Abstract
Objective:
Continuity of patient information across settings can improve transitions after hospital discharge, but outpatient clinicians often have limited access to complete information from recent hospitalizations.
Study Design:
Through a stepped-wedge design, we examined whether providers’ timely access to clinical information through shared inpatient-outpatient electronic health records (EHR) was associated with in-person follow-up visit rates and return emergency department (ED) visits or readmissions after a hospital discharge in patients with diabetes.
Methods:
As an integrated delivery system staggered implementation of a shared inpatient-outpatient EHR, we studied 241,510 hospital discharges in patients with diabetes (2005–2011), examining rates of outpatient follow-up office visits, telemedicine (phone visits and asynchronous secure messages), lab-tests, and return ED visits or re-hospitalizations (as adverse events). We used multivariate logistic regression adjusting for time trends, patient characteristics, medical center, and patient clustering, to predict adjusted follow-up rates.
Results:
For patients with diabetes, provider use of a shared inpatient-outpatient EHR was associated with a statistically significant shift toward follow-up delivered through a combination of telemedicine and outpatient lab tests, and without a traditional in-person visit (from 22.9% with an outpatient-only EHR to 27.0% with a shared inpatient-outpatient EHR). We found no statistically significant differences in 30-day return ED visits (OR 1.02, 95%CI 0.96–1.09) or re-admissions (OR 0.98, 95%CI 0.91–1.06) with the shared EHR.
Discussion and Conclusions:
Real-time clinical information availability during transitions between different health care settings, along with robust telemedicine access, may shift the method of care-delivery without adversely affecting patient health outcomes. Efforts to expand interoperability and information exchange may support follow-up care efficiency.
Précis:
Using a seamlessly shared inpatient-outpatient EHR was associated with greater rates of post-discharge follow-up delivered through telemedicine or lab monitoring and without an in-person office-visit.
Summary
Continuity in access to patient information across providers in different settings can improve patient transitions. We examined whether timely access to complete clinical information through a shared inpatient-outpatient electronic health record (EHR) was associated with changes in rates of in-person follow-up visits after hospital discharge in patients with diabetes.
• Using the shared inpatient-outpatient EHR was associated with a shift toward 7-day follow-up delivered through a combination of telemedicine (telephone and patient-physician secure messages) and outpatient lab tests, without a traditional office visit.
• Patient outcomes, as measured by 30-day return ED visits or hospital readmission were comparable when using the shared EHR.
Timely availability of clinical information during health care transitions, in a setting with robust telemedicine access, can shift the method of care-delivery without adversely affecting patient health outcomes.
BACKGROUND AND SIGNIFICANCE
For the growing number of patients with chronic conditions, care transitions, such as after hospital discharge, require coordination between multiple clinicians practicing in different settings.1–3 Health information exchange that ensures that patient health information follow the patient as they move between care settings is important to providing well-coordinated care.4 Still, developing widespread electronic health record (EHR) interoperability and information exchange between settings remains challenging.5–8 Emerging health care payment models, coordination, and consolidation efforts are likely increasing information-sharing between providers at follow-up visits.9 Still, there is limited evidence on the impact of sharing electronic patient information across settings on patient care transitions and outcomes, particularly on follow-up care and adverse events after a hospitalization.6,10,11
With limited electronic data-sharing, deficiencies in information availability and communication between providers after hospital discharge are regularly reported by both clinicians and patients -- including inconsistent awareness of the hospitalization itself, and limited communication of medications, orders and lab results, leading to medical errors and increases in readmission.12–18,43 In the absence of broad clinical guidelines for optimal post-discharge follow-up interval or encounter type, differences in follow-up visit rates have been associated with mixed outcomes.9,19 Shared seamless access to EHRs, can offer clinicians direct access to fully view and document detailed patient clinical information across health care settings without requiring shifts across systems, modalities (like paper), or capabilities (like limited snapshots, or fragmented documentation).20 The timely exchange of patient information and communication is defined for this paper as data access to support clinical care at any time it is clinically needed, ideally in real-time. Timely and seamless EHR-access across providers can support patient transitions from hospital discharge to outpatient follow-up care, such as by facilitating coordination, risk stratification, and flexibility for telemedicine encounter types, with potential implications for clinical care quality and efficiency.18,21 Early evidence from other settings and patient populations about impacts of health information exchange are mixed, however some studies have suggested that electronic health information availability and exchange are associated with reductions in repeat tests or imaging, and supports the feasibility of telemedicine follow-up. 11,44,45,46
OBJECTIVES
Building on previous findings of improved diabetes care and health outcomes after implementation of an outpatient-only electronic health record (EHR), we studied the subsequent implementation of a shared inpatient EHR which seamlessly integrates patient health information between hospital and outpatient provders.22,23 In patients with diabetes, this study examines the association between provider use of the shared inpatient-outpatient EHR and rates and types of outpatient follow-up, including: office visits, telemedicine encounters (including asynchronous secure patient-physician messages and real-time telephone visits), and lab tests. We also examined the impact on adverse clinical events after hospital discharge, measured by emergency department (ED) visits or hospital readmissions.
MATERIAL AND METHODS
Study design and setting
This quasi-experimental study examined a historical natural experiment in which an integrated delivery system staggered implementation of an inpatient EHR, integrating it with an already existing outpatient EHR, across 17 hospitalist-staffed hospitals (2006–2010). This created a stepped wedge study design to study the impact of shared inpatient-outpatient EHR use (Figure 1). The implementation order was not associated with medical centers’ health care quality or readmission rates.23
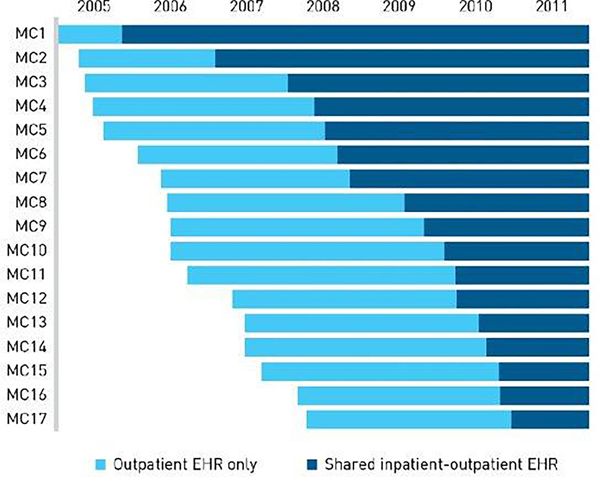
FIGURE 1.
Staggered EHR Implementation by (MC): Quasi-experimental study with concurrent controlsa
EHR, electronic health record; MC, medical center.
aThis figure shows the schedule of staggered inpatient EHR implementation across all study MCs during the study period (2005–2011), which offered a natural experiment using a stepped wedge design. After implementation, the inpatient EHR completely replaced the paper medical chart. During the light blue time periods there was only an outpatient EHR in use, but no inpatient EHR. During the dark-blue time periods, there was an inpatient EHR in use, integrated with the outpatient EHR.
Prior to the study period, the outpatient EHR used by clinicians had already integrated all outpatient records, including primary and specialty care, laboratories, and pharmacy, but did not include complete clinical information from hospitalizations or ED visits. At baseline, providers also already had the capability to conduct scheduled real-time telephone telemedicine visits with patients, and access to a patient portal website which offered patient-provider asynchronous secure messaging tools. As such, our study examines a shift in provider-to-provider access to patient data across settings after implementation of the shared inpatient-outpatient EHR.
The commercially-available complete hospital EHR replaced the inpatient paper medical record and a patchwork of optional health IT tools, creating a shared inpatient-outpatient EHR. Before implementing the inpatient EHR, health information exchange between inpatient and outpatient providers was not consistent and was provider-dependent. After the inpatient EHR was implemented, both inpatient and outpatient EHRs were seamlessly integrated. The hospital EHR automatically integrates patient history and clinical information (clinical notes, procedures, imaging, labs, medications, etc.) with the outpatient EHR used by primary care providers and specialists, including order-entry capability for outpatient follow-up, and medication reconciliation before discharge, secure messaging between providers and with patients, and notifications to outpatient providers that their patient had been hospitalized.
Population
Between 2005 and 2011, we identified all hospitalizations among patients with diabetes (using the clinical diabetes registry) in medical centers where the outpatient EHR was already in use. We examined patients with diabetes as an example of the impact of shared EHR-use in a common chronic condition which has associated complications. We excluded from our study analytic dataset patients that were not health plan members in the year prior to the hospitalization and for 30 days after discharge in order to ensure capture of comorbidities and follow-up. We also excluded hospitalizations that were not discharged home in order to ensure eligibility for outpatient follow-up.
Follow-up Encounters
Our data captured all outpatient office visits, telephone visits, secure electronic messages, and lab tests after hospital discharge. In the absence of broad evidence-based guidelines for any optimal post-discharge follow-up timing, we examined the encounters within 7 and 30 days after hospital discharge.9,19 We also examined any 30-day clinical events as a measure of adverse health events or outcomes, including ED visit or re-hospitalizations, based on the 30-day Medicare readmission measures.
Among hospitalizations with follow-up, we examined the rates of follow-up through a combination of only telemedicine and lab tests.
Analysis
We used multivariate logistic regression models for each type of follow-up encounter outcome with EHR status as the main predictor and adjustment for patient characteristics (age, gender, neighborhood SES, race/ethnicity, copayment, comorbidity score), seasonality (calendar month, categorical variable), time trend (year 1 for 2005, year 2 for 2006, and so on, as continuous variable), time trend2, comorbidity score (centered), interaction term of comorbidity score and time trend, medical center and medical center-specific time trends (interaction term of medical center of time trend and time trend2 , with standard errors corrected for patient clustering (using Stata SE 10.1, StataCorp LP, College Station, TX). We reported adjusted odds ratios (OR) from these multivariate models. For easier interpretation, we also calculated the adjusted rates of each outcome by applying the coefficients from the logistic regression to the entire cohort as if everyone were in pre-inpatient EHR and post-inpatient EHR periods respectively so that patients in pre-inpatient EHR and post-inpatient EHR shared the exact same characteristics (margin command in STATA).
In sensitivity analyses, we examined the subset of hospitalizations categorized as non-elective and findings were comparable (see Appendix).
RESULTS
Among all 241,510 hospitalizations in 104,126 patients with diabetes from 2005 to 2011, 91,331 occurred before the shared inpatient EHR was implemented, and 150,179 occurred afterwards. Table 1 shows patient characteristics.
Table 1.
All hospitalizations among patients with diabetes (2005–2011): Patient characteristics
| Patient Characteristics | Total (N=241,510) | Outpatient EHR Only (N=91,331) | Shared Inpatient-Outpatient EHR (N=150,179) | |
|---|---|---|---|---|
|
| ||||
| Age | <18 | 0.35% | 0.41% | 0.31% |
| 18–39 | 5.16% | 5.01% | 5.24% | |
| 40–64 | 39.42% | 39.07% | 39.64% | |
| 65–74 | 26.94% | 26.90% | 26.97% | |
| ≥75 | 28.13% | 28.61% | 27.84% | |
| Gender | Female | 50.66% | 49.06% | 49.51% |
| Neighborhood SES | Higher | 68.52% | 67.44% | 69.17% |
| Lower | 26.06% | 26.93% | 25.53% | |
| Unknown | 5.42% | 5.62% | 5.30% | |
| Race/Ethnicity | White | 52.04% | 51.51% | 52.36% |
| Black | 12.60% | 13.03% | 12.34% | |
| Hispanic | 18.58% | 19.07% | 18.28% | |
| Asian | 14.92% | 14.63% | 15.09% | |
| Other | 1.87% | 1.76% | 1.93% | |
After multivariate adjustment, the rate of any type of ambulatory follow-up encounter within seven days of hospital discharge decreased from 72.8% to 69.2% after use of the shared EHR (p<0.05, Table 2), and more modestly within 30-days after discharge, from 94.8% to 94.1% after use of the shared EHR (p<0.05). These patterns in care changes associated with shared EHR use were consistent when examining within 30-day period after hospital discharge (see Appendix).
Table 2.
Association between use of shared inpatient-outpatient EHR and follow-up care and events after discharge
| Adjusted Rates | Shared Inpatient-Outpatient EHR vs Outpatient EHR Only | ||||
|---|---|---|---|---|---|
| Outpatient EHR Only | Shared Inpatient-Outpatient EHR | Adjusted OR | 95% CI | ||
|
| |||||
| Follow-up within 7 days after hospital discharge | |||||
| Any follow-up a | 72.83% | 69.21% | 0.84 | 0.80 | 0.87 |
| In-person office visita | 55.91% | 50.48% | 0.80 | 0.77 | 0.84 |
| Phone visit | 9.04% | 8.85% | 0.98 | 0.90 | 1.06 |
| Secure message | 11.50% | 11.74% | 1.03 | 0.94 | 1.12 |
| Lab testa | 32.00% | 30.70% | 0.94 | 0.89 | 0.99 |
| Events 30 days after hospital discharge | |||||
| ED visits | 16.39% | 16.69% | 1.02 | 0.96 | 1.09 |
| Hospital Readmission | 9.49% | 9.35% | 0.98 | 0.91 | 1.06 |
Logistic regression analyses adjusted for patient age, gender, neighborhood SES, race/ethnicity, office copayment, calendar month, time (year, continuous variable), time2, medical center, interaction of medical center and time +time2, comorbidity score (centered), interaction of comorbidity score and time, with standard errors corrected by clustering at patient level. Adjusted rates are calculated by applying the coefficients from the logistic regression to the cohort as if everyone were in pre-inpatient-EHR period and in post-inpatient-EHR period respectively.
p<0.05
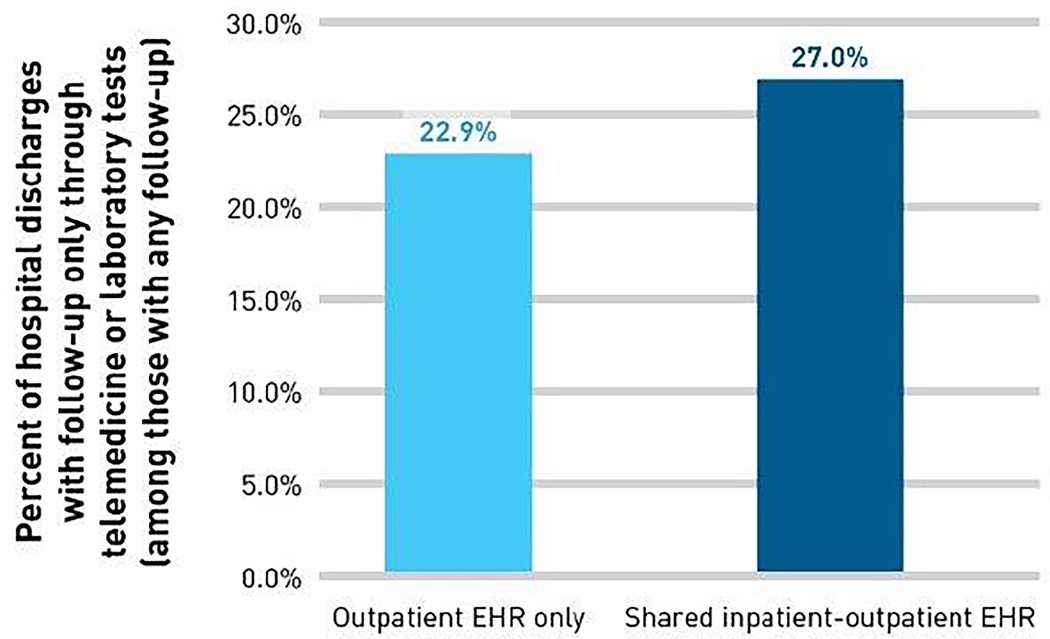
The type of follow-up care also changed after the shared-EHR implementation. The proportion of 7-day follow-up delivered by a combination of telemedicine or lab tests and without an in-person office visit increased from 22.9% before use of the shared EHR to 27.0% (p<0.05, see Figure 2) afterward. Specifically, follow-up with an in-person office visit within 7-days dropped from 55.9% to 50.5% (p<0.05) and use of any laboratory testing within seven days after discharge dropped from 32.0% to 30.7% (p<0.05). There were no statistically significant changes in the rates of telephone visits or secure messages (p>0.05).
FIGURE 2.
Adjusted Rates of Follow-up Care Within 7 Days After Hospital Discharge Delivered Only Through Telemedicine and Laboratory Testsa
EHR, electronic health record.
aAdjusted rates are calculated by applying the coefficients from logistic regression analyses, which include inpatient EHR indicator, patient age, gender, neighborhood socioeconomic status, race/ethnicity, office copayment, calendar month, time (year, continuous variable), quadratic term of time trend, medical center, interaction of medical centerwith time trend and quadratic term of time trend, comorbidity score (centered), and interaction of comorbidity score and time trend, to the cohort as if everyone were in pre-inpatient-EHR period and in post-inpatient-EHR period respectively.
As a measure of adverse health events or outcomes, there were no statistically significant differences in the rates of ED visits or readmission in the 30 days after hospital discharge associated with use of the integrated hospital EHR. After the integrated EHR was in use, 16.7% of hospital discharges were followed by an ED visit (vs. 16.4% before, p>0.05) and 9.4% were followed by another hospitalization within 30 days (vs. 9.5% before, p>0.05), as shown in Table 2.
DISCUSSION
In this natural experiment involving the staggered implementation of a commercially-available inpatient-outpatient shared EHR which shares patient data across providers in inpatient and ambulatory settings, we found that after hospital discharge, patients with diabetes had a higher likelihood of receiving follow-up care delivered only by a combination of telemedicine (telephone visits and asynchronous secure messages) and lab monitoring, and without a traditional in-person visit. We found slightly lower overall rates of follow-up office visits and outpatient lab tests. As a measure of clinical events, we found no statistically significant association between inpatient-outpatient EHR use and rates of return ED visits or hospital readmissions. Together, these findings suggest that the timely availability of complete clinical information from using a shared inpatient-outpatient EHR after a hospital discharge, in a setting with strong telemedicine access, could shift the method of delivering follow-up care without adversely affecting patient health outcomes as measured by repeat ED visits or readmissions.
While EHR interoperability and health information exchange functionality have been consistently promoted as policy priorities for improving the quality and efficiency of the American healthcare system, there is still limited research evidence to inform policy-makers about the effects of continuity in provider access to patient information.8,33,6 Our study builds this evidence as one of the largest rigorously designed studies to examine the impact of shared health information access across providers during patient transitions between health care settings. Our findings from patients with diabetes also complement previous studies in the same integrated delivery system, in patients with diabetes and in general patient populations, in which both providers and patients report that EHR use facilitated care coordination both by providing informational continuity between providers, and by supporting direct communication between clinicians and medical staff through electronic messaging tools.34,35 In a general patient population, primary care providers reported enhanced access to timely and complete patient information, and better agreement on treatment goals and roles and responsibilities after the inpatient EHR was in use.35
The optimal amount and timing of outpatient follow-up care after hospital discharge is not clear.9,19 While some studies have found that follow-up visits or telephone calls after hospital discharge were associated with better patient outcomes, others have found no effect or worse outcomes associated with more follow-up care, and the evidence continues to be mixed.25–29,32,36 In the absence of broad evidence-based clinical guidelines for the optimal type or level of after-discharge follow-up, our study aimed to examine whether use of a shared inpatient-outpatient EHR was associated with shifts in the type of follow-up care delivered after hospital discharge. Since we found that follow-up care was more likely to be delivered only through telemedicine and lab tests, and without any evidence of adverse changes in downstream health events as measured by ED visits and re-hospitalizations, these changes in follow-up care represent potential improvements in the efficiency of health care delivery without adversely affecting quality. Similarly, since in this study the rate of outpatient lab tests was lower after using the shared inpatient-outpatient EHR without measurable impact on ED visits or hospitalizations, it appears that EHR-enabled information availability may have decreased unnecessary testing. Our findings are consistent with early evidence from other settings and across patient populations, which have found that electronic health information availability and exchange are associated with reductions in repeat tests and imaging, and improve the feasibility of telemedicine follow-up.19,37 44,45,46
Seamless and timely electronic health information exchange is still limited across the US health care delivery system. Calls for increases in exchange capabilities at hospital discharge are growing but few settings have measured the large-scale impact of EHR-based information integration across delivery settings.38,39 21,13,42 Our study finds that movement toward more seamless health information access, even within an already integrated system, can affect the efficiency of follow-up care after hospital discharge without adversely effecting quality. These shifts may also potentially improve patient convenience through telemedicine follow-up without requiring the transportation and cost of making an in-person visit to health care providers. Even though our study found modest average decreases in in-person visits, cumulatively impacts of this magnitude may be substantial if replicated broadly across large numbers of annual hospitalizations in patient populations with chronic conditions. In addition, our finding of no significant differences in clinical events can be interpreted as reassuring that negative impacts of care shifts were not detected. Further research is needed to explore patient follow-up care preferences and to explore clinical impacts of variations in follow-up care types in more detail.
There are several limitations to the interpretation and generalizability of our study design and setting. First, the natural experiment of shared inpatient-outpatient EHR implementation in this study is historical and may not fully generalize to current practice, which may vary across settings. Since the sharing of patient data across health care settings is still currently evolving, however, the study findings have potential relevance despite the historical study period. Further, the study relevance is supported by examining a study setting with relatively mature telemedicine and patient portal in which patients could access a portal website schedule a telemedicine visit to communicate with physicians and to review visit details and lab results. The follow-up care patterns we identified would not be feasible without the ability to follow-up with patients readily by phone or through secure messages. In other settings, in-person follow-up office visits may be needed to share paper discharge summaries or to notify providers of a recent hospitalization.13,24 Also, the rates of follow-up care in our study at baseline were higher than previously reported in other settings, and the re-hospitalization rates were somewhat lower, therefore other settings with more limited follow-up patterns at baseline may experience different shifts with the availability of health information exchange across settings.12,14,24–31 Our study examines patterns in follow-up care after implementing a system-wide electronic record system and we are not able to characterize the clinical appropriateness of any specific follow-up care regimen. Further study of the clinical significance of changes in follow-up care encounter types is needed. This study examines only patients with diabetes and we cannot generalize directly to other patient populations. Shared electronic health records and information exchange are only tools to increase information availability; their impact is dependent on the clinical workflow and delivery system context in which they are used.
CONCLUSION
Overall, in a setting which implemented a shared EHR with seamless health information exchange between inpatient and outpatient providers, patient follow-up care after hospital discharge was less likely to include an in-person office visit and instead was managed through exchange of asynchronous secure messages, telephone telemedicine, and outpatient lab tests. We found no statistically significant change in the rate of return ED visits or readmissions within 30 days after discharge, and conclude that increased and timely information availability through the shared inpatient-outpatient EHR changed the pattern of follow-up care after discharge, enabling care delivery through non-office visit encounters without adversely affecting patient short-term outcomes.
Supplementary Material
Take-Away Points:
Continuity in patient information between settings can improve the patient transitions. We examined whether timely access to complete clinical information through a shared inpatient-outpatient electronic health record (EHR) was associated with changes in rates of in-person follow-up visits after hospital discharge.
Using the shared inpatient-outpatient EHR was associated with a statistically significant shift toward 7-day follow-up delivered through a combination of telephone telemedicine, patient-physician secure messages, and outpatient lab tests, without a traditional in-person office visit.
There were no statistically significant differences in 30-day return ED visits or hospital readmission associated with using the shared EHR.
Timely availability of clinical information during health care transitions, in a setting with robust telemedicine access, can shift the method of care-delivery without adversely affecting patient health outcomes.
Funding source:
National Institutes of Diabetes Digestive and Kidney Disorders (NIDDK, R01DK085070). The study sponsor had no role in the design and conduct of the study, including the collection, analysis, and interpretation of data and the writing of the article and the decision to submit it for publication.
Footnotes
This study obtained ethics approval from the Kaiser Permanente Northern California Internal Review Board, which waived the requirement for patient consent for this observational study.
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare no financial or non-financial interests that may be relevant to the submitted work.
References
- 1.Anderson GF. Chronic care: making the case for ongoing care: Robert Wood Johnson Foundation; 2010. [Google Scholar]
- 2.National Center for Health Statistics. Health, United States, 2013: With Special Feature on Prescription Drugs. Hyattsville, MD: 2014. [PubMed] [Google Scholar]
- 3.Thorpe KE, Ogden LL, Galactionova K. Chronic conditions account for rise in Medicare spending from 1987 to 2006. Health Aff 2010;29:718–24. [DOI] [PubMed] [Google Scholar]
- 4.Clancy C Evidence-based Practice Center Systematic Review Protocol - Project Title: Health Information Exchange. Agency for Healthcare Research and Quality 2014. [Google Scholar]
- 5.O’Malley AS, Grossman JM, Cohen GR, et al. Are electronic medical records helpful for care coordination? Experiences of physician practices. J Gen Intern Med 2010;25:177–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rudin RS, Motala A, Goldzweig CL, et al. Usage and Effect of Health Information ExchangeA Systematic ReviewUsage and Effect of Health Information Exchange. Ann Intern Med 2014;161:803–11. [DOI] [PubMed] [Google Scholar]
- 7.The Office of the National Coordinator for Health Information Technology (ONC). 2015 Report to Congress on Health Information Blocking. Washington, DC: Department of Health and Human Services; 2015. [Google Scholar]
- 8.Medicare and Medicaid programs; electronic health record incentive program. Final rule. Federal register 2010;75:44313–588. [PubMed] [Google Scholar]
- 9.Ganguli I, Wasfy JH, Ferris TG. What is the right number of clinic appointments?: Visit frequency and the accountable care organization. JAMA 2015. [DOI] [PubMed] [Google Scholar]
- 10.Callen J, Georgiou A, Li J, et al. The safety implications of missed test results for hospitalised patients: a systematic review. BMJ Qual Saf 2011;20:194–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rahurkar S, Vest JR, Menachemi N. Despite the spread of health information exchange, there is little evidence of its impact on cost, use, and quality of care. Health Aff 2015;34:477–83. [DOI] [PubMed] [Google Scholar]
- 12.Moore C, Wisnivesky J, Williams S, et al. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med 2003;18:646–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA 2007;297:831–41. [DOI] [PubMed] [Google Scholar]
- 14.Bell CM, Schnipper JL, Auerbach AD, et al. Association of communication between hospital-based physicians and primary care providers with patient outcomes. J Gen Intern Med 2009;24:381–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roy CL, Poon EG, Karson AS, et al. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med 2005;143:121–8. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. Summary of the evidence on patient safety: implications for research/Edited by Ashish Jha. 2008. [Google Scholar]
- 17.van Walraven C, Mamdani M, Fang J, et al. Continuity of care and patient outcomes after hospital discharge. J Gen Intern Med 2004;19:624–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones J, Nowels CT, Sudore R, et al. The Future as a Series of Transitions: Qualitative Study of Heart Failure Patients and Their Informal Caregivers. J Gen Intern Med 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Javorsky E, Robinson A, Boer Kimball A. Evidence-based guidelines to determine follow-up intervals: a call for action. The Am J Manag Care 2014;20:17–9. [PubMed] [Google Scholar]
- 20.Rudin RS, Salzberg CA, Szolovits P, et al. Care transitions as opportunities for clinicians to use data exchange services: how often do they occur? J Am Med Inform Assoc 2011;18:853–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rudin RS, Bates DW. Let the left hand know what the right is doing: a vision for care coordination and electronic health records. J Am Med Inform Assoc 2014;21:13–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reed M, Huang J, Brand R, et al. Implementation of an outpatient electronic health record and emergency department visits, hospitalizations, and office visits among patients with diabetes. JAMA 2013;310:1060–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reed M, Huang J, Graetz I, et al. Outpatient electronic health records and the clinical care and outcomes of patients with diabetes mellitus. Ann Intern Med 2012;157:482–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coleman EA, Parry C, Chalmers S, et al. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med 2006;166:1822–8. [DOI] [PubMed] [Google Scholar]
- 25.Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. J Hosp Med 2010;5:392–7. [DOI] [PubMed] [Google Scholar]
- 26.Lin CY, Barnato AE, Degenholtz HB. Physician Follow-Up Visits After Acute Care Hospitalization for Elderly Medicare Beneficiaries Discharged to Noninstitutional Settings. J Am Ger Soc 2011;59:1947–54. [DOI] [PubMed] [Google Scholar]
- 27.Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA 2010;303:1716–22. [DOI] [PubMed] [Google Scholar]
- 28.Hess CN, Shah BR, Peng SA, et al. Association of early physician follow-up and 30-day readmission after non-ST-segment-elevation myocardial infarction among older patients. Circulation 2013;128:1206–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DeLia D, Tong J, Gaboda D, et al. Post-discharge follow-up visits and hospital utilization by Medicare patients, 2007–2010. Medicare Medicaid Res Rev 2014;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kocher KE, Nallamothu BK, Birkmeyer JD, et al. Emergency department visits after surgery are common for Medicare patients, suggesting opportunities to improve care. Health Aff (Millwood) 2013;32:1600–7. [DOI] [PubMed] [Google Scholar]
- 31.Toth M, Holmes M, Van Houtven C, et al. Rural Medicare Beneficiaries Have Fewer Follow-up Visits and Greater Emergency Department Use Post-discharge. Med Care 2015;53:800–8. [DOI] [PubMed] [Google Scholar]
- 32.Grafft CA, McDonald FS, Ruud KL, et al. Effect of hospital follow-up appointment on clinical event outcomes and mortality. Arch Intern Med 2010;170:955–60. [DOI] [PubMed] [Google Scholar]
- 33.Overhage JM. Health information exchange: ‘lex parsimoniae’. Health Aff 2007;26:w595–7. [DOI] [PubMed] [Google Scholar]
- 34.MacPhail LH, Neuwirth EB, Bellows J. Coordination of diabetes care in four delivery models using an electronic health record. Med Care 2009;47:993–9. [DOI] [PubMed] [Google Scholar]
- 35.Graetz I, Reed M, Shortell SM, et al. The next step towards making use meaningful: electronic information exchange and care coordination across clinicians and delivery sites. Med Care 2014;52:1037–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mistiaen P, Poot E. Telephone follow-up, initiated by a hospital-based health professional, for post-discharge problems in patients discharged from hospital to home. Cochrane Database Syst Rev 2006:CD004510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lammers EJ, Adler-Milstein J, Kocher KE. Does health information exchange reduce redundant imaging? Evidence from emergency departments. Med Care 2014;52:227–34. [DOI] [PubMed] [Google Scholar]
- 38.Furukawa MF, King J, Patel V, et al. Despite substantial progress In EHR adoption, health information exchange and patient engagement remain low in office settings. Health Aff 2014;33:1672–9. [DOI] [PubMed] [Google Scholar]
- 39.Adler-Milstein J, DesRoches CM, Jha AK. Health information exchange among US hospitals. Am J Manag Care 2011;17:761–8. [PubMed] [Google Scholar]
- 40.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med 2010;363:501–4. [DOI] [PubMed] [Google Scholar]
- 41.Shortell SM, Casalino LP, Fisher ES. How the center for medicare and medicaid innovation should test accountable care organizations. Health Aff (Millwood) 2010;29:1293–8. [DOI] [PubMed] [Google Scholar]
- 42.Gurwitz JH, Field TS, Ogarek J, et al. An electronic health record-based intervention to increase follow-up office visits and decrease rehospitalization in older adults. J Am Ger Soc 2014;62:865–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Robelia PM, et al. (2017). “Information Transfer and the Hospital Discharge Summary: National Primary Care Provider Perspectives of Challenges and Opportunities.” J Am Board Fam Med 30(6): 758–765. [DOI] [PubMed] [Google Scholar]
- 44.Hwa K and Wren SM (2013). “Telehealth follow-up in lieu of postoperative clinic visit for ambulatory surgery: results of a pilot program.” JAMA Surg 148(9): 823–827. [DOI] [PubMed] [Google Scholar]
- 45.Kummerow Broman K, et al. (2016). “Implementation of a Telephone Postoperative Clinic in an Integrated Health System.” J Am Coll Surg 223(4): 644–651. [DOI] [PubMed] [Google Scholar]
- 46.Soegaard Ballester JM, et al. (2018). “Patient preference for time-saving telehealth postoperative visits after routine surgery in an urban setting.” Surgery 163(4): 672–679. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.