Summary
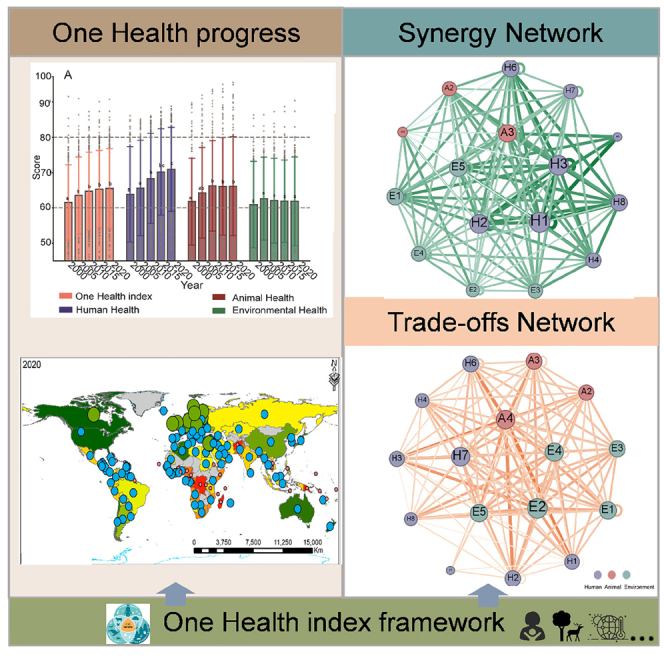
The One Health (OH) approach, integrating aspects of human, animal, and environmental health, still lacks robustly quantified insights into its complex relationships. To fill this knowledge gap, we devised a comprehensive assessment scheme for OH to assess its progress, synergies, trade-offs, and priority targets. From 2000 to 2020, we find evidence for global progress toward OH, albeit uneven, with its average score rising from 61.6 to 65.5, driven primarily by better human health although environmental health lags. Despite synergies prevalent within and between the three health dimensions, over half of the world’s countries, mainly low-income ones, still incur substantial trade-offs impeding OH’s advancement, especially between animal and environmental health. Our in-depth analysis of synergy and trade-off networks reveals that maternal, newborn, and child health are critical synergistic targets, whereas biodiversity and land resources dominate trade-offs. We provide key information for the synergetic and uniform development of global OH and policymaking.
Subject areas: Health sciences, Environment, Animal health management, Social sciences
Graphical abstract
Highlights
-
•
A framework for measuring One Health progress and relationships is developed
-
•
No country performs well in human, animal, and environmental health
-
•
Environmental degradation constrains the realization of One Health
-
•
Child health, animal biodiversity, and land resources should be prioritized
Health sciences; Environment; Animal health management; Social sciences
Introduction
Human, animal, and environmental health are three intricately interconnected domains that collectively influence global security.1,2 Healthy humans have complete physical, psychological, and mental well-being, including positive social relationships.3 Healthy animals are free of physiological, psychological, and behavioral diseases, which enables them to survive and reproduce normally within their habitats.4 Environmental health focuses chiefly on air, water, and soil quality, a stable climate, the safe use of chemicals and waste management, and biodiversity conservation.5 An array of global changes is increasing the risk of infectious disease outbreaks, threatening both human and animal health and jeopardizing the healthcare systems of countries.6 About 75% of all emerging infectious diseases are zoonotic, such as COVID-19, Ebola, and Zika pandemics and epidemics caused by viruses, most of which are influenced by various environmental factors.7 Accordingly, given the evolving global landscape of potential epidemics, the World Health Organization (WHO) Pandemic Agreement indicates that there is now an impetus to design and apply a more integrated framework to strengthen pandemic prevention, preparedness, and response.2
The One Health High-Level Expert Panel (OHHLEP)—on which sit members of the Food and Agriculture Organization of the United Nations, the World Organization for Animal Health, the WHO, and the United Nations Environment Program—has defined One Health (OH) as an integrated, unifying approach that aims to sustainably balance and optimize the health of people, animals, and ecosystem.8 The OH approach is recognized as the currently most effective and sustainable method for averting, readying for, and detecting interconnected health threats, particularly for mitigating the impact of emerging infectious disease outbreaks.9 For example, USAID’s PREDICT project initiated in 2009 has implemented a targeted, risk-based surveillance strategy based on the OH approach to detect the sources of viruses as soon as possible and gauge their risk of spillover.10 This strategy has been very successful so far and has been used to help governments worldwide investigate, detect, and mitigate emerging major disease threats.
Since the introduction of OH in the late 1990s, much effort has been directed to how to measure progress toward achieving OH.11 Zhang and colleagues12 proposed a health cell-like framework that takes a holistic perspective, which can serve as an assessment tool to measure OH performance and gauge the impact of economic and policy-related factors on the three health dimensions. Despite advances in refining the OH concept and its assessment frameworks, vexing challenges prevail in identifying key priorities and quantifying the progress of countries whose socioeconomic, cultural, natural, and health realities differ variously.12 OHHLEP has developed an over-arching Theory of Change in addition to the OH definition that provides a conceptual framework and theoretical foundation for its implementation and evaluation.13,14 Therefore, a systematic analysis of the complex relationships among three health dimensions on both the global and national scale is imperative for distinguishing those priorities and safeguarding OH.15 Employing digital technologies—including artificial intelligence (AI), big data, and related digital technologies—in the operationalization of OH fosters interdisciplinary collaboration and data sharing.16 AI-assisted negotiations based on large language models can promote transparency in balancing diverse risks.17 Nonetheless, a fragmented, distributed, and heterogeneous data environment, coupled with limited access to health data, is hampering the development of systematic data-driven health solutions.16
Several studies have analyzed from different perspectives how the environment and animals could impact human health, e.g., via habitat destruction, environmental pollution, and climate change, all of which can spur the emergence and expand the spatial range of infectious diseases.6,18 Animals are crucial vectors for many potent diseases, such as the syndrome coronavirus and the Ebola virus.19 They are affected by environmental changes and human activities that alter the population and range of host species, as well as their geographical distribution and habitats. These changes contribute to a greater risk of animal-to-human spillover events in newly discovered viruses.20
Despite a better understanding of how environmental and animal factors can influence human health, we still lack systematic, real-world, data-driven assessments and analyses of general relationships within the three health dimensions in terms of synergies (where progress in one goal facilitates another’s advancement) or trade-offs (where progress in one goal impedes another’s advancement), especially regarding their spatial differentiation.21,22 This gap hinders unified progress toward OH, potentially limiting its ability to bolster responses to public health crises. Consequently, this impairs the effective application of the OH approach in crafting policies and corresponding action.23
To comprehensively address this gap, we designed a holistic OH assessment scheme based on the Global One Health Index and health-related Sustainable Development Goals (SDGs) (Tables S1 and S2). Next, we standardized these indicators and analyzed their relationships using Spearman correlations. We then separately examined these statistically significant relationships within OH at both the global and national scales. Our study answers three questions: (1) what are the spatiotemporal characteristics of progress toward OH from 2000 to 2020? (2) which synergies and trade-offs exist between and within the human, animal, and environmental health dimensions? and (3) what are the key synergistic and trade-off targets influencing progress in OH globally and nationally? By quantitatively addressing these pressing questions, our findings can guide countries in pinpointing their health priorities based on relationships between different health aspects, thereby ultimately supporting the promotion of sustainable development and enhancing human responses to global crises.
Results
Spatiotemporal dynamics of OH at the global and national scale
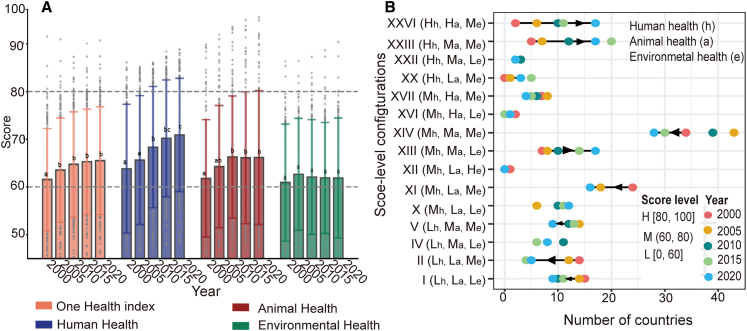
Our results revealed remarkable progress in the globally averaged OH index, which reached 65.54 in 2020, significantly improving over its 2000 benchmark (Figure 1A, p < 0.05). However, this progress is uneven, with disparities across different health dimensions and countries worldwide. This uneven progress toward OH suggests that its benefits are not universally experienced, with several prominent countries deteriorating in their environmental health despite the global increase in OH. In particular, this improvement has been driven by gains in human health, whereas advances in environmental health have been sluggish, stagnant, or reversed (Figure 1A). Specifically, between 2000 and 2020, human health increased by 14.21%, animal health by 7.07%, and environmental health by 2.45%. However, 15.71% of countries in this period incurred negative growth in their respective OH index (Figure S1). Individually, 14.29%, 30.41%, and 38.74% of countries saw human, animal, and environmental health declines, respectively (Figure S1).
Figure 1.
Global One Health progressed and changed in the number of countries with three configurations of scores for human, animal, and environmental health worldwide from 2000 to 2020
(A) Global annual average score of the One Health index, human, animal, and environmental health, from 2000 to 2020. The bar height represents the mean. The upper bound is defined as Q3 + 1.5 ∗ IQR, while the lower bound is Q1 − 1.5 ∗ IQR, where Q1 and Q3 are the 25th and 75th percentiles, respectively, and IQR is the interquartile range for the sample of 148 countries (n = 148).
(B) Countries were grouped into 15 configurations of score levels for human (h), animal (a), and environmental health (e) (see STAR Methods, Table S3). Those with scores ≥80 are performing well (H), those with scores ≤60 are facing substantial challenges (L), and those with scores between 60 and 80 are performing moderately (M).
From their health configurations, we could not find any country that performed well, with a score ≥80, in each of the three health dimensions (Figure S1). This was mainly because no country has an environmental health score above 80 (Figures S1 and S2). This finding suggests that even high-income countries can face substantial hurdles in achieving OH. Moreover, despite gains in OH, formidable challenges persist in improving all three health dimensions. For example, there is a notable rise in the number of countries whose configuration is (Hh, Ha, Me)—well-performing human health, well-performing animal health, with moderately performing (60 < scores <80) environmental health—and likewise (Hh, Ma, Me). Both configurations rose by 750% and 240%, mainly concentrated in high-income and upper-middle-income countries in Europe and North America (Figures 1B and S2).
Moreover, the number of lower-middle-income and low-income countries with daunting configurations, such as (Lh, La, Le) (scores ≤60), (Lh, La, Me), and (Mh, La, Me), experienced a marked decline, respectively falling by 40%, 64.29%, and 33.33%. More importantly, as of 2020, progress toward OH faced considerable challenges across all three health dimensions (Lh, La, Le) in nine middle-income and low-income countries in Asia and Africa (Figure S2). They include four low-income countries (i.e., Afghanistan, the Democratic Republic of the Congo, Burkina Faso, and Madagascar), one upper-middle-income country (Equatorial Guinea), and four middle-income countries (i.e., the Federated States of Micronesia, Papua New Guinea, Solomon Islands, and Kiribati).
Synergies and trade-offs between human, animal, and environmental health
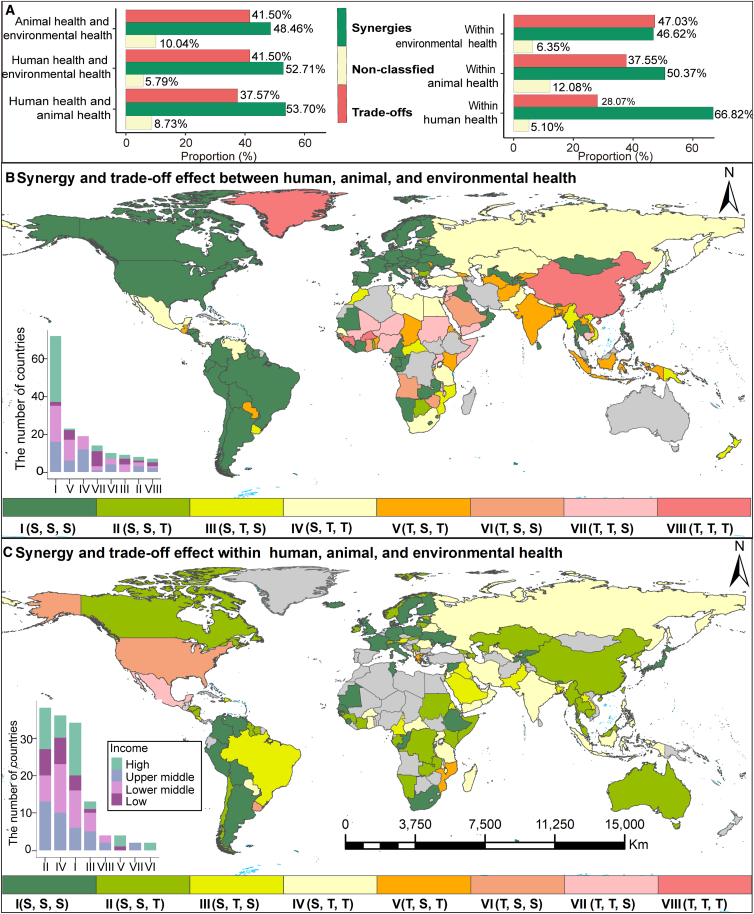
We consistently found a higher proportion of synergies (S) than trade-offs (T) between the three health dimensions. Globally, synergy proportions (S) exceeded trade-offs (T) with absolute differences of 16.13%, 11.20%, and 6.95% for human-animal, human-environmental, and animal-environmental health, respectively (Figure 2A). This implies a trend of mutual enhancement rather than constraint across different health dimensions. Nationally, similar patterns characterized most countries, indicating the prevalence of synergies. Encouragingly, we find that 37.7% of countries have synergistic effects in all three health dimensions (S, S, S), concentrated in high-income and middle-income countries in Europe and the Americas (Figures 2B and S3).
Figure 2.
Global-scale relationship proportions and geographic patterns of synergies and trade-offs between and within human, animal, and environmental health dimensions across countries
(A) Proportion of synergy (green), trade-off (red), and non-classified (yellow) observed between and within three health dimensions at the global scale.
(B) Mapped relationships between these dimensions (human-animal health, human-animal health, and animal-animal health).
(C) The country-level relationships within each health dimension (human, animal, and environmental health). The bar chart inset shows the number of countries with different income levels in various interactive configurations of three health dimensions (both within and between dimensions). The “T” indicates a higher proportion of trade-offs than synergies, while the “S” indicates a higher proportion of synergies than trade-offs.
Despite synergistic effects being widespread, some countries still face substantial challenges to achieving uniform development across three health dimensions, especially in regions with lower income (Figure 2B). Hence, progress along a single health dimension in these countries might negatively impact another. For instance, more than 89 low- and middle-income countries, mainly in Africa and Asia, harbor at least one trade-off across the three health dimensions. Of them, 56 countries displayed additional trade-offs in the other two health relationships. Specifically, 23, 19, and 14 countries, respectively, feature (T, S, T), (S, T, T), and (T, T, S) configurations. Crucially, we identified six countries with trade-offs across all three health dimensions, i.e., (T, T, T), irrespective of their income level (Figure 2B). This group includes not only the low-income countries Guinea, Solomon Islands, and Burkina Faso but also high-income countries (Seychelles) and two upper-middle-income countries (China and Fiji).
Our results show that environmental health faced substantial challenges for relationships within each health dimension, given its higher proportion of trade-offs than synergies (Figure 2A). This pattern was consistently found across countries with varying income levels (Figure S3). According to the interactive health configurations, trade-offs within animal health also pose a critical obstacle, predominantly in low and lower-middle-income countries (Figure 2C). Further, within all three health dimensions, relationships dominated by synergies, i.e., (S, S, S), were prominent in 34 high-income and lower-middle-income countries, mainly in Europe and South America. In contrast, only four island countries had more trade-offs than synergies (Figure 2C).
Although high-income countries exhibit more synergies and low-income countries more trade-offs, this pattern does not hold for all relationships within or between the three health dimensions (Figure S3). For greater insight into the complexities of different health relationships, we analyzed how these shifted with progress in OH. This revealed that when a country’s synergy proportions increase within and between health dimensions, its OH index also rises. Conversely, more trade-off proportions are associated with a lower country OH index (Figures 3 and S4–S8).
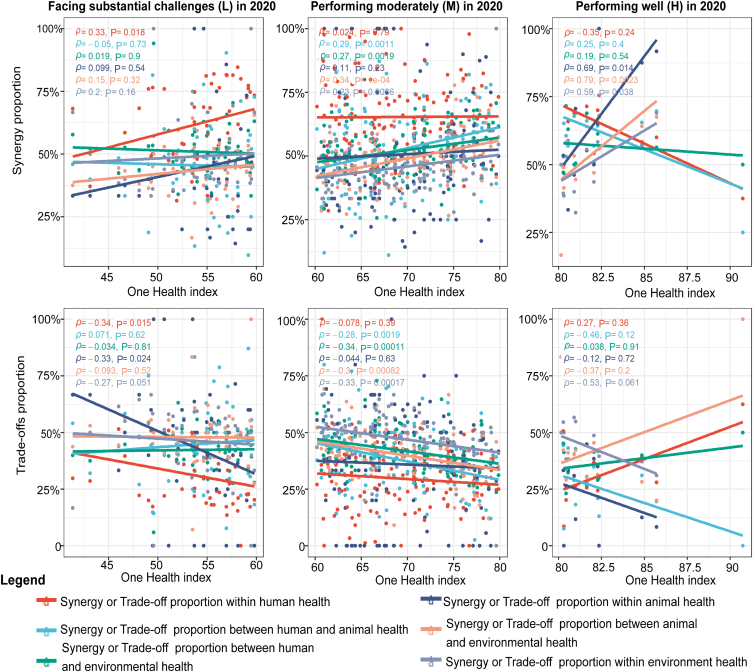
Figure 3.
Correlations between the One Health index and the proportion of synergies or trade-offs within and between human, animal, and environmental health in countries worldwide in 2020, respectively, at three levels of the One Health index
The three levels included countries with scores ≥80 as performing well (H), those with scores ≤60 as facing substantial challenges (L), and scores between 60 and 80 as performing moderately (M). We used linear regression models to fit lines between the One Health index of countries and the proportion of synergies or trade-offs between and within the three health dimensions.
We found further variability in the correlations between the country OH index at three levels and the synergy or trade-off proportions within and between the three health dimensions in 2020 (Figure 3). In those countries facing substantial OH challenges (L), the synergy proportion within human health is positively correlated with the country OH index (ρ = 0.33, p < 0.05). However, it is negatively correlated with the trade-off proportion (ρ = −0.34, p < 0.05) (Figure 3). In moderately performing countries (M), synergy proportions between the three health dimensions and within environmental health are each positively correlated with the country OH index (0.23 < ρ < 0.34, p < 0.05). In contrast, it is negatively correlated with their trade-off proportions (−0.34 < ρ < −0.28, p < 0.05) (Figure 3). Well-performing countries (H) have positive correlations between the country OH index and their synergy proportions within animal or environmental health dimensions and in the animal-environmental health relationship (0.59 < ρ < 0.79, p < 0.05), but lack any significant correlations for trade-off proportions (p > 0.05) (Figure 3).
Key targets of global OH relationships
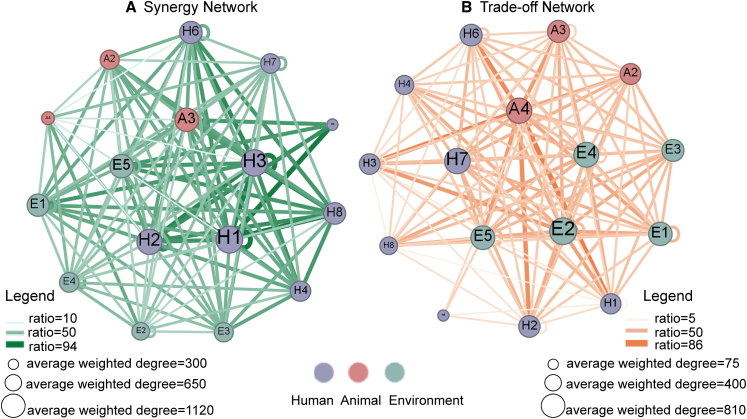
Our results indicate that key synergistic targets can help to reach other OH targets, in this way acting as pivotal leverage points for improving OH. Globally, from the OH synergy network, we identified H1 (maternal, newborn, and child health) as the most influential target, followed by H3 (non-communicable diseases and mental health), H2 (infectious diseases), A3 (animal nutritional status), and E5 (environmental biodiversity) (Figure 4A; Table S4). For instance, H1 had significant synergistic relationships with six OH targets across more than 627 indicator data pairs (p < 0.05; Figure S9). Additionally, improvements to A3 and E5 significantly help to meet four and two OH targets, respectively, involving more than 629 indicator data pairs (p < 0.05; Figure S9).
Figure 4.
Observed synergy and trade-off networks between the One Health target pairs on a global scale
(A) Greenish connecting lines denote the synergy network.
(B) Reddish connecting lines show the trade-off network. Darker and wider lines indicate a stronger correlation between the One Health target pairs. Larger connection nodes (circles) on the lines indicate that the corresponding target substantially impacts the network.
Likewise, progress toward meeting key trade-off targets can slow advances in other OH targets (and vice versa). This calls for careful consideration of their potential impacts to minimize negative effects. In the trade-off network, E2 (land resources) emerged as the most influential target, followed by H7 (food security), A4 (animal biodiversity), and E4 (hazardous chemicals) (Figure 4B; Table S5). Then, environmental health targets dominate the trade-off network, for which all average-weighted degree targets are ranked within the top seven in the network, where E2 is paramount (Table S5). This suggests that it is essential to consider potential limiting effects on other OH targets’ achievement when promoting environmental health targets to avoid or overcome trade-off effects. Specific OH targets can significantly affect synergy and trade-off networks, albeit with different associated targets or countries. For instance, one of the most influential targets in global trade-off and synergy networks is E5, ranked fifth in terms of its average-weighted degree (Tables S4 and S5).
Key OH targets of health relationships across countries
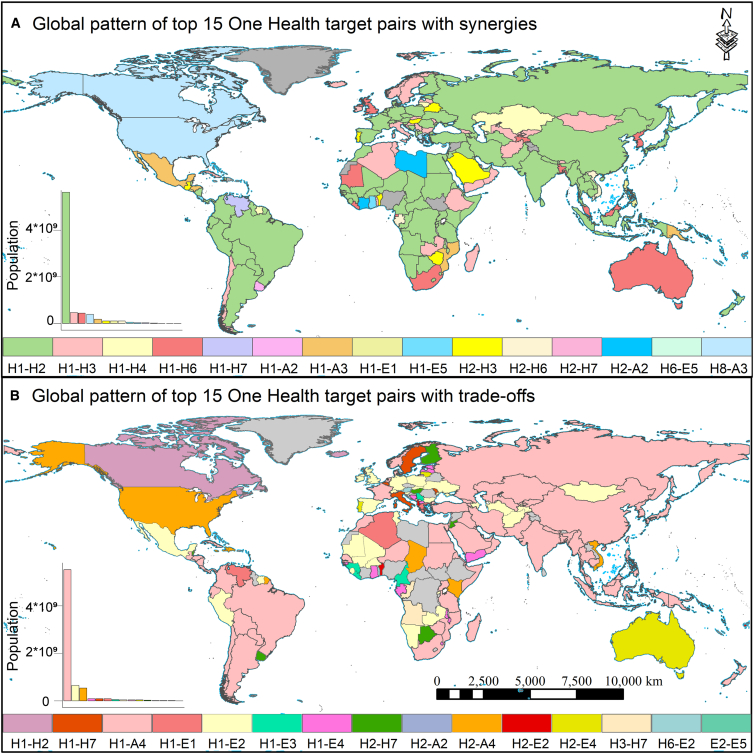
Nationally, we found similarities in the identified influential targets across many countries, but differences did arise in a few countries. Through our analysis, we could identify the key targets exercising the greatest impact across various countries and their affected human populations. Namely, H1 (maternal, newborn, and child health), H2 (infectious diseases), and H3 (non-communicable diseases and mental health) stood out as the most influential synergistic targets. For example, the synergistic targets of H1-H2 prevail in 95 countries across Asia, Africa, South America, and Europe, positively affecting about 5.62 billion people (Figure 5A); H1 and H3 form the top synergistic pairing in 30 countries across Europe, Africa, Asia, and Australia, influencing about 0.48 billion people (Figure 5A). Concerning trade-offs, A4 (animal biodiversity) emerged as the most influential trade-off target, followed by E2 (land resources). A4 leads the trade-off target in 84 countries, mainly with H1, impacting about 6.06 billion people across Asia, Africa, and America. E2 is prominent atop the trade-off target pairings in 27 countries, mainly with H1, affecting 0.66 billion people across Europe and Africa (Figure 5B).
Figure 5.
Global patterns of the top 15 One Health target pairs with synergies and trade-offs across countries
(A) Synergies.
(B) Trade-offs. The bar chart inset shows different One Health targets and their corresponding populations in 2020. The gray color indicates regions with no data or less than n = 3 data pairs.
Our study pinpoints H1, H2, and H3 as key synergy targets at both the global and national scales. It also highlights why it is imperative to address trade-offs related to E2 (land resources), H7 (food security), and A4 (animal biodiversity) to enhance OH progress (Table S5; Figure 5B). At the national scale, H1-H2 and H1-A4 emerge as the most influential pairs of OH target synergies and trade-offs, with associated human populations and countries exceeding those of other OH target pairs. The distribution of countries associated with these pairs was almost identical, mainly concentrated in Asia, Africa, and South America (Figure 5). Therefore, enhancing the synergy among these targets and addressing trade-offs is crucial for bolstering OH progress, given the corresponding implications for a huge portion of the world’s population and its countries.
Discussion
Better putting OH into practice requires fostering synergies among these health dimensions while identifying and minimizing their trade-offs.24 Our study systematically investigated spatiotemporal disparities within and between human, animal, and environmental health dimensions from 2000 to 2020, seeking to identify pertinent synergies and trade-offs. More importantly, we distinguished key OH synergistic and trade-off targets, providing timely information for policymaking to achieve OH uniform progress in various health dimensions and countries.
While our findings agree with other work showing a global improvement in OH,25,26,27,28 we identified uneven progress across various health dimensions and countries. These disparities can be explained by major advances in human health due to rapid progress in medical technology, widespread public health initiatives, and improved education.25,26,27,28,29,30 Nevertheless, environmental health features little, if any, improvement or, in some cases, regression. A case in point: just one-fifth of the strategic and specific goals tied to nature and environmental protection of the world in six global agreements are progressing smoothly.31 In fact, for nearly one-third of specific targets in these conventions, either minimal or no progress has been made, or countries have deviated from certain targets.31
From the analysis of three health configurations, we find that no country performs well overall, with a score above 80. Nonetheless, countries differing in income status may face distinct challenges. For instance, low- and middle-income countries struggle with attaining development in every health dimension, while high-income countries mostly face challenges in environmental health. The obstacles in the way of low- and middle-income countries could be ascribed to a mix of factors, such as heavy population pressure coupled with limited resources, along with rapid urbanization, in addition to the rapid expansion of livestock production and agriculture, all of which are leading to land degradation; biodiversity loss; air, water, and soil pollution; and a greater risk of disease spillover.31,32,33 For high-income countries, however, it is likely that the unsustainable mass production and consumption of non-essential goods and services, which are critical factors underpinning its resource depletion and environmental pollution, lead to trade-offs between environmental health and other health dimensions, namely human and animal health.33,34,35
Our analysis underscores a global trend whereby synergies outweigh trade-offs among the three health dimensions, mainly in high-income countries. This trend has probably been strengthened by introducing and developing the OH approach and SDGs, which have spurred nations to adopt holistic-oriented strategies that align human, animal, and environmental health, resulting in a relatively higher proportion of synergies.36,37,38 For example, the OH approach shows a range of quantitative incremental benefits regarding health services and infrastructure monitoring and response systems, antimicrobial resistance, food safety, nutrition security, environmental sanitation, and zoonosis control.9 Nonetheless, pivotal trade-offs persist within lower- and middle-income countries in Africa and Asia, where economic imperatives often come at the expense of animal and environmental health, given the limited resources and demographic pressures there.32,39 Environmental health is the gravest challenge across countries, irrespective of income, exacerbated by inadequate health policy frameworks, asymmetric regional competition, and escalating demands for public health and food safety.40 These stark disparities emphasize why targeted policies and actions are urgently needed to foster greater synergy relations and facilitate uniform OH progress. However, some high-income countries may face difficulties in achieving synergies.
Although high-income countries generally exhibit more synergies and low-income countries more trade-offs, this pattern does not hold for all relationships examined here. Our in-depth analysis of how the OH index is related to the three health dimensions yielded fresh insight conducive to advancing OH policy initiatives. For example, correlation shifts emerged in the synergy and trade-off proportions among the three health dimensions versus the OH index at its three levels. Tackling the human health dimension has led to better health outcomes in countries with an OH index level of L (score ≤60). For example, global health initiatives have undoubtedly improved health outcomes in low-income and middle-income countries, particularly in Southeast Asia and sub-Saharan Africa.41,42 Countries with an OH index level of H (score ≥80) should instead focus on leveraging synergistic effects between the animal and environmental health dimensions. For example, biodiversity conservation yields stronger synergistic benefits in high-income countries whose overall health performance is also higher.33
Hence, the suite of challenges faced and domains prioritized for intervention are apt to vary drastically across countries at different stages of socioeconomic development, potentially shaped by factors such as their degree of economic modernization, resource endowments, and the extent of policy implementation.24 Future research should aim to stratify countries based on political systems and other relevant traits.12 Embracing this more nuanced approach is needed to better understand the complex interplay between the three health dimensions and provide more valuable insights for customizing cross-sectoral policies.
Since prevailing synergies and trade-offs inevitably differ to some extent across countries, we must strive to craft tailored policies that mitigate likely trade-offs in different countries and contexts.43 So, pursuing synergistic outcomes among the key targets (i.e., H1, H2, and H3) is the most promising strategy for initiating a virtuous cycle of OH progress. Such key synergy targets are closely associated with synergistic co-benefits, which means that progress in one can help fulfill other targets. For example, previous research suggests that good health and well-being engage synergistically with other SDGs, which is conducive to reducing negative environmental impacts, meeting technological demands, and driving healthcare investments, especially in developing countries.33
Our research also underscores the need to dampen potent trade-off effects, mainly concerning land resources (E2) and animal biodiversity (A4). These targets are essential because progress in one could prevent or limit success in others.34 Many studies have stressed that spillover effects of zoonotic diseases, spurred by land-use changes and biodiversity loss, rightly stand out as interdisciplinary priorities.44,45,46 Not surprisingly, those areas under the greatest pressure from land use and biodiversity changes are prone to becoming hotspots for zoonotic disease outbreaks.18
For instance, Southeast Asia and sub-Saharan Africa are hotspots for zoonotic diseases such as the Ebola virus, coronaviruses (pandemics severe acute respiratory syndrome and COVID-19), and the influenza virus (pandemic H5N1).32,45 Rapid agricultural expansion, urbanization, and deforestation to meet growing food and population demands have led to much biodiversity loss and habitat fragmentation.32 From 1998 to 2018, forest coverage in Southeast Asia shrunk by 50%, with over 30% of its remaining forest areas being highly fragmented.47,48 These factors, linked to land-use changes, drive frequent disease outbreaks and pose substantial challenges to human, animal, and environmental health.44 Progress in human health often comes at the expense of animal and environmental health, thus representing pivotal trade-offs. Low-income countries, particularly those in Southeast Asia and sub-Saharan Africa, must often contend with urban growth that exceeds socio-economic development. This inevitably leads to inadequate funding for disease prevention, incoherent policies, limited medical resources, and weak monitoring systems, all heightening the disease risks those countries must bear.49
Nevertheless, our findings do show that promoting the synergy between H1 (maternal, newborn, and child health) and H2 (infectious diseases) while mitigating the trade-offs of A4 (animal biodiversity) can advance the OH index. For instance, Vietnam has significantly reduced its incidence of malaria and dengue fever through vaccination programs and surveillance systems of zoonotic diseases, coupled with improved medical infrastructure and public dissemination of health knowledge.50 From 2008 to 2017, Vietnam’s malaria cases fell by 60%, with the number of deaths reduced by 76%.51 Moreover, by 2023, China had established 82 internationally renowned protected wetlands, ranking the country fourth worldwide in total wetland area. Currently, the national protection rate of wetlands exceeds 52%, thus ensuring water security, markedly enhancing biodiversity, and protecting vital habitats.52 Adapting these measures can effectively promote synergistic outcomes among three health dimensions, thereby enhancing OH progress.
On a global scale, a critical trade-off target is food security (H7). Despite improving global food affordability, the overarching goal of the food system to mitigate environmental and climate change consequences while augmenting nutritional and health outcomes remains elusive.53 The world’s food system is responsible for 29% of anthropogenic greenhouse gas emissions (E1) and contributes to 60% of the loss in global terrestrial biodiversity (A4).54 Food production is associated with more than 50% of zoonotic infectious diseases that emerge in humans, exacerbated by the expansion and intensification of agriculture.55 Rising urban incomes, unbalanced diets, and insufficient physical activity are known contributors to the escalation of cardiovascular diseases (H3).27 Furthermore, including both malnutrition and obesity-related conditions, diet-related diseases now account for 20% of premature deaths worldwide.31 Thus, fruitful and innovative collaborations across multiple sectors, such as animal and human health cooperation and robust environmental monitoring (short- and long-term), are essential pro-active mechanisms for balancing OH targets to avoid conflicts and achieve common interests and goals.56
Limitations of the study
While our study did yield worthwhile findings, it is nonetheless important to recognize its limitations. This includes potential incomplete aspects of our OH indicator framework, lacking a quantitative analysis to explicitly elucidate the drivers behind spatiotemporal changes to the OH index and the dynamics between various health relationships. For instance, we could not incorporate emerging chemical emissions and the COVID-19 pandemic into the OH index framework due to insufficient data support. Thus, we may underestimate the connections between the three health dimensions. Rising emissions of emerging pollutants can disrupt ecosystems and endanger wildlife, posing threats to human well-being and planetary health.57 Although this study did include wastewater treatment (E4.5) in gauging progress toward OH, its assessment framework is still deficient and needs more work.
Future research efforts should focus on continually developing the proposed indicator framework and delving deeper into the factors influencing various health relationships, whether related to politics, economics, culture, sustainable waste management, and the impact of the COVID-19 pandemic, to foster a richer understanding of OH dynamics.12 To resolve extant and looming trade-offs, exploring effectual strategies in the future is imperative. Their practical implementation will likely hit certain economic and social development constraints, highlighting the importance of objectively evaluating cost-effectiveness in managing trade-offs with health dimensions. Overall, our study provides a scientific basis for future research on OH synergy and trade-off mechanisms, including policymaking, by identifying priority development goals and spatial disparities. Furthermore, it enriches current knowledge of integrated health and offers timely scientific evidence for preventing, monitoring, and responding to pandemics. Strengthening this research is now crucial to realizing global OH and sustainable development.
Resource availability
Lead contact
Further information and requests for resources should be directed to and will be fulfilled by the lead contact, Hui Lin (huilin@cuhk.edu.hk).
Materials availability
This study did not generate new unique reagents.
Data and code availability
-
•
Our research data for One Health indicators came from authoritative databases (listed in Table S1). The population data in 2020 were taken from the WorldPop dataset, at https://www.worldpop.org/. Data on income groups in 2020 came from the World Bank dataset, at https://datahelpdesk.worldbank.org/.
-
•
This paper does not report original code.
-
•
Any additional information required to reanalyze the data reported in this paper is available from the lead contact upon request.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (grant no. 42330108, 41930648, and 42201299), the Second Tibetan Plateau Scientific Expedition and Research Program [grant no. 2019QZKK0308], the National Science Fund for Distinguished Young Scholars (grant no. 42325107), the Young Elite Scientists Sponsorship Program by CAST (grant no. 2023QNRC001), the European Research Council Starting Grant 2022 for the BeyondSDG project (grant no. 101077492), and the Graduate Innovation Fund Project of Jiangxi Normal University (grant no. YJS2022009). We especially thank the editor and the anonymous referees for their careful review and insightful comments.
Author contributions
Y.T., J.Z., and M. Chen designed the study. Y.T. and Z.L. performed the experiments and computational analyses. Y.T. and J.Z. drafted the manuscript. M. Chen, J.Z., B.F., and H.L. supervised this study. All authors discussed the results and revised the manuscript.
Declaration of interests
The authors declare no competing interests.
STAR★Methods
Key resources table
| REAGENT or RESOURCE | SOURCE | IDENTIFIER |
|---|---|---|
| Deposited data | ||
| Indicators and data sources for the OH assessment scheme | This paper | Table S1 |
| Descriptive statistics for OH indicators and their attribute characteristics | This paper | Table S2 |
| Global OH progress and change in the number of countries with three configurations of scores for human, animal, and environmental health, from 2000 to 2020 | This paper | Figure 1 |
| The number of countries categorized into three score-level configurations for human, animal, and environmental health from 2000 to 2020 | This paper | Table S3 |
| Global score (2020) and score growth rate of human, animal, environmental health, and OH index from 2000 to 2020 | This paper | Figure S1 |
| Global spatial configurations of score levels for human, animal, environmental health, and OH index from 2000 to 2020 | This paper | Figure S2 |
| Global-scale relationship proportions and geographic patterns of synergies and trade-offs between and within human, animal, and environmental health dimensions across countries | This paper | Figure 2 |
| Differences in the proportion of synergies and trade-offs between and within human, animal, and environmental health at the national scale | This paper | Figure S3 |
| Correlation between the OH index and the proportions of synergies or trade-offs | This paper | Figures 3 and S4–S8 |
| Observed synergy and trade-off networks between the OH target pairs at the global scale | This paper | Figure 4 |
| The average degree and average weighted degree of OH targets in the synergy and trade-offs networks | This paper | Tables S4 and S5 |
| Detected the proportion of synergies and trade-offs between different OH targets and within the same OH target, from 2000 to 2020 | This paper | Figure S9 |
| Global patterns of the top 15 OH target pairs with synergies and trade-offs across countries | This paper | Figure 5 |
| Flowchart for OH assessment and evaluation of synergies and trade-offs among human, animal, and environmental health dimensions on global and national scales. | This paper | Figure S10 |
| Software and algorithms | ||
| MATLAB (version R2019b) | MATLAB R2019b: the 9.7th Release of MATLAB Technical Computing Software | MATLAB (version R2019b) |
Method details
Indicator selection and data sources
This study devised a comprehensive OH assessment scheme by integrating various established indicators from the GOHI and SDGs. The GOHI served as our primary reference, encompassing key indicators from the Environmental Performance Index (EPI), WHO, and WOAH.12 We also took into account additional health-related indicators within the SDGs.58 Our OH indicator framework was organised into three levels corresponding to the three health dimensions (human, animal, environmental), 17 OH targets, and 49 OH indicators (Table S1). Due to the limitations in data availability and accessibility, we collected data from 2000 to 2020 to build the OH indicator database. Consequently, the impact of the COVID-19 pandemic was not accounted for in the analysis. We only extracted data from official databases to ensure their statistical reliability, general applicability, and currency (Tables S1 and S2). These data were selected according to seven recognized principles12 (relevance, authoritative sources, open access, completeness, timeliness, comparability, and national-scale data). Both cross-checks and consistency tests were carried out randomly while collecting the data to uphold its integrity and quality. The latter were linearly interpolated for indicators with missing values using MATLAB R2019b software.
Data processing
To calculate the OH, we used a four-step process: (1) selecting indicators, (2) setting the target and baseline values, (3) normalisation, and (4) aggregation.59 Among the 193 UN Member States, we considered only those countries’ data missing rates below 50% in human, animal, or environmental dimensions.12 Globally, 148 countries met this criterion for inclusion. Like the method used for the Sustainable Development Report 2022 (SDR),60 global and national scale scores were calculated (arithmetic means) for every OH target, the three health dimensions, and the OH index from 2000 to 2020. First, the OH indicator scores were aggregated to yield OH target scores, and then the latter were aggregated to obtain human, animal, and environmental health scores. The OH index was then calculated as the mean of the scores for the three health dimensions. To minimize subjectivity, all OH indicators were equally weighted and considered equally importance.60
We compared the changes in scores for the three health dimensions and the OH index between 2000 and 2020 at national and global scales. To convey the spatial patterning of the OH index and human, animal, and environmental health dimensions, we classified those with a score ≥80 as performing well (H); those with a score ≤60 as facing substantial challenges (L); and those with scores in between 60 and 80 as performing moderately (M). In addition, one-way analysis of variance (ANOVA) was used to test for a difference during the 20-year study period among years (five levels: 2000, 2005, 2010, 2015, and 2020) in the OH index and three health scores of the countries (Figure 1A). According to these score levels, we categorised the countries into 27 possible configuration types spanning the three health dimensions (Table S3). This resulted in 15 configurations having a nonzero number of countries (Figure 1B).
This study inferred relationships by considering statistically significant positive and negative correlations as tentative evidence for synergies and trade-offs. For the entire dataset, bivariate correlations were performed between 173 071 unique OH indicator pairs, encompassing 54 indicators across approximately 148 countries from 2000 to 2020. We used Spearman’s rank-based coefficient61 (ρ) to assess the possible monotonic relationships between all combinations of indicator pairs on a per-country basis from 2000 to 2020. This method offers the advantage of assessing correlations and conducting significance tests with limited data while still enabling adequate interpretability.62 The selected indicator pairs may pertain to either domains of the same health dimension or those of two distinct health dimensions, letting us explore the synergies and trade-offs within and between differing health dimensions in-depth. We restricted this correlation analysis to OH indicator pairs with more than three data points to help lessen the risk of detecting false synergies or trade-offs arising from limited data in light of the experience of related studies and data availability constraints.34
A correlation with a p-value <0.05 was considered significant.34 To avoid over-interpretation of correlation, we define the relationship with ρ ∈[–0.5, 0.5] as “non-classified”, ρ ∈[–1, −0.5] as a “trade-off” and ρ ∈[0.5, 1] as a “synergy”,63 as illustrated in Figure S10. Furthermore, we leveraged the OH indicators as a proxy to convey the complex relationships within and between the three health dimensions, given that eliminating confounding factors among indicators is not feasible. In sum, using a data-driven methodology, this study presented a preliminary systematic assessment of relationships among aspects of human, animal, and environmental health.
Synergies and trade-offs
We systematically analyzed global and national OH relationships to understand their synergy or trade-off among the three health dimensions and identify priority targets. Globally, relationships within OH targets were quantified by assessing their respective proportions (%) of synergies, trade-offs, and non-classified pairs. Likewise, the OH relationships were tallied as proportions (%) per country on a national scale to reduce bias from variation in indicator data availability.
Our initial step involved mapping the global distribution of variations in the proportions (%) of synergies and trade-offs between and within the three health dimensions by country. We then compared the relationships within and between three health dimensions among countries stratified by their World Bank income grouping in 2020. By integrating the relationship configurations within and between the three health dimensions, we globally mapped the patterns for different countries. Finally, we examined the number of countries by their income grouping in 2020 under different relationship configurations of the three health dimensions. In our analysis, we defined situations where the proportion of synergies exceeded that of trade-offs as “S” and, conversely, where that of trade-offs exceeded synergies as “T”.
To further analyze how these relationships evolved in tandem with progress toward OH, we first tested for Spearman correlations and performed linear regression models to fit lines between the OH index of countries and the proportion of synergies or trade-offs between and within the three health dimensions. Next, we compared the difference in correlation strength (coefficient values) across different health dimensions in countries subsumed under the three OH index levels (L, M, H).
Using a network analysis, we then identified the key OH targets influencing the synergies and trade-offs between different health domains or dimensions by employing an average weighted degree64 by considering only the number of data pairs exceeding 100.34 The ‘average degree’ simply refers to the average number of connections per target in the network, ignoring the weights of its connections.64 Hence, ‘average-weighted degree’ refers to the average strength of connections per target in a network, now taking into account the weights of its connections.64 The average-weighted degree was calculated by summing up all the connection weights for a given target and then dividing that value by the total number of targets. In deriving the average-weighted degree, we utilize the proportions of synergy and trade-off relationships specific to each OH target pair as the weights. For this calculation, Gephi software65 was used, to glean insight into the influence of each OH target in the synergy or trade-off scenarios (Tables S4 and S5). The average degree and the average-weighted degree were calculated as follows:
| (Equation 1) |
| (Equation 2) |
where N represents the number of OH targets, ki is the degree of the i-th target. The weight of an edge is denoted as ωij, where i and j are two connected targets. Ν(i) represents the set of all targets directly connected to target i.
We individually ranked the OH target pairs for each country based on the proportion of synergies, trade-offs, and non-classifieds. Given the substantial disparities in OH target rankings across countries, we also determined the relative frequency rank, which indicates how often a specific OH target got ranked globally within the top 15 synergy or trade-off pairs. Finally, we generated a map depicting each country’s highest-ranked OH target pairs among those above-identified top 15 synergy or trade-off pairs. The flowchart for this study’s OH assessment and its evaluation of synergies and trade-offs among the three health dimensions at both the global and national scale is shown in Figure S10.
Quantification and statistical analysis
All quantification and statistical analyses were performed as described in the method details section of the STAR Methods.
Published: November 9, 2024
Footnotes
Supplemental information can be found online at https://doi.org/10.1016/j.isci.2024.111357.
Contributor Information
Junze Zhang, Email: zhangjunze427@126.com.
Min Chen, Email: chenmin0902@njnu.edu.cn.
Hui Lin, Email: huilin@cuhk.edu.hk.
Supplemental information
References
- 1.Kock R., Queenan K., Garnier J., Nielsen R.L., Buttigieg S., de Meneghi D., Holmberg M., Zinsstag J., Rüegg S., Häsler B. Integrated approaches to health. Wageningen Academic; 2018. Health solutions: theoretical foundations of the shift from sectoral to integrated systems; pp. 22–37. [Google Scholar]
- 2.World Health Organization Pandemic prevention, preparedness and response accord. 2022. https://www.who.int/news-room/questions-and-answers/item/pandemic-prevention--preparedness-and-response-accord
- 3.Shimkin M.B. The World Health Organization. Science. 1946;104:281–283. doi: 10.1126/science.104.2700.281. [DOI] [PubMed] [Google Scholar]
- 4.World Organisation for Animal Health (WOAH). (2024). Terrestrial Animal Health Code. https://www.woah.org/en/what-we-do/standards/codes-and-manuals/terrestrial-code-online-access/.
- 5.World Health Organization (WHO) Environmental health. https://www.who.int/health-topics/environmental-health/
- 6.Baker R.E., Mahmud A.S., Miller I.F., Rajeev M., Rasambainarivo F., Rice B.L., Takahashi S., Tatem A.J., Wagner C.E., Wang L.F., et al. Infectious disease in an era of global change. Nat. Rev. Microbiol. 2022;20:193–205. doi: 10.1038/s41579-021-00639-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lawler O.K., Allan H.L., Baxter P.W.J., Castagnino R., Tor M.C., Dann L.E., Hungerford J., Karmacharya D., Lloyd T.J., López-Jara M.J., et al. The COVID-19 pandemic is intricately linked to biodiversity loss and ecosystem health. Lancet Planet. Health. 2021;5:e840–e850. doi: 10.1016/S2542-5196(21)00258-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization Tripartite and UNEP support OHHLEP’s definition of "One Health. 2021. https://www.who.int/news/item/01-12-2021-tripartite-and-unep-support-ohhlep-s-definition-of-one-health
- 9.Zinsstag J., Kaiser-Grolimund A., Heitz-Tokpa K., Sreedharan R., Lubroth J., Caya F., Stone M., Brown H., Bonfoh B., Dobell E., et al. Advancing One human–animal–environment Health for global health security: what does the evidence say? Lancet. 2023;401:591–604. doi: 10.1016/S0140-6736(22)01595-1. [DOI] [PubMed] [Google Scholar]
- 10.Kelly T.R., Karesh W.B., Kreuder C., Gilardi K.V.K., Anthony S.J., Goldstein T., Olson S.H., Machalaba C., Consortium P., Mazet J.A.K. One Health proof of concept : Bringing a transdisciplinary approach to surveillance for zoonotic viruses at the human-wild animal interface. Prev. Vet. Med. 2017;137:112–118. doi: 10.1016/j.prevetmed.2016.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mackenzie J.S., Jeggo M., Daszak P., Richt J.A. One Health: The Human-Animal-Environment Interfaces in Emerging Infectious Diseases. Springer; 2013. [Google Scholar]
- 12.Zhang X.X., Liu J.S., Han L.F., Xia S., Li S.Z., Li O.Y., Kassegne K., Li M., Yin K., Hu Q.Q., et al. Towards a global One Health index: a potential assessment tool for One Health performance. Infect. Dis. Poverty. 2022;11:12–26. doi: 10.1186/s40249-022-00979-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dar, O., Machalaba, C., Adisasmito, W.B., Almuhairi, S., Behravesh, C.B., Bilivogui, P., Bukachi, S.A., Casas, N., Becerra, N.C., Charron, D.F., et al. (2022). One Health Theory of Change One Health Theory of Change Contents, 25.
- 14.Pellet P.E., Mitra S., Holland T.C. Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID- Elsevier hereby grants permission to make all its COVID-19-related research that is available on the COVID-19. Handb. Clin. Neurol. 2020;123:45–66. [Google Scholar]
- 15.Mwatondo A., Rahman-Shepherd A., Hollmann L., Chiossi S., Maina J., Kurup K.K., Hassan O.A., Coates B., Khan M., Spencer J., et al. A global analysis of One Health Networks and the proliferation of One Health collaborations. Lancet. 2023;401:605–616. doi: 10.1016/S0140-6736(22)01596-3. [DOI] [PubMed] [Google Scholar]
- 16.Ho C.W.L. Operationalizing “One Health” as “One Digital Health” Through a Global Framework That Emphasizes Fair and Equitable Sharing of Benefits From the Use of Artificial Intelligence and Related Digital Technologies. Front. Public Health. 2022;10 doi: 10.3389/fpubh.2022.768977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ehling-Schulz M., Filter M., Zinsstag J., Koutsoumanis K., Ellouze M., Teichmann J., Hilbeck A., Tonolla M., Etter D., Stärk K., et al. Risk negotiation: a framework for One Health risk analysis. Bull. World Health Organ. 2024;102:453–456. doi: 10.2471/BLT.23.290672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Muylaert R.L., Wilkinson D.A., Kingston T., D’odorico P., Rulli M.C., Galli N., John R.S., Alviola P., Hayman D.T.S. Using drivers and transmission pathways to identify SARS-like coronavirus spillover risk hotspots. Nat. Commun. 2023;14 doi: 10.1038/s41467-023-42627-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grange Z.L., Goldstein T., Johnson C.K., Anthony S., Gilardi K., Daszak P., Olival K.J., O’Rourke T., Murray S., Olson S.H., et al. Ranking the risk of animal-to-human spillover for newly discovered viruses. Proc. Natl. Acad. Sci. USA. 2021;118 doi: 10.1073/pnas.2002324118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rulli M.C., D’Odorico P., Galli N., Hayman D.T.S. Land-use change and the livestock revolution increase the risk of zoonotic coronavirus transmission from rhinolophid bats. Nat. Food. 2021;2:409–416. doi: 10.1038/s43016-021-00285-x. [DOI] [PubMed] [Google Scholar]
- 21.Zhang J., Skene K.R., Wang S., Ji Q., Zheng H., Zhou C., Tian K., Pradhan P., Meadows M.E., Fu B. Beyond borders: Assessing global sustainability through interconnected systems. Sustain. Dev. 2024:1–12. doi: 10.1002/sd.3218. [DOI] [Google Scholar]
- 22.Zinsstag J., Schelling E., Waltner-Toews D., Tanner M. From “one medicine” to “one health” and systemic approaches to health and well-being. Prev. Vet. Med. 2011;101:148–156. doi: 10.1016/j.prevetmed.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Coker R., Rushton J., Mounier-Jack S., Karimuribo E., Lutumba P., Kambarage D., Pfeiffer D.U., Stärk K., Rweyemamu M. Towards a conceptual framework to support one-health research for policy on emerging zoonoses. Lancet Infect. Dis. 2011;11:326–331. doi: 10.1016/S1473-3099(10)70312-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Traore T., Shanks S., Haider N., Ahmed K., Jain V., Rüegg S.R., Razavi A., Kock R., Erondu N., Rahman-Shepherd A., et al. How prepared is the world? Identifying weaknesses in existing assessment frameworks for global health security through a One Health approach. Lancet. 2023;401:673–687. doi: 10.1016/S0140-6736(22)01589-6. [DOI] [PubMed] [Google Scholar]
- 25.D’Amour C.B., Reitsma F., Baiocchi G., Barthel S., Güneralp B., Erb K.H., Haberl H., Creutzig F., Seto K.C. Future urban land expansion and implications for global croplands. Proc. Natl. Acad. Sci. USA. 2017;114:8939–8944. doi: 10.1073/pnas.1606036114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li G., Fang C., Li Y., Wang Z., Sun S., He S., Qi W., Bao C., Ma H., Fan Y., et al. Global impacts of future urban expansion on terrestrial vertebrate diversity. Nat. Commun. 2022;13:1628. doi: 10.1038/s41467-022-29324-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guo Y., He P., Searchinger T.D., Chen Y., Springmann M., Zhou M., Zhang X., Zhang L., Mauzerall D.L. Environmental and human health trade-offs in potential Chinese dietary shifts. One Earth. 2022;5:268–282. doi: 10.1016/j.oneear.2022.02.002. [DOI] [Google Scholar]
- 28.Zhang J., Chai L. Trade-off between human health and environmental health in global diets. Resour. Conserv. Recycl. 2022;182 doi: 10.1016/j.resconrec.2022.106336. [DOI] [Google Scholar]
- 29.Rohr J.R., Sack A., Bakhoum S., Barrett C.B., Lopez-Carr D., Chamberlin A.J., Civitello D.J., Diatta C., Doruska M.J., De Leo G.A., et al. A planetary health innovation for disease, food and water challenges in Africa. Nature. 2023;619:782–787. doi: 10.1038/s41586-023-06313-z. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization Maximizing Positive Synergies Collaborative Group. Samb B., Evans T., Dybul M., Atun R., Moatti J.P., Nishtar S., Wright A., Celletti F., Hsu J., et al. An assessment of interactions between global health initiatives and country health systems. Lancet. 2009;373:2137–2169. doi: 10.1016/S0140-6736(09)60919-3. [DOI] [PubMed] [Google Scholar]
- 31.Díaz S.M., Settele J., Brondízio E., Ngo H., Guèze M., Agard J., Arneth A., Balvanera P., Brauman K., Butchart S., et al. Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services; 2019. The global assessment report on biodiversity and ecosystem services: Summary for policy makers; p. 56. [Google Scholar]
- 32.Goldstein J.E., Budiman I., Canny A., Dwipartidrisa D. Pandemics and the human-wildlife interface in Asia: Land use change as a driver of zoonotic viral outbreaks. Environ. Res. Lett. 2022;17 doi: 10.1088/1748-9326/ac74d4. [DOI] [Google Scholar]
- 33.Kroll C., Warchold A., Pradhan P. Sustainable Development Goals (SDGs): Are we successful in turning trade-offs into synergies? Palgrave Commun. 2019;5:1–11. doi: 10.1057/s41599-019-0335-5. [DOI] [Google Scholar]
- 34.Pradhan P., Costa L., Rybski D., Lucht W., Kropp J.P. A Systematic Study of Sustainable Development Goal (SDG) Interactions. Earth’s Futur. 2017;5:1169–1179. doi: 10.1002/2017EF000632. [DOI] [Google Scholar]
- 35.Pradhan P., Weitz N., Daioglou V., Abrahão G.M., Allen C., Ambrósio G., Arp F., Asif F., Bennich T., Benton T.G., et al. Three foci at the science-policy interface for systemic Sustainable Development Goal acceleration. Nat. Commun. 2024;15:8600. doi: 10.1038/s41467-024-52926-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.One Health High Level Expert Panel One Health Theory of Change. 2022. https://www.who.int/publications/m/item/one-health-theory-of-change
- 37.Dye C. One Health as a catalyst for sustainable development. Nat. Microbiol. 2022;7:467–468. doi: 10.1038/s41564-022-01076-1. [DOI] [PubMed] [Google Scholar]
- 38.Queenan K., Garnier J., Nielsen L.R., Buttigieg S., Meneghi D.d., Holmberg M., Zinsstag J., Rüegg S., Häsler B., Kock R. Roadmap to a one health agenda 2030. CAB Rev. Perspect. Agric. Vet. Sci. Nutr. Nat. Resour. 2017;12:1–17. doi: 10.1079/PAVSNNR201712014. [DOI] [Google Scholar]
- 39.Rulli M.C., Santini M., Hayman D.T.S., D’Odorico P. The nexus between forest fragmentation in Africa and Ebola virus disease outbreaks. Sci. Rep. 2017;7 doi: 10.1038/srep41613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Elnaiem A., Mohamed-Ahmed O., Zumla A., Mecaskey J., Charron N., Abakar M.F., Raji T., Bahalim A., Manikam L., Risk O., et al. Global and regional governance of One Health and implications for global health security. Lancet. 2023;401:688–704. doi: 10.1016/S0140-6736(22)01597-5. [DOI] [PubMed] [Google Scholar]
- 41.Ngonghala C.N., De Leo G.A., Pascual M.M., Keenan D.C., Dobson A.P., Bonds M.H. General ecological models for human subsistence, health and poverty. Nat. Ecol. Evol. 2017;1:1153–1159. doi: 10.1038/s41559-017-0221-8. [DOI] [PubMed] [Google Scholar]
- 42.Mwisongo A., Nabyonga-Orem J. Global health initiatives in Africa - Governance, priorities, harmonisation and alignment. BMC Health Serv. Res. 2016;16 doi: 10.1186/s12913-016-1448-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.De Neve J.-E., Sachs J.D. The SDGs and human well-being: A global analysis of synergies, trade-offs, and regional differences. Sci. Rep. 2020;10 doi: 10.1038/s41598-020-71916-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Plowright R.K., Reaser J.K., Locke H., Woodley S.J., Patz J.A., Becker D.J., Oppler G., Hudson P.J., Tabor G.M. Land use-induced spillover: a call to action to safeguard environmental, animal, and human health. Lancet Planet. Health. 2021;5:e237–e245. doi: 10.1016/S2542-5196(21)00031-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Allen T., Murray K.A., Zambrana-Torrelio C., Morse S.S., Rondinini C., Di Marco M., Breit N., Olival K.J., Daszak P. Global hotspots and correlates of emerging zoonotic diseases. Nat. Commun. 2017;8:1–10. doi: 10.1038/s41467-017-00923-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mahon M.B., Sack A., Aleuy O.A., Barbera C., Brown E., Buelow H., Civitello D.J., Cohen J.M., de Wit L.A., Forstchen M., et al. Global change drivers and the risk of infectious disease. bioRxiv. 2024 doi: 10.1038/s41586-024-07380-6. Preprint at. [DOI] [PubMed] [Google Scholar]
- 47.Namkhan M., Gale G.A., Savini T., Tantipisanuh N. Loss and vulnerability of lowland forests in mainland Southeast Asia. Conserv. Biol. 2021;35:206–215. doi: 10.1111/cobi.13538. [DOI] [PubMed] [Google Scholar]
- 48.Kenney-Lazar M., Ishikawa N. Mega-plantations in southeast asia landscapes of displacement. Environ. Soc. (N.Y.). 2019;10:63–82. doi: 10.3167/ares.2019.100105. [DOI] [Google Scholar]
- 49.Sun Z.S., Wan E.Y., Agbana Y.L., Zhao H.Q., Yin J.X., Jiang T.G., Li Q., Fei S.W., Wu L.B., Li X.C., et al. Global One Health index for zoonoses: A performance assessment in 160 countries and territories. iScience. 2024;27 doi: 10.1016/j.isci.2024.109297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Huynh L.N., Tran L.B., Nguyen H.S., Ho V.H., Parola P., Nguyen X.Q. Mosquitoes and Mosquito-Borne Diseases in Vietnam. Insects. 2022;13 doi: 10.3390/insects13121076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.World Health Organization . 2021. Malaria in Vietnam.https://www.who.int/vietnam/health-topics/malaria [Google Scholar]
- 52.ZHU H., WU H., XING X., XIE T., SONG C., WANG G., JIANG M. Achievement of wetland protection and restoration and development strategies in China. Bull. Chinese Acad. Sci. (Chinese Version) 2023;38:365–375. [Google Scholar]
- 53.Ambikapathi R., Schneider K.R., Davis B., Herrero M., Winters P., Fanzo J.C. Global food systems transitions have enabled affordable diets but had less favourable outcomes for nutrition, environmental health, inclusion and equity. Nat. Food. 2022;3:764–779. doi: 10.1038/s43016-022-00588-7. [DOI] [PubMed] [Google Scholar]
- 54.Delabre I., Rodriguez L.O., Smallwood J.M., Scharlemann J.P.W., Alcamo J., Antonarakis A.S., Rowhani P., Hazell R.J., Aksnes D.L., Balvanera P., et al. Actions on sustainable food production and consumption for the post-2020 global biodiversity framework. Sci. Adv. 2021;7 doi: 10.1126/sciadv.abc8259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rohr J.R., Barrett C.B., Civitello D.J., Craft M.E., Delius B., DeLeo G.A., Hudson P.J., Jouanard N., Nguyen K.H., Ostfeld R.S., et al. Emerging human infectious diseases and the links to global food production. Nat. Sustain. 2019;2:445–456. doi: 10.1038/s41893-019-0293-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Leboeuf A. Making sense of One Health. Cooperating at the human–animal–ecosystem health interface (IFRI Health and Environment Reports No. 7), (Institut Français des Relations Internationales) 2011. http://www.academia.edu/633338/Making_sense_of_One_Health
- 57.Wang F., Xiang L., Sze-Yin Leung K., Elsner M., Zhang Y., Guo Y., Pan B., Sun H., An T., Ying G., et al. Emerging contaminants: A One Health perspective. Innovation. 2024;5 doi: 10.1016/j.xinn.2024.100612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Johnston R.B. Arsenic and the 2030 Agenda for sustainable development. Arsen Res Glob Sustain. 6th Int Congr Arsen Env. AS. 2016:12–14. [Google Scholar]
- 59.Zhang, J., Wang, S., and Meadows, M.E. (2022). Finding pathways to synergistic development of Sustainable Development Goals in China. 9, 1–10. 10.1057/s41599-022-01036-4. [DOI]
- 60.Sachs J., Kroll C., Lafortune G., Fuller G., Woelm F. Sustainable Development Report 2022. Cambridge University Press; 2022. [Google Scholar]
- 61.Spearman C. The Proof and Measurement of Association Between Two Things. Stud. Individ. Differ. search Intell. 1961;15:45–58. doi: 10.1037/11491-005. [DOI] [Google Scholar]
- 62.Eraslan G., Avsec Ž., Gagneur J., Theis F.J. Deep learning: new computational modelling techniques for genomics. Nat. Rev. Genet. 2019;20:389–403. doi: 10.1038/s41576-019-0122-6. [DOI] [PubMed] [Google Scholar]
- 63.Warchold A., Pradhan P., Kropp J.P. Variations in sustainable development goal interactions: Population, regional, and income disaggregation. Sustain. Dev. 2021;29:285–299. doi: 10.1002/sd.2145. [DOI] [Google Scholar]
- 64.Barrat A., Barthelemy M., Pastor-Satorras R., Vespignani A. The architecture of complex weighted networks. Proc. Natl. Acad. Sci. USA. 2004;101:3747–3752. doi: 10.1073/pnas.0400087101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Grandjean M. 2015. Gephi: Introduction to network analysis and visualization.http://www.martingrandjean.ch/gephi-introduction/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
-
•
Our research data for One Health indicators came from authoritative databases (listed in Table S1). The population data in 2020 were taken from the WorldPop dataset, at https://www.worldpop.org/. Data on income groups in 2020 came from the World Bank dataset, at https://datahelpdesk.worldbank.org/.
-
•
This paper does not report original code.
-
•
Any additional information required to reanalyze the data reported in this paper is available from the lead contact upon request.