups based on workload score and AI acceptance. Given that the odds ratios (ORs) may be distorted when diseases are not rare, adjusted prevalence ratios (PRs) were calculated for joint exposure to AI use in conjunction with high workload or low AI acceptance using log-binomial regression.23 Interaction measures were determined on both additive and multiplicative scales, with additive interaction estimated by the relative excess risk due to interaction (RERI) and multiplicative interaction by the ratio of the PR (RPR). Furthermore, we plotted the burnout prediction probabilities of burnout derived from models incorporating interaction terms to illustrate these interactions. Sensitivity analyses included repeating propensity score–based models by substituting overall workload score with individual workload factors and evaluating regional variations in associations by categorizing radiologists into 4 geographic groups.
Statistical analysis was performed from October 2023 to May 2024. All models were fitted using the glmmTMB package in R statistical software version 4.2.2 (R Foundation for Statistical Computing). The Hochberg method was applied to adjust P values for multiple testing.24 All tests were 2-sided with a significance threshold of P < .05.
Results
Table 1 presents the personal and professional characteristics of the eligible radiologists. Among the 7520 radiologists invited, 6726 responded, yielding a response rate of 89.4% (eFigure 1 in Supplement 1). The median (IQR) age of the participants was 41 (34-48) years; 2376 (35.3%) were female and 4350 (64.7%) were male. Most (4749 [70.6%]) were from eastern and western China, 5716 (85.0%) were married, and 5493 (81.7%) had children. The median (IQR) duration of practice in radiology was 16 (8-25) years, and 3214 (47.8%) provided both first and second opinions in the reporting workflow. There were statistically significant differences in age, having children, marital status, and income level between respondents and nonrespondents (eTable 1 and 2 in Supplement 1).
Table 1. Personal and Professional Characteristics of Radiologists.
| Characteristics | Radiologists, No. (%) | Radiologists after inverse probability weighting, % | |||
|---|---|---|---|---|---|
| Total (N = 6726) | Crude | ||||
| AI group (n = 3017) | Non-AI group (n = 3709) | AI group | Non-AI group | ||
| Personal | |||||
| Age, median (IQR), y | 41 (34-48) | 40 (33-47) | 42 (34-49) | 41 (34-49) | 41 (34-48) |
| Sex | |||||
| Male | 4350 (64.7) | 1883 (62.4) | 2467 (66.5) | 65.2 | 65.1 |
| Female | 2376 (35.3) | 1134 (37.6) | 1242 (33.5) | 34.8 | 34.9 |
| Have children | 5493 (81.7) | 2401 (79.6) | 3092 (83.4) | 82.6 | 82.4 |
| Geographic region | |||||
| Eastern | 2686 (39.9) | 1327 (44.0) | 1359 (36.6) | 41.0 | 41.0 |
| Central | 1147 (17.1) | 456 (15.1) | 691 (18.6) | 16.4 | 16.7 |
| Western | 2063 (30.7) | 919 (30.5) | 1144 (30.8) | 30.6 | 30.2 |
| Northeast | 830 (12.3) | 315 (10.4) | 515 (13.9) | 12.0 | 12.3 |
| Relationship status | |||||
| Single | 905 (13.5) | 436 (14.5) | 469 (12.6) | 12.4 | 13.2 |
| Married | 5716 (85.0) | 2536 (84.1) | 3180 (85.7) | 86.1 | 85.3 |
| Othersa | 105 (1.5) | 45 (1.5) | 60 (1.6) | 1.4 | 1.5 |
| Monthly income, <5000 | 5447 (80.9) | 2132 (70.7) | 3315 (89.4) | 80.5 | 80.4 |
| Education levels, lowb | 5502 (81.8) | 2127 (70.5) | 3375 (91.0) | 81.7 | 82.0 |
| Professional | |||||
| Specialty, breast, chest, or blood vessel | 5513 (82.0) | 2458 (81.5) | 3055 (82.4) | 84.2 | 80.9 |
| Years in practice, median (IQR), y | 16 (8-25) | 15 (8-24) | 17 (9-26) | 17 (9-26) | 16 (9-26) |
| Workload score, median (IQR) | 3 (2-3) | 3 (2-4) | 2 (2-3) | 3 (2-3) | 3 (2-3) |
| Hours worked per week, median (IQR), h | 42 (40-50) | 45 (40-50) | 40 (40-50) | 44 (40-50) | 42 (40-50) |
| No. of images per day, median (IQR) | 115 (72-180) | 131 (90-208) | 100 (60-157) | 120 (75-183) | 112 (72-182) |
| Tertiary hospitals | 3988 (59.3) | 2376 (78.8) | 1612 (43.5) | 60.1 | 59.6 |
| Senior professional title | 2500 (37.2) | 1229 (40.7) | 1271 (34.3) | 41.9 | 37.5 |
| Main working in practice | |||||
| Radiograph | 2526 (37.6) | 913 (30.3) | 1613 (43.9) | 36.1 | 36.3 |
| Computerized tomography | 3754 (55.8) | 1955 (64.8) | 1799 (48.5) | 57.1 | 56.5 |
| Magnetic resonance imaging | 446 (6.6) | 149 (4.9) | 297 (8.0) | 6.8 | 7.2 |
| Role in the workflow | |||||
| Initial opinion | 1774 (26.4) | 759 (25.2) | 1015 (27.4) | 25.2 | 26.0 |
| Second opinion | 1738 (25.8) | 982 (32.6) | 756 (20.4) | 29.9 | 24.8 |
| Both | 3214 (47.8) | 1276 (42.3) | 1938 (52.3) | 44.9 | 49.3 |
| AI acceptance, high | 5222 (77.6) | 2645 (71.3) | 2577 (85.4) | 78.0 | 77.7 |
| Attitude toward AI, positive | 6253 (93.0) | 2930 (97.1) | 3323 (89.6) | 97.1 | 90.3 |
| Knowledge of AI, familiar | 3047 (45.3) | 1582 (52.4) | 1465 (39.5) | 48.7 | 43.6 |
| Confidence on AI, positive | 4482 (66.6) | 2223 (73.7) | 2259 (60.9) | 72.4 | 61.9 |
| Motivation to learn AI, positive | 5254 (78.1) | 2702 (72.9) | 2552 (84.6) | 78.7 | 78.3 |
Abbreviation: AI, artificial intelligence.
Others include divorce, separation, widowed, or widower.
Bachelor’s degree and below.
There were 3017 radiologists regularly or consistently using AI in their practice. These radiologists were younger (median [IQR] ages: 40 [33-47] vs 42 [34-49] years; P < .001), more likely to be female (1134 [37.6%] vs 1242 [33.5%]; P < .001), more likely from eastern China (1327 [44.0%] vs 1359 [36.6%]; P < .001), and had higher educational levels (3890 [29.5%] vs 334 [9.0%]; P < .001) compared with those in the non-AI group. Additionally, the proportion of radiologists primarily practicing computed tomography reading was higher in the AI group compared with the non-AI group (1955 [64.8%] vs 1799 [48.5%]; P < .001). Radiologists in the AI group had fewer median (IQR) full-time working years than their counterparts (15 [8-24] vs 17 [9-26] years; P < .001), but they worked more median (IQR) hours per week (45 [40-50] vs 40 [40-50] hours; P = .001) and interpreted more images per day (131 [90-208] vs 100 [60-157]; P < .001). After adjustment based on propensity score, differences in the characteristics between the AI and non-AI groups were significantly reduced or eliminated (Table 1; eTable 3 in Supplement 1).
Table 2 compares burnout, its components, and psychological factors of job satisfaction between the AI and the non-AI groups. Overall, 2675 radiologists were classified as experiencing burnout. The crude prevalence of burnout among participants was 39.8%, with EE reported by 34.4% and DP by 18.1%. The weighted prevalence of burnout was higher in the AI group than in the non-AI group (40.9% vs 38.6%; P = .006), primarily due to differences in EE (35.4% vs 33.2%; P = .006). The weighted prevalence of DP was similar between groups (18.4% vs 18.1%; P = .64). Additionally, the AI group exhibited higher weighted prevalence of burnout across various subgroups (eTable 4 in Supplement 1).
Table 2. Burnout and Career Satisfaction by AI Use.
| Variable | Total (N = 6726) | Crude, No. (%) | Inverse probability weighting, % | ||
|---|---|---|---|---|---|
| AI group (n = 3017) | Non-AI group (n = 3709) | AI group (n = 3017) | Non-AI group (n = 3709) | ||
| Burnouta | 2675 (39.8) | 1293 (42.9) | 1382 (37.3) | 40.9 | 38.6 |
| Burnout measurement | |||||
| Emotional exhaustion | |||||
| Mean (SD) | 21.3 (14.0) | 22.5 (13.8) | 20.4 (14.1) | 22.0 (20.6) | 20.9 (18.9) |
| Median (IQR) | 19 (10-31) | 21 (11,33) | 17 (9-30) | 19 (10-32) | 18 (9-30) |
| Proportion of ≥27 | 2311 (34.4) | 1140 (37.8) | 1171 (31.6) | 35.4 | 33.2 |
| Depersonalization | |||||
| Mean (SD) | 4.9 (6.1) | 4.9 (5.9) | 4.9 (6.2) | 4.9 (8.9) | 4.9 (8.2) |
| Median (IQR) | 3 (1-7) | 3 (1-7) | 3 (0-7) | 3 (1-7) | 3 (1-7) |
| Proportion of ≥10 | 1214 (18.1) | 545 (18.1) | 669 (18.0) | 18.4 | 18.1 |
| Autonomy, control, and meaning in workb | |||||
| Autonomy, agree | 5242 (77.9) | 2376 (78.8) | 2866 (77.3) | 77.9 | 78.0 |
| Control, agree | 3740 (55.6) | 1800 (59.7) | 1940 (52.3) | 56.1 | 55.7 |
| Meaningful, agree | 4337 (64.5) | 2009 (66.6) | 2328 (62.8) | 64.8 | 64.7 |
| Supporting circumstancec | |||||
| Supporting from staff, agree | 3893 (57.9) | 2168 (71.9) | 2563 (69.1) | 70.1 | 70.2 |
| Supporting from organization, agree | 4031 (59.9) | 1915 (63.5) | 2116 (57.1) | 60.0 | 59.8 |
Abbreviation: AI, artificial intelligence.
Burnout is defined as emotional exhaustion score of at least 27, or depersonalization score of at least 10.
Questions are from the Q3, Q4, Q5, Q8, and Q9 of the Gallup Q12 Employee Engagement scale.
Questions are from the Q5 and Q9 of the Gallup Q12 Employee Engagement scale.
A majority of radiologists reported having autonomy in their practice (77.9%), with no significant difference between the 2 groups. A higher proportion of radiologists in the AI group felt their opinions were valued in practice (59.7%) and that their work was meaningful (66.6%), compared with those in the non-AI group. Additionally, satisfaction with organizational support (1915 [63.5%] vs 2116 [57.1%]; P = .01) and staff (2168 [71.9%] vs 2563 [69.1%]; P < .001) was higher in the AI group.
In crude regression analysis (Table 3), radiologists using AI were more likely to experience burnout than those who did not (OR, 1.26; 95% CI, 1.14-1.40). This association remained significant after adjustment for covariates (adjusted OR, 1.18; 95% CI, 1.05-1.33). Dose-response analysis indicated that the odds of burnout increased with the frequency of AI use (regularly: OR, 1.17; 95% CI, 1.04-1.32; consistently: OR, 1.39; 95% CI, 1.09-1.75). In the primary analysis with IPW, AI use was significantly associated with higher odds of burnout (OR, 1.20; 95% CI, 1.10-1.30). AI use was significantly associated with EE (OR, 1.21; 95% CI, 1.10-1.34), but not with DP.
Table 3. Association of AI Use With Burnout in Crude, Multivariable, and Propensity Score Analysis.
| Burnout | Emotional exhaustion | Depersonalization | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | |
| Crude analysis (yes vs no) | 1.26 (1.14-1.40) | <.001 | 1.31 (1.18-1.45) | <.001 | 1.01 (0.89-1.15) | .86 |
| Multivariable analysis (yes vs no)a | 1.18 (1.05-1.33) | .004 | 1.21 (1.08-1.37) | .002 | 1.03 (0.90-1.19) | .66 |
| Multivariable analysis (vs no)b | ||||||
| Regularly | 1.17 (1.04-1.32) | .008 | 1.19 (1.05-1.34) | .005 | 0.99 (0.86-1.14) | .87 |
| Consistently | 1.39 (1.09-1.75) | .008 | 1.41 (1.11-1.80) | .005 | 1.43 (1.09-1.88) | .02 |
| Multivariable analysis (continuous)c | 1.18 (1.07-1.30) | <.001 | 1.19 (1.08-1.31) | <.001 | 1.09 (0.97-1.22) | .14 |
| Propensity-score analyses | ||||||
| With IPW (yes vs no)d | 1.20 (1.10-1.30) | <.001 | 1.21 (1.10-1.34) | <.001 | 1.11 (0.99-1.23) | .06 |
| With matching (yes vs no)e | 1.28 (1.12-1.46) | <.001 | 1.31 (1.14-1.50) | <.001 | 1.08 (0.92-1.26) | .36 |
| Adjusted for propensity score (yes vs no)f | 1.18 (1.05-1.33) | .005 | 1.21 (1.07-1.36) | .002 | 1.00 (0.87-1.15) | .99 |
Abbreviations: AI, artificial intelligence; IPW, inverse probability weighting; OR, odds ratio.
Result is the adjusted OR from the multivariable logistic regression adjusting for covariates and random effect of provinces. The analysis included 6726 radiologists.
Frequency of using AI in practice was regarded as categorical variable in the multivariable logistic regression adjusting for covariates and random effect of provinces. The analysis included 6726 radiologists. P value was corrected by Hochberg method.
Frequency of using AI in practice was regarded as continuous variable in the multivariable logistic regression adjusting for covariates and random effect of provinces. The analysis included 6726 radiologists.
Result is the adjusted OR from the multivariable logistic regression with IPW, adjusting for covariates and random effect of provinces. The analysis included 6726 radiologists.
Frequency of using AI in practice was regarded as categorical variable in the multivariable logistic regression adjusting for covariates. The analysis included 3978 matching radiologists.
Result is the adjusted OR from the multivariable logistic regression adjusting for covariates, the propensity score, and random effect of provinces. The analysis included 6726 radiologists.
Stratified analysis (Table 4; eFigure 2 in Supplement 1) revealed significant associations between AI use and burnout or EE in most subgroups, except those with higher education levels, secondary hospital, low workload score, and high AI acceptance. No significant associations were found for DP in most subgroups. Associations were stronger among those who consistently used AI, and the dose-response association was significant in most subgroups (eTable 5, 6, and 7 in Supplement 1). Notably, radiologists with low AI acceptance had significant associations for all 3 burnout indices.
Table 4. Association of AI Use by Frequency With Burnout by Demographic Status and Workload and AI Acceptance.
| Characteristics | Burnouta | Emotional exhaustion | Depersonalization | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Regularly AI use, OR (95% CI)b | Consistently AI use, OR (95% CI)b | P value for trendc | Regularly AI use, OR (95% CI)b | Consistently AI use, OR (95% CI)b | P value for trendc | Regularly AI use, OR (95% CI)b | Consistently AI use, OR (95% CI)b | P value for trendc | |
| Sex | |||||||||
| Male | 1.10 (0.97-1.24) | 1.68 (1.24-2.28)d | .002 | 1.08 (0.95-1.23) | 1.63 (1.21-2.18)d | .005 | 1.06 (0.93-1.20) | 1.84 (1.40-2.41)d | .001 |
| Female | 1.37 (1.15-1.63)d | 1.35 (0.96-1.91) | .001 | 1.38 (1.15-1.64)d | 1.37 (0.97-1.93) | <.001 | 0.96 (0.79-1.18) | 1.24 (0.83-1.86) | .66 |
| Age group | |||||||||
| <40 y | 1.23 (1.05-1.43)d | 1.53 (1.10-2.12)d | <.001 | 1.24 (1.06-1.45)d | 1.54 (1.11-2.14)d | <.001 | 1.03 (0.87-1.21) | 1.48 (1.07-2.05)d | .08 |
| ≥40 y | 1.16 (1.01-1.32)d | 1.48 (1.09-2.01)d | .003 | 1.15 (1.00-1.31)d | 1.43 (1.05-1.94)d | .006 | 1.08 (0.94-1.25) | 1.72 (1.27-2.34)d | .005 |
| Education levele | |||||||||
| Low | 1.19 (1.07-1.33)d | 1.57 (1.22-2.02)d | <.001 | 1.18 (1.06-1.32)d | 1.55 (1.21-1.98)d | <.001 | 1.09 (0.97-1.23) | 1.68 (1.32-2.15)d | <.001 |
| High | 1.26 (0.97-1.64) | 1.10 (0.68-1.77) | 0.24 | 1.33 (1.02-1.73) | 1.23 (0.75-2.10) | .08 | 0.90 (0.69-1.20) | 1.19 (0.73-1.95) | .91 |
| Hospital type | |||||||||
| Secondary | 1.14 (0.96-1.34) | 1.42 (0.89-2.28) | .04 | 1.06 (0.89-1.25) | 1.36 (0.85-2.20) | .24 | 1.06 (0.89-1.27) | 1.37 (0.85-2.20) | .22 |
| Tertiary | 1.23 (1.08-1.40)d | 1.48 (1.15-1.92)d | <.001 | 1.29 (1.13-1.47)d | 1.52 (1.18-1.96)d | <.001 | 1.06 (0.92-1.22) | 1.60 (1.24-2.05)d | .003 |
| Workload score | |||||||||
| Low score | 1.09 (0.94-1.27) | 1.73 (1.20-2.49)d | .01 | 1.07 (0.91-1.25) | 1.53 (1.06-2.21)d | .06 | 1.06 (0.90-1.25) | 1.89 (1.29-2.77)d | .02 |
| Medium score | 1.32 (1.11-1.58)d | 1.24 (0.87-1.74) | .006 | 1.30 (1.10-1.54)d | 1.23 (0.87-1.74) | .007 | 1.14 (0.95-1.37) | 1.35 (0.93-1.95) | .06 |
| High score | 1.27 (1.01-1.61) | 1.60 (1.00-2.56)d | .01 | 1.35 (1.07-1.69)d | 1.74 (1.10-2.75)d | .002 | 0.94 (0.76-1.17) | 1.71 (1.14-2.58)d | .16 |
| AI acceptance | |||||||||
| Low | 1.55 (1.24-1.92)d | 2.50 (1.33-4.71)d | <.001 | 1.50 (1.21-1.86)d | 2.68 (1.43-5.02)d | <.001 | 1.43 (1.13-1.79)d | 1.45 (0.81-2.58) | .004 |
| High | 1.10 (0.98-1.24) | 1.30 (1.02-1.65) | .01 | 1.12 (0.99-1.25) | 1.26 (0.99-1.60) | .02 | 0.97 (0.86-1.10) | 1.54 (1.22-1.96)d | .04 |
Abbreviations: AI, artificial intelligence; OR, odds ratio.
Burnout was defined as having at least 1 symptom of the emotional exhaustion (≥27) or depersonalization (≥10).
The regressions with inverse probability weighting were fitted by taking the frequency of AI use as categorical variable, adjusting for covariates and random effect of provinces, with the exception of stratified variables, which were mutually adjusted.
P for trend was calculated by the same model using frequency of AI use as continuous variable.
P < .05 with multiple testing correction by Hochberg method.
Education level was categorized as bachelor’s degree and below and graduate degree and above.
Joint association analysis (Figure) exhibited the highest PR of 1.66 (95% CI, 1.50 to 1.82) among radiologists with high workload scores compared with those with lower workloads. Although there was positive interaction on both additive and multiplicative scales, it was not statistically significant. Conversely, the highest PR of 1.27 (95% CI, 1.14 to 1.42) for burnout was found among radiologists with low AI acceptance, whereas the association attenuated to 1.16 (95% CI, 1.06 to 1.27) among those with high acceptance. There was a significantly negative interaction on both additive (RERI, −0.20; 95% CI, −0.35 to −0.05) and multiplicative scales (RPR, 0.84; 95% CI, 0.73 to 0.95). Similar patterns were observed for EE and DP (eFigure 3, eTable 8, and eTable 9 in Supplement 1).
Figure. Joint Association of AI Use, Workload, and AI Acceptance With Burnout.
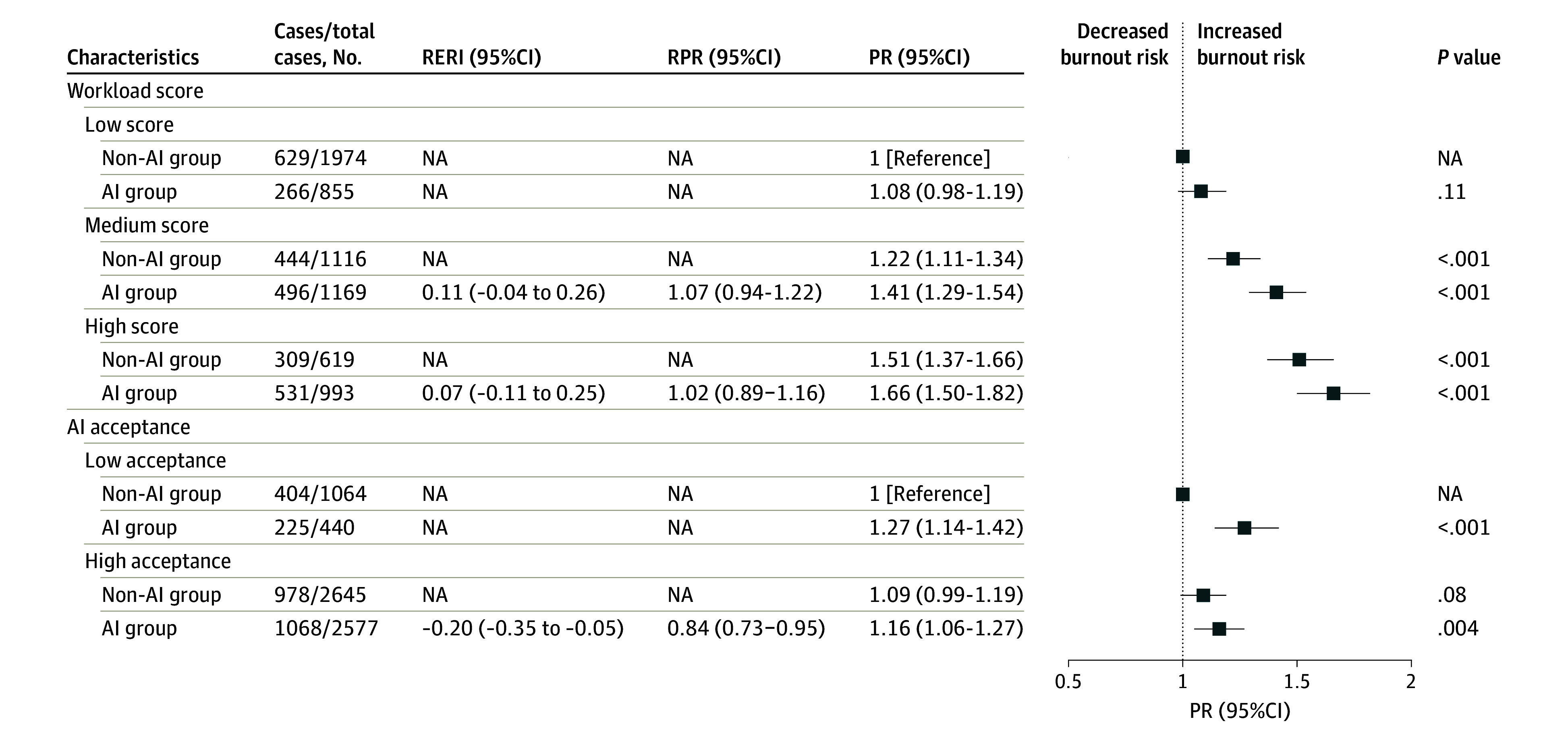
Prevalence ratios (PRs) were calculated for the joint exposure of AI use and workload score groups by binomial-log regression, adjusting for individual and professional characteristics and psychological factors. All analyses were calculated using inverse propensity weighting. Relative excess risk due to interaction (RERI) was estimated using the following formula: PR11 − PR10 − PR01 + 1. Ratio of prevalence risk (RPR) was estimated using PR11 / (PR01 × PR10). P value was corrected by Hochberg method. AI indicates artificial intelligence; NA, not applicable.
Sensitivity analyses supported these findings (Table 3; eTable 10 and 11 in Supplement 1). Multivariable analyses using matching or IPW found a significant association between AI use and radiologist burnout. This association remained robust when substituting overall workload and AI acceptance with individual factors. The association pattern persisted across different regions, even though significance was not consistently achieved.
Discussion
To our knowledge, this study is the first to investigate the association between AI use and radiologist burnout using a large, nationwide cross-sectional sample. We found that AI use was associated with increased odds of burnout among radiologists, exhibiting a significant dose-response association. Moreover, joint exposure to AI use alongside either high workload or low AI acceptance was associated with an additional risk of burnout. These results underscore the need to reassess the role of AI technology in mitigating radiologist burnout. Balancing AI use with an appropriate radiology workforce and maintaining psychological acceptance of AI technology in clinical practice is essential.
The increased burnout associated with AI use in our study primarily stems from EE, driven by elevated work demands and overload.1 Previous studies have identified work overload as a principal risk factor for physician burnout.3,4 To address workload issues in radiology, there is growing interest in AI-assisted imaging identification. Prior studies suggest that AI use could reduce radiologists’ workload by 40% to 90% in cancer screening by minimizing repetitive tasks and unnecessary discussions.25,26 However, the potential drawbacks of AI technologies in clinical settings have often been overlooked. Recent discussions have examined the divergent impacts of AI in public health screening vs clinical care.27 Unlike in screening, where high sensitivity of AI may reduce workload, the clinical setting often necessitates more radiologist time for differential diagnoses. For example, researchers found that AI could decrease reading times for radiologists when no abnormalities are detected, but it could increase reading times when abnormalities are present.28 Furthermore, the increased workload attributed to AI often results from elevated postprocessing and interpretation times.16 Our study underscores a critical knowledge gap, demonstrating a positive association between AI use and radiologist burnout, which longitudinal studies should further explore.
Our results indicate that the association of AI use with burnout may be exacerbated by increasing workload. The integration of AI technology in hospitals could lead to higher consultation volumes and increase radiologists’ workload. Although data to substantiate this are limited, policymakers are considering increasing radiology capacity with AI to address rising care demands, particularly in tertiary hospitals.29,30 For radiologists, the inherently isolated and sedentary nature of their work contributes to higher burnout rates compared with other specialties.4,31 AI may further exacerbate these challenges by diminishing opportunities for peer collaboration and patient interaction, while fears of job displacement and uncertainties surrounding AI use heighten stress.32,33,34 Joint association analyses showed that the risk of burnout associated with AI use was particularly pronounced among radiologists with high workloads, highlighting the urgent need to explore effective coordination strategies between radiologists and AI.
Existing evidence links physician pressure to increase knowledge and skills in clinical practice and job satisfaction to burnout.4,31 Those lacking clinical experience, such as junior or younger physicians, as well as those reporting low job satisfaction, are at a heightened risk for burnout. Our study found a joint association of AI use and high AI acceptance on radiologist burnout. The integration of AI in radiology practice necessitates a shift in knowledge structure, requiring radiologists to learn how to operate, interpret, and interact with these technologies. Radiologists with negative attitudes toward AI, limited knowledge, or a lower intention to use AI may experience diminished job satisfaction, particularly when required to implement AI in their practice. To our knowledge, no prior study has examined modifiable factors of the association between between AI use and burnout. Although there are growing concerns that AI may alleviate physician workload across various medical specialties, the harmonizing of the relationship between physicians and AI tools has not yet been appropriately prioritized. Our findings provide insights in this regard.
A strength of our study is the representative sample of radiologists selected through a national radiology quality control system, ensuring a higher response rate compared with other studies.3,10,32 Participants were enrolled from approximately 70% of prefecture-level cities in all 31 provinces of China, representing a wide range of personal and professional characteristics. Our sample size is the largest among recent studies, enabling analyses with sufficient statistical power.
Radiologists, already in short supply, are overwhelmed by rapidly growing health care needs and medical imaging data.35,36 In China, the annual growth rate of medical imaging data are 7.5 times that of radiologists.30 Therefore, radiologists’ workload and burnout are receiving unprecedented attention. AI technology offers a potential solution to the shortage of radiologists. Policymakers and researchers are planning or have implemented AI strategies in radiology to address the supply-demand imbalance while maintaining the same or a slowly growing radiology workforce. However, the excitement and expectations surrounding technological advances should not overshadow the challenges that remain before AI can be routinely applied in radiology practice. AI tools must provide clinical results that radiologists can understand and trust to truly reduce workload. Few AI technologies have been rigorously validated in randomized clinical trials.37 Furthermore, integrating AI tools into the radiology workflow should be a key research task.29,38 Although further work is needed to establish causal relationships and intervention feasibility, our findings emphasize the importance of creating a suitable environment for the interaction between radiologist and AI. This includes improving the interpretability of AI tools, providing education about AI technology, and increasing AI acceptance among radiologists.
Limitations
Our study has limitations. Despite an approximately 90% response rate, there is a possibility that nonrespondents may be too burned out to participate, potentially introducing nonresponse bias. Including only secondary and higher hospitals may result in insufficient representation of primary hospitals. The cross-sectional design also complicates the ability to confirm the direction of the association. While we suggest that AI use is a risk factor for burnout, it is plausible that burnout could drive the adoption of AI in practice. Additionally, we could not ascertain whether the effects would diminish as radiologists become more adept with AI. Nevertheless, our stratified and dose-response analyses strengthen the validity of our findings. Moreover, we did not collect data on leadership within radiology practices, a factor known to influence burnout.39,40 Additionally, the frequency of AI use was determined through self-report rather than objective records, leaving room for measurement error.
Conclusions
In this cross-sectional study of radiologist burnout, AI use was associated with higher odds of radiologist burnout, with a significant dose-response association. The association was moderated by radiologists’ workload and AI acceptance. The role of AI in alleviating radiologist burnout should be considered cautiously, and longitudinal studies are warranted to further elucidate this association.
eAppendix 1. Description of the Sampling Design in the Survey
eAppendix 2. Assessment of Workload and AI Acceptance
eAppendix 3. Gallup’s Employee Engagement Scale
eAppendix 4. Statistical Analysis
eFigure 1. Flowchart of Study Cohort
eFigure 2. Association of AI Use With Burnout and Its Components by Subgroups
eFigure 3. Predicted Probability of Burnout for Joint Exposure of AI Use, Workload, and AI Acceptance
eTable 1. Distribution of Participants and Response Rate
eTable 2. Personal and Professional Characteristics Between Included and Excluded Radiologists
eTable 3. Personal and Professional Characteristics after Propensity Score Matching
eTable 4. Weighted Prevalence of Radiologist Burnout Between the AI and Non-AI Groups
eTable 5. Dose-Response Association Between the Frequency of AI Use and Burnout in Radiology Practice by Subgroups
eTable 6. Dose-Response Association Between the Frequency of AI Use and Emotional Exhaustion in Radiology Practice by Subgroups
eTable 7. Dose-Response Association Between the Frequency of AI Use and Depersonalization in Radiology Practice by Subgroups
eTable 8. Joint Association of AI Use, Workload, and AI Acceptance With Emotional Exhaustion
eTable 9. Joint Association of AI Use, Workload, and AI Acceptance With Depersonalization
eTable 10. Association of AI Use With Burnout Adjusting for Workload Factors in Regression Models
eTable 11. Association of AI Use With Burnout by Geographic Locations
Data Sharing Statement
References
- 1.Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016;15(2):103-111. doi: 10.1002/wps.20311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320(11):1131-1150. doi: 10.1001/jama.2018.12777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Busis NA, Shanafelt TD, Keran CM, et al. Burnout, career satisfaction, and well-being among US neurologists in 2016. Neurology. 2017;88(8):797-808. doi: 10.1212/WNL.0000000000003640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Amoafo E, Hanbali N, Patel A, Singh P. What are the significant factors associated with burnout in doctors? Occup Med (Lond). 2015;65(2):117-121. doi: 10.1093/occmed/kqu144 [DOI] [PubMed] [Google Scholar]
- 5.Hodkinson A, Zhou A, Johnson J, et al. Associations of physician burnout with career engagement and quality of patient care: systematic review and meta-analysis. BMJ. 2022;378:e070442. doi: 10.1136/bmj-2022-070442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bastian MB, Fröhlich L, Wessendorf J, et al. Prevalence of burnout among German radiologists: a call to action. Eur Radiol. 2024;34(9):5588-5594. doi: 10.1007/s00330-024-10627-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Higgins MCSS, Nguyen MT, Kosowsky T, et al. Burnout, professional fulfillment, intention to leave, and sleep-related impairment among faculty radiologists in the United States: an epidemiologic study. J Am Coll Radiol. 2021;18(9):1359-1364. doi: 10.1016/j.jacr.2021.04.005 [DOI] [PubMed] [Google Scholar]
- 8.Parikh JR, Moore AV, Mead L, Bassett R, Rubin E. Prevalence of burnout of radiologists in private practice. J Am Coll Radiol. 2023;20(7):712-718. doi: 10.1016/j.jacr.2023.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hassankhani A, Amoukhteh M, Valizadeh P, et al. A Meta-analysis of burnout in radiology trainees and radiologists: insights from the Maslach Burnout Inventory. Acad Radiol. 2024;31(3):1198-1216. doi: 10.1016/j.acra.2023.10.046 [DOI] [PubMed] [Google Scholar]
- 10.Al Rekabi A, Chen M, Patel N, et al. Well-being and burnout amongst interventional radiologists in the United Kingdom. Cardiovasc Intervent Radiol. 2023;46(8):1053-1063. doi: 10.1007/s00270-023-03455-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chew FS, Mulcahy MJ, Porrino JA, Mulcahy H, Relyea-Chew A. Prevalence of burnout among musculoskeletal radiologists. Skeletal Radiol. 2017;46(4):497-506. doi: 10.1007/s00256-017-2578-9 [DOI] [PubMed] [Google Scholar]
- 12.Ayyala RS, Ahmed FS, Ruzal-Shapiro C, Taylor GA. Prevalence of burnout among pediatric radiologists. J Am Coll Radiol. 2019;16(4 Pt A):518-522. doi: 10.1016/j.jacr.2018.08.016 [DOI] [PubMed] [Google Scholar]
- 13.Parikh JR, Sun J, Mainiero MB. Prevalence of burnout in breast imaging radiologists. J Breast Imaging. 2020;2(2):112-118. doi: 10.1093/jbi/wbz091 [DOI] [PubMed] [Google Scholar]
- 14.Haug CJ, Drazen JM. Artificial intelligence and machine learning in clinical medicine, 2023. N Engl J Med. 2023;388(13):1201-1208. doi: 10.1056/NEJMra2302038 [DOI] [PubMed] [Google Scholar]
- 15.European Society of Radiology (ESR) . Impact of artificial intelligence on radiology: a EuroAIM survey among members of the European Society of Radiology. Insights Imaging. 2019;10(1):105. doi: 10.1186/s13244-019-0798-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kwee TC, Kwee RM. Workload of diagnostic radiologists in the foreseeable future based on recent scientific advances: growth expectations and role of artificial intelligence. Insights Imaging. 2021;12(1):88. doi: 10.1186/s13244-021-01031-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang J, Han X, Yang Z, et al. Radiology residency training in China: results from the first retrospective nationwide survey. Insights Imaging. 2021;12(1):25. doi: 10.1186/s13244-021-00970-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zalaquett CP, Wood RJ. Evaluating stress: a book of resources. The Scarecrow Press; 1996. [Google Scholar]
- 19.Lintner T. A systematic review of AI literacy scales. NPJ Sci Learn. 2024;9(1):50. doi: 10.1038/s41539-024-00264-4 [DOI] [PMC free article] [PubMed]
- 20.Choudhury A, Shamszare H. Investigating the impact of user trust on the adoption and use of ChatGPT: survey analysis. J Med Internet Res. 2023;25:e47184. doi: 10.2196/47184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. Manage Inf Syst Q. 1989;13(3):319-340. doi: 10.2307/249008 [DOI] [Google Scholar]
- 22.Gallup. Gallup’s Employee Engagement survey: ask the right questions with the Q12 Survey. Accessed May 10, 2023.https://www.gallup.com/q12/
- 23.Petersen MR, Deddens JA. A comparison of two methods for estimating prevalence ratios. BMC Med Res Methodol. 2008;8:9. doi: 10.1186/1471-2288-8-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hochberg Y. A sharper Bonferroni procedure for multiple tests of significance. Biometrika. 1988;75(4):800-802. doi: 10.1093/biomet/75.4.800 [DOI] [Google Scholar]
- 25.Larsen M, Aglen CF, Hoff SR, Lund-Hanssen H, Hofvind S. Possible strategies for use of artificial intelligence in screen-reading of mammograms, based on retrospective data from 122,969 screening examinations. Eur Radiol. 2022;32(12):8238-8246. doi: 10.1007/s00330-022-08909-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Raya-Povedano JL, Romero-Martín S, Elías-Cabot E, Gubern-Mérida A, Rodríguez-Ruiz A, Álvarez-Benito M. AI-based strategies to reduce workload in breast cancer screening with mammography and tomosynthesis: a retrospective evaluation. Radiology. 2021;300(1):57-65. doi: 10.1148/radiol.2021203555 [DOI] [PubMed] [Google Scholar]
- 27.Speechley M, Kunnilathu A, Aluckal E, Balakrishna MS, Mathew B, George EK. Screening in public health and clinical care: similarities and differences in definitions, types, and aims - a systematic review. J Clin Diagn Res. 2017;11(3):LE01-LE04. doi: 10.7860/JCDR/2017/24811.9419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shin HJ, Han K, Ryu L, Kim EK. The impact of artificial intelligence on the reading times of radiologists for chest radiographs. NPJ Digit Med. 2023;6(1):82. doi: 10.1038/s41746-023-00829-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saw SN, Ng KH. Current challenges of implementing artificial intelligence in medical imaging. Phys Med. 2022;100:12-17. doi: 10.1016/j.ejmp.2022.06.003 [DOI] [PubMed] [Google Scholar]
- 30.Meng F, Zhan L, Liu S, Zhang H. The growing problem of radiologist shortage: China’s perspective. Korean J Radiol. 2023;24(11):1046-1048. doi: 10.3348/kjr.2023.0839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harolds JA, Parikh JR, Bluth EI, Dutton SC, Recht MP. Burnout of radiologists: frequency, risk factors, and remedies: a report of the ACR commission on human resources. J Am Coll Radiol. 2016;13(4):411-416. doi: 10.1016/j.jacr.2015.11.003 [DOI] [PubMed] [Google Scholar]
- 32.Luo S, Zhang Y, Wang P, et al. The moderating role of resilience in the association between workload and depressive symptoms among radiology residents in China: results from a nationwide cross-sectional study. Eur Radiol. 2024;34(1):695-704. doi: 10.1007/s00330-023-10021-7 [DOI] [PubMed] [Google Scholar]
- 33.Al-Medfa MK, Al-Ansari AMS, Darwish AH, Qreeballa TA, Jahrami H. Physicians’ attitudes and knowledge toward artificial intelligence in medicine: benefits and drawbacks. Heliyon. 2023;9(4):e14744. doi: 10.1016/j.heliyon.2023.e14744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Qurashi AA, Alanazi RK, Alhazmi YM, Almohammadi AS, Alsharif WM, Alshamrani KM. Saudi radiology personnel’s perceptions of artificial intelligence implementation: a cross-sectional study. J Multidiscip Healthc. 2021;14:3225-3231. doi: 10.2147/JMDH.S340786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Agarwal M, van der Pol CB, Patlas MN, Udare A, Chung AD, Rubino J. Optimizing the radiologist work environment: actionable tips to improve workplace satisfaction, efficiency, and minimize burnout. Radiol Med. 2021;126(10):1255-1257. doi: 10.1007/s11547-021-01397-x [DOI] [PubMed] [Google Scholar]
- 36.Dibble EH, Rubin E, Duszak R Jr, Parris D, Tarrant MJ, Parikh JR. The 2021 ACR/RBMA workforce survey: practice types, employment trends, and hiring needs. J Am Coll Radiol. 2024;21(3):493-502. doi: 10.1016/j.jacr.2023.02.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Plana D, Shung DL, Grimshaw AA, Saraf A, Sung JJY, Kann BH. Randomized clinical trials of machine learning interventions in health care: a systematic review. JAMA Netw Open. 2022;5(9):e2233946. doi: 10.1001/jamanetworkopen.2022.33946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Föllmer B, Williams MC, Dey D, et al. Roadmap on the use of artificial intelligence for imaging of vulnerable atherosclerotic plaque in coronary arteries. Nat Rev Cardiol. 2024;21(1):51-64. doi: 10.1038/s41569-023-00900-3 [DOI] [PubMed] [Google Scholar]
- 39.Mete M, Goldman C, Shanafelt T, Marchalik D. Impact of leadership behaviour on physician well-being, burnout, professional fulfilment and intent to leave: a multicentre cross-sectional survey study. BMJ Open. 2022;12(6):e057554. doi: 10.1136/bmjopen-2021-057554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lexa FJ, Parikh JR. Leadership: causing and curing burnout in radiology. J Am Coll Radiol. 2023;20(5):500-502. doi: 10.1016/j.jacr.2023.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Description of the Sampling Design in the Survey
eAppendix 2. Assessment of Workload and AI Acceptance
eAppendix 3. Gallup’s Employee Engagement Scale
eAppendix 4. Statistical Analysis
eFigure 1. Flowchart of Study Cohort
eFigure 2. Association of AI Use With Burnout and Its Components by Subgroups
eFigure 3. Predicted Probability of Burnout for Joint Exposure of AI Use, Workload, and AI Acceptance
eTable 1. Distribution of Participants and Response Rate
eTable 2. Personal and Professional Characteristics Between Included and Excluded Radiologists
eTable 3. Personal and Professional Characteristics after Propensity Score Matching
eTable 4. Weighted Prevalence of Radiologist Burnout Between the AI and Non-AI Groups
eTable 5. Dose-Response Association Between the Frequency of AI Use and Burnout in Radiology Practice by Subgroups
eTable 6. Dose-Response Association Between the Frequency of AI Use and Emotional Exhaustion in Radiology Practice by Subgroups
eTable 7. Dose-Response Association Between the Frequency of AI Use and Depersonalization in Radiology Practice by Subgroups
eTable 8. Joint Association of AI Use, Workload, and AI Acceptance With Emotional Exhaustion
eTable 9. Joint Association of AI Use, Workload, and AI Acceptance With Depersonalization
eTable 10. Association of AI Use With Burnout Adjusting for Workload Factors in Regression Models
eTable 11. Association of AI Use With Burnout by Geographic Locations
Data Sharing Statement


