Abstract
Objective
This study aims to evaluate the efficacy of acupuncture as an adjunct to lifestyle interventions on weight loss in simple obesity.
Methods
Potentially eligible studies that assessed anthropometric outcomes as well as glucose and lipid metabolism following acupuncture combined with lifestyle interventions in simple obesity patients were searched from eight databases from inception to October 2023. All analyses were performed using the Review Manager software v5.4 and Stata software v17.0.
Results
Herein, 25 randomized controlled trials (RCTs) involving 2018 patients were included. Generally, acupuncture combined with lifestyle interventions outperformed lifestyle interventions alone in terms of body weight (MD = −4.73, 95% CI [−6.32, −3.13], p < 0.00001), body mass index (BMI) (MD = −2.11, 95% CI [−2.75, −1.48], p < 0.00001), waist circumference (WC) (MD = −4.96, 95% CI [−6.89, −3.03], p < 0.00001), body fat percentage (BF %) (MD = −2.61, 95% CI [−4,51, −0.71], p = 0.007), fasting plasma glucose (FPG) (SMD = −0.66, 95% CI [−1.02, −0.31], p = 0.0002), fasting serum insulin (FINS) (SMD = −1.12, 95% CI [−1.44, −0.81], p < 0.00001), homeostasis model assessment-insulin resistance (HOMA-IR) (MD = −1.22, 95% CI [−1.50, −0.94], p < 0.00001), total cholesterol (TC) (SMD = −1.14, 95% CI [−1.83, −0.45], p = 0.001), triglyceride (TG) (SMD = −1.31, 95% CI [−2.07, −0.56], p = 0.0006), and low-density lipoprotein cholesterol (LDL-C) (SMD = −1.81, 95% CI [−3.11, −0.51], p = 0.006). Subgroup analysis based on three subgroup variables (types of acupuncture and lifestyle interventions as well as treatment durations) could partially explain the heterogeneity of the results.
Conclusion
Acupuncture demonstrated an enhancing effect on the benefits of lifestyle interventions for weight loss in patients with simple obesity, including reducing body weight and improving glucose and lipid metabolism. This finding suggests its potential value as a complementary therapy alongside lifestyle interventions in a clinical setting. However, further validation with rigorously designed and high-quality RCTs is still needed in the future.
Keywords: obesity, acupuncture, acupuncture therapy, meta-analysis, systematic review
Introduction
The global prevalence of obesity has risen dramatically, becoming a major public health concern. By 2023, estimates indicate that over 1 billion people worldwide were living with obesity.1,2 The prevalence of obesity has also increased among children and adolescents. In China, the prevalence of obesity is approximately 7.9% in adolescents and 16.4% in adults.3 According to the estimates by the World Obesity Atlas, the number of obese people aged over 5 years will achieve nearly 2 billion by 2035, accounting for 24% of the global population.4 As a result, obesity, a major cause of various metabolic diseases like hyperlipidemia, type 2 diabetes mellitus (T2DM), and cardiovascular disease (CVD),5–7 poses a significant challenge to global public health.
Simple obesity is defined as excessive accumulation of body fat due to intake of calorie exceeding the body’s calorie expenditure, without significant endocrine, metabolic disorders, or other etiologies. It accounts for approximately 95% of all obesity cases worldwide.8,9 The negative effects caused by simple obesity are multifaceted. Besides weight gain resulting from increased size and number of adipocytes, simple obesity also leads to disorder in fat metabolism, increasing serum total cholesterol (TC), triglyceride (TG), and low-density lipoprotein cholesterol (LDL-C) as well as cardiovascular and cerebrovascular risks.10,11 In addition, simple obesity can result in insulin resistance (IR), augmenting blood glucose levels.12 Moreover, simple obesity is a well-established independent risk factor for several cancers. It can significantly increase the risk of endometrial cancer, esophageal cancer, and colorectal cancer.13 Owing to its numerous negative consequences, it is imperative to explore effective and safe treatments for simple obesity.
Obesity is caused by the interaction of multiple factors. Among the recognized risk factors, unhealthy diets and sedentary lifestyles contribute to obesity most.3 As a result, lifestyle interventions such as dieting and exercise are the foundation of obesity management, which are proposed as the first-line treatment for obesity in Chinese, American, and European clinical guidelines.14–16 In addition to facilitating weight loss, adjusting unhealthy lifestyle habits through dieting and exercise also helps reduce the risk of other related diseases (such as T2DM, CVD, et al), highlighting their significance in obesity treatment and prevention.17 However, the curative effect of lifestyle interventions alone is gradual and moderate, at least six months of treatment is needed to achieve significant improvements.18,19 Therefore, good self-discipline and perseverance are critical factors to achieving weight loss when lifestyle interventions alone is used. Unfortunately, many people with obesity struggle to lose weight due to challenges with maintaining motivation and adherence to lifestyle changes. This highlights the importance of identifying safe and effective complementary therapies to support lifestyle interventions in obesity management.
Acupuncture, as a traditional Chinese medicine (TCM) therapy, has been widely used in treating many metabolic diseases such as T2DM, metabolic syndrome and polycystic ovary syndrome because of its effectiveness, safety, and economy.20–22 Preclinical studies in animals have shown promise for acupuncture’s effectiveness in weight loss.23 These findings are echoed by numerous clinical trials suggesting acupuncture’s benefit for weight management in patients with simple obesity, either when used alone (monotherapy) or as an adjunct to other therapies.24–30 Moreover, due to the critical involvement of obesity in the onset and progression of T2DM and cardiovascular accidents, studies also explored the effect of acupuncture in regulating abnormal glucose and lipid metabolism in obese patients.31–33 Enforcement effect of acupuncture on restoring blood glucose and lipid index to lifestyle interventions was found, that might be related to the neuro-endocrine-immune regulation by acupuncture.34,35 Besides, the safety and economy of acupuncture was also proved in previous studies, which is much safer and cheaper than the common anti-obesity drugs.25,36 Thus, it is worthwhile to consider incorporating acupuncture into obesity treatment procedures.
Obesity is a complex metabolic disease requiring a multi-pronged approach within management programs, with lifestyle interventions serving as the cornerstone. Acupuncture offers a safe, effective, and cost-effective therapeutic option in this context. Nonetheless, to our knowledge, no reviews have been published regarding the efficacy of acupuncture on weight loss in simple obesity, on the foundation of dieting or exercise. Thus, this study aims to evaluate and elucidate the efficacy of acupuncture as an adjunct to lifestyle interventions in reducing body weight and improving glucose and lipid metabolism in simple obesity. Our results are expected to provide reliable and evidence-based reference for the clinical application of acupuncture in obesity management programs.
Materials and Methods
Protocol and Registration
The protocol was registered on PROSPERO (No. CRD42023474447).
Search Strategy
This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Table S1).37 All eligible studies were searched from four English databases (PubMed, EMBASE, Web of Science and the Cochrane Library) and four Chinese databases (the Chinese Biomedical Literature Database, China National Knowledge Infrastructure, Wanfang, and the VIP Database) from inception to October 2023. Clinical condition (simple obesity and obesity), intervention methods (acupuncture, body acupuncture, manual acupuncture, and electro-acupuncture), and study type (randomized clinical trial) were used as the search terms in both the Chinese and English databases. Table S2 outlines the complete search strategy.
Inclusion and Exclusion Criteria
Study Type
All randomized controlled trials (RCTs) on acupuncture therapies combined with lifestyle interventions for simple obesity treatment were included. On the other hand, non-randomized clinical studies, animal experiments, conference papers, review papers, and case reports were excluded.
Types of Participants
Studies that involved participants diagnosed with simple obesity using any recognized diagnostic criteria were eligible for inclusion regardless of gender, age, and ethnic group.
Interventions and Comparisons
Studies with trial groups treated with acupuncture therapies [manual acupuncture (MA) or electro-acupuncture (EA)] combined with lifestyle interventions (dieting, exercise, or dieting plus exercise) regardless of the treatment duration and frequency, and control groups treated with lifestyle interventions alone or in combination with sham acupuncture (placebo) were included.
Outcomes
Primary outcomes were body weight and body mass index (BMI). Secondary outcomes included the following four indicators:
Anthropometric outcomes: waist circumference (WC) and body fat percentage (BF %).
Glucose metabolism: fasting plasma glucose (FPG), fasting serum insulin (FINS) and homeostasis model assessment-insulin resistance (HOMA-IR).
Lipid metabolism: TC, TG, high-density lipoprotein cholesterol (HDL-C) and LDL-C.
Adverse events (AEs): severe needle pain, bleeding, subcutaneous hematoma, fainting, and so on.
Study Selection and Data Extraction
Two researchers independently screened the literature. The studies failing to meet the inclusion criteria were excluded by evaluating the title, abstract, and full text. The studies finally included were determined through crosschecking, and a third-party reviewer were engaged in discussing and achieving consensus on differences. Two researchers independently extracted information from the literature into a predesigned form. The form contained general characteristics (first author, publication year, country, and sample size), characteristics of participants (age and BMI), traits of the intervention and control groups (dose of acupuncture, treatment duration, and follow-up time), and outcomes (Table S3).
Risk of Bias Assessment
Two researchers independently evaluated the risk of bias of the included studies using the Cochrane risk of bias tool.38 The domains assessed included sequence generation, allocation concealment, blinding of participants, blinding of outcome assessors, incomplete outcome data, selective outcome reporting, and other sources of bias. The risk of bias in the literature was rated as “low”, “high”, and “uncertain”. A third researcher assisted in the judgment in case of a disagreement.
Certainty Assessment
The quality of each piece of evidence was evaluated using the GRADE guideline (Grading of Recommendations Assessment, Development, and Evaluation).39 Five factors that can reduce the quality of evidence include risk of bias, inconsistency, indirectness, imprecision, and publication bias. By evaluating these factors, the quality of evidence is divided into four levels including high, moderate, low, and very low.
Statistical Analysis
Statistical analysis was performed using the Review Manager software v5.4 and Stata software v17.0. Continuous data were summarized as mean differences (MD) or standardized mean difference (SMD) with 95% confidence intervals (CIs). The inter-study heterogeneity was assessed using I2 statistics. The fixed-effect model was used when p ≥ 0.1 and I2 ≤ 50%. Otherwise, the random-effect model was applied. In case of notable heterogeneity, sensitivity analysis was performed on all studies for detailed examination. Additionally, subgroup analysis was conducted to explore the potential effect modifiers (eg duration of intervention) and heterogeneity sources, that required at least 2 RCTs in each subgroup. Furthermore, publication bias was evaluated through funnel plot and Egger’s test.
Results
Study Identification
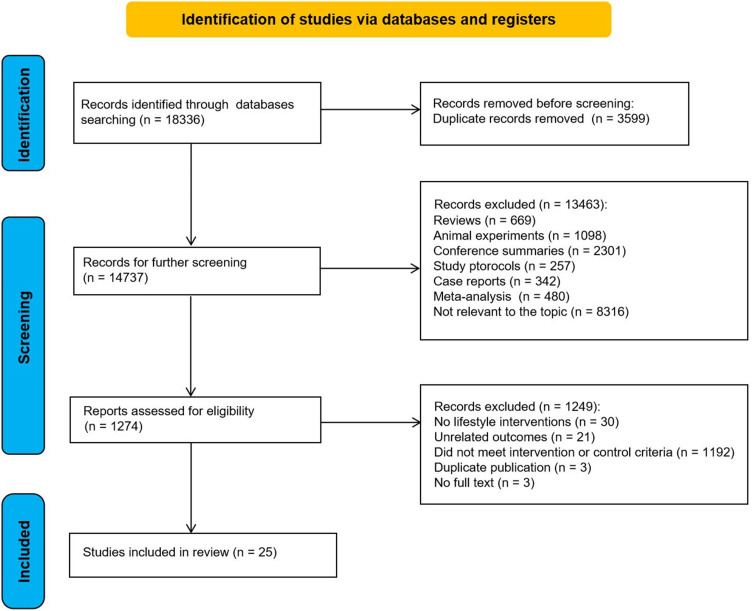
The search strategy yielded 18336 studies. After importing all studies into Endnote X9 and removing duplicates (14737 remained), we screened titles and abstracts. This process yielded 1274 studies for full-text assessment, and ultimately, 25 studies were included in the meta-analysis (Figure 1).
Figure 1.
PRISMA flowchart for literature screening.
Study Characteristics
Table 1 summarizes the characteristics of the included RCTs. The 25 RCTs involving 2018 patients were conducted in China, Malta, South Korea, Australia, Sudan and Iran. The sample sizes of these RCTs published between 2005 and 2023 range from 42 to 240 participants. All control groups received lifestyle interventions, such as dieting, exercise, or a combination of both. Moreover, some control groups received sham acupuncture. Besides, in addition to lifestyle interventions, the trial groups were treated with MA in 12 RCTs,40–51 and with EA in the other studies.52–64 Regarding the treatment duration, 18 RCTs and 7 RCTs lasted short-term40–44,48,52–63 and long-term45–47,49–51,64 (≤ 8 weeks and > 8 weeks), respectively. Except for 3 RCTs,56,59,60 most of the included RCTs did not report follow-up data. Body weight, BMI, WC, BF %, FPG, FINS, HOMA-IR, TC, TG, HDL-C, LDL-C, and AEs were the outcomes considered in the meta-analysis.
Table 1.
Study Characteristics
| Study | Country | Sample Size (n) | Age (Year) | BMI (kg / m2) | Treatment Regimen | Dose of Acupuncture | Treatment Duration | Follow-Up time | Outcomes | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T/C | T | C | T | C | T | C | ||||||
| Tong et al, 201140 | China | 76/42 | 35.08±9.31 | 34.60±8.55 | 30.42±2.94 | 31.41±3.12 | (1) + (4) | (6) | 15 acupoints | 5 weeks | NA | (b) (e) (h) (i) (l) |
| Liang, 201341 | China | 30/30 | 39.70 ± 3.59 | 37.50 ± 5.15 | 30.45 ± 3.25 | 28.32 ± 4.22 | (1) + (4) | (4) | 6 acupoints | 22 days | NA | (a) (b) (f) |
| Zhang and Wu, 201642 | China | 120/120 | 36.9 ± 9.86 | 38.8 ± 10.68 | 29.68 ± 0.56 | 29.80 ± 0.6 | (1) + (3) | (3) | 9 acupoints | 8 weeks | NA | (b) (c) (d) (h) (i) (k) (l) |
| Li et al, 201743 | Susan | 40/30 | 30.5±6.8 | 31.6±7.5 | 30.45±2.13 | 31.26±2.09 | (1) + (5) | (5) | 8 acupoints | 4 weeks | NA | (b) |
| Li et al, 201944 | Australia | 30/30 | 35.92±13.36 | 37.84±13.90 | 28.53±3.52 | 27.77±4.07 | (1) + (5) | (5) | 9 acupoints | 6 weeks | NA | (a) (b) (c) |
| Liu et al, 202145 | China | 46/47 | 43.9 ± 10.2 | 43.6 ± 8.8 | 30.46 ± 1.53 | 30.19 ± 1.36 | (1) + (3) | (3) | 7 acupoints | 3 months | NA | (b) (d) (e) (f) (g) (h) (i) |
| Min, 202146 | South Korea | 33/33 | 18–60 | 18–60 | 26.895±1.9369 | 27.093±4.0498 | (1) + (3) | (3) | 5 acupoints | 16 weeks | NA | (a) (b) (c) (l) |
| Zhang et al, 202147 | China | 30/30 | 39.13 ± 9.97 | 34.66 ± 9.87 | 31.63 ± 4.75 | 31.41 ± 2.43 | (1) + (3) | (3) | 3 acupoints | 3 months | NA | (b) (d) |
| Bi, 202248 | China | 35/35 | 36.71±10.18 | 36.43±9.81 | 29.29±1.10 | 29.87±1.64 | (1) + (3) | (3) | 15 acupoints | 8 weeks | NA | (a) (b) (c) (d) (h) (i) (j) (k) (l) |
| Qi and Shi, 202249 | Malta | 35/35 | 46.89±4.42 | 49.06±8.80 | 33.01±2.35 | 33.57±2.88 | (1) + (3) | (3) | 6 acupoints | 12 weeks | NA | (a) (b) (c) (d) (h) (i) (k) |
| Jia et al, 202350 | China | 40/40 | 37.2 ± 1.2 | 36.2 ± 3.2 | 28.73 ± 1.23 | 28.81 ± 1.18 | (1) + (3) | (3) | 8 acupoints | 10 weeks | NA | (a) (b) (c) (h) (i) (j) (k) |
| Yang et al, 202351 | China | 47/47 | 34.37±7.66 | 33.47±8.18 | 30.58±4.91 | 29.26±4.59 | (1) + (3) | (7) | 16 acupoints | 12 weeks | NA | (a) (b) (c) |
| Li, 200552 | China | 35/33 | 38.97±10.88 | 40.09±11.37 | NR | NR | (2) + (3) | (3) | 8 acupoints | 4 weeks | NA | (a) (c) (d) (h) (i) (j) |
| Luo, 200753 | China | 30/30 | 17–55 | 20–54 | 27.9 | 27.5 | (2) + (4) | (4) | 10 acupoints | 2 months | NA | (h) (i) (j) (k) |
| Xing, 200954 | China | 31/30 | 28.16±7.17 | 28.37±7.13 | 27.83 ± 1.59 | 27.91 ± 1.47 | (2) + (3) | (3) | 10 acupoints | 51 days | NA | (a) (b) (h) (i) (j) (k) |
| Zhao and Shi, 201055 | China | 30/30 | 29.31 ± 8.28 | 30.30 ± 10.41 | 29.09 ± 3.64 | 27.84 ± 3.50 | (2) + (3) | (3) | 14 acupoints | 8 weeks | NA | (a) (b) (c) |
| Abdi et al, 201256 | Iran | 79/82 | 36.88±0.98 | 37.41±1.01 | 32.30±0.52 | 32.74±0.59 | (1) + (4) | (6) | 10 acupoints | 6 weeks | 6 weeks | (a) (b) (c) (d) (e) (h) (i) (j) (k) |
| Wang and Xiao, 201457 | China | 45/45 | 48.8±3.5 | 49.4±3.9 | 30.1±2.2 | 29.8±2.0 | (2) + (3) | (3) | 12 acupoints | 30 days | NA | (a) (b) (d) (l) |
| Bae, 201658 | China | 30/30 | 32.97±8.032 | 29.33±7.485 | 29.363±3.222 | 30.417±4.564 | (2) + (4) | (4) | 19 acupoints | 1 month | NA | (a) (b) (c) (d) |
| Xue et al, 201859 | China | 37/38 | 39.54 ± 6.96 | 36.47 ± 7.65 | 34.59 ± 6.96 | 33.61 ± 4.19 | (2) + (3) | (3) | 10 acupoints | 8 weeks | 3 months | (a) (b) (l) |
| Yin et al, 201860 | China | 43/43 | 34.08±9.68 | 33.81±7.57 | 31.08±9.65 | 30.61±6.05 | (2) + (3) | (3) | 10 acupoints | 8 weeks | 3 months | (a) (b) |
| Wang, 202061 | China | 31/11 | 18–45 | 18–45 | 28.84 ± 2.67 | 28.75 ± 3.23 | (2) + (4) | (4) | 7 acupoints | 5 weeks | NA | (a) (b) (c) (l) |
| Zheng et al, 202162 | China | 30/30 | 35.65 ± 7.84 | 35.65 ± 7.81 | 28.00 ± 0.72 | 26.32 ± 0.39 | (2) + (3) | (3) | 12 acupoints | 4 weeks | NA | (h) (i) (j) (k) |
| Liang, 202263 | China | 30/30 | 37.00 ± 7.82 | 34.80 ± 8.35 | 28.00 ± 2.55 | 28.37 ± 3.08 | (2) + (3) | (3) | 13 acupoints | 8 weeks | NA | (b) (c) (l) |
| Ni et al, 202264 | China | 28/26 | 30.79 ± 8.8 | 30.50 ± 9.53 | 30.37 ± 4.75 | 31.12 ± 4.94 | (2) + (3) | (3) | 13 acupoints | 12 weeks | NA | (a) (b) (c) (e) (f) (g) |
Notes: (1) Manual acupuncture; (2) Electro-acupuncture; (3) Dieting and exercise; (4) Dieting; (5) Exercise; (6) Sham acupuncture and dieting; (a) Body weight.
Abbreviations: C, control group; NA, not available; T, trial group; (b) BMI, body mass index; (c) WC, waist circumference; (d) BF %, body fat percentage; (e) FPG, fasting plasma glucose; (f) FINS, fasting serum insulin; (g) HOMA-IR, homeostasis model assessment-insulin resistance; (h) TC, total cholesterol; (i) TG, triglyceride; (j) HDL-C, high-density lipoprotein cholesterol; (k) LDL-C, low-density lipoprotein cholesterol; (l) Adverse events.
Risk of Bias
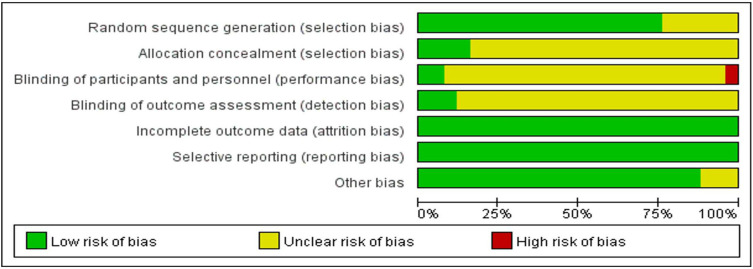
Figure 2 depicts the risk of bias in all the included studies. Based on the applied quality criteria, methodological weaknesses were noted in most of the included RCTs. Regarding selection bias, 19 RCTs40,41,43–48,50,51,53–55,57,60,62–64 utilized random allocation but only 4 RCTs54,55,61,63 mentioned allocation concealment. The blinding of participants and personnel was not mentioned in most studies (except in 3 RCTs40,54,61), indicating an unclear risk of bias. Similarly, only 3 RCTs reported blinding of outcome assessments.40,61,64 However, a low risk of bias was observed in the ‘other bias’ category for 22 RCTs.40–48,50–54,56–60,62–64
Figure 2.
Risk of bias graph.
Outcome Measurements
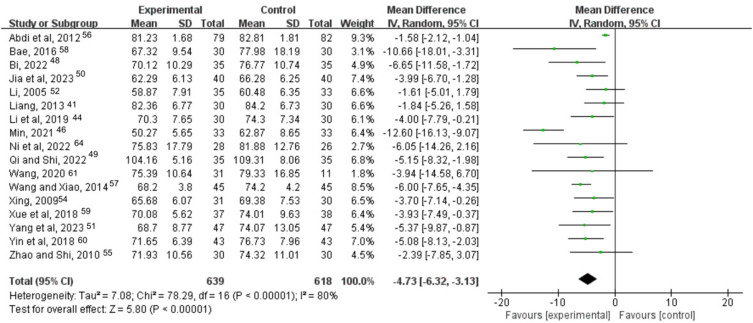
Body Weight
Seventeen studies recorded body weight of participants.41,44,46,48–52,54–61,64 High heterogeneity was found among them (I2 = 80%, p < 0.00001). The random effects model revealed that acupuncture in combination with lifestyle interventions exerted a synergetic effect in decreasing body weight (MD = −4.73, 95% CI [−6.32, −3.13], p < 0.00001) (Figure 3).
Figure 3.
Forest plot of acupuncture combined with lifestyle interventions vs lifestyle interventions on body weight.
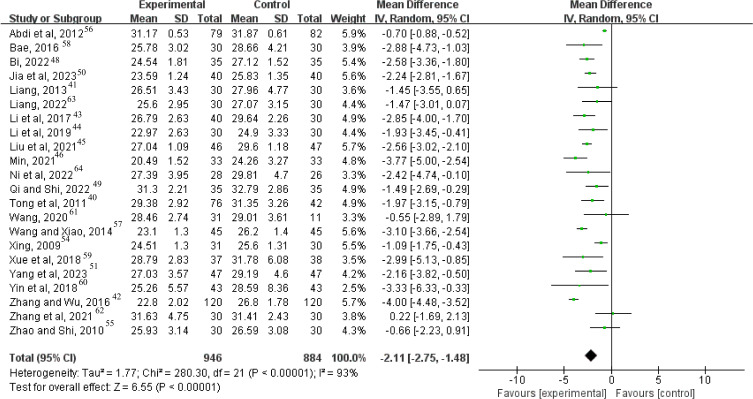
BMI
Twenty-two studies reported BMI.40–51,54–61,63,64 A random-effect model was applied due to their significant heterogeneity (I2 = 93%, p < 0.00001). Compared to lifestyle interventions alone, acupuncture combined with lifestyle interventions exerted better effects in reducing BMI (MD = −2.11, 95% CI [−2.75, −1.48], p < 0.00001) (Figure 4).
Figure 4.
Forest plot of acupuncture combined with lifestyle interventions vs lifestyle interventions on BMI.
Abbreviation: BMI, body mass index.
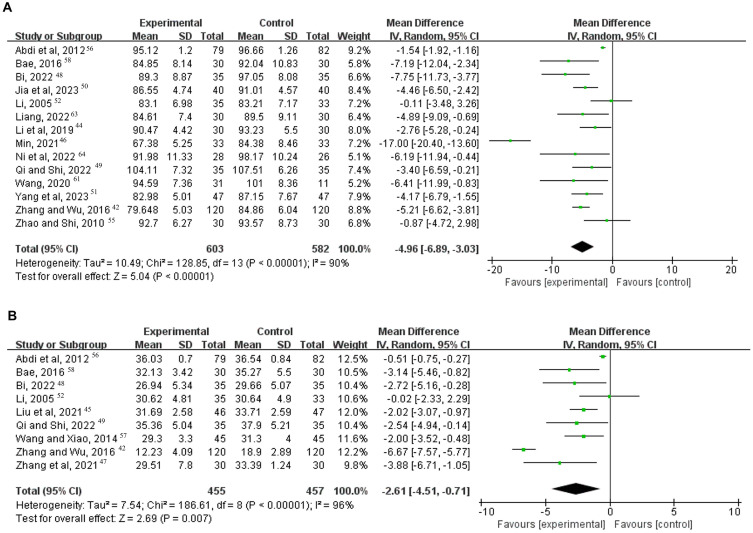
WC
Fourteen studies compared the combination of acupuncture and lifestyle interventions (case group) to lifestyle interventions alone (control group) in obesity treatment using WC as an outcome.42,44,46,48–52,55,56,58,61,63,64 The included studies had high heterogeneity (I2 = 90%, p < 0.00001). This meta-analysis found that acupuncture in conjunction with lifestyle interventions effectively reduced the WC (MD = −4.96, 95% CI [−6.89, −3.03], p < 0.00001; Figure 5A).
Figure 5.
Forest plot of acupuncture combined with lifestyle interventions vs lifestyle interventions on: (A) WC; (B) BF %.
Abbreviations: BF %, body fat percentage; WC, waist circumference.
BF %
Nine studies reported BF % data.42,45,47–49,52,56–58 A random-effect model was used (I2 = 96%, p < 0.00001). Compared to lifestyle interventions alone, acupuncture plus lifestyle interventions exerted a positive effect on BF % (MD = −2.61, 95% CI [−4.51, −0.71], p = 0.007) (Figure 5B).
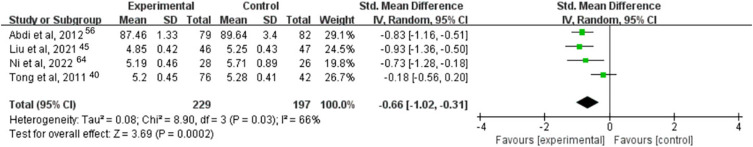
FPG
Only four studies reported FPG data,40,45,56,64 while high heterogeneity was found between them (I2 = 66%, p = 0.03). The results indicated a significant difference in FPG reduction between the trial and control groups (SMD = −0.66, 95% CI [−1.02, −0.31], p = 0.0002) (Figure 6).
Figure 6.
Forest plot of acupuncture combined with lifestyle interventions vs lifestyle interventions on FPG.
Abbreviation: FPG, fasting plasma glucose.
FINS and HOMA-IR
Three studies41,45,64 and two studies45,64 compared the combination of acupuncture with lifestyle interventions against lifestyle interventions only in terms of changes in FINS and HOMA-IR, respectively. The fixed effects model was used due to the homogeneity of the results (I2 = 12%, p = 0.32; I2 = 6%, p = 0.30). Compared to lifestyle interventions alone, acupuncture, used as a supplementary method, significantly reduced FINS (SMD = −1.12, 95% CI [−1.44, −0.81], p < 0.00001) (Figure 7A) and HOMA-IR (MD = −1.22, 95% CI [−1.50, −0.94], p < 0.00001) (Figure 7B).
Figure 7.
Forest plot of acupuncture combined with lifestyle interventions vs lifestyle interventions on: (A) FINS; (B) HOMA-IR.
Abbreviations: FINS, fasting serum insulin; HOMA-IR, homeostasis model assessment-insulin resistance.
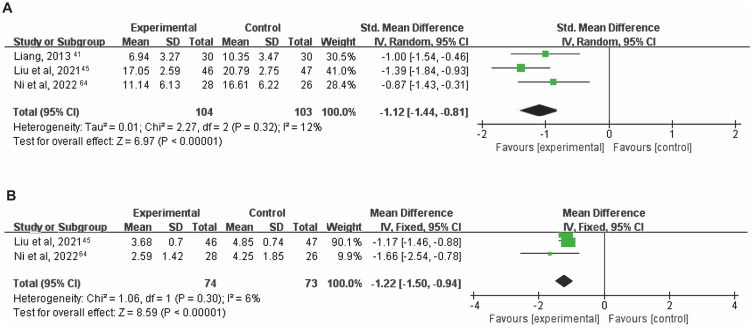
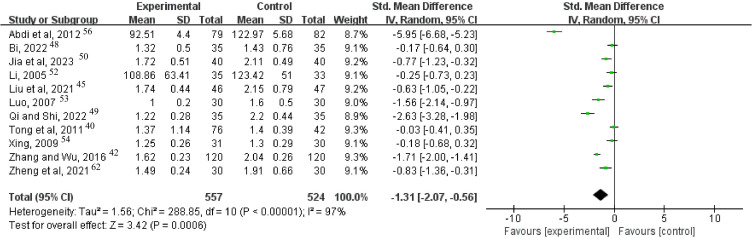
TC and TG
Eleven studies reported TC and TG data.40,42,45,48–50,52–54,56,62 High heterogeneity was detected in TC (I2 = 96%, p < 0.00001) and TG (I2 = 97%, p < 0.00001). According to the results, acupuncture in conjunction with lifestyle interventions is beneficial in reducing TC (SMD = −1.14, 95% CI [−1.83, −0.45], p = 0.001) (Figure 8) and TG (SMD = −1.31, 95% CI [−2.07, −0.56], p = 0.0006) (Figure 9).
Figure 8.
Forest plot of acupuncture combined with lifestyle interventions vs lifestyle interventions on TC.
Abbreviation: TC, total cholesterol.
Figure 9.
Forest plot of acupuncture combined with lifestyle interventions vs lifestyle interventions on TG.
Abbreviation: TG, triglyceride.
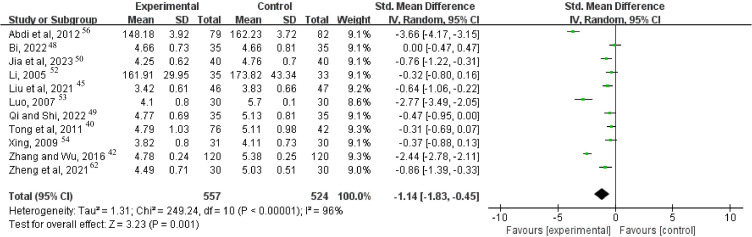
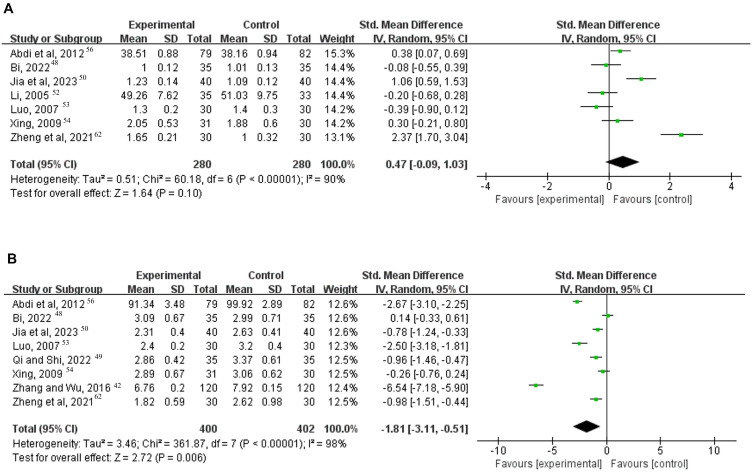
HDL-C and LDL-C
Seven studies48,50,52–54,56,62 and eight studies42,48–50,53,54,56,62 reported changes in HDL-C and LDL-C, respectively. And significant heterogeneity was found in HDL-C (I2 = 90%, p < 0.00001) and LDL-C (I2 = 98%, p < 0.00001). The analysis confirmed that acupuncture plus lifestyle interventions was not superior to lifestyle interventions alone in increasing HDL-C (SMD = 0.47, 95% CI [−0.09, 1.03], p = 0.10) (Figure 10A), whereas reducing LDL-C (SMD = −1.81, 95% CI [−3.11, −0.51], p = 0.006) (Figure 10B).
Figure 10.
Forest plot of acupuncture combined with lifestyle interventions vs lifestyle interventions on: (A) HDL-C; (B) LDL-C.
Abbreviations: HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.
Adverse Events
Only eight studies reported AEs.40,42,46,48,57,59,61,63 Five studies reported no AEs.40,46,48,57,59 Three studies reported mild AEs,42,61,63 most of which were subcutaneous hematoma. All subjects fully recovered from AEs and completed the trial.
Subgroup Analysis
To further investigate the results, we conducted a subgroup analysis considering different types of acupuncture, lifestyle interventions, and treatment durations. In terms of acupuncture methods, both MA and EA, when combined with lifestyle interventions, exerted positive effects on body weight (MD = −5.60, 95% CI [−8.21, −2.99], p < 0.0001; MD = −3.99, 95% CI [−5.89, −2.09], p < 0.0001), BMI (MD = −2.41, 95% CI [−2.99, −1.83], p < 0.00001; MD = −1.80, 95% CI [−2.69, −0.92], p < 0.0001), and WC (MD = −6.23, 95% CI [−9.04, −3.42], p < 0.0001; MD = −3.05, 95% CI [−5.00, −1.10], p = 0.002), compared to lifestyle interventions alone. Regarding the effect on FPG, TC and LDL-C, EA combined with lifestyle interventions was superior to lifestyle interventions alone (SMD = −0.81, 95% CI [−1.09, −0.53], p < 0.00001; SMD = −1.59, 95% CI [−2.95, −0.23], p = 0.02; SMD = −1.60, 95% CI [−2.81, −0.39], p = 0.009). And MA in conjunction with lifestyle interventions is beneficial in reducing BF % and TG (MD = −3.62, 95% CI [−6.09, −1.15], p = 0.004; SMD = −0.97, 95% CI [−1.69, −0.26], p = 0.008) (Table 2 and Figures S1-S8).
Table 2.
Subgroup Analysis of Different Acupuncture Interventions
| Type of Acupuncture Interventions | Study (n) | Case (n) | MD/SMD 95% CI | p | I2 (%) | Model |
|---|---|---|---|---|---|---|
| Manual acupuncture | ||||||
| Body weight | 7 | 500 | −5.60 [−8.21, −2.99] | <0.0001 | 73 | Random |
| BMI | 12 | 1081 | −2.41 [−2.99, −1.83] | <0.00001 | 78 | Random |
| WC | 7 | 680 | −6.23 [−9.04, −3.42] | <0.0001 | 89 | Random |
| BF % | 5 | 533 | −3.62 [−6.09, −1.15] | 0.004 | 92 | Random |
| FPG | 2 | 211 | −0.55 [−1.29, 0.19] | 0.14 | 85 | Random |
| TC | 6 | 671 | −0.78 [−1.57, 0.01] | 0.05 | 95 | Random |
| TG | 6 | 671 | −0.97 [−1.69, −0.26] | 0.008 | 94 | Random |
| LDL-C | 4 | 460 | −2.03 [−4.55, 0.50] | 0.12 | 99 | Random |
| Electro-acupuncture | ||||||
| Body weight | 10 | 757 | −3.99 [−5.89, −2.09] | <0.0001 | 75 | Random |
| BMI | 10 | 749 | −1.80 [−2.69, −0.92] | <0.0001 | 88 | Random |
| WC | 7 | 505 | −3.05 [−5.00, −1.10] | 0.002 | 56 | Random |
| BF % | 4 | 379 | −1.25 [−2.47, −0.02] | 0.05 | 65 | Random |
| FPG | 2 | 215 | −0.81 [−1.09, −0.53] | <0.00001 | 0 | Random |
| TC | 5 | 410 | −1.59 [−2.95, −0.23] | 0.02 | 97 | Random |
| TG | 5 | 410 | −1.74 [−3.48, −0.00] | 0.05 | 98 | Random |
| LDL-C | 4 | 342 | −1.60 [−2.81, −0.39] | 0.009 | 95 | Random |
Notes: The random-effect model was used for the analysis of all indicators to make the results more reliable.
Abbreviations: CI, confidence interval; MD, mean difference; SMD, standard mean difference.
Acupuncture showed a consistent additional effect on body weight (MD = −2.88, 95% CI [−5.07, −0.70], p = 0.010; MD = −5.22, 95% CI [−6.74, −3.69], p < 0.00001), BMI (MD = −1.75, 95% CI [−2.67, −0.84], p = 0.0002; MD = −2.30, 95% CI [−2.88, −1.72], p < 0.00001), and WC (MD = −3.38, 95% CI [−5.75, −1.01], p = 0.005; MD = −5.36, 95% CI [−7.84, −2.89], p < 0.0001) compared to other lifestyle approaches, including diet alone, exercise alone, or both combined. The difference was dieting or exercise alone showed no statistical significance in BF %, FPG, TC and TG while combination dieting and exercise showed no statistical significance in LDL-C (Table 3 and Figures S9-S16).
Table 3.
Subgroup Analysis of Different Lifestyle Interventions
| Type of Lifestyle Interventions | Study (n) | Case (n) | MD/SMD 95% CI | p | I2 (%) | Model |
|---|---|---|---|---|---|---|
| Dieting or exercise alone | ||||||
| Body weight | 5 | 383 | −2.88 [−5.07, −0.70] | 0.010 | 47 | Random |
| BMI | 7 | 571 | −1.75 [−2.67, −0.84] | 0.0002 | 76 | Random |
| WC | 4 | 323 | −3.38 [−5.75, −1.01] | 0.005 | 66 | Random |
| BF % | 2 | 221 | −1.56 [−4.09, 0.96] | 0.23 | 80 | Random |
| FPG | 2 | 279 | −0.52 [−1.16, 0.12] | 0.11 | 85 | Random |
| TC | 3 | 339 | −2.24 [−4.52, 0.04] | 0.05 | 98 | Random |
| TG | 3 | 339 | −2.50 [−5.67, 0.67] | 0.12 | 99 | Random |
| LDL-C | 2 | 221 | −2.62 [−2.99, −2.26] | <0.00001 | 0 | Random |
| Combination of dieting and exercise | ||||||
| Body weight | 12 | 874 | −5.22 [−6.74, −3.69] | <0.00001 | 57 | Random |
| BMI | 15 | 1259 | −2.30 [−2.88, −1.72] | <0.00001 | 83 | Random |
| WC | 10 | 862 | −5.36 [−7.84, −2.89] | <0.0001 | 86 | Random |
| BF % | 7 | 691 | −2.89 [−4.94, −0.83] | 0.006 | 91 | Random |
| FPG | 2 | 147 | −0.86 [−1.20, −0.52] | <0.00001 | 0 | Random |
| TC | 8 | 742 | −0.74 [−1.37, −0.11] | 0.02 | 94 | Random |
| TG | 8 | 742 | −0.89 [−1.43, −0.34] | 0.002 | 91 | Random |
| LDL-C | 6 | 581 | −1.55 [−3.21, 0.10] | 0.07 | 98 | Random |
Notes: The random-effect model was used for the analysis of all indicators to make the results more reliable.
For treatment durations, there were significant reductions after short- and long-term acupuncture (≤8 weeks and >8 weeks, respectively) in body weight (MD = −3,88, 95% CI [−5.49, −2.27], p < 0.00001; MD = −6.66 95% CI [−10.12, −3.20], p = 0.0002), BMI (MD = −2.10, 95% CI [−2.96, −1.25], p < 0.00001; MD = −2.23, 95% CI [−2.86, −1.61], p < 0.00001), WC (MD = −3.72, 95% CI [−5.55, −1.89], p < 0.0001; MD = −7.00, 95% CI [−11.69, −2.31], p = 0.003), TC (SMD = −1.34, 95% CI [−2.28, −0.39], p = 0.006; MD = −0.63, 95% CI [−0.89, −0.37], p < 0.00001), TG (SMD = −1.31, 95% CI [−2.31, −0.32], p = 0.010; SMD = −1.32, 95% CI [−2.39, −0.24], p = 0.02) and LDL-C (SMD = −2.13, 95% CI [−3.91, −0.35], p = 0.02; SMD = −0.87, 95% CI [−1.20, −0.53], p < 0.00001). Furthermore, after long-term acupuncture (>8 weeks), acupuncture assisted lifestyle interventions was superior to lifestyle interventions alone in reducing BF % (MD = −2.29, 95% CI [−3.20, −1.38], p < 0.00001) and FPG (SMD = −0.86, 95% CI [−1.20, −0.52], p < 0.00001) (Table 4 and Figures S17-S24). In the subgroup analysis, we found that a specific type of acupuncture, lifestyle intervention, or treatment duration may be the source of high heterogeneity.
Table 4.
Subgroup Analysis of Different Treatment Durations
| Treatment Duration | Study (n) | Case (n) | MD/SMD 95% CI | p | I2 (%) | Model |
|---|---|---|---|---|---|---|
| ≤8 weeks | ||||||
| Body weight | 12 | 893 | −3.88 [−5.49, −2.27] | <0.00001 | 72 | Random |
| BMI | 15 | 1313 | −2.10 [−2.96, −1.25] | <0.00001 | 94 | Random |
| WC | 9 | 821 | −3.72 [−5.55, −1.89] | <0.0001 | 82 | Random |
| BF % | 6 | 689 | −2,53 [−5.28, 0.21] | 0.07 | 97 | Random |
| FPG | 2 | 279 | −0.52 [−1.16, 0.12] | 0.11 | 85 | Random |
| TC | 8 | 838 | −1.34 [−2.28, −0.39] | 0.006 | 97 | Random |
| TG | 8 | 838 | −1.31 [−2.31, −0.32] | 0.010 | 97 | Random |
| LDL-C | 6 | 652 | −2.13 [−3.91, −0.35] | 0.02 | 99 | Random |
| >8 weeks | ||||||
| Body weight | 5 | 364 | −6.66 [−10.12, −3.20] | 0.0002 | 75 | Random |
| BMI | 7 | 517 | −2.23 [−2.86, −1.61] | <0.00001 | 60 | Random |
| WC | 5 | 364 | −7.00 [−11.69, −2.31] | 0.003 | 91 | Random |
| BF % | 3 | 223 | −2.29 [−3.20, −1.38] | <0.00001 | 0 | Random |
| FPG | 2 | 147 | −0.86 [−1.20, −0.52] | <0.00001 | 0 | Random |
| TC | 3 | 243 | −0.63 [−0.89, −0.37] | <0.00001 | 0 | Random |
| TG | 3 | 243 | −1.32 [−2.39, −0.24] | 0.02 | 93 | Random |
| LDL-C | 2 | 150 | −0.87 [−1.20, −0.53] | <0.00001 | 0 | Random |
Notes: The random-effect model was used for the analysis of all indicators to make the results more reliable.
Sensitivity Analysis
Regarding body weight and BMI, after any study was excluded, the range of change in MD are similar to the combined MD. Similarly, in terms of FPG, TC, and TG, the range of change in SMD is similar to that in the combined SMD. This indicated that each single study did not significantly affect the results, confirming the stability of the research findings. In spite of heterogeneity, the pooled result on these indicators was reliable. The results also showed that Min’s study may be the source of the heterogeneity in WC.46 And the study by Zhang and Wu may have contributed to the heterogeneity in BF % and LDL-C levels.42 When these two studies were excluded from the analysis, the range of change in SMD of the remaining studies are like the combined SMD in WC, BF % and LDL-C. Therefore, the interpretation of the results should be cautious. The details are in Tables S4-S10.
Publication Bias
More than 10 studies in each aspect of body weight, BMI, WC, TC, and TG were included. Funnel plot (Figures S25-S29) and Egger’s test were used for publication bias assessment. The results indicated that it showed asymmetry in terms of body weight and WC in funnel plot. Furthermore, their results in Egger’s test also suggested a significant publication bias between studies (p = 0.005 and p = 0.014, respectively). Despite the poor symmetry of the funnel plot, the results of Egger’s test showed that no significant publication bias in BMI, TC and TG (p = 0.051; p = 0.967; p = 0.266).
Grading the Evidence
GRADE pro 3.6 software was used to assess the quality of evidence for all outcome indicators. The result indicated that the evidence for FPG, FINS and HOMA-IR were low quality, while the body weight, BMI, WC, BF %, TC, TG, HDL-C and LDL-C were very low quality (Table S11).
Discussion
Given its heavy burden on patients and society, obesity has become a global public health concern. Abnormal glucose and lipid metabolism are the main characteristic features of obesity that closely associated with some serious consequences like CVD.65,66 Effective obesity management in obese patients goes beyond weight loss and must also address associated metabolic abnormalities due to the complex nature of the condition. Lifestyle interventions, therefore, serve as the foundation of a multi-component treatment approach. Building on prior research suggesting acupuncture benefits obese patients,31–33 this study investigated its efficacy as an adjunct to lifestyle interventions for obesity treatment. We specifically focused on weight loss and its impact on glucose and lipid metabolism.
Summary of the Results
This meta-analysis is the first to evaluate the efficacy of acupuncture as an adjunct to lifestyle interventions for weight loss in simple obesity. In this study, we investigated the effectiveness of acupuncture when combined with lifestyle interventions, compared to lifestyle interventions alone. Results indicated that addition of acupuncture caused significant improvements in body weight, BMI, WC, BF %, FPG, FINS, HOMA-IR, TC, TG, and LDL-C. Importantly, acupuncture was associated with rare, mild, and self-resolving side effects.
Regarding weight loss, some studies reported that acupuncture might adjust appetite-regulating hormones, such as ghrelin and leptin, inducing a reduction in appetite among obese patients.67,68 Some appetite-related neurotransmitters, such as proopiomelanocortin, neuropeptide Y, agouti-related protein and the anorexigenic a-MSH peptide, were also found to be related to the effect of acupuncture on weight loss.69,70 Besides, one of acupuncture treatment mechanisms for obesity may be the regulation of inflammatory factors.71,72 Previous studies suggested that acupuncture may upregulate anti-inflammatory cytokines and downregulate pro-inflammatory cytokines. These abnormalities in cytokine regulation are thought to underlie the inflammatory mechanisms of obesity.34,73
The benefits of acupuncture on glucose metabolism could be explained by the increase of whole-body glucose uptake induced by the activation of the parasympathetic and sympathetic nervous systems.34 Besides, IR, a key mechanism of glucose metabolism imbalance, is a common pathological state in obese patients,74,75 which could be reversed through acupuncture.76 Previous research also demonstrated the regulatory effect of acupuncture on lipid metabolism, including lipid decomposition, adipogenesis inhibition, and modulation of β- endorphins and leptin secretion.34,77–79
Despite our promising results, we observed high heterogeneity in some indicators, including body weight, BMI, WC, BF %, FPG, TC, TG and LDL-C. We conducted the subgroup analysis and sensitivity analysis to thoroughly investigate potential sources of heterogeneity. The results of subgroup analysis indicated that different types of acupuncture (MA and EA) and lifestyle interventions (dieting or exercise alone, and dieting plus exercise), and different treatment durations (≤8 weeks and > 8 weeks) could partially explain the heterogeneity between studies. Based on these results, clinicians can select long-term treatment (>8 weeks) of EA assisting dieting and exercise intervention to help patients with simple obesity lose weight and improve glucose and lipid metabolism. However, personalized treatment plans still need to be developed based on the physique and condition of patients in clinical practice.
The results of sensitivity analysis demonstrated that the pooled result had been proven to be reliable despite its heterogeneity in terms of body weight, BMI, FPG, TC, and TG. The variation likely stems from methodological flaws, such as differences in diagnostic criteria for simple obesity or variations in acupuncture parameters used across studies. However, it is important to note that these variations did not appear to influence the observed positive effect of acupuncture on these indicators. Besides, regarding of BF % and LDL-C, Zhang’s study may be the cause for high heterogeneity.42 The diagnostic criteria and TCM syndrome types for simple obesity differed from other studies in this research. And the application of midnight-noon ebb-flow acupuncture method in Min’s study is a specific operation method of acupoint selection according to syndrome differentiation and meridian to treat obesity,46 which may be the source of heterogeneity for WC.
Applying the GRADE approach, the certainty of the evidence on the impact of acupuncture-assisted lifestyle interventions on weight loss in obese patients was very low. The quality of evidence for BMI and BF % was downgraded due to serious risks of bias and inconsistency, while for body weight and WC, publication bias further limited the certainty. Regarding glucose metabolism, the credibility of the evidence was low due to serious risks of bias, inconsistency, or imprecision. Additionally, the certainty of evidence for the impact on lipid metabolism was lowered to very low due to severe limitations from publication bias and inconsistency. Therefore, more high-quality RCTs are needed in this field to provide more solid evidence.
Our findings also found the common deficiencies of the RCTs of acupuncture on obesity in methodology. For instance, most of the included RCTs failed to report allocation concealment method, selective bias was unclear. Another potential limitation to consider is performance bias. Only four of the included RCTs mentioned implementing blinding procedures. This challenge is common in acupuncture trials, possibly due to the inherent nature of acupuncture therapy, which involves physical contact and specific needle manipulation techniques.
Comparison of Similar Studies
Consistent with our findings, multiple recent meta-analysis reported that acupuncture improved body weight, BMI, WC, and BF % in obese patients.24–30 Notably, no meta-analysis examined the efficacy of acupuncture as an adjunct to lifestyle interventions on obesity. In other words, all studies overlooked the significance of lifestyle interventions as the first-line treatment for obesity. Fang’s study compared the curative effects of acupuncture to placebo or no treatment groups on obesity, with or without lifestyle interventions.24 BMI and adverse events are the observed outcomes in Fang’s article. While in our study, other than the anthropometric outcomes including body weight and BMI, the results related to glucose and lipid metabolism are also analyzed. Zhong’s study28 and Zhang’s study25 examined the effects of acupuncture on weight loss in comparison to sham acupuncture. Gao’s study established whether acupuncture combined with acupoint catgut embedding was superior to acupuncture alone in obesity treatment.30 Other three studies compared the effects of acupuncture treatment to non-acupuncture therapy on obesity.26,27,29 In contrast to previous research, we investigated the impact of acupuncture on both weight loss and its effects on glucose and lipid metabolism.
Unlike the above-mentioned studies, which overlooked the significance of lifestyle interventions as the first-line treatment for obesity, this study compared the impact of acupuncture combined with lifestyle interventions to that of lifestyle interventions alone in obesity treatment. In addition to the indicators directly related to obesity, the indicators related to glucose and lipid metabolism were also examined, providing comprehensive evidence on the effect of acupuncture on obesity. Performing subgroup analysis, sensitivity analysis, and publication bias to thoroughly explore potential sources of heterogeneity and conducting GRADE assessment for the evidence as well as analysis the clinical significance of the outcomes, are among the most important advantages of this research.
Implications for Clinical Practice
Aside from being a chronic metabolic disease, simple obesity is also an independent risk factor for T2DM and CVD. Obesity treatment not only aims to decrease weight, but also to help the body adapt to a normal status. Lifestyle interventions, proven to reduce body weight and significantly improve blood glucose and lipid metabolism, are the basis of obesity treatment. However, lifestyle interventions could only be independently effective after long-term maintenance, which could be challenging for most obese patients.
Acupuncture, as a non-drug therapy applied for thousands of years, has been widely utilized in the treatment of metabolic diseases. Herein, we demonstrated that acupuncture combined with lifestyle interventions had significant statistical difference on weight loss and glucose and lipid metabolism in obese patients. On the other hand, our findings confirmed that the effect size of acupuncture as an adjunct to lifestyle interventions in reducing body weight, BMI, WC, BF %, and HOMA-IR was higher than the minimal clinically important difference (MCID) for body weight (4.39 kg),80 BMI (1.44 kg/m2),81 WC (3.42 cm),81 BF % (1.93%),81 and HOMA-IR (0.05),82 which is crucial for helping clinicians achieve their treatment goals. These evidence-based findings support the clinical application of acupuncture as an adjunct to lifestyle interventions. Other than this, acupuncture can help obese individuals partly increase their confidence and motivation to lose weight, thereby promoting their long-term adherence to a good lifestyle. By cultivating good lifestyle habits, the occurrence of obesity and its complications can be prevented or reduced.
Limitations of the Study
This study had some limitations. First, the sample sizes of the included studies were generally small except for one that included 240 obese patients. Second, most of the included studies had methodological deficiencies that might have affected the accuracy of our results. Third, due to the deficiency of available data in included studies, unfortunately we were unable to conduct a secondary analysis based on different TCM syndrome types of obesity. Fourth, most studies were published in Chinese and conducted in China, the generalization of these findings might be limited. Fifth, the original data of FPG, FINS, TC, TG, HDL-C and LDL-C used different units of measurement and the differences were resolved by SMD to represent the effect size. This limits the analysis of clinical significance of acupuncture as an adjunct to lifestyle interventions for obesity on these indicators. Finally, following the GRADE approach, the results of evidence quality were generally not optimistic, with all evidence quality being low or very low. Therefore, more well-designed RCTs are needed to further validate and draw more confident conclusions.
Implications for Future Research
Our meta-analysis demonstrates the positive effect of acupuncture as a supplementary therapy for lifestyle interventions on weight loss as well as glucose and lipid metabolism in obesity treatment. Regarding future clinical trials, researchers should adopt stricter trial designs to compensate for the quality deficiencies in methodology and evidence. In term of secondary analysis, researchers need to investigate the appropriate acupuncture therapy, including MA, EA and acupoint catgut embedding, for the management of obesity treatment via network meta-analysis. Furthermore, in addition to physiological improvements, it is also necessary to investigate acupuncture treatment in improving the psychological and social wellness of obese patients.
Conclusion
The findings of our study reveal that acupuncture, when used as an adjunct to lifestyle interventions, is effective in reducing body weight and improving glucose and lipid metabolism in simple obesity treatment. Moreover, the changes in body weight, BMI, WC, BF %, and HOMA-IR have clinical significance. However, considering the shortcomings of this study, such as the low quality of most included studies and the low or very low certainty of the evidence, future high-quality and large-scale RCTs are needed to provide comprehensive and strong evidence for its clinical application in obesity management programs.
Funding Statement
This work was supported by the Fund of Key Laboratory for Sports Medicine of Sichuan Province & General Administration of Sport [grant number 2023-A055], the Innovation Project of Key Laboratory for Sports Medicine of Sichuan Province & General Administration of Sport [grant number SCZJJCC 02], the Natural Science Foundation of Sichuan Province [grant number 2022NSFSC1529], the Scientific and Technological Innovation Project of the General Administration of Sport of China [grant number 22KJCX009], and the High-level Talents Program of Chengdu Sport University [grant number D400828]. The funding body had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data Sharing Statement
All relevant data are within the paper and its Supporting Information files.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
- 1.Boutari C, Mantzoros CS. A 2022 update on the epidemiology of obesity and a call to action: as its twin COVID-19 pandemic appears to be receding, the obesity and dysmetabolism pandemic continues to rage on. Metabolism. 2022;133:155217. doi: 10.1016/j.metabol.2022.155217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Valenzuela PL, Carrera-Bastos P, Castillo-García A, Lieberman DE, Santos-Lozano A, Lucia A. Obesity and the risk of cardiometabolic diseases. Nat Rev Cardiol. 2023;20:475–494. doi: 10.1038/s41569-023-00847-5 [DOI] [PubMed] [Google Scholar]
- 3.Pan XF, Wang L, Pan A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021;9(6):373–392. doi: 10.1016/S2213-8587(21)00045-0 [DOI] [PubMed] [Google Scholar]
- 4.Global Obesity Observatory. World Obesity Atlas. 2023. Available from: https://data.worldobesity.org/publications/?cat=19. Accessed December 20, 2023.
- 5.La Sala L, Pontiroli AE. Prevention of diabetes and cardiovascular disease in obesity. Int J Mol Sci. 2020;21(21):8178. doi: 10.3390/ijms21218178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2021;143(21):e984–e1010. doi: 10.1161/CIR.0000000000000973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bagheri S, Zolghadri S, Stanek A. Beneficial effects of anti-inflammatory diet in modulating gut microbiota and controlling obesity. Nutrients. 2022;14(19):3985. doi: 10.3390/nu14193985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mayoral LP, Andrade GM, Mayoral EP, et al. Obesity subtypes, related biomarkers & heterogeneity. Indian J Med Res. 2020;151(1):11–21. doi: 10.4103/ijmr.IJMR_1768_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shao J, Li C, Bai L, et al. Recent evidence in support of traditional Chinese medicine to restore normal leptin function in simple obesity. Heliyon. 2022;8(5):e09482. doi: 10.1016/j.heliyon.2022.e09482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Su X, Peng D. The exchangeable apolipoproteins in lipid metabolism and obesity. Clin Chim Acta. 2020;503:128–135. doi: 10.1016/j.cca.2020.01.015 [DOI] [PubMed] [Google Scholar]
- 11.Nussbaumerova B, Rosolova H. Obesity and dyslipidemia. Curr Atheroscler Rep. 2023;25:1–9. [DOI] [PubMed] [Google Scholar]
- 12.Wu H, Ballantyne CM. Metabolic inflammation and insulin resistance in obesity. Circ Res. 2020;126(11):1549–1564. doi: 10.1161/CIRCRESAHA.119.315896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Avgerinos KI, Spyrou N, Mantzoros CS, Dalamaga M. Obesity and cancer risk: emerging biological mechanisms and perspectives. Metabolism. 2019;92:121–135. doi: 10.1016/j.metabol.2018.11.001 [DOI] [PubMed] [Google Scholar]
- 14.Jensen MD, Ryan DH, Apovian CM, et al. AHA/ACC/TOS guideline for the management of overweight and obesity in adults. Circulation. 2014;129(25_suppl_2):S102–138. doi: 10.1161/01.cir.0000437739.71477.ee [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yumuk V, Fruhbeck G, Oppert JM, Woodward E, Toplak H. An EASO position statement on multidisciplinary obesity management in adults. Obes Facts. 2014;7(2):96–101. doi: 10.1159/000362191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zeng Q, Li N, Pan XF, Chen L, Pan A. Clinical management and treatment of obesity in China. Lancet Diabetes Endocrinol. 2021;9(6):393–405. doi: 10.1016/S2213-8587(21)00047-4 [DOI] [PubMed] [Google Scholar]
- 17.Wadden TA, Tronieri JS, Butryn ML. Lifestyle modification approaches for the treatment of obesity in adults. Am Psychol. 2020;75(2):235–251. doi: 10.1037/amp0000517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sumithran P, Prendergast LA, Delbridge E, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med. 2011;365(17):1597–1604. doi: 10.1056/NEJMoa1105816 [DOI] [PubMed] [Google Scholar]
- 19.Kesztyus D, Erhardt J, Schonsteiner D, Kesztyus T. Therapeutic treatment for abdominal obesity in adults. Dtsch Arztebl Int. 2018;115(29–30):487–493. doi: 10.3238/arztebl.2018.0487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen C, Liu J, Sun M, Liu W, Han J, Wang H. Acupuncture for type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. Complement Ther Clin Pract. 2019;36:100–112. doi: 10.1016/j.ctcp.2019.04.004 [DOI] [PubMed] [Google Scholar]
- 21.Li X, Jia HX, Yin DQ, Zhang ZJ. Acupuncture for metabolic syndrome: systematic review and meta-analysis. Acupunct Med. 2021;39(4):253–263. doi: 10.1177/0964528420960485 [DOI] [PubMed] [Google Scholar]
- 22.Yang H, Xiao ZY, Yin ZH, et al. Efficacy and safety of acupuncture for polycystic ovary syndrome: an overview of systematic reviews. J Integr Med. 2023;21(2):136–148. doi: 10.1016/j.joim.2022.12.002 [DOI] [PubMed] [Google Scholar]
- 23.Fan XL, Yu ML, Fu SP, Zhuang Y, Lu SF. Effectiveness of acupuncture in treatment of simple obesity in animal models: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2019;2019:5459326. doi: 10.1155/2019/5459326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fang S, Wang M, Zheng Y, Zhou S, Ji G. Acupuncture and lifestyle modification treatment for obesity: a meta-analysis. Am J Chin Med. 2017;45(2):239–254. doi: 10.1142/S0192415X1750015X [DOI] [PubMed] [Google Scholar]
- 25.Zhang RQ, Tan J, Li FY, Ma YH, Han LX, Yang XL. Acupuncture for the treatment of obesity in adults: a systematic review and meta-analysis. Postgrad Med J. 2017;93(1106):743–751. doi: 10.1136/postgradmedj-2017-134969 [DOI] [PubMed] [Google Scholar]
- 26.Chen J, Chen D, Ren Q, et al. Acupuncture and related techniques for obesity and cardiovascular risk factors: a systematic review and meta-regression analysis. Acupunct Med. 2020;38(4):227–234. doi: 10.1136/acupmed-2018-011646 [DOI] [PubMed] [Google Scholar]
- 27.Gao Y, Wang Y, Zhou J, Hu Z, Shi Y. Effectiveness of electroacupuncture for simple obesity: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. 2020;2020:2367610. doi: 10.1155/2020/2367610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhong YM, Luo XC, Chen Y, et al. Acupuncture versus sham acupuncture for simple obesity: a systematic review and meta-analysis. Postgrad Med J. 2020;96(1134):221–227. doi: 10.1136/postgradmedj-2019-137221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yin Y, Zhao Q, Li S, et al. Efficacy of acupuncture and moxibustion therapy for simple obesity in adults: a meta-analysis of randomized controlled trials. Medicine. 2022;101(43):e31148. doi: 10.1097/MD.0000000000031148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gao P, Xu X, Zhou M, Cui J, Yi T, Zhu T. The impact of acupuncture combined with acupoint catgut embedding on simple obesity: a systematic review and meta-analysis. Medicine. 2023;102(28):e34234. doi: 10.1097/MD.0000000000034234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Belivani M, Dimitroula C, Katsiki N, Apostolopoulou M, Cummings M, Hatzitolios AI. Acupuncture in the treatment of obesity: a narrative review of the literature. Acupunct Med. 2013;31(1):88–97. doi: 10.1136/acupmed-2012-010247 [DOI] [PubMed] [Google Scholar]
- 32.Song AQ, Zhang YP, Chen R, Liang FX. Is acupuncture effective for improving insulin resistance? A systematic review and meta-analysis. Curr Med Sci. 2018;38(6):1109–1116. doi: 10.1007/s11596-018-1991-1 [DOI] [PubMed] [Google Scholar]
- 33.Han J, Guo X, Meng XJ, et al. Acupuncture improved lipid metabolism by regulating intestinal absorption in mice. World J Gastroenterol. 2020;26(34):5118–5129. doi: 10.3748/wjg.v26.i34.5118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Landgraaf RG, Bloem MN, Fumagalli M, Benninga MA, de Lorijn F, Nieuwdorp M. Acupuncture as multi-targeted therapy for the multifactorial disease obesity: a complex neuro-endocrine-immune interplay. Front Endocrinol. 2023;14:1236370. doi: 10.3389/fendo.2023.1236370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang M, Liu W, Ge J, Liu S. The immunomodulatory mechanisms for acupuncture practice. Front Immunol. 2023;14:1147718. doi: 10.3389/fimmu.2023.1147718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mittelbach J. Clinical study of acupuncture treatment of obesity with CM3 [Doctor], Shandong University of Traditional Chinese Medicine; 2017. [Google Scholar]
- 37.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int j Surg. 2021;134:178–189. [DOI] [PubMed] [Google Scholar]
- 38.Jpt HJhwc-ho. Cochrane handbook for systematic reviews of interventions. 2008.
- 39.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. doi: 10.1136/bmj.39489.470347.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tong J, Chen JX, Zhang ZQ, et al. Clinical observation on simple obesity treated by acupuncture. Chinese Acupuncture Moxibustion. 2011;31(08):697–701. [PubMed] [Google Scholar]
- 41.Liang L. Acupuncture the points of spleen and stomach meridian research on the effects of fasting insulin levels in patients with simple obesity [Master], Guangxi University of Chinese Medicine; 2013. [Google Scholar]
- 42.Zhang SQ, Wu JD. Clinical observation on 120 cases in the acupuncture treatment for spleen deficiency dampness type simple obesity. Guid J Tradit Chin Med Pharm. 2016;22(6):101–102. [Google Scholar]
- 43.Li PP, Li SA, Li RC, L M, Wang RH. Observation on the therapeutic effect of Bo’s abdominal acupuncture in reducing abdominal fat in Sudanese women with simple obesity. Modern Chin Med. 2017;37(5):42–44,50. [Google Scholar]
- 44.Li ZX, Xu NG, Zhang HH, Xie WT, Yi W. Effect of Acupuncture Combined with Kinesitherapy in Treatment of Simple Obesity. Chinese Gen Pract. 2019;22:A01. [Google Scholar]
- 45.Liu MZ, Liu YT, Yang LB. Effect of acupuncture on serum PYY and nesfatin-1 in obese patients with insulin resistance. J Acupuncture Tuina Sci. 2021;19(6):432–437. doi: 10.1007/s11726-021-1280-6 [DOI] [Google Scholar]
- 46.Min EJ. The research and choosing acupoints methods based on midnight-noon ebb-flow therapy for obesity with spleen qi deficiency and exuberant dampness type [Master], Guangzhou University of Chinese Medicine; 2021. [Google Scholar]
- 47.Zhang YY, Li PP, Gu YJ. The effect of Jin’s three-needle therapy on visceral fat in patients with simple obesity. China’s Naturopathy. 2021;29(13):58–60. [Google Scholar]
- 48.Bi JY. Clinical effect of acupuncture on simple obesity in damp-heat constitution and its effect on lipid metabolism [Master], Shandong University of Traditional Chinese Medicine; 2022. [Google Scholar]
- 49.Qi GH, Shi JF. Clinical study on acupuncture treatment of 35 patients with simple obesity in Malta. Med Health. 2022;2022(10):162–164. [Google Scholar]
- 50.Jia SY, Wang H, Li L. The clinical study of acupuncture treatment for spleen deficiency dampness type simple obesity by invigorating spleen to eliminate dampness. J Pract Trad Chinese Med. 2023;39(1):154–156. [Google Scholar]
- 51.Yang L, Nie Y, Wen YL, Kang Q. Clinical study onneedling “ShuiShu fifty-seven points” on simple obesity with syndrome of spleen and kidney yang deficiency obstruction. Medicine and Health. 2023;2023(11):166–169. [Google Scholar]
- 52.Li DH. Study on the therapeutic effect of low-wavelength electroacupuncture on simple obesity [Dissertation], China Academy of Chinese Medical Sciences; 2005. [Google Scholar]
- 53.Luo SH. Clinical observation on the treatment of 60 cases of simple obesity with acupuncture. J Clin Acupuncture Moxibustion. 2007;23(9):17–18. [Google Scholar]
- 54.Xing HJ. The clinical research on acupuncture combined with dietary adjustments and aerobic exercise for treatment of simple obesity [Master], Hebei Medical University; 2009. [Google Scholar]
- 55.Zhao LQ, Shi Y. Clinical study on the treatment for stomach-intestine excessive heat type simple obesity by electroacupuncture combined with diet and exercise therapy. J Anhui Univ Chinese Med. 2010;29(4):33–37. [Google Scholar]
- 56.Abdi H, Zhao B, Darbandi M, et al. The effects of body acupuncture on obesity: anthropometric parameters, lipid profile, and inflammatory and immunologic markers. Sci World J. 2012;2012(2012):603539. doi: 10.1100/2012/603539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang WJ, Xiao YP. Observation of curative effect of electroacupuncture therapy on obesity. Chinese J Prim Med Pharm. 2014;21(12):1878–1879. [Google Scholar]
- 58.Bae HI. Clinical study of obesity treated by acusector combined with dietary adjustment therapy [Dissertation], Nanjing University Of Chinese Medicine; 2016. [Google Scholar]
- 59.Xue WH, Yin QB, Liu L, Zhou TT, Wang YJ. Clinical study on the treatment for simple obesity by harmonic Yangming acupuncture combined with comprehensive intervention. Hebei J Trad Chin Med. 2018;40(2):280–283. [Google Scholar]
- 60.Yin QB, Duan YF, Cheng XY, Xue WH, Wang YJ. Clinical observation of electroacupuncture combined with comprehensive intervention on simple obesity. Hebei J Trad Chin Med. 2018;40(4):580–583. [Google Scholar]
- 61.Wang Hl. A randomized controlled trial of electroacupuncture for the treatment of obesity to observed resting metabolic rate [Master], Guangzhou University of Chinese Medicine; 2020. [Google Scholar]
- 62.Zheng ZZ, Luo H, You QY, Wang J. 30 cases in the treatment for simple obesity by electroacupuncture combined with nutritional intervention. Fujian J Trad Chinese Med. 2021;52(2):51–52. [Google Scholar]
- 63.Liang ZM. Observation on the curative effect of regulating mentality and spleen strengthening acupuncture on treatment for spleen-deficiency dampness type simple obesity [Master], Guangzhou University of Chinese Medicine; 2022. [Google Scholar]
- 64.Ni W, Wang P, Chen HJ, et al. Obesity complicated with insulin resistance treated with the electroacupuncture at the combination of back-shu and front-mu points. World J Acupuncture - Moxibustion. 2022;32(3):213–217. doi: 10.1016/j.wjam.2021.12.004 [DOI] [Google Scholar]
- 65.Goodpaster BH, Sparks LM. Metabolic flexibility in health and disease. Cell Metab. 2017;25(5):1027–1036. doi: 10.1016/j.cmet.2017.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Guo F, Garvey WT. Cardiometabolic disease staging predicts effectiveness of weight-loss therapy to prevent type 2 diabetes: pooled results from Phase III clinical trials assessing phentermine/topiramate extended release. Diabetes Care. 2017;40(7):856–862. doi: 10.2337/dc17-0088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gong M, Wang X, Mao Z, Shao Q, Xiang X, Xu B. Effect of electroacupuncture on leptin resistance in rats with diet-induced obesity. Am J Chin Med. 2012;40(3):511–520. doi: 10.1142/S0192415X12500395 [DOI] [PubMed] [Google Scholar]
- 68.Li X, Wu Z, Chen Y, Cai R, Wang Z. Effect of acupuncture on simple obesity and serum levels of prostaglandin e and leptin in sprague-dawley rats. Comput Math Methods Med. 2021;2021:6730274. doi: 10.1155/2021/6730274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wang F, TD R, Tso P, Han JS. Arcuate nucleus of hypothalamus is involved in mediating the satiety effect of electroacupuncture in obese rats. Peptides. 2011;32(12):2394–2399. doi: 10.1016/j.peptides.2011.10.019 [DOI] [PubMed] [Google Scholar]
- 70.Ji B, Hu J, Ma SX. Effects of electroacupuncture Zusanli (ST36) on food intake and expression of POMC and TRPV1 through afferents-medulla pathway in obese prone rats. Peptides. 2013;40:188–194. doi: 10.1016/j.peptides.2012.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wang LH, Huang W, Wei D, et al. Mechanisms of acupuncture therapy for simple obesity: an evidence-based review of clinical and animal studies on simple obesity. Evidence-Based Complementary. 2019;2019:5796381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cui JW, Song WR, Jin YP, et al. Research progress on the mechanism of the acupuncture regulating neuro-endocrine-immune network system. Vet Sci. 2021;8(8):149. doi: 10.3390/vetsci8080149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zatterale F, Longo M, Naderi J, et al. Chronic adipose tissue inflammation linking obesity to insulin resistance and type 2 diabetes. Front Physiol. 2020;10:1607. doi: 10.3389/fphys.2019.01607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yan YZ, Ma RL, Zhang JY, et al. Association of insulin resistance with glucose and lipid metabolism: ethnic heterogeneity in far Western China. Mediators Infl. 2016;2016:3825037. doi: 10.1155/2016/3825037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang L, Wang B, Gasek NS, et al. Targeting p21(Cip1) highly expressing cells in adipose tissue alleviates insulin resistance in obesity. Cell Metab 2022;34(1):75–89. doi: 10.1016/j.cmet.2021.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Liang FX, Chen R, Nakagawa A, et al. Low-frequency electroacupuncture improves insulin sensitivity in obese diabetic mice through activation of SIRT1/PGC-1 in skeletal muscle. Evidence-Based Complementary Alt Med. 2011;2011:735297. doi: 10.1155/2011/735297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tuǧrul Cabıoǧlu M, Ergene N. Electroacupuncture therapy for weight loss reduces serum total cholesterol, triglycerides, and LDL cholesterol levels in obese women. Am J Chin Med. 2005;33(04):525–533. doi: 10.1142/S0192415X05003132 [DOI] [PubMed] [Google Scholar]
- 78.Gong M, Cao C, Chen F, et al. Electroacupuncture attenuates hepatic lipid accumulation via AMP-activated protein kinase (AMPK) activation in obese rats. Acupuncture Med. 2016;34(3):209–214. doi: 10.1136/acupmed-2015-010798 [DOI] [PubMed] [Google Scholar]
- 79.Lu M, He Y, Gong M, et al. Role of neuro-immune cross-talk in the anti-obesity effect of electro-acupuncture. Front Neurosci. 2020;14:151. doi: 10.3389/fnins.2020.00151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Soltani S, Jayedi A, Abdollahi S, Vasmehjani AA, Meshkini F, Shab-Bidar S. Effect of carbohydrate restriction on body weight in overweight and obese adults: a systematic review and dose-response meta-analysis of 110 randomized controlled trials. Front Nutr. 2023;10:1287987. doi: 10.3389/fnut.2023.1287987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582–592. doi: 10.1097/01.MLR.0000062554.74615.4C [DOI] [PubMed] [Google Scholar]
- 82.Goldenberg JZ, Day A, Brinkworth GD, et al. Efficacy and safety of low and very low carbohydrate diets for type 2 diabetes remission: systematic review and meta-analysis of published and unpublished randomized trial data. BMJ. 2021;372:m4743. doi: 10.1136/bmj.m4743 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.