Abstract
Quadriceps weakness after anterior cruciate ligament reconstruction (ACLR) is a well-known phenomenon, with more persistent quadriceps weakness observed after ACLR with a bone-patellar tendon-bone or quadriceps tendon autograft than with a hamstring tendon autograft. Longstanding quadriceps weakness after ACLR has been associated with suboptimal postoperative outcomes and the progression of radiographic knee osteoarthritis, making the recovery of quadriceps size and strength a key component of ACLR rehabilitation. However, few articles have been written for the specific purpose of optimizing quadriceps size and strength after ACLR. Therefore, the purpose of this review article is to integrate the existing quadriceps muscle basic science and strength training literature into a best-evidence synthesis of exercise methodologies for restoring quadriceps size and strength after ACLR, as well as outline an evidence-informed quadriceps load-progression for recovering the knee’s capacity to manage the force-profiles associated with high-demand physical activity.
Level of Evidence: 5
Keywords: ACL, exercise selection, hypertrophy training, muscle, physical therapy, strength training
INTRODUCTION
Anterior cruciate ligament (ACL) injuries are common within athletics,1 and ACL reconstruction (ACLR) is the preferred surgical procedure for treating knee instability after a complete ACL tear.2–4 Regarding surgical technique, ACLR with a bone-patellar tendon-bone autograft (BPTB) may optimize ACL graft survivorship in select cohorts (e.g., athletes returning to Level-1 sports).5–7 However, ACLR with the hamstring tendon autograft (HT) is the most popular surgical technique internationally,8,9 and the use of the quadriceps tendon autograft (QT) for ACLR is increasing in popularity.8,10
Partially due to arthrogenic muscle inhibition (AMI) from harvesting the quadriceps/patellar tendon autograft,11–13 more persistent quadriceps weakness has been observed after ACLR with a BPTB or QT than with a HT.14–18 Ongoing quadriceps weakness after ACLR has been associated with impaired knee biomechanics,19,20 a slower functional progression within rehabilitation,21 low return to sport rates and patient satisfaction scores,22–27 and is correlated with the progression of radiographic knee osteoarthritis.28,29 Subsequently, recent literature has focused on improving postoperative strength outcomes,13,30–32 and therapeutic interventions prescribed to optimize the sensory/motor function of the surgical knee have shown efficacy for treating AMI after ACLR.12,31,32
Although the management/treatment of AMI is an important component of ACLR rehabilitation, prescribing exercise to stimulate improvements in muscle size and strength is also required to maximize performance-based outcomes, especially within cohorts returning to high-demand physical activities. Previous literature has explored the indications for various strengthening exercises and their ability to improve outcomes after ACLR,31,33–35 but few articles have been written for the specific purpose of optimizing quadriceps size and strength after ACLR.31 Moreover, few authors have integrated the existing muscle basic science and strength training literature into a review article.36,37 Therefore, the purpose of this commentary is to integrate the existing muscle basic science and strength training literature into a best-evidence synthesis of exercise methodologies for restoring quadriceps size and strength after ACLR.
QUADRICEPS BASIC SCIENCE
Quadriceps Anatomy
The quadriceps (i.e., quadriceps femoris) is typically divided into four muscles: (1) rectus femoris, (2) vastus lateralis, (3) vastus intermedius, and (4) vastus medialis (Figure 1a).38 All four muscles share a common insertion on the patella and tibial tuberosity (via the patellar tendon) and contribute to the primary action of knee extension (Figure 1b). Subsequently, exercises which isolate open-kinetic-chain (OKC) and closed-kinetic-chain (CKC) knee extension will be highly-specific in activating/loading the quadriceps.
Figure 1. Quadriceps Anatomy.
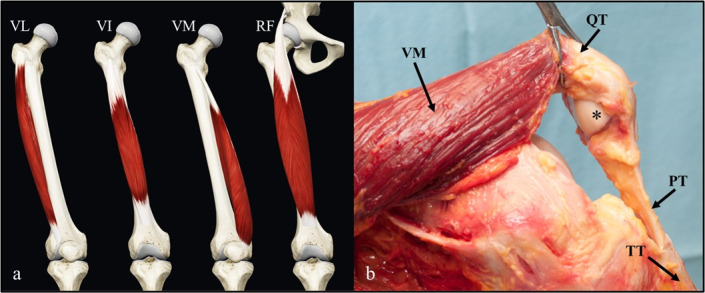
The quadriceps muscle group consists of four muscles (a); all four muscles share a common insertion on the patella and tibial tuberosity via the patellar tendon (b). Asterisks, patella; PT, patellar tendon; QT, quadriceps tendon; RF, rectus femoris; TT, tibial tuberosity; VI, vastus intermedius; VL, vastus lateralis; VM, vastus medialis.
The rectus femoris originates on the anterior inferior iliac spine, making it the only biarticular quadriceps muscle (Figure 1a).38 It contributes to the primary action of hip flexion and knee extension and has an intramuscular tendon running longitudinally from its origin38–40; the intramuscular tendon is utilized to store/transfer energy during the combined motion of hip flexion and knee extension (e.g., mid-swing phase of running).41,42 These anatomic features suggest optimal targeting of the rectus femoris should include exercises that isolate the combined motion of hip flexion with knee extension, such as the straight leg raise (SLR) exercise or high-velocity running/kicking,41–43 whereas combining the primary actions of hip extension with knee extension (e.g., leg press exercise) can reduce rectus femoris recruitment/involvement relative to the other quadriceps muscles.44,45
Quadriceps Innervation
Motor branches from the femoral nerve produce regional innervation pathways within the anterior thigh, which facilitates selective motor unit recruitment within the quadriceps.38,46,47 For example, performing exercises at longer muscle lengths and with the primary action of knee extension can selectively activate the more distal regions of the quadriceps,47,48 whereas exercising with shorter muscle lengths and/or combining the primary action of hip flexion with knee extension may recruit the more proximal regions.46,47 Likewise, OKC tasks may recruit the more proximal regions of the quadriceps/rectus femoris, producing a proximal-to-distal sequence of muscle activity (e.g., OKC knee extensions, kicking, and the swing phase of gait),41–43,45,49 whereas CKC tasks produce a more distal-to-proximal sequence of quadriceps activation and demand less of the rectus femoris (e.g., squatting or a sagittal deceleration task).44,46,49 Altogether, the task-specific activation of the quadriceps exemplifies the need for a variety of OKC and CKC exercises to maximally stimulate quadriceps hypertrophy and strength.
Quadriceps Activation-Threshold and Fiber-Type Distribution
Compared to other muscles of the lower extremity, previous work has observed the quadriceps to possess a relatively high volitional recruitment threshold (Figure 2).50 While higher quadriceps recruitment thresholds may help produce larger knee extension torque-outputs,50 a higher baseline recruitment threshold makes volitional activation of the quadriceps a challenge after ACLR.13,51 Considering this, Boccia et al52 observed higher motor unit discharge rates and synaptic input to the vastus medialis and vastus lateralis with the use of resisted OKC knee extensions compared to the leg press exercise, suggesting OKC exercise may more specifically activate the quadriceps muscles.
Figure 2. Average inactivation by muscle group.
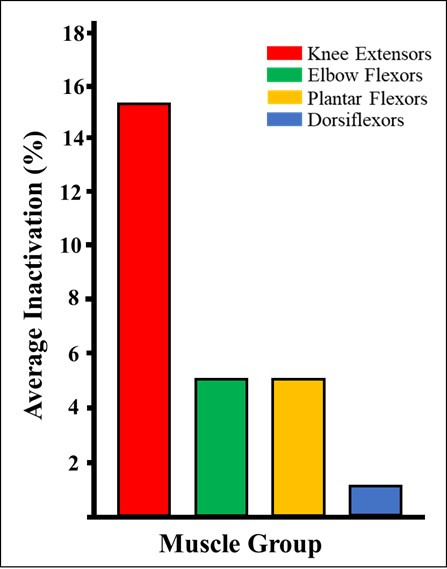
Relative to other muscle groups within the human body, the knee extensors (i.e., quadriceps femoris) have the largest inactivation percentage.50 This higher inactivation percentage suggests maximal, volitional recruitment/activation of the quadriceps is a challenge at baseline (i.e., before knee injury or surgery). %, percentage.
The relative distribution of muscle fiber-type does not appear uniform within the quadriceps; the vastus lateralis is roughly 50% type-II muscle fiber,53 whereas the rectus femoris may be as much as 62%.54 These findings suggest the rectus femoris may experience more post-exercise fatigue and muscle damage than the vastus lateralis,55–57 requiring more time to recover in between exercise bouts (e.g., 72-96 hours of recovery in between fatiguing exposures to high velocity running). The combination of a high volitional recruitment threshold and a relatively lower distribution of type-II fibers within the vastus lateralis may suggest a higher training frequency may be indicated for the single-joint quadriceps muscles (e.g., 48-72 hours of recovery in between exposures to resistance training on a leg press).53,58
Quadriceps Length-Tension
Although a variety of training variables can be manipulated to improve muscle size and strength, exercising within a muscle’s ideal length-tension relationship may help stimulate a greater amount of mechanotransduction,59 and optimal muscle length-tension can improve the intramuscular force-output at any muscle activation level.60,61 Multiple studies have reported different muscular adaptations in response to the manipulation of exercise range-of-motion (ROM),62,63 to which superior improvements in muscular hypertrophy have been observed with resistance training at longer muscle lengths64; this observation may be partially explained by a more optimal length-tension relationship within the muscle when resistance training is prescribed at relatively long muscle lengths.61 Considering the quadriceps consists of four separate muscles, the rehabilitation specialist should understand which hip/knee joint positions will optimize the length-tension properties within each muscle.
Previous work has outlined the sarcomere lengths of each quadriceps muscle (Figure 3).65,66 Due to its biarticular nature, the rectus femoris is the only quadriceps muscle that operates within the ascending limb of the length-tension curve (Figure 3a)65; loading the rectus femoris within higher degrees of hip flexion in combination with low levels of knee extension (e.g., OKC knee extensions between 0-40 degrees of knee flexion with the trunk positioned in 90+ degrees of hip flexion) may create a suboptimal length-tension relationship, producing active insufficiency and impaired force-output.60,61,63,65,67
Figure 3. Length-tension properties of the quadriceps muscle group.
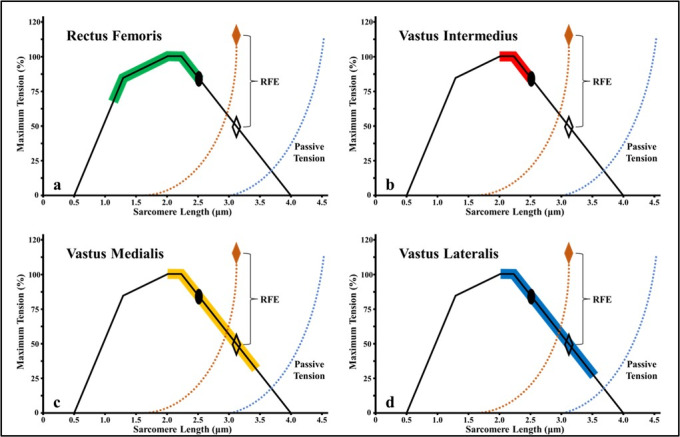
Previous work has outlined the sarcomere lengths of each quadriceps muscle throughout its functional operating range.65,66 The rectus femoris is the only quadriceps muscle that operates within the ascending limb of the length-tension curve. At any degree of knee flexion, the single-joint quadriceps muscles (i.e., vastus medialis, intermedius and lateralis) have sarcomere lengths that are working within the plateau to descending limb of the length-tension curve. %, percentage; μm, micrometers; RFE, residual force enhancement.
At any degree of knee flexion, it appears the single-joint quadriceps muscles have sarcomere lengths operating within the plateau to descending limb of the length-tension curve (Figure 3b-d).60 Therefore, active insufficiency considerations may only apply to the rectus femoris. Resistance training between 0-90 degrees of knee flexion may best activate/load the vastus intermedius,65 because greater regional hypertrophy has been observed within the vastus intermedius when performing the half squat exercise compared to the full squat.68 Inversely, resistance training at longer muscle lengths (i.e., 60-110+ degrees of knee flexion) may best facilitate regional hypertrophy within the distal vastus medialis and vastus lateralis by exercising within the descending limb of their length-tension curves48,65; the vastus medialis has a slightly longer sarcomere length than the vastus lateralis at 90 degrees of knee flexion (Figure 3c-d),66 suggesting resistance training within an even deeper level of knee flexion (i.e., a full squat to 140 degrees of knee flexion) may further facilitate regional hypertrophy within the distal vastus lateralis.48,68
Quadriceps Internal Moment Arm
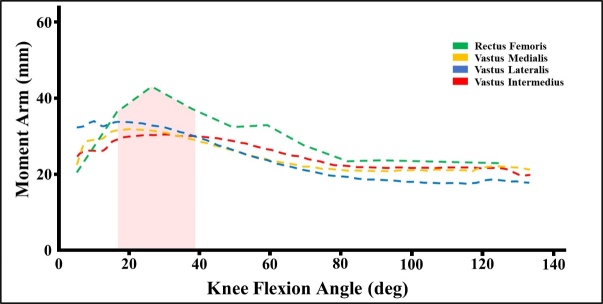
Considering the quadriceps shares a common insertion on the patella (via the quadriceps tendon) and the tibial tuberosity (via the patellar tendon), it is important to consider the internal moment arm curve of each muscle as well as the quadriceps/patellar tendons. When analyzing each quadriceps muscle in isolation, previous literature has reported similar internal moment arm curves for all four muscles (Figure 4)69; the internal moment arm curve for the single-joint quadriceps muscles slightly increases and peaks from 0-30 degrees of knee flexion, then gradually decreases from 30-100 degrees.69 Similarly, the internal moment arm curve of the rectus femoris peaks at 20-30 degrees of knee flexion but has a slightly steeper moment arm curve (Figure 4).69,70
Figure 4. The internal moment arm curves of the quadriceps muscle group.
The internal moment arm curve for the single-joint quadriceps muscles slightly increases and peaks from 0-30 degrees of knee flexion, then gradually decreases from 30-100 degrees.69 Similarly, the internal moment arm curve of rectus femoris peaks between 20-30 degrees of knee flexion but has a slightly steeper moment arm curve.70 Deg, degrees; mm, millimeters; red shading, range of knee flexion associated with peak internal knee extension moment.
To best manage the graft harvest site after ACLR with the BPTB or QT autograft, the internal moment arms of the patellar and quadriceps tendons should also be considered.71 The internal moment arm of the patellar tendon rises and peaks from 0-30 degrees of knee flexion, then reduces from 30-100+ degrees.72 Therefore, exercises prescribed to preferentially load the patellar tendon may benefit from exercise prescriptions that initially emphasize low levels of knee flexion.71,73,74 The internal moment arm of the quadriceps tendon appears relatively constant between 0-25 degrees of knee flexion, with a peak moment greater than the patellar tendon at 20 degrees.75,76 As the knee moves into deeper flexion, force-transmission within the quadriceps tendon increases relative to the patellar tendon (Figure 5)74,77; this increase in quadriceps tendon force-transmission is due to a decrease in internal moment with a concurrent increase in the amount of passive tension within the quadriceps (Figure 6).78 Subsequently, preferential loading of the quadriceps tendon relative to the patellar tendon can be achieved at deeper levels of knee flexion (i.e., 30-100+ degrees), but the rehabilitation specialist should also consider reducing the amount of knee flexion if quadriceps tendon pain is reported during exercise.71
Figure 5. Force-ratio between the quadriceps and patellar tendons.
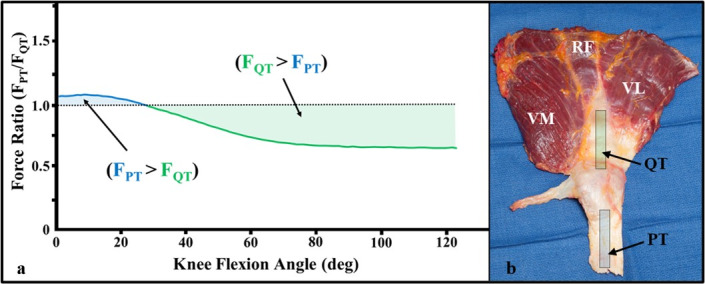
As the knee moves into deeper flexion, force transmission within the quadriceps tendon increases relative to the patellar tendon (a)74,77; this change in force-ratio is due to a decreasing quadriceps tendon internal moment relative to the patellar tendon (see Figure 6) with a concurrent increase in passive tension within the quadriceps muscle group (b). F, force; PT, patellar tendon; QT, quadriceps tendon; RF, rectus femoris; VL, vastus lateralis; VM, vastus medialis.
Figure 6. Internal moment arms of the quadriceps and patellar tendons.
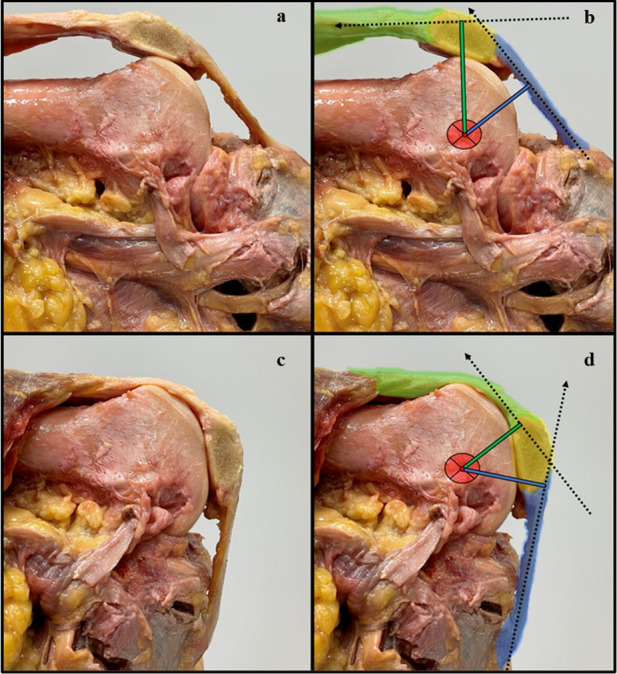
Between 0-30 degrees of knee flexion, the internal moment arm of the quadriceps tendon is larger than the patellar tendon (a, b). The patellar tendon has a larger internal moment arm than the quadriceps tendon in deeper levels of knee flexion (c, d). Blue line, patellar tendon internal moment arm; blue shading, patellar tendon; dotted black lines; resultant intratendinous force-vector from a quadriceps contraction; green line, quadriceps tendon internal moment arm; green shading, quadriceps tendon; red circle; estimated center of joint rotation; yellow shading, patella.
Quadriceps Contraction Mode
Of the various parameters utilized to stimulate exercise-induced adaptations within the neuromusculoskeletal system, muscle contraction mode appears highly influential. Previous literature has observed specific neuromuscular adaptations from exposure to different contraction modes, to which the rehabilitation specialist should be able to effectively manipulate when designing rehabilitation programs. When prescribing the contraction mode, exercise prescriptions are commonly divided into isometric, eccentric and isotonic (i.e., exercises with concentric/eccentric phases) training programs.55,79–84
Isometric training programs are traditionally implemented during the acute phase of rehabilitation.85 However, isometric resistance training is highly effective at improving muscle size and strength and can be prescribed within any rehabilitation phase.62 Studies examining the muscle’s response to isometric exercise have reported multiple types of isometric contractions86–88; yielding/holding isometrics require the muscle to maintain a set joint position as external force is applied, whereas overcoming/pushing isometrics require the muscle to produce/transfer force into a fixed structure.88 Peripheral muscle activation and time to exhaustion may be increased with overcoming/pushing isometrics,86,88 increasing motor recruitment relative to yielding/holding isometrics. Yielding/holding isometrics behave more like eccentric contractions,87 producing less peripheral muscle activation but a more synchronous motor plan; these observations suggest yielding/holding isometrics may require a more complex/specific mechanism of motor control and may accelerate volitional fatigue relative to overcoming/pushing isometrics.86,88 Collectively, overcoming/pushing isometrics may be best implemented when attempting to summate high volitional activation thresholds or mechanically stimulate a greater proportion of the recruited muscle fibers,86,88 whereas yielding/holding isometrics can be utilized to modulate tendon pain,89 manage/treat AMI and improve central motor excitability.90–92
Partially due to residual force enhancement during eccentric contractions (Figure 7),95 the eccentric 1-repitition maximum (1-RM) for a given muscle/muscle group has been observed to be around 41% greater than the concentric 1-RM.94 Eccentric contractions also produce less muscle activation than concentric contractions at any given force-output, making eccentric-specific exercise less metabolically demanding than isotonic/concentric exercise.96,97 Likewise, eccentric-specific training programs can enhance motor control and hypertrophy,51,90 improve strength outcomes,98 and facilitate injury-protective architectural adaptations within skeletal muscle.99,100 Therefore, any rehabilitation program designed to optimize quadriceps size and strength should gradually build the knee’s load-tolerance to a level that supports eccentric-specific training at loads greater than the concentric 1-RM.
Figure 7. Depiction of the Knee Extensor Force-Velocity Relationship.
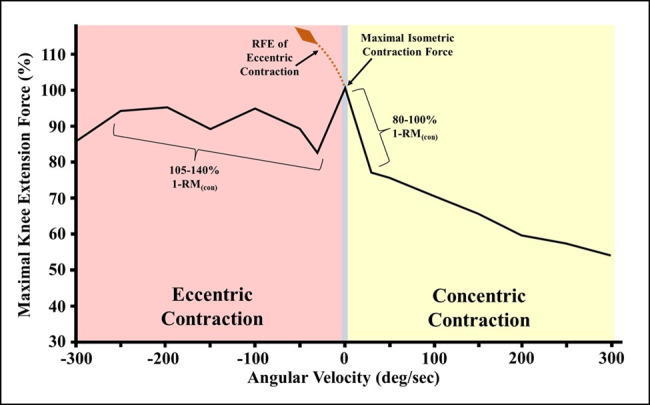
The force-velocity relationship for the quadriceps produces maximal concentric knee extension force/torque at slow contraction velocities (i.e., maximal effort pushing/overcoming isometric contractions or concentric contractions at < 60 degrees/second).93 Partially due to residual force enhancement during eccentric contractions (i.e., active muscle lengthening at maximal effort), maximal knee extension force/torque-output will be higher during eccentric than concentric contractions.94 %, percentage; 1-RM(con), 1-repitition maximum during a concentric contraction; deg, degrees; RFE, residual force enhancement; sec, second.
More recently, eccentric quasi-isometric (EQI) contractions (i.e., a muscle contraction that involves maintaining a yielding/holding isometric contraction until task failure and eccentric muscle activity ensues) has been proposed as a novel stimulus for safely exposing the musculotendinous system to a large mechanical load.101,102 Eccentric quasi-isometric contractions produce similar architectural and neuromuscular adaptations as eccentric-specific contractions, but yield less post-exposure muscle soreness/fatigue.101 Theoretically, EQI resistance training should be prescribed after ACLR to stimulate favorable size, strength, and architectural adaptations within the surgical knee’s extensor mechanism, while concurrently protecting any desired postoperative structures within a predetermined ROM.
Recently, heavy-slow resistance training (HSRT) (i.e., high-load isotonic training at slow contraction velocities) has become popular for treating tendinopathy,103,104 and velocity-based training (i.e., a training method that monitors intraset muscle contraction/exercise velocity) has proven effective in eliciting desirable power/performance adaptations.105 Collectively, individuals with less resistance training experience may benefit from the use of isotonic/concentric training during the early phase of rehabilitation, when self-motivation is low, or when fatigue is high. To treat patellar/quadriceps tendinopathy at the autograft harvest site after ACLR, quadriceps HSRT should be prescribed at a load-intensity ≥ 70-100% of the concentric 1-RM,104 because this load-intensity will produce slow contraction velocities and maximize intramuscular force on the concentric side of the quadricep’s force-velocity relationship (Figure 7).93,106 Lastly, velocity-based training methods can be utilized throughout ACLR rehabilitation to optimize motor unit discharge-rates and quadriceps rate-of-force development.105,107
QUADRICEPS REHABILITATION AFTER ACLR
After ACLR, a needs analysis should be completed and modified throughout rehabilitation based on patient presentation and their objective progress.108 Information regarding the ACLR procedure (e.g., primary vs. revision ACLR); graft selection, composition, and fixation method; or any concomitant repairs/reconstructions should be considered.71 This information dictates the ACL graft ligamentization timeline,109–112 the durability of the graft-bone tunnel construct,113–115 the amount of tissue trauma at the autograft harvest site and other areas,71,116 and the presence of quadriceps weakness related to BPTB or QT harvest from the extensor mechanism.14–18,117 Lastly, non-modifiable risk factors for graft laxity and/or failure should be identified (e.g., knee hypermobility, allograft, hamstring autograft, meniscectomy, and high tibial slope),118–122 because the rehabilitation specialist may elect to change/modify exercises when multiple risk factors are present (e.g., OKC quadriceps resistance training between 0-45 degrees of knee flexion produces more ACL strain than 45-100+ degrees).123,124
The quadriceps rehabilitation program should include both OKC and CKC exercise progressions,31,125 which should be prescribed in line with best-evidence recommendations for hypertrophy and strength training (Figure 8).126 Likewise, exercise prescriptions should consider the procedure specific ACLR technique, biological healing, joint homeostasis and patient preference.71 The sweep test and pain-monitoring model should be used throughout rehabilitation to objectively quantify knee irritability (Figure 8).71,127 Lastly, ACLR rehabilitation should include best-practice strategies for managing AMI,32 and mitigating AMI after ACLR may improve the effectiveness of the quadriceps load-progressions.13,31,51,128
Figure 8. Overview of exercise selection for quadriceps training after anterior cruciate ligament reconstruction (ACLR).
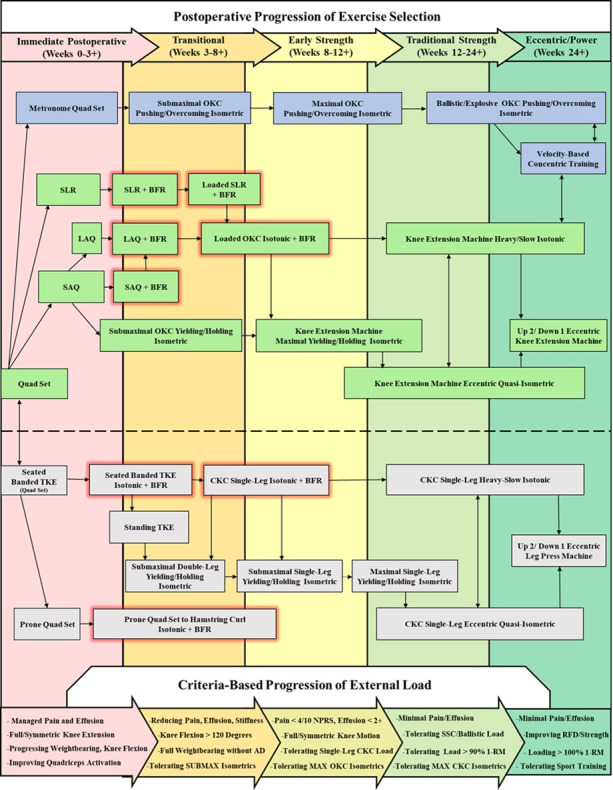
After anterior cruciate ligament reconstruction, quadriceps training should begin with quadriceps setting and be developed onto both open and closed-kinetic-chain load progressions. Strength training load progressions should be primarily advanced through the progression of external load, and exercises that load the quadriceps close to volitional fatigue/task failure at relatively long muscle lengths should be prescribed to enhance muscular hypertrophy. Lastly, a specific load progression to enhance quadriceps rate-of-force development should be prescribed throughout rehabilitation.
1-RM, concentric one-repetition maximum of the surgical limb; AD, assistive device; BFR, blood flow restriction; quad set, quadriceps setting exercise; black arrows, exercise progression pathway; blue boxes, exercise progression for quadriceps rate-of-force development; boxes with red glow, exercise with blood flow restriction; CKC, closed-kinetic-chain; green boxes, open-kinetic-chain exercise selection; grey boxes, closed-kinetic-chain exercise selection; LAQ, long-arc-quad exercise; MAX, maximal; NPRS, numeric pain rating scale; OKC, open-kinetic-chain; RFD, rate-of-force development; SAQ, short-arc-quad exercise; SCC, stretch-shortening cycle; SLR, straight leg raise exercise; SUBMAX, submaximal; TKE, terminal knee extension.
Immediate Postoperative Phase (Weeks 0-3 After ACLR)
The immediate postoperative exercise selection should restore active knee extension as soon as possible (Figure 8),129 because the slightest postoperative loss of knee extension can produce impaired knee arthrokinematics; provoke quadriceps inhibition130,131; and may increase the risk of developing knee osteoarthritis.129,132,133 Given the presence of AMI after ACLR and the high volitional recruitment threshold of the quadriceps (Figure 2),13,50 an OKC quadriceps training program may be more beneficial than a CKC program during the immediate postoperative phase.52 Lastly, high daily exercise-frequencies should be prescribed (Appendix A); high frequency/short duration exercise may work best when pain levels are high, knee motion is limited,134 exercise intensity is low,135 and neuroplastic improvements in quadriceps activation are desired (Appendix A).136
Open-Kinetic-Chain Load-Progression
The OKC quadriceps load-progression should start with quadriceps setting (Figure 8) (Appendix A)71; quadriceps setting in low levels of hip flexion (i.e., a recumbent trunk position) may optimize length-tension of the rectus femoris.63 Likewise, positioning the knee in 20-45 degrees of flexion may be preferred when high levels of AMI are present (Figure 9A) (see Video, Supplemental Material 1, which demonstrates quadriceps setting), because this position will improve quadriceps length-tension and its internal moment arm(s).69,70,137 Prescribing yielding/holding quadriceps isometrics for longer durations (i.e., 45-90+ seconds) may be an effective strategy for improving motor recruitment,86,88,138 and the superimposition of neuromuscular electrostimulation (NMES) during exercise may accelerate the recovery of quadriceps force-output (Appendix A) (see Video, Supplemental Material 2, which demonstrates quadriceps setting with NMES).139 The rehabilitation specialist should also consider advancing the tempo/cadence of quadriceps setting (Appendix A), because higher-velocity quadriceps contractions (i.e., velocity-based training principles) may improve motor recruitment.107 A metronome can be used to advance the tempo/cadence of quadriceps setting, and metronome training should be progressed onto higher cadence drills that challenge the capacity to quickly summate/regulate motor activity (Figure 8) (Appendix A) (see Video, Supplemental Material 3, which demonstrates high tempo quadriceps setting with a metronome).136,140,141
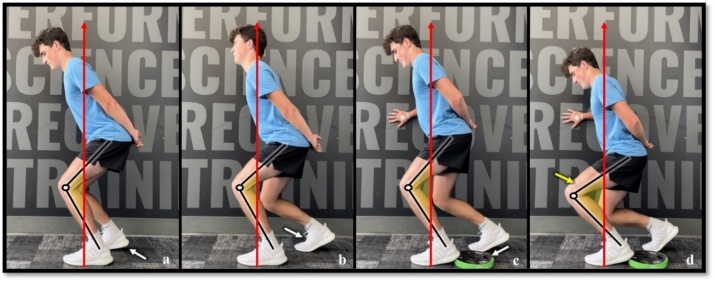
Figure 9. Exercise selection for the immediate postoperative phase.
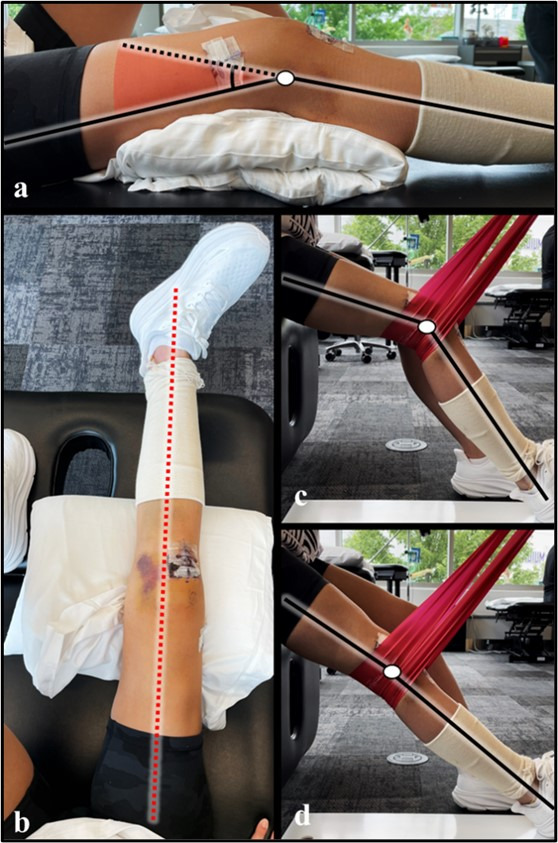
Positioning the knee in 20-45 degrees of knee flexion prior to quadriceps setting will improve global quadriceps length-tension and its internal moment arm(s) (a). Slight femoral external rotation with active ankle dorsiflexion should be maintained throughout the straight leg raise exercise, as this position may maximize force output from the quadriceps (b). The CKC quadriceps load-progression should be initiated in sitting with the terminal knee extension exercise (i.e., isotonic, terminal knee extension with elastic band resistance); this exercise can be utilized to preferentially activate the distal / single-joint quadriceps muscles (c, d). Black lines, approximate tibial and femoral bone markers; dotted red line, midline/neutral hip rotation within the surgical limb; red shading, depiction of a knee flexion angle of 20-45 degrees; white circle; estimated center of joint rotation.
Once a volitional quadriceps contraction is achieved, exercise selection should include the SLR exercise (Figure 8) (Appendix A). To minimize knee flexion lag, cueing should reinforce the initiation of quadriceps setting into maximal superior patellar glide prior to the initiation of the SLR (see Video, Supplemental Material 4, which demonstrates proper straight leg raise technique); slight femoral external rotation with ankle dorsiflexion should be maintained throughout the SLR (Figure 9b), because this positioning can maximize force output from the quadriceps.142 The SLR exercise should start in tall sitting/standing and be progressed into the long-sitting position. Long-duration SLR isometrics and/or blood flow restriction (BFR) can be utilized to accelerate muscular fatigue,138,143–145 and exercise intensity can be advance by adding external load distal to the knee joint (Figure 8).
Quadriceps setting can be progressed onto OKC knee extensions as soon as tolerated (Figure 8).146,147 The rehabilitation specialist may elect to first perform knee extensions between 0-45 degrees (see Video, Supplemental Material 5, which demonstrates the short-arc-quad exercise), because external knee moments are highest within this range.148 As knee flexion improves, full-arc knee extensions may best mechanically-stimulate the distal muscle fibers of the quadriceps and should be preferred to partial ROM exercise at shorter muscle lengths.41–43,45,47–49,61,149 Exercise with BFR can be utilized to accelerate muscular fatigue, and prescribing sets close to volitional fatigue/task failure may best stimulate muscular hypertrophy with low loads (Figure 8) (Appendix A).71,150,151 Lastly, submaximal OKC yielding/holding isometrics can be prescribed between 45-60 degrees of knee flexion to improve quadriceps activation and knee load-tolerance (Appendix A) (see Video, Supplemental Material 6, which demonstrates a submaximal OKC yielding/holding isometric)88; this ROM will preferentially target the quadriceps within the descending phase of the length-tension curve (Figure 3),65,66,137 improve the quadriceps’ internal moment arms relative to deeper knee flexion (Figure 4),69,70 optimize knee extension torque-output,137 decrease ACL graft strain relative to 0-45 degrees of knee flexion,123,152 and may downregulate patellar/quadriceps tendon pain after autograft harvest from the extensor mechanism.89
Closed-Kinetic-Chain Load-Progression
The CKC quadriceps load-progression should begin in sitting with the terminal knee extension (TKE) exercise (Figure 8) (Figure 9c-d),71 which should be utilized to preferentially activate the single-joint quadriceps muscles.44–46,49 The sitting TKE exercise can be progressed by increasing the level of elastic band resistance (Appendix A),71 prescribing longer-duration yielding/holding isometrics,138 or the addition of BFR (Figure 8).143–145 The rehabilitation specialist should also prescribe prone quadriceps setting (Appendix A), because this exercise omits visual feedback and may facilitate improvements in knee proprioception (see Video, Supplemental Material 7, which demonstrates prone quadriceps setting).136
Transitional Phase (Weeks 3-8 After ACLR)
As active knee ROM and volitional quadriceps activation have been recovered, the rehabilitation specialist should transition their quadriceps exercise prescription(s) from volume and variety-based load-progressions,135 onto more seminal load progressions that can be advanced throughout the remainder of the ACLR rehabilitation program.153 During this phase, joint irritability and a knee effusion are likely still present,35 and low-load exercise with BFR is indicated to recover joint homeostasis while mitigating atrophy/stimulating hypertrophy (Appendix A).71,154
Exercise with Blood Flow Restriction
Non-weightbearing quadriceps exercise with BFR should be prescribed 1-2x/day to maximize the anabolic response to exercise with very light loads (i.e., < 20% concentric 1-RM),155,156 and the use of higher individualized occlusion pressures may be recommended.157–159 To specifically stimulate quadriceps hypertrophy, each BFR set (when possible) should be prescribed close to volitional fatigue/task failure (e.g., 0-2 repetitions in reserve) (Appendix A),126,150,151 and combining OKC knee extension variations with the CKC seated TKE exercise may optimally stimulate all four quadriceps muscles in sitting (i.e., both the proximal and distal quadriceps) (Appendix A) (Figure 8) (see Video, Supplemental Material 8 and 9, which demonstrates the long-arc-quad and seated TKE exercise with BFR).45 The rehabilitation specialist should also consider prescribing the prone quad set to hamstring curl exercise (Figure 8); this exercise may improve mechanical signaling/regional hypertrophy within the distal quadriceps through the maximal lengthening of its sarcomeres (see Video, Supplemental Material 10, which demonstrates the prone quad set to hamstring curl exercise with BFR).48,65 Similarly, prescribing loaded inter-set stretching with the prone knee flexion stretch or reverse Nordic exercise can be utilized to therapeutically shear/mobilize the graft harvest site after ACLR with the QT autograft and can help stimulate stretch-mediated quadriceps hypertrophy/sarcomerogenesis (see Video, Supplemental Material 11 and 12, which demonstrates the prone knee flexion stretch and reverse Nordic exercise).71,160,161
Open-Kinetic-Chain Load-Progression
To enhance motor unit recruitment and/or manage tendon pain after ACLR with the BPTB or QT autograft, the OKC quadriceps load-progression should be advanced from yielding/holding quadriceps isometrics at 45-60 degrees of knee flexion, onto overcoming/pushing isometrics between 60-90 degrees of knee flexion (Appendix A) (Figure 8); overcoming/pushing isometrics will summate more motor activity than yielding/holding isometrics.88 Likewise, progressing the level of knee flexion during OKC overcoming/pushing isometrics may help facilitate regional hypertrophy within the distal quadriceps,48,61,65,66 and the superimposition of NMES may improve quadriceps torque-output (see Video, Supplemental Material 13, which demonstrates an OKC overcoming/pushing isometric with NMES).139,162,163
Closed-Kinetic-Chain Load-Progression
Seated TKE contractions should be advanced onto the standing TKE exercise (Figure 8) (see Video, Supplemental Material 14, which demonstrates the standing TKE exercise)71; this exercise should be prescribed to recover TKE control in weightbearing and can be progressed through the addition of elastic band resistance (Appendix A). Due to the relatively large increase in the knee’s articular load when transitioning from non-weightbearing to weightbearing exercises,164,165 consideration should be given for the use of yielding/holding isometrics as the initial form of CKC resistance training; yielding/holding isometrics behave like eccentric contractions and stimulate muscle fatigue faster than overcoming/pushing isometrics.86–88
The double-leg squat exercise can serve as the base regression for a CKC yielding/holding isometric program (Figure 8),71 and the non-surgical limb should be slightly posted to facilitate weight redistribution towards the surgical limb (Figure 10a).71,166 Prescribing submaximal yielding/holding isometrics from 45-60 degrees of knee flexion may be initially recommended, because this level of knee flexion will optimize knee extension torque-output and the internal moment arms of the quadriceps muscles (Figure 4) (Appendix A).69,70,137 Each exposure should include 3-6 sets of long-duration yielding/holding isometric contractions (e.g., submaximal contractions for 45-90 seconds), which are prescribed to improve motor unit recruitment86,88,138; stimulate exercise-induced muscle fatigue138; facilitate stress relaxation of the quadriceps and patellar tendons167,168; and downregulate anterior knee/tendon pain.89 After ACLR with a BPTB or QT, CKC yielding/holding isometrics should be implemented at a frequency of 2 exposures/day (6-8+ hours apart) to optimally stimulate collagen synthesis/repair at the autograft harvest site (Appendix A).71,168,169 Double-leg yielding/holding isometrics should be progressed onto the split-squat position (Figure 10a-b),71 because this progression may mitigate the bilateral force deficit phenomenon as well as other inter-limb compensations.170,171 Lastly, the front-foot elevated split-squat can be used to advance the level of knee flexion from the 45–60-degrees onto 60-90 degrees (see Video, Supplemental Material 15, which demonstrates the front-foot elevated split squat exercise).
Figure 10. Closed-Kinetic-Chain Yielding/Holding Isometric Load-Progression.
The closed-kinetic-chain (CKC) yielding/holding isometric load progression should start with the double-leg squat exercise in low levels of knee flexion (a, non-surgical limb posted). Exercise selection can be advanced to include the split-squat exercise (b), and a heel wedge can be utilized to increase external knee flexion moment/load on the quadriceps (c). Submaximal yielding/holding isometric contractions should be advanced onto maximal effort contractions through increasing the degree of knee flexion/external knee flexion moment (d) or the progression of external load. Maximal effort CKC machine or weightbearing exercises with upper body stabilization (c, d) are preferred to free-weight or compound exercises prescribed without external support. Asterisk, use of wall support to stabilize the body during exercise (c, d); black lines, approximate tibial and femoral bone markers; red arrows; approximate ground reaction force-vector; white arrows, progression of knee/quadriceps load through the advancement of exercise position (a-c); white circle; estimated center of joint rotation; yellow arrow, progression of knee/quadriceps load by advancing the degree of knee flexion/external knee flexion moment (d); yellow shading; depiction of knee/quadriceps-dominant loading with increasing external knee flexion moment (a-d).
Early Strength Phase (Weeks 8-12 After ACLR)
Weeks 8-12 after ACLR, rehabilitation should focus on facilitating the resolution of any knee effusion/joint irritability while progressively loading the quadriceps.35,71 The rehabilitation specialist should consider increasing the level of knee flexion during resistance training before adding external load, because deeper flexion may optimize quadriceps hypertrophy (Figure 10d).48,61,149 However, knee flexion angle does effect the intratendinous force-ratio between the patellar and quadriceps tendons, making frequent monitoring of the autograft harvest site an important component of rehabilitation after ACLR with the BPTB or QT (Figure 5a).71
Open-Kinetic-Chain Load-Progression
The OKC quadriceps load-progression should include resistance training between 45-100+ degrees of knee flexion (unless contraindicated by a concomitant procedure), because autograft harvest from the extensor mechanism appears to produce greater quadriceps weakness at deeper knee flexion angles (Figure 8).71,172–174 Likewise, 45-100+ degrees of knee flexion produces low ACL graft strain (relative to 0-45 degrees) and provides a better length-tension position for facilitating regional hypertrophy within the distal quadriceps.61,123,149 Isometric and/or HSRT should be the preferred contraction mode for loading the quadriceps (especially after ACLR with the BPTB or QT) because the provocation of anterior knee pain with resistance training is still a concern.83,89,91,103,104 Submaximal yielding/holding quadriceps isometrics should be advanced onto maximal effort isometric strength training through the addition of external load,126 and holding isometric contractions close to the point of volitional fatigue/failure may best-stimulate quadriceps hypertrophy.126 Once maximal OKC yielding/holding isometrics can only be sustained for 20-45 seconds in duration,138 resistance training with EQI contractions can be prescribed (Figure 8) (Figure 11).
Figure 11. Open and closed-kinetic-chain eccentric quasi-isometric quadriceps contractions.

Eccentric quasi-isometric (EQI) quadriceps resistance training can be completed on a leg press with a decline ankle-wedge (a-c) or knee extension machine (d-f) by (1) performing a concentric contraction to externally load the surgical knee/limb (a, d), (2) performing a yielding/holding isometric contraction to the point of volitional fatigue/failure (b, e), and (3) continuing to maximally resist the ensuing eccentric contraction throughout the prescribed range of knee motion. Black arrows, contraction direction; black lines, approximate tibial and femoral bone markers; green shading, concentric contractions; red shading, ensuing eccentric contractions as part of the EQI contraction; white asterisk, heel wedge; white circle, estimated center of joint rotation; yellow shading, depiction of large external knee flexion moment during yielding/holding isometric contractions
EQI resistance training should be prescribed on a knee extension machine (Figure 11d-f) (see Video, Supplemental Material 16, which demonstrates an EQI contraction on a knee extension machine). It is advisable to begin EQI contractions between 45-70 degrees of knee flexion before progressing onto deeper flexion angles (Appendix A), because EQI contractions in deeper flexion (i.e., 70-120+ degrees of knee flexion) could theoretically trigger knee irritability if not progressed appropriately.101,102 This recommendation is based on the fact: (1) the internal moment arm of the quadriceps is reducing from 45-100+ degrees of knee flexion (Figure 4); (2) passive quadriceps tension will increase as knee flexion increases78; and (3) eccentric contractions will increase total force within the extensor mechanism (Figure 7).
Closed-Kinetic-Chain Load-Progression
The CKC load-progression should include unilateral exercises that optimize lower extremity stability, because high exercise stability can improve volitional quadriceps activation/force-output.175 Therefore, resistance training machines (e.g., leg press) or other weightbearing exercises with high stability are preferred to free-weight or compound exercises without external support/stability (Figure 10c-d). Similarly, a decline wedge/heel lift can be used to increase the relative contribution of the quadriceps during CKC exercise (Figure 10c).176,177 Submaximal to maximal CKC yielding/holding isometrics in 45-90+ degrees of knee flexion should be prescribed close to volitional fatigue/failure within 20-45 seconds (Appendix A), and task failure should be achieved more quickly as knee flexion/knee moment is increased.138 Once maximal effort CKC yielding/holding isometrics are tolerated for 20-45 seconds in deeper knee flexion (Figure 10d), the addition of external load to the CKC quadriceps load-progression is indicated.
Traditional Strengthening Phase (Weeks 12-24 after ACLR)
Under normal healing conditions, most ACL grafts have integrated by 12-weeks after ACLR,178,179 and any autograft harvest-site within the extensor mechanism has remodeled with scar-like tendon tissue180; this objective increase in load-tolerance permits the full transition to maximal effort quadriceps loading.181 Subsequently, rest and recovery are important during this phase, and training schedules may need to be modified based on muscular soreness and/or the presence of fatigue. Lastly, exercise-intensity should be progressed with frequent monitoring of the knee for soreness/tissue irritability,127,182,183 and loading should be prescribed with graft/procedure-specific considerations in mind.71
Open-Kinetic-Chain Load-Progression
For reasons previously mentioned, OKC resistance training between 45-100+ degrees of knee flexion should be continued during this phase.61,65,123,148,149,160,184 Eccentric quasi-isometric contractions on a knee extension machine can be prescribed to isometric failure within 20-45 seconds (Figure 11d-f),101,102,138 and more formal HSRT can be prescribed close to volitional fatigue/failure with an external load > 70-80% of the concentric 1-RM (Figure 8) (see Video, Supplemental Material 17, which demonstrates heavy-slow resistance exercise on a knee extension machine)104; these load-intensities will produce maximal effort concentric contractions at slow velocities (i.e., < 60 degrees/second), optimizing intramuscular force/mechanical tension within the quadriceps (Figure 7).
Closed-Kinetic-Chain Load-Progression
Single-leg CKC exercises with large external knee flexion moments should be prescribed during this phase (Figure 11b), because unilateral exercises may improve volitional motor unit recruitment/force-output relative to the use of bilateral exercises.170,185,186 To target the quadriceps more specifically, a decline wedge/heel lift should be used to increase knee flexion moment during CKC exercise,176,177 and maximal yielding/holding isometrics can be advanced by increasing the level of knee flexion44,149,160; this progression should be monitored because increasing knee flexion can provoke knee symptoms by increasing compression/shear-forces within the quadriceps/extensor mechanism (Figure 4) (Figure 6d).69,70 As load-tolerance improves, surgical limb EQI contractions can be prescribed by holding a maximal yielding/holding isometric for 20-45 seconds and continuing to resist the ensuing eccentric contraction from 60-90+ degrees of knee flexion (Figure 11a-c) (see Video, Supplemental Material 18, which demonstrates surgical limb EQI contractions on a leg press).187 Likewise, HSRT can be prescribed between 45-120+ degrees of knee flexion with no more than 4-6 achievable repetitions per set (Figure 8) (Appendix A) (see Video, Supplemental Material 19, which demonstrates surgical limb HSRT on a leg press).104,187
Eccentric Strengthening/Power Phase (Weeks 24+ after ACLR)
As the quadriceps develops the capacity to perform high-load resistance training (i.e., >85% of the concentric 1-RM), the quadriceps load-progression should be advanced onto exercises with force-profiles similar to high-level functional tasks. For athletes returning to Level-1 sports, these load-progressions should consider the forces associated with cutting/pivoting, to which peak patellofemoral forces have been reported to be as high as 13-18 times bodyweight.188 Considering this, previous studies have investigated the force-profiles associated with different exercise interventions165; a full squat (to 120 degrees of knee flexion) with a load-intensity of ≥85% of the concentric 1-RM produces a patellofemoral force-profile similar to cutting/pivoting,165,189 but a maximal OKC overcoming/pushing knee extension isometric (at 90 degrees of knee flexion) may only produce a peak patellofemoral force of 7-8 times body weight.190 Collectively, these observations suggest CKC quadriceps resistance training should be progressed into 120+ degrees of knee flexion to best-replicate the force profiles associated with cutting/pivoting165,188,189; but to achieve a similar force-profile, submaximal depth CKC and OKC quadriceps resistance training should be progressed onto eccentric-specific training at a load-intensity > 100% of the concentric 1-RM.190
Eccentric-Specific Quadriceps Training
Due to the load-intensity for eccentric-specific training being greater than the concentric 1-RM, the surgical and non-surgical limb should complete the concentric phase of each repetition, with the subsequent transition to the isolated use of the surgical limb during the eccentric phase (i.e., double-limb concentric, single-limb eccentric training) (Figure 12). Eccentric-specific CKC exercises should be prescribed between 0-110+ degrees of knee flexion and between 45-100+ degrees of knee flexion during OKC exercises (Figure 12) (see Video, Supplemental Material 20 and 21, which demonstrates the technique for both OKC and CKC eccentric-specific training).61,65,123,148,149,160,190 Eccentric-specific training should be integrated with progressive deceleration/change-of-direction tasks, because these tasks require the quadriceps to perform high-velocity eccentric contractions into large external knee flexion moments.44,46,49,71,188
Figure 12. Preferred exercise technique for eccentric-specific resistance training.

Eccentric-specific open and closed-kinetic-chain quadriceps resistance training should be progressed onto load-intensities > 100% of the surgical limb’s concentric 1-repitition maximum. Eccentric-specific quadriceps training can be completed on a leg press with a decline ankle-wedge (a-d) or knee extension machine (e-h) by (1) performing a concentric contraction with both limbs from the machine’s bottom position (a, e) to the top position (b, f), (2) removing/moving the non-surgical limb to place all load on the surgical limb (c, g), and (3) eccentrically lowering the load through the desired range of knee motion. Green shading, concentric phase of exercise; red shading, eccentric phase of exercise; white asterisk, heel wedge; yellow asterisk; movement of the non-surgical limb throughout exercise.
Power and Velocity-Based Training
The rehabilitation specialist should implement load-progressions with the specific intent of improving quadriceps rate-of-force development/knee power.191 Higher level evidence has observed longstanding impairments in quadriceps rate-of-force development after ACLR, and the use of a BPTB or QT autograft for ACLR may exacerbate these impairments.192 Velocity-based training can be utilized to improve quadriceps rate-of-force development,105 and the integration of these exercises with ballistic/plyometric exercise may enhance change-of-direction performance,193 improve knee biomechanics/motor control,194,195 and can mitigate the overall risk of ACL re-injury.196
Velocity-based quadriceps training may be most specifically prescribed utilizing a jump training machine and/or barbell equipped with a linear positioning transducer/accelerometer (Figure 13) (see Video, Supplemental Material 22 and 23, which demonstrate single and double-leg velocity-based training).197,198 To best stimulate improvements in peak quadriceps contraction-velocity/knee power, emphasis should be placed on the importance of a maximal effort/intent on each repetition, and working sets should be discontinued at a 10% velocity-loss threshold.198 Lastly, velocity-based quadriceps training should be integrated with ballistic/plyometric exercises, which may improve the function of the stretch-shortening cycle within the quadriceps (see Video, Supplemental Material 24, which demonstrates a plyometric exercise example).191,193,199
Figure 13. Example of velocity-based training with a linear positioning transducer/accelerometer.
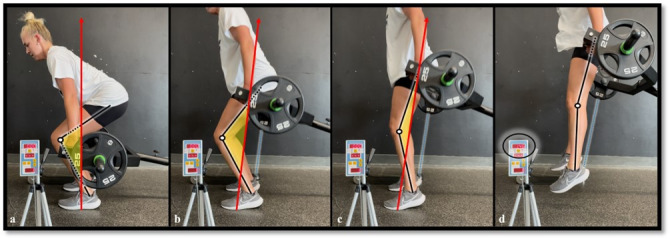
Velocity-based training methods can be utilized after anterior cruciate ligament reconstruction to improve quadriceps motor recruitment and rate-of-force development (a-d). To best stimulate improvements in peak quadriceps contraction-velocity/knee power, emphasis should be placed on the importance of a maximal effort/intent on each repetition. Black lines, approximate tibial and femoral bone markers; black circle, feedback monitor from linear positioning transducer/accelerometer; blue lines, ripcord connecting the exercise bar to the linear positioning transducer/accelerometer; red arrows; approximate ground reaction force-vector; white circles; estimated center of joint rotation; yellow shading; depiction of external knee flexion moment.
High-Velocity Running
To prepare the proximal quadriceps/rectus femoris for sport, graded exposure to high-velocity running should be integrated into the power phase of rehabilitation.30,200 High-velocity running produces large angular velocities at the knee, requiring the quadriceps to perform repeated high-load eccentric contractions (see Video, Supplemental Material 25, which demonstrates high-velocity running on a curved treadmill).201 With this, load management is of extreme importance, and the rehabilitation specialist should gradually increase running volume and intensity. Likewise, an upwards of 3-4 days of recovery may be initially required in between fatiguing exposures to high-velocity running until the repeated bout effect of eccentric training on muscle soreness is reported,202 especially as the rectus femoris appears to have a higher proportion of type-II muscle fibers relative to the other quadriceps muscles.54
CONCLUSION
Quadriceps weakness after ACLR is a well-known phenomenon.13,51,128 Although recent literature has investigated the best-practice methodologies for mitigating AMI after knee injury,31–33 less has been published with respect to the use of exercise therapy to restore quadriceps size and strength after ACLR.31 By combining common ACLR rehabilitation principles with muscle basic science and strength training literature, this review article provides a rehabilitation framework that can be used to optimize the recovery of quadriceps size and strength after ACLR, as well as recover the knee’s ability to manage the force-profiles associated with high-demand physical activities (i.e., Level-1 sport). Lastly, this review article may serve as a foundational piece of literature for the further development of more robust ACLR rehabilitation programs, to which the rehabilitation specialist can use the exercise progressions outline within this article to organize any other loading exposures needed to optimize individualized outcomes after ACLR.
PRACTICAL APPLICATION
After ACLR, optimal quadriceps load-progressions can be derived from combining common rehabilitation principles with the existing muscle basic science and strength training literature. The anatomy, regional innervation, and task-specific activation/sequencing of the quadriceps necessitates the rehabilitation specialist to utilize both OKC and CKC exercises to maximally stimulate quadriceps hypertrophy and strength. Graft-specific load progressions are also indicated after ACLR, and the rehabilitation specialist should consider the exercise type; muscle contraction mode; intensity of external load; and knee flexion angle when prescribing resistance training. To enhance the hypertrophic response to resistance training, exercise selection should include stable, single-limb exercises that load the quadriceps close to volitional fatigue/task failure at relatively long muscle lengths. Lastly, load-progressions for both OKC and CKC quadriceps strength training should be primarily advanced through the progression of knee flexion and external load.
Conflicts of Interest
The above authors have no conflicts of interest related to the development and publication efforts of this manuscript. The authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in this manuscript.
Supplementary Material
Acknowledgments
Acknowledgments
We extend a special thank you to Hollis Fritz, MD; Jill Monson, MPT; and Jon Schoenecker, DPT, for their gift of time, mentoring, and teaching within the Twin Cities. We commemorate Chris Beardsley for his commitment to the dissemination and pragmatic translation of strength training research, which was the inspiration for this manuscript. Lastly, thank you to the physical therapists, licensed athletic trainers, sports scientists, and performance/strength coaches at Training HAUS for their ongoing teamwork and support, as well as the research department and bioengineering lab at Twin Cities Orthopedics for their support with ongoing research projects.
References
- Anterior cruciate ligament injury risk in sport: A systematic review and meta-analysis of injury incidence by sex and sport classification. Montalvo A. M., Schneider D. K., Webster K. E.., et al. 2019J Athl Train. 54(5):472–482. doi: 10.4085/1062-6050-407-16. https://doi.org/10.4085/1062-6050-407-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anatomical versus non-anatomical single bundle anterior cruciate ligament reconstruction: A cadaveric study of comparison of knee stability. Lim H.-C., Yoon Y.-C., Wang J.-H., Bae J.-H. 2012Clin Orthop Surg. 4(4):249. doi: 10.4055/cios.2012.4.4.249. https://doi.org/10.4055/cios.2012.4.4.249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anatomical anterior cruciate ligament reconstruction (ACLR) results in fewer rates of atraumatic graft rupture, and higher rates of rotatory knee stability: a meta-analysis. Eliya Y., Nawar K., Rothrauff B. B., Lesniak B. P., Musahl V., de SA D. 2020Journal of ISAKOS. 5:359–370. doi: 10.1136/jisakos-2020-000476. https://doi.org/10.1136/jisakos-2020-000476 [DOI] [Google Scholar]
- Treatment after anterior cruciate ligament injury: Panther Symposium ACL Treatment Consensus Group. Diermeier T., Rothrauff B. B., Engebretsen L.., et al. 2020Orthop J Sports Med. 8:232596712093109. doi: 10.1177/2325967120931097. https://doi.org/10.1177/2325967120931097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Why bone-patella tendon-bone grafts should still be considered the gold standard for anterior cruciate ligament reconstruction. Carmichael J. R., Cross M. J. 2009Br J Sports Med. 43:323–325. doi: 10.1136/bjsm.2009.058024. https://doi.org/10.1136/bjsm.2009.058024 [DOI] [PubMed] [Google Scholar]
- Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Gifstad T., Foss O. A., Engebretsen L., Lind M., Forssblad M., Albrektsen G., Drogset J. O. 2014Am J Sports Med. 42:2319–28. doi: 10.1177/0363546514548164. https://doi.org/10.1177/0363546514548164 [DOI] [PubMed] [Google Scholar]
- Incidence and predictors of subsequent surgery after anterior cruciate ligament reconstruction: A 6-year follow-up study. Sullivan J. P., Huston L. J., Zajichek A.., et al. 2020Am J Sports Med. 48:2418–2428. doi: 10.1177/0363546520935867. https://doi.org/10.1177/0363546520935867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anatomic anterior cruciate ligament (ACL) reconstruction: a global perspective. Part 1. Middleton K.K., Hamilton T., Irrgang J.J., Karlsson J., Harner C.D., Fu F.H. 2014Knee Surg Sports Traumatol Arthrosc. 22:1467–82. doi: 10.1007/s00167-014-2846-3. https://doi.org/10.1007/s00167-014-2846-3 [DOI] [PubMed] [Google Scholar]
- ACL Study Group survey reveals the evolution of anterior cruciate ligament reconstruction graft choice over the past three decades. Arnold M. P., Calcei J. G., Vogel N.., et al. 2021Knee Surg Sports Traumatol Arthrosc. 29:3871–3876. doi: 10.1007/s00167-021-06443-9. https://doi.org/10.1007/s00167-021-06443-9 [DOI] [PubMed] [Google Scholar]
- Editorial commentary: Quadriceps tendon autograft use for anterior cruciate ligament reconstruction predicted to increase. Lubowitz J. H. 2016Arthroscopy. 32(1):76–77. doi: 10.1016/j.arthro.2015.11.004. https://doi.org/10.1016/j.arthro.2015.11.004 [DOI] [PubMed] [Google Scholar]
- Residual strength of the quadriceps versus patellar tendon after harvesting a central free tendon graft. Adams D. J., Mazzocca A. D., Fulkerson J. P. 2006Arthroscopy. 22(1):76–79. doi: 10.1016/j.arthro.2005.10.015. https://doi.org/10.1016/j.arthro.2005.10.015 [DOI] [PubMed] [Google Scholar]
- Quadriceps arthrogenic muscle inhibition: Neural mechanisms and treatment perspectives. Rice D. A., McNair P. J. Dec;2010 Semin Arthritis Rheum. 40(3):250–266. doi: 10.1016/j.semarthrit.2009.10.001. https://doi.org/10.1016/j.semarthrit.2009.10.001 [DOI] [PubMed] [Google Scholar]
- Arthrogenic muscle inhibition following anterior cruciate ligament injury. Pietrosimone B., Lepley A. S., Kuenze C., Harkey M. S., Hart J. M., Blackburn J. T., Norte G. 2022J Sport Rehabil. 31(6):694–706. doi: 10.1123/jsr.2021-0128. https://doi.org/10.1123/jsr.2021-0128 [DOI] [PubMed] [Google Scholar]
- Bone-patellar tendon-bone versus hamstring tendon autografts for primary anterior cruciate ligament reconstruction: A systematic review of overlapping meta-analyses. Schuette H. B., Kraeutler M. J., Houck D. A., McCarty E. C. 2017Orthop J Sports Med. 5(11):2325967117736484. doi: 10.1177/2325967117736484. https://doi.org/10.1177/2325967117736484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction: a systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone-patellar tendon-bone and hamstring-tendon autografts. Mouarbes D., Menetrey J., Marot V., Courtot L., Berard E., Cavaignac E. 2019Am J Sports Med. 47:3531–3540. doi: 10.1177/0363546518825340. https://doi.org/10.1177/0363546518825340 [DOI] [PubMed] [Google Scholar]
- Knee strength deficits following anterior cruciate ligament reconstruction differ between quadriceps and hamstring tendon autografts. Johnston P. T., Feller J. A., McClelland J. A., Webster K. E. 2021Knee Surg Sports Traumatol Arthrosc. 30(4):1300–1310. doi: 10.1007/s00167-021-06565-0. https://doi.org/10.1007/s00167-021-06565-0 [DOI] [PubMed] [Google Scholar]
- Knee muscle strength after quadriceps tendon autograft anterior cruciate ligament reconstruction: systematic review and meta-analysis. Johnston P. T., McClelland J. A., Feller J. A., Webster K. E. 2021Knee Surg Sports Traumatol Arthrosc. 29(9):2918–2933. doi: 10.1007/s00167-020-06311-y. https://doi.org/10.1007/s00167-020-06311-y [DOI] [PubMed] [Google Scholar]
- Quadriceps strength following anterior cruciate ligament reconstruction: normative values based on sex, graft type and meniscal status at 3, 6 & 9 months. Schwery N. A., Kiely M. T., Larson C. M.., et al. Int J Sports Phys Ther. 2022:17. doi: 10.26603/001c.32378. https://doi.org/10.26603/001c.32378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quadriceps strength asymmetry after anterior cruciate ligament reconstruction alters knee joint biomechanics and functional performance at time of return to activity. Palmieri-Smith R. M., Lepley L. K. 2015Am J Sports Med. 43(7):1662–1669. doi: 10.1177/0363546515578252. https://doi.org/10.1177/0363546515578252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young athletes after ACL reconstruction with asymmetric quadriceps strength at the time of return-to-sport clearance demonstrate drop-landing asymmetries two years later. Ithurburn M. P., Thomas S., Paterno M. V., Schmitt L. C. 2021Knee. 29:520–529. doi: 10.1016/j.knee.2021.02.036. https://doi.org/10.1016/j.knee.2021.02.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Athletes with bone-patellar tendon-bone autograft for anterior cruciate ligament reconstruction were slower to meet rehabilitation milestones and return-to-sport criteria than athletes with hamstring tendon autograft or soft tissue allograft : secondary analysis from the ACL-SPORTS trial. Smith A.H., Capin J.J., Zarzycki R., Snyder-Mackler L. 2020J Orthop Sports Phys Ther. 50:259–266. doi: 10.2519/jospt.2020.9111. https://doi.org/10.2519/jospt.2020.9111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deficits in quadriceps strength and patient-oriented outcomes at return to activity after ACL reconstruction. Lepley L. K. 2015Sports Health. 7(3):231–238. doi: 10.1177/1941738115578112. https://doi.org/10.1177/1941738115578112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quadriceps strength, muscle activation failure, and patient-reported function at the time of return to activity in patients following anterior cruciate ligament reconstruction: A cross-sectional study. Lepley L. K., Palmieri-Smith R. M. 2015J Orthop Sports Phys Ther. 45(12):1017–1025. doi: 10.2519/jospt.2015.5753. https://doi.org/10.2519/jospt.2015.5753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The influence of quadriceps strength asymmetry on patient-reported function at time of return to sport after anterior cruciate ligament reconstruction. Zwolski C., Schmitt L.C., Quatman-Yates C., Thomas S., Hewett T.E., Paterno M.V. 2015Am J Sports Med. 43(9):2242–2249. doi: 10.1177/0363546515591258. https://doi.org/10.1177/0363546515591258 [DOI] [PubMed] [Google Scholar]
- Young athletes after ACL reconstruction with quadriceps strength asymmetry at the time of return-to-sport demonstrate decreased knee function 1 year later. Ithurburn M. P., Altenburger A. R., Thomas S., Hewett T. E., Paterno M. V., Schmitt L. C. 2018Knee Surg Sports Traumatol Arthrosc. 26 doi: 10.1007/s00167-017-4678-4. https://doi.org/10.1007/s00167-017-4678-4 [DOI] [PubMed] [Google Scholar]
- Age, gender, quadriceps strength and hop test performance are the most important factors affecting the achievement of a patient-acceptable symptom state after ACL reconstruction. Cristiani R., Mikkelsen C., Edman G., Forssblad M., Engström B., Stålman A. Knee Surg Sports Traumatol Arthrosc. 2020:28. doi: 10.1007/s00167-019-05576-2. https://doi.org/10.1007/s00167-019-05576-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Symmetries in muscle torque and landing kinematics are associated with maintenance of sports participation at 5 to 10 years after ACL reconstruction in young men. Hetsroni I., Wiener Y., Ben-Sira D., Iacono A.D., Marom N., van Stee M., Ayalon M. 2020Orthop J Sports Med. 8:27. doi: 10.1177/2325967120923267. https://doi.org/10.1177/2325967120923267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post-traumatic osteoarthritis following ACL injury. Wang L.-J., Zeng N., Yan Z.-P., Li J.-T., Ni G.-X. 2020Arthritis Res Ther. 22:57. doi: 10.1186/s13075-020-02156-5. https://doi.org/10.1186/s13075-020-02156-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association of quadriceps strength symmetry and surgical status with clinical osteoarthritis five years after anterior cruciate ligament rupture. Arhos E. K., Thoma L. M., Grindem H., Logerstedt D., Risberg M. A., Snyder-Mackler L. 2022Arthritis Care Res. 74(3):386–391. doi: 10.1002/acr.24479. https://doi.org/10.1002/acr.24479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Optimising the late-stage rehabilitation and return-to-sport training and testing process after ACL reconstruction. Buckthorpe M. 2019Sports Med. 49:30. doi: 10.1007/s40279-019-01102-z. https://doi.org/10.1007/s40279-019-01102-z [DOI] [PubMed] [Google Scholar]
- Restoring knee extensor strength after anterior cruciate ligament reconstruction: A clinical commentary. Buckthorpe M., La Rosa G., Della Villa F. 2019Int J Sports Phys Ther. 14(1):159. doi: 10.26603/ijspt20190159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arthrogenic muscle inhibition after ACL reconstruction: a scoping review of the efficacy of interventions. Sonnery-Cottet B., Saithna A., Quelard B.., et al. 2019Br J Sports Med. 53(5) doi: 10.1136/bjsports-2017-098401. https://doi.org/10.1136/bjsports-2017-098401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quadriceps function following ACL reconstruction and rehabilitation: implications for optimisation of current practices. Gokeler A., Bisschop M., Benjaminse A., Myer G.D., Eppinga P., Otten E. 2014Knee Surg Sports Traumatol Arthrosc. 22:1163–1174. doi: 10.1007/s00167-013-2577-x. https://doi.org/10.1007/s00167-013-2577-x [DOI] [PubMed] [Google Scholar]
- Combination of eccentric exercise and neuromuscular electrical stimulation to improve quadriceps function post-ACL reconstruction. Lepley L. K., Wojtys E. M., Palmieri-Smith R. M. 2015Knee. 22(3):270–277. doi: 10.1016/j.knee.2014.11.013. https://doi.org/10.1016/j.knee.2014.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ACL reconstruction rehabilitation: clinical data, biologic healing, and criterion-based milestones to inform a return-to-sport guideline. Brinlee A. W., Dickenson S. B., Hunter-Giordano A., Snyder-Mackler L. Sports Health. 2022:19417381211056873. doi: 10.1177/19417381211056873. https://doi.org/10.1177/19417381211056873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conceptual framework for strengthening exercises to prevent hamstring strains. Guex K., Millet G. P. 2013Sports Med. 43:1207–1215. doi: 10.1007/s40279-013-0097-y. https://doi.org/10.1007/s40279-013-0097-y [DOI] [PubMed] [Google Scholar]
- An evidence-based framework for strengthening exercises to prevent hamstring injury. Bourne M. N., Timmins R. G., Opar D. A.., et al. 2018Sports Med. 48:251–267. doi: 10.1007/s40279-017-0796-x. https://doi.org/10.1007/s40279-017-0796-x [DOI] [PubMed] [Google Scholar]
- Moore K. L., Dalley A. F., II, Agur A. M. Moore's clinically oriented anatomy. Lippincott Williams & Wilkins; pp. 545–546. [Google Scholar]
- An explanation for various rectus femoris strain injuries using previously undescribed muscle architecture. Hasselman C. T., Best T. M., Hughes C., Martinez S., Garrett W. E. 1995Am J Sports Med. 23(4):493–499. doi: 10.1177/036354659502300421. https://doi.org/10.1177/036354659502300421 [DOI] [PubMed] [Google Scholar]
- Neurovascular anatomy of the rectus femoris muscle related to functioning muscle transfer. Yang D., Morris S.F. 1999Plast Reconstr Surg. 104(1):102–106. doi: 10.1097/00006534-199907000-00014. https://doi.org/10.1097/00006534-199907000-00014 [DOI] [PubMed] [Google Scholar]
- Amplitude and timing of electromyographic activity during sprinting. Jönhagen S., Ericson M. O., Németh G., Eriksson E. 2007Scand J Med Sci Sports. 6(1):15–21. doi: 10.1111/j.1600-0838.1996.tb00064.x. https://doi.org/10.1111/j.1600-0838.1996.tb00064.x [DOI] [PubMed] [Google Scholar]
- Muscular activation patterns during the soccer in-step kick. Cerrah A. O., Gungor E. O., Soylu A. R., Ertan H., Lees A., Bayrak C. 2011Isokinet Exerc Sci. 19(3):181–190. doi: 10.3233/ies-2011-0414. https://doi.org/10.3233/ies-2011-0414 [DOI] [Google Scholar]
- An electromyographic analysis of quadriceps femoris muscle setting and straight leg raising. Soderberg G. L., Cook T. M. 1983Phys Ther. 63(9):1434–1438. doi: 10.1093/ptj/63.9.1434. https://doi.org/10.1093/ptj/63.9.1434 [DOI] [PubMed] [Google Scholar]
- Unique activation of the quadriceps femoris during single- and multi-joint exercises. Ema R., Sakaguchi M., Akagi R., Kawakami Y. 2016Eur J Appl Physiol. 116:1031–1041. doi: 10.1007/s00421-016-3363-5. https://doi.org/10.1007/s00421-016-3363-5 [DOI] [PubMed] [Google Scholar]
- Quadriceps activation in closed and in open kinetic chain exercise. Stensdotter A.-K., Hodges P. W., Mellor R., Sundelin G., Hager-Ross C. 2003Med Sci Sports Exerc. 35(12):2043–2047. doi: 10.1249/01.Mss.0000099107.03704.Ae. https://doi.org/10.1249/01.Mss.0000099107.03704.Ae [DOI] [PubMed] [Google Scholar]
- Longitudinal sequencing in intramuscular coordination: A new hypothesis of dynamic functions in the human rectus femoris muscle. von Laßberg C., Schneid J. A., Graf D., Finger F., Rapp W., Stutzig N. 2017PLoS One. 12(8):e0183204. doi: 10.1371/journal.pone.0183204. https://doi.org/10.1371/journal.pone.0183204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Non-uniform surface electromyographic responses to change in joint angle within rectus femoris muscle. Watanabe K., Kouzaki M., Moritani T. 2014Muscle Nerve. 50(5):794–802. doi: 10.1002/mus.24232. https://doi.org/10.1002/mus.24232 [DOI] [PubMed] [Google Scholar]
- Partial range of motion training elicits favorable improvements in muscular adaptations when carried out at long muscle lengths. Pedrosa G. F., Lima F. V., Schoenfeld B. J.., et al. 2022Eur J Sports Sci. 22(8):1250–1260. doi: 10.1080/17461391.2021.1927199. [DOI] [PubMed] [Google Scholar]
- Signal intensity of MR-images of thigh muscles following acute open- and closed chain kinetic knee extensor exercise - index of muscle use. Enocson A. G., Berg H. E., Vargas R., Jenner G., Tesch P. A. 2005Eur J Appl Physiol. 94:357–63. doi: 10.1007/s00421-005-1339-y. https://doi.org/10.1007/s00421-005-1339-y [DOI] [PubMed] [Google Scholar]
- Intermuscle differences in activation. Behm D. G., Whittle J., Button D., Power K. 2002Muscle Nerve. 25(2):236–243. doi: 10.1002/mus.10008. https://doi.org/10.1002/mus.10008 [DOI] [PubMed] [Google Scholar]
- Muscle atrophy after ACL injury: Implications for clinical practice. Lepley L. K., Davi S. M., Burland J. P., Lepley A. S. 2020Sports Health. 12(6):579–586. doi: 10.1177/1941738120944256. https://doi.org/10.1177/1941738120944256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motor unit discharge rate and the estimated synaptic input to the vasti muscles is higher in open compared with closed kinetic chain exercise. Boccia G., Martinez-Valdes E., Negro F., Rainoldi A., Falla D. 2019J Appl Physiol. 127(4):950–958. doi: 10.1152/japplphysiol.00310.2019. https://doi.org/10.1152/japplphysiol.00310.2019 [DOI] [PubMed] [Google Scholar]
- Reference values for vastus lateralis fiber size and type in healthy subjects over 40 years old: a systematic review and metaanalysis. Gouzi F., Maury J., Molinari N., Pomiès P., Mercier J., Préfaut C., Hayot M. 2013J Appl Physiol. 115(3):346–354. doi: 10.1152/japplphysiol.01352.2012. https://doi.org/10.1152/japplphysiol.01352.2012 [DOI] [PubMed] [Google Scholar]
- Data on the distribution of fibre types in thirty-six human muscles. Johnson M. A., Polgar J., Weightman D., Appleton D. 1973J Neurol Sci. 18(1):111–129. doi: 10.1016/0022-510x(73)90023-3. https://doi.org/10.1016/0022-510x(73)90023-3 [DOI] [PubMed] [Google Scholar]
- Differences in activation patterns between eccentric and concentric quadriceps contractions. Mchugh M. P., Tyler T. F., Greenberg S. C., Gleim G. W. 2002J Sports Sci. 20(2):83–91. doi: 10.1080/026404102317200792. https://doi.org/10.1080/026404102317200792 [DOI] [PubMed] [Google Scholar]
- A review on strength exercise-induced muscle damage: applications, adaptation mechanisms and limitations. Brentano M. A., Kruel M. L. F. 2011J Sports Med Phys Fitness. 51(1):1–10. [PubMed] [Google Scholar]
- Comparison between leg and arm eccentric exercises of the same relative intensity on indices of muscle damage. Jamurtas A. Z., Theocharis V., Tofas T.., et al. 2005Eur J Appl Physiol. 95:179–185. doi: 10.1007/s00421-005-1345-0. https://doi.org/10.1007/s00421-005-1345-0 [DOI] [PubMed] [Google Scholar]
- Damage and the repeated bout effect of arm, leg, and trunk muscles induced by eccentric resistance exercises. Chen T. C., Yang T. J., Huang M. J., Wang H. S., Tseng K. W., Chen H. L., Nosaka K. 2019Scand J Med Sci Sports. 29(5):725–735. doi: 10.1111/sms.13388. https://doi.org/10.1111/sms.13388 [DOI] [PubMed] [Google Scholar]
- Mechanotherapy: how physical therapists' prescription of exercise promotes tissue repair. Khan K. M., Scott A. 2009Br J Sports Med. 43(4):247–252. doi: 10.1136/bjsm.2008.054239. https://doi.org/10.1136/bjsm.2008.054239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dissecting muscle power output. Josephson R. K. 1999J Exp Biol. 202(23):3369–3375. doi: 10.1242/jeb.202.23.3369. [DOI] [PubMed] [Google Scholar]
- Muscle hypertrophy response to range of motion in strength training: a novel approach to understanding the findings. Ottinger C. R., Sharp M. H., Stefan M. W., Gheith R. H., de la Espriella F., Wilson J. M. 2023Strength Cond J. 45(2):162–176. doi: 10.1519/ssc.0000000000000737. https://doi.org/10.1519/ssc.0000000000000737 [DOI] [Google Scholar]
- Isometric training and long-term adaptations: Effects of muscle length, intensity, and intent: A systematic review. Oranchuk D. J., Storey A. G., Nelson A. R., Cronin J. B. 2019Scand J Med Sci Sports. 29(4):484–503. doi: 10.1111/sms.13375. https://doi.org/10.1111/sms.13375 [DOI] [PubMed] [Google Scholar]
- The effects of hip flexion angle on quadriceps femoris muscle hypertrophy in the leg extension exercise. Larsen S., Kristiansen B. S., Swinton P. A.., et al. May 5;2024 SportRxiv. doi: 10.51224/SRXIV.407. https://doi.org/10.51224/SRXIV.407 [DOI]
- Partial vs full range of motion resistance training: A systematic review and meta-analysis. Wolf M., Androulakis-Korakakis P., Fisher J., Schoenfeld B., Steele J. 2023Int J Strength Condit. 3(1):2634–2235. doi: 10.47206/ijsc.v3i1.182. https://doi.org/10.47206/ijsc.v3i1.182 [DOI] [Google Scholar]
- The range of sarcomere lengths in the muscles of the human lower limb. Cutts A. 1988J Anat. 160:79–88. [PMC free article] [PubMed] [Google Scholar]
- Intraoperative and biomechanical studies of human vastus lateralis and vastus medialis sarcomere length operating range. Son J., Indresano A., Sheppard K., Ward S.R., Lieber R.L. 2018J Biomech. 67:91–97. doi: 10.1016/j.jbiomech.2017.11.038. https://doi.org/10.1016/j.jbiomech.2017.11.038 [DOI] [PubMed] [Google Scholar]
- Experiment demonstrating skeletal muscle biomechanics. DiCarlo S. E., Sipe E., Layshock P. J., Varyani S. 1998Adv Physiol Educ. 275(6):59. doi: 10.1152/advances.1998.275.6.S59. [DOI] [PubMed] [Google Scholar]
- Effects of squat training with different depths on lower limb muscle volumes. Kubo K., Ikebukuro T., Yata H. 2019Eur J Appl Physiol. 119:1933–1942. doi: 10.1007/s00421-019-04181-y. https://doi.org/10.1007/s00421-019-04181-y [DOI] [PubMed] [Google Scholar]
- Muscle balance at the knee-moment arms for the normal knee and the ACL-minus knee. Buford W. L., Ivey M. F., Malone D., Patterson R. M., Pearce G. L., Nguyen D. K., Stewart A. A. 1997IEEE Trans Rehabil Eng. 5(4):367–379. doi: 10.1109/86.650292. [DOI] [PubMed] [Google Scholar]
- Knee muscle moment arms from MRI and from tendon travel. Spoor C., Van Leeuwen J. 1992J Biomech. 25(2):201–206. doi: 10.1016/0021-9290(92)90276-7. [DOI] [PubMed] [Google Scholar]
- Graft-specific surgical and rehabilitation considerations for anterior cruciate ligament reconstruction with the quadriceps tendon autograft. Solie B., Monson J., Larson C. 2023Int J Sports Phys Ther. 18(2):493. doi: 10.26603/001c.73797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Variation in the patellar tendon moment arm identified with an improved measurement framework. Dandridge O., Garner A., Amis A.A., Cobb J.P., Arkel R.J. 2022J Orthop Res. 40(4):799–807. doi: 10.1002/jor.25124. https://doi.org/10.1002/jor.25124 [DOI] [PubMed] [Google Scholar]
- An investigation into setting the blood flow restriction pressure based on perception of tightness. Bell Z. W., Dankel S. J., Mattocks K. T.., et al. 2018Physiol Meas. 39(10):105006. doi: 10.1088/1361-6579/aae140. https://doi.org/10.1088/1361-6579/aae140 [DOI] [PubMed] [Google Scholar]
- Multiplane loading of the extensor mechanism alters the patellar ligament force/quadriceps force ratio. Powers C. M., Chen Y.-J., Scher I. S., Lee T. Q. 2010J Biomech Engineer. 132(2) doi: 10.1115/1.4000852. https://doi.org/10.1115/1.4000852 [DOI] [PubMed] [Google Scholar]
- Biomechanics of the knee-extension exercise. Effect of cutting the anterior cruciate ligament. Grood E. S., Suntay W. J., Noyes F. R., Butler D. L. 1984J Bone Joint Surg. 66(5):725–734. doi: 10.2106/00004623-198466050-00011. [DOI] [PubMed] [Google Scholar]
- The effective quadriceps and patellar tendon moment arms relative to the tibiofemoral finite helical axis. Im H. S., Goltzer O., Sheehan F. T. 2015J Biomech. 48(14):3737–3742. doi: 10.1016/j.jbiomech.2015.04.003. https://doi.org/10.1016/j.jbiomech.2015.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biomechanics of the knee extensor mechanism and its relationship to patella tendinopathy: A review. Dan M., Parr W., Broe D., Cross M., Walsh W.R. 2018J Orthop Res. 36(12):3105–3112. doi: 10.1002/jor.24120. https://doi.org/10.1002/jor.24120 [DOI] [PubMed] [Google Scholar]
- Distinguishing quadriceps tendinopathy and patellar tendinopathy: Semantics or significant? Sprague A., Epsley S., Silbernagel K. G. 2019J Orthop Sports Phys Ther. 49(4):627–630. doi: 10.2519/jospt.2019.0611. https://doi.org/10.2519/jospt.2019.0611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Localization of muscle damage within the quadriceps femoris induced by different types of eccentric exercises. Maeo S., Saito A., Otsuka S., Shan X., Kanehisa H., Kawakami Y. 2018Scand J Med Sci Sports. 28(1):95–106. doi: 10.1111/sms.12880. https://doi.org/10.1111/sms.12880 [DOI] [PubMed] [Google Scholar]
- Neuromuscular adaptations to work-matched maximal eccentric versus concentric training. Maeo S., Shan X., Otsuka S., Kanehisa H., Kawakami Y. 2018Med Sci Sports Exerc. 50(8):1629–1640. doi: 10.1249/mss.0000000000001611. https://doi.org/10.1249/mss.0000000000001611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Effects of blood flow restricted low-intensity concentric or eccentric training on muscle size and strength. Yasuda T., Loenneke J. P., Thiebaud R. S., Abe T. 2012PLoS One. 7(12) doi: 10.1371/journal.pone.0052843. https://doi.org/10.1371/journal.pone.0052843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skeletal muscle remodeling in response to eccentric vs. concentric loading: morphological, molecular, and metabolic adaptations. Franchi M. V., Reeves N. D., Narici M. V. 2017Front Physiol. 8:82. doi: 10.3389/fphys.2017.00447. https://doi.org/10.3389/fphys.2017.00447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Effects of isometric, eccentric, or heavy slow resistance exercises on pain and function in individuals with patellar tendinopathy: A systematic review. Lim H. Y., Wong S. H. 2018Physiother Res Int. 23(4):e1721. doi: 10.1002/pri.1721. https://doi.org/10.1002/pri.1721 [DOI] [PubMed] [Google Scholar]
- The effects of eccentric versus concentric resistance training on muscle strength and mass in healthy adults: A systematic review with meta-analysis. Roig M., O'Brien K., Kirk G., Murray R., McKinnon P., Shadgan B., Reid W. D. 2009Br J Sports Med. 43(8):556–568. doi: 10.1136/bjsm.2008.051417. https://doi.org/10.1136/bjsm.2008.051417 [DOI] [PubMed] [Google Scholar]
- Strength and power training in rehabilitation: underpinning principles and practical strategies to return athletes to high performance. Maestroni L., Read P., Bishop C., Turner A. 2020Sports Med. 50(2):239–252. doi: 10.1007/s40279-019-01195-6. https://doi.org/10.1007/s40279-019-01195-6 [DOI] [PubMed] [Google Scholar]
- Task differences with the same load torque alter the endurance time of submaximal fatiguing contractions in humans. Hunter S.K., Ryan D.L., Ortega J.D., Enoka R.M. 2002J Neurophysiol. 88(6):3087–3096. doi: 10.1152/jn.00232.2002. https://doi.org/10.1152/jn.00232.2002 [DOI] [PubMed] [Google Scholar]
- Comparison of electromyographic activity during eccentrically versus concentrically loaded isometric contractions. Garner J. C., Blackburn T., Weimar W., Campbell B. 2008J Electromyogr Kinesiol. 18(3):466–471. doi: 10.1016/j.jelekin.2006.11.006. https://doi.org/10.1016/j.jelekin.2006.11.006 [DOI] [PubMed] [Google Scholar]
- Are there two forms of isometric muscle action? Results of the experimental study support a distinction between a holding and a pushing isometric muscle function. Schaefer L. V., Bittmann F. N. 2017BMC Sports Sci Med Rehabil. 9:11. doi: 10.1186/s13102-017-0075-z. https://doi.org/10.1186/s13102-017-0075-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isometric contractions are more analgesic than isotonic contractions for patellar tendon pain. Rio E., van Ark M., Docking S.., et al. 2017Clin J Sport Med. 27(3):253–259. doi: 10.1097/jsm.0000000000000364. https://doi.org/10.1097/jsm.0000000000000364 [DOI] [PubMed] [Google Scholar]
- Eccentric exercise to enhance neuromuscular control. Lepley L. K., Lepley A. S., Onate J. A., Grooms D. R. 2017Sports Health. 9(4):333–340. doi: 10.1177/1941738117710913. https://doi.org/10.1177/1941738117710913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. Rio E., Kidgell D., Purdam C., Gaida J., Moseley G. L., Pearce A. J., Cook J. 2015Br J Sports Med. 49(19):1277–1283. doi: 10.1136/bjsports-2014-094386. https://doi.org/10.1136/bjsports-2014-094386 [DOI] [PubMed] [Google Scholar]
- Contribution of neuromuscular factors to quadriceps asymmetry after anterior cruciate ligament reconstruction. Johnson A.K., Palmieri-Smith R.M., Lepley L.K. 2018J Athl Train. 53(4):347–354. doi: 10.4085/1062-6050-463-16. https://doi.org/10.4085/1062-6050-463-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Electrically evoked eccentric and concentric torque–velocity relationships in human knee extensor muscles. Seger T., Thorstensson T. 2000Acta Physiol Scand. 169(1):63–69. doi: 10.1046/j.1365-201x.2000.00694.x. [DOI] [PubMed] [Google Scholar]
- The eccentric: concentric strength ratio of human skeletal muscle in vivo: meta-analysis of the influences of sex, age, joint action, and velocity. Nuzzo J. L., Pinto M. D., Nosaka K., Steele J. 2023Sports Med. 53(6):1125–1136. doi: 10.1007/s40279-023-01851-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Current understanding of residual force enhancement: cross-bridge component and non-cross-bridge component. Fukutani A., Herzog W. 2019Int J Molec Sci. 20(21):5479. doi: 10.3390/ijms20215479. https://doi.org/10.3390/ijms20215479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Factors contributing to lower metabolic demand of eccentric compared with concentric cycling. Peñailillo L., Blazevich A. J., Nosaka K. 2017J Appl Physiol. 123(4):884–893. doi: 10.1152/japplphysiol.00536.2016. https://doi.org/10.1152/japplphysiol.00536.2016 [DOI] [PubMed] [Google Scholar]
- Metabolic demand and muscle damage induced by eccentric cycling of knee extensor and flexor muscles. Peñailillo L., Guzmán N., Cangas J., Reyes A., Zbinden-Foncea H. 2017Eur J Sports Sci. 17(2):179–187. doi: 10.1080/17461391.2016.1217278. https://doi.org/10.1080/17461391.2016.1217278 [DOI] [PubMed] [Google Scholar]
- Superior effects of eccentric to concentric knee extensor resistance training on physical fitness, insulin sensitivity and lipid profiles of elderly men. Chen T. C.-C., Tseng W.-C., Huang G.-L., Chen H.-L., Tseng K.-W., Nosaka K. 2017Front Physiol. 8 doi: 10.3389/fphys.2017.00209. https://doi.org/10.3389/fphys.2017.00209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razor hamstring curl and Nordic hamstring exercise architectural adaptations: Impact of exercise selection and intensity. Pollard C. W., Opar D. A., Williams M. D., Bourne M. N., Timmins R. G. 2019Scand J Med Sci Sports. 29(5):706–715. doi: 10.1111/sms.13381. https://doi.org/10.1111/sms.13381 [DOI] [PubMed] [Google Scholar]
- Effect of two eccentric hamstring exercises on muscle architectural characteristics assessed with diffusion tensor MRI. Suskens J. J. M., Secondulfo L., Kiliç Ö.., et al. 2023Scand J Med Sci Sports. 33(4):393–406. doi: 10.1111/sms.14283. https://doi.org/10.1111/sms.14283 [DOI] [PubMed] [Google Scholar]
- Short-term neuromuscular, morphological, and architectural responses to eccentric quasi-isometric muscle actions. Oranchuk D. J., Nelson A. R., Storey A. G., Diewald S. N., Cronin J. B. 2021Eur J Appl Physiol. 121:141–158. doi: 10.1007/s00421-020-04512-4. https://doi.org/10.1007/s00421-020-04512-4 [DOI] [PubMed] [Google Scholar]
- Scientific basis for eccentric quasi-isometric resistance training: a narrative review. Oranchuk D. J., Storey A. G., Nelson A. R., Cronin J. B. 2019J Strength Cond Res. 33(10):2846–2859. doi: 10.1519/jsc.0000000000003291. https://doi.org/10.1519/jsc.0000000000003291 [DOI] [PubMed] [Google Scholar]
- Heavy slow resistance versus eccentric training as treatment for Achilles tendinopathy. Beyer R., Kongsgaard M., Hougs Kjær B., Øhlenschlæger T., Kjær M., Magnusson S.P. 2015Am J Sports Med. 43(7):1704–1711. doi: 10.1177/0363546515584760. https://doi.org/10.1177/0363546515584760 [DOI] [PubMed] [Google Scholar]
- Putting “heavy” into heavy slow resistance. Morrison S., Cook J. 2022Sports Med. 52(6):1219–1222. doi: 10.1007/s40279-022-01641-y. https://doi.org/10.1007/s40279-022-01641-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Effects of velocity-based training on strength and power in elite athletes—a systematic review. Włodarczyk M., Adamus P., Zieliński J., Kantanista A. 2021Int J Environ Res Public Health. 18(10):5257. doi: 10.3390/ijerph18105257. https://doi.org/10.3390/ijerph18105257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The human force: velocity relationship; activity in the knee flexor and extensor muscles before and after eccentric practice. Rutherford O. M., Purcell C., Newham D. J. 2001Eur J Appl Physiol. 84:133–140. doi: 10.1007/s004210000332. [DOI] [PubMed] [Google Scholar]
- You are as fast as your motor neurons: speed of recruitment and maximal discharge of motor neurons determine the maximal rate of force development in humans. Del Vecchio A., Negro F., Holobar A., Casolo A., Folland J.P., Felici F., Farina D. 2019J Physiol. 597(9):2445–2456. doi: 10.1113/jp277396. https://doi.org/10.1113/jp277396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratamess N. ACSM's foundations of strength training and conditioning. Lippincott Williams & Wilkins; [Google Scholar]
- Mechanisms of anterior cruciate ligament neovascularization and ligamentization. Scranton P., Lanzer W., Ferguson M., Kirkman T., Pflaster D. 1998Arthroscopy. 14(7):702–716. doi: 10.1016/s0749-8063(98)70097-0. https://doi.org/10.1016/s0749-8063(98)70097-0 [DOI] [PubMed] [Google Scholar]
- Graft maturity of the reconstructed anterior cruciate ligament 6 months postoperatively: a magnetic resonance imaging evaluation of quadriceps tendon with bone block and hamstring tendon autografts. Ma Y., Murawski C. D., Rahnemai-Azar A. A., Maldjian C., Lynch A. D., Fu F. H. 2015Knee Surg Sports Traumatol Arthrosc. 23:661–668. doi: 10.1007/s00167-014-3302-0. https://doi.org/10.1007/s00167-014-3302-0 [DOI] [PubMed] [Google Scholar]
- Hamstring tendons or bone-patellar tendon-bone graft for anterior cruciate ligament reconstruction? Thaunat M., Fayard J. M., Sonnery-Cottet B. 2019Orthop Traumatol Surg Res. 105(1):S89–S94. doi: 10.1016/j.otsr.2018.05.014. https://doi.org/10.1016/j.otsr.2018.05.014 [DOI] [PubMed] [Google Scholar]
- Bone-patellar tendon–bone autograft maturation is superior to double-bundle hamstring tendon autograft maturation following anatomical anterior cruciate ligament reconstruction. Fukuda H., Ogura T., Asai S.., et al. 2022Knee Surg Sports Traumatol Arthrosc. 30(5):1661–1671. doi: 10.1007/s00167-021-06653-1. https://doi.org/10.1007/s00167-021-06653-1 [DOI] [PubMed] [Google Scholar]
- Tendon healing in a bone tunnel differs at the tunnel entrance versus the tunnel exit: an effect of graft-tunnel motion? Rodeo S. A., Kawamura S., Kim H.-J., Dynybil C., Ying L. 2006Am J Sports Med. 34(11):1790–800. doi: 10.1177/0363546506290059. https://doi.org/10.1177/0363546506290059 [DOI] [PubMed] [Google Scholar]
- Soft tissue fixation strategies of human quadriceps tendon grafts: A biomechanical study. Michel P. A., Domnick C., Raschke M. J.., et al. 2019Arthroscopy. 35(11):3069–3076. doi: 10.1016/j.arthro.2019.05.025. https://doi.org/10.1016/j.arthro.2019.05.025 [DOI] [PubMed] [Google Scholar]
- Biomechanical comparison of three suspensory techniques for all soft tissue central quadriceps tendon graft fixation. Arakgi M. E., Burkhart T. A., Hoshino T., Degen R., Getgood A. 2022Arthrosc Sports Med Rehabil. 4(3):843–851. doi: 10.1016/j.asmr.2021.12.008. https://doi.org/10.1016/j.asmr.2021.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Full thickness quadriceps tendon grafts with bone had similar material properties to bone-patellar tendon-bone and a four-strand semitendinosus grafts: a biomechanical study. Strauss M. J., Miles J. W., Kennedy M. L.., et al. 2022Knee Surg Sports Traumatol Arthrosc. 30(5):1786–1794. doi: 10.1007/s00167-021-06738-x. https://doi.org/10.1007/s00167-021-06738-x [DOI] [PubMed] [Google Scholar]
- Impact of quadriceps tendon graft thickness on electromechanical delay and neuromuscular performance after ACL reconstruction. Parrino R. L., Adams W., Letter M. I.., et al. 2023Orthop J Sports Med. 11(10):23259671231201832. doi: 10.1177/23259671231201832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Early versus late start of open kinetic chain quadriceps exercises after ACL reconstruction with patellar tendon or hamstring grafts: a prospective randomized outcome study. Heijne A., Werner S. 2007Knee Surg Sports Traumatol Arthrosc. 15:472–3. doi: 10.1007/s00167-007-0313-0. https://doi.org/10.1007/s00167-007-0313-0 [DOI] [PubMed] [Google Scholar]
- Tibial slope and medial meniscectomy significantly influence short-term knee laxity following ACL reconstruction. Dejour D., Pungitore M., Valluy J., Nover L., Saffarini M., Demey G. 2019Knee Surg Sports Traumatol Arthrosc. 27:3481–3489. doi: 10.1007/s00167-019-05435-0. https://doi.org/10.1007/s00167-019-05435-0 [DOI] [PubMed] [Google Scholar]
- Generalised joint hypermobility increases ACL injury risk and is associated with inferior outcome after ACL reconstruction: a systematic review. Sundemo D., Hamrin Senorski E., Karlsson L.., et al. 2019BMJ Open Sport Exerc Med. 5:e000620. doi: 10.1136/bmjsem-2019-000620. https://doi.org/10.1136/bmjsem-2019-000620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Validation of a risk calculator to personalize graft choice and reduce rupture rates for anterior cruciate ligament reconstruction. Marmura H., Getgood A. M. J., Spindler K. P., Kattan M. W., Briskin I., Bryant D. M. 2021Am J Sports Med. 49:1777–1785. doi: 10.1177/03635465211010798. https://doi.org/10.1177/03635465211010798 [DOI] [PubMed] [Google Scholar]
- Risk factors for revision or rerupture after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Zhao D., Pan J.-k., Lin F.-z.., et al. 2022Am J Sports Med. :036354652211197. doi: 10.1177/03635465221119787. https://doi.org/10.1177/03635465221119787 [DOI] [PubMed]
- Anterior cruciate ligament strain in-vivo: A review of previous work. Beynnon B. D., Fleming B. C. 1998J Biomech. 31(6):519–525. doi: 10.1016/s0021-9290(98)00044-x. https://doi.org/10.1016/s0021-9290(98)00044-x [DOI] [PubMed] [Google Scholar]
- Loaded open-kinetic-chain exercises stretch the anterior cruciate ligament more than closed-kinetic-chain exercises: In-vivo assessment of anterior cruciate ligament length change. Wang C., Qiu J., Wang Y.., et al. 2022Musculoskelet Sci Pract. 63:102715. doi: 10.1016/j.msksp.2022.102715. https://doi.org/10.1016/j.msksp.2022.102715 [DOI] [PubMed] [Google Scholar]
- Closed kinetic chain alone compared to combined open and closed kinetic chain exercises for quadriceps strengthening after anterior cruciate ligament reconstruction with respect to return to sports: a prospective matched follow-up study. Mikkelsen C., Werner S., Eriksson E. 2000Knee Surg Sports Traumatol Arthrosc. 8(6):337–342. doi: 10.1007/s001670000143. https://doi.org/10.1007/s001670000143 [DOI] [PubMed] [Google Scholar]
- Training for strength and hypertrophy: an evidence-based approach. Morton R. W., Colenso-Semple L., Phillips S. M. 2019Curr Opin Physiol. 10:90–95. doi: 10.1016/j.cophys.2019.04.006. https://doi.org/10.1016/j.cophys.2019.04.006 [DOI] [Google Scholar]
- Return to elite-level basketball after surgical reconstruction of the anterior cruciate ligament and medial collateral ligament of the knee with meniscal repairs– it takes teamwork and time to restore performance: a case report. Solie B., Kiely M., Doney C., Schwery N., Jones J., Bjerke B. 2022J Orthop Sports Phys Ther Cases. 2:1–22. doi: 10.2519/josptcases.2022.11103. [DOI] [Google Scholar]
- Arthrogenic muscle inhibition manifests in thigh musculature motor unit characteristics after anterior cruciate ligament injury. Schilaty N. D., McPherson A. L., Nagai T., Bates N. A. 2022Eur J Sports Sci. 23(5):1–11. doi: 10.1080/17461391.2022.2056520. https://doi.org/10.1080/17461391.2022.2056520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ACL rehabilitation progression: where are we now? Cavanaugh J. T., Powers M. 2017Curr Rev Musculoskel Med. 10:289–296. doi: 10.1007/s12178-017-9426-3. https://doi.org/10.1007/s12178-017-9426-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limited preoperative knee extension in anterior cruciate ligament reconstruction using a hamstring tendon affects improvement of postoperative knee extensor strength. Sengoku T., Nakase J., Mizuno Y., Kanayama T., Ishida Y., Yanatori Y., Arima Y. 2023Knee Surg Sports Traumatol Arthrosc. 31(12):5621–5628. doi: 10.1007/s00167-023-07620-8. [DOI] [PubMed] [Google Scholar]
- Terminal knee extension deficit and female sex predict poorer quadriceps strength following ACL reconstruction using all-soft tissue quadriceps tendon autografts. Hunnicutt J. L., Xerogeanes J. W., Tsai L.-C., Sprague P. A., Newsome M., Slone H. S., Lyle M. A. 2021Knee Surg Sports Traumatol Arthrosc. 29:3085–3095. doi: 10.1007/s00167-020-06351-4. [DOI] [PubMed] [Google Scholar]
- Minimum 10-year results after anterior cruciate ligament reconstruction: how the loss of normal knee motion compounds other factors related to the development of osteoarthritis after surgery. Shelbourne K. D., Gray T. 2009Am J Sports Med. 37:471–80. doi: 10.1177/0363546508326709. https://doi.org/10.1177/0363546508326709 [DOI] [PubMed] [Google Scholar]
- Preventing osteoarthritis after an anterior cruciate ligament injury: an osteoarthritis action alliance consensus statement. Driban J. B., Vincent H. K., Trojian T. H.., et al. 2023J Athl Train. 58:193–197. doi: 10.4085/1062-6050-0255.22. https://doi.org/10.4085/1062-6050-0255.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehabilitation for patients following ACL reconstruction: a knee symmetry model. Biggs A., Jenkins W., Urch S., Shelbourne D. 2009N Am J Sports Phys Ther. 4(1):2–12. [PMC free article] [PubMed] [Google Scholar]
- The influence of frequency, intensity, volume and mode of strength training on whole muscle cross-sectional area in humans. Wernbom M., Augustsson J., Thome R. 2007Sports Med. 37:225–264. doi: 10.2165/00007256-200737030-00004. https://doi.org/10.2165/00007256-200737030-00004 [DOI] [PubMed] [Google Scholar]
- The neuroplastic adaptation trident model: a suggested novel framework for ACL rehabilitation. Machan T., Krupps K. 2021Int J Sports Phys Ther. 16(3) doi: 10.26603/001c.23679. https://doi.org/10.26603/001c.23679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peak torque occurrence in the range of motion during isokinetic extension and flexion of the knee. Kannus P., Beynnon B. 1993Int J Sports Med. 14(08):422–426. doi: 10.1055/s-2007-1021203. [DOI] [PubMed] [Google Scholar]
- A motor unit-based model of muscle fatigue. Potvin J. R., Fuglevand A. J. 2017PLoS Comput Biol. 13(6) doi: 10.1371/journal.pcbi.1005581. https://doi.org/10.1371/journal.pcbi.1005581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The effectiveness of supplementing a standard rehabilitation program with superimposed neuromuscular electrical stimulation after anterior cruciate ligament reconstruction. Feil S., Newell J., Minogue C., Paessler H. H. 2011Am J Sports Med. 39(6):1238–1247. doi: 10.1177/0363546510396180. https://doi.org/10.1177/0363546510396180 [DOI] [PubMed] [Google Scholar]
- Tendon neuroplastic training: changing the way we think about tendon rehabilitation: a narrative review. Rio E., Kidgell D., Moseley G. L., Gaida J., Docking S., Purdam C., Cook J. 2016Br J Sports Med. 50(4):209–215. doi: 10.1136/bjsports-2015-095215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- A review and meta-analysis of interactive metronome training: Positive effects for motor functioning. Lee H.K., Kim H.J., Kim S.B., Kang N. 2022Percept Mot Skills. 129(5):1614–1634. doi: 10.1177/00315125221110403. https://doi.org/10.1177/00315125221110403 [DOI] [PubMed] [Google Scholar]
- Quadriceps force production during straight leg raising at different hip positions with and without concomitant ankle dorsiflexion. Mikaili S., Khademi-Kalantari K., Rezasoltani A., Arzani P., Baghban A.A. 2018J Bodyw Mov Ther. 22(4):904–908. doi: 10.1016/j.jbmt.2017.11.006. https://doi.org/10.1016/j.jbmt.2017.11.006 [DOI] [PubMed] [Google Scholar]
- Perioperative blood flow restriction rehabilitation in patients undergoing ACL reconstruction: A systematic review. Lu Y., Patel B. H., Kym C., Nwachukwu B. U., Beletksy A., Forsythe B., Chahla J. 2020Orthop J Sports Med. 8(3):232596712090682. doi: 10.1177/2325967120906822. https://doi.org/10.1177/2325967120906822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blood flow restriction training in clinical musculoskeletal rehabilitation: a systematic review and meta-analysis. Hughes L., Paton B., Rosenblatt B., Gissane C., Patterson S.D. 2017Br J Sports Med. 51(13):1003–1011. doi: 10.1136/bjsports-2016-097071. https://doi.org/10.1136/bjsports-2016-097071 [DOI] [PubMed] [Google Scholar]
- Effect of low-load blood flow restriction training after anterior cruciate ligament reconstruction: A systematic review. Koc B. B., Truyens A., Heymans M. J. L. F., Jansen E. J. P., Schotanus M. G. M. 2022Int J Sports Phys Ther. 17(3) doi: 10.26603/001c.33151. https://doi.org/10.26603/001c.33151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evaluation of muscle strength and graft laxity with early open kinetic chain exercise after ACL reconstruction: A cohort study. Forelli F., Barbar W., Kersante G.., et al. 2023Orthop J Sports Med. 11(6):23259671231177594. doi: 10.1177/23259671231177594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Who's afraid of the big bad wolf? Open-chain exercises after anterior cruciate ligament reconstruction. Noehren B., Snyder-Mackler L. 2020J Orthop Sports Phys Ther. 50(9):473–475. doi: 10.2519/jospt.2020.0609. [DOI] [PubMed] [Google Scholar]
- Biomechanical considerations for rehabilitation of the knee. McGinty G., Irrgang J. J., Pezzullo D. 2000Clin Biomech. 15(3):160–166. doi: 10.1016/s0268-0033(99)00061-3. https://doi.org/10.1016/s0268-0033(99)00061-3 [DOI] [PubMed] [Google Scholar]
- Which ROMs lead to Rome? A systematic review of the effects of range of motion on muscle hypertrophy. Kassiano W., Costa B., Nunes J. P., Ribeiro A. S., Schoenfeld B. J., Cyrino E. S. 2023J Strength Cond Res. 37(5):1135–1144. doi: 10.1519/jsc.0000000000004415. https://doi.org/10.1519/jsc.0000000000004415 [DOI] [PubMed] [Google Scholar]
- Low-load blood-flow restriction exercise to failure and nonfailure and myoelectric activity: a meta-analysis. Cerqueira M. S., Maciel D. G., Barboza J. A. M., Centner C., Lira M., Pereira R., De Brito Vieira W. H. 2022J Athl Train. 57(4):402–417. doi: 10.4085/1062-6050-0603.20. https://doi.org/10.4085/1062-6050-0603.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blood flow restriction training. Lorenz D. S., Bailey L., Wilk K. E., Mangine R. E., Head P., Grindstaff T. L., Morrison S. 2021J Athl Train. 56(9):937–944. doi: 10.4085/418-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anterior cruciate ligament strain and tensile forces for weight-bearing and non-weight-bearing exercises: a guide to exercise selection. Escamilla R. F., Macleod T. D., Wilk K. E., Paulos L., Andrews J. R. 2012J Orthop Sports Phys Ther. 42(3):209. doi: 10.2519/jospt.2012.3768. [DOI] [PubMed] [Google Scholar]
- Periodization in anterior cruciate ligament rehabilitation: new framework versus old model? a clinical commentary. Kakavas G., Forelli F., Malliaropoulos N., Hewett T.E., Tsaklis P. 2023Int J Sports Phys Ther. 18(2) doi: 10.26603/001c.73035. https://doi.org/10.26603/001c.73035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comparing the effectiveness of blood flow restriction and traditional heavy load resistance training in the post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: a UK national health service randomised controlled trial. Hughes L., Rosenblatt B., Haddad F.., et al. 2019Sports Med. 49:1787–1805. doi: 10.1007/s40279-019-01137-2. [DOI] [PubMed] [Google Scholar]
- The anabolic benefits of venous blood flow restriction training may be induced by muscle cell swelling. Loenneke J. P., Fahs C. A., Rossow L. M., Abe T., Bemben M. G. 2012Med Hypotheses. 78(1):151–154. doi: 10.1016/j.mehy.2011.10.014. https://doi.org/10.1016/j.mehy.2011.10.014 [DOI] [PubMed] [Google Scholar]
- Rehabilitation outcomes and parameters of blood flow restriction training in ACL injury: A scoping review. Caetano D., Oliveira C., Correia C., Barbosa P., Montes A., Carvalho P. 2021Phys Ther Sport. 49:129–137. doi: 10.1016/j.ptsp.2021.01.015. https://doi.org/10.1016/j.ptsp.2021.01.015 [DOI] [PubMed] [Google Scholar]
- Effects of exercise intensity and occlusion pressure after 12 weeks of resistance training with blood-flow restriction. Lixandrão M. E., Ugrinowitsch C., Laurentino G.., et al. 2015Eur J Appl Physiol. 115:2471–2480. doi: 10.1007/s00421-015-3253-2. https://doi.org/10.1007/s00421-015-3253-2 [DOI] [PubMed] [Google Scholar]
- Repetition failure occurs earlier during low-load resistance exercise with high but not low blood flow restriction pressures. Cerqueira M. S., Lira M., Mendonça Barboza J. A., Burr J. F., Wanderley e Lima T. B., Maciel D. G., De Brito Vieira W. H. 2021J Strength Cond Res. doi: 10.1519/jsc.0000000000004093. https://doi.org/10.1519/jsc.0000000000004093 [DOI] [PubMed]
- Effect of quadriceps training at different levels of blood flow restriction on quadriceps strength and thickness in the mid-term postoperative period after anterior cruciate ligament reconstruction: a randomized controlled external pilot study. Li X., Li J., Qing L., Wang H., Ma H., Huang P. 2023BMC Musculoskelet Disord. 24(1):360. doi: 10.1186/s12891-023-06483-x. https://doi.org/10.1186/s12891-023-06483-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Does stretch training induce muscle hypertrophy in humans? A review of the literature. Nunes J. P., Schoenfeld B. J., Nakamura M., Ribeiro A. S., Cunha P. M., Cyrino E. S. 2020Clin Physiol Funct Imaging. 40(3):148–156. doi: 10.1111/cpf.12622. https://doi.org/10.1111/cpf.12622 [DOI] [PubMed] [Google Scholar]
- Changes in rectus femoris architecture induced by the reverse nordic hamstring exercises. Alonso-Fernandez D., Fernandez-Rodriguez R., Abalo-Núñez R. 2018J Sports Med Phys Fitness. 59(4):640–647. doi: 10.23736/S0022-4707.18.08873-4. [DOI] [PubMed] [Google Scholar]
- Neuromuscular electrical stimulation for skeletal muscle function. Doucet B. M., Lam A., Griffin L. 2012Yale J Biol Med. 85(2):201–15. [PMC free article] [PubMed] [Google Scholar]
- Neuromuscular electrical stimulation is effective in strengthening the quadriceps muscle after anterior cruciate ligament surgery. Hauger A. V., Reiman M. P., Bjordal J. M., Sheets C., Ledbetter L., Goode A. P. 2018Knee Surg Sports Traumatol Arthrosc. 26:399–410. doi: 10.1007/s00167-017-4669-5. https://doi.org/10.1007/s00167-017-4669-5 [DOI] [PubMed] [Google Scholar]
- Knee joint loading in healthy adults during functional exercises: implications for rehabilitation guidelines. Van Rossom S., Smith C. R., Thelen D. G., Vanwanseele B., Van Assche D., Jonkers I. 2018J Orthop Sports Phys Ther. 48(3):162–173. doi: 10.2519/jospt.2018.7459. [DOI] [PubMed] [Google Scholar]
- May the force be with you: understanding how patellofemoral joint reaction force compares across different activities and physical interventions—a systematic review and meta-analysis. Hart H. F., Patterson B. E., Crossley K. M., Culvenor A. G., Khan M. C. M., King M. G., Sritharan P. 2022Br J Sports Med. 56(9):521–530. doi: 10.1136/bjsports-2021-104686. https://doi.org/10.1136/bjsports-2021-104686 [DOI] [PubMed] [Google Scholar]
- Elevating the noninvolved limb reduces knee extensor asymmetry during squat exercise in persons with reconstructed anterior cruciate ligament. Jean L. M. Y., Chiu L. Z. F. 2020J Strength Cond Res. 34(8):2120–2127. doi: 10.1519/jsc.0000000000003682. https://doi.org/10.1519/jsc.0000000000003682 [DOI] [PubMed] [Google Scholar]
- The tensile and stress relaxation responses of human patellar tendon varies with specimen cross-sectional area. Atkinson T. S., Ewers B. J., Haut R. C. 1999J Biomech. 32(9):907–914. doi: 10.1016/S0021-9290(99)00089-5. [DOI] [PubMed] [Google Scholar]
- Stress relaxation and targeted nutrition to treat patellar tendinopathy. Baar K. 2019Int J Sport Nutr Exerc Metab. 29(4):453–457. doi: 10.1123/ijsnem.2018-0231. [DOI] [PubMed] [Google Scholar]
- Optimizing an intermittent stretch paradigm using ERK1/2 phosphorylation results in increased collagen synthesis in engineered ligaments. Paxton J. Z., Hagerty P., Andrick J. J., Baar K. 2012Tissue Eng. 18(3-4):277–284. doi: 10.1089/ten.tea.2011.0336. https://doi.org/10.1089/ten.tea.2011.0336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unilateral versus bilateral exercise and the role of the bilateral force deficit. Nijem R. M., Galpin A. J. 2014Strength Cond J. 36(5):113–118. doi: 10.1519/SSC.0000000000000085. [DOI] [Google Scholar]
- Compensatory strategies that reduce knee extensor demand during a bilateral squat change from 3 to 5 months following anterior cruciate ligament reconstruction. Sigward S. M., Chan M.-S., Lin P. E., Almansouri S. Y., Pratt K. A. 2018J Orthop Sports Phys Ther. 48(9):713–718. doi: 10.2519/jospt.2018.7977. [DOI] [PubMed] [Google Scholar]
- Angle-specific analysis of knee strength deficits after ACL reconstruction with patellar and hamstring tendon autografts. Hart L. M., Izri E., King E., Daniels K. A. 2022Scand J Med Sci Sports. 32(12):1781–1790. doi: 10.1111/sms.14229. [DOI] [PubMed] [Google Scholar]
- Asymmetries in functional hop tests, lower extremity kinematics, and isokinetic strength persist 6 to 9 months following anterior cruciate ligament reconstruction. Xergia S. A., Pappas E., Zampeli F., Georgiou S., Georgoulis A. D. 2013J Orthop Sports Phys Ther. 43(3):154–162. doi: 10.2519/jospt.2013.3967. https://doi.org/10.2519/jospt.2013.3967 [DOI] [PubMed] [Google Scholar]
- Association of the single-limb hop test with isokinetic, kinematic, and kinetic asymmetries in patients after anterior cruciate ligament reconstruction. Xergia S. A., Pappas E., Georgoulis A. D. 2015Sports Health. 7(3):217–223. doi: 10.1177/1941738114529532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Interplay between body stabilisation and quadriceps muscle activation capacity. Bampouras T. M., Reeves N. D., Baltzopoulos V., Maganaris C. N. 2017J Electromyogr Kinesiol. 34:44–49. doi: 10.1016/j.jelekin.2017.03.002. [DOI] [PubMed] [Google Scholar]
- Footwear and elevated heel influence on barbell back squat: a review. Pangan A. M., Leineweber M. Sep;2021 J Biomech Engineer. 143(9) doi: 10.1115/1.4050820. https://doi.org/10.1115/1.4050820 [DOI] [PubMed] [Google Scholar]
- Effect of heel lift insoles on lower extremity muscle activation and joint work during barbell squats. Lu Z., Li X., Xuan R., Song Y., Bíró I., Liang M., Gu Y. 2022Bioengineering. 9(7):301. doi: 10.3390/bioengineering9070301. https://doi.org/10.3390/bioengineering9070301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Augmentation of bone tunnel healing in anterior cruciate ligament grafts: application of calcium phosphates and other materials. Baxter F. R., Bach J. S., Detrez F., Cantournet S., Corté L., Cherkaoui M., Ku D. N. 2010J Tissue Eng. 1(1):712370. doi: 10.4061/2010/712370. https://doi.org/10.4061/2010/712370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tendon healing in bone tunnel after human anterior cruciate ligament reconstruction: A systematic review of histological results. Lu H., Chen C., Xie S., Tang Y., Qu J. 2019J Knee Surg. 32(05):454–462. doi: 10.1055/s-0038-1653964. https://doi.org/10.1055/s-0038-1653964 [DOI] [PubMed] [Google Scholar]
- Tendon and ligament regeneration and repair: Clinical relevance and developmental paradigm. Yang G., Rothrauff B. B., Tuan R. S. 2013Birth Defects Res C Embryo Today. 99(3):203–222. doi: 10.1002/bdrc.21041. https://doi.org/10.1002/bdrc.21041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Histological and biomechanical observations of the rabbit patellar tendon after removal of its central one-third. Miyashita H., Ochi M., Ikuta Y. 1997Arch Orthop Trauma Surg. 116:454–462. doi: 10.1007/bf00387577. https://doi.org/10.1007/bf00387577 [DOI] [PubMed] [Google Scholar]
- Interrater reliability of a clinical scale to assess knee joint effusion. Sturgill L. P., Snyder-Mackler L., Manal T. J., Axe M. J. 2009J Orthop Sports Phys Ther. 39(12):845–849. doi: 10.2519/jospt.2009.3143. https://doi.org/10.2519/jospt.2009.3143 [DOI] [PubMed] [Google Scholar]
- Continued sports activity, using a pain-monitoring model, during rehabilitation in patients with Achilles tendinopathy. Silbernagel K. G., Thomeé R., Eriksson B. I., Karlsson J. 2007Am J Sports Med. 35(6):897–906. doi: 10.1177/0363546506298279. https://doi.org/10.1177/0363546506298279 [DOI] [PubMed] [Google Scholar]
- Early accelerated versus delayed conservative rehabilitation protocol after anterior cruciate ligament reconstruction: a prospective randomized trial. Patra S.K., Narayan Nanda S., Prasad Patro B., Kumar Sahu N., Ranjan Mohnaty C., Jain M. 2022Revista Brasileira de Ortopedia. 57:429–436. doi: 10.1055/s-0042-1748970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reduced neural drive in bilateral exertions: a performance-limiting factor? Van Dieën J. H., Ogita F., De Haan A. 2003Med Sci Sports Exerc. 35(1):111–118. doi: 10.1097/00005768-200301000-00018. [DOI] [PubMed] [Google Scholar]
- Muscle activation in unilateral and bilateral efforts assessed by motor nerve and cortical stimulation. Herbert R., Gandevia S. 1996J Appl Physiol. 80(4):1351–1356. doi: 10.1152/jappl.1996.80.4.1351. [DOI] [PubMed] [Google Scholar]
- A brief review on the effects of the squat exercise on lower-limb muscle hypertrophy. Ribeiro A. S., Santos E. D., Nunes J. P., Nascimento M. A., Graça Á., Bezerra E. S., Mayhew J. L. 2023Strength Cond J. 45(1):58–66. doi: 10.1519/ssc.0000000000000709. https://doi.org/10.1519/ssc.0000000000000709 [DOI] [Google Scholar]
- Lower patellofemoral joint contact force during side-step cutting after return-to-sports clearance following anterior cruciate ligament reconstruction. San Jose A. J., Maniar N., Whiteley R., Opar D. A., Timmins R. G., Kotsifaki R. 2023Am J Sports Med. 51(7):1777–1784. doi: 10.1177/03635465231166104. https://doi.org/10.1177/03635465231166104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patellofemoral joint kinetics in females when using different depths and loads during the barbell back squat. Zavala L., Flores V., Cotter J. A., Becker J. 2021Eur J Sports Sci. 21(7):976–984. doi: 10.1080/17461391.2020.1806935. https://doi.org/10.1080/17461391.2020.1806935 [DOI] [PubMed] [Google Scholar]
- Maximal isometric patellofemoral contact force in patients with anterior knee pain. Macdonald D., Hutton J., Kelly I. 1989Bone Joint J. 71-B(2):296–299. doi: 10.1302/0301-620x.71b2.2925750. https://doi.org/10.1302/0301-620x.71b2.2925750 [DOI] [PubMed] [Google Scholar]
- Changes in quadriceps rate of torque development after anterior cruciate ligament reconstruction and association to single-leg hop distance. Tayfur B., Johnson A.K., Palmieri-Smith R. 2023Sports Health. 16(5):808–816. doi: 10.1177/19417381231205295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contractile rate of force development after anterior cruciate ligament reconstruction—a comprehensive review and meta-analysis. Turpeinen J. T., Freitas T. T., Rubio-Arias J. Á., Jordan M. J., Aagaard P. 2020Scand J Med Sci Sports. 30(9):1572–1585. doi: 10.1111/sms.13733. https://doi.org/10.1111/sms.13733 [DOI] [PubMed] [Google Scholar]
- The effects of plyometric training on change-of-direction ability: a meta-analysis. Asadi A., Arazi H., Young W. B., de Villarreal E. S. 2016Int J Sports Physiol Perform. 11(5):563–573. doi: 10.1123/ijspp.2015-0694. https://doi.org/10.1123/ijspp.2015-0694 [DOI] [PubMed] [Google Scholar]
- The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Myer G. D., Ford K. R., McLean S. G., Hewett T. E. 2006Am J Sports Med. 34(3):445–455. doi: 10.1177/0363546505281241. https://doi.org/10.1177/0363546505281241 [DOI] [PubMed] [Google Scholar]
- Recommendations for plyometric training after ACL reconstruction – a clinical commentary. Buckthorpe M., Della Villa F. 2021Int J Sports Phys Ther. 16(3) doi: 10.26603/001c.23549. https://doi.org/10.26603/001c.23549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Secondary anterior cruciate ligament injury prevention training in athletes: what is the missing link? Wong C.-Y., Mok K.-M., Yung S.-H. 2023Int J Environ Res Public Health. 20(6):4821. doi: 10.3390/ijerph20064821. https://doi.org/10.3390/ijerph20064821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The validity and reliability of commercially available resistance training monitoring devices: a systematic review. Weakley J., Morrison M., García-Ramos A., Johnston R., James L., Cole M. H. 2021Sports Med. 51:443–502. doi: 10.1007/s40279-020-01382-w. https://doi.org/10.1007/s40279-020-01382-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velocity-based training: from theory to application. Weakley J., Mann B., Banyard H., McLaren S., Scott T., Garcia-Ramos A. 2021Strength Cond J. 43(2):31–49. doi: 10.1519/ssc.0000000000000560. https://doi.org/10.1519/ssc.0000000000000560 [DOI] [Google Scholar]
- Impaired stretch-shortening cycle function persists despite improvements in reactive strength after anterior cruciate ligament reconstruction. Read P. J., Pedley J. S., Eirug I., Sideris V., Oliver J. L. 2022J Strength Cond Res. 36(5):1238–1244. doi: 10.1519/jsc.0000000000004208. https://doi.org/10.1519/jsc.0000000000004208 [DOI] [PubMed] [Google Scholar]
- Recommendations for movement re-training after ACL reconstruction. Buckthorpe M. 2021Sports Med. 51(8):1601–1618. doi: 10.1007/s40279-021-01454-5. https://doi.org/10.1007/s40279-021-01454-5 [DOI] [PubMed] [Google Scholar]
- Interlimb and intralimb coordination of rectus femoris and biceps femoris muscles at different running speeds. Kakehata G., Goto Y., Yokoyama H., Iso S., Kanosue K. 2023Med Sci Sports Exerc. 55:945–956. doi: 10.1249/mss.0000000000003106. https://doi.org/10.1249/mss.0000000000003106 [DOI] [PubMed] [Google Scholar]
- Metabolic and muscle damage profiles of concentric versus repeated eccentric cycling. Penailillo L., Blazevich A., Numazawa H., Nosaka K. 2013Med Sci Sports Exerc. 45(9):1773–1781. doi: 10.1249/MSS.0b013e31828f8a73. https://doi.org/10.1249/MSS.0b013e31828f8a73 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.