Abstract
Quantifying the COVID-19 burden is critical to public health response, resource allocation, and policies to mitigate the pandemic, reduce its impact on health and well-being, and ensure recovery and resilience of affected communities. Though a lot of research has been done worldwide on the issues of caregivers during the pandemic, the information about the Pakistani context is not sufficient. The present study aims to explore and quantify the social burden of family caregivers of COVID-19 patients in Pakistan on scientific grounds, which will be a foundation for the policy, support services, and eventually the improvements in the caregivers well-being who are facing the unrepresentative challenges during the pandemic. The present research is a cross-sectional study of family caregivers in Punjab-Pakistan during the pandemic and quantifies the social burden of COVID-19 on caregivers through a 22-item scale developed on a binary response. The study’s findings proposed a model of the social burden of caregivers based on five domains . In addition, the study observed significant associations between social burden and some profile variables, such as gender, age, marital status, occupation, income, living arrangements, and caregiving types. The research quantifies the social burden of COVID-19 on family caregivers in Pakistan and will be helpful for researchers, practitioners, and policymakers to understand the social challenges caregivers face during the COVID-19 pandemic in Pakistan.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-74613-z.
Keywords: COVID-19, Social Burden, Caregivers, Structural equation Model, Odds ratio, Tree Diagram
Subject terms: Diseases, Health care, Health occupations
Introduction
Estimating disease burden measures a population’s mortality, morbidity, and disability, highlighting health challenges, resource allocation needs, and interventions, notably concerning COVID-19’s significant societal impact1–3. The COVID-19 pandemic exacerbated global inequities, profoundly impacting health, economies, and societal well-being, especially in Asia4,5. The pandemic’s multifaceted impact encompasses morbidity and mortality, with severe cases leading to death in high-risk groups, profound economic disruptions from employment loss and lockdowns, and exacerbated psychological and social issues6–8. About 5 million deaths and over 47 million confirmed cases were recorded till May 17, 20249. The impact of COVID-19 on Asia is highly diverse, including India, China, Indonesia, and a few other countries with the highest number of cases in the region10. Similarly, Pakistan has witnessed more than 1.58 million cases and over 30 thousand deaths in the same period11.
The social cost of COVID-19 is multifaceted, with effects such as isolation, mental health issues, disturbed interpersonal relations, and increased inequality12. Quarantine measures, such as social distancing, have raised isolation and loneliness to the extreme, especially for older people and those who live alone, which affects social connections and mental health13. Psychosocial stress, in the form of disruptions of social norms and routines, has become one of the contributing factors to mental health problems, with almost every study stating higher rates of anxiety, depression, and psychological distress during the pandemic7.
Family caregivers provide essential physical, emotional, and practical support, enhancing patient compliance, companionship, and stress reduction, thereby improving psychological health and overall coping abilities12,14–17. Family caregivers serve as patient advocates within healthcare systems, ensuring needs are met and enhanced care quality, thereby improving patient outcomes and satisfaction, as substantiated by research findings14,18–21. Hence, family caregivers are the key players in the care process, and they are the ones that contribute to better disease management and overall health outcomes22–24. Family caregivers have faced many problems during the COVID-19 pandemic, such as the increase in caregiving duties, limited access to support services, and high levels of stress and anxiety14,18,25. Additionally, caregivers have to deal with the fear of getting infected, the availability of respite care is reduced, and social isolation is due to the physical distancing measures20,26,27. These difficulties affected the mental health and the well-being of the caregivers, which shows the need for targeted support and resources.
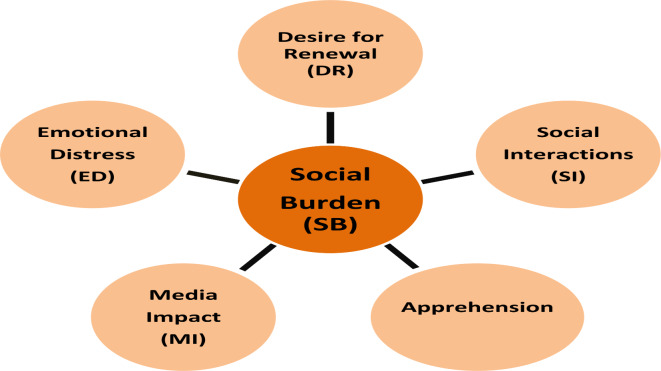
In Pakistan, family caregiving is the most frequent and culturally respected activity because of the close family relationships and traditions28. Female family members predominantly serve as caregivers for elderly, disabled, or chronically ill individuals, providing home-based care, assisting with daily activities, managing medications, and sharing emotional support14,29,30. Nevertheless, the caregiving system in Pakistan is confronted with problems such as the lack of formal support services, the poor healthcare infrastructure, and the cultural norms that may not allow for the discussion of caregiving needs and challenges29,30. Besides, the caregivers’ social and economic status can also affect how they provide care, for example, financial problems and employment opportunities for family members4. The pandemic has revealed the weaknesses of the caregiving system for family carers in Pakistan, which in turn has made the level of stress and burnout go up. Even though many studies have been done in different parts of the world on caregiver experiences during the pandemic, the Pakistani context has not been given much attention. The lack of scientific research on the social issues faced by family caregivers during COVID-19 in Pakistan underlines the fact that this area is not well studied, and, therefore, the problems of family caregivers are not fully understood or solved. This study aims to investigate the social burden experienced by family caregivers of COVID-19 survivors in Pakistan due to COVID-19. Specifically, the research seeks to explore and quantify the social burden across five sub-domains: desire for renewal, social interactions, emotional distress, media impact, and apprehension. Our central hypothesis posits that these five components significantly contribute to social burden. Additionally, the study aims to quantify the impact of these sub-domains in relation to various family caregiver profile variables. By examining these dimensions, the research seeks to provide a comprehensive understanding of the social challenges caregivers face during the pandemic.
Methodology
The study follows a cross-sectional survey research design, and the target population is the family caregivers in Punjab-Pakistan who provide care for COVID-19 patients and are from their social network. There could be many caregivers in a family, but the caregivers who provide the maximum care are the ones who enrol in the study. We assume a  ratio in determining the population of family caregivers against one registered COVID-19 patient. Because the size of the family caregivers population will be the same as that of the COVID-19 patients, we determine the sample size. The average COVID-19 infection rate in Punjab was
ratio in determining the population of family caregivers against one registered COVID-19 patient. Because the size of the family caregivers population will be the same as that of the COVID-19 patients, we determine the sample size. The average COVID-19 infection rate in Punjab was  . The COVID-19 patients without a PCR are excluded from the study. By considering the
. The COVID-19 patients without a PCR are excluded from the study. By considering the  confidence level with a
confidence level with a  margin of error, the sample size is31:
margin of error, the sample size is31:
 |
1 |
The sampled population is the family caregivers from Lahore, the capital of Punjab-Pakistan. A convenient sampling method was used to collect the data. Under this scheme, different approaches were used, including the Google form, where the online form was shared with individuals via email, social groups, etc., and they were asked to participate in the research only if they cared about a COVID-19 patient in the family. Moreover, face-to-face data was collected from the respondents interested in participating in the study. The researcher or trained enumerators contacted these respondents in public places, shopping malls, markets, home visits, institutions, offices, etc. In all these methods, formal written consent was taken from the respondents before they participated in the research. A dichotomous response scale based on  items is designed to quantify the social burden of COVID-19 on family caregivers. The proposed scale is developed based on literature review and focus group discussions with 6–8 stakeholders to collect the scale’s most effective input and adequacy. All the items on the scale are presented as yes or no, making it easier to understand and administer the scale. A pre-testing of the scale was done with the 50 respondents, and the modifications were underlined where necessary.
items is designed to quantify the social burden of COVID-19 on family caregivers. The proposed scale is developed based on literature review and focus group discussions with 6–8 stakeholders to collect the scale’s most effective input and adequacy. All the items on the scale are presented as yes or no, making it easier to understand and administer the scale. A pre-testing of the scale was done with the 50 respondents, and the modifications were underlined where necessary.
The modified questionnaire was then tested through a pilot study of 10% of respondents of the sample size, and the reliability of the questionnaire was assessed. The satisfactory results of Cronbach alpha statistics in the pilot study lead to using the developed scale for the proposed study. The objective is to reliably identify the complex problems and stressors experienced by caregivers during the pandemic. The 22-item scale covers the five domains of Social Burden (SB), including Desire for Renewal (DR), Social Interactions (SI), Emotional Distress (ED), Media Impact (MI), and Apprehension. The reliability of the 22-item scale and the respective domains are provided in Table 132. The data was screened and analyzed through SPSS v23, AMOS v24, and R-studio. The questionnaires with incomplete or inappropriate information were discarded from the analysis, and the final sample size used for analysis after screening was  .
.
Table 1.
Social Burden Domains and Reliability.
| Construct | Items | Cronbach alpha |
|---|---|---|
| Desire for Renewal (DR) | 5 | 0.775 |
| Social Interactions (SI) | 5 | 0.725 |
| Emotional Distress (ED) | 4 | 0.734 |
| Media Impact (MI) | 3 | 0.875 |
| Apprehension | 5 | 0.741 |
| Overall | 22 | 0.847 |
The Cronbach alpha values demonstrated that the developed scale has satisfactory results across all the domains of SB  . The questionnaire was designed to scale the social burden of the family caregivers (FCG) of COVID-19 survivors on five constructs. These constructs include:
. The questionnaire was designed to scale the social burden of the family caregivers (FCG) of COVID-19 survivors on five constructs. These constructs include:
Desire for renewal (DR)
The factor DR with five items covers the FCG strong will and ambition to face the difficulties, gain resilience, and seek positive change and growth in their caregiving roles and personal lives affected by the caregiving.
Social interaction (SI)
The SI domain includes the five items and covers how FCG interacts with others when dealing with their caregiving responsibilities in the face of pandemic-related problems. FCG may feel less on-person social interactions because of the physical distancing rules and isolation. They use virtual communication to contact their family, friends, and support networks.
Emotional distress (ED)
The ED used the four items to scale the FCG feelings related to being emotionally exhausted, overwhelmed, and deprived of routine social communications and accomplishments.
Media impact (MI)
This construct is measured through three items designed to quantify the MI of SB on FCG. The domain encompasses the influence of news coverage, social media, and online information on the FCG lives. The FCG is faced with a lot of information about the pandemic, which is either too much or contradictory, thus making them more anxious and stressed.
Apprehension
The construct apprehension has five items to quantify the fear, panic, disappointment, depression, worry, and anxiety faced by the FCG during the caregiving period of the pandemic.
Social burden (SB)
The latent variable SB is measured through a twenty-two-item scale representing the social hardships faced by the FCG during the disease period.
The proposed model to estimate the SB of FCG based on five constructs is depicted in Fig. 1.
Fig. 1.
Proposed research model for the SB and the associated five domains.
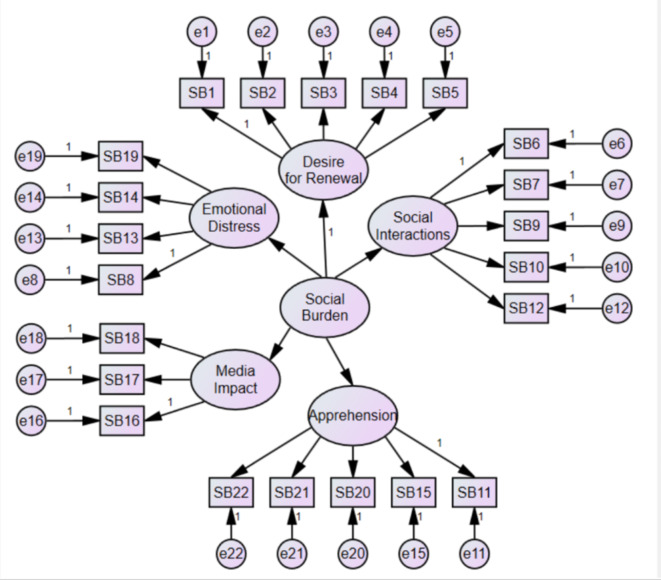
SB is the latent variable, which is estimated based on five domains with different numbers of items, and SEM33 will be used to calculate the SB. The SEM for the latent variable SB based on five constructs and associated items is shown in Fig. 2.
Fig. 2.
The proposed latent variable SB model is based on the five domains and the associated items.
The path model specified in Fig. 2 is defined in SEM notation as:
 |
2 |
where  is a column vector of items used to measure the constructs,
is a column vector of items used to measure the constructs,  is a column vector of constructs,
is a column vector of constructs,  is a matrix of coefficients of relationships between the items and the constructs, and
is a matrix of coefficients of relationships between the items and the constructs, and  is a variance-covariance matrix of relations among the residual terms of exogenous variables (
is a variance-covariance matrix of relations among the residual terms of exogenous variables ( ).
).
Equation (2) states that each domain is characterized by a structural equation linking up  ,
,  ,
,  . This implies that a group of items is used to describe the domains that are meant to be measured, as well as the residual, which is the variation that is specific to the variable and unrelated to the domain. For estimation purposes, Eq. (2) takes the form after integrating a
. This implies that a group of items is used to describe the domains that are meant to be measured, as well as the residual, which is the variation that is specific to the variable and unrelated to the domain. For estimation purposes, Eq. (2) takes the form after integrating a  variance-covariance matrix
variance-covariance matrix  of relationships amid the domains
of relationships amid the domains  :
:
 |
3 |
The maximum likelihood estimates of (3) are obtained by using the likelihood function:
 |
4 |
where,  symbolizes the sample covariance matrix and p denotes the number of items.
symbolizes the sample covariance matrix and p denotes the number of items.
Currently, a single standard measure does not exist for the model’s goodness of fit, so we rely on the commonly used fit criteria. The indices are the ones that are used to evaluate the model performance in terms of how well it fits the data. In AMOS v23, several fit indexes are available to assess the model’s goodness of fit. The goodness of fit index used in the study includes:
Goodness-of-fit index (GFI)
The GFI quantifies the proportion of variance-covariance  predicted by
predicted by  . This index is an equivalent of
. This index is an equivalent of  in regression analysis and is defined as
in regression analysis and is defined as
 |
5 |
The range of GFI is from  to
to  , and the least acceptable value for a model is at least
, and the least acceptable value for a model is at least  34,35.
34,35.
Adjusted GFI (AGFI)
The GFI is sensitive to the sample size and is affected by the number of parameters. AGFI is a modified version of GFI after adjusting the number of parameters. This index is again an analog of adjusted  as in regression analysis and is defined as
as in regression analysis and is defined as
 |
6 |
The AGFI ranges from  to
to  , and this index also has an acceptable model range of
, and this index also has an acceptable model range of  or more34,35.
or more34,35.
Chi-square/degrees of freedom 
This statistic assesses the likelihood of the difference between the population covariance matrix  and the sample covariance matrix
and the sample covariance matrix  . It is defined as
. It is defined as
 |
7 |
and, 
where, t is the number of parameters to be estimated. However, the acceptable range for this statistic is less than three. The statistic is highly sensitive to sample size and is not a good measure for large sample sizes34,35.
Root mean square error (RMSE)
The RMSE quantifies the model adequacy by considering the model complexity in terms of the number of parameters estimated and the model discrepancy. It is defined as.
 |
8 |
The statistic ranges from  to
to  , and the least acceptable value for model adequacy is
, and the least acceptable value for model adequacy is  34,35.
34,35.
Root mean square error approximation (RMSEA)
The RMSEA is a modified version of RMSE defined in Eq. (7). It is adjusted for the model degrees of freedom and defined as.
 |
9 |
The RMSEA ranges from  to
to  , and the least acceptable value for accepting a fitted model is
, and the least acceptable value for accepting a fitted model is  34. The study was approved by the IRB, Department of Statistics, GCU Lahore-Pakistan vide protocol No. St-04 A/23 dated 02-01-2023. All methods of human participation, data collection and analysis were followed accordingly. All methods were carried out in accordance with relevant guidelines and regulations. Informed consent from participants was undertaken.
34. The study was approved by the IRB, Department of Statistics, GCU Lahore-Pakistan vide protocol No. St-04 A/23 dated 02-01-2023. All methods of human participation, data collection and analysis were followed accordingly. All methods were carried out in accordance with relevant guidelines and regulations. Informed consent from participants was undertaken.
Results
This section presents the descriptive and inferential aspects of the study. Section 3.1 will present the descriptive results, Sect. 3.2 will validate the proposed model of SB presented in Figs. 1 and 2, and Sect. 3.3 present the inferential results.
Descriptive results of the study
About  of the family caregivers (FCG) are female,
of the family caregivers (FCG) are female,  are aged more than
are aged more than  years,
years,  belong to urban areas,
belong to urban areas,  are married,
are married,  are employed in some job or have some business,
are employed in some job or have some business,  live in the joint family system, and
live in the joint family system, and  of the FCG live in the same house as the COVID-19 survivor. The family monthly income for FCG is less than 30 thousand (
of the FCG live in the same house as the COVID-19 survivor. The family monthly income for FCG is less than 30 thousand ( ), from
), from  thousand to
thousand to  thousand (
thousand ( ),
),  thousand to
thousand to  thousand (
thousand ( ), and more than
), and more than  thousand (
thousand ( ). Approximately
). Approximately  of the FCG have up to a secondary level of education,
of the FCG have up to a secondary level of education,  with higher secondary,
with higher secondary,  with graduation, and
with graduation, and  with postgraduate level of education. The relationship of FCG with patients is the child (
with postgraduate level of education. The relationship of FCG with patients is the child ( ), spouse (
), spouse ( ), parents (
), parents ( ), siblings (
), siblings ( ) and others (
) and others ( ). The types of care provided by FCG are household tasks (
). The types of care provided by FCG are household tasks ( ), personal tasks (
), personal tasks ( ), and medical tasks (
), and medical tasks ( ). The average time FCG spent for caregiving is
). The average time FCG spent for caregiving is  hours or less (
hours or less ( ),
),  hours (
hours ( ), and more than
), and more than  hours (
hours ( ). The average number of days FCG spent caregiving during the pandemic is up to
). The average number of days FCG spent caregiving during the pandemic is up to  days (
days ( ),
),  days (
days ( ), and
), and  or above days (
or above days ( ). The average amount (PKR) lost by FCG due to caregiving is less than one thousand (
). The average amount (PKR) lost by FCG due to caregiving is less than one thousand ( ), one thousand to four thousand (
), one thousand to four thousand ( ), and more than four thousand (
), and more than four thousand ( ).
).
Validation of the proposed SB model
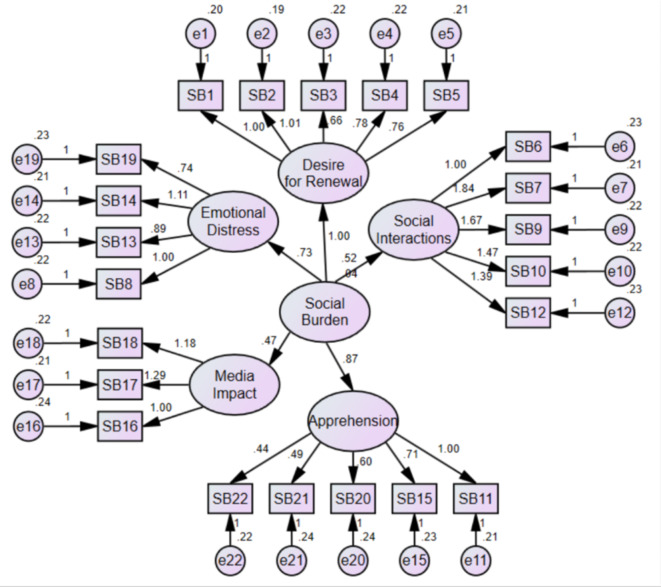
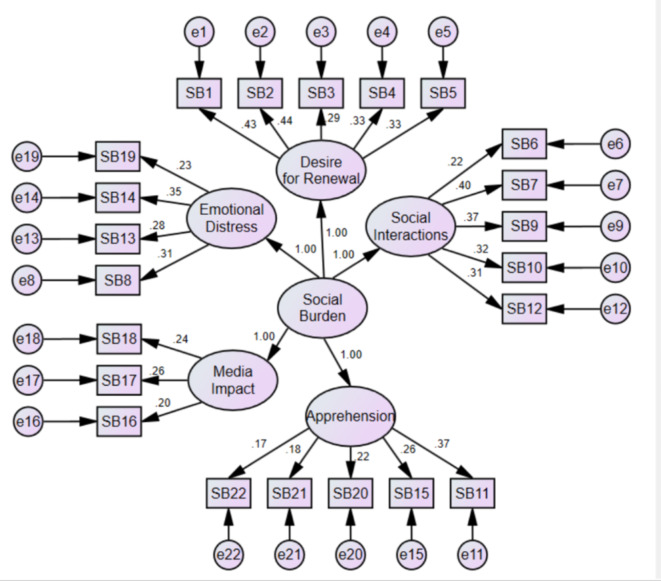
The proposed SB model in Fig. 2 is estimated using the maximum likelihood procedure under large sample properties. The estimated unstandardized coefficients are given in Fig. 3, and the standardized coefficients in Fig. 4.
Fig. 3.
Estimated unstandardized coefficients for the FCG SB.
Fig. 4.
Estimated standardized coefficients for the SB model.
In Table 2, the unstandardized and standardized regression weights, along with their error variances for the estimated SB model, are listed.
Table 2.
Regression weights for the estimated SB model along with error variances.
| Items | Weights | Error Variances |
|
|---|---|---|---|
| Unstandardized | Standardized | ||
| SB1: I think I am not fully living my life because of my caregiving responsibilities. | 1.000 | 0.429 | 0.195*** |
| SB2: I really wish that I could get rid of these circumferences. | 1.014*** | 0.437 | 0.192*** |
| SB3: The caregiving has caused a decrease in my social life. | 0.663*** | 0.285 | 0.219*** |
| SB4: Caring for my care receiver has caused me to feel emotionally exhausted. | 0.778*** | 0.329 | 0.221*** |
| SB5: I had hoped for a different outcome at this stage of my life. | 0.756*** | 0.325 | 0.215*** |
| SB6: I am not as friendly with other family members as I used to be. | 1.000 | 0.224 | 0.226*** |
| SB7: The caregiving work I do for my family is not appreciated by others. | 1.845*** | 0.403 | 0.209*** |
| SB8: My work performance is not as good as it used to be. | 1.000 | 0.314 | 0.217*** |
| SB9: I have resentment towards other relatives who could have provided help but did not. | 1.667*** | 0.365 | 0.216*** |
| SB10: My caregiving has limited me from spending time with my friends and family. | 1.471*** | 0.325 | 0.219*** |
| SB11: I might have anxiety, depression, disappointment, and loneliness as a consequence of reduced social interactions. | 1.000 | 0.370 | 0.212*** |
| SB12: Patients and their caregivers experience disruptions in social relationships. | 1.394*** | 0.306 | 0.225*** |
| SB13: My friends and family members did not connect with me because they believed caregivers could spread diseases, making me feel socially deprived. | 0.895*** | 0.280 | 0.223*** |
| SB14: It is unsafe for others to enter, and at the same time, I can’t leave either. | 1.107*** | 0.348 | 0.211*** |
| SB15: My mental health is impacted by negativity when I am isolated and alone. | 0.741*** | 0.260 | 0.232*** |
| SB16: My social life is negatively impacted by the amount and quality of information on social media. | 1.000 | 0.197 | 0.236*** |
| SB17: I was more panicked when I listened to the news during the pandemic. | 1.285*** | 0.264 | 0.211*** |
| SB18: The events, parties, functions, festivals, and gatherings can be both the sources of information and the reasons for depression and anxiety. | 1.184*** | 0.238 | 0.224*** |
| SB19: I was emotionally stressed out throughout the caring period. | 0.741*** | 0.229 | 0.235*** |
| SB20: Social isolation has badly affected my social life. | 0.602*** | 0.222 | 0.236*** |
| SB21: My fear of mass panic or suspicion of getting infected prevents me from going to hospitals. | 0.493*** | 0.183 | 0.237*** |
| SB22: I am susceptible to over-worrying and fearing my and my family’s health. | 0.440*** | 0.169 | 0.223*** |
* p<0.10, ** p<0.05, *** p<0.01. .
The SB scale items are strongly associated with their respective domains
 which conforms to the development of the scale for the quantification of FCG social constraints they faced during the pandemic. The regression weights, in confirmatory factor analysis, depict the strength of individual items’ effects on their respective domains and the overall SB, e.g., the regression weight of 1.014 for the item ‘I really wish that I could get rid of these circumstances’ indicates a strong and statistically significant (p < 0.01) impact of this item on the ‘desire for renewal’ domain. This high regression weight could mean that the aspect of social strain highly influences the caregivers who want to get away from their situations. The significant p-value (p < 0.01) confirms that this item reliably contributes to measuring the ‘desire for renewal’ domain, affecting the overall assessment of SB. This analysis assists in identifying which particular aspects of caregivers’ experiences are most likely to contribute to their perceived SB. The rest of the items can be explained in the similar fashion. A number of goodness of fit indices are used to evaluate the proposed FCG SB model for acceptance or rejection and are presented in Table 3.
which conforms to the development of the scale for the quantification of FCG social constraints they faced during the pandemic. The regression weights, in confirmatory factor analysis, depict the strength of individual items’ effects on their respective domains and the overall SB, e.g., the regression weight of 1.014 for the item ‘I really wish that I could get rid of these circumstances’ indicates a strong and statistically significant (p < 0.01) impact of this item on the ‘desire for renewal’ domain. This high regression weight could mean that the aspect of social strain highly influences the caregivers who want to get away from their situations. The significant p-value (p < 0.01) confirms that this item reliably contributes to measuring the ‘desire for renewal’ domain, affecting the overall assessment of SB. This analysis assists in identifying which particular aspects of caregivers’ experiences are most likely to contribute to their perceived SB. The rest of the items can be explained in the similar fashion. A number of goodness of fit indices are used to evaluate the proposed FCG SB model for acceptance or rejection and are presented in Table 3.
Table 3.
The goodness of fit indices of the proposed SB SEM model.
| Indices | Values |
|---|---|
| GFI | 0.957 |
| AGFI | 0.948 |
| Chi-square/df | 11.273 |
| RMR | 0.010 |
| RMSEA | 0.043 |
The chi-square/df goodness of fit index is greater than the acceptable cutoff ( ) and is a poor index to use for sample sizes over
) and is a poor index to use for sample sizes over  . The goodness of fit indices less or not sensitive to sample sizes reported in Table 3 are in an acceptable range with respect to their cutoffs, e.g.,
. The goodness of fit indices less or not sensitive to sample sizes reported in Table 3 are in an acceptable range with respect to their cutoffs, e.g.,  (
( ),
), 
 ),
),  (
( ) and
) and  (
( ).
).
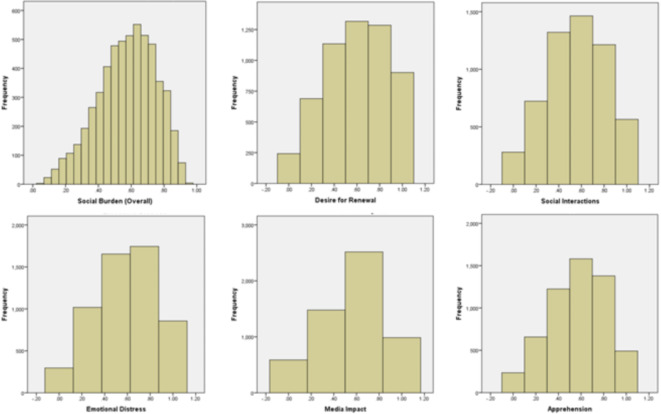
Estimation of SB and associated domains
The results presented in Table 4; Fig. 5 quantify the SB and associated domains. The mean SB score is 0.574 ± 0.18, with a range of 0.05–0.95, reflecting a moderate level of SB experienced by the caregivers. This value is quantified on a dichotomous scale where ‘0’ stands for ‘No’ SB and ‘1’ is for the ‘Highest’ SB, which means that the caregivers are halfway through the maximum level of burden. The value 0.18 depicts the degree of dispersion from the mean, indicating that most of the caregivers experiences are likely to be within this range but can be different. The range of 0.05 to 0.95 reveals that while some caregivers perceive nearly no burden (close to 0), others feel almost the highest burden (close to 1), indicating that the pandemic affects caregivers SB in different ways. The significance of the SB is tested against the assumed hypothetical value of SB to 0.5. The first part of Fig. 5 shows the distribution of SB the caregivers face. The same can be depicted for the statistics under domains of SB presented in Table 4; Fig. 5.
Table 4.
Descriptive statistics of SB and associated domains.
| Construct | N | Minimum | Maximum | Mean | Std. Deviation |
|---|---|---|---|---|---|
| Social Burden (SB)*** | 5568 | .05 | .95 | .5736 | .17693 |
| Desire for Renewal (DR)*** | 5568 | .00 | 1.00 | .5946 | .28053 |
| Social Interactions (SI)*** | 5568 | .00 | 1.00 | .5546 | .26699 |
| Emotional Distress (ED)*** | 5568 | .00 | 1.00 | .5829 | .27545 |
| Media Impact (MI)*** | 5568 | .00 | 1.00 | .5669 | .29342 |
| Apprehension*** | 5568 | .00 | 1.00 | .5683 | .25664 |
* p < 0.10 , ** p < 0.05 , *** p < 0.01 .
Fig. 5.
Distribution of SB and associated domains.
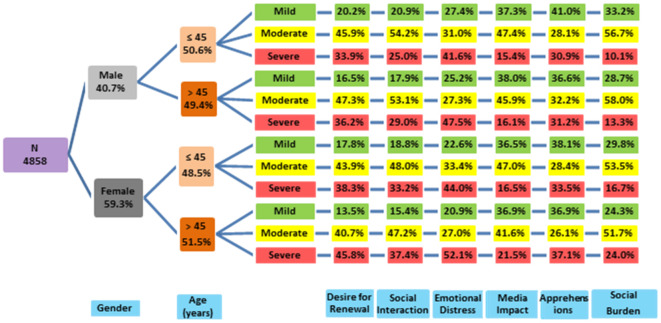
Some further classification of FCG on SB and respective domains with respect to age and gender is portrayed in Fig. 6.
Fig. 6.
Tree diagram of Gender and Age-wise SB of FCG with respect to constructs.
The results presented in Table 5 are the univariate odds ratio (OR) with  confidence limits of COVID-19 FCG profile variables and the five constructs of the SB. These statistics, with their possible significance, are used to test the research objective of exploring the SB of FCG with respect to their demographics. Female FCG are affected more socially than male FCG. The DR of female FCG is
confidence limits of COVID-19 FCG profile variables and the five constructs of the SB. These statistics, with their possible significance, are used to test the research objective of exploring the SB of FCG with respect to their demographics. Female FCG are affected more socially than male FCG. The DR of female FCG is  times higher than male FCG. This implies that female caregivers are more likely to find or look for a way to recharge or be free from their caregiving duties compared to male caregivers. The SI of female FCG is
times higher than male FCG. This implies that female caregivers are more likely to find or look for a way to recharge or be free from their caregiving duties compared to male caregivers. The SI of female FCG is  times more affected than the male FCG, indicating that female caregivers experience a greater disruption in their social lives than male caregivers. The female FCG experienced
times more affected than the male FCG, indicating that female caregivers experience a greater disruption in their social lives than male caregivers. The female FCG experienced  times more ED than the male FCG, suggesting that women go through immense emotional exhaustion and psychological stress in caring for their relatives as compared to men. Although the media did not significantly affect gender, female FCG was
times more ED than the male FCG, suggesting that women go through immense emotional exhaustion and psychological stress in caring for their relatives as compared to men. Although the media did not significantly affect gender, female FCG was  times more affected than male FCG. In particular, the study shows that although there was no significant difference between the overall media effect on male and female caregivers, media exposure had slightly more adverse effects on women than on men. The OR
times more affected than male FCG. In particular, the study shows that although there was no significant difference between the overall media effect on male and female caregivers, media exposure had slightly more adverse effects on women than on men. The OR  for female FCG against the variable apprehension indicates that women who provided care for family members during the COVID-19 pandemic experienced significantly
for female FCG against the variable apprehension indicates that women who provided care for family members during the COVID-19 pandemic experienced significantly  times more fear and anxiety compared to their male counterparts. The overall SB on female FCG is
times more fear and anxiety compared to their male counterparts. The overall SB on female FCG is  times higher than that of male caregivers, amplifying women’s various difficulties in caregiving situations.
times higher than that of male caregivers, amplifying women’s various difficulties in caregiving situations.
Table 5.
The odds ratio with  CI of five SB constructs with FCG profile.
CI of five SB constructs with FCG profile.
| Profile | Categories | Desire for Renewal (DR) |
Social Interactions (SI) |
Emotional Distress (ED) |
Media Impact (MI) |
Apprehension | Social Burden (SB) |
|---|---|---|---|---|---|---|---|
| Gender | Male | ||||||
| Female |
1.591*** [1.315, 1.926] |
1.787*** [1.461, 2.185] |
1.490*** [1.227, 1.809] |
1.167* [0.973, 1.400] |
1.471*** [1.194, 1.812] |
2.675*** [1.975, 3.623] |
|
| Age | ≤ 45 years | ||||||
| > 45 years |
1.681*** [1.393, 2.030] |
1.587*** [1.302, 1.934] |
1.666*** [1.375, 2.018] |
1.195* [0.999, 1.430] |
1.227* [1.000, 1.507] |
2.530*** [1.875, 3.413] |
|
| Marital Status | Single | ||||||
| Married |
1.195 [0.989, 1.445] |
1.268** [1.038, 1.548] |
1.334*** [1.099, 1.620] |
1.255** [1.047, 1.505] |
1.275** [1.036, 1.570] |
1.741*** [1.287, 2.354] |
|
| Occupation | Employed | ||||||
| Unemployed |
1.369*** [1.120, 1.673] |
1.144 [0.928, 1.412] |
1.390*** [1.133, 1.705] |
1.071 [0.885, 1.297] |
1.491*** [1.198, 1.857] |
1.847*** [1.342, 2.541] |
|
| Education | Matriculation or above | ||||||
| Below Matriculation |
1.198 [0.920, 1.561] |
1.029 [0.780, 1.359] |
1.164 [0.889, 1.523] |
1.116 [0.866, 1.437] |
1.183 [0.886, 1.579] |
1.358 [0.894, 2.063] |
|
| Income (PKR) | ≤ 60,000 | ||||||
| > 60,000 |
1.167 [0.961, 1.418] |
0.988 [0.806, 1.211] |
1.356*** [1.113, 1.652] |
1.302*** [1.081, 1.567] |
0.978 [0.791, 1.209] |
1.355* [0.997, 1.842] |
|
| Area | Urban | ||||||
| Rural |
1.182 [0.943, 1.480] |
1.454*** [1.146, 1.843] |
1.056 [0.840, 1.327] |
0.835* [0.674, 1.034] |
0.917 [0.718, 1.172] |
1.225 [0.857, 1.751] |
|
| Living Type | Nuclear | ||||||
| Joint |
1.369*** [1.129, 1.659] |
1.653*** [1.350, 2.024] |
1.233** [1.014, 1.499] |
1.346*** [1.121, 1.618] |
1.578*** [1.279, 1.948] |
2.365*** [1.743, 3.209] |
|
|
Living Place |
Away | ||||||
| Same |
1.289** [1.060, 1.567] |
1.225* [0.998, 1.504] |
1.350*** [1.107, 1.647] |
1.307*** [1.085, 1.575] |
1.242** [1.003, 1.537] |
1.795*** [1.318, 2.446] |
|
| Caregiving Type (Households Tasks) | No | ||||||
| Yes |
1.992*** [1.550, 2.559] |
1.873*** [1.438, 2.440] |
1.454*** [1.126, 1.877] |
1.441*** [1.134, 1.830] |
2.059*** [1.556, 2.706] |
3.858*** [2.601, 5.721] |
|
| Caregiving Type (Personal Tasks) | No | ||||||
| Yes |
1.362*** [1.106, 1.678] |
1.549*** [1.244, 1.928] |
1.441*** [1.165, 1.781] |
1.276** [1.046, 1.556] |
1.412*** [1.124, 1.772] |
2.262*** [1.628, 3.144] |
|
| Caregiving Type (Medical Tasks) | No | ||||||
| Yes |
1.209* [0.988, 1.479] |
1.394*** [1.128, 1.723] |
1.273** [1.037, 1.563] |
1.361*** [1.122, 1.649] |
1.430*** [1.147, 1.782] |
1.957*** [1.423, 2.692] |
* p < 0.10, ** p < 0.05, *** p < 0.01.
The FCG aged more than  years reported
years reported  times higher SB than the comparative counterpart
times higher SB than the comparative counterpart  . The
. The  of
of  for the variable marital status depicted that married FCG experienced an elevated
for the variable marital status depicted that married FCG experienced an elevated  times SB than the single caregivers. The unemployed FCG faced
times SB than the single caregivers. The unemployed FCG faced  times greater social liability than the employed FCG. This difference shows that employment status moderates the social cost of caregiving during the COVID-19 pandemic. Below matriculation, FCG reported
times greater social liability than the employed FCG. This difference shows that employment status moderates the social cost of caregiving during the COVID-19 pandemic. Below matriculation, FCG reported  times higher SB than the counterpart caregivers. The FCG living in a joint family system and the same place reported
times higher SB than the counterpart caregivers. The FCG living in a joint family system and the same place reported  and
and  times greater social liability than the competitive groups. Caregiving types by FCG of COVID-19 patients are strongly associated with the SB, e.g., the OR for household tasks (
times greater social liability than the competitive groups. Caregiving types by FCG of COVID-19 patients are strongly associated with the SB, e.g., the OR for household tasks ( ), personal tasks (
), personal tasks ( ) and medical tasks (
) and medical tasks ( ) suggest that FCG faced an elevated SB than the competitive counterparts.
) suggest that FCG faced an elevated SB than the competitive counterparts.
Discussions
The present study proposed a social strain model of FCG based on five social domains using the confirmatory factor analysis, as previous studies used the methods under similar objectives26,36,37. The Social Burden scale has also shown that items have significant correlations with their respective domains  , which proves the construct validity of this measure of social constraints for FCGs
, which proves the construct validity of this measure of social constraints for FCGs  . This alignment also emphasizes the stability of the scale in terms of the factors mentioned above like Desire for Renewal (DR), Social Interactions (SI), Emotional Distress (ED), Media Impact (MI) and Apprehension which are multiphased issues that FCGs have to deal with during the pandemic. Therefore, it is suggested that this scale be used to measure the intensity of the social costs caregivers face in crises. The overall mean SB estimated to be 0.57 among FCG of COVID-19 patients shows that FCG faced a moderate to high burden during the pandemic, affecting the caregivers social well-being. This result of the moderate effect of SB on FCG is consistent with prior studies22,26. The results indicate that the domains of SB, including the DR, SI, ED, MI and Apprehension, moderately influence the FCG. As noted in the previous investigations19,22,23,25,26,38, our study findings reveal the importance of specific support interventions for caregivers, including providing a break from caregiving, strengthening social networks, providing psychological services, controlling media exposure, and alleviating fear about the future.
. This alignment also emphasizes the stability of the scale in terms of the factors mentioned above like Desire for Renewal (DR), Social Interactions (SI), Emotional Distress (ED), Media Impact (MI) and Apprehension which are multiphased issues that FCGs have to deal with during the pandemic. Therefore, it is suggested that this scale be used to measure the intensity of the social costs caregivers face in crises. The overall mean SB estimated to be 0.57 among FCG of COVID-19 patients shows that FCG faced a moderate to high burden during the pandemic, affecting the caregivers social well-being. This result of the moderate effect of SB on FCG is consistent with prior studies22,26. The results indicate that the domains of SB, including the DR, SI, ED, MI and Apprehension, moderately influence the FCG. As noted in the previous investigations19,22,23,25,26,38, our study findings reveal the importance of specific support interventions for caregivers, including providing a break from caregiving, strengthening social networks, providing psychological services, controlling media exposure, and alleviating fear about the future.
The expressions of the DR domain are significantly associated with its latent variable and reflect the intensity of burdensome that FCG observes in their caregiving role during the pandemic as it tends to interfere with personal goals and personal satisfaction. The caregivers believe that had they been given their expectancies, they might have a better life. Such burdens, combined with the fast pace of the entire process, may not be what caregivers expected to do as their lives progressed or what they had in mind as the lives they wanted to live. The FCG was offensive, and the restriction or figurative restraint through caregiving established in the present research also came forth in different research relating to the effect of caregiving on the FCG general well-being14,22,23,25. In addition, the study highlighted that the conventional family roles tend to place more emphasis on females becoming carers, and hence, there is more physical and psychological fatigue. The desire for escape or replacement, as indicated in a past study by39 is higher for women as they are more likely to perceive that caregiving exhausts them.
The items related to social relationships are significantly associated with the latent variable SI ( ). In this domain of SB, the FCG highlighted how the pandemic disrupted their social relationships and interactions. The pandemic put the FCG in a situation different from anything they had experienced before, and thus, how to communicate with others or move around became affected. The results from the previous studies from Italy26, the United States21, Utah40, Australia41, India42, Bangladesh43, and Pakistan29 are reflections of our findings of disruptions in the social lives of FCG.
). In this domain of SB, the FCG highlighted how the pandemic disrupted their social relationships and interactions. The pandemic put the FCG in a situation different from anything they had experienced before, and thus, how to communicate with others or move around became affected. The results from the previous studies from Italy26, the United States21, Utah40, Australia41, India42, Bangladesh43, and Pakistan29 are reflections of our findings of disruptions in the social lives of FCG.
The statements quantifying the emotional hardships and deprivations of the FCG during the pandemic are significantly related to the latent variable ED ( ). The FCG highlighted how they were deprived of society, friends, relatives, and family due to caregiving during COVID-19. The misconception and the fear of getting infected by others who have been stigmatized are also contributing to social isolation. The limited mobility and the safety concerns of FCG lead them to stay at home, which, in turn, results in loneliness and deprivation. The earlier studies reported FCG deprivation due to caregiving during the pandemic are14,16,38,44.
). The FCG highlighted how they were deprived of society, friends, relatives, and family due to caregiving during COVID-19. The misconception and the fear of getting infected by others who have been stigmatized are also contributing to social isolation. The limited mobility and the safety concerns of FCG lead them to stay at home, which, in turn, results in loneliness and deprivation. The earlier studies reported FCG deprivation due to caregiving during the pandemic are14,16,38,44.
The items under the domain of media’s influence highlight the importance of media in shaping the perception of caregivers. The statements are significantly associated with the latent variable MI ( ). The FCG reported that media greatly affected their perceptions, views, and feelings towards COVID-19 and shaped their caregiving like never before. The FCG were more anxious and stressed since they were constantly exposed to the news about the pandemic, which is primarily alarming. Misinformation and the media’s different opinions were among the factors that made FCG uneasy. The impact of media reporting on caregivers is highlighted by many past researches12,14,41,45and is consistent with our study outcome. The FCG of COVID-19 patients reported an affliction with various apprehensions, including fear and anxiety about their loved ones’ health and safety. The fear of infection and transmission within their households was a common concern for the FCG, which made them take more vigilance and precautions. In agreement with past studies17,24,27,46–48, the apprehensions were intensified because they did not know the progression of the disease and had limited access to healthcare services.
). The FCG reported that media greatly affected their perceptions, views, and feelings towards COVID-19 and shaped their caregiving like never before. The FCG were more anxious and stressed since they were constantly exposed to the news about the pandemic, which is primarily alarming. Misinformation and the media’s different opinions were among the factors that made FCG uneasy. The impact of media reporting on caregivers is highlighted by many past researches12,14,41,45and is consistent with our study outcome. The FCG of COVID-19 patients reported an affliction with various apprehensions, including fear and anxiety about their loved ones’ health and safety. The fear of infection and transmission within their households was a common concern for the FCG, which made them take more vigilance and precautions. In agreement with past studies17,24,27,46–48, the apprehensions were intensified because they did not know the progression of the disease and had limited access to healthcare services.
Although the overall influence of media on caregivers did not vary considerably between genders, female caregivers have marginally higher negative media exposure than male counterparts. This finding of the study is according to49. The study50 findings are also brought into line with our result that female FCG expressed much higher levels of fear and anxiety during COVID-19 than male ones. The finding that FCG aged over  years caring for COVID-19 patients have twice the social liability of their counterparts below
years caring for COVID-19 patients have twice the social liability of their counterparts below  is supported by previous studies14,15,21,22,25,51,52. Older caregivers are at a higher risk for developing health complications and diseases simply because of their age and thus place themselves at risk of developing the effects of caregiving and the stress that comes with caring for a family-infected member. Fear of getting infected themselves or infecting their susceptible relatives worsens their social problems. Our findings imply that marital status is related to the increased social demands for caregivers. It is, however, worth noting that married caregivers have the challenge of taking care of the household work and the children in addition to caring for the COVID-19 patient. The multiple roles are connected to a higher degree of stress and social demands. Marriage is helpful as it can address psychological needs and enhance caregiving activities, as the spouses may depend on one another. This dependence can result in more social burdens, especially if one of the spouses becomes infected with COVID-19. This finding is consistent with other research5,14,20,22,26,38,51,52 in the literature.
is supported by previous studies14,15,21,22,25,51,52. Older caregivers are at a higher risk for developing health complications and diseases simply because of their age and thus place themselves at risk of developing the effects of caregiving and the stress that comes with caring for a family-infected member. Fear of getting infected themselves or infecting their susceptible relatives worsens their social problems. Our findings imply that marital status is related to the increased social demands for caregivers. It is, however, worth noting that married caregivers have the challenge of taking care of the household work and the children in addition to caring for the COVID-19 patient. The multiple roles are connected to a higher degree of stress and social demands. Marriage is helpful as it can address psychological needs and enhance caregiving activities, as the spouses may depend on one another. This dependence can result in more social burdens, especially if one of the spouses becomes infected with COVID-19. This finding is consistent with other research5,14,20,22,26,38,51,52 in the literature.
The social liability for the unemployed FCG of COVID-19 patients was  times higher compared to the employed caregivers. Unemployment might lead to financial constraints, making it challenging for caregivers to get the things they desire and meet the needs of the care recipients. Thus, SB can have adverse interactions with financial stress, and this finding is also reflected by previous studies, e.g5,22,46,48,51,53. , . The living arrangements and proximity of FCG to the care recipients significantly impact their social problems. A joint family system may cause FCG to have higher social liability as there is a higher likelihood of them carrying more caregiving responsibilities, and there may be conflicts between family members. These findings also coincide with past investigations12,16,19,25,54. The FCG reported high SB in household duties, including cooking, cleaning, and other responsibilities for copying household matters. Personal care, including bathing, dressing, and grooming, is also significantly associated with an elevated SB. The other correlation identified concerning SB among FCG entailed medical tasks, including administration of medications, observations of vital signs, and provision for medical needs. The association of caregiving types with the SB is also evident in studies17,23,25,41,51,55 in the literature.
times higher compared to the employed caregivers. Unemployment might lead to financial constraints, making it challenging for caregivers to get the things they desire and meet the needs of the care recipients. Thus, SB can have adverse interactions with financial stress, and this finding is also reflected by previous studies, e.g5,22,46,48,51,53. , . The living arrangements and proximity of FCG to the care recipients significantly impact their social problems. A joint family system may cause FCG to have higher social liability as there is a higher likelihood of them carrying more caregiving responsibilities, and there may be conflicts between family members. These findings also coincide with past investigations12,16,19,25,54. The FCG reported high SB in household duties, including cooking, cleaning, and other responsibilities for copying household matters. Personal care, including bathing, dressing, and grooming, is also significantly associated with an elevated SB. The other correlation identified concerning SB among FCG entailed medical tasks, including administration of medications, observations of vital signs, and provision for medical needs. The association of caregiving types with the SB is also evident in studies17,23,25,41,51,55 in the literature.
Conclusion
The present study aimed to quantify the social issues faced by the family caregivers of COVID-19 patients in Punjab-Pakistan. We explored and discussed the social effect of COVID-19 along with its different domains on family caregivers. The study findings depict that the social burden, along with its proposed domains of desire for renewal, social interactions, emotional distress, media impact, and apprehension, moderately affects family caregivers. The results established the associations between social burden and domains with the family caregivers profile variables like gender, age, income, living arrangements, caregiving types, etc. The research outcomes suggest that policymakers and healthcare practitioners arrange programs to raise awareness of caregiving issues, projects to facilitate access to healthcare services, and programs to strengthen the social support networks for caregivers in Pakistan. The cooperative initiatives of the government, civil society, and healthcare organizations are the key to the development of family caregivers and the assistance they provide their loved ones with the best care.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
Conceptualization: Jamal Abdul Nasir.Data Collection: Shumaila Abbas.Investigation: Shumaila Abbas.Methodology: Shumaila Abbas, Jamal Abdul Nasir.Software: Shumaila Abbas.Supervision: Jamal Abdul Nasir.Writing – original draft: Shumaila Abbas.Writing – review & editing: Jamal Abdul Nasir.
Data availability
The data will be available on a reasonable request from the corresponding author.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Miller, I. F. et al. Disease and healthcare burden of COVID-19 in the United States. 26(8): pp. 1212–1217. (2020). [DOI] [PubMed]
- 2.Collins, T. et al. Addressing the double burden of the COVID-19 and noncommunicable disease pandemics: a new global governance challenge. 26(2): pp. 199–212. (2021).
- 3.Murray, C. J. J. N. The global burden of disease study at 30 years. 28(10): pp. 2019–2026. (2022). [DOI] [PubMed]
- 4.Rasul, G. et al. Socio-economic implications of COVID-19 pandemic in South Asia: emerging risks and growing challenges. 6: p. 629693. (2021). [DOI] [PMC free article] [PubMed]
- 5.Sheikhbardsiri, H. et al. Investigating the burden of disease dimensions (time-dependent, developmental, physical, social and emotional) among family caregivers with COVID-19 patients in Iran. 23(1): p. 165. (2022). [DOI] [PMC free article] [PubMed]
- 6.Zhang, J. et al. Risk and protective factors for COVID-19 morbidity, severity, and mortality. 64(1): pp. 90–107. (2023). [DOI] [PMC free article] [PubMed]
- 7.Dubey, S. et al. Psychosocial impact of COVID-19. 14(5): pp. 779–788. (2020). [DOI] [PMC free article] [PubMed]
- 8.Richards, F. et al. Economic burden of COVID-19: a systematic review. : pp. 293–307. (2022). [DOI] [PMC free article] [PubMed]
- 9.WHO, COVID-19 Epidemiological Update. pp. 1–28. (2024).
- 10.Jones, G. Impact of COVID-19 on mortality in Asia. 19(2): pp. 131–147. (2023).
- 11.Javed, H. et al. Evolution of COVID-19 infection in Punjab; trends during five waves of infection in the province of Punjab. 24(1): p. 348. (2024). [DOI] [PMC free article] [PubMed]
- 12.Fieselmann, J. et al. Additional burdens of family caregivers during the COVID-19 pandemic: a qualitative analysis of social media in Germany. 24(2): pp. 414–422. (2022). [DOI] [PMC free article] [PubMed]
- 13.Völker, B. J. S. N. Networks in lockdown: The consequences of COVID-19 for social relationships and feelings of loneliness. 72: pp. 1–12. (2023). [DOI] [PMC free article] [PubMed]
- 14.Rahimi, T. & Dastyar, N. and F.J.B.f.p. Rafati, experiences of family caregivers of patients with COVID-19. 22: pp. 1–10. (2021). [DOI] [PMC free article] [PubMed]
- 15.Cohen, S. A. et al. Exploring changes in caregiver burden and caregiving intensity due to COVID-19. 7: p. 2333721421999279. (2021). [DOI] [PMC free article] [PubMed]
- 16.Dellafiore, F. et al. The impact of COVID-19 pandemic on family caregivers’. Mental Health: Rapid Syst. Rev. Curr. Evid. (2022). 93(Suppl 2). [DOI] [PMC free article] [PubMed]
- 17.Najafi Ghezeljeh, T. et al. Exploring family caregiver challenges in caring for patients with COVID-19 in intensive care units. 11: p. 1057396. (2023). [DOI] [PMC free article] [PubMed]
- 18.Nia, M. N. et al. The effects of family-centered empowerment model on depression, anxiety, and stress of the family caregivers of patients with COVID-19: a randomized clinical trial. 23(1): p. 185. (2022). [DOI] [PMC free article] [PubMed]
- 19.Irani, E. & Niyomyart, A. and R.L.J.C.n.r. Hickman Jr, Family caregivers’ experiences and changes in caregiving tasks during the COVID-19 pandemic. 30(7): pp. 1088–1097. (2021). [DOI] [PMC free article] [PubMed]
- 20.Jafari-Oori, M. et al. Psychiatric distress in family caregivers of patients with COVID-19. 37: pp. 69–75. (2022). [DOI] [PMC free article] [PubMed]
- 21.Russell, B. S. et al. Short-term impacts of COVID-19 on family caregivers: Emotion regulation, coping, and mental health. 78(2): pp. 357–374. (2022). [DOI] [PMC free article] [PubMed]
- 22.Beach, S. R. et al. Family caregiving during the COVID-19 pandemic. 61(5): pp. 650–660. (2021). [DOI] [PMC free article] [PubMed]
- 23.Robinson-Lane, S. G. et al. Caregiving in the COVID-19 pandemic: family adaptations following an intensive care unit hospitalisation. 33(1): pp. 203–214. (2024). [DOI] [PMC free article] [PubMed]
- 24.Thapa, P. et al. Family caregiver experience of caring COVID-19 patients admitted in COVID-19 hospital of a tertiary care hospital in Nepal. 19(1): p. e0295395. (2024). [DOI] [PMC free article] [PubMed]
- 25.Lightfoot, E. et al. Concerns of family caregivers during COVID-19: the concerns of caregivers and the surprising silver linings, in COVID-19 and Older Adults. Routledge. 88–107. (2023). [DOI] [PubMed]
- 26.Fusar-Poli, L. et al. Psychological well-being and family distress of Italian caregivers during the COVID-19 outbreak. 50(5): pp. 2243–2259. (2022). [DOI] [PubMed]
- 27.Soluk Özdemir, Y. et al. COVID-19-related anxiety and obsession levels in stroke patients and family caregivers and their effects on caregiver burden. : pp. 1–8. (2024). [DOI] [PubMed]
- 28.Jabeen, S. et al. Experiences of family caregivers in dealing with cases of advanced breast cancer: a qualitative study of the sociocultural context in Punjab. Pakistan. 24 (1), 1030 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mansoor, T., Mansoor, S. & U.J.A.o.K.E M.U. bin Zubair, ‘Surviving COVID-19’: Illness narratives of patients and family members in Pakistan. 26(Special Issue): pp. 157–164. (2020).
- 30.Rashid, M. A. H. et al. Religious coping, care burden and psychological distress among informal caregivers of COVID-19 patients: Results of a cross-sectional survey in Pakistan. 69(6): pp. 1369–1376. (2023). [DOI] [PMC free article] [PubMed]
- 31.Althubaiti, A. J. J. G. & Medicine, F. Sample size determination: A practical guide for health researchers. 24(2): pp. 72–78. (2023). [DOI] [PMC free article] [PubMed]
- 32.Kennedy, I. J. B. Sample size determination in test-retest and Cronbach alpha reliability estimates. J. O C E. 2 (1), 17–29 (2022). [Google Scholar]
- 33.Kline, R. B. Principles and Practice of Structural Equation Modeling (Guilford, 2023).
- 34.West, S. G. et al. Model fit in structural equation modeling. 2: pp. 184–205. (2023).
- 35.Collier, J. Applied Structural Equation Modeling Using AMOS: Basic to Advanced Techniques (Routledge, 2020).
- 36.Mohammadi Ferizi, M. et al. COVID-19 pandemic and the mental health of caregivers of the elderly with chronic diseases. 20(2): pp. 225–236. (2022).
- 37.Lalani, N. et al. Structural equation model of coping and life satisfaction of community-dwelling older people during the COVID-19 pandemic. 7(1): p. 46. (2023). [DOI] [PMC free article] [PubMed]
- 38.Chiu, M. Y. et al. Family caregiving during the COVID-19 pandemic: factors associated with anxiety and depression of carers for community-dwelling older adults in Hong Kong. 22(1): p. 125. (2022). [DOI] [PMC free article] [PubMed]
- 39.Pinquart, M., S.J.T.J.o.G.S.B.P, S., Sörensen & Sciences, S. Gender differences in caregiver stressors, social resources, and health: An updated meta-analysis. 61(1): pp. P33-P45. (2006). [DOI] [PubMed]
- 40.Bristol, A. A. et al. You feel very isolated: Effects of COVID-19 pandemic on caregiver social connections. 7: p. 23337214211060166. (2021). [DOI] [PMC free article] [PubMed]
- 41.Hunter, S. C. et al. Family life during and beyond COVID-19: the impact of relationship quality on caregivers’ management of paid work, caregiving, and self-care. 45(3): pp. 647–673. (2024).
- 42.Balachandran, K. P. & Mohanraj, B. Family Carers During the COVID-19 Pandemic: A Paradigm Shift in Caregiving, in Community Mental Health and Well-Being in the New Normal. IGI Global. pp. 122–140. (2023).
- 43.Nasrin, N. et al. A qualitative investigation of stressful life events and mental health disorders: The views of patients and caregivers in Bangladesh. 18(2): p. e0281649. (2023). [DOI] [PMC free article] [PubMed]
- 44.Berntzen, H. et al. Coping in times of disruption and deprivation—Experiences of family members during COVID-19 patients’ critical illness: A qualitative study. 10(7): pp. 4825–4837. (2023). [DOI] [PMC free article] [PubMed]
- 45.McCaughey, D. et al. Public health messaging during the COVID-19 pandemic and its impact on family Caregivers’ COVID-19 knowledge. 18(1): p. 75. (2022). [DOI] [PMC free article] [PubMed]
- 46.Picardi, A. et al. A qualitative study regarding COVID-19 inpatient family caregivers’ need for supportive care. 17: p. 161. (2021). [DOI] [PMC free article] [PubMed]
- 47.Muldrew, D. H. et al. Impact of the COVID-19 pandemic on family carers in the community: a scoping review. 30(4): pp. 1275–1285. (2022). [DOI] [PubMed]
- 48.Parmar, J. et al. Double-duty caregivers enduring COVID-19 pandemic to endemic:it’s just wearing me down. 19(4): p. e0298584. (2024). [DOI] [PMC free article] [PubMed]
- 49.Bueno, M. V., J.-A.D.J.W.J.o.N, R. & Chase Gend. Differences Adverse Psychosocial Outcomes among Family Caregivers: Syst. Rev.45(1): 78–92. (2023). [DOI] [PubMed] [Google Scholar]
- 50.Fernandez, C. The Impact of the COVID-19 Pandemic on Compassion Fatigue in Healthcare Workers (The Chicago School of Professional Psychology, 2023).
- 51.Mirzaei, A. et al. Evaluation of family caregiver burden among COVID-19 patients. 13(1). (2020).
- 52.Ebrahimi, H. et al. Care burden of home caregivers of patients with COVID-19. 32(208): pp. 75–83. (2022).
- 53.Phillips, D. et al. The invisible workforce during the COVID-19 pandemic: Family carers at the frontline. 3. (2020). [DOI] [PMC free article] [PubMed]
- 54.Noguchi, T. et al. Association between family caregivers and depressive symptoms among community-dwelling older adults in Japan: a cross-sectional study during the COVID-19 pandemic. 96: p. 104468. (2021). [DOI] [PMC free article] [PubMed]
- 55.Truskinovsky, Y. et al. Caregiving in a pandemic: COVID-19 and the well-being of family caregivers 55 + in the United States. 79(5): pp. 663–675. (2022). [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data will be available on a reasonable request from the corresponding author.