Abstract
Patient: Female, 55-year-old
Final Diagnosis: Prolapse of sigmoid colon epiploica through vagina
Symptoms: Vaginal mass
Clinical Procedure: —
Specialty: Pathology
Objective:
Rare disease
Background:
Hysterectomy is a gynecological procedure that can lead to complications arising from structural changes incurred during the surgical process. Vaginal nodules may appear at the vaginal cuff after hysterectomy, which could be indicative of recurring cancer, endometriosis, or formation of fistulae or granulation tissue. In rare instances, abdominal organ prolapse occurs after vaginal cuff dehiscence. Prolapse of the terminal ileum is the most common type of prolapse from vaginal cuff dehiscence, but prolapsed epiploica of colon after hysterectomy occurs in rare instances. Epiploic appendages are a type of fatty tissue attached to the colonic surface that can become inflamed or necrotic and detach from the colon. The purpose of this report is to describe a rare case of prolapsed epiploica of colon at the vaginal cuff.
Case Report:
A 55-year-old woman who had robot-assisted laparoscopic hysterectomy for endometrioid carcinoma presented with a vaginal polyp 2 months after surgery. Histological analysis of the excised polyp revealed adipose tissue with fat necrosis and calcification, indicative of prolapsed epiploica of colon. This is the first report of post-hysterectomy epiploica of colon at the vaginal cuff not associated with obvious dehiscence.
Conclusions:
This case highlights the importance of thorough histological analysis of excised vaginal nodules and consideration of prolapsed epiploica of colon in the differential diagnoses in addition to benign and malignant vaginal neoplasms.
Key words: Hysterectomy, Prolapse, Vaginal Neoplasms, Colposcopy
Introduction
Epiploic appendages, also referred to as appendices epiploicae, consist of pedunculated fat tissue attached to the colonic surface, most commonly on the taeniae of the cecum and sigmoid colon [1]. Typical appendices epiploicae appear as lobulated masses of pericolic fat, usually around 0.5 to 5 cm long. These structures generally remain attached to the peritoneum, but in some instances, they become inflamed or necrotic and detach from the colon to become free-floating bodies [2]. In rare instances, prolapse of the epiploica occurs as a complication of gynecologic surgical procedures, such as hysterectomy. Epiploica appendagitis can be completely asymptomatic or can present with acute abdominal pain or vaginal prolapse. It can clinically mimic acute appendicitis, acute diverticulitis, or pelvic inflammatory disease [3,4]. Diagnosis is based on clinical examination, imaging studies, serology, colposcopic examination, and biopsy, depending on the patient’s clinical presentation, with management being decided accordingly [5]. The purpose of this case study is to report a rare presentation of prolapsed epipoloica of colon with emphasis on the clinical presentation, diagnostic pitfalls, and management, with a literature review.
Case Report
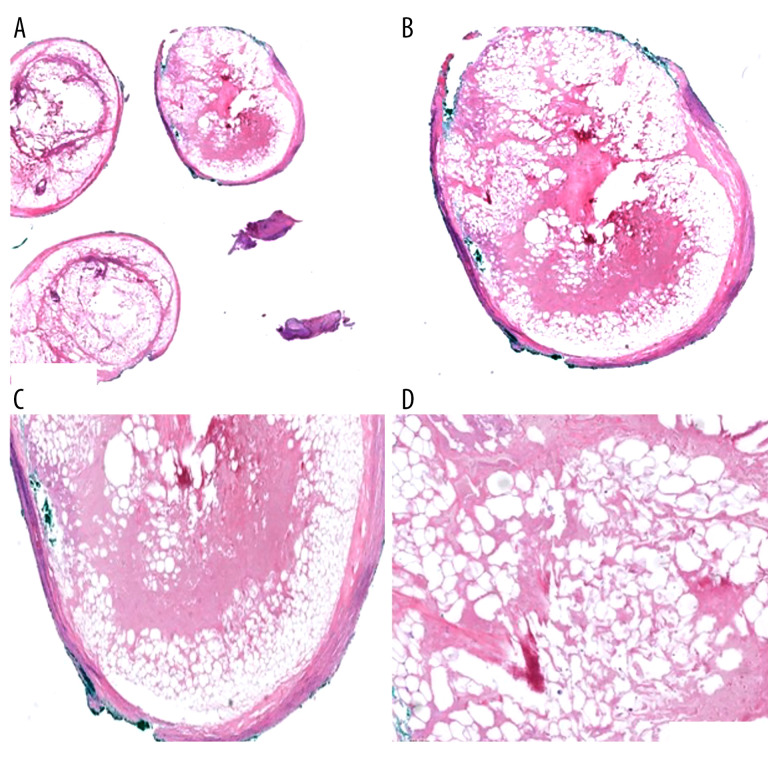
A 55-year-old woman G2P2 with BMI 28.8 and a history of diabetes mellitus and Addison’s disease presented to the gynecologist with several weeks of postmenopausal bleeding. She was vitally stable and pelvic ultrasound revealed endometrial thickening. The subsequent endometrial biopsy showed endometrial carcinoma. She underwent robot-assisted total laparoscopic hysterectomy and bilateral salpingo-oophorectomy with pelvic sentinel lymph node dissection for surgical staging. The surgical procedure was uncomplicated and was not technically challenging. The vagina was closed using a 12 inch 2-0 Stratafix suture. The stich was anchored at the right vaginal apex and run continuously to the contralateral apex. Once the entire length of vagina was closed, the suture was then run back to the right vaginal apex to complete a 2-layered closure with a single suture. The patient did well on postoperative day (POD) 0 and was then sent home on POD 1. Pathological analysis revealed mixed high-grade carcinoma of the endometrium involving the inner half of the myometrium, with extensive lymphovascular invasion and a MELF (microcystic elongated and fragmented) pattern of invasion. Lymph nodes were negative for metastatic carcinoma. Immunohistochemical staining for mismatch repair proteins revealed retained expression of all 4 proteins included in the assay (MLH1, PMS2, MSH2, and MSH6). She was asymptomatic at her 2-month postoperative follow-up. However, the colposcopic examination showed a small vaginal polyp. The imaging studies were negative for metastatic disease. Considering the patient’s recent carcinoma history, tumor recurrence was suspected, and the polyp was excised. Gross examination showed 3 separate 4–11 mm fragments, including a well-circumscribed 7 mm nodule. Microscopic examination showed fragments of inflamed squamous mucosa and detached fragments of well-circumscribed adipose tissue with fat necrosis and calcification surrounded by inflamed and fibrotic tissue indicative of a prolapsed epiploica of colon (Figure 1A–1D). The patient recovered from the procedure well with no postoperative complications. Informed consent was obtained by the patient’s treating physician. After 1.5 years, the patient is disease-free and was doing well at her most recent follow-up examination.
Figure 1.
Histologic sections of the colonic epiploica. Microscopic examination shows well-circumscribed adipose tissue with fibrotic wall (A, B) demonstrating fat necrosis (C, D). Hematoxylin and eosin, magnification in (A) 2×, (B) 4×, (C) 10×, (D) 20×.
Discussion
Hysterectomy is a commonly performed gynecologic surgical procedure, and a number of complications may arise from the structural changes incurred from surgery. One such complication of hysterectomy is organ prolapse through the vaginal cuff. The vaginal cuff comprises of the reconstructed pubocervical fascia, vaginal epithelium, and uterosacral ligament complex. Vaginal cuff dehiscence is when the anterior and posterior edges of the vaginal cuff separate, and evisceration describes prolapse of abdominal organs through the cuff defect [6]. The incidence of vaginal cuff dehiscence is reported to be 0.8% after laparoscopic hysterectomy and up to 2.3% after robot-assisted hysterectomy [7]. The most common organ to eviscerate through the vagina after hysterectomy is the terminal ileum, but evisceration of other organs such as the fallopian tube, omentum, colon, appendix, and appendix epiploica have also been reported [8–11].
The differential diagnoses for vaginal cuff nodules include granulation tissue, fibroepithelial polyp, endometriosis, vaginal adenosis, leiomyoma, vesicovaginal, and ureterovaginal fistulae, and importantly, primary or metastatic carcinoma [12,13]. Another less common diagnostic consideration is organ prolapse, such as prolapsed appendage epiploica, which may result from inadequate operative technique or difficulties encountered during closure of the vaginal cuff [14].
Morphologic examination of prolapsed epiploica shows well-circumscribed adipose tissue with fat necrosis and inflammation. The surgical site granulation tissue consists of small newly-formed blood vessels, inflammation, and fibroblasts. Endometriosis is characterized by the presence of endometrial gland, endometrial stroma, and hemosiderin-laden macrophages, while vaginal adenosis is characterized by the presence of benign endocervical type glands in the vaginal lamina propria. The fibroepithelial polyp has variably cellular stroma extending up to epithelium, with characteristic stellate and multinucleated stromal cells [15].
Few cases of vaginally prolapsed epiploica of colon after hysterectomy have been reported. One case of prolapsed epiploica of the bowel reported by Chen et al in 2020 described a patient who presented with a 4 cm protruding vaginal mass with vaginal cuff dehiscence and bilateral hydronephrosis after robotic hysterectomy. The patient had histologic findings similar to our patient’s, including predominance of adipose tissue and substantial inflammation [16]. As with our patient, the authors also initially suspected cancer recurrence, which is logical within the context of surgery for tumor removal. Askari et al reported a patient with prolapsed epiploica of sigmoid colon through the dehisced vaginal cuff, but after total laparoscopic hysterectomy rather than robot-assisted hysterectomy [17].
These reports suggest that regardless of surgical approach, post-hysterectomy nodules associated with the vaginal cuff, either with dehiscence as in the previously reported cases or without dehiscence as in our patient’s case, could be prolapsed epiploica of the colon. Although these complications are rare, physicians should be aware of this possibility while still maintaining vigilance for possible cancer recurrence. Close attention to thorough histological analysis is key for differentiating prolapsed epiploica from other more serious issues such as tumor recurrence.
Although our patient had prolapsed epiploica of colon in the absence of clinically apparent vaginal cuff dehiscence, vaginal cuff defects may occur after hysterectomy and can lead to serious complications. The possible causes of prolapse through the vaginal cuff include complete vaginal dehiscence, small partial dehiscence, and inadvertent strangulation of the epiploica during vaginal closure. The major risk factors for vaginal cuff dehiscence include vaginal atrophy, radiation therapy, postoperative infection, steroid use, connective tissue disease, diabetes, and early resumption of sexual activity after surgery. However, most cuff separations occur without any identifiable predisposing conditions [18]. However, as our patient’s case illustrates, the vaginal cuff may be associated with complications in the absence of clinically obvious dehiscence, and organ prolapse such as prolapsed epiploic appendages should be considered in the differential diagnosis of vaginal cuff nodules after gynecologic procedures, with prompt tissue repair and monitoring for infection and other serious sequelae.
Conclusions
This rare occurrence of prolapsed epiploica of the colon is an unusual non-neoplastic post-hysterectomy complication that may be considered in the differential diagnosis, in addition to other types of tissue abnormalities associated with vaginal nodules that arise after hysterectomy.
Footnotes
Publisher’s note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher
Institution Where Work Was Done
Henry Ford Hospital, Detroit, MI, USA.
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References:
- 1.Giannis D, Matenoglou E, Sidiropoulou MS, et al. Epiploic appendagitis: Pathogenesis, clinical findings and imaging clues of a misdiagnosed mimicker. Ann Transl Med. 2019;7(24):814. doi: 10.21037/atm.2019.12.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sand M, Gelos M, Bechara FG, et al. Epiploic appendagitis – clinical characteristics of an uncommon surgical diagnosis. BMC Surg. 2007;7:11. doi: 10.1186/1471-2482-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lien WC, Lai TI, Lin GS, et al. Epiploic appendagitis mimicking acute cholecystitis. Am J Emerg Med. 2004;22(6):507–8. doi: 10.1016/j.ajem.2004.07.018. [DOI] [PubMed] [Google Scholar]
- 4.Singh AK, Gervais DA, Hahn PF, et al. Acute epiploic appendagitis and its mimics. Radiographics. 2005;25(6):1521–34. doi: 10.1148/rg.256055030. [DOI] [PubMed] [Google Scholar]
- 5.Suresh Kumar VC, Mani KK, Alwakkaa H, Shina J. Epiploic appendagitis: An often-misdiagnosed cause of acute abdomen. Case Rep Gastroenterol. 2020;13(3):364–68. doi: 10.1159/000502683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nezhat C, Burns MK, Wood M, et al. Vaginal cuff dehiscence and evisceration: A review. Obstet Gynecol. 2018;132(4):972–85. doi: 10.1097/AOG.0000000000002852. [DOI] [PubMed] [Google Scholar]
- 7.Hur HC, Lightfoot M, McMillin MG, Kho KA. Vaginal cuff dehiscence and evisceration: a review of the literature. Curr Opin Obstet Gynecol. 2016;28(4):297–303. doi: 10.1097/GCO.0000000000000294. [DOI] [PubMed] [Google Scholar]
- 8.Ouldamer L, Caille A, Body G. Fallopian tube prolapse after hysterectomy: A systematic review. PLoS One. 2013;8(10):e76543. doi: 10.1371/journal.pone.0076543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thomopoulos T, Zufferey G. Totally laparoscopic treatment of vaginal cuff dehiscence: A case report and systematic literature review. Int J Surg Case Rep. 2016;25:79–82. doi: 10.1016/j.ijscr.2016.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cardosi RJ, Hoffman MS, Roberts WS, Spellacy WN. Vaginal evisceration after hysterectomy in premenopausal women. Obstet Gynecol. 1999;94(5 Part 2):859. doi: 10.1016/s0029-7844(99)00530-x. [DOI] [PubMed] [Google Scholar]
- 11.Lane D. Strangulated appendix epiploica presenting per vaginam. Med J Aust. 1965;2(17):712. doi: 10.5694/j.1326-5377.1965.tb19182.x. [DOI] [PubMed] [Google Scholar]
- 12.Halvorsen TB, Johannesen E. Fibroepithelial polyps of the vagina: Are they old granulation tissue polyps? J Clin Pathol. 1992;45(3):235–40. doi: 10.1136/jcp.45.3.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ho YJ, Li PC, Cheng CH, Ding DC. Pelvic myoma arising from vaginal cuff after hysterectomy: A case report and literature review. Tzu Chi Med J. 2020;32(4):398–400. doi: 10.4103/tcmj.tcmj_169_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eoh KJ, Lee YJ, Nam EJ, et al. Vaginal cuff dehiscence and a guideline to determine treatment strategy. J Pers Med. 2023;13(6):890. doi: 10.3390/jpm13060890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ogura N, Inagaki M, Yasuda R, et al. A vaginal fibroepithelial stromal polyp: A case report with magnetic resonance images. BJR Case Rep. 2022;8(2):20210189. doi: 10.1259/bjrcr.20210189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen HY, Sheu BC, Chang WC. Prolapsed epiploica of bowel after robotic hysterectomy: A case report. Ann Med Surg. 2020;60:146–48. doi: 10.1016/j.amsu.2020.10.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Askari R, Ravangard SF, Ghomi A. Prolapsed epiploica of the sigmoid colon after total laparoscopic hysterectomy. JSLS. 2011;15(2):252. doi: 10.4293/108680811X13071180406718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uccella S, Ceccaroni M, Cromi A, et al. Vaginal cuff dehiscence in a series of 12,398 hysterectomies: Effect of different types of colpotomy and vaginal closure. Obstet Gynecol. 2012;120(3):516–23. doi: 10.1097/AOG.0b013e318264f848. [DOI] [PubMed] [Google Scholar]