Abstract
BACKGROUND:
Exercise is a first-line treatment for chronic non-specific low back pain (CNSLBP). Exercise combined with specific breathing techniques have the potential to improve multifactorial outcomes. No previous studies, however, have compared outcomes between identical exercises with or without a specific breathing protocol in a uniform clinical study setting.
OBJECTIVES:
1) To investigate the feasibility of combining synchronized breathing with movement control exercises and evaluate eligibility criteria, randomization procedures, and dropout rates. 2) To study the preliminary efficacy of the interventions on multifactorial outcome measures.
METHODS:
Thirty subjects with CNSLBP were randomized into two groups. Both groups had four contact clinic visits where they received personalized home movement control exercises to practice over two months. The experimental group included a movement control exercise intervention combined with synchronized breathing techniques. Trial registration number: NCT05268822.
RESULTS:
Feasibility was demonstrated by meeting the recruitment goal of 30 subjects within the pre-specified timeframe with enrolment rate of 24.8% (30/121). Synchronized breathing techniques were successfully adhered by participants. Home exercise adherence was nearly identical between the groups without any adverse events. Preliminary efficacy findings on pain intensity, disability, and self-efficacy in the experimental group exceeded the minimal clinically important difference. No such findings were observed in any outcome measures within the control group. Overall, multifactorial differences were consistent because nine out of eleven outcome measures showed greater improvements for the experimental group.
CONCLUSION:
The synchronized breathing with movement control exercises protocol was feasible and may be more beneficial for improving multifactorial outcomes compared to identical exercises alone. Results suggested progression to a full-scale trial.
Keywords: Chronic musculoskeletal pain, feasibility, breathing exercises, specific breathing technique, motor control exercises, yoga, pilates
1. Introduction
Chronic non-specific low back pain (CNSLBP) is the most prevalent musculoskeletal pain syndrome [1, 2]. It is widely recognized that different biopsychosocial factors lead to CNSLBP [3]. Exercise therapies, including movement control exercises utilized in this study, are the most used conservative interventions to treat CNSLBP and have small-to-moderate treatment effect sizes on pain intensity and disability [4, 5, 6, 7]. The modest effectiveness of existing pain treatments has been a major challenge, so there has been a call for novel solutions to promote more effective management strategies for CNSLBP [5, 8].
Exercise interventions incorporating specific breathing techniques, like yoga and Pilates, are among the most effective exercises for treating CNSLBP [9, 10, 11, 12]. These exercises include specific breathing techniques combined with movement, which may have multifactorial effectiveness beyond CNSLBP core outcome measures of pain and disability [13, 14, 15, 16, 17, 18]. Previous studies are limited in their ability to directly test the effectiveness of specific breathing techniques due to study cohort demographics, contextual factors (e.g., clinic environment, therapists experience and attitudes), exercise (e.g., content, duration) and the add-on breathing protocols are very heterogenous [19, 20, 21, 22]. Because of this, this study carefully designed and conducted the current study with substantial efforts to monitor and promote identical exercise programs in uniform study groups and clinical settings to study the feasibility of specific breathing add-on and quantify possible multifactorial changes in patient-reported outcomes measures (PROMs). There are no previous studies that have compared the outcomes of identical exercises with or without specific breathing techniques in a uniform clinical study setting.
Study objectives: (1) To investigate the feasibility of combining synchronized breathing with movement control exercises and evaluate eligibility criteria, randomization procedures, and dropout rates. (2) To use a daily diary to quantify type and adherence to home exercises as well as monitor pain medication, other treatment modality usage, and possible adverse events during exercise. (3) To quantify the changes in PROMs to help determine whether progression to a full-scale trial is warranted as well as to inform the choice of the most relevant and responsive PROM for a larger-scale study.
2. Methods
2.1. Trial design
The design for this study was a parallel group, single-blind, randomised pilot trial with a two-month intervention period. Similar to most behavioural interventions, the therapist was not blind to treatment assignment, but the statistical analyst and outcome assessors were blind to study condition. Participants were unaware of the differences between the two intervention groups, which was intended to match engagement and expectations of benefit across groups. Eligible participants were allocated at a 1:1 ratio with simple randomization to a movement control exercise group (control group) or to a movement control exercise group that included synchronized breathing (experimental group). Participants attended four one-on-one sessions (30-min per session, about biweekly) over the course of eight weeks to practice their assigned intervention with a clinician. These sessions occurred in a single private chiropractic clinic and were conducted by the same clinician who provided individualized feedback and guidance about the exercises. All participants were asked to practice their assigned movement control exercises (with and without synchronized breathing) every day for eight weeks. More information about the trial design is included in the publication for this protocol [23]. Trial registration number: NCT05268822. Registered on 8th February 2022, https://clinicaltrials.gov/study/NCT05268822.
2.2. Eligibility criteria
The subjects were eligible for the study if they met all inclusion and no exclusion criteria
Inclusion criteria:
-
•
Males and females aged 18–68 years;
-
•
Low back pain at least more than three days in a week and lasting more than three months;
-
•
A numerical pain scale of 4 or higher on a scale of 0 to 10 to prevent floor effects in outcome measurement [24];
-
•
Roland-Morris Disability Questionnaire score of 5 or higher on a scale of 0 to 24 to prevent floor effects in outcome measurement [25];
-
•
Physically able to perform movement control tests and provide written informed consent;
-
•
positive low back movement control tests as described by Luomajoki et al. [26, 27, 28].
Exclusion criteria:
-
•
Any history of malignancy;
-
•
Previous diagnosis of neurological disease affecting the central nervous system (MS, dementia);
-
•
Previous diagnosis of rheumatic disease (fibro-myalgia, ankylosing spondylitis/rheumatoid arthritis);
-
•
Chronic obstructive pulmonary disease or other disease that affect the lungs and cause difficulties of breathing;
-
•
Spinal surgery in the last 12 months;
-
•
Cardiac pacemaker;
-
•
Pregnancy;
-
•
Signs and symptoms of lumbar nerve root pathology during the eligibility assessment with a neurological examination at the clinic [29].
2.3. Data collection
The data collection was carried out from 16th February 2022 to 20th December 2022. The subjects were recruited from the Finnish Spine Association, pain peer support group, by authors, and other healthcare colleagues who promoted the study on their web pages and social media. Eligible subjects meeting the study criteria were invited to read the subject information sheet and consider enrolling in the study. Enrolled subjects booked eligibility assessment appointments at the first author’s clinic, where written consent for the study was given. After written consent, a neurological examination of nerve root pathology and low back movement control clinical tests were performed as described by Luomajoki et al. [31, 32]. These tests include a battery of six standardized clinical tests, which enable reliable quantification of the severity of movement control impairment from zero to six according to number of positive tests [26].
After the clinic visit, the subjects completed PROMs at home on the webpages of Nordhealth Connect, which is a Finnish company providing an electronic platform with strong electronic authentication for data collection and storage. The subjects meeting the inclusion criteria and no exclusion criteria subsequently were invited to book their first research appointment via the internet calendar booking system according to their timetables. Recruitment and data collection are described in more detail in the previous protocol publication [23].
2.4. Outcome variables
2.4.1. Demographics, pain history, and home diary
Each subject completed structured web-based pain history questions, which asked dichotomous yes/no questions to determine whether they belonged to the CNSLBP group, which was defined as having low back pain present for more than three days per week for more than three months [30, 31]. Demographic questions included age in years, height in centimetres, weight in kilograms, and educational level on a scale; 1. Elementary school 2. High school or vocational school 3. Lower university degree 4. Higher university.
Identical daily home diaries for the two-month study period were used to monitor:
-
(I)
The regularity and estimate of the amount of time spent in minutes per day on home exercises;
-
(II)
Use of pain medication (frequency of use, type, dose);
-
(III)
Other treatments or co-interventions for the treatment of pain (e.g. massage, chiropractic, other manual therapy, physiotherapy);
-
(IV)
Possible adverse events and injuries related to the movement control exercises at home.
2.4.2. Patient-reported outcome measures
Minimal detectable change (MDC) and/or minimal clinically important difference (MCID) values are included in each PROM if these are established for low back pain.
-
1.
Numerical pain rating scale (NRPS). The NRPS is a widely used subjective assessment of pain. It is an 11-point scale ranging from 0 (no pain) to 10 (worst imaginable) [32]. More than a 1.5-point change represents MDC [33] and a 2-point represents MCID in subjects with low back pain [24].
-
2.
The Roland-Morris Disability Questionnaire(RMDQ) is a 24-item questionnaire used to evaluate low back pain-related disability. The scale ranges from 0 (no disability) to 24 (maximum low back pain-related disability) [34, 35]. The MCID is estimated to be a change of 2 to 3 points compared to the baseline score for low back pain patients [36].
-
3.
The Central Sensitization Inventory (CSI) was developed as a screening tool for central sensitisation [37]. It is a two-part questionnaire in which part A contains 25 questions on central sensitization-related symptomology using a Likert scale from 0 never to 4 always. The total score ranges from 0 to 100 with higher scores indicating more severe central sensitization. Part B includes ‘No/Yes’ and ‘year diagnosed’ questions about previous diagnoses related to CS-related disorders [38]. MDC varies from 5.9 to 8.9 between different low back pain populations [39]. The CSI has been translated into Finnish and validated among a Finnish CNSLBP population [40].
-
4.
The Generalized Anxiety Disorder Assessment (GAD-7) is a self-reported measure of generalised anxiety disorder – related symptoms. The items are rated over the preceding two weeks from not at all 0 to 3 nearly every day. Thus, the total scale ranges from 0 (the most minimal anxiety) to 21 (the most severe anxiety) [41]. The MCID score for GAD-7 is 4 [42]. The GAD-7 has been adapted and validated in Finnish [43].
-
5.
The Tampa Scale of Kinesiophobia (TSK) is used for the assessment of subjective kinesiophobia (fear of movement). It has 17 statements related to kinesiophobia, with answers ranging from ‘strongly disagree’ to ‘strongly agree’. Thus, the total range is from 17 (minimal kinesiophobia) to 68 (maximal kinesiophobia) [44]. The MDC score is 8 [45] and the MCID score TSK is 5.5 [46]. The TSK has been translated into and validated in Finnish [47].
-
6.
The Pain Catastrophizing Scale (PCS) is used to assess the tendency to magnify the threat value of a pain stimulus. Thirteen items are scored on a Likert scale from 0 to 4, producing total scores from 0 (no catastrophizing thoughts) to 52 (maximum catastrophizing thoughts) [48]. The MDC score is 8 [48]. The PCS has been translated into Finnish but has not been cross-culturally validated. This study is part of its cross-cultural validation in Finnish.
-
7.
The Pain Self-Efficacy Questionnaire (PSEQ) includes 10 items to assess the self-efficacy that people in pain have in their daily activities. The scale ranges from 0 points (not at all confident) to 6 points (completely confident). The PSEQ applies to all chronic pain conditions but has mostly been validated on CNSLBP populations with MCID scores of 5.5 to 8.5 [49]. The PSEQ has been translated into and validated in the Finnish language [50].
-
8.
The Pain and Sleep Questionnaire Three-Item Index (PSQ-3) directly assessed the impact of pain on sleep during the previous week. The three items are “1. How often have you had trouble falling asleep because of pain?”, “2. How often have you been awakened by pain during the night?”,”3. How often have you been awakened by pain in the morning?”. The possible answers range on a scale from 0 indicating “never” to 10 representing “always”. The scale ranges from 0 (pain does not affect sleep) to 30 (pain has maximum effect on sleep) [51]. The PSQ-3 has been translated into Finnish and validated among a Finnish CLBP population [52].
-
9.
The first part of the EuroQol (EQ-5D-5L) is used to assess five dimensions of health-related quality of life [53] – mobility, self-care, usual activities, pain/discomfort and anxiety/depression – on a Likert scale (0 no problems, 1 slight problems, 2 moderate problems, 3 severe problems, 4 unable/extreme problems). The EQ visual analogue scale (EQ VAS) is the second part of the EQ-5D-5L [53]. As a standard value set has not yet been studied for the Finnish population, a value set from the Danish population was used to calculate the index value. This is recommended by the EuroQol EQ-5D-5L User Guide [54].
-
10.
The Well-Being in Pain Questionnaire is a self-developed 11-item questionnaire to assess the effects of pain on a subject’s biopsychosocial well-being using a Likert scale from 0 never to 4 always. Thus, total scores range from 0 (no subjective well-being in pain) to 44 (maximum subjective well-being in pain). The questionnaire is a novel measurement developed by the first author and collaborators and the PROMs validation is in process.
2.5. Interventions
Both study groups received movement control exercise protocol. Exercises were based on standardized and reliable low back movement control tests by Luomajoki et al. [26, 27, 28]. The movement control exercise goal is to train coordination of the spine, pelvis, hips and limbs to avoid ongoing nociceptive input secondary to suboptimal tissue loading [55]. The movement control exercises are intended to treat flexion, extension, and/or lateral flexion – rotational movement impairments according to test findings [28]. Exercises included 2–4 sets and 6–10 repetitions based on the therapist’s judgement of a participant’s ability to perform the exercise from exercises published in protocol. In-clinic exercise sessions occurred bi-weekly after the first visit (i.e., weeks 1, 2, 4, and 6). Movement exercises, their clinical application, and the theoretical background of maladaptive movements that contribute to CNSLBP are described in more detail in the protocol publication of this study [23] and previous movement control clinical studies [55, 56, 58].
The synchronized breathing techniques in the experimental group included instructions to breathe through one’s nose, with abdominal breathing, and synchronize breathing with each movement. These instructions are consistent with principles of multiple therapeutic yoga styles [59, 60, 61] and breathing exercises often used in healthcare settings [62]. The main practical aim of synchronized breathing with movement control exercises protocol was to keep it as easy as possible so it could be adapted to other exercise treatment protocols in the future. Detailed instructions for synchronization of the breathing cycle for each specific movement control exercise are provided in the previously published protocol [23].
2.6. Data analysis
Statistical analyses were conducted using SPSS version 25 (IBM Corp., Armonk, NY, USA). Descriptive statistical methods were used throughout this pilot study, which was based on data analysis recommendations of CONSORT 2010 statement: extension to randomised pilot and feasibility trials [63]. Data were reported as (%) or means with standard deviations (mean SD or 95% confidence interval, lower and upper bounds). Feasibility was assessed as rates of intervention completion and exercise adherence. MDC and MCID in outcome variables were calculated as within-group differences from post-intervention to baseline. Consistent with the goals and recommendations for conducting pilot feasibility studies, no inferential statistics were presented [63, 64].
3. Results
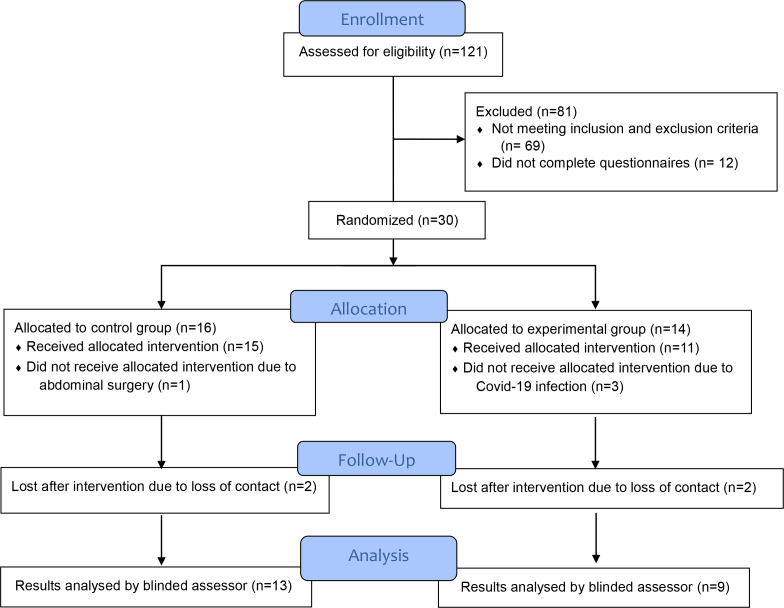
One-hundred twenty-one subjects with NSCLBP were assessed for eligibility. Thirty eligible subjects were allocated with a 1:1 ratio using simple randomisation to either movement control exercises only (control group) or movement control exercises with synchronized breathing (experimental group). Between the two groups, 16 subjects were allocated to the control group and 14 subjects were allocated to the experimental group with add-on synchronized breathing. Fourteen subjects finished (2 drop-outs) in the control group and 9 subjects (5 drop-outs) finished in the experimental group and therefore were included in the final analysis after two-month study period. Figure 1. Flow diagram.
Figure 1.
Flow diagram.
As shown in Table 1, demographics of age, gender, height, weight, body mass index, and education level were equivalent between groups. Groups were similar in analgesics usage and use of other therapies during the two-month study period. There were only minor differences in analgesic usage between groups at baseline and within study groups between the first and second months of the study. The mean days of Paracetamol and NSAIDs per subject increased by 0.4 days per month in the control group and decreased by 0.8 days per month in the experimental groups. Muscle relaxants and antidepressants per subject decreased by 1.1 days per month in the control group and by 1.5 days per month in the experimental groups. Weak opioids usage remained the same in the control group and decreased by 0.1 days in the experimental groups.
Table 1.
Baseline demographics, analgesics and other intervention usage of study groups
| Control group with movement control exercises only ( 13) | Experimental group with movement control exercises and synchronized breathing ( 9) | |
|---|---|---|
| Age | 53.5 9.7 | 50.1 11.9 |
| Gender | 8 females (57%) | 6 females (67%) |
| Height | 173 8.9 | 170.4 3.5 |
| Weight | 75.9 14.9 | 76.4 9.3 |
| Body mass index | 25.4 3.2 | 25.8 2.8 |
| Education level | 2.8 1.1 | 3.3 0.71 |
| Paracetamol and NSAIDS mean days per subject | 6.4 | 10.8 |
| Muscle relaxants and anti-depressants mean days per subject | 6.1 | 9.7 |
| Weak opioids mean days per subject | 0.2 | 0.3 |
| Other therapies | 0.6 | 0.7 |
Educational level categories: 1. Elementary school 2. High school or vocational school 3. Lower university degree 4. Higher university degree. The mean usage of analgesics per subject is calculated as total usage in days divided by subjects per group. NSAIDS non-steroidal anti-inflammatory drugs. Other therapies include physiotherapy, chiropractic or other manual therapies, and massage therapy Therapies reported the number of sessions per subject during two-month study period.
All study subjects received 8 to 14 different movement control exercises across four in-clinic sessions. Table 2 shows comparable specific types of home exercises between study groups. Mean exercise adherence per day was calculated from daily diary data and was found to be very similar in both groups. Mean exercise adherence was 16.7 minutes per day per subject for the control group and 17.1 minutes per day per subject for the experimental group. The number of positive movement control tests was similar between groups at baseline (control group; 3.7 1.3 vs. experimental group; 3.2 0.8) and post-intervention (control group; 0.4 0.1 vs. experimental group; 0.4 0.1) indicating virtually identical improvement in movement control between groups. No adverse events were reported in either group during the study.
Table 2.
Comparison of exercises chosen by the therapist across study groups
| Flexion | Extension | Lateral flexion and rotation | ||||
|---|---|---|---|---|---|---|
| A. | Waiters bow
|

|
Pelvic tilt
|

|
One leg stance with weight shift
|

|
| B. | One leg raise on standing
|

|
Lunge
|
|
Transverse lunge
|

|
| C. | Squat
|

|
All fours forwards
|

|
All fours rotation
|

|
| D. | Leg extension on sitting
|
|
All fours forward arm raise
|

|
All fours knee sideway raise
|

|
| E. | All fours backwards
|
|
All fours leg raise backwards
|
|
Prone knee hip internal rotation
|

|
| F. | All fours hip flexion
|

|
All fours alternative leg and arm raise
|

|
||
| G. | Camel exercise
|
|
Cat exercise
|
|
||
| 8. | Dead bug exercise
|

|
Prone knee flexion
|
|
||
| 9. | Kneeling forward bending
|

|
Bridge
|

|
||
1 Control group with movement control exercises only. 2 Experimental study group with movement control exercises and synchronized breathing. The percentage of subjects receiving this type of exercise during the study.
Table 3 displays mean changes and group differences from baseline to post-intervention. Changes in outcomes with established MDC and MCID criteria are indicated in Table 3. Worth noting, that both groups exceeded an MDC in pain intensity from baseline to post-intervention. Only the experimental group had an MCID in pain intensity (NRPS), disability (RMDQ), and self-efficacy (PSEQ) from baseline to post-intervention. The other largest mean differences between groups, with greater improvements in the experimental group, were for sleep quality, quality of life, and well-being where there are no established MDC and MCID values for subjects with low back pain. Both groups had relatively large decreases in pain catastrophizing following the intervention with the experimental group showing MDC. Overall, group multifactorial differences were consistent because nine out of eleven PROMs showed better results for the experimental group. The results of central sensitization and anxiety favouring the control group were very small.
Table 3.
Patient-reported outcome baseline and post-intervention changes, and mean group differences
| Control group with movement control exercises only ( 13) | Experimental group with movement control exercises and synchronized breathing ( 9) | ||||||
| Variable | Baseline | Post- intervention | Change from baseline | Baseline | Post- intervention | Change from baseline | Mean group difference |
| Pain intensity (NRPS) | 5.8 (4.9–6.7) | 4.3 (3.2–5.3) | 1.5* | 6.9 (5.7–8.0) | 4.4 (2.8–6.0) | 2.5** | 1.0 |
| Disability (RMDQ) | 8.8 (7.9–10.6) | 6.9 (4.7–9.1) | 1.9 | 10.0 (5.3–14.8) | 4.6 (2.3–6.9) | 5.4** | 3.5** |
| Central sensitization (CSI) | 38.5 (28.3–48.7) | 37.3 (28.0–46.5) | 1.2 | 40.3 (33.6–47.3) | 39.4 (31.5–47.4) | 0.9 | 0.3 |
| Anxiety (GAD-7) | 3.5 (1.9–5.1) | 3.8 (2.0–5.6) | 0.3 | 4.7 (2.5–7.0) | 4.6 (0.5–8.7) | 0.1 | 0.2 |
| Kinesiophobia (TSK) | 35.9 (30.6–41.2) | 33.2 (29.8–36.6) | 2.7 | 32.9 (24.5–41.2) | 28.9 (20.7–37.1) | 4.0 | 1.3 |
| Catastrophizing (PCS) | 16.9 (11.4–22.5) | 11.1 (8.9–13.3) | 5.8 | 21.4 (9.7–33.2) | 13.1 (1.2–25.1) | 8.3* | 2.5 |
| Self-efficacy (PSEQ) | 44.3 (38.9–49.7) | 46.9 (40.8–53.1) | 2.6 | 38.1 (23.3–53.0) | 44.4 (35.6–53.3) | 6.3** | 3.7 |
| Sleep quality (PSQ-3) | 11.0 (5.2–16.8) | 10.2 (3.9–16.4) | 0.8 | 14.7 (5.6–23.9) | 5.1 (1.3–11.6) | 9.6 | 8.8 |
| Life quality (EQ-5D-5L) | 0.65 (0.58–0.73) | 0.72 (0.67–0.78) | 0.07 | 0.68 (0.60–0.75) | 0.77 (0.70–0.85) | 0.09 | 0.02 |
| Life quality visual analogue scale (EQ VAS) | 63.1 (46.2–80) | 67.3 (52.8–81.6) | 4.2 | 58.0 (43.6–72.4) | 76.6 (64.0–89.1) | 18.6 | 14.4 |
| Well-being (WPQ) | 32.4 (27.3–37.4) | 31.0 (26.5–36.6) | 1.4 | 29.6 (22.4–37.2) | 32.6 (26.7–38.5) | 3.0 | 4.4 |
Numerical pain rating scale (NRPS). The Roland-Morris Disability Questionnaire (RMDQ), The Central Sensitization Inventory (CSI), The Generalized Anxiety Disorder Assessment (GAD-7), The Tampa Scale of Kinesiophobia (TSK), The Pain Catastrophizing Scale (PCS), The Pain Self-Efficacy Questionnaire (PSEQ), The Pain and Sleep Questionnaire Three-Item Index (PSQ-3), The EuroQol (EQ-5D-5L), The EQ visual analogue scale (EQ VAS), The Well-Being in Pain Questionnaire (WPQ). Exceeded minimal detectable change (MCD) *Exceeded minimal clinical important difference (MCID)**.
4. Discussion
This pilot study showed that previously published feasibility criteria [32] were met. The intervention adherence rates and daily exercise time were equivalent across both groups, which suggests that the addition of synchronized breathing techniques with the movement control exercises was acceptable and did not add a significant participant burden. Eligibility criteria were neither too inclusive nor restrictive to recruit subjects in a reasonable time frame. We achieved recruitment target of 30 study subjects in less than one year after screening 121 potentially eligible subjects. Simple randomisation was feasible but resulted in an error and slightly unbalanced study groups. All subjects completed and returned the daily diary assessments. The dropout rate in this study was 27% for the control group and 36% for the experimental group. Three subjects dropped out in the experimental group due to a COVID-19 diagnosis and one subject dropped out in the control group due to an unexpected surgery. In both groups, two subjects were lost after the study period due to loss of contact. Naturally, the dropout rate in this smaller-scale study was more sensitive to random incidents and does not suggest that people withdrew because of the intervention differences (e.g., because synchronized breathing was too difficult to comprehend or it included other significant burden).
This pilot study was not powered to test for differences in the efficacy between groups, however, the preliminary findings provide information regarding the plausibility of clinically meaningful effects following each intervention [65]. The largest group differences favouring the experimental group were in pain intensity, disability, catastrophizing, sleep quality, self-efficacy, and health-related quality of life. Interestingly, these include all core PROMs of CNSLBP [4]: pain intensity, disability, and quality of life. The group differences that were observed were likely due directly to the synchronized breathing, because movement control exercises and adherence, and contextual factors related to the therapist, clinical setting, analgesic usage, or participation in other interventions were matched across both groups. To support findings in some extent, improvements in the movement control exercises alone are consistent with a recent meta-analysis showing equivalent effects on pain intensity and disability for those with CNSLBP [7].
Synchronized breathing protocol is feasible and easily accessible and could be incorporated into these other exercise therapies with little extra training for therapists, without extra equipment, additional costs, or increased risk of injury for subjects.
The promising findings of this pilot study encourage the development of larger-scale studies that incorporate synchronized breathing techniques add-on with exercise in the treatment of CNSLBP. Like any small-scale pilot study, replication of findings related to multifactorial outcome measures within and between groups remains to be answered in future larger-scale studies with a variety of pain populations and different study designs.
4.1. Strengths and limitations
The major strengths of this study were: (i) Easy-to-implement synchronized breathing with movement evidence-based exercises, (ii) well-documented identical movement control assessment and exercise programs, (iii) detailed study of demographics, exercise content, adherence, safety, and analgesics and other therapy usage without contextual differences in clinic or therapist. A major limitation is the lack of intervention blinding for the therapist and subjects, which is not generally possible in exercise intervention studies [66].
5. Conclusions
This pilot study met feasibility criteria in terms of implementing the study protocol with satisfactory participant recruitment and retention rates. Home exercise adherence was nearly identical between the groups without any adverse events. Preliminary efficacy findings related to pain intensity, disability, and self-efficacy exceeded minimal clinically important difference. Outcomes of sleep quality, quality of life, and well-being where there are no published minimal clinically important difference values for subjects with CNSLBP were also promising. These findings taken together support the progression to a full-scale study.
Author contributions
JM, VL, OA, and HL designed the study. JM collected data. JM, VL, LG performed statistical analyses with assistance from HL. JM drafted the first manuscript. VL, HL, LG, SP, and OA provided input on the interpretation of the results and revised the manuscript. VL provided supervision of the ethical approval of the study. All authors read and approved the final version of the paper.
Data availability
Data is available from the corresponding author upon written request.
Ethical approval
Ethical approval for the study was obtained from the Research Ethics Committee of the Northern Savo Hospital District with identification number 2131/2022 on 31st January 2022.
Funding
This work was supported by the Chiropractic Knowledge Hub ECCRE under Grant 48-2021-FIN/JM. The funder did not have a role in study design, analysis, or manuscript drafting.
Informed consent
All enrolled subjects provided written consent prior the study.
Acknowledgments
The authors would like to thank the study subjects for their time and effort. The authors also thank Kirsi Töyrylä and Milla Suomi from Selkäliitto Ry as well as the chronic pain peer group Kipumatkalla moderators Sirpa Tahko and Päivi Vaarakallio for their invaluable contributions to data collection. Finally, we would like to thank Aleksi Reito for his contributions to data analysis.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- [1]. Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. Lancet. 2018; 391(10137): 2356-67. [DOI] [PubMed] [Google Scholar]
- [2]. Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017; 389(10070): 736-47. [DOI] [PubMed] [Google Scholar]
- [3]. Chou R, Qaseem A, Owens DK, Shekelle P, Physicians CGCotACo. Diagnostic imaging for low back pain: advice for high-value health care from the American College of Physicians. Ann Intern Med. 2011; 154(3): 181-9. [DOI] [PubMed] [Google Scholar]
- [4]. Chiarotto A, Boers M, Deyo RA, Buchbinder R, Corbin TP, Costa LOP, et al. Core outcome measurement instruments for clinical trials in nonspecific low back pain. Pain. 2018; 159(3): 481-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5]. Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018; 391(10137): 2368-83. [DOI] [PubMed] [Google Scholar]
- [6]. Qaseem A, Wilt TJ, McLean RM, Forciea MA, Physicians CGCotACo. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2017; 166(7): 514-30. [DOI] [PubMed] [Google Scholar]
- [7]. Luomajoki HA, Bonet Beltran MB, Careddu S, Bauer CM. Effectiveness of movement control exercise on patients with non-specific low back pain and movement control impairment: A systematic review and meta-analysis. Musculoskelet Sci Pract. 2018; 36: 1-11. [DOI] [PubMed] [Google Scholar]
- [8]. Buchbinder R, Underwood M, Hartvigsen J, Maher CG. The Lancet Series call to action to reduce low value care for low back pain: an update. Pain. 2020; 161(Suppl 1): S57-S64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9]. Fernández-Rodríguez R, Álvarez-Bueno C, Cavero-Redondo I, Torres-Costoso A, Pozuelo-Carrascosa DP, Reina-Gutiérrez S, et al. Best Exercise Options for Reducing Pain and Disability in Adults With Chronic Low Back Pain: Pilates, Strength, Core-Based, and Mind-Body. A Network Meta-analysis. J Orthop Sports Phys Ther. 2022; 52(8): 505-21. [DOI] [PubMed] [Google Scholar]
- [10]. Hayden JA, Ellis J, Ogilvie R, Stewart SA, Bagg MK, Stanojevic S, et al. Some types of exercise are more effective than others in people with chronic low back pain: a network meta-analysis. J Physiother. 2021; 67(4): 252-62. [DOI] [PubMed] [Google Scholar]
- [11]. Büssing A, Ostermann T, Lüdtke R, Michalsen A. Effects of yoga interventions on pain and pain-associated disability: a meta-analysis. J Pain. 2012; 13(1): 1-9. [DOI] [PubMed] [Google Scholar]
- [12]. Owen PJ, Miller CT, Mundell NL, Verswijveren SJJM, Tagliaferri SD, Brisby H, et al. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br J Sports Med. 2020; 54(21): 1279-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13]. Ross A, Thomas S. The health benefits of yoga and exercise: a review of comparison studies. J Altern Complement Med. 2010; 16(1): 3-12. [DOI] [PubMed] [Google Scholar]
- [14]. Govindaraj R, Karmani S, Varambally S, Gangadhar BN. Yoga and physical exercise – a review and comparison. Int Rev Psychiatry. 2016; 28(3): 242-53. [DOI] [PubMed] [Google Scholar]
- [15]. Cramer H, Anheyer D, Lauche R, Dobos G. A systematic review of yoga for major depressive disorder. J Affect Disord. 2017; 213: 70-7. [DOI] [PubMed] [Google Scholar]
- [16]. Cramer H, Lauche R, Anheyer D, Pilkington K, de Manincor M, Dobos G, et al. Yoga for anxiety: A systematic review and meta-analysis of randomized controlled trials. Depress Anxiety. 2018; 35(9): 830-43. [DOI] [PubMed] [Google Scholar]
- [17]. Pascoe MC, Bauer IE. A systematic review of randomised control trials on the effects of yoga on stress measures and mood. J Psychiatr Res. 2015; 68: 270-82. [DOI] [PubMed] [Google Scholar]
- [18]. Pascoe MC, Thompson DR, Ski CF. Yoga, mindfulness-based stress reduction and stress-related physiological measures: A meta-analysis. Psychoneuroendocrinology. 2017; 86: 152-68. [DOI] [PubMed] [Google Scholar]
- [19]. Elwy AR, Groessl EJ, Eisen SV, Riley KE, Maiya M, Lee JP, et al. A systematic scoping review of yoga intervention components and study quality. Am J Prev Med. 2014; 47(2): 220-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20]. Lin HT, Hung WC, Hung JL, Wu PS, Liaw LJ, Chang JH. Effects of pilates on patients with chronic non-specific low back pain: a systematic review. J Phys Ther Sci. 2016; 28(10): 2961-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21]. Wong CM, Rugg B, Geere JA. The effects of Pilates exercise in comparison to other forms of exercise on pain and disability in individuals with chronic non-specific low back pain: A systematic review with meta-analysis. Musculoskeletal Care. 2023; 21(1): 78-96. [DOI] [PubMed] [Google Scholar]
- [22]. Rossettini G, Carlino E, Testa M. Clinical relevance of contextual factors as triggers of placebo and nocebo effects in musculoskeletal pain. BMC Musculoskelet Disord. 2018; 19(1): 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23]. Mikkonen J, Luomajoki H, Airaksinen O, Goubert L, Leinonen V. Protocol of identical exercise programs with and without specific breathing techniques for the treatment of chronic non-specific low back pain: randomized feasibility trial with two-month follow-up. BMC Musculoskelet Disord. 2023; 24(1): 354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24]. Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976). 2005; 30(11): 1331-4. [DOI] [PubMed] [Google Scholar]
- [25]. Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine (Phila Pa 1976). 1983; 8(2): 141-4. [DOI] [PubMed] [Google Scholar]
- [26]. Luomajoki H, Kool J, de Bruin ED, Airaksinen O. Reliability of movement control tests in the lumbar spine. BMC Musculoskelet Disord. 2007; 8: 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27]. Luomajoki H, Kool J, de Bruin ED, Airaksinen O. Movement control tests of the low back; evaluation of the difference between patients with low back pain and healthy controls. BMC Musculoskelet Disord. 2008; 9: 170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28]. Meier R, Emch C, Gross-Wolf C, Pfeiffer F, Meichtry A, Schmid A, et al. Sensorimotor and body perception assessments of nonspecific chronic low back pain: a cross-sectional study. BMC Musculoskelet Disord. 2021; 22(1): 391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29]. Biller J, Gruener G, Brazis PW. DeMyer’s The neurologic examination: a programmed text. Seventh edition. ed. New York: McGraw-Hill Education; 2017. xxiv, 631 pages p. [Google Scholar]
- [30]. Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014; 73(6): 968-74. [DOI] [PubMed] [Google Scholar]
- [31]. Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ. 2006; 332(7555): 1430-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32]. Haefeli M, Elfering A. Pain assessment. Eur Spine J. 2006; 15(Suppl 1): S17-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33]. Kovacs FM, Abraira V, Royuela A, Corcoll J, Alegre L, Tomás M, et al. Minimum detectable and minimal clinically important changes for pain in patients with nonspecific neck pain. BMC Musculoskelet Disord. 2008; 9: 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34]. Stevens ML, Lin CC, Maher CG. The Roland Morris Disability Questionnaire. J Physiother. 2016; 62(2): 116. [DOI] [PubMed] [Google Scholar]
- [35]. Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine (Phila Pa 1976). 2000; 25(24): 3115-24. [DOI] [PubMed] [Google Scholar]
- [36]. Bombardier C, Hayden J, Beaton DE. Minimal clinically important difference. Low back pain: outcome measures. J Rheumatol. 2001; 28(2): 431-8. [PubMed] [Google Scholar]
- [37]. Mayer TG, Neblett R, Cohen H, Howard KJ, Choi YH, Williams MJ, et al. The development and psychometric validation of the central sensitization inventory. Pain Pract. 2012; 12(4): 276-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38]. Neblett R. The central sensitization inventory: A user’s manual. J Appl Behav Res. 2018. [Google Scholar]
- [39]. Sharma S, Jha J, Pathak A, Neblett R. Translation, cross-cultural adaptation, and measurement properties of the Nepali version of the central sensitization inventory (CSI). BMC Neurol. 2020; 20(1): 286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40]. Mikkonen J, Luomajoki H, Airaksinen O, Neblett R, Selander T, Leinonen V. Cross-cultural adaptation and validation of the Finnish version of the central sensitization inventory and its relationship with dizziness and postural control. BMC Neurol. 2021; 21(1): 141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41]. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006; 166(10): 1092-7. [DOI] [PubMed] [Google Scholar]
- [42]. Toussaint A, Hüsing P, Gumz A, Wingenfeld K, Härter M, Schramm E, et al. Sensitivity to change and minimal clinically important difference of the 7-item Generalized Anxiety Disorder Questionnaire (GAD-7). J Affect Disord. 2020; 265: 395-401. [DOI] [PubMed] [Google Scholar]
- [43]. Kujanpä"a T, Ylisaukko-Oja T, Jokelainen J, Hirsikangas S, Kanste O, Kyngäs H, et al. Prevalence of anxiety disorders among Finnish primary care high utilizers and validation of Finnish translation of GAD-7 and GAD-2 screening tools. Scand J Prim Health Care. 2014; 32(2): 78-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44]. Miller RP, Kori SH, Todd DD. The Tampa Scale. A Measure of Kinesiophobia. The Clinical Journal of Pain. 1991; 7(1). [Google Scholar]
- [45]. Lüning Bergsten C, Lundberg M, Lindberg P, Elfving B. Change in kinesiophobia and its relation to activity limitation after multidisciplinary rehabilitation in patients with chronic back pain. Disabil Rehabil. 2012; 34(10): 852-8. [DOI] [PubMed] [Google Scholar]
- [46]. Monticone M, Ambrosini E, Rocca B, Foti C, Ferrante S. Responsiveness of the Tampa Scale of Kinesiophobia in Italian subjects with chronic low back pain undergoing motor and cognitive rehabilitation. Eur Spine J. 2016; 25(9): 2882-8. [DOI] [PubMed] [Google Scholar]
- [47]. Koho P, Borodulin K, Kautiainen H, Kujala U, Pohjolainen T, Hurri H. Finnish version of the Tampa Scale of Kinesiophobia: Reference values in the Finnish general population and associations with leisure-time physical activity. J Rehabil Med. 2015; 47(3): 249-55. [DOI] [PubMed] [Google Scholar]
- [48]. Osman A, Barrios FX, Kopper BA, Hauptmann W, Jones J, O’Neill E. Factor structure, reliability, and validity of the Pain Catastrophizing Scale. J Behav Med. 1997; 20(6): 589-605. [DOI] [PubMed] [Google Scholar]
- [49]. Dubé MO, Langevin P, Roy JS. Measurement properties of the Pain Self-Efficacy Questionnaire in populations with musculoskeletal disorders: a systematic review. Pain Rep. 2021; 6(4): e972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50]. Karkkola P, Kuittinen M. Kipupystyvyyskyselyn ominaisuudet tuki-ja liikuntaelinkuntoutujilla. Psykologi. 2007; 52: 4. [Google Scholar]
- [51]. Ayearst L, Harsanyi Z, Michalko KJ. The Pain and Sleep Questionnaire three-item index (PSQ-3): a reliable and valid measure of the impact of pain on sleep in chronic nonmalignant pain of various etiologies. Pain Res Manag. 2012; 17(4): 281-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52]. Mikkonen J, Leinonen V, Luomajoki H, Kaski D, Kupari S, Tarvainen M, et al. Cross-Cultural Adaptation, Reliability, and Psychophysical Validation of the Pain and Sleep Questionnaire Three-Item Index in Finnish. Journal of Clinical Medicine. 2021; 10(21): 4887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53]. Janssen MF, Pickard AS, Golicki D, Gudex C, Niewada M, Scalone L, et al. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual Life Res. 2013; 22(7): 1717-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54]. van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. 2012; 15(5): 708-15. [DOI] [PubMed] [Google Scholar]
- [55]. O’Sullivan P. Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism. Man Ther. 2005; 10(4): 242-55. [DOI] [PubMed] [Google Scholar]
- [56]. Lehtola V, Luomajoki H, Leinonen V, Gibbons S, Airaksinen O. Sub-classification based specific movement control exercises are superior to general exercise in sub-acute low back pain when both are combined with manual therapy: A randomized controlled trial. BMC Musculoskelet Disord. 2016; 17: 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57]. Lehtola V, Luomajoki H, Leinonen V, Gibbons S, Airaksinen O. Efficacy of movement control exercises versus general exercises on recurrent sub-acute nonspecific low back pain in a sub-group of patients with movement control dysfunction. Protocol of a randomized controlled trial. BMC Musculoskelet Disord. 2012; 13: 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58]. Saner J, Kool J, Sieben JM, Luomajoki H, Bastiaenen CH, de Bie RA. A tailored exercise program versus general exercise for a subgroup of patients with low back pain and movement control impairment: A randomised controlled trial with one-year follow-up. Man Ther. 2015; 20(5): 672-9. [DOI] [PubMed] [Google Scholar]
- [59]. Mohan AG, Mohan I. Yoga therapy: a guide to the therapeutic use of yoga and ayurveda for health and fitness. 1st ed. Boston: Shambhala Publications; 2004. vii, 218 p. p. [Google Scholar]
- [60]. TKV D. The Heart of Yoga. 1st Edition ed. Rochester, Vermont: Inner Traditions International, 1999. [Google Scholar]
- [61]. Farhi D. The breathing book: good health and vitality through essential breath work. 1st ed. New York: Henry Holt; 1996. xvi, 238 p. p. [Google Scholar]
- [62]. Chaitow La, Gilbert Ca, Bradley Da. Recognizing and treating breathing disorders: a multidisciplinary approach. [Google Scholar]
- [63]. Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ. 2016; 355: i5239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64]. Thabane L, Ma J, Chu R, Cheng J, Ismaila A, Rios LP, et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010; 10: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65]. Freedland KE. Pilot trials in health-related behavioral intervention research: Problems, solutions, and recommendations. Health Psychol. 2020; 39(10): 851-62. [DOI] [PubMed] [Google Scholar]
- [66]. Hohenschurz-Schmidt D, Draper-Rodi J, Vase L, Scott W, McGregor A, Soliman N, et al. Blinding and sham control methods in trials of physical, psychological, and self-management interventions for pain (article I): a systematic review and description of methods. Pain. 2023; 164(3): 469-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is available from the corresponding author upon written request.