Abstract
The pelvic floor and its associated disorders are a unique and often overlooked aspect of women's rugby. This review discusses relevant biopsychosocial considerations specific to the pelvic floor and rugby. Pelvic floor disorders can present at any time across the female lifespan but are more prevalent during pregnancy and postpartum. This is due to the substantial physiological and anatomical changes experienced during pregnancy and vaginal childbirth. Consequently, pelvic floor disorders can impact a player's ability to perform, maintain engagement with, or return to, rugby due to symptoms. Players need to be informed, supported, and guided through focused pelvic floor muscle training to condition the muscles and ‘ready’ them for the varied demands of rugby. Health and fitness professionals should understand the risk of pelvic floor disorders across the female lifespan and screen players for symptoms when supporting them to maintain or return to rugby. Rugby players who are symptomatic of pelvic floor disorders should be signposted to specialist services and/or resources to manage their symptoms. Once engaging in rugby training, ongoing evaluation of player load tolerance and implementation of individualized strategies to support managing rugby‐related loads to the pelvic floor should be considered. Finally, surveillance and research focusing specifically on rugby players and pelvic floor function are needed.
Keywords: female athlete, genital hiatus, incontinence, lifespan, perinatal, return to sport
Highlights
High force‐related activities, such as rugby, challenge the pelvic floor muscles (PFMs) and can increase a player's susceptibility to pelvic floor disorders (e.g., stress urinary incontinence, feeling a bulge inside or outside the vagina)
Pelvic floor disorders can present at any time across the female lifespan, with pregnancy and childbirth being two commonly reported risk factors for such disorders
Predisposing (genetics), inciting (pregnancy and vaginal childbirth) and intervening (lifestyle, aging) factors likely influence pelvic floor load tolerance
PFM training has level 1 evidence to be a first line treatment for urinary incontinence and pelvic organ prolapse in the general female population. We encourage PFM training to be incorporated into rugby training programmes across all ages, levels and roles regardless of whether pelvic floor disorder symptoms are present or not
1. INTRODUCTION
The pelvic floor is a unique and often overlooked characteristic of women's rugby. Taking a cupuliform shape, the pelvic floor muscles (PFMs) span the outlet at the base of the pelvis (Bordoni et al., 2022; Herschorn, 2004). Their role is multifactorial and includes (i) maintaining continence (bladder and bowel); (ii) facilitating excretion (bladder and bowel); (iii) supporting the pelvic organs and; and (iv) enabling sexual function (Donnelly et al., 2023). Compromise to any of these roles may lead to signs and symptoms of pelvic floor disorders, also referred to as pelvic floor dysfunction, (PFD) such as incontinence (bladder or bowel), pelvic organ prolapse or pain (Donnelly et al., 2023; NICE, 2021). Symptoms of PFD can occur at any time across the female lifespan and are attributed to combinations of anatomical, physiological, genetic, lifestyle and reproductive factors, rather than a single cause (Delancey et al., 2008). For example, the perinatal period (pregnancy and postpartum) is one factor that increases a woman's predisposition to PFD (Delancey et al., 2008; Donnelly et al., 2023; McCarthy‐Ryan et al., 2024; NICE, 2021). To reduce the risk of provoking, or worsening, symptoms of PFD, women's rugby players must be pelvic floor ‘ready’ for training and performance. It is therefore essential that all supporting professionals, regardless of health or fitness background, are aware of the importance of including focused PFM training within strength and conditioning programing, as well as screening for PFD and signposting to specialist services.
The aim of this review is to discuss the importance of the PFMs across the lifespan of women's rugby players using a biopsychosocial‐informed approach. First, we outline the PFM anatomy, physiology and functioning during rugby. Then, we outline the prevalence and risk of PFD across the female lifespan. We cover key changes to the PFMs during pregnancy, childbirth, postpartum and advancing age along with identifying signs and symptoms of PFD. The final sections will discuss rugby‐specific PFM load tolerance and conditioning, alongside strategies and adjuncts to aid PFD management and optimize successful female engagement in rugby.
2. THE FEMALE PELVIC FLOOR COMPLEX
There are many distinct differences in male and female anatomy, one of the main ones is the anatomical structure and role of the pelvic floor. The female PFMs span a wider pelvic outlet than in males and include an additional orifice, the vagina. As a result, the female pelvic floor relies on a more complex system of myofascial connective tissue integrity, neural innervation, vascularization and PFM function to manage the intra‐abdominal pressure (IAP) and external load demands (e.g., ground reaction forces) placed upon it (Donnelly et al., 2023). The PFMs contract during occurrences of elevated IAP (Constantinou et al., 1982) to limit the downward displacement of the pelvic organs (Junginger et al., 2010; Lovegrove Jones et al., 2010; Sapsford et al., 2001; Williams et al., 2022). Typically, PFM activation precedes rises in IAP (Sapsford et al., 2001) and movement‐related load (Okeahialam et al., 2022) in an anticipatory and feed‐forward manner. It is proposed that delayed activation and impaired speed of PFM activity may predispose symptoms of stress urinary incontinence (SUI). However, research is conflicting regarding this mechanism (Kharaji et al., 2019; Leitner et al., 2017; Moser et al., 2018, 2019; Smith et al., 2007), and other factors relating to the anatomical integrity of the pelvic floor complex, discussed below, also influence the continence mechanism.
Looking closer at the anatomical design of the PFMs, they can be considered in subsections (Table 1, Figure 1). The levator ani is a group of muscles making up a funnel shaped area in the lower part of the pelvis. From medial to lateral, they include the puborectalis, pubococcygeus and iliococcygeus (Kearney et al., 2004). The pelvic floor is further defined by two spaces, the levator hiatus and urogenital hiatus, both of which are bordered by the pubic symphysis ventrally and the medial borders of the levator ani laterally (Cheng et al., 2023) (Figure 1). The levator hiatus appears as a ‘V’‐shaped area which extends dorsally to the sides of the anorectum and is enclosed by the puborectalis muscle (Cheng et al., 2023; Delancey et al., 1998). The more caudal urogenital hiatus encloses the pubococcygeal portion of the levator ani muscles and extends dorsally from the center of the urethra to the perineal body (Cheng et al., 2023; Delancey et al., 1998).
TABLE 1.
Overview of pelvic floor anatomy.
| Pelvic floor anatomy, risks and consequences | Description |
|---|---|
| Anatomy and grouping | Levator Ani muscle group: Puborectalis, pubococcygeus and iliococcygeus |
| Urogenital diaphragm: Deep transverse perineal muscles, constrictor of the urethra and internal and external fascial coverings | |
| Urogenital hiatus: Bounded laterally by the medial margins of the levator ani, specifically the pubococcygeal portion, it extends from the center of the urethral meatus to the posterior midline of the hymen | |
| Levator hiatus: ‘V’‐shaped medial component of the levator ani muscle, corresponds with the puborectalis muscle | |
| Role | Support and maintain the position of the pelvic organs |
| Support and maintain the continence mechanism for the bladder and bowel. | |
| Normal excretion of urine and feces | |
| Sexual function | |
| Potential pelvic floor risk to the postpartum player | Sustained stretch and loading of the muscles during pregnancy and childbirth, alongside associated tissue trauma |
| Hiatal ballooning leading to pelvic organ prolapse and descent of the perineal structures | |
| Potential compromise to function | |
| Birth induced injury to the pubococcygeal muscle portion of the levator ani muscles is strongly associated with pelvic organ prolapse and descent of the perineal structures | |
| Potential for pelvic floor muscle avulsion injury | |
| Birth induced pudendal nerve injury | |
| Potential consequence of pelvic floor risk to return to rugby | Slow or delay rehabilitation progression |
| Delay return to training or matches | |
| Limit time played during training/matches | |
| Limit sport performance | |
| Negatively impact player quality of life and sport enjoyment | |
| Negatively impact player mental health |
FIGURE 1.
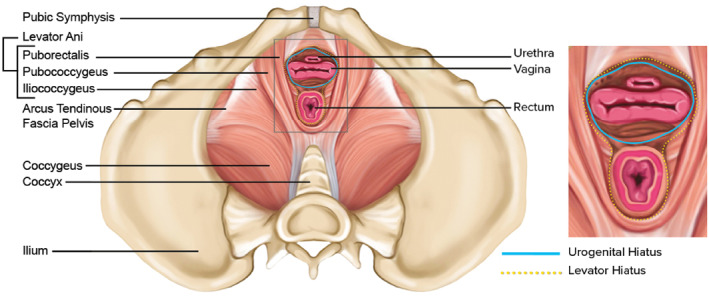
The female pelvic floor muscles and hiatal areas [Adapted from Cheng et al. (2023), Hiatal failure: effects of pregnancy, delivery and pelvic floor disorders on level III factors, International Urogynaecology Journal].
While focus has been on the deep layer of PFMs, anatomical understanding should extend to the role of connective tissue in pelvic organ support and the continence mechanism, particularly the endopelvic fascia. This layer of dense, fibrous connective tissue attaches the bladder, uterus, vagina and rectum to the pelvic walls via fascial attachments with the arcus tendinous fascia pelvis and the medial portion of the levator ani (Roch et al., 2021). One of the endopelvic fascia's recognized roles is to provide tensile strength to the anterior pelvic structures (e.g., urethra, bladder) (Ashton‐miller et al., 2007). In addition to compromised pelvic organ support via changes to the endopelvic fascia, poor levator hiatal closure may also negatively impact the continence mechanism as the habitual stiffness of the PFMs will be reduced allowing greater downward movement of the pelvic viscera and possible disruption of the urethral closure mechanism. Specifically, if the PFMs are situated adequately and the levator hiatus remains closed, the stiffness in the tissues limits excessive downward movement and ballooning of the hiatus (Bø, 2020).
3. THE PELVIC FLOOR DURING RUGBY
The mechanisms and behavior of the PFMs prior to, or during, movement are not well understood (Bø et al., 2020). One research group used a novel wireless intravaginal pressure transducer during a range of movements that required regulation of effort (Shaw et al., 2014) and analyzed the IAP of the activities relative to each individual's maximum potential IAP, determined via seated straining (Valsalva) (Dietze‐Hermosa et al., 2020). Walking generated mean IAPs of 21% of maximum IAP, whilst running, generated 56% of maximum IAP, with some individuals reaching as high as 203% (Dietze‐Hermosa et al., 2020). However, findings from studies to date regarding IAP or PFM activity should be considered with caution, as intravaginal measurement devices are likely to move and pick up artifact from surrounding muscles and tissues. Further, the dynamic forces the PFMs must be able to tolerate during movements are not well understood and are likely to be highly individualized. Valid measuring systems to quantify IAP and PFM activity during vigorous physical activities, such as those involved in rugby, need to be developed and investigated.
Several factors are likely to influence the demands and loads placed upon the PFMs, such as the ability of the body to attenuate force. For instance, a player's running technique will affect the ground reaction forces produced (Breine et al., 2017) and it is not known how much the lower limb attenuates ground reaction forces prior to reaching the PFMs. In addition to ground reaction forces, IAPs exert a load onto the PFMs. What constitutes a high magnitude of IAP appears to depend upon an individual's capacity to generate and manage IAP.
In the context of rugby, many of the movements a player is exposed to result in large forces (Nagahara et al., 2021; Trewartha et al., 2015; Usman et al., 2011) being transferred either directly to the abdomino‐lumbopelvic region (e.g., being tackled with contact to this region) or indirectly from load transferred through the body (e.g., force transferred through the shoulders during a scrum). These forces are likely to produce high IAPs (Kawabata et al., 2010; Nagahara et al., 2021) and subsequently direct high forces toward the PFMs (Bø et al., 2020; Shaw et al., 2014). To withstand this pressure, it is thought that PFM activity must increase from baseline to anticipate and accommodate the demands of movement or force (Moser et al., 2018). For example, the PFMs will theoretically be required to anticipate a tackle and accommodate forces received whilst being tackled. The ability to manage and tolerate these loads is likely to be player‐specific and influenced by several factors discussed further in this paper. Furthermore, symptomatic players may be able to tolerate the load in some movements but not others, and the ability to tolerate load will most likely reduce with training and match‐related fatigue (Thomaz et al., 2018).
4. PELVIC FLOOR DYSFUNCTION
4.1. Symptoms and prevalence
Impairment to the function of the PFMs may result from compromised connective tissue support, compromised innervation, PFM weakness or injury. Symptoms of PFD (Table 2) relate to the impairment of any role that the PFMs are involved in. Players with PFD may present with specific symptoms that relate to a subset of the anatomical structures discussed previously. Each structure should therefore be considered in its role in pelvic organ support and continence and contextualized by individual whole‐system considerations, such as aging and lifestyle factors (Delancey et al., 2008).
TABLE 2.
Considerations for symptoms, cues, training dosage, progression, adjuncts and signposting for pelvic floor disorders.
| Consideration | Recommendation |
|---|---|
| Symptoms of PFD | Urgency, frequency and/or incontinence (bladder and/or bowel, including flatus) |
| Heaviness, pressure, bulge, dragging in the vaginal area | |
| Issues emptying bladder or bowel (e.g. obstructive defecation, post‐void residual) | |
| Recurrent urinary tract infections | |
| Pelvic floor pain, dyspareunia, sexual dysfunction | |
| Vaginal dryness while lactating or associated with age‐related changes | |
| Cues for pelvic floor muscle training | “Stop gas escaping” |
| “Squeeze and lift around the urethra, vagina and rectum” | |
| “Stop the flow or urine mid‐flow” | |
| “Close a zip back passage to front passage” | |
| “Close the vagina” | |
| “Close the anus” | |
| Training dosage and progressions | Step 1: Basic focused pelvic floor training program of 8–12 MVC's aiming to hold up to 10 s each. Repeat 2–3 times per day if symptomatic |
| Step 2: The pelvic floor can also be recruited in preparation for a leakage‐provoking event (the “knack”) | |
| Step 3: Vary positions of pelvic floor training to reflect upright and task specific activities in rugby | |
| Step 4: Graded exposure to resistance/weights training beginning with static, closed chain options and progressing to dynamic options. Monitor for symptoms of PFD as weight and difficulty of training increase. Modify and regress as indicated | |
| Step 5: Graded exposure to impact activities, for example, running and jumping. Monitor for symptoms of PFD. Modify and regress as indicated | |
| Step 6: Graded exposure to spontaneous load through tackle training. Monitor for symptoms of PFD. Modify and regress as indicated | |
| Step 7: Return to simulated match play. Monitor for symptoms of PFD. Modify and regress as indicated. | |
| Step 8: Return‐to‐sport. Monitor for symptoms of PFD as training and match volume increase. | |
| Step 9: Long term adherence—include focused pelvic floor muscle training 1–2 times per week. May be part of a wider training program. | |
| Adjuncts to pelvic floor muscle training and symptom management | Vaginal pessaries for stress urinary incontinence and/or pelvic organ prolapse |
| Targeted pelvic floor compression garments | |
| Femtech | |
| Indication for signposting and onward referral | No improvement in symptoms despite adhering to regular pelvic floor muscle training |
| Unsure how to locate and train the pelvic floor despite information and cues | |
| Symptom progression | |
| Persisting pelvic pain | |
| Suspected medical issues (e.g. urinary tract infection, vaginal infection, postpartum complication, poor healing postpartum, presence of red flags) |
Abbreviations: Femtech, female technology; MVC's, maximum voluntary contractions; PFD, pelvic floor disorders/pelvic floor dysfunction.
Within the general population, it is estimated that one in three women experience urinary incontinence, up to one in 10 experience fecal incontinence and up to one in every two women have some degree of pelvic organ descent (NICE, 2021; Woodley et al., 2020; Brown et al., 2019). High force‐related activities, such as rugby, challenge the PFMs and can increase a player's susceptibility to PFD symptoms (Almeida et al., 2016; Campbell et al., 2023; de Mattos Lourenco et al., 2018; Delancey et al., 2008; Donnelly et al., 2023; McCarthy‐Ryan et al., 2024; Moore et al., 2021; Sandwith et al., 2021). In a cohort of 95 female University varsity rugby players, 54% of players leaked urine of which 90% leaked when competing and 88% leaked when being tackled or hit (Sandwith et al., 2021). A larger study (n = 396) of women's Rugby Union community to national level players across four Nations found 63% had general SUI and 43% leaked during rugby. The most prevalent symptom‐inciting events were the tackle, running and jumping. Identified risk factors for SUI during rugby included being postpartum, having a higher body mass index, being a forward and having a lower level of playing experience (McCarthy‐Ryan et al., 2024). Furthermore, reporting constipation was associated with rugby‐related SUI (McCarthy‐Ryan et al., 2024), which may result from persistent constipation increasing the strain on the PFMs over time (Delancey et al., 2008). This highlights the interaction of co‐existing symptoms and behaviors and the need to consider the wider whole‐system factors in individual player presentations (Donnelly et al., 2022).
To date, studies have determined the prevalence of PFD in women's rugby players as a collective, but we do not understand its prevalence or impact in subpopulations such as perinatal players. This is due to the lack of surveillance and the overall paucity of research investigating female‐specific health domains (Moore et al., 2023) with previously only McCarthy‐Ryan and colleagues (McCarthy‐Ryan et al., 2024) including postpartum rugby players. Consequently, there is a need for research to investigate how the risk factor of being postpartum influences the prevalence and severity of PFD in women's rugby (Heyward et al., 2022; McCarthy‐Ryan et al., 2024).
4.2. Predisposing, inciting and intervening factors
De Lancey and colleagues (Delancey et al., 2008; DeLancey et al., 2024) outline three major phases across the female lifespan where PFM function and dysfunction relate (Figure 2). Phase 1 is predisposing factors (development and functional reserve during an individual's growth); Phase 2 is inciting factors (variations in the amount of injury and potential recovery that occur during and after vaginal childbirth); and Phase 3 is intervening factors (lifestyle, deterioration occurring with advancing age). Each of these will be discussed briefly below.
FIGURE 2.
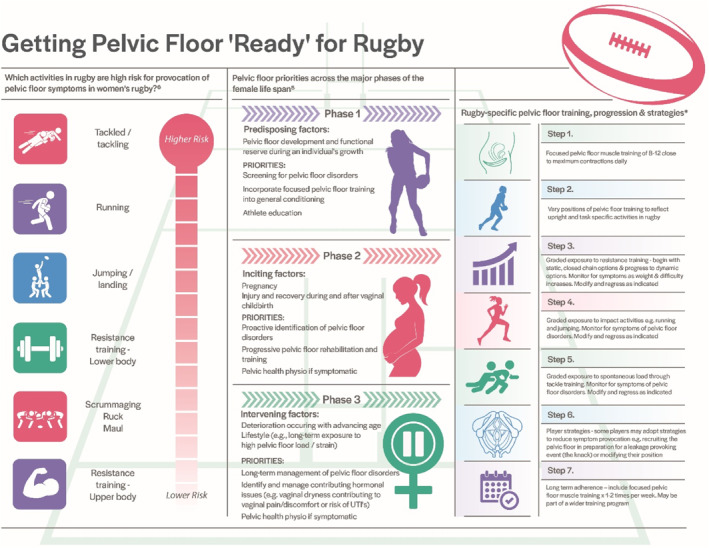
Getting Pelvic Floor ‘Ready’ for Rugby. *These recommendations are based on exercise prescription principles and research on the general population. Research specific to women's rugby players across all ages and levels is needed to better inform this population.
4.2.1. Phase 1—Predisposing factors
Development and functional reserve
It is proposed that the development of the PFMs early in the female lifespan will influence an individual's functional reserve and thus future likelihood of PFD (Delancey et al., 2008). Development and functional reserve of the PFMs are likely to be determined by several factors, including genetics, lifestyle, diet and environment (Delancey et al., 2008). For example, high body mass index and constipation are established risk factors for PFD (NICE, 2021). Early education about physical activity (Chief Medical Officer, 2019), lifestyle, the anatomy and function of the pelvic floor and how to locate and train the PFMs during adolescence is advocated to promote improved development and functional reserve (DeLancey et al., 2024; NICE, 2021). However, this theory needs to be investigated further, especially in the context of sports‐specific PFM function.
4.2.2. Phase 2—Inciting factors
Pregnancy and childbirth
The PFMs are exposed to an increasing magnitude of load from the growing uterus as a pregnancy progresses. Accordingly, the dimensions of the PFMs, and associated hiatal areas (Figure 1), increase in size to prepare for childbirth, regardless of the mode of delivery (Stær‐Jensen et al., 2013). The levator hiatal area enlarges from the first to the third trimester of pregnancy at rest, on PFM contraction, and during bearing down, by an average of 13%, 10% and 29%, respectively (Cheng et al., 2023). These normal, anticipated changes are important to ready the body and facilitate potential vaginal childbirth. However, they also carry a risk for negative implications associated with increasing hiatal distensibility, especially when subsequent vaginal childbirth is considered too. For women who experience vaginal childbirth (approximately 80% of worldwide childbirths) (Betran et al., 2021), major changes to the PFMs occur including compression and stretching of PFM soft tissues that extend beyond the capacity of most other muscles in the body. Specifically, the baby's head stretches the levator ani muscle, generating predominantly passive forces in the tissue of the levator hiatus as it passes through the PFMs (Tracy et al., 2016). For non‐pregnant muscle tissue, the maximum non‐injurious stretch (lengthening) that a muscle can undergo before injury is estimated to be 150% of its original length (Brooks et al., 1995). Comparatively, the PFMs experience a stretch much higher than this during vaginal childbirth, up to 250% their original length (Krofta et al., 2017). Therefore, birth‐induced injury to the levator ani muscles during vaginal childbirth includes over‐stretching (microtrauma) or tearing and avulsion (macrotrauma) and varying degrees of either are considered to occur in all vaginal deliveries. The prevalence of PFM injury (macrotrauma) specifically from vaginal childbirth ranges from 18% to 41% (Cardozo et al., 2023; Miller et al., 2015). Additionally, obstetric anal sphincter injuries (also known as third and fourth degree perineal tears) have been reported in up to 8% of vaginal deliveries in the UK (Thiagamoorthy et al., 2014). A recent meta‐analysis of risk factors for perineal laceration covering all degrees reported risks to include primiparity, instrumental delivery (particularly forceps) and newborn birthweight (Pergialiotis et al., 2020).
Birth‐induced injuries are associated with descent of the pelvic organs and perineal structures (Cheng et al., 2023; Clark et al., 2010; DeLancey et al., 2012). Specifically, the distensibility of the levator ani causes an increase in the cross‐sectional area of the levator hiatus. Excessive distensibility, termed hiatal ballooning, is associated with the occurrence of pelvic organ prolapse (Siahkal et al., 2021; Xuan et al., 2019). In fact, this region is considered to have the largest potential hernia portal in the human body (Xuan et al., 2019). Most of the recovery in size of the levator hiatus occurs within 4–6 months after delivery (Cheng et al., 2023). However, it does not return to pre‐pregnancy size, and this recovery time is further complicated depending on the degree of trauma at the time of delivery (Bø et al., 2022; Cheng et al., 2023; Stær‐Jensen et al., 2015). Whilst the transition into and beyond pregnancy is a normal bodily process, it can impair the function of the PFMs and lead to reduced sport participation, time loss from sport and career cessation (Dakic et al., 2021; McCarthy‐Ryan et al., 2024). Unlike return‐to‐sport following injury, which is widely discussed in the sports medicine and science literature, return‐to‐sport after pregnancy and childbirth have been largely overlooked. The physiological changes to the PFMs during pregnancy warrant consideration and purposeful strengthening and conditioning, even in players who experience childbirth via caesarean section. Given the increased size of the levator hiatal area by the third trimester of pregnancy (Bø et al., 2015), reconditioning to encourage a return toward baseline size, resting tone and strength is paramount, especially in the context of the load tolerance required of the PFMs during rugby. In most countries, a large focus is placed on PFM training during pregnancy, as early structured PFM training can prevent the onset of urinary incontinence in mid and late pregnancy (Woodley et al., 2020) and limit the perceived symptoms of pelvic organ descent (Hagen et al., 2014, 2017). Evidence has shown that women with enhanced understanding of the PFMs are 57% less likely to develop urinary incontinence (Cardoso et al., 2018). Consequently, from a PFD prevention perspective, rugby players across all ages and levels should be educated on the anatomy and function of the PFMs.
4.2.3. Phase 3—Intervening factors
Lifestyle
The type of sport women longitudinally engage in may expose the PFMs to different loads that appear to effect PFM morphology (Menezes et al., 2023) and contribute to the risk of PFDs. That is, high force activities such as rugby may alter morphology in a way that increases the risk. When compared to non‐active/low impact exercising controls, competitive athletes engaging in high‐impact training for over 5 years exhibit greater levator hiatal width (Kruger et al., 2007; Menezes et al., 2023) and distensibility as well as higher degrees of pelvic organ descent (Kruger et al., 2007). Further, engaging with 30 min of exercise 3 times per week during pregnancy leads to a larger hiatal area at rest and during PFM contraction compared to not exercising in the third but not the second trimester (Bø et al., 2015). These studies highlight the potential changes that can present in nulliparous athletes through exposure to sports like rugby, with pregnancy possibly modifying this interaction. Exposure to high‐impact sports can also lead to acute changes in hiatal dimensions, but this is consistent in runners with and without SUI (Bérubé et al., 2023) and the long‐term consequences are not fully understood.
Deterioration occurring with advancing age
With player longevity being an important consideration as more women potentially take up rugby in later life or continue participating for longer (e.g., beyond motherhood), an understanding of the age‐related deterioration in PFMs is needed. Normal decline of the PFMs is expected with age‐related changes including increased fiber length (Alperin et al., 2016; Cook et al., 2017), fibrosis (Alperin et al., 2016) and a reduction in muscle mass and connective tissue tensile strength associated with the decline in estrogen (Chidi‐Ogbolu et al., 2018). The decline of the PFMs across the lifespan may also be influenced by several factors including obesity, arduous occupations or chronic constipation (DeLancey et al., 2023; Jackson et al., 2022; NICE, 2021). For women, menopause may interact with the risk of PFD due to associated hormonal changes during this age‐related transition (Angelou et al., 2020; Peinado‐Molina et al., 2023). However, to the authors' knowledge, no studies have examined the influence of hormonal changes or the transition into menopause in women's rugby players. Raising awareness of the impact that advancing age and the transition into menopause can have on an individual's PFMs and associated function is important.
5. RECONDITIONING THE PELVIC FLOOR
Like other muscle groups, the PFMs can be trained via targeted strengthening and conditioning and there is consistent evidence that PFM training can induce muscle hypertrophy, reduce the levator hiatal area and improve the symptoms associated with PFD (Cacciari et al., 2021, 2022; Hagovska et al., 2022; Hoff Brækken et al., 2010). Regardless of the predisposing, inciting and or intervening factor(s), symptomatic players should engage in appropriate PFM training. For example, postpartum rugby players should be informed about commencing PFM training as soon as possible following childbirth. Following vaginal delivery, even in the presence of perineal tears and stitches, PFM training can gently commence. Medically complicated deliveries or any delivery that results in a catheter in situ will delay PFM training until the catheter is removed. Based upon exercise prescription principles, rugby players should follow general strength training recommendations (Garber et al., 2011). In terms of the PFMs, strength training dosage should aim for fatigue of the PFMs by the end of the set(s). This could involve engaging in focused PFM training of 3 sets of 8 to 12 close to maximum PFM contractions repeated daily (Bø et al., 2024; Fleck, 2004) during early rehabilitation and reducing to one to two times per week for maintenance as recovery progresses or symptoms resolve (Bø et al., 2020; Garber et al., 2011). However, more research is required in relation to PFM training dosage in athletic populations such as rugby and players will have differing reconditioning needs dependent upon individual predisposing, inciting and intervening factors. Where possible, PFM reconditioning should be informed and guided by a pelvic health physiotherapist (sometimes referred to as women's health physiotherapist) (Pelvic Obstetric and Gynaecological Physiotherapy, 2022). Table 2 offers useful prompts to help rugby players understand how to locate and train their PFMs as well as guidance on load progression, adjuncts and when to signpost or refer onwards for specialist support.
5.1. Vaginal tissue health
Lower levels of estrogen in the female body can increase vaginal dryness and sensitivity (Goncharenko et al., 2019). These vaginal changes may have a negative impact upon sexual function, player comfort and ability to train or play matches. There may also be an increased risk of health problems (e.g., urinary tract infections) (Goncharenko et al., 2019). Lower estrogen levels are associated with lactation (Calik‐Ksepka et al., 2022) and aging (menopause) (Angelou et al., 2020) and therefore breastfeeding and perimenopausal rugby players are likely to be impacted. Player support staff should be aware of these challenges and signpost players to appropriate healthcare professionals for management (e.g., General Practitioner, Gynecologist) where vaginal moisturisers or localized estrogen may be indicated.
5.2. Psychological wellbeing
Focusing beyond localized muscle dysfunction or tissue trauma, wider whole‐system factors associated with mental health, psychosexual trauma (Karsten et al., 2020) or birth trauma (Greenfield et al., 2016) can negatively impact PFM function. The reverse is also true whereby psychological wellbeing (across the female lifespan) is negatively impacted by PFD (NICE, 2021). The transition into motherhood, for example, can be challenging for many women, with up to 40% experiencing perinatal mental health problems such as postpartum depression (Wang et al., 2021). In fact, postpartum depression is three times as prevalent in women with PFD than women without it (Mazi et al., 2019). Furthermore, their experience of interactions and events directly related to childbirth may cause overwhelming distressing emotions and reactions, leading to short and long‐term negative implications on their health and wellbeing (Leinweber et al., 2022). This means that both physical and/or psychologically traumatic experiences during childbirth (“birth trauma”) can incur ongoing psychological consequences including catastrophizing and compromised mental health (Leinweber et al., 2022; Shorey et al., 2022). Physical symptoms of birth trauma include birth‐related tissue injury, reduction in functional capacity, fatigue and persistent postpartum pain (Daly et al., 2017; Kainu et al., 2010; Taghizadeh et al., 2013). Consequently, postpartum players experiencing birth trauma may be disengaged from adhering to postpartum rehabilitation advice, such as PFM training. They may also perceive the area to be vulnerable or fragile, impacting their ability to participate in reconditioning and progressive loading and potentially increasing the risk for fear of movement. Awareness of these conditions along with regular screening and monitoring should be in place so that players can be signposted to specialist psychological support as necessary. A validated tool, such as the Edinburgh Postnatal Depression Scale (Gollan et al., 2021) or the Clinician Administered Post‐Traumatic Stress Disorder Scale (de Graaff et al., 2018), can be used to screen players as appropriate.
6. PELVIC FLOOR LOAD TOLERANCE
An integral part of rugby‐specific training includes strength training. Progressive and functional strength training helps prepare players for the demands of rugby, which involves player‐to‐player contact and multidirectional movements (Dane et al., 2022). The tackle is the most frequent contact event in Rugby Union and Rugby League, with a mean of 280 (West et al., 2022) and 512 (Cummins et al., 2020) tackles per game, respectively. In both Union and League matches, player‐to‐player contacts are higher in forwards than in backs (Cummins et al., 2020; Woodhouse et al., 2021). Additionally, players perform high‐speed running, accelerations and decelerations, change of directions, lineout lifts with high‐impact landings, as well as skill‐based events such as catching, passing and kicking the ball. Players must successfully execute these technical actions numerous times over the course of a game, whilst under pressure and experiencing fatigue (Dane et al., 2022). The frequency of these contact and non‐contact skills is dependent on playing position, meaning strength requirements are position‐specific.
Training requirements for women's rugby should include focused PFM training (Table 2, Figure 2) (Donnelly et al., 2023) alongside whole‐body resistance training. Whole‐body resistance training is an important part of conditioning a player for the demands of rugby. In the context of the PFMs, whole‐body resistance training may enable insight into PFM load tolerance. If symptoms of PFD are only provoked as resistance training is progressed, it highlights the need for further focused PFM training and/or review by a pelvic health physiotherapist. Whilst there is limited research examining the effect of whole‐body resistance training and the response of the PFMs, lifting higher loads is considered to increase the IAP placed upon the PFMs (Bø et al., 2020), which may increase the risk of PFD. This may explain the higher prevalence of PFD symptoms, (specifically urinary and anal incontinence) observed in Norwegian female powerlifters (Skaug et al., 2022) compared to the general population (NICE, 2021). In rugby, nulliparous and parous women report SUI to be prevalent (42%) during lower body strength training (McCarthy‐Ryan et al., 2024). However, when considering the loads associated with strength training, women lifting heavy weights (>50 kg) do not report more symptoms of pelvic organ prolapse compared to women lifting lower weights (<15 kg) (Forner et al., 2020). Additionally, acute exposure to heavy lifting does not appear to have negative effects on PFM strength (Skaug et al., 2023). Further research is needed to understand the prevalence of PFD in rugby players exposed to acute and chronic heavy resistance training as well as the long‐term implication of whole‐body resistance training on the PFMs.
The Valsalva strategy that is often necessary to lift heavy loads and prepare for rugby demands has been shown to produce high levels of IAP (Cummins et al., 2020; Dane et al., 2022; Eliasson et al., 2008; West et al., 2022; Woodhouse et al., 2021). Strenuous activity and sport can result in SUI even in nulliparous athletes (Eliasson et al., 2008; Kruger et al., 2007), with the risk for SUI and compromised pelvic organ support further increased in vaginally parous athletes. Studies comparing the impact of pregnancy and vaginal childbirth on the PFMs found that women who delivered vaginally had a greater hiatal area on Valsalva compared to nulliparous women (Cattani et al., 2022). This lack of support and low stiffness in the PFM tissues can compromise the continence mechanism and pelvic organ support. This is supported by Howard and colleagues (Howard et al., 2000) who found that SUI parous women demonstrate greater bladder neck descent during a cough than continent parous women. A non‐significant lower stiffness was also observed for the SUI group. Teams supporting postpartum players to return to rugby should be aware of the increased risk of PFD associated with vaginal delivery and manage players accordingly.
It is not only the mode of delivery but also the likely generalized deconditioning incurred during the perinatal period that should be considered for rugby players who need to cease contact‐related rugby activities during pregnancy and have individualized levels of associated rest from rugby postpartum (World Rugby, 2024). Such generalized deconditioning may also present following severe injuries, such as anterior cruciate ligament rupture. As a result, most postpartum rugby players will have reconditioning needs to prepare for the physical demands, skills and high‐volume of contacts required during rugby (Dane et al., 2022). Graded exposure to postpartum strength training is encouraged and should center around symptom‐free training (Donnelly et al., 2024; World Rugby, 2024). Evidence regarding appropriate timeframes to return‐to‐sport postpartum is lacking. Based on clinical and exercise professional expert opinion, a Delphi study recommended a minimum timeframe of 3–6 weeks relative rest prior to returning to running postpartum (Christopher et al., 2023) and recent World Rugby guidelines indicate 16 weeks postpartum as a minimum time for returning to rugby matches (World Rugby, 2024). Individual timeframes will vary based on whole‐system factors (e.g., delivery mode, psychological readiness to return) and more detail is provided by Donnelly and colleagues (Donnelly et al., 2024) in this special issue.
When undertaking rugby training across the female lifespan, symptoms of PFD should be appropriately identified, managed and addressed according to individual needs. If symptoms are present, strength training should be modified to reduce the training load by way of lowering the weight, reducing the number of repetitions or modifying the resistance exercise or position to reduce the PFM load. If PFM weakness has been assessed as a contributing factor to PFD symptoms, focused PFM training may need to be adjusted to address this. Strategies which may assist PFM function during return to load exposure are discussed later.
Traditionally, sports medicine and science research have focused on the training load accumulated by a player (acute and chronic volume) when assessing injury risk (Blanch et al., 2016) and return‐to‐sport load (Ritchie et al., 2017). However, for a postpartum player as one example, load considerations must go beyond training volume and perceived effort. Specifically, the new life demands brought on by the role of motherhood may mean that atypical daily activity loads accumulate (e.g., lifting, carrying a baby, pushing the pram up hills). Additionally, the wider biopsychosocial challenges that may present after having a baby (e.g., sleep deprivation, lactation, inadequate nutrition, mental health) will ultimately influence a player's recovery, conditioning and tolerance for training. Therefore, psychosocial loads should also be considered when evaluating PFM load tolerance. Collectively, non‐rugby, daily physical activity loads, biopsychosocial loads and additional rugby loads will contribute to a player's readiness and return to rugby training and game play.
7. PELVIC FLOOR STRATEGIES FOR RUGBY PLAYERS
How different players tolerate the same PFM load may be explained by predisposing, inciting and intervening factors (Delancey et al., 2008; DeLancey et al., 2023) discussed earlier in this review. For example, variation in player tolerance may also be relative to the functional reserve each player achieved during growth and development (Delancey et al., 2008). Players who progress to superior PFM strength and tolerance to load during earlier life are likely to have more functional reserve and resilience to inciting (pregnancy and childbirth) and intervening (lifestyle and age‐related decline) factors which increase the risk of PFD. Further, player strategies employed during rugby may add to the combination of factors influencing a player's risk including behavioral and non‐behavioral strategies.
7.1. Behavioral strategies
Symptoms of PFD suggest that a player is not tolerating the load being placed upon the PFMs, yet many players continue to play when experiencing symptoms (McCarthy‐Ryan et al., 2024; Sandwith et al., 2021). Where a player is symptomatic, symptoms may be reduced or overcome by implementing rugby‐specific strategies. Specifically, rugby players who leak urine during contact‐related activities report modifying their body position (technique) and reducing the number of contact activities they engage in (McCarthy‐Ryan et al., 2024). Whereas the most common strategy for non‐contact activities was reducing movement speed or height jumped as well as modifying technique and reducing the number of non‐contact activities engaged.
Some players may use Valsalva during strenuous rugby movements (e.g., a scrum) to achieve the required magnitude of strength, as Valsalva results in increased trunk stiffness (Hughes et al., 1989) and increases IAP (Blazek et al., 2019). This associated increase in IAP (internal load) can elevate the load placed onto the PFMs and therefore may increase the risk of PFD symptoms due to the repetitive exposure to larger IAPs and potentially higher loads being transferred to the PFMs. However, further research is required to understand the consequences of the Valsalva in female athletes, including rugby players. Furthermore, recently published expert opinion suggests that strategies, including (i) optimizing the technique of abdominal bracing to optimize abdominal cavity force distribution and (ii) engaging in subthreshold training while pelvic floor capacity is increased, may be worthwhile approaches for players who achieve performance benefits with the Valsalva (Prevett et al., 2024).
Another strategy from clinical practice is changing from a Valsalva strategy to purposively breathing, grunting or vocalizing during effort. This has been shown to reduce IAP in weightlifters compared to that generated during Valsalva strategies (Hagins et al., 2006) and therefore may theoretically reduce the IAP forces directed toward the PFMs. Providing players with possible strategies allows them to choose the most effective strategy for reducing their symptoms, as well as potentially helping to reduce the cumulative impact of loads on the PFMs; however, research is needed to substantiate this. Irrespective of these rugby specific strategies, PFM training should be included as first line management where load tolerance deficits are identified. Additionally, players should be signposted to a pelvic health physiotherapist for individualized evaluation of their rehabilitation needs.
7.2. Non‐rugby behavioral strategies
Players may try to manage symptoms of PFD by altering their bladder emptying behavior and fluid intake, which can lead to the development of further symptoms of PFD. For example, a rugby player who suffers from SUI may try to reduce symptoms by restricting their fluid intake (Culleton‐Quinn et al., 2022; Johnston et al., 2023) and frequently emptying their bladder before and during training (Culleton‐Quinn et al., 2022). This reduction in fluid intake and simultaneous purposeful increase in frequency of voiding is hypothesized to influence the risk of developing further urinary symptoms. For example, urinary frequency, urgency and urge incontinence could develop due to conditioning of the bladder to smaller, more concentrated urine volumes and disruption to the normal urge capacity prior to voiding. However, such behavioral causes of overactive bladder presentations have yet to be supported by research. Nonetheless, it is important that evidence‐based guidance is provided to rugby players regarding maladaptive bladder behaviors and best practice strategies and behaviors (e.g., adequate fluid intake, PFM training) (Booth et al., 2023).
8. ADJUNCTS AND ADDITIONAL CONSIDERATIONS
Available options to help minimize the disruption experienced and adjustment required as a consequence of PFD should be communicated to players across all ages and levels. This extends to wider roles involved in rugby (e.g., female coaches and match officials). One example includes digital applications within female technology, which can prompt reminders, direct technique and reinforce educational guidance on PFM exercises. However, the evidence informed quality and efficacy of some digital applications are low (Jaffar et al., 2022; Sudol et al., 2019), and therefore, recommendations of specific applications should be carefully informed.
Players experiencing symptoms of SUI or pelvic organ prolapse may benefit from trying an intravaginal support or continence device (such as a vaginal pessary) to facilitate return to training and match‐play and sustain symptom management. Pessaries for SUI and pelvic organ prolapse have the potential to fully manage and alleviate symptoms (Donnelly et al., 2023; NICE, 2021), thereby allowing women's rugby players to continue engaging with training and return‐to‐sport. Players may also benefit from wearing targeted compression garments during training and matches. Compression garments targeting the PFMs are relatively new and have received limited research attention. Studies have highlighted that they reduce SUI and positively influence the perception of PFD symptoms (Ninomiya et al., 2014; Okayama et al., 2019), which may subsequently improve a symptomatic player's confidence to exercise. Additionally, consideration should be given to the practicality, color, and comfort of player uniform as a study involving commonwealth athletes (that included a small sample of women's rugby players) identified sports involving fitted uniforms (e.g., gymnastics) created worry about an incontinence pad being visible (Johnston et al., 2023). Therefore athletes, including rugby players, need to be able to wear comfortable clothing that facilitates discrete wearing of incontinence or menstrual products.
9. PELVIC FLOOR SURVEILLANCE AND FUTURE RESEARCH
Appropriate injury and illness surveillance should be in place to capture any PFD. Pelvic floor health and postpartum are two female athlete health domains recently proposed as key considerations when undertaking female injury and illness surveillance (Moore et al., 2023). Moore and colleagues (Moore et al., 2024) in this special issue highlight that in a rugby context, a non‐time‐loss health problem definition should be implemented to enable PFD data to be recorded as rugby players suffering from PFD do not necessarily stop training or discuss symptoms with their coaches, but rather modify training activities and continue playing (McCarthy‐Ryan et al., 2024). Annual baseline screening as well as ongoing screening during postpartum rehabilitation is advocated for PFD due to the accumulated and changing rugby exposure experienced by players. Whilst validated questionnaires for PFD can be used and allow comparisons between different populations, such questionnaires are general and not sport‐specific. The first sports‐specific screening tool for PFD has been developed (The PFD‐SENTINEL) (Giagio et al., 2023) and may assist with player screening and surveillance; however, it has not yet been validated.
Drawing on postpartum return to running evidence (Christopher et al., 2023; Donnelly et al., 2020; Moore et al., 2021), for the postpartum rugby player, it may be appropriate to ask about urinary and fecal incontinence, flatus incontinence, feeling of vaginal heaviness or, a bulge inside or outside the vagina and musculoskeletal pelvic pain during rugby‐specific activities (e.g., being tackled, tackling, running, rucks and scrums) to determine the intervening event and inform management strategies. Research specific to the PFMs and rugby, which focuses on better understanding the normal behavior of the PFMs during exercise as well as prevention, childbirth related injury and physical performance, is needed to better understand and guide PFM preparation and recovery in anticipation for playing rugby.
10. SUMMARY
Awareness and recognition of the changes the PFMs go through during development, pregnancy, childbirth and advancing age is the first step to understanding how to support players to be PFM ‘ready’ for engaging in rugby. The next step is understanding signs and symptoms of PFD and being able to evaluate player load tolerance, considering physical and psychosocial (external and internal) loads. We have outlined several strategies that rugby players may use to reduce or overcome symptoms of PFD, whilst recommending that PFM training is undertaken by all rugby players as a prophylactic approach and as a first line treatment for PFD. Being PFM ready for rugby will require symptomatic players to engage in a reconditioning program with progressive loading. By applying the steps and recommendations identified in this review, enhanced rehabilitation support can be provided to all women's players by health and fitness professionals, which can minimize the risk and or symptoms of PFD and enable continued rugby participation across all age, roles and levels of the game.
CONFLICT OF INTEREST STATEMENT
ISM receives funding from the Welsh Rugby Union and World Rugby and is an advisor to the Rugby Player's Association Women's Welfare group.
COMPETING INTEREST STATEMENT
The authors report there are no competing interests to declare.
ACKNOWLEDGMENTS
The authors would like to thank Roisin Bradley for the design of the pelvic floor illustration (Figure 1).
REFERENCES
- Almeida, M. B. A. , Barra A. A., Saltiel F., Silva‐Filho A. L., Fonseca A. M. R. M., and Figueiredo E. M.. 2016. “Urinary Incontinence and Other Pelvic Floor Dysfunctions in Female Athletes in Brazil: A Cross‐Sectional Study.” Scandinavian Journal of Medicine & Science in Sports 26(9): 1109–1116: Epub 20150915. PubMed PMID: 26369504. 10.1111/sms.12546. [DOI] [PubMed] [Google Scholar]
- Alperin, Marianna , Cook Mark, Tuttle Lori J., Esparza Mary C., and Lieber Richard L.. 2016. “Impact of Vaginal Parity and Aging on the Architectural Design of Pelvic Floor Muscles.” American Journal of Obstetrics and Gynecology 215(3): 312.e1–312.e9. 10.1016/j.ajog.2016.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angelou, Kyveli , Grigoriadis Themos, Diakosavvas Michail, Zacharakis Dimitris, and Athanasiou Stavros. 2020. “The Genitourinary Syndrome of Menopause: An Overview of the Recent Data.” Cureus 12(4): e7586: Epub 20200408. PubMed PMID: 32399320; PubMed Central PMCID: PMC7212735. 10.7759/cureus.7586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashton‐miller, James A. , and DeLANCEY John O. L.. 2007. “Functional Anatomy of the Female Pelvic Floor.” Annals of the New York Academy of Sciences 1101(1): 266–296: Epub 20070407. PubMed PMID: 17416924. 10.1196/annals.1389.034. [DOI] [PubMed] [Google Scholar]
- Bérubé, Marie‐Ève , and McLean Linda. 2023. “The Acute Effects of Running on Pelvic Floor Morphology and Function in Runners with and without Running‐Induced Stress Urinary Incontinence.” International Urogynecology Journal 35(1): 127–138. 10.1007/s00192-023-05674-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betran, Ana Pilar , Ye Jiangfeng, Moller A.‐Beth, Souza João Paulo, and Zhang Jun. 2021. “Trends and Projections of Caesarean Section Rates: Global and Regional Estimates.” BMJ Global Health 6(6): e005671: PubMed PMID: 34130991; PubMed Central PMCID: PMC8208001. 10.1136/bmjgh-2021-005671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanch, Peter , and Gabbett Tim J.. 2016. “Has the Athlete Trained Enough to Return to Play Safely? The Acute:Chronic Workload Ratio Permits Clinicians to Quantify a Player's Risk of Subsequent Injury.” British Journal of Sports Medicine 50(8): 471–475: Epub 20151223. PubMed PMID: 26701923. 10.1136/bjsports-2015-095445. [DOI] [PubMed] [Google Scholar]
- Blazek, Dusan , Stastny Petr, Maszczyk Adam, Krawczyk Magdalena, Matykiewicz Patryk, and Petr Miroslav. 2019. “Systematic Review of Intra‐abdominal and Intrathoracic Pressures Initiated by the Valsalva Manoeuvre During High‐Intensity Resistance Exercises.” Biology of Sport 36(4): 373–386: Epub 20191017. PubMed PMID: 31938009; PubMed Central PMCID: PMC6945051. 10.5114/biolsport.2019.88759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bø, Kari . 2020. “Physiotherapy Management of Urinary Incontinence in Females.” Journal of Physiotherapy 66(3): 147–154. 10.1016/j.jphys.2020.06.011. [DOI] [PubMed] [Google Scholar]
- Bø, Kari , Hilde Gunvor, Stær‐Jensen Jette, Siafarikas Franziska, Tennfjord Merete Kolberg, and Engh Marie Ellstrøm. 2015. “Does General Exercise Training before and during Pregnancy Influence the Pelvic Floor “Opening” and Delivery Outcome? A 3D/4D Ultrasound Study Following Nulliparous Pregnant Women from Mid‐pregnancy to Childbirth.” British Journal of Sports Medicine 49(3): 196–199. 10.1136/bjsports-2014-093548. [DOI] [PubMed] [Google Scholar]
- Bø, Kari , Næss Karoline, Stær‐Jensen Jette, Siafarikas Franziska, Ellström Engh Marie, and Hilde Gunvor. 2022. “Recovery of Pelvic Floor Muscle Strength and Endurance 6 and 12 Months Postpartum in Primiparous Women‐A Prospective Cohort Study.” International Urogynecology Journal 33(12): 3455–3464: Epub 20220901. PubMed PMID: 36048249; PubMed Central PMCID: PMC9666345. 10.1007/s00192-022-05334-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bø, Kari , and Nygaard Ingrid Elisabeth. 2020. “Is Physical Activity Good or Bad for the Female Pelvic Floor? A Narrative Review.” Sports Medicine 50(3): 471–484: PubMed PMID: 31820378; PubMed Central PMCID: PMC7018791. 10.1007/s40279-019-01243-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bø, K. M. S . 2024. “Pelvic Floor and Exercise Science ‐ Strength Training.” In Evidence‐Based Physical Therapy for the Pelvic Floor ‐ Bridging Science and Clinical Practice, edited by Bo K. B., Morkved S. and Van Kampen M.. 3rd ed., 148–165. Elsevier. [Google Scholar]
- Booth, J. , Cacciari L., Campbell P., Dumoulin C., Hagen S., Homsi J., Morin M., et al. 2023. “Conservative Management of UI and POP in Adults, Including Neurological Patients.” In ICI‐ICS, edited by Abrams P.. Incontinence 7th ed.: Bristol UK. [Google Scholar]
- Bordoni, B. , Sugumar Kavin, and Leslie Stephen W.. 2022. Anatomy, Abdomen and Pelvis, Pelvic Floor. StatPearls [Internet]. StatPearls Publishing. [PubMed] [Google Scholar]
- Breine, Bastiaan , Malcolm Philippe, Van Caekenberghe Ine, Fiers Pieter, Frederick Edward C., and De Clercq Dirk. 2017. “Initial Foot Contact and Related Kinematics Affect Impact Loading Rate in Running.” Journal of Sports Sciences 35(15): 1556–1564: Epub 20160913. PubMed PMID: 27624557. 10.1080/02640414.2016.1225970. [DOI] [PubMed] [Google Scholar]
- Brooks, S. V. , Zerba E., and Faulkner J. A.. 1995. “Injury to Muscle Fibres after Single Stretches of Passive and Maximally Stimulated Muscles in Mice.” Journal of Physiology 488(Pt 2): 459–469: PubMed PMID: 8568684; PubMed Central PMCID: PMC1156684. 10.1113/jphysiol.1995.sp020980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, James C. , Cross Matthew, England Michael, Finch Caroline F., Fuller Gordon W., Kemp Simon P. T., Quarrie Ken, et al. 2019. “Guidelines for Community‐Based Injury Surveillance in Rugby Union.” Journal of Science and Medicine in Sport 22(12): 1314–1318: Epub 20190812. PubMed PMID: 31445950. 10.1016/j.jsams.2019.08.006. [DOI] [PubMed] [Google Scholar]
- Cacciari, Licia P. , Morin Mélanie, Mayrand M.‐Hélène, and Dumoulin Chantale. 2022. “Never Too Late to Train: The Effects of Pelvic Floor Muscle Training on the Shape of the Levator Hiatus in Incontinent Older Women.” International Journal of Environmental Research and Public Health 19(17): 11078: Epub 20220904. PubMed PMID: 36078794; PubMed Central PMCID: PMC9518531. 10.3390/ijerph191711078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacciari, Licia P. , Morin Mélanie, Mayrand M.‐Hélène, Tousignant Michel, Abrahamowicz Michal, and Dumoulin Chantale. 2021. “Pelvic Floor Morphometrical and Functional Changes Immediately after Pelvic Floor Muscle Training and at 1‐year Follow‐Up, in Older Incontinent Women.” Neurourology and Urodynamics 40(1): 245–255: Epub 20201019. PubMed PMID: 33075192. 10.1002/nau.24542. [DOI] [PubMed] [Google Scholar]
- Calik‐Ksepka, Anna , Stradczuk Monika, Czarnecka Karolina, Grymowicz Monika, and Smolarczyk Roman. 2022. “Lactational Amenorrhea: Neuroendocrine Pathways Controlling Fertility and Bone Turnover.” International Journal of Molecular Sciences 23(3): 1633: Epub 20220131. PubMed PMID: 35163554; PubMed Central PMCID: PMC8835773. 10.3390/ijms23031633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, K. Gillian , Batt Mark E., and Drummond Avril. 2023. “Prevalence of Pelvic Floor Dysfunction in Recreational Athletes: A Cross‐Sectional Survey.” International Urogynecology Journal 34(10): 2429–2437: Epub 20230510. PubMed PMID: 37162534. 10.1007/s00192-023-05548-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardoso, Amanda Maria Brito , Lima Cláudia Regina Oliveira de Paiva, and Ferreira Caroline Wanderley Souto. 2018. “Prevalence of Urinary Incontinence in High‐Impact Sports Athletes and Their Association with Knowledge, Attitude and Practice about This Dysfunction.” European Journal of Sport Science 18(10): 1405–1412: PubMed PMID: 30025510. 10.1080/17461391.2018.1496146. [DOI] [PubMed] [Google Scholar]
- Cardozo, L. , Rovner E., Wagg A., Wein A., and Abrams P.. 2023. “Incontinence.” In ICI‐ICS. 7th ed. Bristol UK: International Continence Society. [Google Scholar]
- Cattani, L. , Van Schoubroeck D., and Deprest J.. 2022. “EP48.08: Comparing Pelvic Floor Findings during Pregnancy in Nulliparous and in Parous Women.” Ultrasound in Obstetrics and Gynecology 60(S1): 314–315. 10.1002/uog.26013. [DOI] [Google Scholar]
- Cheng, Wenjin , English Emily, Horner Whitney, Swenson Carolyn W., Chen Luyun, Pipitone Fernanda, Ashton‐Miller James A., and DeLancey John O. L.. 2023. “Hiatal Failure: Effects of Pregnancy, Delivery, and Pelvic Floor Disorders on Level III Factors.” International Urogynecology Journal 34(2): 327–343: Epub 20220921. PubMed PMID: 36129480; PubMed Central PMCID: PMC10171831. 10.1007/s00192-022-05354-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chidi‐Ogbolu, Nkechinyere , and Baar Keith. 2018. “Effect of Estrogen on Musculoskeletal Performance and Injury Risk.” Frontiers in Physiology 9: 1834: Epub 20190115. PubMed PMID: 30697162; PubMed Central PMCID: PMC6341375. 10.3389/fphys.2018.01834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chief Medical Officer . 2019. Physical Activity for Children and Young People: 5 to 18 Years.
- Christopher, Shefali Mathur , Donnelly Gráinne, Brockwell Emma, Bo Kari, Davenport Margie H., De Vivo Marlize, Dufour Sinead, et al. 2023. “Clinical and Exercise Professional Opinion of Return‐To‐Running Readiness after Childbirth: an International Delphi Study and Consensus Statement.” British Journal of Sports Medicine 58(6): 299–312: bjsports‐2023‐107489. 10.1136/bjsports-2023-107489. [DOI] [PubMed] [Google Scholar]
- Clark, Natalie A. , Brincat Cynthia A., Yousuf Aisha A., and DeLancey John O. L.. 2010. “Levator Defects Affect Perineal Position Independently of Prolapse Status.” American Journal of Obstetrics and Gynecology 203(6): 595.e17–595.e22: PubMed PMID: 20869037. 10.1016/j.ajog.2010.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantinou, C. E. , and Govan D. E.. 1982. “Spatial Distribution and Timing of Transmitted and Reflexly Generated Urethral Pressures in Healthy Women.” The Journal of Urology 127(5): 964–969: PubMed PMID: 7201031. 10.1016/s0022-5347(17)54148-8. [DOI] [PubMed] [Google Scholar]
- Cook, Mark S. , Bou‐Malham Laura, Esparza Mary C., and Alperin Marianna. 2017. “Age‐related Alterations in Female Obturator Internus Muscle.” International Urogynecology Journal 28(5): 729–734. 10.1007/s00192-016-3167-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culleton‐Quinn, Elizabeth , Bø Kari, Fleming Neil, Mockler David, Cusack Cinny, and Daly Déirdre. 2022. “Elite Female Athletes' Experiences of Symptoms of Pelvic Floor Dysfunction: A Systematic Review.” International Urogynecology Journal 33(10): 2681–2711: Epub 20220830. PubMed PMID: 36040507; PubMed Central PMCID: PMC9477953. 10.1007/s00192-022-05302-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummins, Cloe , Melinz Jaede, King Doug, Sanctuary Colin, and Murphy Aron. 2020. “Call to Action: A Collaborative Framework to Better Support Female Rugby League Players.” British Journal of Sports Medicine 54(9): 501–502: Epub 20200129. PubMed PMID: 31996346. 10.1136/bjsports-2019-101403. [DOI] [PubMed] [Google Scholar]
- Dakic, Jodie G. , Cook Jill, Hay‐Smith Jean, Lin K.‐Yin, and Frawley Helena. 2021. “Pelvic Floor Disorders Stop Women Exercising: A Survey of 4556 Symptomatic Women.” Journal of Science and Medicine in Sport 24(12): 1211–1217. 10.1016/j.jsams.2021.06.003. [DOI] [PubMed] [Google Scholar]
- Daly, B. , Young S., Marla R., Riddell L., Junkin R., Weidenhammer N., Dolan J., Kinsella J., and Zhang R.. 2017. “Persistent Pain after Caesarean Section and its Association with Maternal Anxiety and Socioeconomic Background.” International Journal of Obstetric Anesthesia 29: 57–63. 10.1016/j.ijoa.2016.10.004. [DOI] [PubMed] [Google Scholar]
- Dane, Kathryn , Simms Ciaran, Hendricks Sharief, West Stephen W., Griffin Steffan, Nugent Frank J., Farrell Garreth, Mockler David, and Wilson Fiona. 2022. “Physical and Technical Demands and Preparatory Strategies in Female Field Collision Sports: A Scoping Review.” International Journal of Sports Medicine 43(14): 1173–1182. 10.1055/a-1839-6040. [DOI] [PubMed] [Google Scholar]
- de Graaff, Lisanne F. , Honig Adriaan, van Pampus Mariëlle G., and Stramrood Claire A. I.. 2018. “Preventing Post‐traumatic Stress Disorder Following Childbirth and Traumatic Birth Experiences: A Systematic Review.” Acta Obstetricia et Gynecologica Scandinavica 97(6): 648–656: Epub 20180302. PubMed PMID: 29336486. 10.1111/aogs.13291. [DOI] [PubMed] [Google Scholar]
- Delancey, J. , and Hurd W. W.. 1998. “Size of the Urogenital Hiatus in the Levator Ani Muscles in Normal Women and Women with Pelvic Organ Prolapse.” Obstetrics & Gynecology 91(3): 364–368: PubMed PMID: 9491861. 10.1016/s0029-7844(97)00682-0. [DOI] [PubMed] [Google Scholar]
- Delancey, J. O. , Kane Low L., Miller J. M., Patel D. A., and Tumbarello J. A.. 2008. “Graphic Integration of Causal Factors of Pelvic Floor Disorders: An Integrated Life Span Model.” American Journal of Obstetrics and Gynecology 199(6): 610.e1‐5: Epub 20080604. PubMed PMID: 18533115; PubMed Central PMCID: PMC2764236. 10.1016/j.ajog.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLancey, J. O. , Xie B., Pipitone F., Swenson C. W., Masteling M., and Chen L.. 2023. “Functional Anatomy of the Perineal Complex as it Relates to Urogenital Hiatus Closure.” American Journal of Obstetrics and Gynecology 228(3): S812–S813. 10.1016/j.ajog.2022.12.042. [DOI] [Google Scholar]
- DeLancey, John O. L. , Masteling Mariana, Pipitone Fernanda, LaCross Jennifer, Mastrovito Sara, and Ashton‐Miller James A.. 2024. “Pelvic Floor Injury during Vaginal Birth Is Life‐Altering and Preventable: What Can We Do about it?” American Journal of Obstetrics and Gynecology 230(3): 279.e2–294.e2. 10.1016/j.ajog.2023.11.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLancey, John O. L. , Sørensen Helle Christina, Lewicky‐Gaupp Christina, and Smith Tovia M.. 2012. “Comparison of the Puborectal Muscle on MRI in Women with POP and Levator Ani Defects with Those with Normal Support and No Defect.” International Urogynecology Journal 23(1): 73–77: Epub 20110806. PubMed PMID: 21822711; PubMed Central PMCID: PMC3508430. 10.1007/s00192-011-1527-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Mattos Lourenco, Thais Regina , Matsuoka Priscila Katsumi, Baracat Edmund Chada, and Haddad Jorge Milhem. 2018. “Urinary Incontinence in Female Athletes: A Systematic Review.” International Urogynecology Journal 29(12): 1757–1763: Epub 20180319. PubMed PMID: 29552736. 10.1007/s00192-018-3629-z. [DOI] [PubMed] [Google Scholar]
- Dietze‐Hermosa, Martin , Hitchcock Robert, Nygaard Ingrid E., and Shaw Janet M.. 2020. “Intra‐abdominal Pressure and Pelvic Floor Health: Should We Be Thinking about This Relationship Differently?” Urogynecology 26(7): 409–414. 10.1097/spv.0000000000000799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly, Gráinne M. , Brockwell Emma, Rankin Alan, and Moore Isabel S.. 2022. “Beyond the Musculoskeletal System: Considering Whole‐Systems Readiness for Running Postpartum.” The Journal of Women's & Pelvic Health Physical Therapy 46(1): 48–56: PubMed PMID: 01274882‐202201000‐00007. 10.1097/jwh.0000000000000218. [DOI] [Google Scholar]
- Donnelly, G. M. , and Moore I. S.. 2023. “Sports Medicine and the Pelvic Floor.” Current Sports Medicine Reports 22(3): 82–90: PubMed PMID: 00149619‐202303000‐00007. 10.1249/jsr.0000000000001045. [DOI] [PubMed] [Google Scholar]
- Donnelly, Grainne Marie , Rankin Alan, Mills Hayley, De Vivo Marlize, Goom Thomas S. H., and Brockwell Emma. 2020. “Guidance for Medical, Health and Fitness Professionals to Support Women in Returning to Running Postnatally.” British Journal of Sports Medicine 54(18): 1114–1115: Epub 20200506. PubMed PMID: 32376675. 10.1136/bjsports-2020-102139. [DOI] [PubMed] [Google Scholar]
- Donnelly, G. M. C. C. , Dane K., Elliot‐Sale K. J., Hayman M., McCarthy‐Ryan M. F., Perkins J., Rollins S., and Moore I. S.. 2024. “Prioritise Safety, Optimise Success! Return to Contact Sport Postpartum.” European Journal of Sport Science. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliasson, Kerstin , Edner Ann, and Mattsson Eva. 2008. “Urinary Incontinence in Very Young and Mostly Nulliparous Women with a History of Regular Organised High‐Impact Trampoline Training: Occurrence and Risk Factors.” International Urogynecology Journal 19(5): 687–696. 10.1007/s00192-007-0508-4. [DOI] [PubMed] [Google Scholar]
- Fleck, S. J. K. W . 2004. Designing Resistance Training Programs. 4th ed. Champaign, IL: Human Kinetics. [Google Scholar]
- Forner, Lori B. , Beckman Emma M., and Smith Michelle D.. 2020. “Symptoms of Pelvic Organ Prolapse in Women Who Lift Heavy Weights for Exercise: A Cross‐Sectional Survey.” International Urogynecology Journal 31(8): 1551–1558: Epub 20191207. PubMed PMID: 31813038. 10.1007/s00192-019-04163-w. [DOI] [PubMed] [Google Scholar]
- Garber, Carol Ewing , Blissmer Bryan, Deschenes Michael R., Franklin Barry A., Lamonte Michael J., Lee I.‐Min, Nieman David C., and Swain David P.. 2011. “American College of Sports Medicine Position Stand. Quantity and Quality of Exercise for Developing and Maintaining Cardiorespiratory, Musculoskeletal, and Neuromotor Fitness in Apparently Healthy Adults: Guidance for Prescribing Exercise.” Medicine & Science in Sports & Exercise 43(7): 1334–1359: PubMed PMID: 21694556. 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- Giagio, Silvia , Salvioli Stefano, Innocenti Tiziano, Gava Giulia, Vecchiato Marco, Pillastrini Paolo, and Turolla Andrea. 2023. “PFD‐SENTINEL: Development of a Screening Tool for Pelvic Floor Dysfunction in Female Athletes through an International Delphi Consensus.” British Journal of Sports Medicine 57(14): 899–905. 10.1136/bjsports-2022-105985. [DOI] [PubMed] [Google Scholar]
- Gollan, J. K. , Mesches G. A., and Gortner I. A.. 2021. “Chapter 20 ‐ Edinburgh postnatal Depression Scale: Description and Applications.” In The Neuroscience of Depression, edited by Martin C. R., Hunter L.‐A., Patel V. B., Preedy V. R. and Rajendram R., 205–210. Academic Press. [Google Scholar]
- Goncharenko, Vadym , Bubnov Rostyslav, Polivka Jiri, Zubor Pavol, Biringer Kamil, Bielik Tibor, Kuhn Walther, and Golubnitschaja Olga. 2019. “Vaginal Dryness: Individualised Patient Profiles, Risks and Mitigating Measures.” The EPMA Journal 10(1): 73–79: Epub 20190302. PubMed PMID: 30984316; PubMed Central PMCID: PMC6459457. 10.1007/s13167-019-00164-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield, Mari , Jomeen Julie, and Glover Lesley. 2016. “What Is Traumatic Birth? A Concept Analysis and Literature Review.” British Journal of Midwifery 24(4): 254–267. 10.12968/bjom.2016.24.4.254. [DOI] [Google Scholar]
- Hagen, Suzanne , Glazener Cathryn, McClurg Doreen, Macarthur Christine, Elders Andrew, Herbison Peter, Wilson Don, et al. 2017. “Pelvic Floor Muscle Training for Secondary Prevention of Pelvic Organ Prolapse (PREVPROL): A Multicentre Randomised Controlled Trial.” The Lancet 389(10067): 393–402. 10.1016/S0140-6736(16)32109-2. [DOI] [PubMed] [Google Scholar]
- Hagen, Suzanne , Stark Diane, Glazener Cathryn, Dickson Sylvia, Barry Sarah, Elders Andrew, Frawley Helena, et al. 2014. “Individualised Pelvic Floor Muscle Training in Women with Pelvic Organ Prolapse (POPPY): A Multicentre Randomised Controlled Trial.” Lancet 383(9919): 796–806: Epub 20131128. PubMed PMID: 24290404. 10.1016/s0140-6736(13)61977-7. [DOI] [PubMed] [Google Scholar]
- Hagins, Marshall , Pietrek Markus, Sheikhzadeh Ali, and Nordin Margareta. 2006. “The Effects of Breath Control on Maximum Force and IAP during a Maximum Isometric Lifting Task.” Clinical Biomechanics 21(8): 775–780. 10.1016/j.clinbiomech.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Hagovska, Magdalena , Svihra Ján, and Urdzik Peter. 2022. “Predictive Value of Pelvic Floor Muscle Morphometry Using 3D/4D Ultrasound in Relation to the Success of Pelvic Floor Muscle Training in Women with Stress Urinary Incontinence.” International Journal of Environmental Research and Public Health 19(22): 14757: Epub 20221110. PubMed PMID: 36429476; PubMed Central PMCID: PMC9690680. 10.3390/ijerph192214757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herschorn, S . 2004. “Female Pelvic Floor Anatomy: The Pelvic Floor, Supporting Structures, and Pelvic Organs.” Reviews in Urology 6(Suppl 5): S2–s10: PubMed PMID: 16985905; PubMed Central PMCID: PMC1472875. [PMC free article] [PubMed] [Google Scholar]
- Heyward, Omar , Emmonds Stacey, Roe Gregory, Scantlebury Sean, Stokes Keith, and Jones Ben. 2022. “Applied Sports Science and Sports Medicine in Women's Rugby: Systematic Scoping Review and Delphi Study to Establish Future Research Priorities.” BMJ Open Sport Exerc Med 8(3): e001287: Epub 20220721. PubMed PMID: 35979431; PubMed Central PMCID: PMC9310180. 10.1136/bmjsem-2021-001287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoff Brækken, Ingeborg , Majida Memona, Engh Marie Ellström, and Bø Kari. 2010. “Morphological Changes after Pelvic Floor Muscle Training Measured by 3‐dimensional Ultrasonography: A Randomized Controlled Trial.” Obstetrics & Gynecology 115(2 Pt 1): 317–324: PubMed PMID: 20093905. 10.1097/AOG.0b013e3181cbd35f. [DOI] [PubMed] [Google Scholar]
- Howard, D. , Miller J. M., Delancey J. O., and Ashton‐Miller J. A.. 2000. “Differential Effects of Cough, Valsalva, and Continence Status on Vesical Neck Movement.” Obstetrics & Gynecology 95(4): 535–540: PubMed PMID: 10725485; PubMed Central PMCID: PMC1226414. 10.1016/s0029-7844(99)00618-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes L. O. Heber M. E., Lahiri A., Harries M. Raftery, E. B . Haemodynamic Advantage of the Valsalva Manoeuvre during Heavy Resistance Training. European Heart Journal 1989;10(10):896–902, 10.1093/oxfordjournals.eurheartj.a059399. [DOI] [PubMed] [Google Scholar]
- Jackson, Thea , Bostock Emma L., Hassan Amal, Greeves Julie P., Sale Craig, and Elliott‐Sale Kirsty J.. 2022. “The Legacy of Pregnancy: Elite Athletes and Women in Arduous Occupations.” Exercise and Sport Sciences Reviews 50(1): 14–24. 10.1249/jes.0000000000000274. [DOI] [PubMed] [Google Scholar]
- Jaffar, Aida , Tan C.‐Eng, Mohd‐Sidik Sherina, Admodisastro Novia, and Goodyear‐Smith Felicity. 2022. “Persuasive Technology in an mHealth App Designed for Pelvic Floor Muscle Training Among Women: Systematic Review.” JMIR Mhealth Uhealth 10(3): e28751: Epub 20220322. PubMed PMID: 35315777; PubMed Central PMCID: PMC8984823. 10.2196/28751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston, Catherine L. , Negus Michael F., Rossiter Michael A., and Phillips Christian G.. 2023. “A National Survey of Urinary Incontinence in Professional Team England Female Athletes.” European Journal of Obstetrics & Gynecology and Reproductive Biology 282: 12–16. 10.1016/j.ejogrb.2022.12.031. [DOI] [PubMed] [Google Scholar]
- Junginger, Baerbel , Baessler Kaven, Sapsford Ruth, and Hodges Paul W.. 2010. “Effect of Abdominal and Pelvic Floor Tasks on Muscle Activity, Abdominal Pressure and Bladder Neck.” International Urogynecology Journal 21(1): 69–77. 10.1007/s00192-009-0981-z. [DOI] [PubMed] [Google Scholar]
- Kainu, J. P. , Sarvela J., Tiippana E., Halmesmäki E., and Korttila K. T.. 2010. “Persistent Pain after Caesarean Section and Vaginal Birth: A Cohort Study.” International Journal of Obstetric Anesthesia 19(1): 4–9: Epub 20090903. PubMed PMID: 19733050. 10.1016/j.ijoa.2009.03.013. [DOI] [PubMed] [Google Scholar]
- Karsten, Matty D. A. , Wekker Vincent, Bakker Anne, Groen Henk, Olff Miranda, Hoek Annemieke, Laan Ellen T. M., and Roseboom Tessa J.. 2020. “Sexual Function and Pelvic Floor Activity in Women: The Role of Traumatic Events and PTSD Symptoms.” European Journal of Psychotraumatology 11(1): 1764246: Epub 20200616. PubMed PMID: 33029306; PubMed Central PMCID: PMC7473031. 10.1080/20008198.2020.1764246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawabata, Masashi , Shima Norihiro, Hamada Hatsuyuki, Nakamura Isamu, and Nishizono Hidetsugu. 2010. “Changes in Intra‐abdominal Pressure and Spontaneous Breath Volume by Magnitude of Lifting Effort: Highly Trained Athletes versus Healthy Men.” European Journal of Applied Physiology 109(2): 279–286. 10.1007/s00421-009-1344-7. [DOI] [PubMed] [Google Scholar]
- Kearney, Rohna , Sawhney Raja, and DeLancey John O. L.. 2004. “Levator Ani Muscle Anatomy Evaluated by Origin‐Insertion Pairs.” Obstetrics & Gynecology 104(1): 168–173: PubMed PMID: 00006250‐200407000‐00026. 10.1097/01.AOG.0000128906.61529.6b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kharaji, Ghazal , Nikjooy Afsaneh, Amiri Ali, and Sanjari Mohammad Ali. 2019. “Proprioception in Stress Urinary Incontinence: A Narrative Review.” Medical Journal of the Islamic Republic of Iran 33: 60: PubMed Epub 20190625. PMID: 31456984; PubMed Central PMCID: PMC6708112. 10.34171/mjiri.33.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krofta, Ladislav , Havelková Linda, Urbánková Iva, Krčmář Michal, Hynčík Luděk, and Feyereisl Jaroslav. 2017. “Finite Element Model Focused on Stress Distribution in the Levator Ani Muscle during Vaginal Delivery.” International Urogynecology Journal 28(2): 275–284: Epub 20160825. PubMed PMID: 27562467; PubMed Central PMCID: PMC5306065. 10.1007/s00192-016-3126-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruger, J. A. , Dietz H. P., and Murphy B. A.. 2007. “Pelvic Floor Function in Elite Nulliparous Athletes.” Ultrasound in Obstetrics and Gynecology 30(1): 81–85: PubMed PMID: 17497753. 10.1002/uog.4027. [DOI] [PubMed] [Google Scholar]
- Leinweber, Julia , Fontein‐Kuipers Yvonne, Thomson Gill, Karlsdottir Sigfridur Inga, Nilsson Christina, Ekström‐Bergström Anette, Olza Ibone, Hadjigeorgiou Eleni, and Stramrood Claire. 2022. “Developing a Woman‐Centered, Inclusive Definition of Traumatic Childbirth Experiences: A Discussion Paper.” Birth 49(4): 687–696: Epub 20220411. PubMed PMID: 35403241. 10.1111/birt.12634. [DOI] [PubMed] [Google Scholar]
- Leitner, Monika , Moser Helene, Eichelberger Patric, Kuhn Annette, and Radlinger Lorenz. 2017. “Evaluation of Pelvic Floor Muscle Activity during Running in Continent and Incontinent Women: An Exploratory Study.” Neurourology and Urodynamics 36(6): 1570–1576: Epub 20161029. PubMed PMID: 27794169. 10.1002/nau.23151. [DOI] [PubMed] [Google Scholar]
- Lovegrove Jones, Ruth C. , Peng Qiyu, Stokes Maria, Humphrey Victor F., Payne Christopher, and Constantinou Christos E.. 2010. “Mechanisms of Pelvic Floor Muscle Function and the Effect on the Urethra during a Cough.” European Urology 57(6): 1101–1110: Epub 20090621. PubMed PMID: 19560261; PubMed Central PMCID: PMC2889228. 10.1016/j.eururo.2009.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazi, Baraa , Kaddour Ouhoud, and Al‐Badr Ahmed. 2019. “Depression Symptoms in Women with Pelvic Floor Dysfunction: A Case‐Control Study.” International Journal of Women's Health 11: 143–148: Epub 20190222. PubMed PMID: 30863189; PubMed Central PMCID: PMC6390859. 10.2147/ijwh.S187417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy‐Ryan, Molly , Perkins Joanna, Donnelly Gráinne M., Caithriona Yeomans, Liston Mairead, Leahy Karina, Bø Kari, O'Halloran Patrick, and Moore Isabel S.. 2024. “Urinary Incontinence Prevalence and Risk Factors in Female Rugby Union Players: A Common Health Problem across Four Nations.” BMJ Open Sport & Exercise Medicine 10(1): e001832. 10.1136/bmjsem-2023-001832. [DOI] [Google Scholar]
- Menezes, Enaiane Cristina , da Silva Pereira Franciele, Porto Rafaela Maria, Fank Felipe, and Mazo Giovana Zarpellon. 2023. “Effect of Exercise on Female Pelvic Floor Morphology and Muscle Function: A Systematic Review.” International Urogynecology Journal 34(5): 963–977. 10.1007/s00192-022-05375-3. [DOI] [PubMed] [Google Scholar]
- Miller, Janis M. , Low Lisa Kane, Zielinski Ruth, Smith Abigail R., DeLancey John O. L., and Brandon Catherine. 2015. “Evaluating Maternal Recovery from Labor and Delivery: Bone and Levator Ani Injuries.” American Journal of Obstetrics and Gynecology 213(2): 188.e1–188.e11: Epub 20150505. PubMed PMID: 25957022; PubMed Central PMCID: PMC4519404. 10.1016/j.ajog.2015.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore, Isabel S. , Crossley Kay M., Bo Kari, Mountjoy Margo, Ackerman Kathryn E., Antero Juliana da Silva, Sundgot Borgen Jorunn, et al. 2023. “Female Athlete Health Domains: A Supplement to the International Olympic Committee Consensus Statement on Methods for Recording and Reporting Epidemiological Data on Injury and Illness in Sport.” British Journal of Sports Medicine 57(18): 1164–1174: bjsports‐2022‐106620. 10.1136/bjsports-2022-106620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore, Isabel S. , James Megan L., Brockwell Emma, Perkins Joanna, Jones Alex L., and Donnelly Gráinne M.. 2021. “Multidisciplinary, Biopsychosocial Factors Contributing to Return to Running and Running Related Stress Urinary Incontinence in Postpartum Women.” British Journal of Sports Medicine 55(22): 1286–1292. 10.1136/bjsports-2021-104168. [DOI] [PubMed] [Google Scholar]
- Moore, Isabel S. , McCarthy‐Ryan Molly, Palmer Debbie, Perkins Joanna, and Verhagen Evert. 2024. “Is Your System Fit for Purpose? Female Athlete Health Considerations for Rugby Injury and Illness Surveillance Systems.” European Journal of Sport Science: Special Issue. 10.1002/ejsc.12089. [DOI] [PubMed] [Google Scholar]
- Moser, Helene , Leitner Monika, Baeyens J.‐Pierre, and Radlinger Lorenz. 2018. “Pelvic Floor Muscle Activity during Impact Activities in Continent and Incontinent Women: A Systematic Review.” International Urogynecology Journal 29(2): 179–196. 10.1007/s00192-017-3441-1. [DOI] [PubMed] [Google Scholar]
- Moser, Helene , Leitner Monika, Eichelberger Patric, Kuhn Annette, Baeyens J.‐Pierre, and Radlinger Lorenz. 2019. “Pelvic Floor Muscle Displacement during Jumps in Continent and Incontinent Women: An Exploratory Study.” Neurourology and Urodynamics 38(8): 2374–2382: Epub 20190907. PubMed PMID: 31493349. 10.1002/nau.24161. [DOI] [PubMed] [Google Scholar]
- Nagahara, Ryu , and Girard Olivier. 2021. “Alterations of Spatiotemporal and Ground Reaction Force Variables during Decelerated Sprinting.” Scandinavian Journal of Medicine & Science in Sports 31(3): 586–596: Epub 20201201. PubMed PMID: 33217086. 10.1111/sms.13884. [DOI] [PubMed] [Google Scholar]
- NICE . 2021. Pelvic Floor Dysfunction: Prevention and Non‐surgical Management. National Institute of Clinical Guidelines.NG210. [Google Scholar]
- Ninomiya, Sanae , Saito Izumi, Masaki Kiyoko, Endo Yoshihiro, Morikawa Shigehiro, and Okayama Hisayo. 2014. “Single‐Arm Pilot Study to Determine the Effectiveness of the Support Power of Underwear in Elevating the Bladder Neck and Reducing Symptoms of Stress Urinary Incontinence in Women.” Lower Urinary Tract Symptoms 6(2): 81–87: Epub 20130620. PubMed PMID: 26663545. 10.1111/luts.12023. [DOI] [PubMed] [Google Scholar]
- Okayama, Hisayo , Ninomiya Sanae, Naito Kiyoko, Endo Yoshihiro, and Morikawa Shigehiro. 2019. “Effects of Wearing Supportive Underwear versus Pelvic Floor Muscle Training or No Treatment in Women with Symptoms of Stress Urinary Incontinence: An Assessor‐Blinded Randomized Control Trial.” International Urogynecology Journal 30(7): 1093–1099: Epub 20190109. PubMed PMID: 30627829. 10.1007/s00192-018-03855-z. [DOI] [PubMed] [Google Scholar]
- Okeahialam, Nicola Adanna , Oldfield Maria, Stewart Ellie, Bonfield Carol, and Carboni Cristiane. 2022. “Pelvic Floor Muscle Training: A Practical Guide.” BMJ 378: e070186. 10.1136/bmj-2022-070186. [DOI] [Google Scholar]
- Peinado‐Molina, Rocío Adriana , Hernández‐Martínez Antonio, Martínez‐Vázquez Sergio, Rodríguez‐Almagro Julián, and Martínez‐Galiano Juan Miguel. 2023. “Pelvic Floor Dysfunction: Prevalence and Associated Factors.” BMC Public Health 23(1): 2005: Epub 20231014. PubMed PMID: 37838661; PubMed Central PMCID: PMC10576367. 10.1186/s12889-023-16901-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelvic Obstetric and Gynaecological Physiotherapy . 2022. POGP EXERCISE and ADVICE after Pregnancy POGP: https://thepogp.co.uk/Resources/113/exercise_and_advice_after_pregnancy.
- Pergialiotis, Vasilios , Bellos Ioannis, Fanaki Maria, Vrachnis Nikolaos, and Doumouchtsis Stergios K.. 2020. “Risk Factors for Severe Perineal Trauma during Childbirth: An Updated Meta‐Analysis.” European Journal of Obstetrics & Gynecology and Reproductive Biology 247: 94–100. 10.1016/j.ejogrb.2020.02.025. [DOI] [PubMed] [Google Scholar]
- Prevett, C. , and Moore R.. 2024. “Nuances of the Valsalva Manoeuvre and Bracing with Regard to Resistance Training Performance and its Effects on the Pelvic Floor.” Journal of Pelvic, Obstetric and Gynaecological Physiotherapy 134(Spring): 31–34. 10.62399/yxrs8863. [DOI] [Google Scholar]
- Ritchie, Dean , Hopkins Will G., Buchheit Martin, Cordy Justin, and Bartlett Jonathan D.. 2017. “Quantification of Training Load during Return to Play after Upper‐ and Lower‐Body Injury in Australian Rules Football.” International Journal of Sports Physiology and Performance 12(5): 634–641: Epub 20160915. PubMed PMID: 27632415. 10.1123/ijspp.2016-0300. [DOI] [PubMed] [Google Scholar]
- Roch, Mélanie , Gaudreault Nathaly, Cyr M.‐Pierre, Venne Gabriel, Bureau Nathalie J., and Morin Mélanie. 2021. “The Female Pelvic Floor Fascia Anatomy: A Systematic Search and Review.” Life (Basel) 11(9): 900: Epub 20210830. PubMed PMID: 34575049; PubMed Central PMCID: PMC8467746. 10.3390/life11090900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandwith, Emily , and Robert Magali. 2021. “Rug‐pee Study: The Prevalence of Urinary Incontinence Among Female University Rugby Players.” International Urogynecology Journal 32(2): 281–285: Epub 20200828. PubMed PMID: 32857177. 10.1007/s00192-020-04510-2. [DOI] [PubMed] [Google Scholar]
- Sapsford, Ruth R. , and Hodges Paul W.. 2001. “Contraction of the Pelvic Floor Muscles during Abdominal Maneuvers.” Archives of Physical Medicine and Rehabilitation 82(8): 1081–1088: PubMed PMID: 11494188. 10.1053/apmr.2001.24297. [DOI] [PubMed] [Google Scholar]
- Shaw Janet M., Hamad Nadia M., Coleman Tanner J., Egger Marlene J., Hsu Yvonne, Hitchcock Robert, Nygaard, Ingrid E . Intra‐abdominal Pressures during Activity in Women Using an Intra‐vaginal Pressure Transducer. Journal of Sports Sciences. 2014;32(12):1176–1185. oi: 10.1080/02640414.2014.889845. Epub 20140228. PubMed PMID: 24575741; PubMed Central PMCID: PMC3992988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shorey, Shefaly , and Wong Phyllis Zhi En. 2022. “Traumatic Childbirth Experiences of New Parents: A Meta‐Synthesis.” Trauma, Violence, & Abuse 23(3): 748–763: PubMed Epub 20201201. PMID: 33256544. 10.1177/1524838020977161. [DOI] [PubMed] [Google Scholar]
- Siahkal, Shahla Faal , Iravani Mina, Mohaghegh Zeynab, Sharifipour Foruzan, Zahedian Maryam, and Nasab Maryam Beheshti. 2021. “Investigating the Association of the Dimensions of Genital Hiatus and Levator Hiatus with Pelvic Organ Prolapse: A Systematic Review.” International Urogynecology Journal 32(8): 2095–2109. 10.1007/s00192-020-04639-0. [DOI] [PubMed] [Google Scholar]
- Skaug, K. , Engh M., and Bø K.. 2023. “282 ‐ Acute Effect of Heavy Weightlifting on the Pelvic Floor Muscles – An Experimental Crossover Study.” Continence 7: 100999. 10.1016/j.cont.2023.100999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skaug, Kristina Lindquist , Engh Marie Ellström, Frawley Helena, and Bø Kari. 2022. “Prevalence of Pelvic Floor Dysfunction, Bother, and Risk Factors and Knowledge of the Pelvic Floor Muscles in Norwegian Male and Female Powerlifters and Olympic Weightlifters.” The Journal of Strength & Conditioning Research 36(10): 2800–2807: Epub 20201203. PubMed PMID: 33278274. 10.1519/jsc.0000000000003919. [DOI] [PubMed] [Google Scholar]
- Smith, Michelle D. , Coppieters Michel W., and Hodges Paul W.. 2007. “Postural Response of the Pelvic Floor and Abdominal Muscles in Women with and without Incontinence.” Neurourology and Urodynamics 26(3): 377–385. 10.1002/nau.20336. [DOI] [PubMed] [Google Scholar]
- Stær‐Jensen, Jette , Siafarikas Franziska, Hilde Gunvor, Benth Jūratė Šaltytė, Bø Kari, and Engh Marie Ellström. 2015. “Postpartum Recovery of Levator Hiatus and Bladder Neck Mobility in Relation to Pregnancy.” Obstetrics & Gynecology 125(3): 531–539: PubMed PMID: 25730212. 10.1097/aog.0000000000000645. [DOI] [PubMed] [Google Scholar]
- Stær‐Jensen, Jette , Siafarikas Franziska, Hilde Gunvor, Bø Kari, and Engh Marie Ellström. 2013. “Ultrasonographic Evaluation of Pelvic Organ Support during Pregnancy.” Obstetrics & Gynecology 122(2 Pt 1): 329–336: PubMed PMID: 23969802. 10.1097/AOG.0b013e318299f62c. [DOI] [PubMed] [Google Scholar]
- Sudol, Neha T. , Adams‐Piper Emily, Perry Rachel, Lane Felicia, and Chen Katherine T.. 2019. “In Search of Mobile Applications for Patients with Pelvic Floor Disorders.” Urogynecology 25(3): 252–256: PubMed PMID: 01436319‐201905000‐00011. 10.1097/spv.0000000000000527. [DOI] [PubMed] [Google Scholar]
- Taghizadeh, Ziba , Irajpour Alireza, and Arbabi Mohammad. 2013. “Mothers' Response to Psychological Birth Trauma: A Qualitative Study.” Iranian Red Crescent Medical Journal 15(10): e10572: Epub 20131005. PubMed PMID: 24693361; PubMed Central PMCID: PMC3950773. 10.5812/ircmj.10572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiagamoorthy, G. , Johnson A., Thakar R., and Sultan A. H.. 2014. “National Survey of Perineal Trauma and its Subsequent Management in the United Kingdom.” International Urogynecology Journal 25(12): 1621–1627: Epub 20140516. PubMed PMID: 24832856. 10.1007/s00192-014-2406-x. [DOI] [PubMed] [Google Scholar]
- Thomaz, Rafaela Prusch , Colla Cássia, Darski Caroline, and Paiva Luciana Laureano. 2018. “Influence of Pelvic Floor Muscle Fatigue on Stress Urinary Incontinence: A Systematic Review.” International Urogynecology Journal 29(2): 197–204: Epub 20171220. PubMed PMID: 29264615. 10.1007/s00192-017-3538-6. [DOI] [PubMed] [Google Scholar]
- Tracy Paige V., DeLancey John O., & Ashton‐Miller James A. A Geometric Capacity–Demand Analysis of Maternal Levator Muscle Stretch Required for Vaginal Delivery. Journal of Biomechanical Engineering. 2016;138(2). 10.1115/1.4032424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trewartha, Grant , Preatoni Ezio, England Michael E., and Stokes Keith A.. 2015. “Injury and Biomechanical Perspectives on the Rugby Scrum: A Review of the Literature.” British Journal of Sports Medicine 49(7): 425–433: Epub 20140107. PubMed PMID: 24398223. 10.1136/bjsports-2013-092972. [DOI] [PubMed] [Google Scholar]
- Usman, Juliana , McIntosh Andrew S., and Fréchède Bertrand. 2011. “An Investigation of Shoulder Forces in Active Shoulder Tackles in Rugby Union Football.” Journal of Science and Medicine in Sport 14(6): 547–552: PubMed PMID: 21689986. 10.1016/j.jsams.2011.05.006. [DOI] [PubMed] [Google Scholar]
- Wang, Ziyi , Liu Jiaye, Shuai Huan, Cai Zhongxiang, Fu Xia, Liu Yang, Xiao Xiong, et al. 2021. “Mapping Global Prevalence of Depression Among Postpartum Women.” Translational Psychiatry 11(1): 543. 10.1038/s41398-021-01663-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West, Stephen W. , Shill Isla J., Clermont Christian, Pavlovic Nina, Cairns Joshua, Seselja Berlyn, Hancock Matthew V., Roberts Simon P., Hendricks Sharief, and Emery Carolyn A.. 2022. “Same Name, Same Game, but Is it Different? an Investigation of Female Rugby Union Match Events in Canadian Varsity Players.” International Journal of Sports Science & Coaching 17(5): 1119–1127. 10.1177/17479541211051961. [DOI] [Google Scholar]
- Williams, Alison M. M. , Sato‐Klemm Maya, Deegan Emily G., Eginyan Gevorg, and Lam Tania. 2022. “Characterizing Pelvic Floor Muscle Activity during Walking and Jogging in Continent Adults: A Cross‐Sectional Study.” Frontiers in Human Neuroscience 16: 912839: Epub 20220630. PubMed PMID: 35845247; PubMed Central PMCID: PMC9279930. 10.3389/fnhum.2022.912839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodhouse, Luke Nicholas , Tallent Jamie, Patterson Stephen David, and Waldron Mark. 2021. “Elite International Female Rugby Union Physical Match Demands: A Five‐Year Longitudinal Analysis by Position and Opposition Quality.” Journal of Science and Medicine in Sport 24(11): 1173–1179: Epub 20210406. PubMed PMID: 33858761. 10.1016/j.jsams.2021.03.018. [DOI] [PubMed] [Google Scholar]
- Woodley, Stephanie J. , Lawrenson Peter, Boyle Rhianon, Cody June D., Mørkved Siv, Kernohan Ashleigh, and Hay‐Smith E. Jean C.. 2020. “Pelvic Floor Muscle Training for Preventing and Treating Urinary and Faecal Incontinence in Antenatal and Postnatal Women.” Cochrane Database of Systematic Reviews 5(5): Cd007471: Epub 20200506. PubMed PMID: 32378735; PubMed Central PMCID: PMC7203602. 10.1002/14651858.CD007471.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Rugby . 2024. Return to Rugby Union Postpartum Guidelines: Elite Pathway. 10.25401/cardiffmet.24759906. [DOI]
- Xuan, Y. , Friedman T., and Dietz H. P.. 2019. “Does Levator Ani Hiatal Area Configuration Affect Pelvic Organ Prolapse?” Ultrasound in Obstetrics and Gynecology 54(1): 124–127: Epub 20190612. PubMed PMID: 30584675. 10.1002/uog.20210. [DOI] [PubMed] [Google Scholar]


