ABSTRACT
Background
The COVID‐19 pandemic precipitated a rapid roll‐out of virtual health care services to people with intellectual disabilities. Limited evidence is available for clinicians to guide virtual care delivery.
Method
Twenty‐three studies were identified through systematic searching of 16 databases. Extracted data were mapped to the NSW Virtual Health Strategy.
Results
Evidence exists to support the use of virtual care for screening, diagnosis, assessment, and review of people with intellectual disabilities, with benefits for clients, carers, and clinicians. Evidence mapped well to the priority areas of the NSW Virtual Health Strategy, highlighting the need for clinician training and specific supports and adaptations to ensure accessibility for people with intellectual disabilities.
Conclusions
The use of virtual care to assess the health needs of people with intellectual disabilities across the lifespan is nascent. An opportunity exists for co‐design with people with intellectual disabilities to reduce barriers to accessing and engaging in virtual care.
Keywords: health assessment, health care access, intellectual developmental disorder, telehealth, virtual care
1. Introduction
The Australian Disability Royal Commission into Violence, Abuse, Neglect, and Exploitation of People with Disability (Royal Commission 2023a) highlighted the ongoing inequity in health care access experienced by people with disabilities and a lack of consumer consultation in the design of health services. The rapid uptake of virtual care during the COVID‐19 pandemic prompted questions regarding equity of access to virtual care and about the quality and safety of virtual care for people with intellectual disabilities (Selick et al. 2021). As using virtual care to assess the health needs of people with intellectual disabilities is relatively new, a unique opportunity exists to co‐design this mode of care with people with intellectual disabilities and their carers, and to improve access to virtual care by providing necessary supports and adjustments to enable engagement (Royal Commission 2023a). Research, evaluation, and the development of policy and resources are essential to ensure virtual care services meet the needs of people with intellectual disabilities and provide clinicians with evidence‐informed tools and guidelines to support their use of virtual care with this population (Intellectual Disability Health Network 2017).
This scoping review was undertaken by Specialised Intellectual Disability clinicians, 1 who experienced a rapid shift from in‐person to virtual service delivery during the pandemic, with little clinical guidance. A small number of systematic scoping reviews (Selick et al. 2021; Oudshoorn et al. 2021; Chadwick et al. 2022) published during and following the COVID‐19 pandemic, collectively endorse the feasibility and acceptability of using virtual care to complement in‐person services for people with intellectual and developmental disabilities. All three reviews highlight the need for the inclusion of supports and adjustments for people with intellectual disabilities to support full engagement in virtual care. Experiences of parents, carers, and staff of a specialist paediatric service in Australia support the acceptability of hybrid service delivery models, including online assessment, and highlight benefits to families including reduced health care costs, increased flexibility, and the ability to accommodate family needs (Esther et al. 2022). Furthermore, the firsthand experiences of Specialist Intellectual Disability Community Teams in the United Kingdom have highlighted the successful delivery of remote consultations via video and telephone (Nicholson et al. 2023), whilst also supporting the preferences of some clients for a hybrid online and in‐person service delivery model.
We were interested in exploring what is known about using virtual care to assess the health needs of people of all ages with intellectual disabilities. The findings from this scoping review were mapped to the NSW Health Virtual Care Strategy (NSW Health 2022) to understand if it meets the needs of people with intellectual disabilities and intellectual disabilities health services, with a particular focus on identifying barriers to digital inclusion for people with intellectual disabilities.
This review was undertaken prior to the release of the Australian Disability Royal Commission Report (Royal Commission 2023a). Its recommendations reinforce key considerations for virtual care strategy development.
2. Methods
2.1. Study Design
A systematic scoping review was undertaken, informed by Arksey and O'Malley's (2005) five‐stage methodological framework.
2.1.1. Stage 1: Identifying the Research Question
The research questions were identified with reference to current clinical practice, existing literature, and identified gaps:
What is the evidence for using virtual care services to assess the health needs of people with intellectual disabilities?
What is the experience of using virtual care services from the perspective of clients with intellectual disabilities and their carers?
2.1.2. Stage 2: Identifying Relevant Studies
Studies relevant to the research question were identified through systematic searching of university library databases. Key search terms were identified, and synonyms were used to create a search strategy with assistance from a university librarian. The synonyms were combined with the Boolean operators ‘OR’ for parallel concepts, and then ‘AND’ to link concepts. Truncation characters were used. Search terms are outlined in Table 1.
TABLE 1.
Search terms.
| Concept term | Intellectual disability | Virtual care |
|---|---|---|
|
Concept terms in each list were combined with OR The concepts were combined with AND |
‘Intellectual dis*’ ‘Intellectual dev*’ ‘Disorder of intellectual development’ ‘Developmental delay’ ‘Developmental dis*’ ‘Learning dis*’ ‘Mental retardation’ |
‘Virtual care’ ‘Virtual health care’ Telehealth Telecare Teleconsultation Telemedicine Telepsychiatry e‐health e‐health ‘On‐line health’ |
Note: *denotes wildcard symbol to broaden search by finding all works with the same root e.g., dis∗ will search disability, disabilities, disabled.
The following databases were searched individually in June 2022: CINAHL, Scopus, MEDLINE via OVID, Academic Search Complete, Health Source: Nursing/Academic Edition, Psychology and Behavioural Sciences Collection, Health Business Elite, SocINDEX with Full Text, Health Source—Consumer Edition, Consumer Health database, Health and Medical Collection, Healthcare Administration Database, ProQuest Nursing & Allied Health database, Psychology Database, ProQuest Dissertations and Theses Global: Health & Medicine, Public Health database via the ProQuest Health and Medicine platform. The search was limited to English‐language publications. No time limits were set as virtual care services for people with intellectual disabilities are likely to be recent initiatives. The search was re‐run in December 2022 prior to charting and summarising the data.
2.1.3. Stage 3: Study Selection
All authors participated in the third stage. Inclusion and exclusion criteria were determined by the authors to identify studies relevant to the research questions (see Table 2). Studies were selected via f: title and abstract screening followed by full‐text review. Each abstract and title was reviewed independently by two authors to identify studies for exclusion.
TABLE 2.
Inclusion and exclusion criteria.
| Inclusion | Exclusion |
|---|---|
|
|
Abbreviations: ID = intellectual disability; RCT = randomised control trial.
Multiple studies were found that focused on the use of virtual care for the remote monitoring of individuals (telemonitoring), thus the exclusion criteria were adjusted to exclude these studies. Forty‐five studies were included for full‐text review and were thoroughly reviewed independently by two authors using the inclusion/exclusion criteria. Any conflicts were resolved by the decision of a third author.
2.1.4. Stage 4: Charting the Data/Data Extraction
All authors were involved in charting the data. Studies were divided amongst the team for data extraction which was completed using Covidence and Microsoft Excel. The following information was collected: author, country, study design, number of participants, referral source, participant age, primary diagnosis, study aims, context of virtual care delivery, location of clinicians and participants, format and duration of delivery, pre‐consultation activities, discipline of clinicians involved in virtual care delivery. Extracted data were mapped to the key areas and implementation goals of the NSW Health Virtual Care Strategy (NSW Health 2022). No quality assessment of the studies was done, as this was not the intention of the scoping review.
2.1.5. Stage 5: Collating, Summarising, and Reporting Results
The authors worked in pairs to synthesise the findings and map them to the three key areas of the NSW Virtual Care Strategy (NSW Health 2022). Areas of alignment were noted, as were findings that did not closely align with the three key areas of the strategy. Gaps not addressed by the included studies were also identified.
3. Results
The systematic search identified 173 studies for screening following the removal of 11 duplicates. Forty‐five full texts were reviewed against the inclusion and exclusion criteria. Twenty‐two were excluded. Data were extracted from the final 23 studies (see Figure 1).
FIGURE 1.
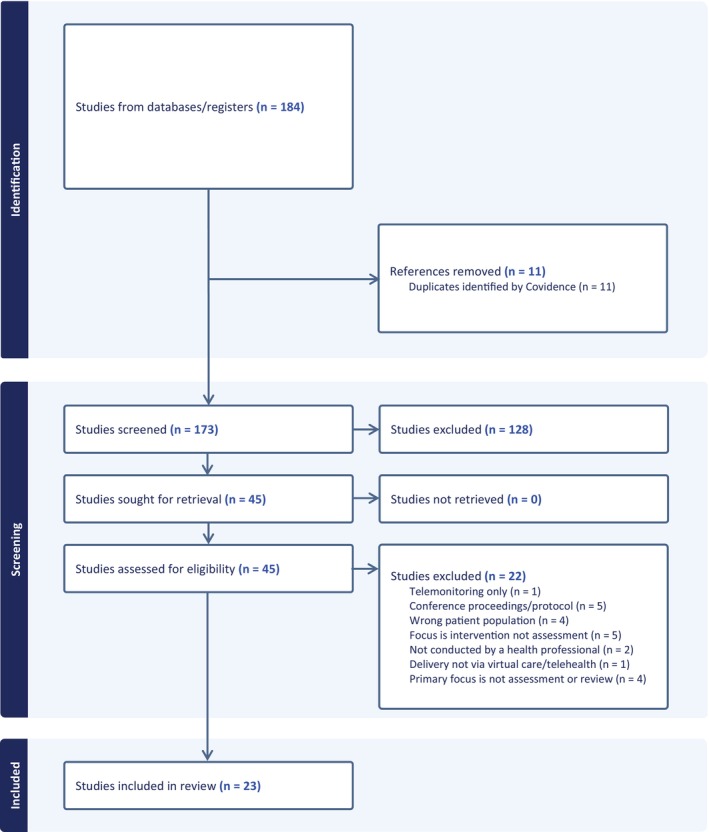
PRISMA flow chart of study selection.
3.1. Description of the Literature
Of the 23 included studies, most were from the United States (n = 12, 52%), then Australia (n = 5, 22%), Canada (n = 3, 13%), and single studies from the United Kingdom, Italy, and The Netherlands. Half the studies (n = 12, 53%) were published from 2020 to 2022 (inclusive), representing a significant increase in virtual care research in response to the COVID‐19 pandemic.
Most studies were retrospective or prospective cohort studies (n = 9), descriptive studies (n = 6), non‐randomised experimental studies (n = 5), two literature reviews, and one RCT. Studies reported data collected from one or more participant groups including clients (n = 19), carers (n = 7), and/or clinicians (n = 4). The age ranges and diagnoses of clients are reported in Table 3.
TABLE 3.
Characteristics of 23 included studies (In alphabetical order).
| Lead Author (year) | Country | Study design | Number of participants | Participants | Participant age group | Primary diagnosis of client participnts |
|---|---|---|---|---|---|---|
| Bullard, Harvey, and Abbeduto (2021) | US | Cohort | 40 participants | Clients and carers | Children | Fragile‐X syndrome |
| (Delves et al. 2022) | Australia | Cohort | 191 participants | Clients and carers | Adults | Mental health conditions with ID |
| (Eapen, Hiscock, and Williams 2021) | Australia | Descriptive | — | Clients | — | DD, ASD, ID |
| (Gentile et al. 2018) | US | Descriptive | Over 900 participants | Clients | — | Mental health condition and ID |
| (Hodge et al. 2019) | Australia | Non‐randomised experimental | 39 participants | Clients and clinicians | Children | Specific learning disorder with ADHD, ID |
| (Hopper, Buckman, and Edwards 2011) | Australia | Non‐randomised experimental | 10 participants |
Clients |
Children | DD, ID |
| (Langkamp, McManus, and Blakemore 2015) | US | Cohort | 295 participants | Clients and carers | Children and young people | DD, ASD, CP, ADHD, Down syndrome |
| (Letourneau et al. 2003) | Canada | Descriptive | 208 participants | Clients | Children | Epilepsy, DD, headache |
| (Madhavan 2019) | US | Literature review | 5 studies | Adults and children | Mental health care patients with ID | |
| (McNally et al. 2022) | US | Cohort | 382 participants | Clients, carers, and clinicians | Children | ASD, DD, ID, LD |
| (Merrill, Cowan, and Gentile 2017) | US | Descriptive | Over 1000 participants | Clients | — | Mental health condition and ID |
| (Nicholson et al. 2023) | UK | Cohort | 61 participants | Clinicians | — | ID Clinicians |
| (Pearl et al. 2014) | US, UAE | Descriptive | Not given | Clients | Adults and children | CP, ASD, DD, epilepsy, neurogenetic disorders, congenital abnormalities |
| (Prelack et al. 2022) | US | Descriptive | 7130 participants | Clients | Children | Epilepsy, migraine, DD |
| (Reese et al. 2013) | US | RCT | 47 participants | Clients, carers, and clinicians |
Children |
ASD, DD |
| (Rosen et al. 2022) | US | Cohort | 640 participants | Carers | Adults and children | ID |
| (Rowell et al. 2014) | Australia | Cohort | 126 participants | Clients | Children | CP, ID, DD, Down syndrome, Noonan Syndrome, mitochondrial disorders |
| (Shawler et al. 2021) | US | Non‐randomised experimental | 1 participant |
Client |
Adult | ASD, ID, Down syndrome |
| (Spaan, Verzaal, and Kaal 2021) | The Netherlands | Non‐randomised experimental | 89 participants | Client | Adults | Suspected mild to borderline ID |
| (Temple et al. 2010) | Canada | Non‐randomised experimental | 19 participants |
Clients |
Adults | ID, ASD, Down syndrome, Mixed expressive‐receptive disorder |
| (Trivisano et al. 2020) | Italy | Cohort | 3321 participants | Clients and carers | Adults and child(ren | Epilepsy |
| (Verma et al. (2022) | US | Cohort | 5 clinics | Clients | Children | ASD, DD |
| (Whittingham and Coons‐Harding 2021) |
Canada |
Literature review |
3 studies | Children | Foetal Alcohol Spectrum Disorders |
Abbreviations: ADHD = attention deficit hyperactivity disorder; ASD = autism spectrum disorder; CP = cerebral palsy; DD = developmental delay; ID = intellectual disability; LD = learning disorder/disability; UAE = United Arab Emirates; UK = United Kingdom; US = United States.
3.2. Description of Virtual Care Delivery
Included studies delivered a range of virtual assessments including specialist assessments (n = 5), comprehensive/multidisciplinary team assessments (n = 5), telepsychiatry assessments (n = 3), diagnostic assessments (n = 2), brief assessments or screening (n = 2), and one study reported primary care assessment via virtual care. Not all studies reported assessment type (see Table 4).
TABLE 4.
Characteristics of virtual care delivery in 23 included studies.
| Author (year) | Type of VC assessment | Location of client receiving VC | Format of delivery including duration/frequency of VC | Supports provide pre‐ or during appointment | Health professionals involved |
|---|---|---|---|---|---|
| Bullard et al. (2021) | Behavioural and psychological assessment |
Home |
Skype—interfacing with various devices/platforms 5–6 sessions |
Technology consultation and parent training. Carer support | Not reported |
| Delves et al. (2022) | Specialist assessment | Home, group home, community health service, ED |
PEXIP + various video platforms −interfacing with smartphone or laptop 4 appointments (average) |
Pre‐consultation re: client communication, client VC preference, and tolerance. Carer support | Psychiatrist |
| Eapen et al. (2021) | Not reported | Not reported | Not reported | Not reported | Not reported |
| Gentile et al. (2018) | Specialist assessment and intervention | Home, school | Phone with webcam | Not reported | Psychiatric, Nurse, SW, Counsellors, Behavioural specialists, Case managers |
| Hodge et al. (2019) | Cognitive assessment |
Specialist education clinic |
Video 1 appointment; 1 h duration |
Parent present but not directly involved in the assessment | Psychologist |
| Hopper et al. (2011) | Specialist assessment |
Outreach clinic |
Video 1 appointment. Duration not reported |
Pre‐assessment with the paediatrician. Technical support. Carer support | Geneticist and genetic counsellor |
| Langkamp et al. (2015) | Primary care assessment |
School |
Asynchronous store‐and‐forward, video camera and telephonic stethoscope 1 h appointment |
Pre‐survey re: telemedicine knowledge. Technical support and support from the school nurse | Primary care physician, Nurse |
| Letourneau et al. (2003) | Brief assessment | Not reported | Telephone calls | Not reported | Neurologist, Nurse |
| Madhavan (2019) | Telepsychiatry assessment and FU | Not reported | Various formats | Not reported | Nurse, Psychiatrist |
| McNally et al. (2022) | Diagnostic assessment | Home |
Secure email and Zoom. Telephone IT hotline 2 h diagnostic evaluation + behavioural observations |
Pre‐appointment email with written instructions via email and IT hotline. Carer support | Psychologist, Developmental‐behavioural paediatrician |
| Merrill et al. (2017) | Telepsychiatry | Home | Video | In‐person for first appointment. Carer support. |
Psychiatrist and interdisciplinary team |
| Nicholson et al. (2023) | Screening, comprehensive assessments, and FU. | Not reported | Telephone or video |
Carer support |
Psychiatrist, OT, PT, SLT |
| Pearl et al. (2014) | Comprehensive assessment | Rehabilitation Centre |
Video 1‐h weekly clinic |
Carer support | Paediatric neurologist, Geneticist, PT, OT, SLT, Rehabilitation specialist, Psychologist |
| Prelack et al. (2022) | Specialist assessment | Not reported | Audio–video or telephone | Not reported | Paediatric neurologist |
| Reese et al. (2013) | Comprehensive assessment | University Healthcare Facility |
Video Single assessment |
Carer support | Not reported |
| Rosen et al. (2022) | Specialist assessment | Home. | Video | Carer support | Psychologist and psychiatrist |
| Rowell et al. (2014) | Comprehensive assessment | Rural hospital |
Video 2‐h, 3 monthly clinics |
Not reported | Paediatrician, allied health, nurse |
| Shawler et al. (2021) | Comprehensive assessment | Home |
Zoom via iPhone, email, phone Talk Go button Assessment = naturalistic observation 10 min Intervention support = 5 h/day |
Pre‐appointment screening and, risk assessment via telehealth. Carer support × 2 | Psychologist, Behaviour analyst, Graduate psychology student |
| Spaan et al. (2021) | Research assessment | Not reported | Skype video conferencing | Technical assistance | Not reported |
| Temple et al. (2010) | Research assessment | Not reported | Video with two screens |
Agency staff present |
Psychologist |
| Trivisano et al. (2020) | Not reported | Not reported | Telephone, video call, email, text message | Not reported | MDT |
| Verma et al. (2022) | Telepsychiatry assessment | Home | Video | Not reported | Psychiatrist |
| Whittingham and Coons‐Harding (2021) | Diagnostic assessment and FU interventions | Not reported | Not reported | Pre‐appointment IT testing. Technical support | Nurse, Clinical Psychologist, Program Coordinator |
Abbreviations: ED = emergency department; FU = follow‐up; IT = information technology; MDT = multidisciplinary team; OT = occupational therapist; PT = physiotherapist; SLT = speech and language therapist; SW = social worker; VC = virtual care.
Clinicians conducted virtual care assessments from a range of locations, including specialist services (children's hospitals n = 5, university or specialised health care facilities n = 3), outpatient clinics (n = 4), community health services or primary care (n = 3), and school‐based (n = 1). Not all studies provided adequate information to determine the location of service provision.
Clients receiving virtual care services were primarily located in their own home or a group home (n = 9), at another health care facility (emergency department, rural hospital, outreach clinic, rehabilitation hospital, and community health service; n = 5), or at school (n = 3). Not all studies provided adequate information to determine the location of clients participating in virtual care appointments. Some studies reported multiple locations.
Both audio‐only (via telephone) and audio–video (via a videoconferencing platform) were used. Commercially available software such as Skype and Zoom were used, in addition to software designed specifically for health service delivery (e.g., PEXIP). Email and text messaging were reported in two studies, and an additional study used asynchronous store‐and‐forward technology to share resources. The reporting of assessment duration and frequency was variable and influenced by whether it was a single assessment or an assessment with follow‐up.
Prior consultation with the client or carer occurred in seven studies to screen for client communication needs and required supports, conduct risk assessments, technology training, and testing. One study reported conducting initial assessments in person, then subsequently via virtual care. Carer support during the appointment was described in many studies (n = 10) whilst technical support was less common (n = 4).
A range of individual discipline and multidisciplinary approaches were reported. Single discipline service provision was most often provided by a psychologist (n = 2), psychiatrist (n = 2) or neurologist (n = 1). Multidisciplinary approaches were more frequently reported (n = 14) involving a wide range of clinicians such as nurses, social workers, occupational therapists, physiotherapists, speech and language therapists, counsellors (including genetics counsellors), behaviour analysists/specialists, case workers, program coordinators, psychologists, psychiatrists, paediatricians, rehabilitation specialists, and neurologists.
3.3. Mapping to the NSW Health Virtual Care Strategy
The reported experiences and evidence for using virtual care with people with intellectual disabilities were mapped to the NSW Health Virtual Care Strategy (NSW Health 2022), with a specific focus on aligning evidence from the literature with the strategic implementation goals of ‘Investing in People’, ‘Designing Processes’, and ‘Building Technology’. An overview of literature relevant to each goal is provided in Tables 5, 5, 5, together with the number of studies providing supporting evidence (for additional detail see Supplementary Information). Each table is followed by a synthesis of relevant evidence.
TABLE 5.
(A) Mapping of evidence to the NSW Health (2022) Focus Area 1: Investing in people.
| Implementation goal | Number of studies |
|---|---|
|
3 |
|
5 |
|
1 |
|
13 |
|
15 |
|
6 |
|
11 |
|
0 |
|
2 |
|
3 |
|
— |
TABLE 5.
(B) Mapping of evidence to the NSW Health (2022) Focus Area 2: Designing Processes.
| Implementation goal | Number of studies |
|---|---|
|
7 |
|
3 |
|
4 |
|
5 |
|
3 |
|
0 |
|
5 |
|
0 |
|
0 |
|
3 |
|
9 |
|
4 |
TABLE 5.
(C) Mapping of evidence to the NSW Health (2022) Focus Area 3: Building Technology.
| Implementation goal | Number of studies |
|---|---|
|
14 |
|
1 |
|
4 |
|
3 |
|
4 |
|
0 |
|
0 |
3.3.1. Focus Area 1: Investing in People
Much of the emerging literature identified in this scoping review mapped to the strategic focus area of ‘Investing in People’ (see Table 5). The greatest number of studies focused on promoting the benefits of virtual care to clinicians and health staff (n = 15), raising awareness and promoting the benefits of virtual care to clients and carers (n = 13), and supporting equitable access to health care (n = 11). We were unable to locate evidence aligning with the implementation goals of involving people with intellectual disabilities and carers in the co‐design of virtual care services and resources or supporting Aboriginal populations in using virtual care. To reduce overlap in reporting, evidence related to internet connectivity is presented with implementation goal 3.1 Drive the technology roll‐out.
3.3.1.1. Experiences of Virtual Care
Several studies reported the benefits of virtual care from the perspectives of clients, carers, and clinicians. Authors reported that people with intellectual disabilities and their carers were more comfortable using virtual care and less anxious, engaged in greater levels of eye contact, and that video technology was effective for building positive rapport and engagement (Delves et al. 2022; Gentile et al. 2018; Hodge et al. 2019; Merrill, Cowan, and Gentile 2017; Pearl et al. 2014; Rosen et al. 2022; Shawler et al. 2021). One study highlighted that online therapy was more responsive than in‐person (McNally et al. 2022). Other reported benefits included greater flexibility and ease of scheduling appointments (Rosen et al. 2022; Langkamp, McManus, and Blakemore 2015), reduced cost, reduced travel, reduced waiting times, and reduced carer stress (Gentile et al. 2018; Merrill, Cowan, and Gentile 2017; Shawler et al. 2021; McNally et al. 2022; Langkamp, McManus, and Blakemore 2015; Rowell et al. 2014; Trivisano et al. 2020; Whittingham and Coons‐Harding 2021). Carers of children with intellectual disabilities reported reduced sensory overload and reduced distress caused by travel and unfamiliar environments (Rosen et al. 2022; Langkamp, McManus, and Blakemore 2015; Madhavan 2019; Verma et al. 2022). Early indicators of positive health outcomes included reduced hospitalisation and emergency department visits of people with intellectual disabilities accessing telepsychiatry services (Merrill, Cowan, and Gentile 2017).
Whilst satisfied with virtual care, some people with intellectual disabilities and carers would prefer in‐person consultation, seeking greater personal connection with the clinician (Merrill, Cowan, and Gentile 2017; Whittingham and Coons‐Harding 2021). Authors reported that engagement and communication became increasingly difficult when working with people with more severe intellectual disabilities (Nicholson et al. 2023; Merrill, Cowan, and Gentile 2017; Pearl et al. 2014; Trivisano et al. 2020; Hopper, Buckman, and Edwards 2011; Reese et al. 2013). In these cases, clinicians preferred to decide whether virtual care or in‐person assessment was most appropriate (Nicholson et al. 2023; Prelack et al. 2022).
A small number of studies reported negative client and carer experiences. Where reported, these included confidentiality concerns, technology difficulties, difficulty keeping clients engaged and compliant, particularly children, and the resultant burden and stress placed on the carer to facilitate the virtual assessment (Hodge et al. 2019; Rosen et al. 2022; Whittingham and Coons‐Harding 2021; Bullard, Harvey, and Abbeduto 2021). Two studies highlighted the additional challenges experienced by people from non‐English speaking backgrounds (Verma et al. 2022), suggesting the use of an interpreter during virtual care consultations adds complexity (Nicholson et al. 2023).
3.3.1.2. Access to Health Care
Improved access to health care services through the utilisation of virtual care was reported in many studies, with greater access enabled by eliminating barriers such as geographical remoteness, lack of specialised transport, and poor mobility (Merrill, Cowan, and Gentile 2017; Whittingham and Coons‐Harding 2021; Madhavan 2019; Verma et al. 2022). Access to virtual care decreased time to diagnosis for families (Whittingham and Coons‐Harding 2021), enabled earlier provision of treatment (Pearl et al. 2014), addressed health care gaps in rural communities (Whittingham and Coons‐Harding 2021), and supported links with non‐health care settings such as schools (Langkamp, McManus, and Blakemore 2015). Access to telepsychiatry assessment was found to be convenient and expedited the assessment process (Delves et al. 2022).
3.3.1.3. Skill Development
Many studies indicated the need to rapidly increase the skills, confidence, and competence of clinicians through training and education (Hodge et al. 2019; Pearl et al. 2014; Rosen et al. 2022; Whittingham and Coons‐Harding 2021; Hopper, Buckman, and Edwards 2011). In addition, the need for client and carer supports are also required to reduce barriers such as low levels of digital literacy, lack of experience, and lack of familiarity with technology (Nicholson et al. 2023; McNally et al. 2022; Whittingham and Coons‐Harding 2021; Verma et al. 2022). Supports provided before and during the virtual care appointment may be effectively provided in the form of written instructions and telephone technical assistance (McNally et al. 2022). Some studies provided ‘concierge’ administration support and troubleshooting (Gentile et al. 2018; Merrill, Cowan, and Gentile 2017; Langkamp, McManus, and Blakemore 2015; Rowell et al. 2014; Whittingham and Coons‐Harding 2021).
3.3.2. Focus Area 2: Designing Processes
Table 5 outlines the literature that mapped to the strategic focus area of ‘Designing Processes’ supporting delivery of virtual care to clients with intellectual disabilities (see Table 5). Several studies mapped to the implementation goals of shared care (n = 9), funding models (n = 7), supporting the roll‐out of virtual care to priority populations (n = 5), and monitoring and evaluation (n = 5). We were unable to locate evidence aligning with three implementation goals in this key area including: enabling effective change management, consolidating patient‐reported measures, or facilitating safety intelligence for virtual care.
3.3.2.1. Shared Care
The opportunity for virtual care to enhance shared care, improve access to multidisciplinary teams, and improve stakeholder coordination was reported in several studies (Whittingham and Coons‐Harding 2021; Verma et al. 2022). Virtual care increased patient and family‐oriented care via telenursing (Letourneau et al. 2003), multidisciplinary service provision, and meetings (Nicholson et al. 2023; Letourneau et al. 2003), and enabled the participation of health providers at non‐health sites such as schools (Langkamp, McManus, and Blakemore 2015). Shared virtual care was not without challenges such as attempting to complete a multidisciplinary assessment in a single session (Trivisano et al. 2020), logistical and resource challenges, and inadequate health policies or frameworks to guide delivery (Whittingham and Coons‐Harding 2021; Prelack et al. 2022).
3.3.2.2. Priority Populations
Delivery of virtual care to people with intellectual disabilities living in rural and remote locations was identified as a priority in two studies (Delves et al. 2022; Gentile et al. 2018), however, limited access to technology and low patient numbers in rural areas were identified as challenges (Hodge et al. 2019; Rowell et al. 2014). Further research is required to identify priority populations and areas for the roll‐out of virtual care including consideration of existing services, service gaps, and clinical scenarios where virtual care is appropriate (Pearl et al. 2014; Trivisano et al. 2020).
3.3.2.3. Deciding When to Use (or Not to Use) Virtual Care
Some studies identified that virtual care was not always suitable, for example conducting physical examinations, assessing clients with unstable medical conditions (Trivisano et al. 2020; Prelack et al. 2022), and using psychological assessments not validated for use via virtual care (Verma et al. 2022). The need to modify the virtual assessment of people with intellectual disabilities to include screening for communication difficulties was also identified (Delves et al. 2022). Notwithstanding the above‐identified challenges, studies reported successful adaptation of assessment practices for administration via virtual care (Hodge et al. 2019; Trivisano et al. 2020; Hopper, Buckman, and Edwards 2011).
3.3.2.4. Clinical Governance
There is an urgent need to develop policies and procedures to address standards of care (Whittingham and Coons‐Harding 2021) and management of acute health issues or risks such as behavioural dysregulation or suicidality (Verma et al. 2022). Clinical governance considerations should include assessing different models of care to determine which services are appropriate to be delivered via virtual care and should consider the location of clients in relation to the health care providers (Trivisano et al. 2020). Other studies highlighted the need to assess the appropriateness of virtual or hybrid models (Trivisano et al. 2020; Whittingham and Coons‐Harding 2021). Models of virtual care services need flexibility to accommodate delivery in both clinical settings and clients' homes (Delves et al. 2022; Merrill, Cowan, and Gentile 2017; Hopper, Buckman, and Edwards 2011). One study highlighted that the physical environment in which virtual care is received also needs consideration as part of future governance frameworks (Whittingham and Coons‐Harding 2021).
3.3.2.5. Funding Implications
The financial benefits and efficiencies for clinicians included reduced travel and travel‐related expenses, and reduced health care delivery costs (Pearl et al. 2014; Madhavan 2019). However, the significant establishment costs of setting up virtual care services need to be managed in order to support broad health service‐wide implementation (Hodge et al. 2019). One study also highlighted that achieving the required economies of scale may be a specific challenge in rural areas for services with low patient numbers (Rowell et al. 2014). System scaling will be supported by the planned use of technology that is financially practical and readily available (Hodge et al. 2019).
3.3.3. Focus Area 3: Building Technology
With the exception of driving the technology roll‐out, few studies were identified that focused on building technology to support virtual care for clients with intellectual disabilities (see Table 5). A total of 14 studies were identified that focused on one or more aspects of technology roll‐out. No studies were located that focused on the implementation goals of developing new virtual care applications or the creation of a virtual care simulator.
3.3.3.1. Technology Roll‐Out
Several studies highlighted that the technology roll‐out must consider appropriate equipment with suitable internet connectivity to enable quality images and audio, routine maintenance, and software updates as virtual models of care evolve (Merrill, Cowan, and Gentile 2017; Rowell et al. 2014; Trivisano et al. 2020; Whittingham and Coons‐Harding 2021; Madhavan 2019; Bullard, Harvey, and Abbeduto 2021). To enable equitable access to virtual care, several studies endorsed the need to allow flexibility of device and software (Delves et al. 2022; Hodge et al. 2019; Bullard, Harvey, and Abbeduto 2021) such as the choice to use the client's device or have one provided (Bullard, Harvey, and Abbeduto 2021) and the ability to use commercially available and portable devices (Hodge et al. 2019). These considerations can mitigate foreseeable technical challenges experienced by clients with intellectual disabilities and/or clinicians (Prelack et al. 2022).
Technology that supports the combination of video and audio was considered superior to audio alone (Nicholson et al. 2023; Pearl et al. 2014). Technology can be used to enhance engagement of clients including via sharing videos, visual aids, and games during appointments (Merrill, Cowan, and Gentile 2017; Whittingham and Coons‐Harding 2021; Verma et al. 2022).
3.3.3.2. Data Sharing and Privacy
Virtual care presents some risks to data privacy. People with intellectual disabilities and carers may have concerns regarding data privacy (Gentile et al. 2018), however, these concerns can be well managed. Technology and devices need to be secure to meet confidentiality standards (Pearl et al. 2014; Verma et al. 2022). In one study, clients and carers agreed their virtual care appointment was private (McNally et al. 2022). One study conducted across multiple health care sites reported difficulties with health record integration when different sites used different software (Langkamp, McManus, and Blakemore 2015).
4. Discussion
This scoping review included 23 studies each reporting on the successful delivery of virtual care assessments involving people with intellectual disabilities across the lifespan. Virtual care was typically delivered by clinicians located in hospital‐based, outpatient, or community‐based services, to clients and carers located in their own home or group home, at another health service, or at school. A range of assessments, including specialist, multidisciplinary, psychiatry, diagnostic, and screening assessments, was delivered via virtual care. People with neurodevelopmental disorders including intellectual developmental disorder, mental health conditions, and neurological conditions engaged with virtual care assessment. Most evidence collated and synthesised in this review mapped well to the NSW Virtual Care Strategy (NSW Health 2022). Key findings are discussed below with evidence gaps then highlighted.
The rapid acceleration of virtual care since the COVID‐19 pandemic has generally occurred without consideration of clinician education and training (Palesy, Forrest, and Crowley 2023a). The need for sustained investment in building the confidence, competence, and capacity of the clinical workforce to deliver virtual care for people with intellectual disabilities is recommended in the NSW Virtual Care Strategy, reinforced throughout this review. Recently published educational frameworks (Health Education and Training Institute 2022) reiterate the need for evidence‐informed curriculum and pedagogical approaches to prepare current and future clinicians to deliver virtual care encompassing the seven domains of compliance, professional practice, patient safety, communication, interprofessional collaboration, patient assessment, and care planning, delivery, and coordination. Recently published reviews (Palesy, Forrest, and Crowley 2023a, 2023b) highlight key educational strategies and supports for clinicians to build confidence in using virtual care, including virtual care checklists, clinical champions, and models that are co‐designed with clinicians, content experts, and care recipients. Delves et al. (Delves et al. 2022) demonstrated that technology issues during the delivery of virtual care are minimised when it is delivered by experienced clinicians who have received virtual care training.
This review was unable to find evidence of consultation with people with intellectual disabilities or carers in the design or delivery of virtual care services which is an identified implementation goal of the NSW Virtual Care Strategy (NSW Health 2022). The value of a national plan for co‐designing health care in partnership with people who have lived experience of disability is explicitly highlighted in the findings of the Royal Commission (Royal Commission 2023a), enabling people with intellectual disabilities and those who support them to exercise greater choice and control over their health care (Recommendation 6.1, p. 213).
Enabling people with intellectual disabilities and their carers to access virtual health care requires consideration of specific supports and accommodations. Lack of experience with digital technologies, low levels of digital literacy, and fewer opportunities to build technology skills are known barriers for people with intellectual disabilities (Khanlou et al. 2021). Pre‐appointment assessment of communication needs and familiarisation with the client and family (Delves et al. 2022; Whittingham and Coons‐Harding 2021) were identified in this scoping review as enabling strategies that could support client autonomy and promote greater inclusion in the virtual appointment. Services that offered pre‐appointment IT support and screening for technical issues reported fewer barriers to accessing virtual care. Virtual care concierge services reported in other areas of health care service delivery (Rariy et al. 2021) report high levels of client and clinician satisfaction. Other service models (e.g., in telepsychiatry) include a virtual care navigator (Johnston and Yellowlees 2016), a non‐clinical liaison role, collecting clinical and administrative information prior to appointments, and providing education and training to clients and carers to facilitate access. In line with these findings, the Royal Commission (Royal Commission 2023b) also recommends the introduction of disability health navigators to support people with disabilities access health services (Recommendation 6.34, p. 402).
People with intellectual disabilities often have multiple specialists and health professionals involved in their care. Lack of coordination between health professionals can be a barrier to receiving continuity of health care and create clinical risk. The findings of this review suggest that virtual care supports clinicians, disability workers, and educational support staff to be involved simultaneously (Langkamp, McManus, and Blakemore 2015) to provide time‐sensitive input to client discussions. The Royal Commission has highlighted the benefits of effective communication and the need for coordination between health professionals to achieve continuity of care (p. 348, 35). Greater integration of virtual care into health services may be one strategy to enhance multidisciplinary care for people with intellectual disabilities who have complex care and support needs.
People with intellectual disabilities living in regional and remote areas typically face significant challenges accessing specialist services that are often concentrated in large metropolitan centres (NSW Health 2023). This scoping review noted the clear benefit of improved access to specialists when the person with intellectual disabilities is geographically remote (Verma et al. 2022), and for those with transport and mobility challenges. Article 25 of the Convention on the Rights of Persons with Disabilities (United Nations 2008) outlines the obligation to provide ‘health services as close as possible to people's own communities, including in rural areas.’ Enabling virtual access to specialist intellectual disability services may create an opportunity to meet national obligations under the United Nations Convention whilst simultaneously improving health service access and health outcomes for people living in regional, rural, and remote communities (NSW Health 2023).
As in other areas of managing chronic health conditions (Brody et al. 2020), virtual care for people with intellectual disabilities can offer opportunities to strengthen person‐centred and family‐centred care. Receiving virtual care at or close to home allowed people with intellectual disabilities to be more comfortable during their appointments, reduced sensory distress caused by unfamiliar clinical environments, and also reduced travel distress (Delves et al. 2022; Merrill, Cowan, and Gentile 2017; Rosen et al. 2022; Rowell et al. 2014; Trivisano et al. 2020; Verma et al. 2022). Virtual care may be one strategy to bring health care services closer to home as recommended by state (NSW Health 2023) and national (Royal Commission 2023b) health care directives. This scoping review highlights a generally positive experience of virtual care reported by clients and carers with overall high levels of acceptability. Additional benefits to people with intellectual disabilities and carers included several pragmatic benefits such as convenience, ease of scheduling appointments, flexibility of appointments, cost, and time savings (Delves et al. 2022; Shawler et al. 2021; Trivisano et al. 2020; Verma et al. 2022; Bullard, Harvey, and Abbeduto 2021).
Access to virtual care is enabled by socioeconomic advantages such as higher income and education levels (Bullard, Harvey, and Abbeduto 2021). Health inequities in accessing digital health solutions have been broadly identified (Yao et al. 2022). To achieve broad system scaling of virtual health care, the systems and software required by clients, need to be commercially available at no or low cost, accessible by portable devices and a range of web platforms (Hodge et al. 2019; Bullard, Harvey, and Abbeduto 2021). While the NSW Virtual Care Strategy (NSW Health 2022) incorporates several implementation goals to build technology that supports virtual care access, the digital exclusion of people with intellectual disabilities has been highlighted during the COVID‐19 pandemic, exacerbated by sociopolitical, structural, individual, and support‐related barriers (Chadwick et al. 2022). Digital poverty, literacy, and exclusion remain significant issues for people with intellectual disabilities internationally (Chadwick et al. 2022). Several studies in this scoping review advocated for consideration of people with intellectual disabilities when building technology and digital infrastructure, however, this goal remains elusive. No studies were identified that described or evaluated patient‐reported measures being used with or by people with intellectual disabilities to give feedback on their experiences of virtual care. People with intellectual disabilities are often excluded from participation in surveys of patient experience due to the format, nature, and distribution methods by which patient experience surveys are implemented (Shogren et al. 2021).
The Royal Commission explicitly highlighted that people with disabilities can only access environments, facilities, services, and information if they are able to use and interact with them in a way that responds to their needs (Royal Commission 2023a). This is inclusive of the online environment. This review found limited evidence for consideration of the needs of people with intellectual disabilities in building the technology to support the virtual care roll‐out. It is critical that future health technologies consider accessibility for people with intellectual and communication disabilities.
4.1. Limitations
This review focused on the use of virtual care to assess the health needs of people with intellectual disabilities. It did not extend to the use of virtual care for other digital health innovations including remote health monitoring or therapeutic interventions such as positive behaviour supports. An evaluation of the methodological quality of each included study was not conducted. This review was limited to studies published in English. Studies from all countries were included, however, the findings are considered in an Australian context, with reference to the NSW Virtual Care Strategy (NSW Health 2022) and the recently published findings of the Royal Commission (Royal Commission 2023a). These frameworks and recommendations may not generalise to all health and disability service models beyond the Australian context. The authors also note the limitation that arises from the conflation of viewpoints of individuals with intellectual disabilities and their carers. Studies included in this review predominantly expressed views and perspectives from both viewpoints, without differentiation between these. As such, the authors were not able to separate the voices of people with intellectual disabilities from the voices of carers in the included studies, however, we recognise that people with intellectual disabilities may have conflicting preferences from their carers in terms of health care service delivery.
4.2. Future Research and Policy Implications
Following the authors' mapping of current literature to the NSW Virtual Care Strategy (NSW Health 2022), several critical gaps were identified that warrant further research. Most importantly, there was a lack of studies that involved people with intellectual disabilities and carers in the co‐design, co‐delivery, and co‐evaluation of virtual care services or supports. When considering specific population groups, future research should conside the use of virtual care by people with intellectual disabilities who are from an Aboriginal or Torres Strait Islander background and other ethnically and linguistically diverse groups.
4.3. Conclusion
This scoping review supports the safe and effective use of virtual care to assess the health needs of people across the lifespan with intellectual disabilities. It provides supporting evidence for the use of multidisciplinary assessment and specialist individual disciplinary assessment for the purposes of screening, diagnosis, comprehensive assessment, and review. Clients with intellectual disabilities and carers generally reported positive experiences with virtual care, and greater access to services was a highlighted benefit, particularly for priory populations such as regional, rural, and remote communities. The existing literature mapped well to the NSW Virtual Care Strategy (NSW Health 2022) and highlighted policy and practice implications for clinician training and education, client and carer supports, and considerations for people with intellectual disabilities during the roll‐out of virtual care technologies.
Ethics Statement
The authors have nothing to report.
Consent
The authors have nothing to report.
Conflicts of Interest
The authors declare no conflicts of interest.
Supporting information
Data S1. NSW Virtual Care Strategy (NSW Health, 2022) implementation goals and related evidence from ID literature.
Funding: This work was supported by the Australian Government's Rural Health Multidisciplinary Training (RHMT) Scheme.
Endnotes
Specialised Intellectual Disability clinicians include medical, nursing, and allied health professionals employed by the specialised Intellectual Disability Health Service https://www.health.nsw.gov.au/disability/Pages/statewide‐intellectual‐disability‐health‐service.aspx.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
References
- Arksey, H. , and O'Malley L.. 2005. “Scoping Studies: Towards a Methodological Framework.” International Journal of Social Research Methodology 8, no. 1: 19–32. [Google Scholar]
- Brody, A. A. , Sadarangani T., Jones T. M., et al. 2020. “Family‐ and Person‐Centered Interdisciplinary Telehealth: Policy and Practice Implications Following Onset of the COVID‐19 Pandemic.” Journal of Gerontological Nursing 46, no. 9: 9–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bullard, L. , Harvey D., and Abbeduto L.. 2021. “Exploring the Feasibility of Collecting Multimodal Multiperson Assessment Data via Distance in Families Affected by Fragile X Syndrome.” Journal of Telemedicine and Telecare 29: 1–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chadwick, D. , Ågren K. A., Caton S., et al. 2022. “Digital Inclusion and Participation of People With Intellectual Disabilities During COVID‐19: A Rapid Review and International Bricolage.” Journal of Policy and Practice in Intellectual Disabilities 19, no. 3: 242–256. [Google Scholar]
- Delves, M. , Luscombe G. M., Juratowitch R., et al. 2022. “‘Say Hi to the Lady on the Television’: A Review of Clinic Presentations and Comparison of Telepsychiatry and In‐Person Mental Health Assessments for People With Intellectual Disability in Rural New South Wales.” Journal of Policy & Practice in Intellectual Disabilities 20: 177–191. [Google Scholar]
- Eapen, V. , Hiscock H., and Williams K.. 2021. “Adaptive Innovations to Provide Services to Children With Developmental Disabilities During the COVID‐19 Pandemic.” Journal of Paediatrics and Child Health 57, no. 1: 9–11. [DOI] [PubMed] [Google Scholar]
- Esther, C. , Natalie O., Diana B., et al. 2022. “Telehealth in a Paediatric Developmental Metropolitan Assessment Clinic: Perspectives and Experiences of Families and Clinicians.” Health Expectations 25, no. 5: 2557–2569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentile, J. P. , Cowan A. E., Harper B., Mast R., and Merrill B.. 2018. “Reaching Rural Ohio With Intellectual Disability Psychiatry.” Journal of Telemedicine and Telecare 24, no. 6: 434–439. [DOI] [PubMed] [Google Scholar]
- Health Education and Training Institute . 2022. “NSW Health Virtual Care Education Framework.”
- Hodge, M. A. , Sutherland R., Jeng K., et al. 2019. “Agreement Between Telehealth and Face‐To‐Face Assessment of Intellectual Ability in Children With Specific Learning Disorder.” Journal of Telemedicine and Telecare 25, no. 7: 431–437. [DOI] [PubMed] [Google Scholar]
- Hopper, B. , Buckman M., and Edwards M.. 2011. “Evaluation of Satisfaction of Parents With the Use of Videoconferencing for a Pediatric Genetic Consultation.” Twin Research and Human Genetics 14, no. 4: 343–346. [DOI] [PubMed] [Google Scholar]
- Intellectual Disability Health Network . 2017. “Building Capability in NSW Health Services for People With Intellectual Disability: The Essentials.” In Innovation AfC. Sydney, Australia: Agency for Clinical Innovation. [Google Scholar]
- Johnston, B. , and Yellowlees P.. 2016. “Telepsychiatry Consultations in Primary Care Coordinated by Virtual Care Navigators.” Psychiatric Services 67, no. 1: 142. [DOI] [PubMed] [Google Scholar]
- Khanlou, N. , Khan A., Vazquez L. M., and Zangeneh M.. 2021. “Digital literacy, Access to Technology and Inclusion for Young Adults with Developmental Disabilities.” Journal of Developmental and Physical Disabilities 33, no. 1: 1–25. [Google Scholar]
- Langkamp, D. L. , McManus M. D., and Blakemore S. D.. 2015. “Telemedicine for Children With Developmental Disabilities: A More Effective Clinical Process Than Office‐Based Care.” Telemedicine and e‐Health 21, no. 2: 110–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letourneau, M. A. , MacGregor D. L., Dick P. T., et al. 2003. “Use of a Telephone Nursing Line in a Pediatric Neurology Clinic: One Approach to the Shortage of Subspecialists.” Pediatrics 112, no. 5: 1083–1087. [DOI] [PubMed] [Google Scholar]
- Madhavan, G. 2019. “Telepsychiatry in Intellectual Disability Psychiatry: Literature Review.” BJPsych Bulletin 43, no. 4: 167–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally, K. R. , Enneking B., James C., et al. 2022. “Telehealth Evaluation of Pediatric Neurodevelopmental Disabilities During the COVID‐19 Pandemic: Clinician and Caregiver Perspectives.” Journal of Developmental and Behavioral Pediatrics 43, no. 5: 262–272. [DOI] [PubMed] [Google Scholar]
- Merrill, B. , Cowan A. E., and Gentile J. P.. 2017. “House Calls: Telepsychiatry With Patients With Intellectual Disability.” Annals of Medical and Health Sciences Research 7, no. 6: 463–465. [Google Scholar]
- Nicholson, L. , Sharma S., Andrews S., Farquharson A., and Welsh H.. 2023. “A Survey on the Use of Remote Consultation for People With Intellectual Disability: The Experience of Community Intellectual Disability Teams.” Journal of Intellectual & Developmental Disability 48, no. 1: 85–90. [Google Scholar]
- NSW Health . 2022. NSW Virtual Care Strategy 2021–2026: Connecting Patients to Care. St Leonards: NSW Ministry of Health. [Google Scholar]
- NSW Health . 2023. NSW Regional Health Strategic Plan 2022–2032. Australia: NSW Ministry of Health. [Google Scholar]
- Oudshoorn, C. E. M. , Frielink N., Nijs S. L. P., and Embregts P. J. C. M.. 2021. “Psychological eHealth Interventions for People With Intellectual Disabilities: A Scoping Review.” Journal of Applied Research in Intellectual Disabilities 34, no. 4: 950–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palesy, D. , Forrest G., and Crowley M. E.. 2023a. “Education Guidelines, Frameworks and Resources for Building Virtual Care Capacity: An Integrative Review.” Journal of Telemedicine and Telecare 29, no. 3: 222–243. [DOI] [PubMed] [Google Scholar]
- Palesy, D. , Forrest G., and Crowley M. E.. 2023b. “Curriculum Interventions and Pedagogical Approaches for Virtual Care Delivery: A Scoping Review.” Home Health Care Management and Practice 35, no. 1: 40–47. [Google Scholar]
- Pearl, P. L. , Sable C., Evans S., et al. 2014. “International Telemedicine Consultations for Neurodevelopmental Disabilities.” Telemedicine and e‐Health 20, no. 6: 559–562. [DOI] [PubMed] [Google Scholar]
- Prelack, M. , Fridinger S., Gonzalez A. K., et al. 2022. “Visits of Concern in Child Neurology Telemedicine.” Developmental Medicine and Child Neurology 64: 1351–1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rariy, C. , Truesdale L., Greenman J., and Schink J. C.. 2021. “Key Features to Ensure Sustainability of a Tele‐Oncology Program at a National Cancer Center.” Journal of Clinical Oncology 39: e13613‐e–e13613. [Google Scholar]
- Reese, R. M. , Jamison R., Wendland M., et al. 2013. “Evaluating Interactive Videoconferencing for Assessing Symptoms of Autism.” Telemedicine and e‐Health 19, no. 9: 671–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen, V. , Blank E., Lampert E., et al. 2022. “Brief Report: Telehealth Satisfaction Among Caregivers of Pediatric and Adult Psychology and Psychiatry Patients With Intellectual and Developmental Disability in the Wake of Covid‐19.” Journal of Autism and Developmental Disorders 52, no. 12: 5253–5265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowell, P. D. , Pincus P., White M., and Smith A. C.. 2014. “Telehealth in Paediatric Orthopaedic Surgery in Queensland: A 10‐Year Review.” ANZ Journal of Surgery 84, no. 12: 955–959. [DOI] [PubMed] [Google Scholar]
- Royal Commission . 2023a. “Final Report—Executive Summary, Our Vision for an Inclusive Australia and Recommendations.” In Australia co. Australia: Commonwealth of Australia. [Google Scholar]
- Royal Commission . 2023b. “Enabling Autonomy and Access.” In Australia co. Canberra, Australia: Commonwealth of Australia. [Google Scholar]
- Selick, A. , Bobbette N., Lunsky Y., Hamdani Y., Rayner J., and Durbin J.. 2021. “Virtual Health Care for Adult Patients With Intellectual and Developmental Disabilities: A Scoping Review.” Disability and Health Journal 14, no. 4: 101132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shawler, L. A. , Clayborne J. C., Nasca B., and O'Connor J. T.. 2021. “An Intensive Telehealth Assessment and Treatment Model for an Adult With Developmental Disabilities.” Research in Developmental Disabilities 111: 103876. [DOI] [PubMed] [Google Scholar]
- Shogren, K. A. , Bonardi A., Cobranchi C., et al. 2021. “State of the Field: The Need for Self‐Report Measures of Health and Quality of Life for People With Intellectual and Developmental Disabilities.” Journal of Policy and Practice in Intellectual Disabilities 18, no. 4: 286–295. [Google Scholar]
- Spaan, N. A. , Verzaal M., and Kaal H. L.. 2021. “Feasibility and Reliability of Screening on Mild to Borderline Intellectual Disabilities Using SCIL Through Video‐Administration.” Journal of Intellectual Disabilities & Offending Behaviour 12, no. 1: 12–22. [Google Scholar]
- Temple, V. , Drummond C., Valiquette S., and Jozsvai E.. 2010. “A Comparison of Intellectual Assessments Over Video Conferencing and In‐Person for Individuals With ID: Preliminary Data.” Journal of Intellectual Disability Research 54, no. 6: 573–577. [DOI] [PubMed] [Google Scholar]
- Trivisano, M. , Specchio N., Pietrafusa N., et al. 2020. “Impact of COVID‐19 Pandemic on Pediatric Patients With Epilepsy—The Caregiver Perspective.” Epilepsy & Behavior 113: 107527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations . 2008. Convention on the Rights of Persons With Disabilities. New York: United Nations. https://social.desa.un.org/issues/disability/crpd/convention‐on‐the‐rights‐of‐persons‐with‐disabilities‐crpd?page=2. [Google Scholar]
- Verma, S. , Vandana P., Soda T., et al. 2022. “Incorporation of Telepsychiatry for Patients With Developmental Disorders Into Routine Clinical Practice—A Survey of Specialty Clinics Adapting to Telepsychiatry During the COVID‐19 Pandemic.” Journal of Autism and Developmental Disorders 52: 5280–5284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittingham, L. M. , and Coons‐Harding K. D.. 2021. “Connecting People With People: Diagnosing Persons With Fetal Alcohol Spectrum Disorder Using Telehealth.” Journal of Autism and Developmental Disorders 51, no. 4: 1067–1080. [DOI] [PubMed] [Google Scholar]
- Yao, R. , Zhang W., Evans R., Cao G., Rui T., and Shen L.. 2022. “Inequities in Health Care Services Caused by the Adoption of Digital Health Technologies: Scoping Review.” Journal of Medical Internet Research 24, no. 3: e34144. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. NSW Virtual Care Strategy (NSW Health, 2022) implementation goals and related evidence from ID literature.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.


