Abstract
To identify sites in gp120 that interact with the CCR5 coreceptor and to analyze the mechanisms of infection, we selected variants of the CCR5-dependent JRCSF molecular clone of human immunodeficiency virus type 1 (HIV-1) that adapted to replicate in HeLa-CD4 cells that express the mutant coreceptor CCR5(Y14N) or CCR5(G163R), which were previously shown to bind purified gp120-CD4 complexes only weakly. Correspondingly, these mutant CCR5s mediate infections of wild-type virus only at relatively high cell surface concentrations, demonstrating a concentration-dependent assembly requirement for infection. The plots of viral infectivity versus concentration of coreceptors had sigmoidal shapes, implying involvement of multiple coreceptors, with an estimated stoichiometry of four to six CCR5s in the active complexes. All of the adapted viruses had mutations in the V3 loops of their gp120s. The titers of recombinant HIV-1 virions with these V3 mutations were determined in previously described panels of HeLa-CD4 cell clones that express discrete amounts of CCR5(Y14N) or CCR5(G163R). The V3 loop mutations did not alter viral utilization of wild-type CCR5, but they specifically enhanced utilization of the mutant CCR5s by two distinct mechanisms. Several mutant envelope glycoproteins were highly fusogenic in syncytium assays, and these all increased the efficiency of infection of the CCR5(Y14N) or CCR5(G163R) clonal panels without enhancing virus adsorption onto the cells or viral affinity for the coreceptor. In contrast, V3 loop mutation N300Y was selected during virus replication in cells that contained only a trace of CCR5(Y14N) and this mutation increased the apparent affinity of the virus for this coreceptor, as indicated by a shift in the sigmoid-shaped infectivity curve toward lower concentrations. Surprisingly, N300Y increased viral affinity for the second extracellular loop of CCR5(Y14N) rather than for the mutated amino terminus. Indeed, the resulting virus was able to use a mutant CCR5 that lacks 16 amino acids at its amino terminus, a region previously considered essential for CCR5 coreceptor function. Our results demonstrate that the role of CCR5 in infection involves at least two steps that can be strongly and differentially altered by mutations in either CCR5 or the V3 loop of gp120: a concentration-dependent binding step that assembles a critical multivalent virus-coreceptor complex and a postassembly step that likely involves a structural rearrangement of the complex. The postassembly step can severely limit HIV-1 infections and is not an automatic consequence of virus-coreceptor binding, as was previously assumed. These results have important implications for our understanding of the mechanism of HIV-1 infection and the factors that may select for fusogenic gp120 variants during AIDS progression.
Sequential binding of human immunodeficiency virus (HIV-1) surface glycoprotein gp120 to CD4 and coreceptors initiates HIV-1 infection. CD4 attachment induces a conformational change in gp120 that exposes a coreceptor binding domain (34, 55, 63, 66, 67). Subsequent interaction with the coreceptor induces further structural rearrangements that expose a fusion peptide of transmembrane glycoprotein gp41, pulls the virus closer to the cell surface, and allows subsequent fusion of viral and cellular membranes (7, 34, 35, 65). HIV-1 coreceptors are a family of seven transmembrane G protein-coupled receptors that are activated by chemotactic cytokines (chemokines) (1, 4, 9, 14, 16, 17, 24). Viruses (termed R5) that use the CCR5 coreceptor are transmitted between individuals and generally persist throughout disease (13, 37, 54, 57), whereas viruses able to use CXCR4 (termed X4) accumulate in the late stages of disease progression in some patients (10, 59). Similarly, R5 viruses evolve throughout disease progression and eventually may become more active in causing depletion of CD4-positive T cells (31, 60). Recent studies of macaques infected with cloned viral variants have implied that fusogenicity of the envelope glycoprotein is a critical determinant for rapid progression to AIDS (19, 20). However, the host and viral factors that control the fusogenic and pathogenic properties of HIV-1 envelope glycoproteins are poorly understood.
Mutagenesis and biochemical studies have implied that the highly acidic and tyrosine-rich amino-terminal region of CCR5 plays a crucial role in infections by R5 strains of HIV-1 (18, 21, 22, 33, 52, 56). Tyrosine residues at positions 3, 10, 14, and 15 contribute substantially to coreceptor activity, with Y14 and Y15 being especially important (18, 32, 33). Interestingly, these tyrosines are all modified by sulfation during processing of HIV-1 glycoproteins and this posttranslational modification is essential for gp120 binding to CCR5 and for infections (11, 22, 23). However, other extracellular regions of CCR5 also contribute to coreceptor function. Polyclonal and monoclonal antibodies targeted to the CCR5 amino terminus inhibit gp120 binding but not infection, while monoclonal antibodies recognizing CCR5 extracellular loop 2 (ECL2) have minimal effects on gp120 binding but strongly inhibit infection (36, 44). We previously described evidence that amino acid G163 in the TM4-ECL2 junction of CCR5 is critically important for gp120 binding and for HIV-1 infections (61). African green monkeys contain a G163R substitution in CCR5 that inhibits HIV-1 binding and utilization of that coreceptor but has no inhibitory effect on endemic infections by simian immunodeficiency viruses or on chemokine-mediated signal transduction (61). Similarly, a Y14N substitution polymorphism is prevalent in African green monkeys and it also severely inhibits gp120 binding and coreceptor activity without preventing chemokine binding or signaling (32, 33). Indeed, HIV-1 infections of cells that express human CCR5(Y14N) are only approximately 1.5% as efficient as infections mediated by wild-type CCR5 (32). Studies using chimeric CCR5 proteins were also compatible with the above conclusions (2, 5, 33, 47, 56). Considered together, these results suggest that HIV-1 gp120 binds to several regions of CCR5 and that all of these interactions contribute to infection.
Recent crystallographic studies have elucidated the structure of a radically modified (variable loops and glycosyl residues removed) gp120 molecule in a ternary complex with an N-terminal CD4 fragment and the Fab fragment of monoclonal antibody 17b that binds to a CD4-induced epitope (34). These studies, combined with gp120 mutagenesis, suggest that several variable loops (V1/V2 stem and V3 base), along with conserved region 4 (C4), form a coreceptor binding template (34, 55). The V3 loop contributes to coreceptor binding and is a critical determinant of coreceptor choice (9, 62, 63, 66).
In this study, we sought to more precisely identify critical factors that control HIV-1 interactions with CCR5. We reasoned that passage of a wild-type R5 isolate in HeLa-CD4 cells that express severely attenuated mutant forms of CCR5 might select viruses with adaptive mutations in gp120. Consequently, we passaged the molecularly cloned JRCSF isolate of HIV-1 in cells expressing the well-characterized mutant coreceptors CCR5(Y14N) and CCR5(G163R), which bind gp120 only weakly (32, 33, 61). Interestingly, the adapted viruses all had mutations in their V3 loops. Unexpectedly, most of these V3 loop mutations did not appear to increase HIV-1 affinity for the mutant coreceptors. Rather, they enhanced the efficiency with which the assembled virus-coreceptor complexes functioned in the downstream membrane fusion step of infection. Our results suggest that specific interactions of R5 HIV-1 and CCR5 are critical not only for assembly of a multivalent complex necessary for infection but also for a subsequent step, presumably a conformational change that is a prerequisite for fusion of the viral and cellular membranes. The assembly step is limiting when the coreceptor concentration is low, whereas the postassembly step becomes severely limiting at high saturating concentrations of the mutant coreceptors. Accordingly, the types of viral adaptive mutations that we obtained depended on the concentrations of the mutant coreceptors in the cells used for the selection. These results demonstrate a critical need for analyses of coreceptor concentrations in studies designed to explain their functions in HIV-1 infection and pathogenesis.
MATERIALS AND METHODS
Cells, viruses, and plasmids.
Panels of HeLa-CD4 cells expressing various amounts of CCR5 with either the Y14N or the G163R mutation were generated, characterized, and maintained as previously described (32, 50). H1-J, JC.53, COS7, and 293T cells were maintained as previously described (32, 49, 50).
R5 HIV-1 isolate JRCSF was grown from an infectious molecular clone, pYK-JRCSF, that had been obtained from the AIDS Research and Reference Reagent Program, Division of AIDS, National Institute of Allergy and Infectious Diseases, National Institutes of Health, and was contributed by Irvin Chen and Yoshio Koyanagi. We generated high-titer JRCFS stocks by transfecting HeLa cells, harvesting virus at the time of peak production, and then expanding this virus in HeLa-CD4/CCR5 cell cultures for 2 to 3 days. Pseudotyped HIV-gpt viruses bearing wild-type or mutant JRCSF envelopes were produced as previously described (27, 49). The pSVIIIenv expression vector (generously provided by J. Sodroski, Dana-Farber Cancer Institute, Boston, Mass.) was used to generate control HIV-gpt virions pseudotyped with the X4 LAV/IIIB envelope. The pcDNA3.0-CCR5 vector has been described previously (33). Retroviral vectors encoding CCR5s with amino-terminal deletions were constructed by ligating the BamHI/XhoI fragments from the pcDNA3.0 expression vectors into pSFF (27, 32, 33, 50) digested with the same enzymes. Retroviral vectors encoding wild-type CCR5 and CCR5(Y14N) were created and used to make virus stocks for gene transduction as previously described (33, 50).
Adaptation of JRCSF HIV-1 isolate for vigorous growth on HeLa-CD4 cells expressing mutant coreceptors.
We adapted JRCSF to grow on cells expressing defective CCR5(Y14N) or CCR5(G163R) (32, 33, 61). In order to establish an infection, we repeatedly (three or four times for 12 h each) exposed cells, seeded 24 h previously at 5 × 105 cells per filter-capped T-75 flask, to 1 × 106 focusing-forming units of virus. Every 4 to 5 days, we harvested and filtered conditioned medium that was then used to infect a fresh culture of cells expressing defective CCR5. Virus aliquots were also reserved for titer determination on cells expressing wild-type and mutant CCR5s. Initially, we observed little cytopathic effect; however, within 8 to 10 passages, we observed the formation of large syncytia. Determination of the virus titer at this stage revealed an increase in infectivity in cells expressing mutant coreceptors. We continued passaging in cells with virus-containing medium that was diluted 10-fold in order to limit propagation of defective proviruses. Since the Y14N mutation was more crippling for CCR5 coreceptor function, yielding 1.5% of wild-type activity at high expression levels, we initially passaged high-titer JRCSF virus in cell clone YB8, which expresses a large amount of cell surface CCR5(Y14N) (1.7 × 105 molecules/cell) (32). The resulting adapted virus was then secondarily passaged in cell clone JYN.4, which express a relatively small amount of CCR5(Y14N) (i.e., 6.0 × 104 molecules/cell) (32). Since the CCR5(G163R) mutation had a less deleterious effect on infection, we used cells expressing a small amount of CCR5(G163R) (clone JGR.H4 [1.9 × 104 molecules/cell]) to generate G163R-adapted variants of JRCSF (32).
Cloning, sequencing, and expression of envelope genes from adapted viruses.
Envelope clones were obtained from cells infected with an adapted virus population by isolating genomic DNA (Easy-DNA Kit; Invitrogen, Carlsbad, Calif.) and PCR amplifying the envelope genes. This step was performed only after we had obtained a virus population that caused cytopathic effects and that had substantial titers in cells expressing mutant coreceptors. PCR was performed with cloned Pfu polymerase (Stratagene, La Jolla, Calif.) in accordance with the manufacturer's instructions. Reactions were performed as previously described (33). The primers used to amplify envelope sequences were as follows: forward, 5′ CCGGAATTCACAGTGGCAATGAGAGTG 3′; reverse, 5′ GCTCTAGAGCCACCCATCTTATAGCAAAGC 3′. The start and stop codons and EcoRI and XbaI restriction endonuclease sites are underlined. The 2.5-kb PCR fragments were digested with EcoRI/XbaI and ligated into pBluescript II(KS+) (Stratagene) that had been digested with the same enzymes. Entire envelope genes were sequenced by fluorescent DNA sequence determination, performed by the Microbiology and Molecular Immunology Core Facility at the Oregon Health Sciences University on a PE/ABD 377 DNA sequencer using dye terminator cycle chemistry (PE Applied Biosystems, Foster City, Calif.). For sequencing, we used the M13 universal (−20) and M13 reverse (United States Biochemical Corporation, Cleveland, Ohio) primers, which anneal to the vector 3′ and 5′, respectively, of the insert. Internal sequences were obtained with primers 6660 (5′ TGAGGGAATGATGGAGAG 3′), 7090 (5′ CAGCTGAATGAATCTGTA 3′), 7690 (5′ TGAACCATTAGGAGTAGC 3′), and 8083 (5′ AACATGACCTGGATGGAG 3′).
Wild-type and mutant envelope sequences created by site-directed mutagenesis (see below) were cloned into the pcDNA3.0 expression vector by using the EcoRI and XbaI sites described above. To obtain efficient envelope expression, we introduced exon I of the rev gene in cis into these expression vectors by ligating a 593-bp HindIII fragment from the JRenv plasmid (described below) into these vectors digested with the same enzyme. JRenv was constructed by PCR amplifying rev exon I and the entire wild-type envelope gene from pYK-JRCSF with primers rev 5′ (5′ CCGGAATTCATCTCCTATGGCAGGAAGAAGCGGA 3′) and 3′ envX (5′ TTCCAGGTCTCGAGATACTGCTCC 3′). The primers encompass the initiation codon in rev exon I and the XhoI site 3′ to the envelope termination codon. The rev start codon and EcoRI and XhoI restriction endonuclease sites are underlined. The 2.9-kb PCR product was ligated into the pPCR-ScriptAmp (Stratagene) vector in accordance with the manufacturer's recommendations. This plasmid was amplified in Escherichia coli, and the rev/env-containing fragment was excised by EcoRI/XhoI digestion and ligated into pcDNA3.0 digested with the same enzymes to generate the JRenv plasmid.
Mutagenesis was performed with the QuickChange (Stratagene) site-directed mutagenesis kit in accordance with the manufacturer's instructions. Templates for mutagenesis were prepared by ligating the BamHI fragments of the pcDNA3.0 rev-containing vectors encoding either wild-type JRCSF or mutant S298N into the BamHI site of pBluescript II(KS+). Primers used for env mutagenesis were the following: (i) F313L mutation, forward (F313L FWD; 5′ GGGAGAGCATTGTATACAACAGGAG 3′) and reverse (F313L REV; 5′ CTCCTGTTGTATACAATGCTCTCCC 3′); (ii) N300Y mutation, forward (NY FWD; 5′ GGCCCAGCAACTATACAAGAAAAAG 3′) and reverse (NY REV; 5′ CTTTTTCTTGTATAGTTGCTGGGCC 3′); (iii) S298N and N300Y mutations, forward (SNNY FWD; 5′ GGCCCAACAACTATACAAGAAAAAG 3′) and reverse (SNNY REV; 5′ CTTTTTCTTGTATAGTTGTTGGGCC 3′); (iv) F313L and N300Y mutations, primers from set ii (used to amplify from the F313L mutant env template); (v) S298N and F313L mutations, primers from set i (used to amplify from the S298N mutant env template); (vi) S298N, N300Y, and F313L mutations, primers from set i (used to amplify from the S298N and N300Y mutations). Underlined bases denote the point mutations created to generate the mutant envelopes. The regions of the plasmids encoding the mutant BamHI env fragments were sequenced in their entirety and then excised with BamHI and cloned back into the pcDNA3.0-rev/env expression vectors that had been digested with the same enzyme.
CCR5 mutagenesis.
By using PCR mutagenesis and the following mutagenic primers, we generated amino-terminal deletions of CCR5 lacking either 16 or 18 amino acids: forward, R5d16 FWD (5′ GGGGATCCGGTGGAACAAGATGGAGCCCTGCCAAAAAAT 3′) and R5d18 FWD (5′ GGGGATCCGGTGGAACAAGATGTGCCAAAAAATCAATGTG 3′). Initiator codons for methionine are underlined, as are the BamHI restriction enzyme sites. The codons for the 18th and 20th CCR5 amino-terminal amino acids are in bold. We used reverse primer R5R1 (5′ GGCCAAAGAATTCCTGGAAGGT 3′), which encompassed the unique EcoRI site in CCR5 (underlined). We used our pcDNA3.0-CCR5 plasmid as a template (33). The approximately 0.8-kb PCR fragments were digested with BamHI/EcoRI and ligated into pCDNA3.0-CCR5 digested with the same enzymes. N-terminal deletion mutations of CCR5 were verified by sequencing.
Infectivity assays.
We generated infectious, replication-defective HIV-gpt virions bearing wild-type or mutant JRCSF envelopes by cotransfecting COS-7 cells (27, 49) with the pHIV-gpt plasmid (45, 46) and pcDNA3.0 rev/env expression vectors that encoded either wild-type JRCSF env or a single env mutation (S298N, F313L, F313I, or N300Y), a double env mutation (S298N and N300Y, N300Y and F313L, or S298N and F313L), or a triple env mutation (S298N, N300Y, and F313L). Virus was harvested 48 h posttransfection and used to infect panels of HeLa-CD4 cells expressing discrete, various amounts of CCR5(Y14N) or CCR5(G163R). Each clone from the cell panels was seeded in duplicate wells of six-well plates at 5 × 104 cells/well 24 h before infection. Cells were treated with 8 μg of Polybrene per ml for 20 min prior to infection and then washed, and 1 ml of virus was added to each duplicate well either undiluted or at a 1:10 dilution in complete medium (Dulbecco's modified Eagle's medium with 10% fetal bovine serum). The cells and virus were incubated overnight (14 to 16 h). On the following morning, the virus was aspirated and the cells were fed with complete medium. At 24 h later, the complete medium was aspirated and selective medium was added to the cells (27, 49). After 8 days of selection, colonies that grew were fixed, stained, and counted.
Soluble CD4 (sCD4) inactivation studies were carried out on pseudotyped HIV-gpt virions by performing infectivity assays as described above in the absence or presence of various concentrations of sCD4 (NEN Life Science Products, Boston, Mass.). Viruses were incubated with sCD4 for 30 min before addition to cells. We used JC.53 cells that express large amounts of CD4 and wild-type CCR5 as target cells (50).
CCR5s with amino-terminal deletions were tested for coreceptor activity by transduction of HI-J cells with retroviral vectors encoding wild-type CCR5, CCR5(Y14N), CCR5(R5d16), or CCR5(R5d18) as previously described (30, 50). Transduced populations of cells were infected with pseudotyped viruses. At 48 h after infection, cells were placed in selective medium. Resistant colonies were fixed, stained, and counted.
Fusion assays.
293T cells were transfected with plasmids encoding wild-type and mutant JRCSF envelope genes with PolyFect (Qiagen, Valencia, Calif.) in accordance with the manufacturer's instructions. After 48 h, transfected cells were harvested with quick-lift (0.9% NaCl, 8 mM EDTA) and 7.5 × 102 cells were seeded onto 48-well dishes containing confluent monolayers of HeLa-CD4 cells expressing wild-type CCR5 (JC.53 cells with 1.9 × 105 molecules/cell), CCR5(Y14N) (YB8 and JYN.4 cells with 1.7 × 105 and 6 × 104 molecules/cell, respectively), or CCR5(G163R) (JGR.H4 cells with 1.9 × 104 molecules/cell). The cocultures were incubated for 6 h, fixed, and stained (0.1% toluidine blue in 30% ethanol), and the number of syncytia per well was determined.
Immunoprecipitation-Western blot analysis of HIV-1 proteins.
Harvesting of samples and immunoprecipitation-Western blot analysis were performed as previously described (49).
RESULTS
Selection of JRCSF variants by forced passages in cells that express mutant CCR5s.
Initially, as outlined in Fig. 1, we passaged molecularly cloned R5 HIV-1 isolate JRCSF in a HeLa-CD4 cell clone (YB8) that constitutively expresses a large amount of CCR5(Y14N) (1.7 × 105 molecules per cell) (32). For the first few passages, a very low level of virus replication was evidenced by the occasional appearance of syncytia. In contrast, at passage 8, large syncytia with numerous nuclei rapidly formed. Subsequent studies confirmed that this adapted virus was much more infectious than the parental JRCSF virus for cells that express the CCR5(Y14N) coreceptor. Cloning and sequencing of envelope genes from this adapted virus population revealed that all of the cloned envelopes had mutations in the V3 loop (Table 1). In contrast, JRCSF virus grown for 12 passages in cells expressing wild-type CCR5 had no V3 mutations (data not shown). The envelopes of the adapted viruses had mutations of residue S298 to N, although one clone also had the F313L mutation (Table 1). Single clones with V3 mutations also had additional mutations of F173S and T295I in gp120 and mutations of R525A, A809T, and T818I in gp41. None of the latter mutations appeared to correlate with adaptation to CCR5(Y14N) use, since they were not propagated upon further passage of the virus population in cells expressing low levels of CCR5(Y14N) (see below). Additional mutations within gp41 included one clone that had an 11-residue in-frame deletion of amino acids 822 to 832, while many clones had a mutation of T769I. Preliminary studies indicated that neither of these mutations enhanced infectivity in CCR5(Y14N)-expressing cells.
FIG. 1.
Schematic diagram of adapted HIV-1 JRCSF virus production by passage in cells expressing mutant coreceptors. High-titer HIV-1 JRCSF was propagated on HeLa-CD4 cells expressing either CCR5(Y14N) or CCR5(G163R), and the envelope genes of emergent variants were cloned and sequenced as described in Materials and Methods.
TABLE 1.
V3 loop sequences of adapted HIV-1JRCSFa
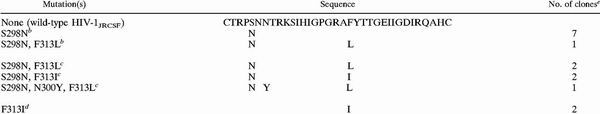 |
Envelope sequences were obtained as described in Materials and Methods. The V3 loop sequences are shown.
Adaptation on high CCR5(Y14N) expressing HeLa-CD4 cells. The mutant coreceptor concentration was 1.7 × 105 CCR5(Y14N) molecules/cell.
Adaptation on low CCR5 (Y14N) expressing HeLa-CD4 cells. The mutant coreceptor concentration was 6.0 × 104 CCR5(Y14N) molecules/cell.
Adaptation on low CCR5(G163R) expressing HeLa-CD4 cells. The mutant coreceptor concentration was 1.9 × 104 CCR5(G163R) molecules/cell.
The numbers of clones with specific mutations per total envelopes cloned are shown. Total envelopes cloned: nine on high CCR5(Y14N) expressing cells [a clone not shown had a T295I mutation that did not correlate with CCR5(Y14N) adaptation], five on low CCR5(Y14N) expressing cells, and three on high-expressing JGR H4-cells (a clone not shown had a premature termination codon in the V3 loop.)
We then applied more stringent conditions in a subsequent selection by passaging the initially adapted virus population described above in HeLa-CD4 cells (clone JYN.4) that contained a much smaller amount of CCR5(Y14N) (i.e., 6 × 104 molecules per cell) (32). Initially, the JYN.4 cells were poorly infected but after approximately six passages, rapid and extensive cytopathic effects became evident. This secondarily adapted virus population had a substantially increased infectivity for cells that expressed CCR5(Y14N). Cloning and sequencing of envelope genes from the secondary selection revealed an additional mutation of N300Y in the V3 loop (Table 1). Single clones with V3 mutations had additional changes of K32E and I162K in gp120 and E654K and A809V in gp41.
Similarly, we passaged the JRCSF virus in HeLa-CD4 cells (JGR.H4 clone) that express a small amount of CCR5(G163R) (1.9 × 104 molecules per cell) (32). In this case, the adapted variants had one V3 loop change of F313I (Table 1).
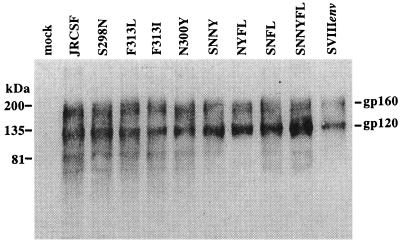
To analyze the biological effects of each envelope mutation or combination of mutations, we constructed the mutant envelopes indicated in Table 2. We then cloned the wild-type and mutant JRCSF envelopes into the pcDNA3.0 expression vector along with coding sequences for rev and analyzed their functions. Western blotting of cell extracts from transfected COS-7 cells demonstrated that the wild-type and mutant envelope glycoproteins were well expressed and processed normally (Fig. 2).
TABLE 2.
HIV-1JRCSF envelope constructs and their infectivity characteristics
| Envelope designation | Mutation(s) | Derivation | Maximum irela
|
Fold increaseb
|
||
|---|---|---|---|---|---|---|
| Y14N | G163R | Y14N | G163R | |||
| JRCSF | None | NAe | 0.015 | 0.20 | NA | NA |
| S298N | S298N | Adaptationc | 0.10 | 0.24 | 7 | 1.2 |
| F313L | F313L | Mutagenesisd | 0.10 | 0.24 | 7 | 1.2 |
| F313I | F313I | Adaptation | 0.075 | 0.50 | 5 | 2.5 |
| N300Y | N300Y | Mutagenesis | 0.04 | NDf | 3 | ND |
| SNFL | S298N, F313L | Adaptation | 0.34 | 0.65 | 23 | 3 |
| SNNY | S298N, N300Y | Mutagenesis | 0.20 | ND | 13 | ND |
| NYFL | N300Y, F313L | Mutagenesis | 0.30 | ND | 20 | ND |
| SNNYFL | S298N, N300Y, F313L | Adaptation | 0.60 | ND | 40 | ND |
Maximum irel was determined by dividing the maximum titer of each mutant virus in the clonal panel expressing CCR5(Y14N) or CCR5(G163R) by its titer in cells expressing an optimum quantity of wild-type CCR5. Thus, it is the asymptote on the irel axis of each curve in Fig. 3.
Fold increase refers to the increase in the maximum irel. It was determined by dividing the maximum irel of each mutant virus by that of wild-type HIV-1JRCSF.
Adapted envelopes were cloned and sequenced as described in Materials and Methods.
Mutant envelopes were constructed as described in Materials and Methods.
NA, not applicable.
ND, not determined, since these clones had titers below the limit of detection in CCR5(G163R)-expressing cells.
FIG. 2.
Immunoprecipitation-Western blot analysis of wild-type and mutant JRCSF envelope proteins. Cell extracts were harvested from transfected COS-7 cells and subjected to immunoprecipitation-Western blot analysis as described previously (49). Mock-transfected cell extract and well-characterized SVIIIenv were included as negative and positive controls, respectively. Mutant envelope nomenclature is defined in Table 2.
Effects of adaptive V3 loop mutations on infections of HeLa-CD4 cell clones that express discrete amounts of CCR5(Y14N).
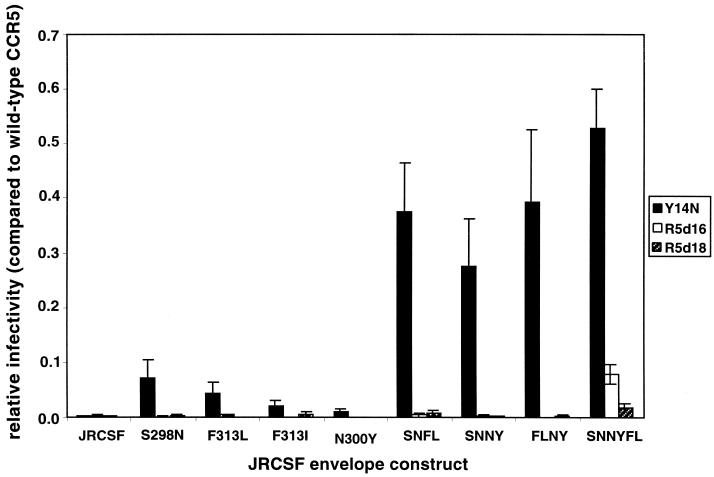
We used HIV-gpt virions pseudotyped with each of the wild-type and mutant envelope glycoproteins indicated in Table 2 to infect previously described panels of HeLa-CD4 cell clones that express a constant large amount of CD4 (i.e., 1.5 × 105 molecules of CD4/cell) and various discrete amounts of the mutant coreceptor CCR5(Y14N) or CCR5(G163R) (32, 48). Pseudotyped viruses were prepared by cotransfecting COS-7 cells with each envelope expression vector in the presence of the pHIV-gpt plasmid (27). Interestingly, the pseudotyped viruses that were prepared in parallel had equal titers within experimental error when assayed in the JC.53 clone of HeLa-CD4 cells, which expresses the same amount of CD4 as the clonal panels and a large optimal concentration of wild-type CCR5 (i.e., 1.9 × 105 molecules of CCR5/cell [32, 50]), whereas the titers were all zero in control HeLa-CD4 cells that lack CCR5 and in HeLa cells that contain CCR5 but not CD4 (data not shown). These results were consistent with the idea that the adaptive mutations in gp120 did not significantly alter the yields or infectivities of the pseudotyped viruses or modify their binding to the cells or their abilities to utilize wild-type CCR5. Furthermore, previous evidence has shown that HIV-1 adsorption onto HeLa-CD4 cells is independent of the presence or quantity of CCR5 (29, 41). This was expected because the binding sites for CCR5 are only exposed following HIV-1 adsorption onto cells and association with CD4 (34, 55, 63, 66, 67). Therefore, we concluded that the pseudotyped viruses adsorbed equally onto the surfaces of the cells used in this investigation. In contrast to the above-described results, pseudotyped viruses that were produced on different occasions had distinct titers, presumably because the COS-7 cell concentrations and transfection conditions were somewhat variable. Consequently, for comparisons of different preparations of the same virus and for standardization of results of multiple assays, it was necessary to normalize the titer of each virus preparation relative to its titer in optimal JC.53 cells. These relative infectivity (irel) values are plotted versus the concentrations of CCR5(Y14N) and CCR5(G163R) in Fig. 3.
FIG. 3.
HIV-1 infections mediated by mutant CCR5 coreceptors. (A and B) Infection of the CCR5(Y14N) clonal panel by pseudotyped HIV-gpt virions bearing the wild-type envelope or the mutant JRCSF envelopes described in Table 2. Infections were performed and quantitated as described in Materials and Methods. Relative infectivities were determined by dividing the titer measured on a given cell clone by the titer determined on a HeLa-CD4 clone expressing high levels of wild-type CCR5 (clone JC.53). (C and D) Infection of the CCR5(G163R) clonal panel by the same pseudotyped viruses as in panels A and B. Data points represent means of four independent assays, and error bars represent the standard error of the mean. The CCR5(Y14N) and CCR5(G163R) clonal panels were described previously (32).
As expected, the cell clones that express CCR5(Y14N) or CCR5(G163R) were much less susceptible to infection than the JC.53 cells that express an optimal quantity of wild-type CCR5 (Fig. 3). Thus, the irel values are all less than 1.0. In agreement with our previous investigation (32), the curves in Fig. 3 have sigmoidal shapes that differ not only in their displacement along the coreceptor concentration axes but also in the maximum irel values obtained at saturating concentrations of the coreceptors (i.e., the asymptotes on the infectivity axes). As described previously (32) and in more detail below, we infer from these results that the adsorbed HIV-1 virions associate with CCR5 coreceptors in a concentration-dependent manner and that infection requires a complex that contains multiple CCR5s. In addition, as discussed below, the fact that these curves do not all plateau at the same irel value of 1.0 implies that the fully assembled complexes that form at saturating coreceptor concentrations may not mediate infections with the same efficiency.
In the CCR5(Y14N) clonal panel, the viruses with the single adaptive mutation S298N, F313L, F313I, or N300Y showed modest increases in relative titers compared to the wild-type JRCSF virus, with three- to sevenfold increases in the maximum irel at high coreceptor concentrations (Fig. 3A and B and Table 2). For these single mutations, there was no shift in the infectivity curves toward lower CCR5(Y14N) expression levels, implying that the enhanced infectivities were accomplished by increased efficiency of the entry pathway rather than by enhancement of viral affinity for the mutant CCR5(Y14N) molecules. Pseudotyped virions with envelopes containing the double mutant SNFL, SNNY, or NYFL exhibited even larger 13- to 23-fold increases in their maximum relative titers (Table 2 and Fig. 3A and B), also without shifting the curves toward lower CCR5(Y14N) concentrations. Similarly, the SNNYFL virus, with V3 mutations at all three sites, exhibited the greatest increase (ca. 40-fold) in the maximum irel compared to wild-type JRCSF (Fig. 3B and Table 2). In addition, this triple mutation caused a shift in the infectivity curve to lower CCR5(Y14N) concentrations, suggesting that it increased the apparent virus affinity for this mutant coreceptor. Indeed, the 50% effective concentration (EC50; the CCR5 concentration corresponding to the midpoint of the sigmoidal curves) for this triple mutant was decreased almost twofold compared to that of the wild-type virus (Fig. 3B and Table 3). Together, these data indicate that the adaptive V3 loop mutations enhance infectivity in an additive or synergistic manner. The mutations that were initially selected in cells that contain a saturating quantity of CCR5(Y14N) appear to increase the efficiency of infection without increasing viral affinity for the coreceptor, whereas the triple mutant that formed during selection in cells that contain a limiting concentration of CCR5(Y14N) had an enhanced apparent coreceptor affinity, as well as an increased efficiency of infection. As shown in Fig. 3A and B, the cells used for the initial selection had a saturating concentration of CCR5(Y14N) (i.e., 1.7 × 105 molecules per cell) whereas the secondary selection was done at a concentration (i.e., 6 × 104 molecules per cell) that was clearly subsaturating and severely limiting for infectivities of the JRCSF virus and for the viruses that grew during the initial selection.
TABLE 3.
Mathematical analysis of HIV-gpt infectivity dataa generated on the (CCR5)Y14N panel
| Envelope | R | m | EC50b |
|---|---|---|---|
| JRCSF | 0.84 | 6.6 ± 1.6 | 1.3 ± 0.2 |
| S298N | 0.96 | 6.2 ± 0.7 | 1.2 ± 0.08 |
| F313L | 0.95 | 5.2 ± 0.6 | 1.3 ± 0.08 |
| F313I | 0.95 | 7.3 ± 1.0 | 1.1 ± 0.08 |
| N300Y | 0.93 | 5.5 ± 0.8 | 1.3 ± 0.1 |
| SNFL | 0.90 | 3.8 ± 0.9 | 1.5 ± 0.2 |
| SNNY | 0.94 | 5.4 ± 0.7 | 1.1 ± 0.06 |
| NYFL | 0.96 | 6.6 ± 0.7 | 1.2 ± 0.07 |
| SNNYFL | 0.90 | 4.2 ± 0.9 | 0.73 ± 0.07 |
The data plotted in Fig. 4 were fitted to equation 9 in reference 32 by using Kaleidagraph (Synergy Software, Reading; Pa.). The calculated linear coefficients are reported in the R column. R values are regression coefficients showing a strong correlation between the magnitudes of the two axes. EC50s and m values are reported as means ± the standard error of the mean as calculated by Kaleidagraph.
Expressed as the number of CCR5 molecules per cell (105).
Infectivities of the adapted viruses in the CCR5(G163R) clonal panel.
Figure 3C and D show the relative infectivities of these same viruses in the panel of cell clones that express different amounts of CCR5(G163R). Among the single mutations, only F313I enhanced infection compared to the wild-type virus in CCR5(G163R)-expressing cells. This is perhaps not surprising, because only the F313I mutation was generated during selection in CCR5(G163R)-expressing cells (Table 1). Specifically, F313I enhanced the efficiency of infection (i.e., the maximum value on the irel axis) without significantly shifting the EC50. The maximum irel of the CCR5(Y14N)-adapted SNFL mutant in the CCR5(G163R) panel increased to an extent similar to that of the F313I mutant, supporting the idea that this double mutation also increases the efficiency of infection without increasing binding to any specific CCR5 site. Surprisingly, pseudotyped viruses containing the N300Y mutation, alone or in combination with the other mutations, were completely noninfectious in CCR5(G163R) cells, even at the highest coreceptor concentrations (Fig. 3D). These data are consistent with other evidence described below that N300Y weakens viral interactions with the CCR5 amino terminus and strengthens interactions with the TM4-ECL2 region that contains the G163 residue. Because they are more dependent on the G163 region, viruses with N300Y are completely unable to use CCR5(G163R).
Quantitative analysis of infectivity data.
The above interpretations of Fig. 3 were based on a previously described biophysical model (32). According to this model, the adsorbed virus that is associated with CD4 reversibly interacts with coreceptors to form a multimeric complex that is necessary for infection. Furthermore, the efficiency with which the properly assembled multimeric complexes infect the cells strongly depends upon the particular coreceptor and the viral gp120. A prediction of this model is that a plot of log [irel/(Erel − irel)] versus log [CCR5] should yield a straight line with a slope of m, where irel is the titer of the virus in each cell clone divided by the titer in JC.53 cells that express an excess of wild-type CCR5, Erel is the maximum irel for each sigmoidal curve, and m is the number of CCR5 molecules required to mediate R5 HIV-1 infections. Consistent with this prediction, the corresponding plots of the data derived from Fig. 3A and B fall approximately on straight lines (Fig. 4). Accordingly, the correlation coefficients (R values) for these plots were close to unity (Table 3). Furthermore, the m values, displayed in Table 3, were all within the range of four to six CCR5 molecules, in close agreement with previous estimates (32). The EC50s were also relatively constant for these assays [i.e., 1.1 × 105 to 1.5 × 105 CCR5(Y14N) molecules/cell], except for the SNNYFL triple mutant, which had a lower EC50 of 0.73 × 105 ± 0.07 × 105 CCR5(Y14N) molecules/cell (Table 3).
FIG. 4.
Mathematical analyses of infectivity data generated on the CCR5(Y14N) panel. The data in Fig. 3A and B were analyzed in accordance with the mathematical model derived by Kuhmann et al. (32). The irel at the highest concentration of mutant CCR5 that was assayed was used as the Erel value, and all of the other irel values that were defined were plotted as log [irel/(Erel − irel)] versus log [CCR5]. Only data points where CCR5 is at subsaturating concentrations can be plotted in this analysis, because when irel approaches Erel, the difference becomes inaccurate. Therefore, the number of data points is not the same for each pseudotyped virus but represents all of the significant information.
A similar analysis of the data obtained with the CCR5(G163R) panel was also performed. Although the results were fully compatible with the conclusions described above, there was more scatter in the data, as indicated by the lower R values, and the estimates of m were therefore uncertain. Previous studies using this panel with other viruses also yielded m values in the range of four to six molecules (32).
Membrane fusion activities of adapted envelope glycoproteins.
As described above and summarized in Table 2, mutations in CCR5 and in the V3 loop of gp120 can both strongly influence the asymptotes of the sigmoidal curves in Fig. 3. Thus, for example, the JRCSF virus is only 0.015 times as infectious in cells that express a saturating amount of CCR5(Y14N) as in cells with a saturating amount of wild-type CCR5, whereas the NYFL mutant has a much larger maximum irel (ca. 0.30) in CCR5(Y14N) cells. As discussed below, one possible interpretation is that the JRCSF virus that is saturated with CCR5(Y14N) functions inefficiently in a subsequent reaction that is essential for membrane fusion and that the NYFL mutant virus is more efficient in this postassembly step of infection. An alternative interpretation, that these viruses adsorb onto cells with different efficiencies, would be difficult to reconcile with their equal titers in cells that express wild-type CCR5 (see above) and with their similar apparent affinities for CCR5(Y14N) (EC50s in Table 3). A specific prediction of the former, but not of the latter, interpretation is that the envelope glycoprotein mutations that cause large increases in maximum relative infectivities of the pseudotyped viruses should be more active than the parental JRCSF glycoprotein in causing cell-cell fusion in syncytium assays.
We tested this by coculturing 293T cells expressing the envelope constructs described in Table 2 with HeLa-CD4 cells that expressed either wild-type CCR5 (JC.53 cells), a large amount of CCR5(Y14N) (YB8 cells), a small amount of CCR5(Y14N) (JYN.4 cells), or a small amount of CCR5(G163R) (JGR.H4 cells) and then quantitating the number of syncytia. The data are presented as a histogram in Fig. 5. Consistent with previous observations (32), syncytium formation caused by the wild-type JRCSF envelope was much reduced on cells expressing CCR5(Y14N) compared to that on those expressing wild-type CCR5. Indeed, syncytia were completely absent on JYN.4 cells, which express only a small quantity of CCR5(Y14N). Both the S298N and F313L mutations, alone or in combination, increased syncytium formation with CCR5(Y14N)-expressing cell lines, with the double mutation having a more potent effect. In contrast, the N300Y mutation, when expressed alone, did not significantly enhance syncytium induction. Consistent with our interpretation of Fig. 3, these data suggest that N300Y may enhance infection of cells by means other than membrane fusion. However, when acting in concert with either S298N, F313L, or both, N300Y contributed strongly to syncytium induction, especially in JYN.4 cells, which express only a low concentration of CCR5(Y14N). These results are consistent with the hypothesis that N300Y functions by increasing the assembly of virus-CCR5(Y14N) complexes and also by potentiating the fusogenic effects of the S298N and F313L mutations.
FIG. 5.
Syncytium induction by wild-type and adapted JRCSF envelopes on cells expressing CCR5(Y14N) and CCR5(G163R). 293T cells that had been transfected with JRCSF envelope expression vectors (described in Materials and Methods and Table 2) were cocultured for 6 h with HeLa-CD4 cells expressing either the wild-type or a mutant CCR5 coreceptor and then fixed and stained, and the syncytia in each well were counted. Percent syncytia compared to JC.53 was calculated for each envelope construct by dividing the number of syncytia obtained on cells expressing mutant coreceptors by the number of syncytia generated on JC.53 cells expressing wild-type CCR5 and multiplying by 100. These values were, in turn, normalized to the fusogenicity of wild-type JRCSF obtained on JC.53 cells (see values below). YB8 cells express 1.7 × 105 CCR5(Y14N) molecules per cell. JYN.4 cells express 6.0 × 104 CCR5(Y14N) molecules per cell. JGR.H4 cells express 1.9 × 104 CCR5(G163R) molecules per cell. JC.53 cells express 1.9 × 105 CCR5 molecules per cell. A representative assay, performed in triplicate, is shown, and the error bars represent standard deviations. The numbers of syncytia caused by the different envelope glycoproteins with JC.53 cells were similar but not identical. Thus, in a representative experiment, the normalized fusogenicities on the JC.53 cells were as follows: wild-type JRCSF, 1; S298N, 1.4; F313I, 1.2; F313L, 1.6; N300Y, 0.7; SNFL, 1.7; SNNY, 3.1; NYFL, 2.1; SNNYFL, 1.8. The expression levels of the envelope constructs were approximately equal, as measured by Western blot analysis (data not shown).
In agreement with our infectivity data (Fig. 3C and D), the N300Y mutation blocked utilization of the CCR5(G163R) coreceptor, as shown by the absence of syncytium formation in JGR.H4 cells. Also in agreement with Fig. 3, the F313I V3 loop mutation preferentially increased the fusogenicity mediated by CCR5(G163R) and had a relatively minor effect on the fusion mediated by CCR5(Y14N). Strikingly, there is a perfect correlation between the effects of the V3 loop mutations on the maximum relative infectivities of pseudotyped viruses (Fig. 3 and Table 2) and their effects on syncytium formation. This supports the idea that the adaptive V3 loop mutations influence a membrane fusion process rather than a virus adsorption process.
Infectivities of the adapted viruses in HeLa-CD4 cells that express CCR5 mutants with major amino-terminal deletions.
The above-described results suggested that the adapted viruses selected in cells that expressed the severely damaged CCR5(Y14N) coreceptor might have become less dependent on the amino-terminal region of this protein. To test this, we produced a population of HeLa-CD4 cells that express a deletion mutant CCR5 that lacks either 16 or 18 of the amino-terminal residues (this mutant CCR5 is termed R5d16 or R5d18, respectively). As shown in Fig. 6, the relative infectivities of the viruses in cells that express CCR5(Y14N) were similar to the results in Fig. 3. More interestingly, the triple mutant SNNYFL, which contained N300Y, was able to use the R5d16 and R5d18 coreceptors to a substantial extent. Presumably, the efficiencies of utilization of these coreceptors would be even higher in cell clones that expressed them uniformly at high concentrations (32). We conclude that the tyrosine sulfate-containing amino-terminal region of CCR5 is not absolutely required for infections by R5 strains of HIV-1.
FIG. 6.
Infections of HeLa-CD4 cells expressing CCR5 coreceptors with amino-terminal deletions. Populations of HeLa-CD4 cells expressing CCR5 with 16 (R5d16) or 18 (R5d18) amino-terminal residues removed, wild-type CCR5, or Y14N(CCR5) were generated by transduction with retroviral vectors (see Materials and Methods for details). Transduced cells were infected with pseudotyped viruses bearing the wild-type envelope or one of the mutant envelopes described in Table 2. Cells were placed in selective medium 48 h after infection. Drug-resistant colonies were stained and counted. The percentages of HeLa-CD4 cells expressing wild-type or mutant CCR5, determined by fluorescence-activated cell sorter analysis, were as follows: wild-type CCR5, 7.5%; CCR5(Y14N), 9.2%; R5d16, 8.2%; R5d18, 5.1%. Relative titers for each envelope construct in cells expressing mutant coreceptors were calculated by normalizing to the wild-type coreceptor activity and expression level with the following formula: (titer on mutant CCR5/titer on wild-type CCR5) × (wild-type CCR5 transduction efficiency/mutant CCR5 transduction efficiency). The average of three independent assays is shown, and error bars represent the standard error of the mean.
sCD4 inactivation of adapted viruses.
To determine whether the adaptive V3 loop mutations altered the viral sCD4 sensitivities, we preincubated the pseudotyped HIV-gpt virions with various concentrations of sCD4 before measuring the titers in cells expressing wild-type CCR5 (JC.53). Titers in the presence of sCD4 were divided by titers in the absence of sCD4 to generate relative values that were plotted versus sCD4 concentrations. As shown in Fig. 7, the relative infectivities of the mutant viruses were compared to those of wild-type JRCSF and laboratory-adapted SVIIIenv, which are sCD4 resistant and sensitive, respectively. Four mutations (F313I, SNFL, NYFL, and SNNYFL) caused increases in sCD4 sensitivities compared to the parental JRCSF envelope. Only two of these mutations, F313I and SNFL, produced greater titers on both CCR5(Y14N)- and CCR5(G163R)-expressing cells, while the others produced increased titers on CCR5(Y14N)-expressing cells only (see below; Fig. 3A to C). The remaining mutations (S298N, F313L, N300Y, and SNNY) caused either no changes or decreases in sCD4 sensitivities compared to the wild-type JRCSF virus, despite producing increased titers in Y14N(CCR5)-expressing cells (Fig. 3A and B). Thus, the V3 loop mutations caused large changes in sCD4 sensitivities that did not correlate with the viral adaptive properties.
FIG. 7.
sCD4 inactivation of pseudotyped HIV-gpt. HIV-gpt pseudotyped with the wild-type or mutant JRCSF envelope was subjected to treatment with various concentrations (5, 25, and 50 μg/ml) of sCD4 for 30 min prior to infection as previously described (49). Relative infectivities are plotted versus sCD4 concentrations with values in the absence of sCD4 equal to 1. All of the mutant envelopes described in Table 2 were tested, and the data have been divided into two panels (A and B) for ease of interpretation. SVIIIenv was included as a positive control for sCD4 sensitivity.
DISCUSSION
Interaction of viral gp120 and CCR5 involves at least two steps.
These results confirm our previous evidence (32) that there is a sigmoidal relationship between cell surface CCR5 concentrations and HIV-1 infectivities (Fig. 3). As we showed previously, mutations in CCR5 that reduce its affinity for purified gp120-sCD4 complexes cause dramatic shifts in the EC50s (midpoints of the sigmoidal curves) toward higher coreceptor concentrations (32). This strongly implies that CCR5 associates with HIV-1–CD4 complexes in a concentration-dependent manner to form fusion-competent complexes that contain multiple CCR5s. Consistent with the mathematical implications of this model and with previous evidence (32), the data in Fig. 4 fall approximately on straight lines with a common slope, m (m is the estimated number of CCR5 molecules in the competent complexes), suggesting m values in the range of approximately four to six molecules, regardless of the virus or the CCR5 mutant being analyzed (Table 3). Based on this apparent constancy of m values, we propose that m is the stoichiometry of CCR5 in the viral complexes that infect cells and that this number of CCR5s may occur in fusion pores that form in the membrane.
We emphasize in this context that EC50s, while strongly affected by HIV-1 affinities for the coreceptor (32), could also be influenced by other aspects of virus structure and function. For example, EC50s would be expected to depend, to a degree, on the number (m) of CCR5s that comprise the fusion-competent complexes with the virus. Thus, if an adaptive mutation in gp120 enabled the virus to use fewer CCR5s for infection but did not change the affinity of CCR5 monomer binding, the requisite complex would form at a lower CCR5 concentration. Although the data in Table 3 suggest that the m values are not significantly smaller for the SNNYFL mutant, which has a lower EC50 than the other viruses, these data also cannot fully exclude that interpretation. Consequently, our inference that this mutant virus has an increased affinity for CCR5(Y14N) compared to those of the other viruses is somewhat uncertain. Although we have not directly measured the affinities of the adapted viruses for these mutant CCR5s, this would be very difficult because the relevant affinities involve virus-CD4 complexes that interact with the coreceptor by cell surface (two-dimensional) diffusion rather than in solution. The binding affinity of purified gp120 would probably also differ from that of virus-assembled gp120-gp41 trimers. These issues require further investigation.
A striking result of the present study is that the sigmoid-shaped curves for wild-type and adapted mutant viruses do not all plateau at the same maximum irel value of 1.0 (Fig. 3 and Table 2). Thus, for example, the parental JRCSF virus was only 0.015 times as infectious in HeLa-CD4 cells that express a saturating concentration of CCR5(Y14N) as it is in JC.53 cells that express a saturating amount of wild-type CCR5. In contrast, the SNNY and NYFL adapted viruses infected CCR5(Y14N)-expressing cells 13 to 23 times more efficiently (Table 2) without causing any change in the EC50 or m value for these infections (Table 3). These differences in maximum relative efficiency were clearly determined by both the virus and the coreceptor with which it interacts and were not simply caused by differences in virus yield or infectivity. Indeed, all of the HIV-gpt viruses that were prepared in parallel had identical titers in JC.53 cells that contained wild-type CCR5, suggesting that the viruses were equally infectious and equally able to adsorb onto those cells.
We have been able to imagine only three possible mechanisms that could explain the low plateaus for many of the irel curves shown in Fig. 3 and summarized in Table 2. One possibility is that the viruses in these examples may adsorb inefficiently onto HeLa-CD4 cells that express the mutant coreceptors. We consider this extremely unlikely because these viruses all adsorb equally onto HeLa-CD4 cells that express wild-type CCR5 (see above) and because these viruses are CD4 dependent and are therefore adsorbed onto the cells prior to exposure of their coreceptor binding sites. In addition, HIV-1 binding studies have shown that adsorption onto HeLa cells does not require a coreceptor (29, 41). A second possibility is that these viruses adsorb normally onto the cells but their associations with the mutant CCR5s are so slow or so rapidly reversed by dissociation that the viruses become spontaneously inactivated prior to assembly of the critical fusion-competent complexes. Although it is conceivable, we also consider this to be unlikely because most of the adapted viruses infect the cells much more efficiently than does the parental JRCSF virus yet have identical EC50s and m values. Since binding affinities are determined by ratios of association and dissociation reactions and strongly affect EC50s (32), it seems very unlikely that EC50s and m values could remain constant for all of these viruses if the adaptive mutations had major effects on the rates of coreceptor association or dissociation. Furthermore, if the assembly process were slow, it would continue to be accelerated at high coreceptor concentrations, yet our infectivity curves reach flat plateaus. For these reasons, we believe that the low maximum irel values for the viruses studied in Fig. 3 and Table 2 must be caused by low efficiency at a critical step of infection that follows assembly of the fusion-competent virus-coreceptor complexes. This conclusion is compatible with the cell-cell fusion assays in Fig. 5. In particular, the maximum relative infectivities of the viruses in the CCR5(Y14N) and CCR5(G163R) clonal panels correlated strongly with the fusogenicities of their envelope glycoproteins in the syncytium assays.
What else can we infer about this putative postassembly step of the HIV-1 infection pathway? First, it is essential for membrane fusion and can severely limit infections of cells that contain suboptimal concentrations or types of coreceptors. It is not an automatic or necessarily efficient consequence of virus-coreceptor associations, as has been previously assumed. Second, because the infectivity curves reach plateaus at high coreceptor concentrations, this postassembly step is independent of the CCR5 concentration. Third, we believe that this postassembly step is most likely a conformational change in the complex. If the interaction of the virus with the coreceptor is suboptimal, the postassembly step might often be abortive, causing the overall efficiency of infection to decline.
Adaptive mutations of HIV-1 to attenuated CCR5s cluster within the gp120 V3 loop.
Interestingly, the adaptive mutations in the JRCSF isolate of HIV-1 that we were able to identify all occurred within the gp120 V3 loop. These adaptive V3 mutations strongly and differentially affected both the assembly and postassembly steps of the entry pathway. In particular, the SNNYFL triple mutant was more efficient in the assembly process, as indicated by a reduction in its EC50 in the CCR5(Y14N) clonal panel. Presumably, this assembly change was caused by an increased affinity of the virus for this coreceptor or, less likely, by a decrease in m (see above). In contrast, the other adaptive V3 loop mutations were more efficient in the putative postassembly process. These results support the idea that the V3 loop can function as a modular element that is capable of adapting to changing concentrations or structures of coreceptors present in different cells. Moreover, our data suggest that the V3 loop may serve as a transducer that interacts directly with the coreceptor in an assembly pathway and then also participates directly in mediation of the conformational changes that ensue. The V3 loop also interacts, at least indirectly, with the CD4 binding site, as indicated by its exposure following CD4 attachment and by the strong effects of V3 mutations on the sCD4 sensitivities of viruses (Fig. 7) (26). In this context, it is intriguing that CXCR4 seems to bind to X4 strains of HIV-1 only relatively weakly (25, 40) and that X4 viruses differ from R5 isolates in their gp120 V3 loops (42, 58, 62, 64) and in their enhanced fusogenicities in certain assays (8, 16, 24, 26, 43, 58). These differences all correspond to the concerted changes that we have observed in JRCSF mutants that have adapted to forced passages in cells that express attenuated coreceptors.
Redundant interactions of gp120 with different regions of CCR5 and expendability of the CCR5 amino terminus.
The Y14N mutation severely disables the amino terminus of CCR5 by eliminating an important tyrosine sulfation site and converting a YYT sequence into an NYT consensus site for N-linked glycosylation (32). Although we initially anticipated that adaptive mutations in gp120 might function by increasing binding to this severely disabled site, our results strongly suggest that the adaptations were accomplished by other means. In particular, the S298N and F313L V3 loop mutations appear to function by enhancing viral fusogenicity rather than by increasing viral affinity for CCR5(Y14N) (Fig. 3 and 5 and Table 3). Furthermore, although the N300Y substitution is not fusogenic by itself, it appears to potentiate the fusogenicities of S298N and F313L and also to increase viral affinity for CCR5(Y14N) in the context of these other mutations. Unexpectedly, however, the N300Y substitution prevents viral utilization of CCR5(G163R), as indicated by both infectivity (Fig. 3) and syncytium (Fig. 5) assays. Moreover, as shown in Fig. 6, the N300Y mutation, in conjunction with S298N and F313L, enabled HIV-1 to abandon its dependency on the amino-terminal region of CCR5 and to better utilize a deletion-containing form of CCR5 that lacks this tyrosine sulfate-containing region. Based on these results, we propose that N300Y increases viral affinity for the TM4-ECL2 junction region of CCR5 that contains G163 and thereby weakens viral dependency on the CCR5 amino terminus. Conversely, because the N300Y mutant is more dependent on the G163 region of CCR5, its infectivity is abolished by the G163R substitution.
An important corollary of these results is that interactions of HIV-1 with the amino-terminal and TM4-ECL2 regions of CCR5 perform additive and redundant rather than individually essential functions in infection. Consequently, a disabling mutation in one region of CCR5 can be counteracted by an adaptive viral mutation that increases interactions with another region of the coreceptor. Furthermore, we conclude that the amino-terminal region of CCR5 is not essential for its coreceptor activity. In support of this conclusion, we have recently selected additional adapted derivatives of the JRCSF virus that efficiently and rapidly replicate in HeLa-CD4 cells that express the R5d16 and R5d18 CCR5 deletion mutants (results not shown). Similarly, the amino-terminal region of CXCR4 is not essential for infections by X4 strains of HIV-1 (15).
Two groups have described a region encompassing the N300Y mutation, composed of residues within the V3 loop and C4, that contributes to the specific binding of a sulfated CCR5 amino-terminal peptide (12, 23). Some mutations within this critical region destroyed the N-linked glycosylation site at position 299 within the V3 loop and inhibited binding of the gp120-CD4 complex to sulfated CCR5 peptides and to cell surface-expressed CCR5 (12). Other recent work implicates the loss of this glycan in coreceptor switching and in increased susceptibility to inhibitors of coreceptor binding (38, 51). The JRCSF N300Y mutation occurs at position X in the N-linked glycosylation consensus sequence (NXT) within the V3 loop and thus preserves this modification. Consistent with this, N300Y did not cause a shift to CXCR4 use or abrogation of wild-type CCR5 use. The loss of CCR5 amino-terminal dependency effected by the N300Y mutation is consistent with data cited above suggesting that mutations in this region decrease CCR5 sulfated-peptide binding. However, the increased dependency of HIV-1 envelopes with the N300Y mutation on the wild-type core region of CCR5 suggests that N300Y also increases interactions with the TM4-ECL2 junction region. Because the N300Y substitution would probably be substantially buried by the adjacent N-linked oligosaccharide at position N299, it seems unlikely that it would be directly accessible to CCR5. Indeed, it is well known that N-linked glycosylation of receptors can block binding of retroviruses to nearby sites (6, 39). However, the local amino acid sequence has a strong effect on the processing of N-linked oligosaccharides, often determining whether they are complex or simple neutral structures (28, 53). The V3 loop and adjacent region of gp120 is generally considered to be highly basic (35, 55), but this property would be substantially modified by sialylation and/or sulfation (3) of a complex N-linked oligosaccharide at position N299. Based on these considerations, we propose that the structure of the N-linked oligosaccharide at position N299 in the V3 loop may influence associations of HIV-1 with specific sites in CCR5.
ACKNOWLEDGMENTS
This research was supported by NIH grant R01 CA67358.
We are grateful to our coworkers and colleagues Sue Kozak, Sean Kelly, Dimitri Lavillette, Navid Madani, Mariana Marin, and Chetankumar Tailor for encouragement and advice. We thank Anthony Bakke and Randy Smith for assistance with flow cytometry.
REFERENCES
- 1.Alkhatib G, Combadiere C, Broder C C, Feng Y, Kennedy P E, Murphy P M, Berger E A. CC CKR5: a RANTES, MIP-1α, MIP-1β receptor as a fusion cofactor for macrophage-tropic HIV-1. Science. 1996;272:1955–1958. doi: 10.1126/science.272.5270.1955. [DOI] [PubMed] [Google Scholar]
- 2.Atchison R E, Gosling J, Monteclaro F S, Franci C, Digilio L, Charo I F, Goldsmith M A. Multiple extracellular elements of CCR5 and HIV-1 entry: dissociation from response to chemokines. Science. 1996;274:1924–1926. doi: 10.1126/science.274.5294.1924. [DOI] [PubMed] [Google Scholar]
- 3.Bernstein H B, Compans R W. Sulfation of the human immunodeficiency virus envelope glycoprotein. J Virol. 1992;66:6953–6959. doi: 10.1128/jvi.66.12.6953-6959.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berson J F, Long D, Doranz B J, Rucker J, Jirik F R, Doms R W. A seven-transmembrane domain receptor involved in fusion and entry of T-cell-tropic human immunodeficiency virus type 1 strains. J Virol. 1996;70:6288–6295. doi: 10.1128/jvi.70.9.6288-6295.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bieniasz P D, Fridell R A, Aramori I, Ferguson S S, Caron M G, Cullen B R. HIV-1-induced cell fusion is mediated by multiple regions within both the viral envelope and the CCR-5 co-receptor. EMBO J. 1997;16:2599–2609. doi: 10.1093/emboj/16.10.2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chabot D J, Chen H, Dimitrov D S, Broder C C. N-linked glycosylation of CXCR4 masks coreceptor function for CCR5-dependent human immunodeficiency virus type 1 isolates. J Virol. 2000;74:4404–4413. doi: 10.1128/jvi.74.9.4404-4413.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan D C, Kim P S. HIV entry and its inhibition. Cell. 1998;93:681–684. doi: 10.1016/s0092-8674(00)81430-0. [DOI] [PubMed] [Google Scholar]
- 8.Cheng-Mayer C, Quiroga M, Tung J W, Dina D, Levy J A. Viral determinants of human immunodeficiency virus type 1 T-cell or macrophage tropism, cytopathogenicity, and CD4 antigen modulation. J Virol. 1990;64:4390–4398. doi: 10.1128/jvi.64.9.4390-4398.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choe H, Farazan M, Sun Y, Sullivan N, Rollins B, Ponath P D, Wu L, Mackay C R, LaRosa G, Newman W, Gerard N, Gerard C, Sodroski J. The β-chemokine receptors CCR3 and CCR5 facilitate infection by primary HIV-1 isolates. Cell. 1996;85:1135–1148. doi: 10.1016/s0092-8674(00)81313-6. [DOI] [PubMed] [Google Scholar]
- 10.Connor R I, Sheridan K E, Ceradini D, Choe S, Landau N R. Change in coreceptor use correlates with disease progression in HIV-1-infected individuals. J Exp Med. 1997;185:621–628. doi: 10.1084/jem.185.4.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cormier E G, Persuh M, Thompson D A, Lin S W, Sakmar T P, Olson W C, Dragic T. Specific interaction of CCR5 amino-terminal domain peptides containing sulfotyrosines with HIV-1 envelope glycoprotein gp120. Proc Natl Acad Sci USA. 2000;97:5762–5767. doi: 10.1073/pnas.97.11.5762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cormier E G, Tran D N, Yukhayeva L, Olson W C, Dragic T. Mapping the determinants of the CCR5 amino-terminal sulfopeptide interaction with soluble human immunodeficiency virus type 1 gp120-CD4 complexes. J Virol. 2001;75:5541–5549. doi: 10.1128/JVI.75.12.5541-5549.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dean M, Carrington M, Winkler C, Huttley G A, Smith M W, Allikmets R, Goedert J J, Buchbinder S P, Vittinghoff E, Gomperts E, Donfield S, Vlahov D, Kaslow R, Saah A, Rinaldo C, Detels R, O'Brien S J. Genetic restriction of HIV-1 infection and progression to AIDS by a deletion allele of the CKR5 structural gene. Hemophilia Growth and Development Study, Multicenter AIDS Cohort Study, Multicenter Hemophilia Cohort Study, San Francisco City Cohort, ALIVE Study. Science. 1996;273:1856–1862. doi: 10.1126/science.273.5283.1856. [DOI] [PubMed] [Google Scholar]
- 14.Deng H, Liu R, Ellmeier W, Choe S, Unutmaz D, Burkhart M, Di Marzio P, Marmon S, Sutton R E, Hill C M, Davis C B, Peiper S C, Schall T J, Littman D R, Landau N R. Identification of a major co-receptor for primary isolates of HIV-1. Nature. 1996;381:661–666. doi: 10.1038/381661a0. [DOI] [PubMed] [Google Scholar]
- 15.Doranz B J, Orsini M J, Turner J D, Hoffman T L, Berson J F, Hoxie J A, Peiper S C, Brass L F, Doms R W. Identification of CXCR4 domains that support coreceptor and chemokine receptor functions. J Virol. 1999;73:2752–2761. doi: 10.1128/jvi.73.4.2752-2761.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Doranz B J, Rucker J, Yi Y, Smyth R J, Samson M, Peiper S C, Parmentier M, Collman R G, Doms R W. A dual-tropic primary HIV-1 isolate that uses fusin and the β-chemokine receptors CKR-5, CKR-3, and CKR-2b as fusion cofactors. Cell. 1996;85:1149–1158. doi: 10.1016/s0092-8674(00)81314-8. [DOI] [PubMed] [Google Scholar]
- 17.Dragic T, Litwin V, Allaway G P, Martin S R, Huang Y, Nagashima K A, Cayanan C, Maddon P J, Koup R A, Moore J P, Paxton W A. HIV-1 entry into CD4+ cells is mediated by the chemokine receptor CC-CKR-5. Nature. 1996;381:667–673. doi: 10.1038/381667a0. [DOI] [PubMed] [Google Scholar]
- 18.Dragic T, Trkola A, Lin S W, Nagashima K A, Kajumo F, Zhao L, Olson W C, Wu L, Mackay C R, Allaway G P, Sakmar T P, Moore J P, Maddon P J. Amino-terminal substitutions in the CCR5 coreceptor impair gp120 binding and human immunodeficiency virus type 1 entry. J Virol. 1998;72:279–285. doi: 10.1128/jvi.72.1.279-285.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Etemad-Moghadam B, Rhone D, Steenbeke T, Sun Y, Manola J, Gelman R, Fanton J W, Racz P, Tenner-Racz K, Axthelm M K, Letvin N L, Sodroski J. Membrane-fusing capacity of the human immunodeficiency virus envelope proteins determines the efficiency of CD4+ T-cell depletion in macaques infected by a simian-human immunodeficiency virus. J Virol. 2001;75:5646–5655. doi: 10.1128/JVI.75.12.5646-5655.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Etemad-Moghadam B, Sun Y, Nicholson E K, Fernandes M, Liou K, Gomila R, Lee J, Sodroski J. Envelope glycoprotein determinants of increased fusogenicity in a pathogenic simian-human immunodeficiency virus (SHIV-KB9) passaged in vivo. J Virol. 2000;74:4433–4440. doi: 10.1128/jvi.74.9.4433-4440.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Farzan M, Choe H, Vaca L, Martin K, Sun Y, Desjardins E, Ruffing N, Wu L, Wyatt R, Gerard N, Gerard C, Sodroski J. A tyrosine-rich region in the N terminus of CCR5 is important for human immunodeficiency virus type 1 entry and mediates an association between gp120 and CCR5. J Virol. 1998;72:1160–1164. doi: 10.1128/jvi.72.2.1160-1164.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Farzan M, Mirzabekov T, Kolchinsky P, Wyatt R, Cayabyab M, Gerard N P, Gerard C, Sodroski J, Choe H. Tyrosine sulfation of the amino terminus of CCR5 facilitates HIV-1 entry. Cell. 1999;96:667–676. doi: 10.1016/s0092-8674(00)80577-2. [DOI] [PubMed] [Google Scholar]
- 23.Farzan M, Vasilieva N, Schnitzler C E, Chung S, Robinson J, Gerard N P, Gerard C, Choe H, Sodroski J. A tyrosine-sulfated peptide based on the N terminus of CCR5 interacts with a CD4-enhanced epitope of the HIV-1 gp120 envelope glycoprotein and inhibits HIV-1 entry. J Biol Chem. 2000;275:33516–33521. doi: 10.1074/jbc.M007228200. [DOI] [PubMed] [Google Scholar]
- 24.Feng Y, Broder C C, Kennedy P E, Berger E A. HIV-1 entry cofactor: functional cDNA cloning of a seven-transmembrane, G protein-coupled receptor. Science. 1996;272:872–877. doi: 10.1126/science.272.5263.872. [DOI] [PubMed] [Google Scholar]
- 25.Hoffman T L, Canziani G, Jia L, Rucker J, Doms R W. A biosensor assay for studying ligand-membrane receptor interactions: binding of antibodies and HIV-1 Env to chemokine receptors. Proc Natl Acad Sci USA. 2000;97:11215–11220. doi: 10.1073/pnas.190274097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hwang S S, Boyle T J, Lyerly H K, Cullen B R. Identification of envelope V3 loop as the major determinant of CD4 neutralization sensitivity of HIV-1. Science. 1992;257:535–537. doi: 10.1126/science.1636088. [DOI] [PubMed] [Google Scholar]
- 27.Kabat D, Kozak S L, Wehrly K, Chesebro B. Differences in CD4 dependence for infectivity of laboratory-adapted and primary patient isolates of human immunodeficiency virus type 1. J Virol. 1994;68:2570–2577. doi: 10.1128/jvi.68.4.2570-2577.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kornfield R, Kornfield S. Assembly of asparagine-linked oligosaccharides. Annu Rev Biochem. 1985;54:631–634. doi: 10.1146/annurev.bi.54.070185.003215. [DOI] [PubMed] [Google Scholar]
- 29.Kozak, S. L., V. Marechal, J. M. Heard, and D. Kabat. Segregation of CD4 and CXCR4 into distinct lipid microdomains in T lymphocytes suggests a mechanism for membrane destabilization by human immunodeficiency virus. J. Virol., in press. [DOI] [PMC free article] [PubMed]
- 30.Kozak S L, Platt E J, Madani N, Ferro F E, Jr, Peden K, Kabat D. CD4, CXCR-4, and CCR-5 dependencies for infections by primary patient and laboratory-adapted isolates of human immunodeficiency virus type 1. J Virol. 1997;71:873–882. doi: 10.1128/jvi.71.2.873-882.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kreisberg J F, Kwa D, Schramm B, Trautner V, Connor R, Schuitemaker H, Mullins J I, van't Wout A B, Goldsmith M A. Cytopathicity of human immunodeficiency virus type 1 primary isolates depends on coreceptor usage and not patient disease status. J Virol. 2001;75:8842–8847. doi: 10.1128/JVI.75.18.8842-8847.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kuhmann S E, Platt E J, Kozak S L, Kabat D. Cooperation of multiple CCR5 coreceptors is required for infections by human immunodeficiency virus type 1. J Virol. 2000;74:7005–7015. doi: 10.1128/jvi.74.15.7005-7015.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kuhmann S E, Platt E J, Kozak S L, Kabat D. Polymorphisms in the CCR5 genes of African green monkeys and mice implicate specific amino acids in infections by simian and human immunodeficiency viruses. J Virol. 1997;71:8642–8656. doi: 10.1128/jvi.71.11.8642-8656.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kwong P D, Wyatt R, Robinson J, Sweet R W, Sodroski J, Hendrickson W A. Structure of an HIV gp120 envelope glycoprotein in complex with the CD4 receptor and a neutralizing human antibody. Nature. 1998;393:648–659. doi: 10.1038/31405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kwong P D, Wyatt R, Sattentau Q J, Sodroski J, Hendrickson W A. Oligomeric modeling and electrostatic analysis of the gp120 envelope glycoprotein of human immunodeficiency virus. J Virol. 2000;74:1961–1972. doi: 10.1128/jvi.74.4.1961-1972.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee B, Sharron M, Blanpain C, Doranz B J, Vakili J, Setoh P, Berg E, Liu G, Guy H R, Durell S R, Parmentier M, Chang C N, Price K, Tsang M, Doms R W. Epitope mapping of CCR5 reveals multiple conformational states and distinct but overlapping structures involved in chemokine and coreceptor function. J Biol Chem. 1999;274:9617–9626. doi: 10.1074/jbc.274.14.9617. [DOI] [PubMed] [Google Scholar]
- 37.Liu R, Paxton W A, Choe S, Ceradini D, Martin S R, Horuk R, MacDonald M E, Stuhlmann H, Koup R A, Landau N R. Homozygous defect in HIV-1 coreceptor accounts for resistance of some multiply-exposed individuals to HIV-1 infection. Cell. 1996;86:367–377. doi: 10.1016/s0092-8674(00)80110-5. [DOI] [PubMed] [Google Scholar]
- 38.Malenbaum S E, Yang D, Cavacini L, Posner M, Robinson J, Cheng-Mayer C. The N-terminal V3 loop glycan modulates the interaction of clade A and B human immunodeficiency virus type 1 envelopes with CD4 and chemokine receptors. J Virol. 2000;74:11008–11016. doi: 10.1128/jvi.74.23.11008-11016.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marin M, Tailor C S, Nouri A, Kabat D. Sodium-dependent neutral amino acid transporter type 1 is an auxiliary receptor for baboon endogenous retrovirus. J Virol. 2000;74:8085–8093. doi: 10.1128/jvi.74.17.8085-8093.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mondor I, Moulard M, Ugolini S, Klasse P J, Hoxie J, Amara A, Delaunay T, Wyatt R, Sodroski J, Sattentau Q J. Interactions among HIV gp120, CD4, and CXCR4: dependence on CD4 expression level, gp120 viral origin, conservation of the gp120 COOH- and NH2-termini and V1/V2 and V3 loops, and sensitivity to neutralizing antibodies. Virology. 1998;248:394–405. doi: 10.1006/viro.1998.9282. [DOI] [PubMed] [Google Scholar]
- 41.Mondor I, Ugolini S, Sattentau Q J. Human immunodeficiency virus type 1 attachment to HeLa CD4 cells is CD4 independent and gp120 dependent and requires cell surface heparans. J Virol. 1998;72:3623–3634. doi: 10.1128/jvi.72.5.3623-3634.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nelson J A, Baribaud F, Edwards T, Swanstrom R. Patterns of changes in human immunodeficiency virus type 1 V3 sequence populations late in infection. J Virol. 2000;74:8494–8501. doi: 10.1128/jvi.74.18.8494-8501.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.O'Brien W A, Koyanagi Y, Namazie A, Zhao J Q, Diagne A, Idler K, Zack J A, Chen I S. HIV-1 tropism for mononuclear phagocytes can be determined by regions of gp120 outside the CD4-binding domain. Nature. 1990;348:69–73. doi: 10.1038/348069a0. [DOI] [PubMed] [Google Scholar]
- 44.Olson W C, Rabut G E, Nagashima K A, Tran D N, Anselma D J, Monard S P, Segal J P, Thompson D A, Kajumo F, Guo Y, Moore J P, Maddon P J, Dragic T. Differential inhibition of human immunodeficiency virus type 1 fusion, gp120 binding, and CC-chemokine activity by monoclonal antibodies to CCR5. J Virol. 1999;73:4145–4155. doi: 10.1128/jvi.73.5.4145-4155.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Page K A, Landau N R, Littman D R. Construction and use of a human immunodeficiency virus vector for analysis of virus infectivity. J Virol. 1990;64:5270–5276. doi: 10.1128/jvi.64.11.5270-5276.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Page K A, Stearns S M, Littman D R. Analysis of mutations in the V3 domain of gp160 that affect fusion and infectivity. J Virol. 1992;66:524–533. doi: 10.1128/jvi.66.1.524-533.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Picard L, Simmons G, Power C A, Meyer A, Weiss R A, Clapham P R. Multiple extracellular domains of CCR-5 contribute to human immunodeficiency virus type 1 entry and fusion. J Virol. 1997;71:5003–5011. doi: 10.1128/jvi.71.7.5003-5011.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Platt E J, Kozak S L, Kabat D. Critical role of enhanced CD4 affinity in laboratory adaptation of human immunodeficiency virus type 1. AIDS Res Hum Retrovir. 2000;16:871–882. doi: 10.1089/08892220050042819. [DOI] [PubMed] [Google Scholar]
- 49.Platt E J, Madani N, Kozak S L, Kabat D. Infectious properties of human immunodeficiency virus type 1 mutants with distinct affinities for the CD4 receptor. J Virol. 1997;71:883–890. doi: 10.1128/jvi.71.2.883-890.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Platt E J, Wehrly K, Kuhmann S E, Chesebro B, Kabat D. Effects of CCR5 and CD4 cell surface concentrations on infections by macrophage-tropic isolates of human immunodeficiency virus type 1. J Virol. 1998;72:2855–2864. doi: 10.1128/jvi.72.4.2855-2864.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pollakis G, Kang S, Kliphuis A, Chalaby M I, Goudsmit J, Paxton W A. N-linked glycosylation of the HIV type-1 gp120 envelope glycoprotein as a major determinant of CCR5 and CXCR4 coreceptor utilization. J Biol Chem. 2001;276:13433–13441. doi: 10.1074/jbc.M009779200. [DOI] [PubMed] [Google Scholar]
- 52.Rabut G E, Konner J A, Kajumo F, Moore J P, Dragic T. Alanine substitutions of polar and nonpolar residues in the amino-terminal domain of CCR5 differently impair entry of macrophage- and dual-tropic isolates of human immunodeficiency virus type 1. J Virol. 1998;72:3464–3468. doi: 10.1128/jvi.72.4.3464-3468.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rademacher T W, Parekh R B, Dwek R A. Glycobiology. Annu Rev Biochem. 1988;57:785–838. doi: 10.1146/annurev.bi.57.070188.004033. [DOI] [PubMed] [Google Scholar]
- 54.Rana S, Besson G, Cook D G, Rucker J, Smyth R J, Yi Y, Turner J D, Guo H-H, Du J-G, Peiper S C, Lavi E, Samson M, Libert F, Liesnard C, Vassart G, Doms R W, Parmentier M, Collman R G. Role of CCR5 in infection of primary macrophages and lymphocytes by macrophage-tropic strains of human immunodeficiency virus: resistance to patient-derived and prototype isolates resulting from the Δccr5 mutation. J Virol. 1997;71:3219–3227. doi: 10.1128/jvi.71.4.3219-3227.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rizzuto C D, Wyatt R, Hernandez-Ramos N, Sun Y, Kwong P D, Hendrickson W A, Sodroski J. A conserved HIV gp120 glycoprotein structure involved in chemokine receptor binding. Science. 1998;280:1949–1953. doi: 10.1126/science.280.5371.1949. [DOI] [PubMed] [Google Scholar]
- 56.Rucker J, Samson M, Doranz B J, Libert F, Berson J F, Yi Y, Smyth R J, Collman R G, Broder C C, Vassart G, Doms R W, Parmentier M. Regions in beta-chemokine receptors CCR5 and CCR2b that determine HIV-1 cofactor specificity. Cell. 1996;87:437–446. doi: 10.1016/s0092-8674(00)81364-1. [DOI] [PubMed] [Google Scholar]
- 57.Samson M, Libert F, Doranz B J, Rucker J, Liesnard C, Farber C M, Saragosti S, Lapoumeroulie C, Cognaux J, Forceille C, Muyldermans G, Verhofstede C, Burtonboy G, Georges M, Imai T, Rana S, Yi Y, Smyth R J, Collman R G, Doms R W, Vassart G, Parmentier M. Resistance to HIV-1 infection in Caucasian individuals bearing mutant alleles of the CCR-5 chemokine receptor gene. Nature. 1996;382:722–725. doi: 10.1038/382722a0. [DOI] [PubMed] [Google Scholar]
- 58.Scarlatti G, Tresoldi E, Bjorndal A, Fredriksson R, Colognesi C, Deng H K, Malnati M S, Plebani A, Siccardi A G, Littman D R, Fenyo E M, Lusso P. In vivo evolution of HIV-1 co-receptor usage and sensitivity to chemokine-mediated suppression. Nat Med. 1997;3:1259–1265. doi: 10.1038/nm1197-1259. [DOI] [PubMed] [Google Scholar]
- 59.Schuitemaker H, Koot M, Kootstra N A, Dercksen M W, de Goede R E, van Steenwijk R P, Lange J M A, Eeftink Schattenkerk J K M, Miedema F, Tersmette M. Biological phenotype of human immunodeficiency virus type 1 clones at different stages of infection: progression of disease is associated with a shift from monocytotropic to T-cell-tropic virus populations. J Virol. 1992;66:1354–1360. doi: 10.1128/jvi.66.3.1354-1360.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Scoggins R M, Taylor J R, Jr, Patrie J, van't Wout A B, Schuitemaker H, Camerini D. Pathogenesis of primary R5 human immunodeficiency virus type 1 clones in SCID-hu mice. J Virol. 2000;74:3205–3216. doi: 10.1128/jvi.74.7.3205-3216.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Siciliano S J, Kuhmann S E, Weng Y, Madani N, Springer M S, Lineberger J E, Danzeisen R, Miller M D, Kavanaugh M P, DeMartino J A, Kabat D. A critical site in the core of the CCR5 chemokine receptor required for binding and infectivity of human immunodeficiency virus type 1. J Biol Chem. 1999;274:1905–1913. doi: 10.1074/jbc.274.4.1905. [DOI] [PubMed] [Google Scholar]
- 62.Speck R F, Wehrly K, Platt E J, Atchison R E, Charo I F, Kabat D, Chesebro B, Goldsmith M A. Selective employment of chemokine receptors as human immunodeficiency virus type 1 coreceptors determined by individual amino acids within the envelope V3 loop. J Virol. 1997;71:7136–7139. doi: 10.1128/jvi.71.9.7136-7139.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Trkola A, Dragic T, Arthos J, Binley J M, Olson W C, Allaway G P, Cheng-Mayer C, Robinson J, Maddon P J, Moore J P. CD4-dependent, antibody-sensitive interactions between HIV-1 and its co-receptor CCR-5. Nature. 1996;384:184–187. doi: 10.1038/384184a0. [DOI] [PubMed] [Google Scholar]
- 64.Wang W K, Dudek T, Essex M, Lee T H. Hypervariable region 3 residues of HIV type 1 gp120 involved in CCR5 coreceptor utilization: therapeutic and prophylactic implications. Proc Natl Acad Sci USA. 1999;96:4558–4562. doi: 10.1073/pnas.96.8.4558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Weissenhorn W, Dessen A, Harrison S C, Skehel J J, Wiley D C. Atomic structure of the ectodomain from HIV-1 gp41. Nature. 1997;387:426–430. doi: 10.1038/387426a0. [DOI] [PubMed] [Google Scholar]
- 66.Wu L, Gerard N P, Wyatt R, Choe H, Parolin C, Ruffing N, Borsetti A, Cardoso A A, Desjardin E, Newman W, Gerard C, Sodroski J. CD4-induced interaction of primary HIV-1 gp120 glycoproteins with the chemokine receptor CCR-5. Nature. 1996;384:179–183. doi: 10.1038/384179a0. [DOI] [PubMed] [Google Scholar]
- 67.Wyatt R, Kwong P D, Desjardins E, Sweet R W, Robinson J, Hendrickson W A, Sodroski J G. The antigenic structure of the HIV gp120 envelope glycoprotein. Nature. 1998;393:705–711. doi: 10.1038/31514. [DOI] [PubMed] [Google Scholar]