Abstract
Background
Email is a popular and commonly‐used method of communication, but its use in health care is not routine. Where email communication has been demonstrated in health care this has included its use for communication between patients/caregivers and healthcare professionals for clinical purposes, but the effects of using email in this way is not known.This review addresses the use of email for two‐way clinical communication between patients/caregivers and healthcare professionals.
Objectives
To assess the effects of healthcare professionals and patients using email to communicate with each other, on patient outcomes, health service performance, service efficiency and acceptability.
Search methods
We searched: the Cochrane Consumers and Communication Review Group Specialised Register, Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 1 2010), MEDLINE (OvidSP) (1950 to January 2010), EMBASE (OvidSP) (1980 to January 2010), PsycINFO (OvidSP) (1967 to January 2010), CINAHL (EbscoHOST) (1982 to February 2010) and ERIC (CSA) (1965 to January 2010). We searched grey literature: theses/dissertation repositories, trials registers and Google Scholar (searched July 2010). We used additional search methods: examining reference lists, contacting authors.
Selection criteria
Randomised controlled trials, quasi‐randomised trials, controlled before and after studies and interrupted time series studies examining interventions using email to allow patients to communicate clinical concerns to a healthcare professional and receive a reply, and taking the form of 1) unsecured email 2) secure email or 3) web messaging. All healthcare professionals, patients and caregivers in all settings were considered.
Data collection and analysis
Two authors independently assessed the risk of bias of included studies and extracted data. We contacted study authors for additional information. We assessed risk of bias according to the Cochrane Handbook for Systematic Reviews of Interventions. For continuous measures, we report effect sizes as mean differences (MD). For dichotomous outcome measures, we report effect sizes as odds ratios and rate ratios. Where it was not possible to calculate an effect estimate we report mean values for both intervention and control groups and the total number of participants in each group. Where data are available only as median values it is presented as such. It was not possible to carry out any meta‐analysis of the data.
Main results
We included nine trials enrolling 1733 patients; all trials were judged to be at risk of bias. Seven were randomised controlled trials; two were cluster‐randomised controlled designs. Eight examined email as compared to standard methods of communication. One compared email with telephone for the delivery of counselling. When email was compared to standard methods, for the majority of patient/caregiver outcomes it was not possible to adequately assess whether email had any effect. For health service use outcomes it was not possible to adequately assess whether email has any effect on resource use, but some results indicated that an email intervention leads to an increased number of emails and telephone calls being received by healthcare professionals. Three studies reported some type of adverse event but it was not clear if the adverse event had any impact on the health of the patient or the quality of health care. When email counselling was compared to telephone counselling only patient outcomes were measured, and for the majority of measures there was no difference between groups. Where there were differences these showed that telephone counselling leads to greater change in lifestyle modification factors than email counselling. There was one outcome relating to harm, which showed no difference between the email and the telephone counselling groups. There were no primary outcomes relating to healthcare professionals for either comparison.
Authors' conclusions
The evidence base was found to be limited with variable results and missing data, and therefore it was not possible to adequately assess the effect of email for clinical communication between patients/caregivers and healthcare professionals. Recommendations for clinical practice could not be made. Future research should ideally address the issue of missing data and methodological concerns by adhering to published reporting standards. The rapidly changing nature of technology should be taken into account when designing and conducting future studies and barriers to trial development and implementation should also be tackled. Potential outcomes of interest for future research include cost‐effectiveness and health service resource use.
Keywords: Humans, Professional‐Patient Relations, Caregivers, Caregivers/statistics & numerical data, Electronic Mail, Electronic Mail/statistics & numerical data, Health Personnel, Health Personnel/statistics & numerical data, Randomized Controlled Trials as Topic, Telephone, Telephone/statistics & numerical data
Plain language summary
Using email for patients/caregivers and healthcare professionals to contact each other
Email is widely used in many sectors and lots of people use it in their day to day lives. The use of email in health care is not yet so common, although one use for it is for patients/caregivers and healthcare professionals to contact each other. This review examines how patients, healthcare professionals and health services may be affected by using email in this way. We looked for trials examining the use of email for patients/caregivers and healthcare professionals to contact each other and found nine trials with 1733 participants in total.
Eight of the trials looked at email compared with standard methods of communication. Where email was compared to standard methods of communication we found that we could not properly determine what effect email was having on patient/caregiver outcomes, as there were missing data and the results of the different studies varied. For health service use outcomes the situation was the same, but some results seemed to show that an email intervention may lead to an increased number of emails and telephone calls being received by healthcare professionals.
One of the trials looked at email counselling compared with telephone counselling. We found that it only looked at patient outcomes, and found few differences between groups. Where there were differences these showed that telephone counselling leads to greater changes in lifestyle than email counselling.
None of the trials measured how email affects healthcare professionals and only one measured whether email can cause harm. All of the trials were biased in some way and when we measured the quality of all of the results we found them to be of low or very low quality. As a result the results of this review should be viewed with caution.
The nature of the results means that we cannot make any recommendations for how email might best be used in clinical practice. Future research should make allowances for how quickly technology changes, and should consider how much email would cost to introduce and what effect it has on the use of healthcare resources. Research reports should be sure to clearly report their methods and findings, and researchers interested in carrying out research in this area should be assisted in developing ideas and put them into action.
Summary of findings
Summary of findings for the main comparison. Summary of findings: Email as additional communication method compared to standard methods: Patient participants.
| Email as additional method of communication compared to standard methods of communication | |||
| Patient or population: Healthcare usersa Settings: Different healthcare settings b Intervention: Email communicationc | |||
| Outcomes | No of Participants (studies) | Quality of the evidence (GRADE) | Impact |
| Patient's understanding | 74 (1 study) | ⊕⊝⊝⊝ very lowd,e,f | It was not possible to adequately assess whether email has any effect on a patient's understanding. |
| Patient health status and wellbeing | 147 (2 studies) | ⊕⊝⊝⊝ very lowg,h,i,j,k | It was not possible to adequately assess whether email has any effect on a patient's health status and wellbeing |
| Patient/caregiver views | 90 (2 studies) | ⊕⊝⊝⊝ very lowl, m | It was not possible to adequately assess whether email has any effect on patient/caregiver views |
| Patient behaviours and actions | 147 (2 studies) | ⊕⊝⊝⊝ very lown,o,p,q | It was not possible to adequately assess whether email has any effect on patient behaviours and actions, though it is possible to report that email did not have any effect on a patient's use of the internet. |
| Health service outcome; resource use | 379 (3 studies) | ⊕⊝⊝⊝ very lowr,s,t,u | It is unclear to what extent email impacts on resource use when compared with standard methods of communication, with studies reporting variable results or having missing data. |
| Health professional outcomes | 0 (0) | See impact | NOT MEASURED |
| Harms | 0 (0) | See impact | NOT MEASURED |
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
a children & young adults, caregivers, adults b head and neck surgery, paediatric dermatology clinic, augmentative communication service, heart failure clinic, primary care. c standard email, secure web system, patient portal. d Serious limitation, 3 of 6 domains have high risk of bias e Examines patient understanding in relation to post‐operative instructions only f One study for this outcome, 74 participants responding, measure using median values as data not normally distributed. g Two studies, one with 3 of 6 domains high risk, another with 4 of 6 high risk h Both studies found no significant difference between groups. One study has missing data i Both studies found no significant difference between groups. One study has missing data j Not possible to fully assess precision due to missing data for one of the studies. One of the studies uses median values. k One measure for this outcome was not fully reported, and author told us upon contact that this was because the difference between groups was not significant. l Both studies with 3 of 6 domains high risk m One study looks only at median values. Other study had very small sample size and did not carry out any analysis of data. n Two studies, one with 3 of 6 domains high risk, another with 4 of 6. o A mix of general measures (use of Internet, costs, resources) and setting specific measures. p One measure uses median values, other measures do not present confidence intervals, data are partly missing for two measures. q Three measures for this outcome were not fully reported, and author told us upon contact that this was because the difference between groups was not significant. r One study has 1 of 6 domains high risk, two have 4 of 6 domains s Evidence is inconclusive,each study has contradictory results for different measures under this outcome t One measure looked at use of complementary therapy. Three measures set in heart failure clinic with heart failure patients. But all measures general in relation to resource use. u For one measure data are missing and authors say this is because the difference between groups was not significant. Two measures look at the same thing over two different time points, no justification given for splitting the time period (first 6 months, second 6 months of intervention) and data are not presented for the study period overall. This could be construed as selective reporting.
Summary of findings 2. Summary of findings: Email as additional communication method compared to standard methods: Healthcare professional participants.
| Email as additional method of communication compared to standard methods of communication | |||
| Patient or population: Physicians Settings: Primary care clinics Intervention: Email communication1 | |||
| Outcomes | No of Participants (studies) | Quality of the evidence (GRADE) | Impact |
| Patient related outcomes | 0 (0) | See impact | NOT MEASURED |
| Health service outcome; resource use | 230 (2 studies) | ⊕⊝⊝⊝ very low2,3 | It is unclear to what extent email impacts on resource use when compared with standard methods of communication, with studies reporting variable results or having missing data, though results indicate that an email intervention leads to an increased number of emails and telephone calls being received by healthcare professionals as compared to standard methods of communication. |
| Health professional outcome | 0 (0) | See impact | NOT MEASURED |
| Harms | 0 (0) | See impact | NOT MEASURED |
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
1 Secure email interface, secure web based tool 2 Both studies have 3 of 6 domains at high risk of bias, and one domain unclear. 3 Evidence within studies is inconclusive; each study has contradictory results for different measures under the same outcome; some measures are significantly different, others not.
Summary of findings 3. Summary of findings: Email counselling compared with telephone counselling.
| Email counselling compared with telephone counselling | |||
| Patient or population: Adults (25‐60 years) Settings: Independent research clinic Intervention: Email counselling Comparison: Telephone counselling | |||
| Outcomes | No of Participants (studies) | Quality of the evidence (GRADE) | Impact |
| Patient health status and wellbeing | 105 (1 study) | ⊕⊝⊝⊝ very low1,2,3,4,5 | Telephone counselling leads to greater change than email counselling for some, but not all, measures of patient health status and wellbeing. There was no difference between groups for the majority of measures. |
| Patient behaviours and actions | 105 (1 study) | ⊕⊝⊝⊝ very low6,7 | Telephone counselling leads to greater change than email counselling for some, but not all, measures of patient behaviours and actions. There was no difference between groups for the majority of measures. |
| Health service outcomes | 0 (0) | See impact | NOT MEASURED |
| Health professional outcomes | 0 (0) | See impact | NOT MEASURED |
| Harms | 105 (1 study) |
⊕⊝⊝⊝ very low6,7 | There is no difference in harms between the email and telephone counselling groups. |
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
1 For this study 4 of 6 domains have high risk of bias. 2 One study with twelve different measures from the same study for this outcome. No comparison data, but 9 measures in favour of telephone and 3 in favour of email. Two post hoc measures favoured the telephone. 3 Population is patients meeting very specific criteria for obesity and drug intake. Setting is research clinic, which is not very applicable in the real world sense intended by this review. 4 Only one study. Confidence intervals visibly wide for three measures. 5 Two measures presented that were from a post hoc analysis. 6 For this study 4 of 6 domains with high risk of bias. 7 Population is patients meeting very specific criteria for obesity and drug intake. Setting is research clinic, which is not very applicable in the real world sense intended by this review.
Background
Related systematic reviews
This review forms part of a suite of reviews, incorporating four other reviews:
email for the provision of information on disease prevention and health promotion (Sawmynaden 2012);
email for communicating results of diagnostic medical investigations to patients (Meyer 2012);
email for the clinical communication between healthcare professionals (Pappas 2012); and
email for the coordination of healthcare appointments and attendance reminders (Atherton 2012).
The use of email
Email is easy to use, widely available across the world, and inexpensive. It is used in many areas of life, such as banking, travel and retail. Despite the ubiquity of email in day‐to‐day life and in other sectors of the economy, its use in the healthcare sector is still not routine (Neville 2004; Dixon 2010) though is on the increase. Factors driving the trend of increasing email use include the natural demographic shift towards an increasing proportion of people comfortable with using technology‐driven care solutions, and increasing demands on healthcare resources(OECD 2006).
In 1998 a survey of American physicians showed that less than seven per cent had used email to contact their patients (Lacher 2000); however more recent surveys show this to be increasing. US surveys have revealed that the increase in use is variable, from 16% of physicians using email in a survey of primary care practitioners to as many as 72% in a large outpatients' department (Gaster 2003; Brooks 2006). Uptake may vary according to patient group. The majority (79%) of doctors at a student health centre in Finland reported email use with patients (Castren 2005).
Nonetheless, the volume of email communication remains low, with surveys reporting averages from 7.7 emails per month to 8.6 emails per week in the aforementioned Finnish student healthcare centre (Gaster 2003; Castren 2005). Email communication was used for requesting prescriptions, booking appointments and for clinical consultation. It was commonly noted that email was used for non‐urgent communication only (Gaster 2003; Brooks 2006).
Several factors are likely to continue to drive the trend of increasing email use, including increasing patient demand, (Couchman 2001; Kleiner 2002; Moyer 2002),Harris 2006a natural demographic shift toward an increasing proportion of doctors (and patients) comfortable with using technology‐driven care solutions, and increasing per capita demand on healthcare resources (OECD 2006).
Email for clinical communication between patients and healthcare professionals
Email for clinical communication between patients and healthcare professionals can take several forms. Email consultations can be used instead of telephone consultations for simple and non‐urgent conditions (Car 2004b) such as urinary tract infections or back pain (Kassirer 2000). This may help to address unmet need for some patients in primary care, who may not otherwise be able to contact their practitioner easily (Katz 2003; White 2004). Healthcare professionals as well as patients have been shown to prefer email over telephone consultations for non‐urgent problems (Liederman 2003). This may act as a complementary method of communication, rather than wholly replacing face‐to‐face consultations.
Qualitative evidence has shown that healthcare professionals who use email for patient consultations think it is a useful addition to conventional methods of consultation, being easy to use and improving communication. Email may also enhance management of chronic diseases, improve continuity of care and increase healthcare professionals' flexibility in responding to non‐urgent issues (Liederman 2003; Patt 2003).
Email consultations are not appropriate for every circumstance, such as urgent communications and queries about symptoms like or chest pain that could indicate an emergency situation (Car 2004a), and for controversial topics such as illicit drug use (Dunbar 2003; Katz 2003). In some cases patients may provide incomplete, abstract or inappropriate information via email, requiring professionals to use a different method of communication such as telephone or face‐to‐face consultation for clarification (Patt 2003). Car 2004b There is recognition that the acceptability and potential of email communication will vary from patient to patient (Kassirer 2000).
The use of a standard protocol for email communication by both healthcare professional and patient might address these circumstances. This may include the types of communication permitted via email, such as administrative issues or specific clinical conditions. The patient could be advised not to email their healthcare provider regarding urgent conditions (Car 2004b).
Triage
Possible systems for implementation include triage‐based systems for messages about health concerns, prescription renewals and referrals, all controlled by a nurse 'navigator' (Katz 2003).
Sensitive issues
Email communication, by removing the face‐to‐face element of an 'in person' consultation, may encourage patients to raise sensitive or embarrassing issues that they may not otherwise discuss, thus addressing an unmet need. Caregivers have been documented as raising on behalf of the patient an issue that they have been reluctant to discuss with the healthcare professional (Patt 2003). Awareness of such an issue may provide a lead in to their discussion in any future consultation.
Chronic diseases
Email consultation allows ongoing and close monitoring and support of patients with chronic diseases (Kleiner 2002). Patients may also be able to communicate health data such as blood pressure levels or glucose levels to their healthcare professional for monitoring (Katz 2004). This type of service can improve continuity of care (Balas 1997), reduce the number of face‐to‐face consultations required, and improve quality of care and quality of life (Perlemuter 2002).
Follow up
Email can be used for communicating reminders to encourage adherence to treatment, and to solicit responses about side effects of medication. Dunbar 2003 reports high satisfaction and improved medication adherence with such systems. Email can also be used for follow up, for instance after an appointment with a physician (Katz 2003), when clarification or added information may be required (Patt 2003). Email can be used before an appointment, for ongoing health updates from patient to physician (White 2004), and to replace outpatient appointments after day surgery(Wedderburn 1996; Ellis 1999).
Advantages and disadvantages
The key advantages of email for clinical communication between patients and healthcare professionals include the following (adapted from Freed 2003; Car 2004a):
Timely and low cost delivery of information (relative to conventional mail) (Houston 2003)
Convenience: emails can be sent and subsequently read at an opportune time, outside of traditional office hours where convenient (Leong 2005).
'Read receipts' can be used to confirm that communications have been received.
Relative to oral communication, the written nature of the communication can be of value as reference for the patient, aiding recall and providing evidence of the exchange (Car 2004a; Car 2004b).
Email addresses usually stay constant when an address or telephone number changes (Virji 2006) making this a reliable way of maintaining communication with transient patients.
Email may improve access for non‐urgent and simple enquiries (Kassirer 2000, Katz 2003).
Emails can be archived in online or offline folders separate from the inbox of the email account so that they do not use up space in the inbox but can be kept for reference (Car 2004a; Car 2004b).
Patients may perceive email as a more intimate and considered form of communication than using the telephone (Katz 2003).
Email is an easier communication method for patients with disabilities, and with patients who are temporarily overseas e.g. seconded employees (Goodyear‐Smith 2005).
There are also potential downsides, including the following.
There is evidence of patient and physician concerns about privacy, confidentiality and potential misuse of information (Fridsma 1994; Harris 2006; Kleiner 2002; Moyer 2002; Katzen 2005).
Physicians may be wary of the potential for email to generate an increased workload (Mandl 1998; Pondichetty 2004).
Patients may expect a quick response, often within 48 hours, which may be problematic for healthcare professionals (Couchman 2001; Sittig 2001; Liederman 2003).
Email as a communication tool provides a different context for interaction. Face‐to‐face communication and telephone calls contain many layers of communication that are lost in an email; such as the emotive cues from vocal intonation or body language (Car 2004a). This may lead to misunderstandings.
The possible misuse of email for urgent clinical matters (Couchman 2001).
Recovery of implementation and other associated costs (especially in fee‐for‐service healthcare systems) (Mandl 1998).
Medico‐legal issues (including informed consent and use of non‐encrypted email) (Bitter 2000).
The potential to widen health inequalities via the digital divide (Kleiner 2002; Katz 2003; Goodyear‐Smith 2005; Virji 2006).
Technological issues may occur, such as recipients having a full mailbox causing email to bounce back to the sender (Virji 2006).
Systems may be at risk of failure, for instance a loss of the link to a central server (a computer which provides services used by other computers, such as email) (Car 2008a).
Potential for human error which can lead to unintended content or incorrect recipients.
Quality and safety issues
The main quality and safety issues around email consultation, as demonstrated in the previous section; advantages and disadvantages, are: privacy and confidentiality; potential for errors and ensuing liability; identifying clinical situations where email consultation is inefficient or inappropriate; securing payment; incorporating email into existing work patterns; and achievable costs (Moyer 1999; Kleiner 2002; Gaster 2003; Gordon 2003; Hobbs 2003, Houston 2003; Car 2004b).
Web messaging systems can address issues around security and liability that are associated with conventional email communication since they offer encryption capability and access controls (Liederman 2003). Such systems allow the structuring of communication; for example, messages can be triaged to the correct members of staff (Moyer 2002). However not all healthcare institutions are capable of providing such a facility and instead rely on standardised mail (Car 2004b).
Suggestions for minimising the legal risks of using email in practice include: adherence to the same strict data protection rules that must be followed in business and industry; adequate infrastructure to provide encrypted secure email transit and storage; and informed consent by the patient (Car 2004b). Additionally healthcare professionals may wish to exercise discretion about the patient's capability to use email communication. There may be patients who should be advised not to use this method of communication, and this should be at the discretion of the healthcare professional (Medem 2007).
Patient opinion of such systems is also important. Issues facing service users have included questionable reliability, timeliness and the impersonal nature of email (Katz 2003). However high patient satisfaction has been found in trials of email consultation, with patients preferring this method to telephone consultations and finding it easy to use (Liederman 2003). A content analysis of email communication between patients and healthcare professionals in the US found that only 1.8% of emails analysed were complaints, and these concerned timeliness and difficulties contacting the clinic via telephone (White 2004). The same content analysis found that patients adhered to guidelines for the use of email, avoiding urgent or sensitive requests and keeping emails formal and concise.
Education and training results in capable and competent end‐users of any technology. This can be costly and time consuming, but enhances the chance of effective implementation of such systems and thus should be a priority. A UK‐based survey showed that clinicians recently‐qualified feel more comfortable using the Internet and consider it reliable (Potts 2002). This is unsurprising given the relatively recent introduction of such technologies, and illustrates a potential generational effect on their use. This may influence training needs and the types of demographic groups leading the use of this technology. As well as the requirement for initial training, on‐going support is usually necessary to ensure continuing use and further development (Car 2008a).
Such issues are wide ranging and encompass both healthcare professional and patient perspective. All issues of quality and safety arising will be identified and addressed in the review.
Forms of electronic mail
In the absence of a standardised email communication infrastructure in the healthcare sector, email has been adopted in an ad‐hoc fashion and this has included the use of unsecured and secured email communication.
Standard unsecured email is email which is sent unencrypted. Secured email is encrypted; encryption transforms the text into an un‐interpretable format as it is transferred across the Internet. Encryption protects the confidentiality of the data, however both sender and recipient must have the appropriate software for encryption and decoding (TechWeb Network 2008).
Secure email also includes various specifically‐developed applications such as secure patient portals which utilise web messaging. Such portals provide pro‐formas into which patients can enter their message. The message is sent to the recipient as an email (TechWeb Network 2008). Secure websites are distributed by secure web servers. Web servers store and disseminate web pages. Secure servers ensure data from an Internet browser are encrypted before being uploaded to the relevant website. This makes it difficult for the data to be intercepted and deciphered (TechWeb Network 2008).
There are significant differences in terms of the applications. Bespoke secure email programmes may incorporate special features such as standard forms guiding the use and content of the email sent, ability to show read receipts (in order to confirm the patient has received the correspondence) and, if necessary, facilities for receiving payment (Liederman 2005). However they are costly to set up and may require a greater degree of skill on the part of the user than standard unsecured email (Katz 2004). For the purpose of the review we included all forms of email although secured versus unsecured email was to be considered in a subgroup analysis.
Methods of accessing email
Methods of accessing the Internet and thus an email account have changed with time. Traditionally access was via a personal computer or laptop at home or work, connecting to the Internet using a fixed line. There are now several methods of accessing the Internet. Wireless networks (known colloquially as wifi) allow Internet connection to a personal computer, laptop computer or other device wherever a network is available (TechWeb Network 2008). Internet connection is also possible via alternative networks using mobile devices. This includes access via mobile telephones to a wireless application protocol (WAP) network (rather than to the www) or to third generation (3G) network. Adaptors connecting to a universal serial bus (USB) port can be used to access the 3G network using a laptop computer (TechWeb Network 2008). Therefore email can be accessed away from the office or home in a variety of ways.
For the purposes of the review we included all methods of accessing email.
Objectives
To assess the effects of healthcare professionals and patients using email to communicate with each other; on patient outcomes, health service performance, service efficiency and acceptability, when compared to other forms of communicating clinical information.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs), quasi‐randomised trials, controlled before and after studies (CBAs) with at least two intervention and two control sites, and interrupted time series (ITS) with at least three time points before and after intervention.
Due to the practicalities of organisational change in a healthcare environment, most studies are not randomised and therefore we included quasi‐randomised trials and CBAs. The inclusion of ITS is particularly valuable in assessing the ongoing merits of a new technology which may require a 'settling in' period. We included trials with individual and cluster randomisation, and relevant trials with economic evaluations.
Types of participants
We included all healthcare professionals, patients and caregivers regardless of age, gender and ethnicity. We included studies in all settings i.e. primary care settings (services of primary health care), outpatient settings (outpatient clinics), community settings (public health settings) and hospital settings. We did not exclude studies according to the type of healthcare professional (e.g. surgeon, nurse, doctor, allied staff).
We considered participants originating the email communication, receiving the email communication and copied into the email communication.
Types of interventions
We included studies in which email was used for two‐way clinical communication between patients/caregivers and healthcare professionals. We included interventions that use email to allow patients to communicate clinical concerns to a healthcare professional and receive a reply.
We included interventions that used email in any of the following three forms:
Unsecured standard email to/from a standard email account.
Secure email which is encrypted in transit and sent to/from a standard email account with the appropriate encryption decoding software.
Web messaging; whereby the message is entered into a pro‐forma which is sent to a specific email account, the address of which is not available to the sender.
We included all methods of accessing email, including broadband via a fixed line, broadband via a wireless connection, and connecting to the 3G network and the WAP network.
We excluded studies which considered the general use of email for healthcare professional‐patient contact for multiple purposes but did not separately consider clinical communication between patients/caregivers and healthcare professionals. We included studies in which email was one part of a multifaceted intervention, if the effects of the email component were individually reported, even if they did not represent the primary outcome. However these were only included where they achieved the appropriate statistical power. Where this could not be determined or where it was not possible to separate the effects of the multifaceted intervention, they were not included.
We considered comparisons between outcomes of email communication and no intervention, as well as other modes of communication such as face‐to‐face, postal letters, calls to a landline or mobile telephone, text messaging using a mobile telephone, and automated versus personal emails.
Types of outcome measures
Primary outcomes of interest were whether the email was understood and acted upon correctly by the recipient as intended by the sender, and secondary outcomes were whether email was an appropriate mode for the communication exchange.
Primary outcomes
Healthcare professional outcomes resulting from whether the email was understood and acted upon correctly by the recipient as intended by the sender (where this impacts on the healthcare professional), e.g. professional knowledge and understanding, professional preferences or views, and behaviour, action or performance.
Patient outcomes associated with whether email has been understood and acted upon correctly by the recipient as intended by the sender, e.g. patient's understanding, patient health status and well‐being, patient views and patient behaviours or actions (such as adherence to treatment advice).
Health service outcomes associated with whether email has been understood and acted upon correctly by the recipient as intended by the sender, e.g. rates of treatment adherence.
Harms e.g. effects on safety or quality of care such as missed diagnoses, breaches in privacy, technology failures.
Secondary outcomes
Professional, patient or caregiver outcomes associated with whether email was an appropriate mode for the communication exchange, e.g. knowledge and understanding, effects on professional‐patient or professional‐caregiver communication or relationship, evaluations of care (convenience, timeliness, acceptability, satisfaction).
Health service outcomes associated with whether email was an appropriate mode for the communication exchange, e.g. use of resources or time, costs, use of medical services, referrals, admissions.
Search methods for identification of studies
Electronic searches
We searched:
Cochrane Consumers and Communication Review Group Specialised Register (searched 8 January 2010)
Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 1 2010)
MEDLINE (OvidSP) (1950 to 5 January 2010)
EMBASE (OvidSP) (1980 to 7 January 2010)
PsycINFO (OvidSP) (1967 to 5 January 2010)
CINAHL (EbscoHOST) (1982 to 2 February 2010)
ERIC (CSA) (1965 to 7 January 2010)
We present detailed search strategies in Appendices 1 to 5. John Kis‐Rigo, Trials Search Coordinator for the Cochrane Consumers and Communication Group compiled the strategies.
There were no language or date restrictions.
Searching other resources
Grey literature
We searched:
Australasian Digital Theses Program (http://adt.caul.edu.au/) (searched July 2010)
Networked Digital Library of Theses and Dissertations (http://www.ndltd.org) (searched July 2010)
UMI ProQuest Digital Dissertations (http://wwwlib.umi.com/dissertations/) (searched July 2010)
Index to Theses (http://www.theses.com/) (Great Britain and Ireland) (searched July 2010)
Clinical trials register (Clinicaltrials.gov) (searched July 2010)
WHO Clinical Trial Search Portal (www.who.int/trialsearch) (searched July 2010)
Current Controlled Trials (www.controlled‐trials.com) (searched July 2010)
Google Scholar (http://scholar.google.co.uk/) (we examined the first 500 hits) (searched July 2010)
We searched online trials registers for ongoing and recently completed studies and contacted authors where relevant. We kept detailed records of all the search strategies applied.
Reference lists
We also examined the reference lists of retrieved relevant studies.
Correspondence
We contacted the authors of included studies for advice as to any further studies or unpublished data that they were aware of. Many of the authors of included studies were also experts in the field.
Data collection and analysis
Selection of studies
Two review authors (HA and PS) independently assessed the potential relevance of all titles and abstracts identified from electronic searches. We retrieved full text copies of all articles judged to be potentially relevant. Both HA and PS independently assessed these retrieved articles for inclusion. Where HA and PS could not reach consensus a third author, JC, examined these articles.
During a meeting of all review authors, we verified the final list of included and excluded studies. Any disagreements about particular studies were resolved by discussion. Where the description of a study was insufficiently detailed to allow us to judge whether it met the review's inclusion criteria, we contacted the study authors seeking more detailed information to allow a final judgement regarding inclusion or exclusion. We retain detailed records of these communications.
Data extraction and management
We extracted data from all included studies using a standard form derived from the data extraction template provided by the Cochrane Consumers and Communication Review Group. We extracted the following data:
General information: Title, authors, source, publication status, date published, language, review author information, date reviewed.
Details of study: Aim of intervention and study, study design, location and details of setting, methods of recruitment of participants, inclusion/exclusion criteria, ethical approval and informed consent, consumer involvement.
Assessment of study quality: Key features of allocation, contemporaneous data collection for intervention and control groups; and for interrupted time series, number of data points collected before and after the intervention, follow‐up of participants.
Risk of bias: data to be extracted was dependent on study design (see Assessment of risk of bias in included studies).
Participants: Description, geographical location, setting, number screened, number randomised, number completing the study, age, gender, ethnicity, socio‐economic grouping and other baseline characteristics, health problem, diagnosis, treatment.
Health service: description, geographical location, setting, age, gender, population served, medical setting and clinical context of patients.
Intervention: Description of the intervention and control including rationale for intervention versus the control (usual care). Delivery of the intervention including email type (standard unsecured email, secure email, web portal or hybrid). Type of clinical information communicated. Content of communication (e.g. text, image). Purpose of communication (e.g. obtaining information, providing information). Communication protocols in place. Who delivers the intervention (e.g. healthcare professional, administrative staff). How consumers of interventions are identified. Sender of first communication (health service, professional, patient and/or caregiver). Recipients of first communication (health service, professional, patient and/or caregiver). Whether communication is responded to (content, frequency, method of media). Any co‐interventions included. Duration of intervention. Quality of intervention. Follow up period and rationale for chosen period.
Outcomes: principal and secondary outcomes, methods for measuring outcomes, methods of follow‐up, tools used to measure outcomes, whether the outcome is validated.
Results: for outcomes and timing of outcome assessment, control and intervention groups where applicable.
HA and PS piloted the data extraction template. For every included study both HA and PS independently performed the data extraction. Any discrepancies between the review authors' data extraction sheets were discussed and resolved by HA and PS. Where necessary, we involved JC to resolve discrepancies.
Assessment of risk of bias in included studies
Two review authors, HA and PS, independently assessed the risk of bias of included studies, with any disagreements resolved by discussion and consensus, and by consulting a third author, JC, where necessary.
We assessed and reported on the following elements that contribute to bias, according to the guidelines outlined in Higgins 2008:
Sequence generation;
Allocation concealment;
Blinding (outcomes assessors);
Intention‐to‐treat analysis;
Incomplete outcome data;
Selective outcome reporting.
We assigned a judgement relating to the risk of bias for each item. We used a template to guide the assessment of risk of bias, based upon Higgins 2008, judging each item as low, unclear or high risk of bias. We summarised risk of bias for each outcome where this differed within studies.
We also assessed a range of other possible sources of bias and indicators of study quality, in accordance with the guidelines of the Cochrane Consumers and Communication Review Group (Ryan 2007), including:
Baseline comparability of groups;
Validation of outcome assessment tools;
Reliability of outcome measures;
Other possible sources of bias
We present the results of the risk of bias assessment in tables and have incorporated the results of the assessment into the review through systematic narrative description and commentary about each of the risk of bias items. This led to an overall assessment of the risk of bias across the included studies and a judgement about the possible effects of bias on the effect sizes of the included studies.
We contacted study authors (where possible) for additional information about the included studies, or for clarification of the study methods as required.
For the cluster randomised trials we used chapter 16, section 16.3.2 of Higgins 2008 to aid assessment of risk of bias.
Measures of treatment effect
For dichotomous data, where data were available, we report the odds ratio/rate ratio and confidence intervals. For continuous data, where data were available, we report the mean difference and confidence intervals. For outcomes where data were missing, where possible we calculated standard error from confidence intervals, or P values where these were available. The standard error value was calculated presuming that a Z test had been used in the study in question, unless authors stated that a t test had been used. We could then calculate a mean difference using generic inverse variance.
Where confidence intervals or a P value were not available, it was not possible to calculate standard error values and so we have reported the mean values for the intervention versus control group and total number of participants in each group, in 'other data' tables. Where data were available only as median values, we present them as such.
Unit of analysis issues
We included two cluster randomised trials in the review (Katz 2003; Katz 2004). These were identified as cluster randomised trials after contact with the authors revealed a cluster method of randomisation had been used, but the trial was presented as a parallel group trial with some variables controlled for 'physician clinic.' It is possible to correct for data that have been analysed as though individual randomisation has taken place, but we were unable to do this because the required data were not available to us, either in the report or via the authors (see Appendix 2 for list of required information). Therefore any outcome data presented for these studies must be viewed in light of the potential unit of analysis errors. As the unit of analysis is different from the unit of allocation, any resulting P values are artificially small, which can result in false positive conclusions that the intervention had an effect (Higgins 2008). This does not bias the estimate of effect, but was considered in presenting the results of the review.
Dealing with missing data
Where data were not available with which to calculate an effect estimate, we contacted authors of the studies to obtain relevant information.
Data synthesis
In a meeting of three of the review authors (HA, PS, JC) the included studies were assessed and it was decided that it was not possible to combine the data in a meta‐analysis. Most outcomes were represented by only one study, and there were unobtainable missing data which meant that effect estimates could not always be calculated. The methods that we would have applied had data analysis and pooling been possible are outlined in Appendix 2 and will be applied to future updates of the review. Instead, we provide a summary of the overall findings for each outcome group at Effects of interventions.
We also applied the GRADE approach to assessing the quality of outcomes, and produced three Summary of findings Tables to outline the overall result for each individual outcome. In order to rate each outcome according to quality, two authors (HA and PS) each independently rated the outcomes according to the five factors, using guidance from the Cochrane Handbook of Systematic Reviews and the GRADE working group (Higgins 2008; GRADE 2010). Where ratings differed these were discussed until consensus was reached. Where consensus could not be reached a third author, JC, was consulted. We entered the finalised ratings into the GRADEpro software.
A typical Summary of Findings table produced in GRADEpro software contains a list of all important outcomes (usually primary outcomes per the review), a measure of the typical burden of these outcomes, the absolute and relative magnitude of effect (either/or), the number of participants and studies addressing these outcomes and a grade score for the overall quality of evidence for each outcome (rather than by study). For the purposes of this review we adapted the tables to account for the lack of data pooling. Although there was a lack of numerical data the Summary of Findings table was still a useful tool in summarising the findings of the review for the reader, and allowing for the quality of the outcomes to be assessed using the GRADE quality of the evidence framework.
We designed the Summary of Findings tables to contain the following:
Each primary outcome (patient outcomes, health professional outcomes, health service outcomes and harms).
Corresponding number of participants and studies.
Quality of the evidence (GRADE score).
Impact (via brief narrative summary).
We used an impact statement for each outcome to summarise the evidence available in the absence of statistical pooling. This statement was based on the measures of effect as entered into the review. Where the outcome had not been measured by any study in the review we stated this in the Summary of Findings tables. (See Table 1; Table 2; Table 3).
Consumer input
We asked two consumers, a health services researcher (UK) and healthcare consultant (Saudi Arabia) to comment on the completed review before submitting the review for the peer‐review process, with a view to improving the applicability of the review to potential users. The review also received feedback from two consumer referees as part of the Cochrane Consumers and Communication Review Group's standard editorial process.
Results
Description of studies
Results of the search
As this review was one in a suite of five looking at varying uses of email in healthcare, we conducted a common search for all five reviews (Atherton 2012; Meyer 2012; Pappas 2012; Sawmynaden 2012). We allocated relevant articles to each review after assessing them in full text. Figure 1 shows the search and selection process.
1.
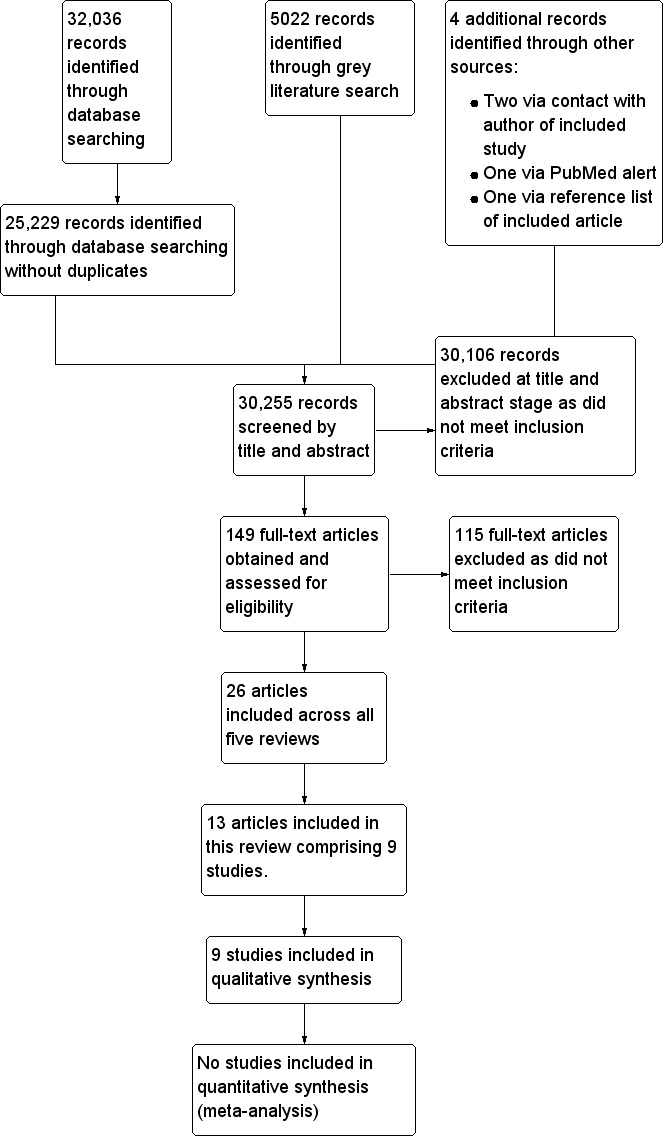
Flow diagram illustrating search results.
Included studies
We included nine studies enrolling 1733 participants (MacKinnon 1995; Katz 2003; Katz 2004; Kummervold 2004; Ross 2004; Lin 2005; Stalberg 2008; Bergmo 2009; Digenio 2009). These 9 studies were reported in 13 papers; Kummervold 2004 was reported in a thesis and 3 journal articles, and Katz 2003 was reported in an abstract and a journal article.
Design
All of the included studies were randomised controlled trials. However not all authors described their studies as such. Digenio 2009 describes the study as a "randomised 6 month open label study" because all participants were aware that they were receiving a weight loss drug. MacKinnon 1995 describes the study as a pretest‐post‐test control group design with random assignment. Stalberg 2008 described the study as a ‘prospective randomised controlled clinical trial’.
Two studies (Katz 2003; Katz 2004) were described and analysed by the authors as parallel group randomised controlled trials, but contact with one of the authors revealed that the method of randomisation used involved randomising individuals in groups to avoid contamination. For the purposes of the review we classified these two studies as cluster‐RCTs.
Sample sizes
Sample sizes ranged from n = 16 to n = 606 participants.Three studies used power calculations (Ross 2004; Lin 2005; Digenio 2009). Two used post‐hoc power calculations (Katz 2003; Katz 2004) and four did not use a power calculation (MacKinnon 1995; Kummervold 2004; Stalberg 2008; Bergmo 2009). Of the three studies using power calculations one was adequately powered (Digenio 2009).
Setting
All studies were conducted in high income countries, as follows:
| Country | Study |
| USA | 5 studies: Katz 2003; Katz 2004; Ross 2004; Lin 2005; Digenio 2009 |
| Norway | 2 studies: Kummervold 2004; Bergmo 2009 |
| Canada | MacKinnon 1995 |
| Australia | Stalberg 2008 |
Studies were conducted in a variety of healthcare settings across primary, secondary and tertiary care, and in the community.
Primary care
Three studies were set in primary care settings; Katz 2003 and Katz 2004 in primary care clinics affiliated with the University of Michigan and Kummervold 2004 in a group general practice with a city office and two district practices.
Secondary and tertiary care
Three studies were set in secondary care, specifically in outpatient settings. Bergmo 2009 was set in a paediatric and dermatology outpatient clinic in a secondary care hospital, Lin 2005 was set in an ambulatory internal medical practice affiliated with the University of Colorado Hospital. Ross 2004 was also set at the University of Colorado Hospital in a speciality outpatient clinic for heart failure. Stalberg 2008 was set in tertiary care, specifically a peri‐operative surgical setting for head and neck surgery at a tertiary referral centre.
Community and other care
MacKinnon 1995 was set in a rehabilitation centre providing an augmentative communication service for children/young adults with physical disability. Finally, Digenio 2009 was set in 12 research centres comprised mostly of non‐academic independent clinics. This setting was different to the others in that it was a research‐focused healthcare setting, rather than a conventional healthcare setting.
Participants
Participants were adults in all studies except MacKinnon 1995, in which participants were children and young adults with physical disabilities. These children and young adults (aged 7 to 25 years) were already clients of an augmentative communication service. They had a range of physical disabilities, though the majority suffered from cerebral palsy (12 of 16 participants). In Bergmo 2009 participants were the parents (caregivers) of the children attending the paediatric dermatology clinic and the intervention was aimed at the parent, although the outcomes assessed concerned both parents (parental behaviour) and children (child health status).
Five studies included adult patient participants. In Digenio 2009 participants had to be aged 25 to 60 years and have a body mass index of between 30 and 40. For Ross 2004 and Lin 2005 patients had to be at least 18 years old and English speaking. For Stalberg 2008 participants were those referred for thyroid or parathyroid surgery and aged 18 to 65. In Kummervold 2004 participants were patients at the general practice.
In the remaining two studies the adult participants were physicians; specifically a mixture of staff and resident physicians (Katz 2004), and faculty and resident physicians in primary care (Katz 2003).
Access to email
Some studies specified that participants should have a certain level of Internet or email access. Specifications included having access to the Internet and email (Digenio 2009), having access to the Internet and a personal cell phone (Kummervold 2004) and having both home and work access to the Internet (Stalberg 2008). In MacKinnon 1995 participants in the intervention group were provided with the equipment needed to use the email service because the use of the Internet and email was not widespread at that time. For two studies patients only had to have experience of using an Internet browser (Ross 2004, Lin 2005).
Interventions
Each study featured a different intervention.
Purpose and type
Five studies used some form of web‐messaging as their intervention (Katz 2004; Kummervold 2004; Ross 2004; Lin 2005; Bergmo 2009). In the remaining four studies the type of email was not specified, but in two of these studies (Stalberg 2008; Digenio 2009) it was presumed to be standard email because of the nature of the intervention described.
The intervention by Bergmo 2009 was a secure messaging system allowing parents of children to contact a dermatological specialist with a written description of the child’s condition along with the option to attach photos of the eczema area. Parents received a reply containing treatment advice. This was the only study to utilise images.
Three studies set in primary care examined interventions consisting of messages with general content (such as general enquiries, test results, and information). Katz 2004 trialled a secure web‐based patient‐provider tool, which allowed patients to communicate with clinic staff. Kummervold 2004 used a system called 'PatientLink', an electronic messaging system for sending unstructured messages between doctors and patients. Patients used a web browser to log in and send messages to the doctor. Katz 2003 trialled an intervention known as EMAIL (Electronic Messaging, Advice and Information Link). It is not clear what type of email is used in the EMAIL intervention other than it being described as an ‘email interface’ between patients and the health system, mediated by triage nurses.
Two studies featured multi‐faceted interventions and for the purposes of this review the outcomes relating to electronic messaging were of interest. 'My Doctor’s Office', a patient portal, was trialled by Lin 2005. This intervention allowed patients to request appointments, prescription refills and specialist referrals, and send secure electronic messages to their physicians. Clinical messages were sent directly to the physician, who could send an electronic response to the patient or forward the message with instructions to clinic nurses. Ross 2004 trialled SPPARO (System Providing Patients Access to Records Online). There were three components to SPPARO: access to the medical record, an educational guide and an electronic messaging system. The messaging system allowed patients to exchange secure messages with nursing staff in the speciality heart failure clinic.
Both MacKinnon 1995 and Stalberg 2008 asked patients in the intervention group to use email as their first line of contact with their health professional. In MacKinnon 1995 participants were asked to make all of their contacts to the augmentative communication service by email. The exact type of email is unknown because of the age of the study and subsequent changes in technology. In Stalberg 2008 participants were given an information sheet relating to their surgery with the surgeon’s email address as the top listed method of communication.
Digenio 2009 administered a lifestyle modification programme. Participants received weekly dietician contact via email during the first three months of the study and every other week during the following three months. This study also did not specify the type of email used, but it was presumed to be standard email.
Comparator
Email with usual care compared to usual care alone (standard methods of communication)
Eight studies compared the intervention as being additional to usual care for patients, usual care being the standard methods of communication offered in these settings (MacKinnon 1995; Katz 2003; Katz 2004; Kummervold 2004; Ross 2004; Lin 2005; Stalberg 2008; Bergmo 2009).
Email compared to telephone for delivery of counselling
Digenio 2009 was multi‐interventional with five arms. The group of interest was high frequency email counselling. Of the other four arms of the study (high frequency face to face counselling, low frequency face to face counselling, high frequency telephone counselling and lifestyle modification information with self care), high frequency telephone counselling was chosen as the comparator for the purpose of this review. Telephone is one of the specified comparators in this review, and in the context of the study provided the most appropriate comparison.
Communication protocol
Five studies had some sort of protocol around how the intervention should and would be used. This took the form of informal guidance and did not constitute a formal part of the trial. Four studies did not have any communication protocol at all according to the published reports (MacKinnon 1995; Ross 2004; Stalberg 2008; Digenio 2009).
Bergmo 2009 placed no restrictions on the number of messages each family could send during the 1‐year trial period and parents were informed that the specialist would respond within 24 hours or during the next working day. Katz 2003 asked patients to follow specific guidelines when emailing their physicians. The secure web site in Katz 2004 contained educational content addressing appropriate message content, expected response times and message handling by clinic staff.
Participants in Kummervold 2004 using the PasientLink system were free to decide the content, the length, the number of messages and the time of day that they wished to send messages, but they were told not to use it for acute problems. Participants in Lin 2005 using ‘My Doctor’s Office’ were warned in advance not to send urgent messages.
Outcomes
We outline details of the specific outcome measures in each study in the Characteristics of included studies table.
Patient/caregiver outcomes
Four studies reported primary patient outcomes. Three studies assessed both patient health and wellbeing and patient behaviour outcomes. Additionally Stalberg 2008 assessed patient understanding and patient views. MacKinnon 1995 assessed patient views. Three studies reported secondary patient outcomes, Lin 2005 and Stalberg 2008 reported the effect of email on patient‐professional communication, Kummervold 2004 and Stalberg 2008 reported evaluation of care and Kummervold 2004 also reported value of service.
Health professional outcomes
The only health professional outcome reported was a secondary outcome. Katz 2003 and Katz 2004 reported health professional perceptions.
Health service outcomes
Five studies reported primary health service outcomes. Kummervold 2004; Ross 2004 and Bergmo 2009 had patient participants and reported resource use outcomes. Katz 2003 and Katz 2004 had physician participants and also reported resource use outcomes. Three studies reported secondary health service outcomes and in all studies these were use of medical services outcomes (MacKinnon 1995; Lin 2005; Stalberg 2008).
Harms
One study reported data relating to harms (Digenio 2009). Three studies (MacKinnon 1995; Katz 2004; Lin 2005) did report some information on adverse events but this was not in the form of outcomes.
Missing data
Data were missing from all studies and we contacted all authors to try and obtain it. Four provided some or all additional data when requested (Kummervold 2004; Ross 2004; Lin 2005; Digenio 2009). Authors for five studies were unable to provide requested data (MacKinnon 1995; Katz 2003; Katz 2004; Stalberg 2008; Bergmo 2009).
Excluded studies
Of the 149 full text articles retrieved across the suite of five reviews, eleven of these were deemed potentially relevant to this review and subsequently excluded upon further inspection (see Characteristics of excluded studies table). Six of these studies were multi‐faceted interventions with an email component, in which the effects of email were not individually reported (Tate 2003; Carlbring 2006; Klein 2006; Hanauer 2009; Klein 2009b; Leveille 2009). Two studies looking at email for follow‐up featured two‐way communication where the patient response was administrative rather than for clinical communication (Ezenkwele 2003; Goldman 2004). One study compared two interventions with differing frequencies of email support and rather than assessing the effect of the email, assessed only frequency (Klein 2009a). Two studies had an inappropriate study design (Leong 2005, Pier 2008).
Risk of bias in included studies
All of the studies featured some bias. Figure 2 summarises the risk of bias for each included study and Figure 3 summarises the risk of bias for each domain. For three of the studies (MacKinnon 1995; Katz 2003; Katz 2004) there were unclear domains in the assessment of risk of bias; these remained unclear even after author contact.
2.
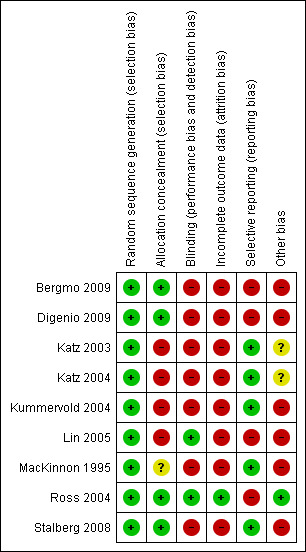
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.
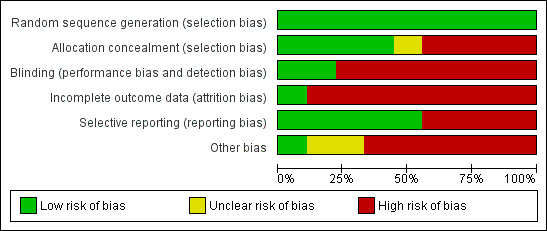
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
All of the included studies used adequate generation of allocation sequence. Just four studies reported adequate allocation concealment. (Ross 2004; Stalberg 2008; Bergmo 2009; Digenio 2009). MacKinnon 1995 did not provide information on allocation concealment and the author was unable to provide information when contacted. The remaining four studies reported inadequate allocation concealment.
Blinding
For many of the interventions in the review the blinding of participants (patients/caregivers, health professionals) was not feasible. Where participants were allocated to the intervention it was apparent, for instance that intervention participants had access to an email system, and control participants did not. Therefore for the purpose of this review we decided that the main focus in assessing of risk of bias related to blinding would be whether the investigators were blind to the allocation status of their participants.
Only two studies were adequately blinded (Ross 2004; Lin 2005). In Bergmo 2009 not all investigators were blinded. The dermatologist assessing the severity of eczema in participants was aware of group allocation. For all other outcomes investigators were blinded.
In the remaining studies investigators were not blind to participant allocation. Contact with the authors of MacKinnon 1995; Katz 2003; Katz 2004 and Digenio 2009 confirmed that investigators were not blinded. Kummervold 2004 state in one of the four publications associated with the study that blinding was not conducted in the project. In Stalberg 2008 investigators had routine access to the patient notes which contained the allocation data.
Incomplete outcome data
Only one study adequately addressed incomplete outcome data. Ross 2004 carried out a repeated measures analysis to account for missing participants across all relevant outcomes. The remaining studies featured some incomplete outcome data that was judged to introduce bias into the studies. This mostly concerned response rates to questionnaires, whereby non‐responders were not described or investigated. In Bergmo 2009 the response rate to the post‐intervention questionnaire was 74%, In Katz 2003 and Katz 2004 the response rates to the physician surveys were 91% and 71% respectively. In Kummervold 2004 the response rate to the patient survey was 93% in the intervention group and 73% in the control group, and for the willingness to pay element of the questionnaire the response rate was 68% for the intervention group and 84% for the control group. In Stalberg 2008 the response rate to the post‐operative feedback questionnaire, which addressed the patient satisfaction outcome, was 76% for the intervention group and 77% for the control group. Lin 2005 did investigate non‐responders, comparing overall satisfaction with care (as per the baseline survey) between participants who completed the study and those who did not (those participants lost to follow up along with those who did not complete final survey). Those not completing were less satisfied on the baseline survey, and this difference was significant. Therefore the least satisfied participants were not in the final analysis and this will have biased the final overall result.
The majority of studies did not carry out an intention‐to‐treat (ITT) analysis, or it was not clear if one had been carried out. MacKinnon 1995; Katz 2003; Katz 2004 did not carry out an ITT analysis. Despite stating that they would be carrying out a 'modified ITT,' in Digenio 2009 data are presented for the completers in the study only. In Stalberg 2008 an ITT analysis could not be completed for the patient satisfaction outcome as not all patients proceeded to surgery, and thus could not complete the post‐operative questionnaire. Bergmo 2009 provided insufficient information to assess whether an ITT analysis was carried out.
Other incidences of incomplete outcome data include Bergmo 2009 not stating how many participants were assessed for severity of eczema, and Katz 2003 and Katz 2004 imputing missing values to zero for the email volume outcome, stating that this was to account for incomplete data, but using zero meant that this served to enable analysis and did not account for the missing data. In MacKinnon 1995, for the outcome ‘number of independent contacts’ the method of contact was recorded for only 24 of 32 contacts. Upon contact the authors stated that this was because clinicians did not specify this information on the contact forms they were required to complete for the purposes of the study.
Selective reporting
Only one study had a published trial protocol (Digenio 2009).
Four studies were judged to have selective outcome reporting. In Bergmo 2009, the results for the primary outcomes are presented as mean values for the whole sample before the intervention versus the whole sample at the end of the intervention, rather than for the intervention and control groups independently. Selective reporting of data was confirmed during contact with the author. Digenio 2009 presents a post‐hoc analysis of two measures (proportions of participants achieving 5% and 10% weight loss) that was not pre‐specified. The study report also states that self‐reported data collected through the website would be descriptively summarised (collection of this descriptive data was not pre‐specified in the protocol) but for two measures (steps per day and calories per day) the data were not presented nor mentioned in the results section. Lin 2005 introduced an additional group to the study analysis: intervention non‐user. This group was compared to both the intervention and control groups. This addition was not pre‐specified. The content of messages was analysed according to two sub‐groups (clinical phone messages and clinical portal messages), and these groups constituted only around half of the originally randomised participants in each group. Therefore we were unable to use these data. 'Value to patient' data were presented for the whole sample and not by group, and the study author informed us that this was because they deemed this outcome as a peripheral part of the study. Whilst Ross 2004 addressed all outcomes in the results section this was sometimes in the form of a P‐value alone, with no other values presented. Categories of messages are presented graphically for the whole sample but not by group, despite the text stating that there were significant differences between the groups.
Other potential sources of bias
Six studies were assessed as having a high risk of other sources of bias. These included potential issues with the reliability of measures (MacKinnon 1995; Kummervold 2004; Stalberg 2008; Bergmo 2009; Digenio 2009), recall bias (Bergmo 2009) and participant bias (Lin 2005) amongst other sources (Characteristics of included studies).
In Digenio 2009 the study authors were all employees of a pharmaceutical company (Pfizer) that funded the research and this represents a conflict of interest in their conducting the research.
Effects of interventions
See: Table 1; Table 2; Table 3
We present data for primary outcomes for each comparison in turn, and then secondary outcomes. Table 1; Table 2; and Table 3 present a summary of the results of the primary outcome measures.
Email compared to standard methods of communication: primary outcomes
Healthcare professional outcomes
No primary healthcare professional outcomes were reported.
Patient/caregiver outcomes
Patient's understanding
It is not possible to adequately assess whether email has any effect on a patient's understanding when compared with standard methods of communication, due to missing data. Stalberg 2008 examined understanding of post‐operative instructions using a rating scale (1 to 7). A higher score indicated a more favourable outcome. Mean values were the same for email and standard groups (rating 6.1) but an effect estimate could not be calculated (Analysis 1.1).
1.1. Analysis.
Comparison 1 Email compared to standard methods of communication: Primary outcome, patient understanding:, Outcome 1 How did communication with the surgeon affect your understanding of postoperative instructions? (Scale 1‐7).
| How did communication with the surgeon affect your understanding of postoperative instructions? (Scale 1‐7) | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (Total) | Standard group (mean) | Standard group (total) |
| Stalberg 2008 | 6.1 | 37 | 6.1 | 37 |
Patient health status and wellbeing
It is not possible to adequately assess whether email has any effect on a patient's health status and wellbeing when compared with standard methods of communication, due to missing data. Stalberg 2008 examined anxiety level on the day of operation using a rating scale (1 to 7). They reported a 0.4 difference in mean values between email (rating 4.3) and standard method (rating 4.7) groups, but an effect estimate could not be calculated (Analysis 2.1). Bergmo 2009 examined severity of eczema. The authors described no significant interaction between email and standard method groups for severity of asthma but did not present any values. Study authors were unable to provide these data.
2.1. Analysis.
Comparison 2 Email compared to standard methods of communication: Primary outcome, patient health status and wellbeing, Outcome 1 How did communication with the surgeon affect your anxiety level on the day of the operation? (Scale 1‐7).
| How did communication with the surgeon affect your anxiety level on the day of the operation? (Scale 1‐7) | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| Stalberg 2008 | 4.3 | 37 | 4.7 | 37 |
Patient/caregiver views
It is not possible to adequately assess whether email had any effect on a patient/caregiver's views when compared with standard methods of communication, due to missing data. Stalberg 2008 examined whether ‘questions and concerns were addressed in a satisfactory manner,’ ‘how communication with the surgeon affected sense of preparedness for the operation’ and ‘how communication with the surgeon affected sense that the surgeon was available to deal with any problems that might arise using a rating scale (1 to 7). They reported little difference in mean values between email and standard groups for all three measures but an effect estimate could not be calculated. (Analysis 3.1; Analysis 3.2; Analysis 3.3). MacKinnon 1995 reported mean satisfaction ratings for ‘requests and questions dealt with in a timely manner’ and ‘problems dealt with adequately,’ using a rating scale (1 to 5). A higher score indicated a more favourable outcome. They reported little difference in mean values between email and standard groups however an effect estimate could not be calculated (Analysis 3.4; Analysis 3.5).
3.1. Analysis.
Comparison 3 Email compared to standard methods of communication: Primary outcome, patient/caregiver views, Outcome 1 How did communication with the surgeon affect your sense of preparedness for the operation (Scale 1‐7).
| How did communication with the surgeon affect your sense of preparedness for the operation (Scale 1‐7) | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| Stalberg 2008 | 6.2 | 37 | 6.4 | 37 |
3.2. Analysis.
Comparison 3 Email compared to standard methods of communication: Primary outcome, patient/caregiver views, Outcome 2 Questions and concerns addressed in a satisfactory manner? (Scale 1‐7).
| Questions and concerns addressed in a satisfactory manner? (Scale 1‐7) | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| Stalberg 2008 | 6.4 | 37 | 6.3 | 37 |
3.3. Analysis.
Comparison 3 Email compared to standard methods of communication: Primary outcome, patient/caregiver views, Outcome 3 How did communication with the surgeon affect your sense that the surgeon was available to deal with any problems that might arise? (Scale 1‐7).
| How did communication with the surgeon affect your sense that the surgeon was available to deal with any problems that might arise? (Scale 1‐7) | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| Stalberg 2008 | 6 | 37 | 6.4 | 37 |
3.4. Analysis.
Comparison 3 Email compared to standard methods of communication: Primary outcome, patient/caregiver views, Outcome 4 Requests and questions dealt with in a timely manner (satisfaction rating at 6 months) (Scale 1‐5).
| Requests and questions dealt with in a timely manner (satisfaction rating at 6 months) (Scale 1‐5) | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| MacKinnon 1995 | 4 | 7 | 3.3 | 9 |
3.5. Analysis.
Comparison 3 Email compared to standard methods of communication: Primary outcome, patient/caregiver views, Outcome 5 Problems dealt with adequately (satisfaction rating at 6 months) (Scale 1‐5).
| Problems dealt with adequately (satisfaction rating at 6 months) (Scale 1‐5) | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| MacKinnon 1995 | 4.3 | 7 | 3.3 | 9 |
Patient behaviours and actions
It is not possible to adequately assess whether email had any effect on patient behaviours and actions, though it is possible to report that email did not have any effect on a patient's use of the Internet. Stalberg 2008 examined whether patients used the Internet to find information about their disease (OR 1.13; 95% CI 0.42 to 3.04; Analysis 4.1) and whether they used it to find information about where to seek treatment (OR 0.65; 95% CI 0.10 to 4.12; Analysis 4.2). There was no significant difference between groups for either measure.
4.1. Analysis.
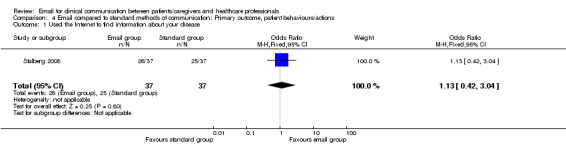
Comparison 4 Email compared to standard methods of communication: Primary outcome, patient behaviours/actions, Outcome 1 Used the Internet to find information about your disease.
4.2. Analysis.
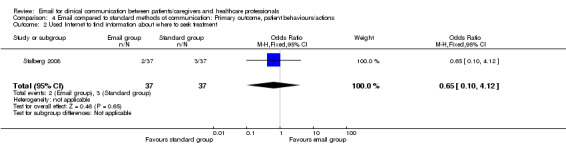
Comparison 4 Email compared to standard methods of communication: Primary outcome, patient behaviours/actions, Outcome 2 Used Internet to find information about where to seek treatment.
The authors also examined ‘ability to make appropriate work/family arrangements for your operation’ using a rating scale (1 to 7). The mean values were similar for email and standard groups but an effect estimate could not be calculated (Analysis 4.3). Bergmo 2009 examined: mean number of skin care treatments per week performed by parents; family costs; and loss of employment. The authors state that there is no significant interaction between email and standard method groups but do not present values. Authors were unable to provide these data.
4.3. Analysis.
Comparison 4 Email compared to standard methods of communication: Primary outcome, patient behaviours/actions, Outcome 3 How did communication with the surgeon affect your ability to make appropriate work/family arrangements for the operation (Scale 1‐7).
| How did communication with the surgeon affect your ability to make appropriate work/family arrangements for the operation (Scale 1‐7) | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| Stalberg 2008 | 6.3 | 37 | 5.9 | 37 |
Health service outcomes
Resource use
Patient participants
It is unclear to what extent email impacts on resource use by patients when compared with standard methods of communication, with studies reporting variable results or having missing data.
There was some indication that email impacted on resource use; Kummervold 2004 found that reduction in the mean number of contacts to the GP and front office was greater in the email group (MD ‐1.26; 95% CI ‐1.85 to ‐0.67; Analysis 5.1), and reduction was also greater in office visits per patient per year (MD ‐1.10; 95% CI ‐1.87 to ‐0.33; Analysis 5.2) and in telephone consultations (MD ‐0.80; 95% CI ‐1.37 to ‐0.23 (Analysis 5.3). However another study showed no difference between groups. Bergmo 2009 examined reduction in visits to a complementary therapist during the intervention period. There was no significant difference between email and standard groups for the reduction in visits (MD 0.71; 95% CI ‐0.10 to 1.52; Analysis 5.4). Bergmo 2009 also examined resource use, overall healthcare visits and hospital admissions. For resource use, they showed that there was no significant difference between groups but did not present values. For the other two outcomes data were only presented for the group as whole and authors were unable to provide missing data.
5.1. Analysis.
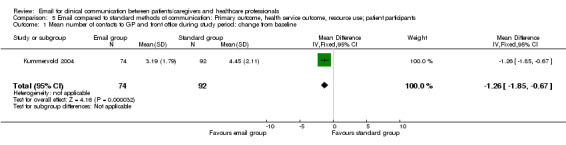
Comparison 5 Email compared to standard methods of communication: Primary outcome, health service outcome, resource use; patient participants, Outcome 1 Mean number of contacts to GP and front office during study period: change from baseline.
5.2. Analysis.
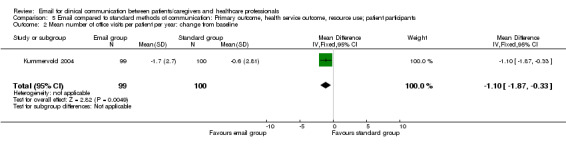
Comparison 5 Email compared to standard methods of communication: Primary outcome, health service outcome, resource use; patient participants, Outcome 2 Mean number of office visits per patient per year: change from baseline.
5.3. Analysis.
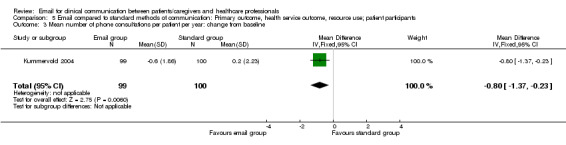
Comparison 5 Email compared to standard methods of communication: Primary outcome, health service outcome, resource use; patient participants, Outcome 3 Mean number of phone consultations per patient per year: change from baseline.
5.4. Analysis.
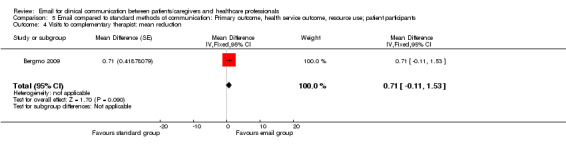
Comparison 5 Email compared to standard methods of communication: Primary outcome, health service outcome, resource use; patient participants, Outcome 4 Visits to complementary therapist: mean reduction.
Ross 2004 examined the number of messages sent to the practice during the year long intervention period. They reported a 1.5 message difference between groups (email group: 6.5, standard group: 5, Analysis 5.5) but an effect estimate could not be calculated.
5.5. Analysis.
Comparison 5 Email compared to standard methods of communication: Primary outcome, health service outcome, resource use; patient participants, Outcome 5 Number of messages sent to the practice (mean per patient).
| Number of messages sent to the practice (mean per patient) | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| Ross 2004 | 6.5 | 54 | 5 | 53 |
Healthcare professional participants
It is unclear to what extent email impacts on resource use when compared with standard methods of communication, as studies reported variable results or had missing data, though results indicate that an email intervention leads to an increased number of emails being received as compared to standard methods of communication.
Email rates
The two studies examining changes in email rates over the intervention period found that rates were increased for the email group over the standard group. Katz 2003 saw more of an increase in emails during the intervention period (rate ratio 3.60; 95% CI 2.10 to 6.19; Analysis 6.1). Katz 2004 reported higher email rates in the email group at the final intervention time point (email: 13.7, standard: 12.2; Analysis 6.2) but an effect estimate could not be calculated.
6.1. Analysis.
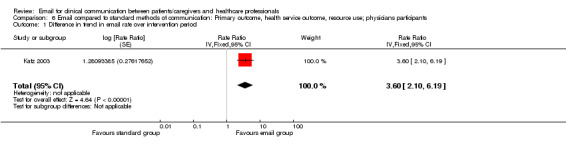
Comparison 6 Email compared to standard methods of communication: Primary outcome, health service outcome, resource use; physicians participants, Outcome 1 Difference in trend in email rate over intervention period.
6.2. Analysis.
Comparison 6 Email compared to standard methods of communication: Primary outcome, health service outcome, resource use; physicians participants, Outcome 2 Email rate (per 100 average weekly scheduled visits) for final intervention time period.
| Email rate (per 100 average weekly scheduled visits) for final intervention time period | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| Katz 2003 | 27 | 43 | 10.4 | 46 |
| Katz 2004 | 13.7 | 48 | 12.2 | 46 |
Telephone rates
Both studies also examined changes in phone rates over the intervention period and obtained conflicting results. Katz 2003 saw more of an increase in telephone calls during the intervention period for the email group over the standard methods group (rate ratio 1.20; 95% CI 0.96 to 1.50; Analysis 6.3). Katz 2004 reported higher phone call rates in the standard group at the final intervention time point (email: 63.7, standard: 70.6; Analysis 6.4) but an effect estimate could not be calculated. See also Analysis 6.5.
6.3. Analysis.
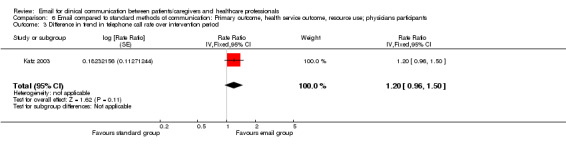
Comparison 6 Email compared to standard methods of communication: Primary outcome, health service outcome, resource use; physicians participants, Outcome 3 Difference in trend in telephone call rate over intervention period.
6.4. Analysis.
Comparison 6 Email compared to standard methods of communication: Primary outcome, health service outcome, resource use; physicians participants, Outcome 4 Telephone call rate (per 100 average weekly scheduled visits) for final intervention time period.
| Telephone call rate (per 100 average weekly scheduled visits) for final intervention time period | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Control group (mean) | Control group (total) |
| Katz 2003 | 75.2 | 43 | 70 | 46 |
| Katz 2004 | 63.7 | 48 | 70.6 | 46 |
6.5. Analysis.
Comparison 6 Email compared to standard methods of communication: Primary outcome, health service outcome, resource use; physicians participants, Outcome 5 Change in telephone call rate (per 100 average weekly scheduled visits) between intervention periods 1 & 5.
| Change in telephone call rate (per 100 average weekly scheduled visits) between intervention periods 1 & 5 | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| Katz 2004 | ‐7.5 | 48 | ‐9.9 | 46 |
'No‐show' rates
Katz 2003 also examined changes in no‐show rates (at appointments) over the intervention period and these were slightly higher for the email group (email: 12.2, standard: 11.5; Analysis 6.6; see also Analysis 6.7) but an effect estimate could not be calculated.
6.6. Analysis.
Comparison 6 Email compared to standard methods of communication: Primary outcome, health service outcome, resource use; physicians participants, Outcome 6 No‐show rate (per 100 average scheduled visits) for final intervention period.
| No‐show rate (per 100 average scheduled visits) for final intervention period | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| Katz 2003 | 12.2 | 43 | 11.5 | 46 |
6.7. Analysis.
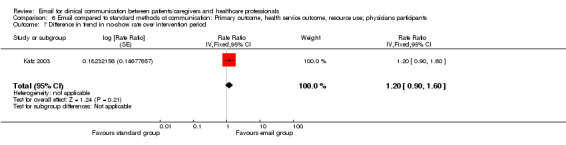
Comparison 6 Email compared to standard methods of communication: Primary outcome, health service outcome, resource use; physicians participants, Outcome 7 Difference in trend in no‐show rate over intervention period.
Volume of emails
Katz 2003 also examined the volume of weekly emails received by each group, comparing this by subgroup: resident physicians and faculty physicians. There were more emails received by those in the email group than the standard group for both resident physicians (MD 1.60; 95% CI 0.38 to 2.82; Analysis 6.8) and faculty physicians (MD 6.80; 95% CI 1.63 to 11.97; Analysis 6.9) See also Analysis 6.10.
6.8. Analysis.
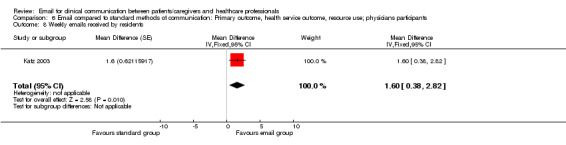
Comparison 6 Email compared to standard methods of communication: Primary outcome, health service outcome, resource use; physicians participants, Outcome 8 Weekly emails received by residents.
6.9. Analysis.
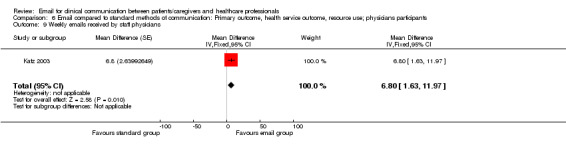
Comparison 6 Email compared to standard methods of communication: Primary outcome, health service outcome, resource use; physicians participants, Outcome 9 Weekly emails received by staff physicians.
6.10. Analysis.
Comparison 6 Email compared to standard methods of communication: Primary outcome, health service outcome, resource use; physicians participants, Outcome 10 Change in email rate (per 100 average weekly scheduled visits) between intervention periods 1 & 5.
| Change in email rate (per 100 average weekly scheduled visits) between intervention periods 1 & 5 | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| Katz 2003 | 18 | 43 | 4 | 46 |
| Katz 2004 | 2.2 | 48 | 2 | 46 |
Due to the unit of analysis errors occurring in both of these studies we must be aware of the risk of false positive conclusions (see Unit of analysis issues) where a significant difference between groups is reported.
Harms
For this comparison there were no outcomes relating to harms, however three studies reported some form of adverse event. Katz 2004 reported that many patients did not have sufficient web‐based experience to navigate the intervention website, though they did not measure this. Lin 2005 reported that two portal messages were deemed urgent but the receiving physicians did not consider these problematic. MacKinnon 1995 reported that one participant in the intervention group dropped out because of technical difficulties.
Email compared to telephone for delivery of counselling: primary outcomes
Only one study fell under this comparison, Digenio 2009, which compared the effect of telephone counselling with email counselling on various lifestyle modification related outcomes.
Patient outcomes
Patient health status and wellbeing
Telephone counselling has a greater effect than email counselling on some measures of patient health status and wellbeing. The study included fourteen measures of patient health status and wellbeing. Two of these showed a significant difference between groups, favouring the telephone counselling group. The percentage reduction in body weight from baseline was greater for the telephone counselling group (MD 1.80; 95% CI 1.75 to 1.85; Analysis 7.1) and percentage change in HDL cholesterol ('good cholesterol') was greater for the telephone counselling group (MD ‐5.90; 95% CI ‐11.55 to ‐0.25; Analysis 7.9). The other measures of patient health status and wellbeing reported in this study showed no difference between the email and telephone counselling groups (See Data and analyses 7).
7.1. Analysis.
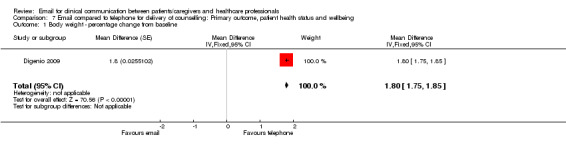
Comparison 7 Email compared to telephone for delivery of counselling: Primary outcome, patient health status and wellbeing, Outcome 1 Body weight ‐ percentage change from baseline.
7.9. Analysis.
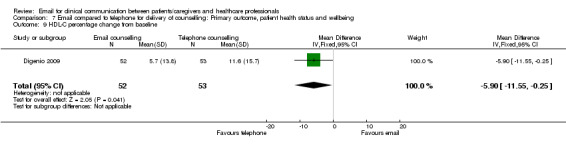
Comparison 7 Email compared to telephone for delivery of counselling: Primary outcome, patient health status and wellbeing, Outcome 9 HDL‐C percentage change from baseline.
Patient behaviours and actions
Telephone counselling has a greater effect than email counselling on some measures of patient behaviours and actions in Digenio 2009. The study included six measures of patient behaviours and actions and one of these showed a significant difference between groups, favouring the telephone counselling group. The mean number of logins to the website was greater for the telephone counselling group (MD ‐11.00; 95% CI ‐16.04 to ‐5.96; Analysis 8.5). There was no difference between telephone counselling and email counselling on the five other reported measures of patient behaviours and actions (Data and analyses 8).
8.5. Analysis.
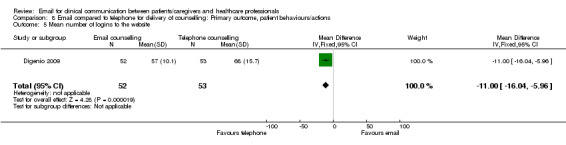
Comparison 8 Email compared to telephone for delivery of counselling: Primary outcome, patient behaviours/actions, Outcome 5 Mean number of logins to the website.
Harms
Digenio 2009 presented outcome data for discontinued participation due to adverse events and there was no significant difference in the numbers of participants discontinuing participation between the email and telephone counselling groups (OR 1.30; 95% CI 0.34 to 5.06; Analysis 9.1). However these events were attributed to the drug component of the study which participants in both groups received, rather than the communication element of the study.
9.1. Analysis.
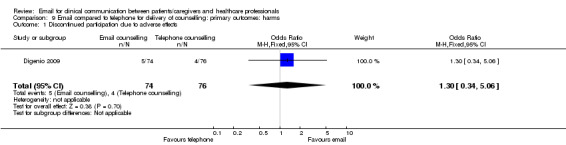
Comparison 9 Email compared to telephone for delivery of counselling: primary outcomes: harms, Outcome 1 Discontinued participation due to adverse effects.
Email compared to standard methods of communication: secondary outcomes
Healthcare professional outcomes
Healthcare professional perceptions (acceptability and satisfaction)
It is unclear what effect email has on healthcare professional perceptions when compared with standard methods of communication, as the two studies in this category reported variable results or had missing data, though results indicate that healthcare professional acceptability and satisfaction is higher for those physicians in the email group when compared to those in the standard group. Due to the unit of analysis errors occurring in both of these studies (Katz 2003; Katz 2004) we must be aware of the risk of false positive conclusions where significant results are obtained.
Nine measures of physician perception across these two studies, six measures by Katz 2003 and three measures by Katz 2004, showed significant differences between the email and standard methods group, with satisfaction and acceptability reported as significantly higher in the email group, and level of dissatisfaction being lower in the email group (see Data and analyses 10). There was just one measure for which no significant difference was found between groups ('email would be a good way for my patients to contact me'; proportion agreeing/strongly agreeing) and another measure where mean values reported were higher for the email group (web benefits scale mean score (email: 4, standard: 1.1; Analysis 10.7)), but it was not possible to calculate an effect estimate.
10.7. Analysis.
Comparison 10 Email compared to standard methods of communication: Secondary outcome, health professional perceptions, Outcome 7 Physicians' web benefits scale (perceived benefits of web communication with patients).
| Physicians' web benefits scale (perceived benefits of web communication with patients) | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| Katz 2004 | 4 | 48 | 1.1 | 46 |
Both studies examined attitudes towards general communication with patients, using a general communication scale, and physician satisfaction with patient communication outside of clinical visits. The data for these measures could not be pooled due to potential unit of analysis errors in the studies, however both studies found a mean difference of ‐0.30 between email and standard method groups for the general communication scale (Analysis 10.12), and the odds ratios for physician satisfaction with patient communication outside of clinical visits did not indicate any significant difference between groups in either study (OR 0.80; 95% CI 0.35 to 1.83) (Katz 2003) and (OR 0.78; 95% CI 0.34 to 1.76; Analysis 10.13) (Katz 2004).
10.12. Analysis.
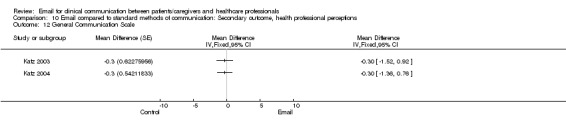
Comparison 10 Email compared to standard methods of communication: Secondary outcome, health professional perceptions, Outcome 12 General Communication Scale.
10.13. Analysis.
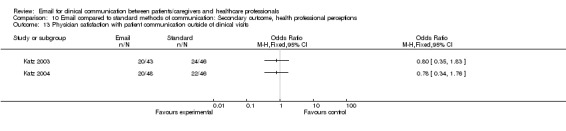
Comparison 10 Email compared to standard methods of communication: Secondary outcome, health professional perceptions, Outcome 13 Physician satisfaction with patient communication outside of clinical visits.
Katz 2003 also examined a further nine outcomes all related to physician perceptions of email use for which they reported only a P value. They found no significant difference between groups for any of these measures but did not present values. As it was not possible to obtain these data an effect estimate could not be calculated.
Patient outcomes
Effect on patient‐professional communication
It is unclear what effect email has on patient professional communication when compared with standard methods of communication, as studies reported variable results or had missing data, though results indicate that those in the email group reported more positive experiences.
Participant satisfaction with communicating non‐urgent messages to a doctor and/or nurse was rated excellent/very good by more people in the email than the standard group (OR 2.63; 95% CI 1.61 to 4.29; Analysis 11.1) but there was no difference between groups for those rating it as poor (OR 0.56; 95% CI 0.25 to 1.23; Analysis 11.2) (Lin 2005).
11.1. Analysis.
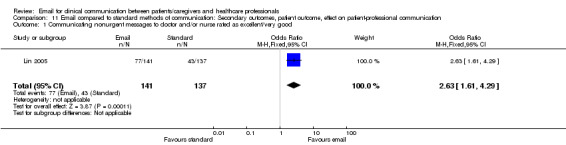
Comparison 11 Email compared to standard methods of communication: Secondary outcomes, patient outcome, effect on patient‐professional communication, Outcome 1 Communicating nonurgent messages to doctor and/or nurse rated as excellent/very good.
11.2. Analysis.
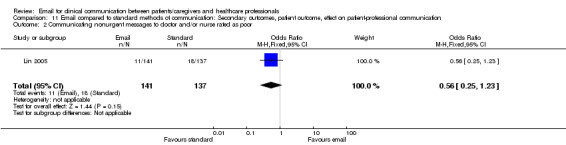
Comparison 11 Email compared to standard methods of communication: Secondary outcomes, patient outcome, effect on patient‐professional communication, Outcome 2 Communicating nonurgent messages to doctor and/or nurse rated as poor.
Stalberg 2008 examined three measures of patient‐professional communication: 'how effective was the communication with your surgeon prior to surgery?', 'how effective was the communication with your surgeon after surgery?' and 'overall, how effective was the communication with your surgeon?' They reported similar mean values for both groups, but an effect estimate could not be calculated (Analysis 11.3; Analysis 11.4; Analysis 11.5).
11.3. Analysis.
Comparison 11 Email compared to standard methods of communication: Secondary outcomes, patient outcome, effect on patient‐professional communication, Outcome 3 How effective was the communication with your surgeon prior to surgery? (Scale 1‐7).
| How effective was the communication with your surgeon prior to surgery? (Scale 1‐7) | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| Stalberg 2008 | 6.3 | 37 | 6 | 37 |
11.4. Analysis.
Comparison 11 Email compared to standard methods of communication: Secondary outcomes, patient outcome, effect on patient‐professional communication, Outcome 4 How effective was the communication with your surgeon after surgery? (Scale 1‐7).
| How effective was the communication with your surgeon after surgery? (Scale 1‐7) | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| Stalberg 2008 | 5.8 | 37 | 5.9 | 37 |
11.5. Analysis.
Comparison 11 Email compared to standard methods of communication: Secondary outcomes, patient outcome, effect on patient‐professional communication, Outcome 5 Overall, how effective was the communication with your surgeon? (Scale 1‐7).
| Overall, how effective was the communication with your surgeon? (Scale 1‐7) | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| Stalberg 2008 | 6.1 | 37 | 6.3 | 37 |
Evaluation of care
It was not possible to adequately assess what effect email has on patient evaluation of care. Stalberg 2008 examined ‘overall satisfaction with surgical experience.’ They reported a 0.2 difference in mean values between email (rating 6.4) and standard method (rating 6.6) groups on a scale of 1 to 7, but an effect estimate could not be calculated (Analysis 12.1).
12.1. Analysis.
Comparison 12 Email compared to standard methods of communication: Secondary outcome, patient outcome, evaluation of care, Outcome 1 Overall satisfaction with surgical experience? (Scale 1‐7).
| Overall satisfaction with surgical experience? (Scale 1‐7) | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| Stalberg 2008 | 6.4 | 37 | 6.6 | 37 |
Value of service
It appears that using email may impact on how patients perceive the value of a service. Kummervold 2004 assessed willingness to pay per online consultation, in euros. This measure is reported as median values and so an effect estimate could not be calculated. The email group, who actually received the online consultations, were willing to pay fewer euros per consultation than the standard group who had not received the intervention (Email group (median Euros) 4.39; Control group (median Euros): 6.28).The authors report a significant difference between groups (Analysis 13.1).
13.1. Analysis.
Comparison 13 Email compared to standard methods of communication: Secondary outcome, patient outcome, value of service, Outcome 1 Amount willing to pay per online consultation in euros (median and percentiles).
| Amount willing to pay per online consultation in euros (median and percentiles) | |||
|---|---|---|---|
| Study | Intervention (n=38) | Control (n=52) | Test for difference |
| Kummervold 2004 | 4.39 euros (1.26 to 6.28) | 6.28 euros (3.14 to 12.55) | P=0.028 |
Health service outcomes
Use of medical services (contact with healthcare professionals)
It is unclear whether email has any impact on the use of medical services when compared with standard methods of communication, as studies reported had variable results or had missing data, though results indicate that those in the email group reported more use of services.
Stalberg 2008 examined whether participants initiated any form of contact with their surgeon and found that those in the email group were more likely to initiate contact than those in the standard group (OR 3.76; 95% CI 1.41 to 10.05; Analysis 14.1). Lin 2005 carried out an analysis on a subgroup of participants: those consenting for their medical record to be viewed for the purposes of information collection. The authors reported the number of telephone messages sent per patient (MD ‐0.06; 95% CI ‐0.33 to 0.21; Analysis 14.2) and the total number of messages (telephone plus email) sent per patient (MD 0.19; 95% CI ‐0.15 to 0.53; Analysis 14.3). The email group sent more telephone messages per patient and more messages overall (telephone and portal messages), however the difference between groups was not significant.
14.1. Analysis.
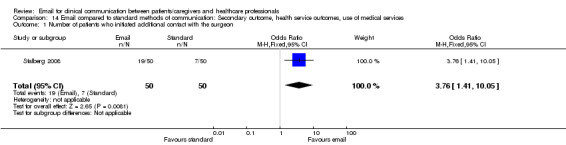
Comparison 14 Email compared to standard methods of communication: Secondary outcome, health service outcomes, use of medical services, Outcome 1 Number of patients who initiated additional contact with the surgeon.
14.2. Analysis.
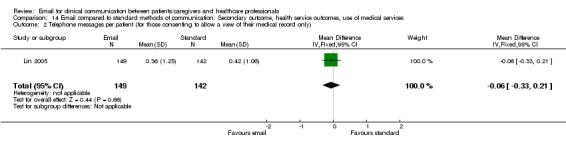
Comparison 14 Email compared to standard methods of communication: Secondary outcome, health service outcomes, use of medical services, Outcome 2 Telephone messages per patient (for those consenting to allow a view of their medical record only).
14.3. Analysis.
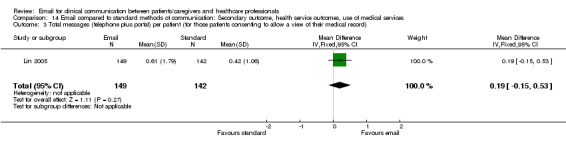
Comparison 14 Email compared to standard methods of communication: Secondary outcome, health service outcomes, use of medical services, Outcome 3 Total messages (telephone plus portal) per patient (for those patients consenting to allow a view of their medical record).
MacKinnon 1995 examined mean number of contacts, and of independent contacts, with the augmentative communication service. The mean number of contacts was higher in the email group (email: 6.4, standard: 1; Analysis 14.4) than in the standard group, and the same was true of independent contacts (email: 4.6, standard: 0.1; Analysis 14.5). However an effect estimate could not be calculated.
14.4. Analysis.
Comparison 14 Email compared to standard methods of communication: Secondary outcome, health service outcomes, use of medical services, Outcome 4 Number of contacts with the augmentative communication service.
| Number of contacts with the augmentative communication service | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| MacKinnon 1995 | 6.4 | 7 | 1 | 9 |
14.5. Analysis.
Comparison 14 Email compared to standard methods of communication: Secondary outcome, health service outcomes, use of medical services, Outcome 5 Number of independent contacts with the augmentative communication service.
| Number of independent contacts with the augmentative communication service | ||||
|---|---|---|---|---|
| Study | Email group (mean) | Email group (total) | Standard group (mean) | Standard group (total) |
| MacKinnon 1995 | 4.6 | 7 | 0.1 | 9 |
Discussion
Summary of main results
Based on the findings of this review, it is not possible to adequately assess the effect of email for clinical communication between patients/caregivers and healthcare professionals. The review identified relatively few studies and these are of low quality. The nature of the evidence base means that we are uncertain about the majority of primary and secondary outcomes.
For the comparison ‘email compared to standard methods of communication,’ for the majority of patient/caregiver outcomes it is not possible to adequately assess whether email has any effect, although for patient behaviours and actions it is possible to report that being in the email group did not have an effect on whether patients used the Internet for finding out about their disease, or whether they used it for finding information about were to seek treatment (Table 1).
The health service outcome (resource use) was split into those studies with patient participants and those studies with physician participants. For patient participants it was not possible to adequately assess whether email has any effect on resource use (Table 2). For physician participants it was unclear to what extent email impacted on resource use with studies reporting varied results or having missing data, although results indicated that an email intervention leads to an increased number of emails and telephone calls being received by healthcare professionals (Table 3).
Three studies reported some type of adverse event but it was not clear if the adverse event had any impact on the health of the patient or the quality of health care (MacKinnon 1995; Katz 2004; Lin 2005).
For the comparison ‘email counselling compared with telephone counselling’, studies only measured patient outcomes, and for most of the of measures there was no difference between groups. Where there were differences, these showed that telephone counselling leads to greater change than email counselling for lifestyle modification factors (Table 3). One outcome was identified relating to harms, but the harm in question (discontinued participation due to adverse events), was attributed to the drug component of the study, which was administered to all participants.
No primary healthcare professional outcomes were measured in any of the included studies falling under either comparison.
Secondary outcomes were all related to the comparison ‘email compared to standard methods of communication,’ and included healthcare professional, patient and health service outcomes. There were no secondary outcomes reported for the comparison of ‘email compared to telephone for delivery of counselling.’
For all secondary outcomes, it was unclear what effect email had, as studies reported variable results or had missing data. Despite this, for healthcare professional perceptions, results indicate that acceptability and satisfaction is higher for those physicians in the email group. For patient‐professional communication, results indicate that those in the email group reported more positive experiences. For value of service, it appears that using email may impact on how patients perceive the value of a service, with those in the email group willing to pay less for an online consultation. For the health service outcome; use of medical services, results indicate that those in the email group reported more use of services. For evaluation of care it was not possible to adequately assess whether email had any effect on evaluation of care.
Overall completeness and applicability of evidence
The included studies lacked data relating to healthcare professional outcomes and harms. This is reflected in the lack of focus on health professional workload and reimbursement. The lack of harm outcomes is clear in the absence of information on privacy and security, technology failures and medico‐legal issues. We had expected to see these issues addressed in the included studies.
Two comparisons were identified; email versus telephone for counselling and email compared to standard methods of communication. The comparison with standard methods could be said to mirror any potential real world use of email, as it would likely be introduced alongside existing standard methods of communication.
Digenio 2009 considered a counselling intervention delivered in different ways to patients, one method being email. This type of study is more similar to other intervention studies for behaviour change than to some of the other studies in the review. The factor setting this study apart from the excluded studies that also looked at email as a method of administering an intervention (Tate 2003; Carlbring 2006; Klein 2006; Klein 2009b), was that the effect of email was considered alone and not as part of a wider intervention. As Digenio 2009 is the only study under the comparison ‘email compared to the telephone for delivery of counselling,’ the transferability of the results is questionable.
The study by MacKinnon 1995 was carried out nearly 20 years ago, and the major changes in technology since its publication may render the results less useful to the present day. This study measured patient views amongst other things, and it is likely that views of technology use amongst patients will have changed considerably in the interim period. More generally, developments in technology have occurred since the publication of many of the included studies.
All of the studies were carried out in high income countries. The majority of studies in the review were set in the United States, the remainder in Norway, Canada and Australia.
One article was published only in Norwegian (Kummervold 2004). All other publications in the review were published in English. With the exception of Norway, English is the predominant language of these countries. Culturally and ethnically these countries are similar, which may limit the transferability of the findings to other settings.
Eight of the studies were set in urban areas and one in a mixed urban/rural population (Bergmo 2009) thus making the relevance of the results of this review to non‐urban areas questionable. This was interesting because of the perception that email as a distance technology might be useful for rural populations where attending healthcare services may be more difficult (Hilty 2006).
In addition, the study settings differ with regard to health systems. Canada, Australia and Norway have universal healthcare systems. The United States does not, instead having a more mixed system with both government and insurance‐based coverage schemes, and a significant number of people who are not covered by these schemes. These differences may impact on the transferability of the results of the studies in other settings. In particular, the differences may affect the context in which the studies were carried out, where introduction of email might be more open to market forces.
We had expected to see information on the impact of Internet and email access, along with data on socio‐economic status because of the importance of the ‘digital divide’. However, none of the included studies measured the socio‐economic status or ethnicity of participants. The issue of connection and access to the Internet and email in a broader context was rarely mentioned in any of the included studies, despite five of the studies including only participants who had access to email and/or the Internet. Demographic information presented in these studies tended to concern age and gender, but even then, there was no mention of potential generational effects and no subgroup analysis based on characteristics such as age.
The included studies featured various types of email and for the purposes of the review these were regarded as comparable. However, systems like that in Lin 2005, which featured an Internet‐based patient portal with multiple services (appointments, referrals) including electronic messaging, may be different to studies where standard email from one email account to another is used (Stalberg 2008). When the use of such technologies in healthcare is at an early stage, including all types of electronic mail together in one comparison can be justified, but future reviews may wish to consider the differences between the types of email and method of access, even if subtle.
The nature of studies concerning new methods of communication means that there is no common set of outcomes used consistently. The wide variety of outcome measures used in these reviews makes it difficult to assess exactly what is missing from the evidence base.
Quality of the evidence
We have seen that the results of this review are equivocal and in interpreting the results we must also consider the high risk of bias in included studies, with a high risk being reported for at least one domain in each study.
We used the GRADE system (Guyatt 2008) to examine the quality of the evidence for each outcome, but as we were assessing data as per each outcome rather than for pooled data the ratings should be seen as a guide to quality and strength of evidence, and not as definitive. The GRADE score for the outcomes in this review was low or very low quality. This finding reiterates that we must view the results of this review with caution.
There was a great deal of missing data in the review, with some data missing from every study. This meant that for many measures it was not possible to calculate an effect estimate. Data remained missing for many outcomes even after author contact. It is possible that had the data been available more definitive findings may have arisen, and pooling of the data may have been possible.
Of the nine studies; several were by the same authors or group of authors; Katz 2003 and Katz 2004, Bergmo 2009 and Kummervold 2004, and Lin 2005 and Ross 2004. Therefore this review identified only four different groups of authors worldwide who have carried out trials on email for clinical communication between patients/caregivers and healthcare professionals. The number of participants in the individual studies varied, from 16 to 606. The number of participants for the individual outcomes assessed in the review ranged from 74 to 379. Worldwide, this is not a large number.
There was considerable incomplete outcome reporting, occurring in all studies except one. Other types of bias were common; these included issues with the reliability of measures and how they were administered within the studies. Many of the patient outcomes were measured using scale scores. As outlined in the results section of this review (Assessment of risk of bias in included studies) many of these were not validated. Only two studies used validated measures (Bergmo 2009; Digenio 2009) and this was only for some of their measures, not all. This limits the transferability of any results obtained using such measures. It is difficult to ascertain whether they measured what was actually intended and whether the patient interpreted the scale correctly. Additionally, this also limits the ability of the instrument to measure change where change from baseline is the factor being measured, which was the case in many studies.
In Digenio 2009 the study authors were all employees of a pharmaceutical company that funded the research and this represents a conflict of interest in their conducting the research.
Potential biases in the review process
As well as database searches, we carried out an extensive search of the grey literature; this was helpful in providing a fuller picture of the evidence base. For one study we identified the thesis from which the published report originated via a Google scholar search.
As this is a fledgling field which has only become relevant alongside the increase in email use in day to day life, we can be certain to have searched the relevant time frame. By searching trial registers we will have identified any ongoing studies. The evidence base for eHealth interventions is smaller than for other fields of medicine and so the likelihood of missing studies of this nature (RCTs etc) is lower.
Terminology is an ongoing problem with searching for evidence on new technologies, especially those used for communication. Several different terms can be used to describe email: electronic mail, electronic messaging, web messaging, web consultation, amongst many others. Although the search used a wide selection of terms and truncation of terms to ensure that all variations were found, it is possible that we missed other relevant terms. The changing nature of terms for technology should be considered in any future update of this review.
The broad criteria used in this review for types of studies, participants, interventions, and outcome measures will have ensured that studies were not excluded based on these factors. However restricting the review to those studies in which there was two‐way communication for clinical purposes led to the exclusion of two studies where email was used for follow‐up and the two‐way communication was for administrative purposes (rather than clinical) (Ezenkwele 2003; Goldman 2004), though such studies could be deemed relevant for a separate review considering broader administrative purposes for email use in healthcare.
We chose to group the studies broadly with regard to comparison, taking a pragmatic approach. This was so that we were able to get an overall picture of the effects of healthcare professionals communicating with patients via email. However we could have further divided the studies under the comparison, for instance by setting, participant or intervention. This may apply to participants, where some were suffering from a particular condition (Ross 2004) and others were part of general patient population (Kummervold 2004) or where parents were proxy participants for their children rather than suffering from the condition themselves (Bergmo 2009). It is possible that the groupings we chose may have introduced bias and future versions of this review should consider the comparisons.
In addition, the methods we chose for presenting the data, that is, categorising study outcomes as per the outcomes outlined in the review, may have introduced some bias, as any assessment of category could be deemed subjective, even where more than one author is involved in making these decisions. A lack of detail in the published reports was counteracted by contacting authors for further information, but this did not always lead to our obtaining the required information. For many authors this was due to the amount of time that had elapsed since publication.
As we were unable to produce funnel plots, it was not possible to ascertain the likelihood of publication bias for individual outcomes. Despite our sensitive search strategy, it is possible that there are data that was unavailable to us. For instance, if commercial companies have carried out trials and found these results to be negative or equivocal, they may choose not to publicise these results. The need for trial registration may not be apparent to organisation embarking on their first trials and doing so for commercial reasons.
The search for this review was conducted in January 2010. A long period of time has elapsed between the search date and the publication of this review and this is a limitation as it is possible that relevant studies have been published in the interim period. To counter this, the review will be updated in the near future.
Agreements and disagreements with other studies or reviews
Other reviews have addressed the use of email in healthcare. These reviews have taken different approaches.
Ye 2010 conducted a systematic review of ‘email in patient‐provider communication’. The authors searched for empirical studies, restricting their search to those studies carried out in the US between 2000 and 2008 and written in English. They included one of the same studies as in this review (Katz 2003). The remaining included studies were not trials in design, being mostly cross‐sectional surveys. They found that personal and institutional factors were associated with the likelihood of email use between patients and providers, and that both benefits and concerns were expressed. They conclude that email is transforming the relationship between patients and providers. It is important to view the results of this review in light of the study designs included, as cross‐sectional surveys can only tell us about a particular population and are not a reliable source of evidence.
Wallwiener 2009 reviewed the literature on ‘the impact of electronic messaging on the patient‐physician interaction’. This non‐systematic review did not restrict by study design. The authors justify this by stating that ‘relatively few publications deal with electronic messaging’. They included two of the same studies as in this review (Ross 2004; Lin 2005). They state that their review found that patients are satisfied with the use of secure physician messaging and that physicians do not report adverse effects. They also state that the economic benefits of such systems are apparent. However, the authors reach their conclusions based upon a review that includes studies that are of low quality design, and mixes the results from different types of studies. Additionally the review itself considers a broad range of settings and email types.
McGeady 2007 reviewed the literature on the ‘impact of patient–physician web messaging on healthcare service provision.’ This non‐systematic review restricted only by language, searching only for studies in English. They included two of the same studies as in this review (Katz 2004; Bergmo 2005 (for Kummervold 2004)). They found that demand and support for online communication tools was strong amongst patients and that increased communication can increase quality of care. They also state that there is insufficient evidence to suggest that web‐messaging would increase process efficiency. This is the only review to acknowledge any lack of evidence, suggesting further quantitative research is necessary. However the non‐systematic nature of this review and the focus on ‘web‐messaging’ limits the validity of the conclusions concerning quality of care and patient demand and support.
Car carried out a review of the literature, split into two publications: ‘email consultations in health care: 1—scope and effectiveness’ (Car 2004a) and ‘email consultations in health care: 2—acceptability and safe application' Car 2004b. Systematic review methods were applied to identify original research and systematic reviews that evaluated the role of email communication in healthcare. The Car et al reviews report in a narrative style and focus on advantages and disadvantages of using email in healthcare, covering a broad range of uses for email. They report that interventions for professional to patient email communication mostly combine email and the Internet, via a 'patient portal' style system and several studies in this review utilised web messaging. These 'portals' often target participants with specific conditions; this was also the case for five of our included studies. In addition they conclude that email communication can assist in sustaining the doctor‐patient relationship and that its use increases patient choice. The aim of Car 2004a and Car 2004b was much wider than the present review and this is reflected in their presentation, which constitutes more of a scoping exercise.
We decided to include other types of study designs as well as randomised controlled trials in this review, but none of the non‐RCT designs were identified for inclusion. This may be explained in part by the many studies carried out using cross‐sectional survey methods and other non‐trial methodology. An example of this are studies by various US health system organisations. Kaiser Permanente published an analysis of data collected via their integrated electronic health record system concerning the use of email communication between physician and patient and the impact on quality of care (Zhou 2010). Geisinger, another US health system organisation, published the results of an online survey of patients using their patient portal for messaging their healthcare provider (Hassol 2004). Both of these studies utilised systems already in place in the form of integrated electronic healthcare records to carry out their research rather than conducting trials. Other organisations in the US (Abbott 2002; Adamson 2010) and across the world have carried out similar research on existing systems (Neville 2004).
Existing reviews on email have been broad and have provided a narrative overview of the situation to date, according to the interpretation of the authors. This has been useful in ‘setting the scene’ for the use of email in this way. Our review differs in considering closely the quality of studies and the evidence they provide. Conversely, studies of in‐situ systems provide very specific accounts of how email can work, and these are not as applicable to others working in healthcare. The state of the evidence base is such that direction is needed to ensure that future research targets the areas where definitive answers are most needed.
Authors' conclusions
Implications for practice.
Owing to the inconclusive evidence presented for the outcomes in this review, it is not possible to make recommendations for practice. However there is no evidence of harms caused by email interventions. This review highlights an evidence gap in this area of research due to the lack of high‐quality evidence.
Implications for research.
Though the findings for this review are inconclusive there were some that indicate possible important areas for future exploration. The impact of email use on healthcare professional workload may be one area in which to focus future research, since results suggest that the introduction of email may lead to an increase in emails and telephone calls to the healthcare professional; and high levels of contact with healthcare services by patients, though it should be noted that these data come from studies rated as low in quality and with some methodological flaws.
Additionally, it appears that the perceptions of email use by healthcare professionals and patients are more positive in those that are using email, than in those being asked to consider the prospect of using it. Future approaches may wish to focus less on comparing perceptions between intervention and control groups, instead focusing on outcomes that can be objectively measured in both groups. Qualitative research methods could be utilised to explore in more detail the factors that are important to the public, patients, physicians and other stakeholders.
The indication that telephone counselling may be more favourable than email counselling could be explored further in relation to the differences between the two communication methods. This may relate to factors such as the lack of vocal cues occurring with email. Further to this, changes to technology are often rapid and we should be careful to choose outcomes that remain applicable in the face of such changes. This may also involve concentrating on those elements that make email different from other methods of communication (lack of vocal cues, asynchronous nature, stability of email address versus other personal details). Such factors do not change with time as the technology changes. Otherwise randomised controlled trials may find their intervention dated by the time of their completion.
The included trials did not consider cost‐effectiveness. The costs of using email are likely to be the deciding factor for policy makers even where all outcomes are positive. Reporting the costs of email alongside the results of a trial would add context to studies as the use of a successful email system may be prohibited on cost alone.
Several outcomes in this review could not be assessed due to missing data. This may be due to poor reporting. In addition to considering the type of research that should be carried out in future, it is crucial to address the reporting of trials. Much of the uncertainty concerning the included studies in this review could have been avoided if standards for the planning, execution and presentation of trials were adhered to. Use of the CONSORT statement (transparent reporting of trials) for both RCTs and cluster RCTs (Campbell 2004; Schulz 2010) should be strongly encouraged. However, the complexity of interventions such as email can make trial reporting in traditional journals with strict word limits difficult. Interventions may require much explanation and methods of analysis may be detailed. Newer online journals often offer the opportunity to place more detail in the appendix section of a publication and this is very useful for those wishing to read about a trial in full. Additionally, registration of trials via online repositories such as clinicaltrials.gov should be strongly encouraged to discourage publication bias and selective outcome reporting. The lack of trial registration in our included studies may be due to those carrying out trials on communication systems within their own practices not seeing the need for registration as being as pressing as for drug trials and clinical interventions, or more simply because the process of doing so is not familiar to them.
Prompting the development of future research may involve addressing the barriers concerning trial development and implementation. These may include funding and time. Many of the studies in this field, both trial and non‐trial, are carried out by clinicians in practice who may be time poor and lack the resources to carry out large scale trials.
It is very likely that future versions of this review and others like it will change as the evidence base expands and as the use of email becomes more common in healthcare.
Acknowledgements
We thank the staff and editors of the Cochrane Consumers and Communication Review Group, especially Sophie Hill and Megan Prictor for their prompt and helpful advice and assistance.
We thank John Kis‐Rigo, Trials Search Co‐ordinator, Cochrane Consumers and Communication Group for compiling the search strategy.
We thank the authors of Car 2012, de Jongh 2012, Gurol‐Urganci 2012 and Vodopivec‐Jamsek 2008 for the use of their data management and analysis framework. In devising the protocol for this review we adapted their selection criteria for types of studies, participants and interventions for use in this review.
We thank Carina King and Riyadh Alshamsan for consumer input at the review stage.
We thank Toby Lasserson, Senior Editor at the Cochrane Editorial Unit for ongoing advice and assistance.
Appendices
Appendix 1. CENTRAL search strategy
| #1 | MeSH descriptor Electronic Mail, this term only |
| #2 | (electronic‐mail* or email* or e‐mail* or web‐mail* or webmail* or internet‐mail* or mailing‐list or discussion‐list or listserv*):ti,ab,kw |
| #3 | (patient or health or information or web or Internet) next portal |
| #4 | patient next (web or Internet) |
| #5 | (web* or Internet or www or electronic* or online or on‐line) near (messag* or communicat* or transmi* or transfer* or send* or deliver* or feedback or letter or interactiv* or input* or forum or appointment or booking or schedul* or remind* or referral or consult* or prescri*) |
| #6 | (online or on‐line or web* or Internet) near (service or intervention or therap* or treatment or counsel*) |
| #7 | e‐communication or e‐consult* or e‐visit or e‐referral or e‐booking or e‐prescri* |
| #8 | MeSH descriptor Computer Communication Networks, this term only |
| #9 | (#8), from 1996 to 2002 |
| #10 | (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #9) |
| #11 | MeSH descriptor Physician‐Patient Relations, this term only |
| #12 | MeSH descriptor Professional‐Patient Relations, this term only |
| #13 | MeSH descriptor Interprofessional Relations, this term only |
| #14 | "doctor patient relation":kw |
| #15 | "interpersonal communication":kw |
| #16 | "human relation":kw |
| #17 | "patient counseling":kw |
| #18 | MeSH descriptor Telemedicine explode all trees |
| #19 | telehealth or telemedicine or teleconsultation or telecommunication |
| #20 | diagnostic‐test or laboratory‐test |
| #21 | (#11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20) |
| #22 | Internet:kw,ti |
| #23 | (#21 AND #22) |
| #24 | (#10 OR #23) |
| #25 | (#24)…………….[in Clinical Trials] |
Appendix 2. Methods for application in future updates
Unit of analysis issues
Issues may arise from the inclusion of cluster‐randomised trials, repeated measurements and studies with more than two treatment groups. It is possible to correct for data that has been analysed as though individual randomisation has taken place if the following information is available:
the number of clusters (or groups) randomised to each intervention group; or the average (mean) size of each cluster;
the outcome data ignoring the cluster design for the total number of individuals (for example, number or proportion of individuals with events, or means and standard deviations); and
an estimate of the intracluster (or intraclass) correlation coefficient (ICC).
Details on how to conduct such an analysis are available in the Cochrane Collaboration Open Learning Module on issues related to the unit of analysis (Alderson 2002).
Assessment of heterogeneity
Firstly, heterogeneity will be identified by visual inspection of forest plots. Where confidence intervals for individual studies have poor overlap it generally indicates the presence of statistical heterogeneity.
Secondly, a standard Chi2 test will be used to formally test for the presence of statistical heterogeneity. Where a meta‐analysis includes studies with a small sample size or where studies are few in number the Chi2 test has low power. To allow for this a P value of 0.10 (rather than 0.05) will be used to determine statistical significance. Though a significant result may indicate a problem with heterogeneity, a non‐significant result does not provide evidence of no heterogeneity.
As well as carrying out a Chi2 test, an I2 statistic will be used. The test assesses the impact of heterogeneity on the meta‐analysis, rather than simply testing whether heterogeneity is present. The I2 statistic quantifies inconsistency across the studies. It describes the % of the variability in effect estimates that is due to heterogeneity rather than sampling error.
The importance of the observed value of I2 depends on the magnitude and direction of effects, and the strength of the evidence for heterogeneity (Chi2 test, confidence intervals for I2). Both the Chi2 value and the I2 value can be used together to assess the potential statistical heterogeneity in a meta‐analysis.
Where statistical heterogeneity is identified reasons for the heterogeneity will be sought by examining clinical and methodological heterogeneity. These are assessed by comparing the included studies according to participants, interventions, outcomes and study designs, by assessing the risk of bias and by examining subgroups. The level of statistical heterogeneity present will be taken into account when choosing the method of analysis for the review.
Assessment of reporting biases
Where data in the review have been standardised and pooled funnel plots will be used to check for publication bias. Funnel plots are produced using Review Manager5 software.
In interpreting the funnel plot it is necessary to consider possible reasons for asymmetry other than publication bias and these might include poor methodological design and sampling variation.
Data synthesis
Data synthesis will comprise a narrative overview of the findings. This would be followed by a quantitative meta‐analysis if appropriate.
The decision to carry out a meta‐analysis is dependent on the nature of the studies included in the review. The diversity between studies according to clinical factors, comparisons and outcomes will be considered.
The decision is likely to depend upon the type of intervention and the outcome measures used in the study. Therefore studies should be classified according to:
Study design: RCTs, CBAs, ITS.
Outcome measures used, as described under Types of outcome measures
The risk of bias in the included studies will also be considered. Where there is great diversity between studies, and/or a high risk of bias, it is not necessarily appropriate to pool the data. A decision on whether to carry out a meta‐analysis will made be according to these factors and after discussion amongst study authors.
Where it is deemed appropriate to carry out a meta‐analysis the choice of model will be influenced by the level of statistical heterogeneity identified using both the Chi2 and I2 test.
A random‐effects meta‐analysis assumes that the studies are not all estimating the same intervention effect. It can be used to incorporate heterogeneity among studies. It is not a substitute for a thorough investigation of heterogeneity and is intended primarily for heterogeneity that cannot be explained. It provides a more conservative estimate of effect. A fixed‐effect meta‐analysis assumes that each study is estimating exactly the same quantity and that any variation between the results of the studies is due to chance. It more precise than a random‐effects model, because in the presence of statistical heterogeneity it usually has narrower confidence intervals.
We will conduct the analysis according to Cochrane Handbook guidance (Higgins 2008).
Subgroup analysis and investigation of heterogeneity
Where relevant, subgroup analysis will allow the examination of the effect of certain studies on the pooled effects of the intervention.
1. Age
Consideration of the acceptability to different age groups (for both healthcare professionals and patients). This is important as there is clear evidence that the use of email is predicted by age with a clear tailing off in the generation who have not grown up in the digital age. It is therefore important to consider the intervention effect in the groups which are accustomed to the technology, since the intervention is likely to become more generalisable to the population as it ages. This will be considered where the primary studies seek to consider age group from the outset. We would have distributed patients into three age subgroups: 0 to 17, 18 to 64, over 65. The choice of distribution was made on the basis of two surveys by The Pew Internet & American Life survey (Pew 2005).
2. Location
Location of the studies will also be considered, since differing environments may condition the accessibility of the technology. For instance we might expect communication technologies and their accessibility to differ according to country and/or region, or according to whether the study is set in a rural or urban area.
3. Type of email communication
Additionally we propose to analyse the results by method of electronic mail utilized e.g. standard email versus a secure web messaging service where relevant.
4. Year of Publication
Lastly we will consider results by year of publication, as those more recent studies may be more relevant given evidence of increasing usage and therefore assumed acceptability.
Sensitivity analysis
Studies deemed to be of lower quality after examination of individual study characteristics and assessment of risk of bias will be removed from the analysis to examine the effects of this on the pooled effects of the intervention.
We would exclude studies according to the following filters:
Outlying studies after initial analysis.
Largest studies.
Unpublished studies.
Language of publication.
Source of funding (e.g. public versus industry).
Other possible considerations for sensitivity analysis would include different measures of effect size (risk difference, odds ratios).
Appendix 3. MEDLINE (OvidSP) search strategy
1. computer communication networks/
2. limit 1 to yr="1996 ‐ 2002"
3. electronic mail/
4. (electronic mail* or email* or e‐mail* or web mail* or webmail* or Internet mail* or mailing list* or discussion list* or listserv*).tw.
5. ((patient or health or information or web or Internet) adj portal*).tw.
6. (patient adj (web* or Internet)).tw.
7. ((web* or Internet or www or electronic* or online) adj5 (messag* or communicat* or transmi* or transfer* or send* or deliver* or feedback or letter* or interactiv* or input* or forum or appointment* or booking* or remind* or referral* or consult* or prescri*)).tw.
8. ((online or web* or Internet) adj4 (service* or intervention* or therap* or treatment* or counsel*)).tw.
9. (e‐communication* or e‐consult* or e‐visit* or e‐referral* or e‐booking* or e‐prescri*).tw.
10. or/2‐9
11. physician patient relations/
12. professional patient relations/
13. interprofessional relations/
14. remote consultation/
15. or/11‐14
16. Internet/
17. 15 and 16
18. 10 or 17
19. randomized controlled trial.pt.
20. controlled clinical trial.pt.
21. random*.tw.
22. placebo*.tw.
23. drug therapy.fs.
24. trial.tw.
25. groups.tw.
26. clinical trial.pt.
27. evaluation studies.pt.
28. research design/
29. follow up studies/
30. prospective studies/
31. (control* or prospectiv* or volunteer*).tw.
32. cross over studies/
33. comparative study.pt.
34. experiment*.tw.
35. time series.tw.
36. (pre test or pretest or post test or posttest).tw.
37. (pre intervention or preintervention or post intervention or postintervention).tw.
38. (impact* or intervention* or chang*).tw.
39. effect?.tw.
40. or/19‐39
41. exp animals/ not humans.sh.
42. 40 not 41
43. 18 and 42
Appendix 4. EMBASE (OvidSP) search strategy
1. e‐mail/
2. (electronic mail* or email* or e‐mail* or web mail* or webmail* or Internet mail* or mailing list* or discussion list* or listserv*).tw.
3. ((patient or health or information or web or Internet) adj portal*).tw.
4. (patient adj (web* or Internet)).tw.
5. ((web* or Internet or www or electronic* or online) adj5 (messag* or communicat* or transmi* or transfer* or send* or deliver* or feedback or letter* or interactiv* or input* or forum or appointment* or booking* or scheduling or remind* or referral* or consult* or prescri*)).tw.
6. ((online or web* or Internet) adj4 (service* or intervention* or therap* or treatment* or counsel*)).tw.
7. (e‐communication* or e‐consult* or e‐visit* or e‐referral* or e‐booking* or e‐prescri*).tw.
8. or/1‐7
9. doctor patient relation/
10. interpersonal communication/
11. human relation/
12. patient counseling/
13. exp telemedicine/
14. telecommunication/
15. exp diagnostic test/
16. or/9‐15
17. Internet/
18. 16 and 17
19. 8 or 18
20. randomized controlled trial/
21. single blind procedure/ or double blind procedure/
22. crossover procedure/
23. random*.tw.
24. trial.tw.
25. placebo*.tw.
26. ((singl* or doubl*) adj (blind* or mask*)).tw.
27. (experiment* or intervention*).tw.
28. (pre test or pretest or post test or posttest).tw.
29. (preintervention or postintervention).tw.
30. (cross over or crossover or factorial* or latin square).tw.
31. (assign* or allocat* or volunteer*).tw.
32. (control* or compar* or prospectiv*).tw.
33. (impact* or effect? or chang* or evaluat*).tw.
34. time series.tw.
35. or/20‐34
36. nonhuman/
37. 35 not 36
38. 19 and 37
Appendix 5. PsycINFO (OvidSP) search strategy
1. exp electronic communication/
2. (electronic mail* or email* or e‐mail* or web mail* or webmail* or Internet mail* or mailing list* or discussion list* or listserv*).tw.
3. ((patient or health or information or web or Internet) adj portal*).tw.
4. (patient adj (web* or Internet)).tw.
5. ((web* or Internet or www or electronic* or online) adj5 (messag* or communicat* or transmi* or transfer* or send* or deliver* or feedback or letter* or interactiv* or input* or forum or appointment* or booking* or schedul* or remind* or referral* or consult* or prescri*)).tw.
6. ((online or web* or Internet) adj4 (service* or intervention* or therap* or treatment* or counsel*)).tw.
7. online therapy/
8. (e‐communication* or e‐consult* or e‐visit* or e‐referral* or e‐booking* or e‐prescri*).tw.
9. or/1‐8
10. exp therapeutic processes/
11. interpersonal communication/
12. telemedicine/
13. feedback/
14. or/10‐13
15. Internet/
16. exp Internet usage/
17. 15 or 16
18. 14 and 17
19. 9 or 18
20. ("32" or "33" or "34").cc.
21. (health* or medic* or patient* or clinic* or hospital* or illness* or disease* or disorder* or therap* or physician* or doctor* or psychotherap* or psychiatr* or telemedic* or treatment* or consult* or counsel* or referral* or remind* or appointment* or booking* or schedul* or visit* or prescri* or promot* or prevent* or diagnos* or test result* or screen* or intervention* or care).ti,ab,hw,id.
22. 20 or 21
23. 19 and 22
24. random*.ti,ab,hw,id.
25. (experiment* or intervention*).ti,ab,hw,id.
26. trial*.ti,ab,hw,id.
27. placebo*.ti,ab,hw,id.
28. groups.ab.
29. ((singl* or doubl* or trebl* or tripl*) and (blind* or mask*)).ti,ab,hw,id.
30. (pre test or pretest or post test or posttest).ti,ab,hw,id.
31. (preintervention or postintervention).ti,ab,hw,id.
32. (cross over or crossover or factorial* or latin square).ti,ab,hw,id.
33. (assign* or allocat* or volunteer*).ti,ab,hw,id.
34. (control* or compar* or prospectiv*).ti,ab,hw,id.
35. (impact* or effect? or chang* or evaluat*).ti,ab,hw,id.
36. time series.ti,ab,hw,id.
37. exp experimental design/
38. ("0430" or "0450" or "0451" or "1800" or "2000").md.
39. or/24‐38
40. limit 39 to human
41. 23 and 40
Appendix 6. CINAHL (EbscoHOST) search strategy
Cochrane Consumers and Communication Review Group ran the search.
Appendix 7. ERIC (CSA) search strategy
(KW=(computer mediated communication* or electronic mail* or email* or e‐mail* or web mail* or webmail* or Internet mail* or mailing list* or discussion list* or listserv*) or KW=((patient or health or information or web or Internet) within 1 portal*) or KW=(patient within 1 (web* or Internet)) or KW=((web* or Internet or www or electronic* or online or on‐line) within 5 (messag* or communicat* or transmi* or transfer* or send* or deliver* or feedback or letter* or interactiv* or input* or forum or appointment* or booking* or schedul* or remind* or referral* or consult* or prescri*)) or KW=((online or on‐line or web* or Internet) within 4 (service* or intervention* or therap* or treatment* or counsel*)) or KW=(e‐communication* or e‐consult* or e‐visit* or e‐referral* or e‐booking* or e‐prescri*)) and (KW=(health* or medic* or patient* or clinic* or hospital* or illness* or disease* or disorder* or therap* or physician* or doctor* or psychotherap* or psychiatr* or telemedic* or treatment* or consult* or counsel* or referral* or remind* or appointment* or booking* or schedul* or visit* or prescri* or promot* or prevent* or diagnos* or test result* or screen* or intervention* or care)) and (KW=(random* or trial* or placebo* or assign* or allocat* or volunteer* or crossover or cross over or factorial* or singl* blind* or doubl* blind* or clinical stud* or longitudinal stud* or control* or compar* or intervention* or preintervention or postintervention or pre test or pretest or post test or posttest or experiment* or prospectiv* or chang* or evaluat* or impact* or effect* or time series))
Data and analyses
Comparison 1. Email compared to standard methods of communication: Primary outcome, patient understanding:
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 How did communication with the surgeon affect your understanding of postoperative instructions? (Scale 1‐7) | Other data | No numeric data |
Comparison 2. Email compared to standard methods of communication: Primary outcome, patient health status and wellbeing.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 How did communication with the surgeon affect your anxiety level on the day of the operation? (Scale 1‐7) | Other data | No numeric data |
Comparison 3. Email compared to standard methods of communication: Primary outcome, patient/caregiver views.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 How did communication with the surgeon affect your sense of preparedness for the operation (Scale 1‐7) | Other data | No numeric data | ||
| 2 Questions and concerns addressed in a satisfactory manner? (Scale 1‐7) | Other data | No numeric data | ||
| 3 How did communication with the surgeon affect your sense that the surgeon was available to deal with any problems that might arise? (Scale 1‐7) | Other data | No numeric data | ||
| 4 Requests and questions dealt with in a timely manner (satisfaction rating at 6 months) (Scale 1‐5) | Other data | No numeric data | ||
| 5 Problems dealt with adequately (satisfaction rating at 6 months) (Scale 1‐5) | Other data | No numeric data |
Comparison 4. Email compared to standard methods of communication: Primary outcome, patient behaviours/actions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Used the Internet to find information about your disease | 1 | 74 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.42, 3.04] |
| 2 Used Internet to find information about where to seek treatment | 1 | 74 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.10, 4.12] |
| 3 How did communication with the surgeon affect your ability to make appropriate work/family arrangements for the operation (Scale 1‐7) | Other data | No numeric data |
Comparison 5. Email compared to standard methods of communication: Primary outcome, health service outcome, resource use; patient participants.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean number of contacts to GP and front office during study period: change from baseline | 1 | 166 | Mean Difference (IV, Fixed, 95% CI) | ‐1.26 [‐1.85, ‐0.67] |
| 2 Mean number of office visits per patient per year: change from baseline | 1 | 199 | Mean Difference (IV, Fixed, 95% CI) | ‐1.1 [‐1.87, ‐0.33] |
| 3 Mean number of phone consultations per patient per year: change from baseline | 1 | 199 | Mean Difference (IV, Fixed, 95% CI) | ‐0.8 [‐1.37, ‐0.23] |
| 4 Visits to complementary therapist: mean reduction | 1 | Mean Difference (Fixed, 95% CI) | 0.71 [‐0.11, 1.53] | |
| 5 Number of messages sent to the practice (mean per patient) | Other data | No numeric data |
Comparison 6. Email compared to standard methods of communication: Primary outcome, health service outcome, resource use; physicians participants.
Comparison 7. Email compared to telephone for delivery of counselling: Primary outcome, patient health status and wellbeing.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Body weight ‐ percentage change from baseline | 1 | Mean Difference (Fixed, 95% CI) | 1.8 [1.75, 1.85] | |
| 2 Mean absolute weight loss at 6 months (kg) | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | ‐1.86 [‐4.02, 0.30] |
| 3 Waist circumference ‐ mean absolute change from baseline (inches) | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.98, 1.18] |
| 4 Systolic blood pressure ‐ mean absolute change from baseline (mmHg) | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [‐2.84, 4.64] |
| 5 Diastolic blood pressure ‐ mean absolute from baseline (mmHg) | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.7 [‐1.79, 3.19] |
| 6 Pulse rate (bpm) | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | ‐0.5 [‐3.55, 2.55] |
| 7 Total cholesterol ‐ percentage change from baseline | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐4.81, 5.01] |
| 8 Triglycerides ‐ percentage change from baseline | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 4.80 [‐9.77, 19.37] |
| 9 HDL‐C percentage change from baseline | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | ‐5.90 [‐11.55, ‐0.25] |
| 10 LDL‐C ‐ percentage change from baseline | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | ‐1.50 [‐13.80, 10.80] |
| 11 Fasting glucose ‐ percentage change from baseline | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 2.60 [‐1.45, 6.65] |
| 12 Insulin ‐ percentage change from baseline | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 9.5 [‐15.53, 34.53] |
| 13 Weight loss of at least 5% | 1 | 105 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.30, 1.41] |
| 14 Weight loss of at least 10% | 1 | 105 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.23, 1.50] |
7.2. Analysis.
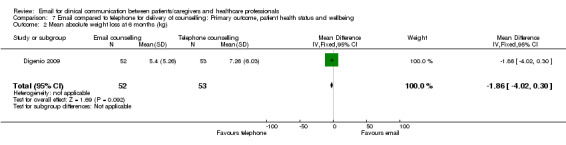
Comparison 7 Email compared to telephone for delivery of counselling: Primary outcome, patient health status and wellbeing, Outcome 2 Mean absolute weight loss at 6 months (kg).
7.3. Analysis.
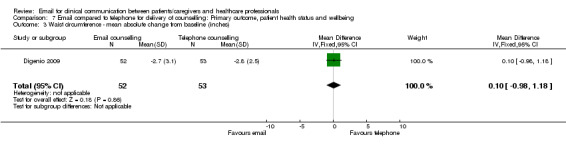
Comparison 7 Email compared to telephone for delivery of counselling: Primary outcome, patient health status and wellbeing, Outcome 3 Waist circumference ‐ mean absolute change from baseline (inches).
7.4. Analysis.
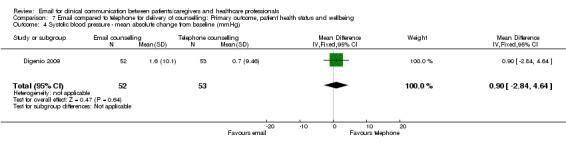
Comparison 7 Email compared to telephone for delivery of counselling: Primary outcome, patient health status and wellbeing, Outcome 4 Systolic blood pressure ‐ mean absolute change from baseline (mmHg).
7.5. Analysis.
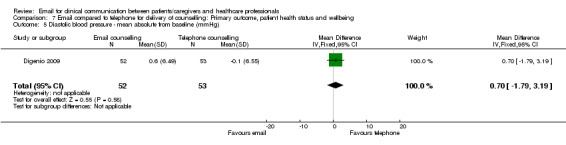
Comparison 7 Email compared to telephone for delivery of counselling: Primary outcome, patient health status and wellbeing, Outcome 5 Diastolic blood pressure ‐ mean absolute from baseline (mmHg).
7.6. Analysis.
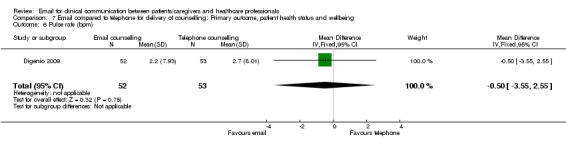
Comparison 7 Email compared to telephone for delivery of counselling: Primary outcome, patient health status and wellbeing, Outcome 6 Pulse rate (bpm).
7.7. Analysis.
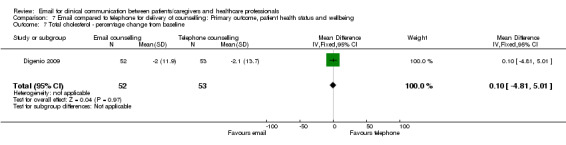
Comparison 7 Email compared to telephone for delivery of counselling: Primary outcome, patient health status and wellbeing, Outcome 7 Total cholesterol ‐ percentage change from baseline.
7.8. Analysis.
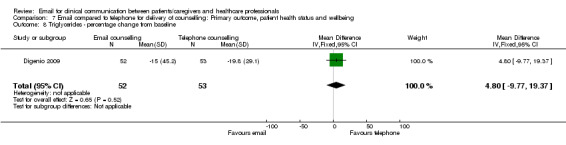
Comparison 7 Email compared to telephone for delivery of counselling: Primary outcome, patient health status and wellbeing, Outcome 8 Triglycerides ‐ percentage change from baseline.
7.10. Analysis.
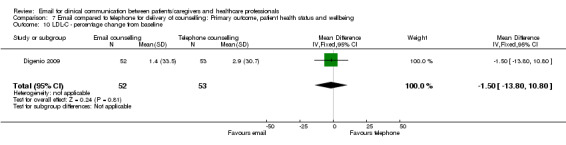
Comparison 7 Email compared to telephone for delivery of counselling: Primary outcome, patient health status and wellbeing, Outcome 10 LDL‐C ‐ percentage change from baseline.
7.11. Analysis.
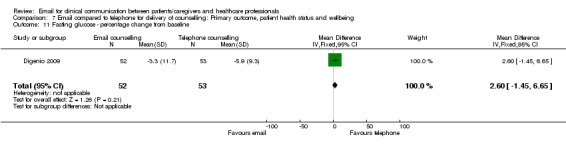
Comparison 7 Email compared to telephone for delivery of counselling: Primary outcome, patient health status and wellbeing, Outcome 11 Fasting glucose ‐ percentage change from baseline.
7.12. Analysis.
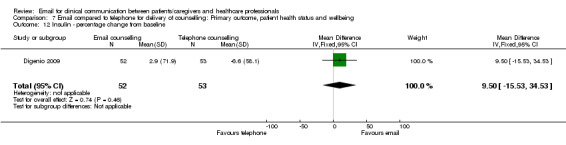
Comparison 7 Email compared to telephone for delivery of counselling: Primary outcome, patient health status and wellbeing, Outcome 12 Insulin ‐ percentage change from baseline.
7.13. Analysis.

Comparison 7 Email compared to telephone for delivery of counselling: Primary outcome, patient health status and wellbeing, Outcome 13 Weight loss of at least 5%.
7.14. Analysis.

Comparison 7 Email compared to telephone for delivery of counselling: Primary outcome, patient health status and wellbeing, Outcome 14 Weight loss of at least 10%.
Comparison 8. Email compared to telephone for delivery of counselling: Primary outcome, patient behaviours/actions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 IWQOL‐Lite score ‐ mean absolute change from baseline | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | ‐1.30 [‐32.21, 29.61] |
| 2 WRSM total bothersome score ‐ mean absolute change from baseline | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | ‐2.40 [‐50.94, 46.14] |
| 3 Adherence to dietician contact | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 3.70 [‐7.52, 14.92] |
| 4 Web utilisation | 1 | 105 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.02, 2.14] |
| 5 Mean number of logins to the website | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | ‐11.0 [‐16.04, ‐5.96] |
| 6 Mean number of days participants logged into website to enter information | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐3.02, 3.02] |
8.1. Analysis.
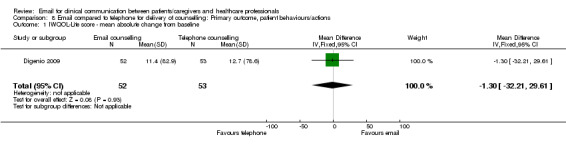
Comparison 8 Email compared to telephone for delivery of counselling: Primary outcome, patient behaviours/actions, Outcome 1 IWQOL‐Lite score ‐ mean absolute change from baseline.
8.2. Analysis.
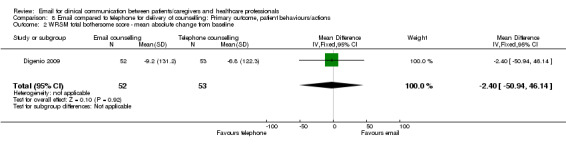
Comparison 8 Email compared to telephone for delivery of counselling: Primary outcome, patient behaviours/actions, Outcome 2 WRSM total bothersome score ‐ mean absolute change from baseline.
8.3. Analysis.
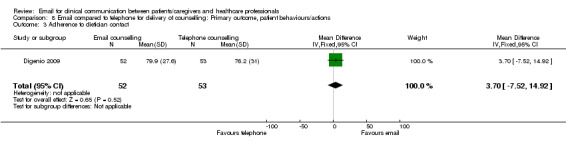
Comparison 8 Email compared to telephone for delivery of counselling: Primary outcome, patient behaviours/actions, Outcome 3 Adherence to dietician contact.
8.4. Analysis.
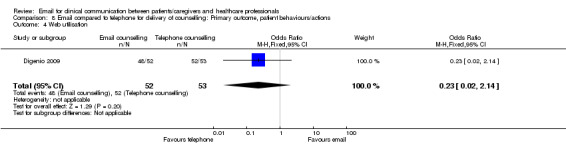
Comparison 8 Email compared to telephone for delivery of counselling: Primary outcome, patient behaviours/actions, Outcome 4 Web utilisation.
8.6. Analysis.
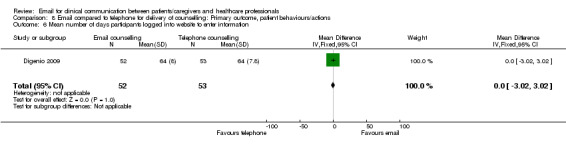
Comparison 8 Email compared to telephone for delivery of counselling: Primary outcome, patient behaviours/actions, Outcome 6 Mean number of days participants logged into website to enter information.
Comparison 9. Email compared to telephone for delivery of counselling: primary outcomes: harms.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Discontinued participation due to adverse effects | 1 | 150 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.34, 5.06] |
Comparison 10. Email compared to standard methods of communication: Secondary outcome, health professional perceptions.
10.1. Analysis.
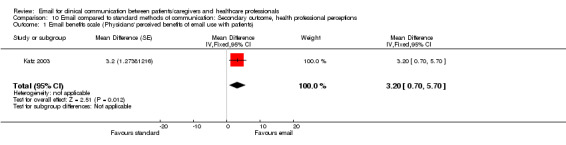
Comparison 10 Email compared to standard methods of communication: Secondary outcome, health professional perceptions, Outcome 1 Email benefits scale (Physicians' perceived benefits of email use with patients).
10.2. Analysis.
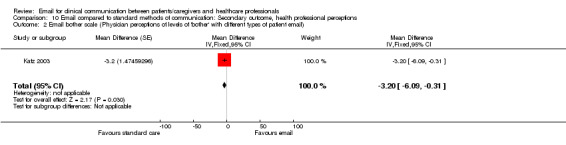
Comparison 10 Email compared to standard methods of communication: Secondary outcome, health professional perceptions, Outcome 2 Email bother scale (Physician perceptions of levels of 'bother' with different types of patient email).
10.3. Analysis.
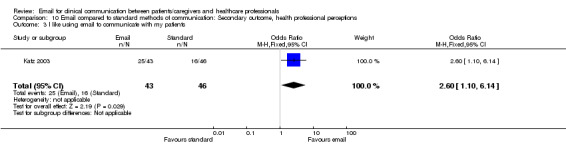
Comparison 10 Email compared to standard methods of communication: Secondary outcome, health professional perceptions, Outcome 3 I like using email to communicate with my patients.
10.4. Analysis.
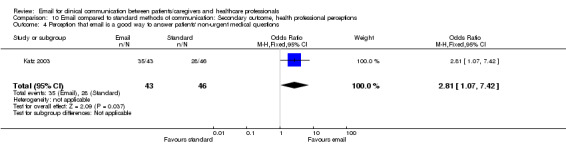
Comparison 10 Email compared to standard methods of communication: Secondary outcome, health professional perceptions, Outcome 4 Perception that email is a good way to answer patients' non‐urgent medical questions.
10.5. Analysis.
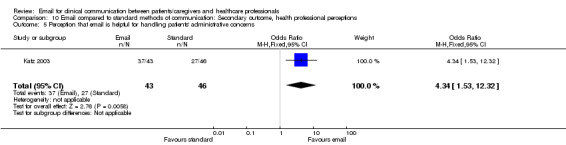
Comparison 10 Email compared to standard methods of communication: Secondary outcome, health professional perceptions, Outcome 5 Perception that email is helpful for handling patients' administrative concerns.
10.6. Analysis.
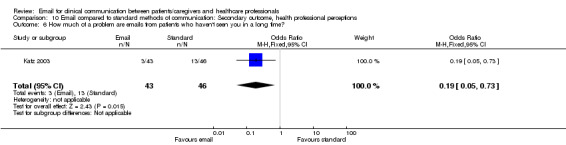
Comparison 10 Email compared to standard methods of communication: Secondary outcome, health professional perceptions, Outcome 6 How much of a problem are emails from patients who haven't seen you in a long time?.
10.8. Analysis.
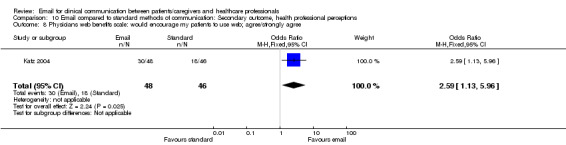
Comparison 10 Email compared to standard methods of communication: Secondary outcome, health professional perceptions, Outcome 8 Physicians web benefits scale: would encourage my patients to use web; agree/strongly agree.
10.9. Analysis.
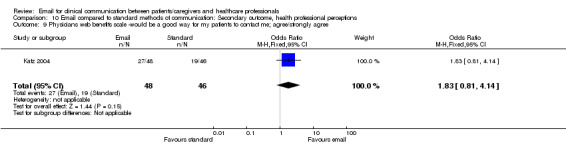
Comparison 10 Email compared to standard methods of communication: Secondary outcome, health professional perceptions, Outcome 9 Physicians web benefits scale ‐would be a good way for my patients to contact me; agree/strongly agree.
10.10. Analysis.
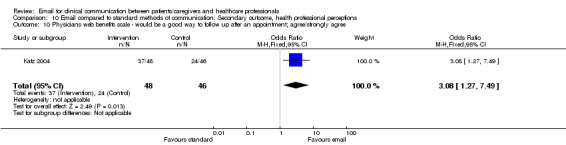
Comparison 10 Email compared to standard methods of communication: Secondary outcome, health professional perceptions, Outcome 10 Physicians web benefits scale ‐ would be a good way to follow up after an appointment; agree/strongly agree.
10.11. Analysis.
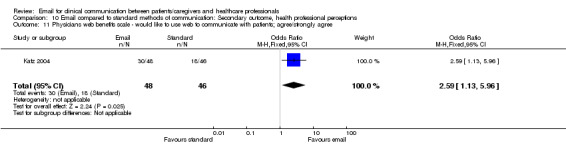
Comparison 10 Email compared to standard methods of communication: Secondary outcome, health professional perceptions, Outcome 11 Physicians web benefits scale ‐ would like to use web to communicate with patients; agree/strongly agree.
Comparison 11. Email compared to standard methods of communication: Secondary outcomes, patient outcome, effect on patient‐professional communication.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Communicating nonurgent messages to doctor and/or nurse rated as excellent/very good | 1 | 278 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.63 [1.61, 4.29] |
| 2 Communicating nonurgent messages to doctor and/or nurse rated as poor | 1 | 278 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.25, 1.23] |
| 3 How effective was the communication with your surgeon prior to surgery? (Scale 1‐7) | Other data | No numeric data | ||
| 4 How effective was the communication with your surgeon after surgery? (Scale 1‐7) | Other data | No numeric data | ||
| 5 Overall, how effective was the communication with your surgeon? (Scale 1‐7) | Other data | No numeric data |
Comparison 12. Email compared to standard methods of communication: Secondary outcome, patient outcome, evaluation of care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Overall satisfaction with surgical experience? (Scale 1‐7) | Other data | No numeric data |
Comparison 13. Email compared to standard methods of communication: Secondary outcome, patient outcome, value of service.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Amount willing to pay per online consultation in euros (median and percentiles) | Other data | No numeric data |
Comparison 14. Email compared to standard methods of communication: Secondary outcome, health service outcomes, use of medical services.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of patients who initiated additional contact with the surgeon | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.76 [1.41, 10.05] |
| 2 Telephone messages per patient (for those consenting to allow a view of their medical record only) | 1 | 291 | Mean Difference (IV, Fixed, 95% CI) | ‐0.06 [‐0.33, 0.21] |
| 3 Total messages (telephone plus portal) per patient (for those patients consenting to allow a view of their medical record) | 1 | 291 | Mean Difference (IV, Fixed, 95% CI) | 0.19 [‐0.15, 0.53] |
| 4 Number of contacts with the augmentative communication service | Other data | No numeric data | ||
| 5 Number of independent contacts with the augmentative communication service | Other data | No numeric data |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bergmo 2009.
| Methods | Study design: Randomised controlled trial Duration of intervention: 1 year Recruitment: 131 parents invited to participate during outpatient consultation at the paediatric and dermatology clinic. Recruitment period lasted 15 months. |
|
| Participants | Description: Parents of children who visited the Paediatric and Dermatology clinic. Setting: Paediatric and Dermatology clinics at secondary care hospitals in Norway. No inclusion or exclusion criteria. 119 parents agreed to participate, 21 did not return consent form, 98 children randomised, 50 to intervention group and 48 to control group. |
|
| Interventions | Intervention: System allowed parents of children to send photos of the eczema area and a written description of the child's condition to the specialist. Provision of software to parents enabling them to use the secure messaging system. A digital camera was loaned to parents who did not own one. Parents log in with a user name and a password over an encrypted connection. Two‐phased authentication, one‐time password sent to participant cell phone, valid for 10 min. Procedure repeated for sending messages/retrieving responses. Specialist responds with treatment advice. Control: Received standard treatment without access to specialist care. Encouraged to seek treatment through traditional means such as GP visits and hospital care. Co‐interventions: Both groups took part in a 30 min individual face‐to‐face educational session prior to the intervention ‐ knowledge of Atopic Dermatitis and self‐management skills were strengthened by instruction in eczema‐related skin care from a specialist nurse. |
|
| Outcomes | Use of web consultations (during study period, unclear how measured). Self management behaviour (via self‐reported questionnaire on treatments used, at 12 months). Severity of eczema (health outcomes, assessed by physicians using the SCOring Atopic Dermatitis (SCORAD) tool at 12 months). Resource use (healthcare visits/expenses via self‐reported questionnaire at 12 months). Parents absence from employment (family costs via self‐reported questionnaire at 12 months). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Children were consecutively randomised into two groups, using the simple randomisation method with shuffled envelopes. |
| Allocation concealment (selection bias) | Low risk | The envelopes used were sealed. |
| Blinding (performance bias and detection bias) All outcomes | High risk | The dermatologist assessing the severity of eczema in participants was aware of group allocation. For all other outcomes investigators were blinded. This was confirmed by contact with the author. Parents received a letter informing them of their group allocation. |
| Incomplete outcome data (attrition bias) All outcomes. | High risk | Self management behaviour, resource use, parents absence from employment: only 74% of participants responded to the post‐intervention questionnaire and no information is given on non‐responders. Severity of eczema: No information given on whether the SCORAD for measuring severity of eczema was completed for all participants and as the results are not presented by group it is not possible to tell. Not possible to tell if an intention to treat analysis was carried out as the results are not presented as intervention versus control group. |
| Selective reporting (reporting bias) | High risk | The results are presented such that it is not possible to see how many were in each group (I/C) for the main outcome measures. The results for the primary outcomes are presented by intervention and control group at baseline, but not at the end of the intervention period, where they are presented for the whole sample only. Pre intervention/post intervention figures are presented for the whole sample rather than by intervention/control group. Author contact confirmed that authors chose to present the data in this way 'We would have presented the results separately for the two groups in more detail if we had found an interaction effect (between group differences). But we did not.' |
| Other bias | High risk | Baseline comparability: Sample differed significantly by age of parents (P = 0.02) (control parents older) and number of people living in urban areas (P = 0.006) with more people in the control group living in urban areas. Otherwise comparable. Validation of measures: No information is given on whether the participant questionnaire is validated. SCORAD tool is validated. Reliability of measures: Authors state that the lack of inter‐rater reliability in the estimated SCORAD is a limitation. Selection bias: There was potential for selection bias as all study participants had Internet access, and they were recruited at outpatient clinics (authors discuss 'bias towards technology acceptance and a higher frequency of health care visits than children with AD in general'). Recall bias: questionnaires and data on resource use were self‐reported. |
Digenio 2009.
| Methods | Study design: Randomised 6 month open label study. Follow‐up: At 2, 4, 12 and 24 weeks. Recruitment: Advertisements placed in the community. |
|
| Participants | Description: Community based persons fitting eligibility criteria. Setting: 12 US research centres comprising mostly non‐academic independent clinics that had experience running clinical trials with obese patients. Inclusions: Aged 25 to 60 years, body mass index of at least 30kg/m2 but less than 40kg/m2. Eligible to receive sibutramine (per the US package inset), able to adhere to study procedures and have access to the Internet and email. Exclusions: Uncontrolled blood pressure (≥ 140/90 mm Hg); type 1 or 2 diabetes; coronary heart disease; chronic congestive heart failure; stroke; substantial metabolic, hepatic or renal disease; current cancer or gastric bypass surgery. Lost 10% or more of initial weight in last 6 months, participated in a structured weight loss program or taken weight loss drugs. Women who are pregnant or breastfeeding. Other: Women of childbearing potential had to use adequate contraception. 437 potential participants screened, 376 assigned to the study and randomised. Assignment of participants to groups: HF‐F2F = 74, LF‐F2F = 76, HF‐TEL = 76, HF‐EMAIL = 74, SELF = 76. |
|
| Interventions | Intervention: Lifestyle modification program with varying frequency and type of contact with a dietician. Five intervention groups: high frequency* face‐to‐face counselling (HF‐F2F). Low frequency face‐to‐face counselling (LF‐F2F). High frequency telephone counselling (HF‐TEL). High frequency email counselling (HF‐EMAIL). Lifestyle modification program but with no dietician contact (SELF). *High frequency = weekly dietician contact during first 3 months of study and every other week during the following 3 months. Low frequency = monthly dietician contact. Co‐interventions: All 5 groups received same drug treatment (sibutramine, 10mg/d) and a standardised life modification program for weight‐loss that included a printed manual and access to a weight‐loss website. All participants to adopt a 750 kcal/deficit diet with a minimum intake of 1000 kcal/d for women and 1200 kcal/d for men. Macronutrient composition of the diet consisted of 15% protein, 30% (or less) fat and 55% carbohydrate. Recommended walking as the primary method of physical activity. All participants given a pedometer and recommended increasing their number of steps per day by approximately 500 steps each week. Participants encouraged to build to a goal of 10,000 steps per day. Behavioural treatment strategies included goal setting, self‐monitoring (including weekly weighing and completion of daily food intake and physical activity logs), stimulus control, enlisting the support of family and friends, use of problem‐solving skills to overcome barriers, cognitive restructuring, and coping with slips and lapses. All participants received the same support materials, which were a lifestyle modification manual (both in print and electronic format) and access to an interactive weight‐loss website application. Participants were encouraged to log on to the website at least once a week |
|
| Outcomes | Primary outcome:
Secondary outcomes:
Also included descriptively summarised data: frequency of logins, number of days logged (collected via website, ongoing). |
|
| Notes | Research grant from Pfizer Global Research and Development, Groton, Connecticut. Funding source participated in study design and protocol development; logistical support for study conduct, data collection and data analysis and prepared the manuscript. Potential financial conflicts of interest: all authors employed by Pfizer, all authors have stock ownership or options (other than mutual funds) in Pfizer. Nineteen participants discontinued the study because of adverse events. Authors state 'none were serious or attributed to the intervention.' Event included: dizziness, headache, depression, palpitations, amnesia, insomnia, nausea, vomiting, chest pain. Authors state 'rate of occurrence similar amongst groups' and 'no changes of clinical significance in urinalysis, serum chemistry or hematologic test results.' |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Assigned participants to 1 of 5 intervention groups using computer‐generated randomisation schedule consisting of randomly permuted blocks. Block length was 5. |
| Allocation concealment (selection bias) | Low risk | A central telephone randomisation system was used. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Study is described as 'open‐label' because participants were aware that they would receive the drug Sibutramine. Contact with author confirmed that dieticians, patients and investigators were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes. | High risk | Participants excluded after randomisation are accounted for and reasons for exclusion provided. Number of participants not completing the study given along with reasons (111 (30%) did not complete; adverse events:19, defaulted (at their request or lost to follow up): 85, other: 7). Results for all outcomes (body weight, waist circumference, lipid, glucose and insulin levels, blood pressure, changes in quality of life and weight related symptoms and adherence to the intervention for the groups with dietician contacts) are presented in a table as having been calculated for the number of completers only. This is despite the authors describing a modified intention‐to‐treat analysis which included all randomly assigned participants who had a baseline measurement and at least 1 post baseline measurement of body weight. Participants were stated as being considered members of the intervention group in which they were randomly assigned, regardless of adherence. Additionally a sensitivity analysis was carried out using three imputation methods. The same uncertainty applies to the post‐hoc analysis of weight loss of at least 5% and 10% where the denominator is not known. |
| Selective reporting (reporting bias) | High risk | All outcomes are presented as per protocol, however also presented is an additional post‐hoc analysis comparing the proportions of participants achieving 5% and 10% weight loss at 24 weeks. Additionally the result for a comparison (Low Frequency F2F, SELF and EMAIL) is described as being non‐significant but a P‐value is not presented so this cannot be confirmed. None of the website data (web utilisation, number of logins, number of days logged, steps per day and calories per day) were pre‐specified in the study protocol. The published report states that self‐reported data collected through the website will be descriptively summarised (web utilisation, number of logins, number of days logged, steps per day (pedometer readings) and calories per day) . However data for steps per day (pedometer readings) and calories per day are not presented in the results section. |
| Other bias | High risk | Baseline comparability: Authors state that 'There were no differences of clinical or statistical significance in baseline characteristics among treatment groups' however no P values are presented. Validation of measures:IWQOL‐Lite and the WRSM are validated. No information given on whether other measures were validated. Reliability of measures: Patient‐reported scales (IWQOL‐Lite, WRSM) may be subject to reporting bias by patients. Body weight measurements were obtained using a calibrated scale with the same scale used at each site. No Information given on reliability of biochemical measurements Lack of usual care control group: Five interventions were compared, but all groups received the drug sibutramine. This makes it difficult to separate the effects of the drug and intervention. The authors mention this in the discussion: 'lack of randomly assigned group without sibutramine does not allow us to properly separate the effect of the drug from the lifestyle intervention.' |
Katz 2003.
| Methods | Study design: Cluster randomised controlled trial. The study report describes this as a randomised controlled trial. Duration of study: 11 months. Recruitment: Invited all practising physicians in the two participating clinics. |
|
| Participants | Description: Physicians (faculty and resident) in internal medicine and family practice in primary care clinics. Setting:Two university affiliated primary care clinics, Michigan, Mid‐West America. There were no inclusion and exclusion criteria. Physician sample consisting of 98 physicians (24 staff physicians, 74 resident physicians) randomised, 50 to intervention group, 48 to control group. |
|
| Interventions | Intervention: EMAIL ‐ Electronic messaging, advice and information link. The system consists of an e‐mail interface between patients and the health system mediated by triage nurses. All emails automatically routed to a central resource account managed by a nurse navigator who routed messages within the account to appropriate staff. Physicians received copies of their messages but replied to only those requiring physician input, such as patient‐specific health questions. Clinic staff entered the central account to receive and respond to messages not requiring physician input. Intervention promoted to patients of intervention physicians in several ways 1) Intervention physicians encouraged to give their patients a card during clinic visits with a study specific e‐mail address on it and a description of the triage system and how to use it. 2) flyers mailed to a random sample of 5,000 patients who had visited an intervention doctor in the prior 6 months of the study period or were scheduled to visit an intervention doctor during the study period. The flyers encouraged patients to e‐mail their physician using the special email addresses and educated patients about appropriate content, response times, and message handling by the clinics. 3) intervention physicians were encouraged to forward patient emails from their personal email accounts to the triage account and to encourage patients to use their study‐specific addresses in future correspondence. Control: Physicians did not have access to the EMAIL account. |
|
| Outcomes | Email volume (physician recall of all types of email not just those via EMAIL system) Phone call volume (staff logs) Visit distribution (via medical centre information system) (all measured during 5 two‐week periods spread evenly over the course of the study). Physician opinion on use of email with patients, attitudes towards the benefits of email, how much they are bothered by different types of patient email messages and satisfaction with patient and staff communication (via questionnaire at end of study). |
|
| Notes | Study also featured an end of study patient satisfaction questionnaire, however this was not part of the randomised controlled trial. Participant groups for this survey (intervention and control) were derived from a random sample of 900 patients (450 who had seen an intervention physician 1 or more times and a control physician no more than once during the study period and 450 patients who has seen a control doctor one or more times during the study period and an intervention physician no more than one time during the study period). Therefore these data were not included in the review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The study randomised by half‐day clinic block; all physicians seeing patients during a certain half day window were randomised to treatment or control. This is a cluster randomisation technique. A coin was flipped, assigning 'heads' to treatment, 'tails' to control. |
| Allocation concealment (selection bias) | High risk | Contact with the author confirmed that the study did not conceal the random allocation sequence. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Contact with the author confirmed that staff and investigators were not blind to group assignment. |
| Incomplete outcome data (attrition bias) All outcomes. | High risk | An intention to treat analysis was not carried out. Approximately 20% of physicians did not report patient email volume during waves of data collection, so missing estimates were imputed to 0. The response rate to the physician survey was high (90.8%) however no information was given on characteristics of non‐responders. |
| Selective reporting (reporting bias) | Low risk | Results reported as per the intended outcomes and as outlined in the statistical methods. No published protocol. |
| Other bias | Unclear risk | Baseline comparability: Potential concerns with cluster randomised trials include baseline imbalances between the randomised groups, with regard to individuals and groups. No significant differences were observed between the intervention and control groups at individual level however because the authors were not aware that they had carried out a cluster randomised trial they did not assess comparability at group level. Validation of measures: No information is given on whether the measures are validated. It is unclear whether the utilisation variable created for analysis purposes is validated despite the claim that volume of communication is highly correlated with the level of clinical activity of individual physicians. Reliability of measures: Cronbach's alpha coefficient for internal consistency reliability is presented for the different scales used in the physician survey: 'email benefits scale', 7 items, α=.0.87, 'email bother scale', 8 items, α = 0.87, 'general communication scale', 8 items, α = 0.95. As a higher score means higher reliability, and a score of 0.7 is a recommended threshold for reliability, then the reliability of these scales is acceptable. Recall and reporting bias: For baseline data physicians were asked to self report (recall) number of email messages received directly from patients in the previous 2 weeks. The physician survey was also self‐administered. Information on phone call volume and type of call was collected from staff logs, these may be subject to some reporting unreliability. Contamination: Both groups had access to standard email with their physician throughout the intervention. Independent of the study patients of intervention and control physicians could email their physicians by using the physician's personal email account available through physician's personal cards or by searching the medical centre directory. As there was no valid primary care patient roster the intervention system was promoted to patients who were likely to be those of intervention physicians but some may have been patients of control physicians. |
Katz 2004.
| Methods | Study design: Cluster randomised controlled trial. The study report describes this as a randomised controlled trial. Duration of study: 40 weeks. Recruitment: Invited all practising physicians in the four participating clinics. |
|
| Participants | Description: Physicians (faculty and resident) in internal medicine and family practice in primary care clinics. Setting: Four university affiliated primary care clinics, Michigan, Mid‐West America. There were no inclusion and exclusion criteria. Physician sample consisting of 132 physicians (41 faculty physicians, 91 resident physicians) randomised, 65 to intervention group, 67 to control group. |
|
| Interventions | Intervention: Secure web‐based patient ‐provider communication tool to allow communication with clinic staff. Web site contained educational content addressing appropriate message content, expected response times and message handling by clinic staff. Patients prompted through regular e‐mail to enter the Website to read responses from the staff. Patients of intervention physicians were encouraged to use the Web system through promotion, including cards distributed by intervention physicians and brochures mailed to patient homes. Control: Did not have access to the secure web‐based patient ‐provider communication tool. |
|
| Outcomes | Number and type of web‐messages (from website) . Email volume (physician recall) Telephone call volume by type of call and physician (staff logs) (all measured during a one‐week collection period across the 40 week duration of the study, no detail on frequency of one‐week period) Attitudes toward web and e‐mail communication, preferences for different modes of communication and satisfaction with communication (via physician questionnaire at end of study). |
|
| Notes | Study also featured an end of study patient satisfaction questionnaire, however this was not part of the randomised controlled trial. Participant groups for this survey (intervention and control) were derived from a random sample of 900 patients (425 who had seen an intervention physician 1 or more times and a control physician no more than once during the study period and 425 patients who has seen a control doctor one or more times during the study period and an intervention physician no more than one time during the study period). Therefore this data was not included in the review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The study randomised by half‐day clinic block; all physicians seeing patients during a certain half day window were randomised to treatment or control. This is a cluster randomisation technique. A coin was flipped, assigning 'heads' to treatment, 'tails' to control. |
| Allocation concealment (selection bias) | High risk | Contact with the author confirmed that the study did not conceal the random allocation sequence. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Contact with the author confirmed that staff and investigators were not blind to group assignment. |
| Incomplete outcome data (attrition bias) All outcomes. | High risk | The response rate to the physician survey was 71.2% however no information was given on characteristics of non‐responders. An intention to treat analysis was not carried out. For email volume on average 91.7% of staff physicians responded vs 67.4% of residents. Missing estimates for residents were imputed to zero 'because feedback suggested that these residents had low email use with patients' |
| Selective reporting (reporting bias) | Low risk | Physician preferences for mode of communication for selected health issues are presented for the whole physician sample and not by intervention and control groups. All other outcomes are presented by intervention and control group. |
| Other bias | Unclear risk | Baseline comparability: Potential concerns with cluster randomised trials include baseline imbalances between the randomised groups, with regard to individuals and groups. No significant differences were observed between the intervention and control groups at individual level for the demographic data that is presented (faculty physicians, female sex and mean number of scheduled visits per week) however because the authors were not aware that they had carried out a cluster randomised trial they did not assess comparability at group level. Validation of measures: No information is given on whether the measures are validated. It is unclear whether the utilisation variable created for analysis purposes is validated despite the claim that volume of communication is highly correlated with the level of clinical activity of individual physicians. Reliability of measures: Cronbach's alpha coefficient for internal consistency reliability is presented for the different scales used in the physician survey: 'web benefits scale' 4 items, α =.88, general communication scale, 4 items, α = .82.As a higher score means higher reliability, and a score of 0.7 is a recommended threshold for reliability, then the reliability of these scales is acceptable. Recall and reporting bias: for email volume physicians were asked to recall the number of email messages received directly from patients during the previous week. The physician survey was also self‐administered. Information on phone call volume and type of call was collected from staff logs, these may be subject to some reporting unreliability. |
Kummervold 2004.
| Methods | Study design: Randomised controlled trial. Duration of intervention: 1 year. Recruitment: Recruitment forms were handed out to all adults (18 and over) with a scheduled appointment to see the GP, in the primary clinic's waiting room. Participants not recruited in this way were recruited via posters and flyers in the following month. |
|
| Participants | Description: Patients at a general practice, Tromso, Northern Norway. Setting: Sentrum Legekontor, a general practitioners office in Tromso, Northern Norway. It is a group practice with a City office and two district practices a day a week. The office has 6 doctors, 4 full time, 2 part time, 5 medical secretaries and 7500 patients on practice list. Inclusion criteria were: must have access to the Internet and a personal cell phone. There were no exclusion criteria. 335 participants approached in the waiting room. 126 were eligible and willing to participate. A further 75 recruited via posters/flyers. 1 excluded for medical reasons before randomisation. 200 participants entered the study. 100 participants randomised into the intervention group, 100 into the control group. |
|
| Interventions | Intervention: PasientLink, an electronic messaging system for sending messages between doctors and patients. Intervention participants sent a registered letter with information about the technical solution, user name and password. Patients use a web browser to log in and send patient‐link (secure messaging system) messages to the doctor. Single email interface used to send messages to the doctor. No length/content restriction. Doctors alerted about new messages using a flashing icon on the computer desktop, messages automatically stored in the registry system. Patients notified by text message when doctor responds to their request. Control: Standard care only. |
|
| Outcomes | Differences between groups in the number of telephone/visits to the doctors office (Measured for 1 year before and for the intervention period) Number of online consultations during study period for each patient. (All registered office visits, phone consultations and letters counted by health personnel from system logs). Patients experiences of the scheme (measured at baseline and end of study using questionnaire). Doctors experiences of the scheme (measured qualitatively using interviews after completion of end of study questionnaire). Willingness to pay (WTP) for electronic GP contact (measured at baseline and end of study using specific questions as part of the questionnaire). |
|
| Notes | This study is reported across four publications (Kummervold 2004 & 2008, Bergmo 2005 & 2007). One of the publications was in Norwegian and we had to obtain a translation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants separated into three groups; more than 60 years, women less than 60, men less than 60. A stratified sample was used to ensure equal distribution of males/females and those aged over 60 in the two groups. Each group then centrally randomised into two groups and one randomly chosen to be the intervention group. Randomisation was by drawing of lots. |
| Allocation concealment (selection bias) | High risk | Drew lots and then at the end looked up the numbers from the participation list. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Authors state that blinding 'was not included in the project, but would not have been impossible to accomplish' (Kummervold 2008). |
| Incomplete outcome data (attrition bias) All outcomes. | High risk | An intention to treat analysis was not carried out (although only one participant withdrew post randomisation). Questionnaire: response rate 73% for the intervention group, and 93% for the control group ( 83% of participants in total). Analysis was based on those who completed the survey and the non‐responders are not accounted for. WTP element of questionnaire: response rate 68% for the intervention group and 84% for the control group. Analysis was based on those who completed the survey and the non‐responders are not accounted for. |
| Selective reporting (reporting bias) | Low risk | Results reported as per the intended outcomes and as outlined in the statistical methods. No published protocol. |
| Other bias | High risk | Baseline comparability: A comparison of demographic characteristics is presented and the authors state that there are no significant differences between intervention and control groups for demographic variables but no P values are presented. Validation of measures: No information given on whether the questionnaire was validated. Validation not relevant for other outcomes where information was collected via systems/professionals. Reliability of measures: Questionnaire self‐reported with open‐ended questions which can introduce bias. Performance bias is a potential problem, authors acknowledge this: 'the staff at the practice might have registered clinical activity more conscientiously during the second year of the data collection period than the first due to our intervention'. For the WTP element of the questionnaire the authors eliminated a series of what they describe as 'protest' zeros, but these were determined by the authors and this was not quantitatively decided. Selection bias ‐ all patients had access to the Internet and mobile phones and expressed an interest in participating in electronic communication with their doctor ‐ this would not representative of the general population and such participants may be more sympathetic to the intervention. The GP surgery used was chosen because physicians were positive towards receiving electronic messages from their patients. |
Lin 2005.
| Methods | Study design: Randomised controlled trial. Duration of study: 6 months Recruitment: Recruited via descriptive brochures,a poster and a research assistant in the practice waiting room and via additional brochures in the examination rooms. Two broadcast emails were sent to 6000 employees of the University of Colorado Health Science Center. An article about the study was also distributed to 2000 employees in the hospital's newsletter. |
|
| Participants | Description: Patients at an ambulatory internal medicine practice. Setting: Academic ambulatory internal medicine practice affiliated with the University of Colorado Hospital, Denver, CO, USA. All 14 physicians at the medical practice and participating in the study were already using an electronic medical record (EMR) which included an electronic messaging system to document patients' incoming telephone calls. Inclusions: Patients at least 18 years old, English speaking and having experience using an Internet browser. There were no specified exclusion criteria. 7100 patients visited the clinic during the enrolment period; 606 patients randomised after completing the baseline questionnaire: 305 into the Intervention group, 301 into the control group. |
|
| Interventions | Intervention: 'My Doctor's Office', a patient portal allowing patients to request appointments, prescription refills, specialist referrals and send secure electronic messages to their physicians. Portal patients instructed to register a username and password for the patient portal and asked to register online. Control: usual care, and received access to a website providing general health advice. Received access to the portal after the study ended. All participants could contact the clinic by telephone at their discretion or for urgent messages. Both groups had access to the incoming telephone triage system (for both portal and control patients) via the Electronic Medical Record, and could use standard email to communicate with physicians. Broadcast emails were sent monthly during the study to patients in both groups. |
|
| Outcomes | Not all of the outcomes in this study are relevant to the review but they are listed here for completeness. Primary outcomes:
Secondary outcomes:
|
|
| Notes | Fewer people registered with and used the system than the investigators anticipated despite all intervention participants having access to it. This intervention is multifaceted. Only the outcomes relating to the use of electronic messaging will be of relevance to this review, but all outcomes are outlined here. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Patients consecutively assigned to intervention (access to the portal) or control (usual care) groups by a research assistant according to a predetermined randomisation scheme developed using a statistical software package, with equal numbers of portal and control participants in blocks of 10. |
| Allocation concealment (selection bias) | High risk | The random allocation sequence was not concealed from the research assistant carrying out the randomisation ( as confirmed by communication with author). |
| Blinding (performance bias and detection bias) All outcomes | Low risk | The research assistant conducted the randomisation process and the principal investigators did not see the list of patient group assignments. Authors state that 'physicians and clinic staff could not be blinded to the enrolment status of patients, since patients in the portal group could send messages to physicians through the portal. |
| Incomplete outcome data (attrition bias) All outcomes. | High risk | An intention to treat analysis was not carried out. Numbers of participants lost to follow up in each group are stated and the numbers are comparable: (I = 42, 14%; C = 46, 15%). Throughout the study those who had an invalid email address were 'disenrolled from the study' but no numbers are presented in the report. Response rate to the follow‐up questionnaire was: I = 67%, C = 65%. Authors compared overall satisfaction with care on the baseline survey between participants who completed the study and those who did not (lost to follow up plus those who did not complete final survey). Those not completing were less satisfied on the baseline survey, and this difference was significant. Therefore the least satisfied participants were not in the final analysis and this may have biased the final overall result. There were no significant differences in initial satisfaction between intervention and control groups in those participants completing the study. |
| Selective reporting (reporting bias) | High risk | There is a discrepancy in numbers presented for participants in the intervention group between the study flow chart and the text. The study flow chart reports the number of returned follow up questionnaires as = 175, and the number of participants giving consent to view record = 149. In the text this is reported as returned follow up questionnaire = 174, consent to view record = 148. We are unable to clarify this as the corresponding author informed us that they no longer have access to the primary data to confirm the accuracy of the numbers. The addition of an intervention ‘non‐user’ group to the patient satisfaction outcome as part of the analysis was not pre‐specified. In the text, under the heading ‘qualitative content analysis of administrative requests and clinical messaging’ it is stated that only 95 patients used the portal, and according to table 2 there were 98 non‐portal users in the portal group. Combined this is 193 participants, yet the portal group comprises 175 participants. We are unable to clarify this as corresponding author informed us that they no longer have access to the primary data to confirm the accuracy of the numbers. Where ‘type of message’ is examined, it is between two groups; clinical phone messages and clinical portal messages. This is a subgroup analysis based on participants who returned the follow‐up questionnaire and consented for investigators to review their medical record and who had a completed clinical message exchange (as defined by the study investigators). It constitutes only around half of the originally randomised participants in each group and no information is given on these participants, nor how they compare to those not responding to the follow up questionnaire, those not consenting, and those not fulfilling the definition of completed clinical message exchange. The assessment of clinical messages only completed clinical messages are included and those encompassing routine prescription refills, appointment requests and referral requests are excluded. For the value to patients outcome, data are presented for the whole sample and not by group (portal versus control). The corresponding author informed us that this was a 'peripheral part of our study and we elected not to break apart the responses for portal versus control. Most responses were “ZERO” and those who were willing to pay varied from a few pennies to $25, and it did not appear to be different between groups.' |
| Other bias | High risk | Baseline comparability: there were no significant differences between the intervention and control group with regard to age, gender, education and income. Validation of measures: The patient satisfaction survey was adapted from prior instruments by the investigators .References given to prior instrument in two studies, but these are not validated instruments. The surveys were piloted in non study patients. Where clinical messages were divided into categories, categories were from a previously published validated taxonomy of clinical requests, however the author added categories for the purpose of the study. Value to patients element of the survey not validated. Reliability of measures: Survey was piloted first which increases potential reliability. The patient satisfaction questionnaire was self‐administered and used Likert scales, these are subjective measures. The questionnaire was carried out online and it is not clear whether the control group definitely have access to the Internet. Contamination: the authors state in the discussion ' control group patients who continued emailing their physician may have diluted the difference between groups' Participant bias: A third of participants were employees of the Hospital and 70% were college graduates. This could have several effects on the study; 1) the sample is a very select population and therefore not likely to be generalisable. The authors raise this in the discussion ' results may not be generalisable to an Internet‐naive, less affluent sample.' 2) Being an employee of the hospital may influence the way the participant approaches use of the service and the way in which they answer the questionnaire, they may wish to please the researchers and this may introduce bias into the answers. |
MacKinnon 1995.
| Methods | Study design: Pretest‐post‐test control group design with random assignment. Three time points, pretest, 3 months and post‐test (the study design meets the criteria for RCT design). Duration of study: 6 months. Recruitment: Subjects existing clients of the service and asked to participate (if eligible). |
|
| Participants | Description: Caregivers and children/young adults with physical disability attending the rehabilitation centre. Setting: Augementative Communication Service at Thames Valley Children's Centre. A rehabilitation centre for children and young adults with physical disabilities serving southwestern Ontario, Canada. Inclusions: Clients must have been involved with the augmentative communication service for at least 4 months, be physically able to use a computer and modem for written communication purposes as determined by clinic staff, have had a home computer system available for at least a 3‐month period, and with a working knowledge of a word processing program. There were no specified exclusion criteria. Twenty‐five individuals met the inclusion criteria, 17 (68%) agreed to participate. 17 participants were randomised, 8 to the intervention, 9 to the control. After assignment one individual dropped out of the intervention group due to technical difficulties, leaving 16 participants, 7 in the intervention group, 9 in the control group. |
|
| Interventions | Augmentative Communication Service staff provided a communication service which included all types of communication. Intervention: Participants asked to make all of their contacts to the augmentative communication service by electronic mail via the disability information service of Canada (DISC) telecommunications system. A presentation oriented the subjects to the use of the electronic mail feature of the DISC telecommunications system. Each participant received a demonstration, a full DISC users manual and a set of reduced instructions for easy reference. A home installation visit was then conducted; operational aspects of using electronic mail were reviewed. Participants asked to make one independent contact to the augmentative communication service within 48 hours of the home installation. Study made use of the subjects' existing computer systems, which were prescribed through the Ontario government's funding system. Control: Continued to contact the augmentative communication system in their usual manner: letter,telephone, and/or site visit and did not receive any equipment to access the service. Long distance calls were covered within the project's budget to ensure that the cost of contacting the service did not deter control subjects from initiating contact. |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Report states that 'the 17 consenting individuals were randomly assigned to the experimental or control groups'. Authors informed us that names were drawn randomly by someone not involved in the research. |
| Allocation concealment (selection bias) | Unclear risk | No information is given in the report or by authors on the nature of concealment other than names being drawn randomly. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Pre‐study satisfaction questionnaire administered to all subjects by research assistant not associated with the service. Staff responding to messages were not blinded to the allocation, this was confirmed by contact with authors who told us that staff interacted with all subjects as part of their day to day work. Authors state 'for procedural reasons subjects therefore were aware of their random assignment to condition at the time that they completed the first satisfaction questionnaire.' Authors state in discussion when suggesting reasons for the lack of effect of the intervention: 'initially inflated satisfaction ratings for the experimental group due to knowledge that they would be receiving the electronic mail service (a bias in the design of the study.)' |
| Incomplete outcome data (attrition bias) All outcomes. | High risk | An intention to treat analysis is not carried out .One intervention participant dropped out post randomisation and the reason is given; technical difficulties. The method of contact for independent contacts in the intervention group was recorded only for 24 of 32 contacts. Authors confirmed via contact that this omission was because clinicians did not specify this information on the contact forms they were required to complete. |
| Selective reporting (reporting bias) | Low risk | The outcomes listed in the 'procedure' section are represented in the results section. |
| Other bias | High risk | During the fifth month of the study the network agency (DISC) made a major change to their computer system and directions for usage had to be reissued. Some participant computers required technical/software changes.In the results the authors saw a drop in the number of independent contacts by the intervention group at the point where DISC changed the system set up and organisation. They speculate that without this interruption which involved orientation and system set up, ' a plateau might have been seen in the number of independent contacts by the experimental group as was the case for the number of contacts. Authors also state that 'the unforeseen technical problems likely affected subjects' attitudes towards electronic mail and its potential use, and may have affected the primary outcome of interest.' These unforeseen problems may feasibly have affected the effect size. Baseline comparability: Investigators measured receptive vocabulary (measured at baseline using Peabody Picture Vocabulary Test‐Revised (PPVT‐R)) and there was no significant difference between the two groups in their mean age equivalence scores. Validity of measures: PPVT‐R is a validated questionnaire. Seven references are provided on its use and adaptation for non‐speakers (of which there are 5 in the study). No information given on the satisfaction questionnaire and whether it was validated. Reliability of measures: The baseline PPVT‐R was administered face‐to face by a qualified speech/language pathologist. The patient satisfaction questionnaire was administered to all subjects by a research assistant not associated with the augmentative communication service. The satisfaction questionnaires were carried out either face‐to‐face or over telephone. The different delivery methods may have led to differing responses. Number of contacts data relies on self‐report by staff (contact forms) and this introduces a risk of bias, especially given that staff were not blinded to group allocation. |
Ross 2004.
| Methods | Study design: Randomised controlled trial. Duration of study: 1 year Recruitment: Initial approach involved sending a recruitment letter explaining the study was sent to eligible patients. Secondary approach involved a research assistant approaching patients in the waiting room of the practice, asking them if they would be interested in reading their medical records online in the context of a study. |
|
| Participants | Description: Heart failure patients attending a speciality clinic. Setting: Speciality clinic for heart failure, University of Colorado Hospital, US. Majority of patients in the practice have New York Heart Association Class II or Class III symptoms of heart failure. Inclusions: followed in the practice, speak English and 18 years of age or older. Participants needed to have used a web browser before. Exclusions; physicians, nurses, physician assistants and nurse practitioners as not typical users. In total 394 patients were approached to participate, 312 received the mailing prior to the recruitment period and 82 presented to the clinic during the recruitment period without receiving the mailing. Of these, 287 declined access to online medical records, 144 returned the baseline survey before declining. In total 107 (27% of eligible) participants were randomised; 54 into the intervention group, 53 into the control group. |
|
| Interventions | Intervention: SPPARO (System Providing Patients Access to Records Online). Three components to SPPARO; medical record, educational guide and messaging system. Participants given user identification and password and a written user guide to the system. The messaging system allowed patients to exchange secure messages with the nursing staff in the practice. Patients were reminded to call the research assistant if they had problems using SPPARO. Control: Patients in control group continued to receive standard care in the practice and were offered use of SPARRO after the study was completed as an incentive to participate. Co‐interventions: all participants will have seen the guide in one form or another as the educational guide is an online version of the printed materials that all patients in the heart failure practice receive at their first visit. Periodic messages were sent by the research staff to all participants ‐ they were informed about upcoming surveys and encouraged to contact the research assistant if they had a change of address or telephone number |
|
| Outcomes | Not all outcomes were relevant to the review but are listed here for completeness. Primary outcome:
Other outcomes:
Outcomes relevant to review:
|
|
| Notes | This intervention is multifaceted. Only the outcomes relating to the use of secure messaging will be of relevance to this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | As initial questionnaires were received patients were consecutively assigned identification numbers that were linked to either intervention or control group according to a predefined computer‐generated randomisation scheme. Randomisation was restricted so that equal numbers of patients were assigned to the intervention and control groups in blocks of 10. |
| Allocation concealment (selection bias) | Low risk | Sequential sealed envelopes were used. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Investigators (PI and data analyst) were blind to group allocation. Participants were blind to group allocation when they completed the baseline questionnaire: 'when patients completed the initial questionnaire they were blinded to their enrolment status.' Staff administering the service were blind to group allocation: 'physicians and practice staff not told which patients were enrolled into the study. They could become aware of a patient's enrolment status, however, if a patient directly mentioned using it, or if a patient sent an electronic message using SPPARO.' |
| Incomplete outcome data (attrition bias) All outcomes. | Low risk | Participant attrition is acknowledged and reasons for drop‐outs are given. An intention to treat analysis is not carried out, however statistical methods are used to account for missing participants in the analysis for the scored questionnaire items (repeated measures analysis) across all outcomes. Repeated measures analysis involved using baseline data for censored individuals and using association data from uncensored individuals to provide an estimate. This implicitly assumed that the associations observed among the baseline, 6‐month, and 12‐month measures in the uncensored subjects would have been observed in the censored subjects. |
| Selective reporting (reporting bias) | High risk | All outcomes are addressed in the results section of this study, however not all values are reported, for example; P value is provided for the number of messages sent per patient but the actual number of messages is not presented. Categories of messages sent using SPPARO are presented graphically for the whole sample and not by group. Information in the text states that there was no significant difference between groups for category of message but the P values are not presented, nor the data for category by group. |
| Other bias | Low risk | Baseline comparability: Baseline demographic statistics are presented for both intervention and control groups, but then the overall sample is compared statistically to the decliners group rather than by group assignment. The authors state in the results that 'at baseline, the intervention and control groups did not differ in their socio‐economic characteristics, or in their health status as assessed by the KCCQ symptom score.' Validity of measures: Authors 'used previously validated survey instruments where available.' KCCQ for self‐efficacy required a change of 7.7 on the scaled score as the minimally clinically significant difference in this measure. This was based on a validation study of the KCCQ which found mean difference in self‐efficacy score during and 3 months after hospitalisation for congestive heart failure was 15.4 points, for this study criterion of clinical significance set to be half this difference. Art of Medicine questionnaire, Morisky and MOS tools are validated. No information given on how messages were categorised or how the categories were devised. Reliability of measures: Potential response and recall bias: all questionnaire were self‐administered. Phone messages were tracked by asking nurses to keep logs and by referring to medical record. This may introduce some unreliability. Generalisability: study investigators identified 288 patients who did not enrol in the primary study and of these144 completed a 'decliners survey'. There was found to be no difference in socioeconomic characteristics and health status assessed by the KCCQ symptom score between decliners and participants. Therefore the study population is a good representation of the practice population. |
Stalberg 2008.
| Methods | Study design: Prospective randomised controlled clinical trial Duration of study: rolling, with final outcome assessment administered following the first postoperative consultation of each patient. Recruitment: All patients referred to single surgeon for thyroid or parathyroid surgery during the study were randomised into the study (those older than the age limits subsequently excluded). |
|
| Participants | Description: Patients referred for thyroid or parathyroid surgery. Setting: Peri‐operative surgical setting for head and neck surgery, tertiary referral centre, Australia Inclusions: Aged 18 to 65, able to access to the Internet at work as well as at home (authors link Internet access at work to being of working age and so exclude those people above retirement age). Patients randomised until number meeting inclusion criteria (≤ 65 years of age) was 50 in intervention group and 50 in control group. Two participants in intervention group and one in the control group did not proceed to surgery leaving 48 in intervention group and 49 in control group. |
|
| Interventions | Co‐intervention: all participants in the study received a standardised approach to information including a detailed discussion of the indications, risks and complications of thyroid/parathyroid surgery, a hand drawn diagram detailing the proposed procedure, copy of the Royal Australasian College of Surgeons brochure entitled "Patient Guide on Surgery of the Thyroid Gland and Parathyroid Glands". All participants were given a typed sheet entitled 'If you have further questions about your operation' which emphasised the need for participants to have any outstanding issues or questions addressed or explained before the date of surgery. Intervention: On the typed sheet, the sheet listed in order ‐ surgeon's email address, office telephone number, office fax number and office mailing address and participants were informed by the surgeon that e‐mail was the preferred mode of communication. Control: On the typed sheet the email address was not present and participants did not receive the verbal statement about email being the preferred method of communication. |
|
| Outcomes | Numbers, age and sex distribution of patients using any form of communication with the surgeon in the perioperative period outside of the routine booked consultations (via patient files at end of study period). Method of communication used (via patient files at end of study period). Number of emails per patient, content of the emails, origin of the email (patient, relative etc) (emails printed out and placed in patient file and examined at end of study period). Patient satisfaction (via questionnaire administered during the first post‐operative consultation). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Investigator confirmed 'sealed envelopes with equal numbers of envelopes containing “email” or “no email”. Envelopes were handed out to every patient at consultation and after exclusion of patients based on age limits, randomisation was terminated when 50 patients had been acquired in each group.' |
| Allocation concealment (selection bias) | Low risk | Investigator confirmed 'Envelopes were opened by the surgeon at the time of consultation after the provision of information session' |
| Blinding (performance bias and detection bias) All outcomes | High risk | Investigators were not blind to the group assignment of participants. Investigators had access to the patient notes which contained the randomisation. It was not possible to blind patients to allocation owing to the nature of the intervention. |
| Incomplete outcome data (attrition bias) All outcomes. | High risk | An intention to treat analysis was carried out for all outcomes other than patient satisfaction. An intention to treat analysis could not be carried out on the patient satisfaction outcome as the patients not proceeding to surgery did not complete the post‐operative questionnaire. Additionally, the response rate to the questionnaire was 76% (Intervention: 77%, Control: 76%) and there is no exploration of non‐responders. |
| Selective reporting (reporting bias) | Low risk | There is no evidence of selective outcome reporting. |
| Other bias | High risk | Baseline comparability: study states 'no statistically significant difference between the 2 groups with respect to either age distribution or sex distribution (P = 0.18)' Validation of measures: Confirmation obtained from investigator that patient satisfaction questionnaire was not validated. Validation not relevant for other outcomes. Reliability of measures: both response and recall bias are possible with a self‐completed patient questionnaire. Other outcomes measured via collation of emails from each participant. Authors use age as a proxy for Internet access at work which may exclude those aged over 65 and still working. No rationale is given for why both work and home Internet access was required for participation. Contamination: Study states that control participants would still have had access to the surgeon's email address, which was available on the appointment card as well as on the Australian Endocrine Surgeons Web site, although attention was not specifically drawn to it. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Carlbring 2006 | Multifaceted Internet intervention with an email component. The effects of email are not individually reported. |
| Ezenkwele 2003 | This study compares email with telephone for follow‐up after an emergency department visit. The intervention email requires a one off response from the participants. It does not constitute two‐way communication for communicating clinical concerns. |
| Goldman 2004 | This study compares email with telephone for follow‐up after a paediatric emergency department visit. The intervention email requires a one off response from the participants. It does not constitute a two‐way communication for communicating clinical concerns. |
| Hanauer 2009 | This study assesses the use of email reminders to support diabetes management. This was a multi‐faceted intervention comprising a web‐based module and a messaging/reminder module designed to run autonomously. Communication was between the participant and the web system. The communication was not with a healthcare professional. |
| Klein 2006 | This study assesses the effect of Internet‐based cognitive behavioural therapy. One of the three interventions had an email component. However the effects of email are not individually reported. |
| Klein 2009a | This study compares two interventions each offering differing frequencies of email support (1 email per week versus 3 emails per week). |
| Klein 2009b | Multifaceted Internet intervention with an email component. The effects of email are not individually reported. |
| Leong 2005 | Despite being described as a study with an intervention and control group, the authors acknowledge that participants were not randomised, 'thereby creating uncertainty regarding the effects of the intervention'. Therefore this study does not meet the inclusion criteria for type of study in this review. |
| Leveille 2009 | 'Patientsite' Internet portal based intervention. Multifaceted intervention. This study is focused on content of emails (aimed towards behaviour change) rather than email itself. The control group also received emails, but with different content. The two groups were then compared. |
| Pier 2008 | This study had a natural groups design (participants assigned into groups according to how they learned of the programme) and so it did not meet the inclusion criteria for type of study, despite being described as a controlled trial. |
| Tate 2003 | This study compared an Internet intervention to an Internet intervention with behavioural e‐counselling. The behavioural e‐counselling consisted of two‐way email communication between counsellor and participant, however there was an additional element to the e‐counselling intervention in the form of daily diaries submitted by participants. Therefore the effects reported cannot be solely attributed to the email component. |
Characteristics of ongoing studies [ordered by study ID]
Ruland NCT00971139.
| Trial name or title | Implementing Online Patient‐Provider Communication Into Clinical Practice (OPPC) |
| Methods | RCT (Parallel) |
| Participants | Inclusion Criteria:
Exclusion Criteria:
The investigators will include patients with various diagnoses from heterogeneous practice settings to increase external validity. |
| Interventions | Access to the online patient‐provider communication (OPPC) service. A service where patients can ask questions and receive advice and support from care providers and social counsellors. |
| Outcomes | Primary Outcome :
Secondary Outcomes:
|
| Starting date | November 2009 |
| Contact information | Cornelia M Ruland, PhD. Oslo University Hospital. cornelia.ruland@rr‐research.no Cecilie Varsi, MS. Oslo University Hospital. cecilie.varsi@rr‐research.no |
| Notes | This study is currently recruiting participants. March 2011 is the final data collection date for the primary outcome measure. The anticipated completion date is 21/12/2011. |
Simon NCT00755235.
| Trial name or title | Feasibility of Depression Care Management via E‐mail |
| Methods | RCT (Parallel) |
| Participants | Inclusion Criteria
Exclusion criteria
|
| Interventions | Participants will receive depression care management by secure messaging. Participants will receive electronic messages welcoming them and monitoring their antidepressant treatment. Care managers will use monitoring data to aid participants' physicians, coordinate physician follow‐ups, facilitate emergency care, and facilitate specialty referrals. Care managers will also provide motivation and education to participants. |
| Outcomes | Primary Outcome:
Secondary Outcome:
|
| Starting date | April 2009 |
| Contact information | Gregory E Simon, MD, MPH. Group Health Cooperative Center for Health Studies. simon.g@ghc.org |
| Notes | This study is completed and pending submission for publication by the authors. |
Differences between protocol and review
Background
We have amended the Background section of the review since the protocol stage, to update the cited literature (Atherton 2010).
Methods
Type of interventions
While the content has not been changed, we have clarified the information on multifaceted interventions and interventions for general use, in line with the interpretation of this information in the review.
Search methods for identification of studies
We stated in the protocol (Atherton 2010) that we would search the following databases as part of the grey literature search:
Dissertation Abstracts (North American and European theses) via British Library
TrialsCentralTM (www.trialscentral.org)
We did not search these databases, after discussion with the Review Group. TrialsCentral TM was unsearchable; the website seemed only to pull information in from other sources. The only search options were to search by condition or intervention for clinical and drug interventions only (no free text). We did not search Dissertation Abstracts as several of the other databases would duplicate this search (Index to Theses, ProQuest).
MEDLINE search
We made minor changes to the MEDLINE search strategy since the protocol stage (Atherton 2010) in conjunction with the Review Group's Trials Search Coordinator; we present the latest version at Appendix 3. The changes involve the removal of the term 'on‐line' from the strategy. This is because OvidSP MEDLINE changed the way it processed this term, and we were retrieving a very high number of articles (20,000+) whereas before the change in processing we had obtained around 8000. Removing this term brought the retrieval rate back down to acceptable levels.
Unit of analysis issues
Owing to the nature of the included studies, we added material to the Unit of analysis issues section.
Measures of treatment effect
Owing to the nature of the included studies being different to that presumed at the time of writing the protocol, we added material to the Measures of treatment effect section.
Data synthesis
We changed the Data synthesis section to accommodate the type of data identified in this review. We present details of methods that will be used if meta‐analysis is possible in future updates of the review, in Appendix 2.
Contributions of authors
Helen Atherton wrote the protocol, carried out the search, carried out data extraction and analysis and wrote the review.
Prescilla Sawmynaden assisted with the search, was second reviewer and data extractor, assisted in analysis and co‐wrote the review.
Aziz Sheikh commented on drafts of the review.
Azeem Majeed commented on drafts of the review.
Josip Car conceived the idea for the review and supervised the production.
Sources of support
Internal sources
-
Department of Primary Care and Public Health, Imperial College London, UK.
The review received a partial financial contribution from The Department of Primary Care and Public Health, Imperial College London. The Department of Primary Care & Public Health at Imperial College is grateful for support from the NIHR Collaboration for Leadership in Applied Health Research & Care (CLAHRC) Scheme, the NIHR Biomedical Research Centre scheme, and the Imperial Centre for Patient Safety and Service Quality.
External sources
-
Medical Research Council, UK.
HA was the recipient of a Medical Research Council PhD Studentship, administered by Imperial College, London, UK (October 2008‐2011).
-
NHS Connecting for Health Evaluation Programme (NHS CFHEP 001), UK.
http://www.haps.bham.ac.uk/publichealth/cfhep/
-
National School of Primary Care Research, UK.
HA is the recipient of a research fellowship from the National School of Primary Care Research (from January 2012) at the University of Oxford
Declarations of interest
None known.
New
References
References to studies included in this review
Bergmo 2009 {published and unpublished data}
- Bergmo TS, Wangberg SC, Schopf TR, Solvoll T. Web‐based consultations for parents of children with atopic dermatitis: results of a randomized controlled trial. Acta Paediatrica 2009;98:316‐20. [DOI] [PubMed] [Google Scholar]
Digenio 2009 {published and unpublished data}
- Digenio AG, Mancuso JP, Gerber RA, Dvorak RV. Comparison of methods for delivering a lifestyle modification program for obese patients: a randomized trial. Annals of Internal Medicine 2009;150:255‐62. [DOI] [PubMed] [Google Scholar]
Katz 2003 {published and unpublished data}
- Katz SJ, Moyer CA, Cox DT, Stern DT. Effect of a triage‐based e‐mail system on clinic resource use and patient and physician satisfaction in primary care: a randomized controlled trial. Journal of General Internal Medicine 2003;18(9):736‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyer CA, Katz SJ, Williams B, Stern DT. The effect of facilitated e‐mail access on patient and resident physician communication and satisfaction. 15th Annual Meeting of the International Society of Technology Assessment in Health Care. 1999:40.
Katz 2004 {published data only}
- Katz SJ, Nissan N, Moyer CA. Crossing the digital divide: evaluating online communication between patients and their providers. The American Journal of Managed Care 2004;10:593‐8. [PubMed] [Google Scholar]
Kummervold 2004 {published and unpublished data}
- Bergmo TS, Kummervold PE, Gammon D, Dahl LB. Electronic patient‐provider communication: will it offset office visits and telephone consultations in primary care?. International Journal of Medical Informatics 2005;74:705‐10. [DOI] [PubMed] [Google Scholar]
- Bergmo TS, Wangberg SC. Patients' willingness to pay for electronic communication with their general practitioner. The European Journal of Health Economics: HEPAC: Health Economics in Prevention and Care 2007;8:105‐10. [DOI] [PubMed] [Google Scholar]
- Kummervold PE. Internet‐Based Patient Communication. Dissertation for the degree of Philosophiae Doctor. University of Tromso, Faculty of Medicine, Institute of Clinical Medicine 2008.
- Kummervold PE, Trondsen M, Andreassen H, Gammon D, Hjortdahl P. Patient‐physician interaction over the internet [Erfaringer med lege‐pasient‐kontaktover Internett]. Tidsskrift for den NorskeLaegeforening 2004;124(20):2633‐6. [PubMed] [Google Scholar]
Lin 2005 {published data only}
- Lin CT, Wittevrongel L, Moore L, Beaty BL, Ross SE. An Internet‐based patient‐provider communication system: randomized controlled trial. Journal of Medical Internet Research 2005;7(4):e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
MacKinnon 1995 {published data only}
- MacKinnon E, King G, Cathers T, Scott J. Electronic mail: service from afar for individuals with physical disabilities. Augmentative & Alternative Communication 1995;11(4):236‐43. [Google Scholar]
Ross 2004 {published data only}
- Ross SE, Moore LA, Earnest MA, Wittevrongel L, Lin CT. Providing a web‐based online medical record with electronic communication capabilities to patients with congestive heart failure: randomized trial. Journal of Medical Internet Research 2004;6:e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stalberg 2008 {published data only}
- Stalberg P, Yeh M, Ketteridge G, Delbridge H, Delbridge L. E‐mail access and improved communication between patient and surgeon. Archives of Surgery 2008;143:164‐8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Carlbring 2006 {published data only}
- Carlbring P, Furmark T, Steczko J, Ekselius L, Andersson G. An open study of internet‐based bibliotherapy with minimal therapist contact via email for social phobia. Clinical Psychologist 2006;10(1):30‐8. [Google Scholar]
Ezenkwele 2003 {published data only}
- Ezenkwele UA, Sites FD, Shofer FS, Pritchett EN, Hollander JE. A randomized study of electronic mail versus telephone follow‐up after emergency department visit. Journal of Emergency Medicine 24;2:125‐30. [DOI] [PubMed] [Google Scholar]
Goldman 2004 {published data only}
- Goldman RD, Mehrotra S, Pinto TR, Mounstephen W. Follow‐up after a pediatric emergency department visit: telephone versus e‐mail?. Pediatrics 2004;114:988‐91. [DOI] [PubMed] [Google Scholar]
Hanauer 2009 {published data only}
- Hanauer DA, Wentzell K, Laffel N, Laffel LM. Computerized Automated Reminder Diabetes System (CARDS): E‐mail and SMS cell phone text messaging reminders to support diabetes management. Diabetes Technology and Therapeutics 2009;2:99‐106. [DOI] [PMC free article] [PubMed] [Google Scholar]
Klein 2006 {published data only}
- Klein B, Richards JC, Austin DW. Efficacy of internet therapy for panic disorder. Journal of Behavior Therapy and Experimental Psychiatry 2006;37:213‐38. [DOI] [PubMed] [Google Scholar]
Klein 2009a {published data only}
- Klein B, Mitchell J, Gibson K, Shandley K, Austin D, Kiropoulos L, et al. A therapist‐assisted Internet‐based CBT intervention for post traumatic stress disorder: Preliminary results. Cognitive Behaviour Therapy 2009;38(2):121‐31. [DOI] [PubMed] [Google Scholar]
Klein 2009b {published data only}
- Klein B, Austin D, Pier C, Kiropoulos L, Shandley K, Mitchell J, et al. Internet‐based treatment for panic disorder: Does frequency of therapist contact make a difference?. Cognitive Behaviour Therapy 2009;38(2):100‐13. [DOI] [PubMed] [Google Scholar]
Leong 2005 {published data only}
- Leong SL, Gingrich D, Lewis PR, Mauger DT, George JH. Enhancing doctor‐patient communication using email: a pilot study. Journal of the American Board of Family Practice 2005;18(3):180‐88. [DOI] [PubMed] [Google Scholar]
Leveille 2009 {published data only}
- Leveille SG, Huang A, Tsai SB, Allen M, Weingart SN, Iezzoni LI. Health coaching via an internet portal for primary care patients with chronic conditions: a randomized controlled trial. Medical Care 2009;47:41‐7. [DOI] [PubMed] [Google Scholar]
Pier 2008 {published data only}
- Pier C, Austin DW, Klein B, Mitchell J, Schattner P, Ciechomski L, et al. A controlled trial of Internet‐based cognitive‐behavioural therapy for panic disorder with face‐to‐face support from a general practitioner or email support from a psychologist. Mental Health in Family Medicine 2008;5(1):29‐39. [PMC free article] [PubMed] [Google Scholar]
Tate 2003 {published data only}
- Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a randomized trial. Journal of the American Medical Association 2003;289:1833‐6. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Ruland NCT00971139 {published data only}
- Implementing Online Patient‐Provider Communication Into Clinical Practice (OPPC). Ongoing study November 2009.
Simon NCT00755235 {unpublished data only}
- Feasibility of Depression Care Management via E‐mail. Ongoing study April 2009.
Additional references
Abbott 2002
- Abbott KC, Mann S, DeWitt D, Youngblood SL, Kennedy S, Poropatich RK. Physician‐to‐physician consultation via electronic mail: The Walter Reed Army Medical Center ask a doc system. Military Medicine 2002;167(3):200‐4. [PubMed] [Google Scholar]
Adamson 2010
- Adamson SC, Bachman JW. Pilot study of providing online care in a primary care setting.. Mayo Clinic Proceedings 2010;85(8):704‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Atherton 2012
- Atherton H, Sawmynaden P, Meyer B, Car J. Email for the coordination of healthcare appointments and attendance reminders. Cochrane Database of Systematic Reviews 2012, Issue 8. [DOI: 10.1002/14651858.CD007981.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Balas 1997
- Balas EA, Jaffrey F, Kuperman GJ, Boren SA, Brown GD, Pinciroli F. Electronic communication with patients. Evaluation of distance medicine technology. Journal of the American Medical Association 1997;278:152‐9. [PubMed] [Google Scholar]
Bergmo 2005
- Bergmo TS, Kummervold PE, Gammon D, Dahl LB. Electronic patient‐provider communication: will it offset office visits and telephone consultations in primary care?. International Journal of Medical Informatics 2005;74(9):705‐10. [DOI] [PubMed] [Google Scholar]
Bitter 2000
- Bitter J. E‐mail in medical practice: legal and ethical concerns. QRC Advisor 2000;16(3):1‐8. [PubMed] [Google Scholar]
Brooks 2006
- Brooks RG, Menachemi N. Physicians' use of email with patients: factors influencing electronic communication and adherence to best practices. Journal of Medical Internet Research 2006;8(1):e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2004
- Campbell MK, Elbourne DR, Altman DG. CONSORT statement: extension to cluster randomised trials. BMJ 2004;328(7441):702‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Car 2004a
- Car J, Sheikh A. Email consultations in health care: 1. scope and effectiveness. BMJ 2004;329(7463):435‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Car 2004b
- Car J, Sheikh A. Email consultations in health care: 2. acceptability and safe application. BMJ 2004;329(7463):439‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Car 2008a
- Car J, Black A, Anandan C, Cresswell K, Pagliari C, McKinstry B, et al. The impact of eHealth on the quality and safety of healthcare. http://www1.imperial.ac.uk/resources/4565EF18‐662B‐448B‐90C2‐E7372B4C2E09/ 2008. [DOI] [PMC free article] [PubMed]
Car 2012
- Car J, Gurol‐Urganci I, Jongh T, Vodopivec‐Jamsek V, Atun R. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database of Systematic Reviews 2012, Issue 7. [DOI: 10.1002/14651858.CD007458.pub2] [DOI] [PubMed] [Google Scholar]
Castren 2005
- Castren J, Niemi M, Virjo I. Use of email for patient communication in student health care: a cross‐sectional study. BMC Medical Informatics and Decision Making 2005;5(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Couchman 2001
- Couchman GR, Forjuoh SN, Rascoe TG. E‐mail communications in family practice: what do patients expect?. The Journal of Family Practice 2001;50(5):414‐8. [PubMed] [Google Scholar]
de Jongh 2012
- Jongh T, Gurol‐Urganci I, Vodopivec‐Jamsek V, Car J, Atun R. Mobile phone messaging for facilitating self‐management of long‐term illnesses. Cochrane Database of Systematic Reviews 2012, Issue in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dixon 2010
- Dixon RF. Enhancing primary care through online communication.. Health Affairs 2010;29(7):1364‐9. [DOI] [PubMed] [Google Scholar]
Dunbar 2003
- Dunbar PJ, Madigan D, Grohskopf LA, Revere D, Woodward J, Minstrell J, et al. A two‐way messaging system to enhance antiretroviral adherence. Journal of the American Medical Informatics Association 2003;10(1):11‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ellis 1999
- Ellis JE, Klock PA, Mingay DJ, Roizen MF. Use of electronic mail for postoperative follow‐up after ambulatory surgery. Journal of Clinical Anesthesia 1999;11(2):136‐9. [DOI] [PubMed] [Google Scholar]
Freed 2003
- Freed DH. Patient‐physician e‐mail: passion or fashion?. Health Care Manager 2003;22(3):265‐74. [DOI] [PubMed] [Google Scholar]
Fridsma 1994
- Fridsma DB, Ford P, Altman R. A survey of patient access to electronic mail: attitudes, barriers, and opportunities. Proceedings of the Annual Symposium on Computer Applied Medical Care 1994:15‐9. [PMC free article] [PubMed] [Google Scholar]
Gaster 2003
- Gaster B, Knight CL, DeWitt DE, Sheffield JV, Assefi NP, Buchwald D. Physicians' use of and attitudes toward electronic mail for patient communication. Journal of General Internal Medicine 2003;18(5):385‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goodyear‐Smith 2005
- Goodyear‐Smith F, Wearn A, Everts H, Huggard P, Halliwell J. Pandora's electronic box: GPs reflect upon email communication with their patients. Informatics in Primary Care 2005;13(3):195‐02. [DOI] [PubMed] [Google Scholar]
Gordon 2003
- Gordon C, Krimholtz M. E‐mail and patients: a medicolegal minefield. Lancet 2003;362(9397):1768. [DOI] [PubMed] [Google Scholar]
GRADE 2010
- GRADE. Examples, tools and presentations. http://www.gradeworkinggroup.org/toolbox/index.htm 2010 [Accessed 01/07/12]. [Google Scholar]
Gurol‐Urganci 2012
- Gurol‐Urganci I, Jongh T, Vodopivec‐Jamsek V, Car J, Atun R. Mobile phone messaging for communicating results of medical investigations. Cochrane Database of Systematic Reviews 2012, Issue 6. [DOI: 10.1002/14651858.CD007456.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2008
- Guyatt H, Oxman AD, Vist GE, Kunz R, Falck‐Y Y, Onso‐Coello P, et al. for the GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harris 2006
- Harris Interactive. Few patients use or have access to online services for communicating with their doctors, but most would like to. www.harrisinteractive.com/news/allnewsbydate.asp?NewsID=1096 2006.
Hassol 2004
- Hassol A, Walker JM, Kidder D, Rokita K, Young D, Pierdon S, et al. Patient experiences and attitudes about access to a patient electronic health care record and linked web messaging. Journal of the American Medical Informatics Association 2004;11(6):505‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1. www.cochrane‐handbook.org 2008.
Hilty 2006
- Hilty DM, Yellowlees PM, Cobb HC, Neufeld JD, Bourgeois JA. Use of secure e‐mail and telephone: psychiatric consultations to accelerate rural health service delivery. Telemedicine and e‐Health 2006;12:490. [DOI] [PubMed] [Google Scholar]
Hobbs 2003
- Hobbs J, Wald J, Jagannath YS, Kittler A, Pizziferri L, Volk LA, et al. Opportunities to enhance patient and physician e‐mail contact. The Internet Journal of Medical Informatics 2003;70(1):1‐9. [DOI] [PubMed] [Google Scholar]
Houston 2003
- Houston TK, Sands DZ, Nash BR, Ford DE. Experiences of physicians who frequently use e‐mail with patients. Health Communication 2003;15(4):515‐25. [DOI] [PubMed] [Google Scholar]
Kassirer 2000
- Kassirer JP. Patients, physicians, and the Internet. Health Affairs 2000;19(6):115‐23. [DOI] [PubMed] [Google Scholar]
Katzen 2005
- Katzen C, Solan MJ, Dicker AP. E‐mail and oncology: a survey of radiation oncology patients and their attitudes to a new generation of health communication. Prostate Cancer Prostatic Disease 2005;8(2):189‐93. [DOI] [PubMed] [Google Scholar]
Kleiner 2002
- Kleiner KD, Akers R, Burke BL, Werner EJ. Parent and physician attitudes regarding electronic communication in pediatric practices. Pediatrics 2002;109(5):740‐4. [DOI] [PubMed] [Google Scholar]
Kummervold 2008
- Kummervold PE. Internet‐Based Patient Communication. University of Tromso 2008.
Lacher 2000
- Lacher D, Nelson E, Bylsma W, Spena R. Computer use and needs of internists: a survey of members of the American College of Physicians‐American Society of Internal Medicine. Proceedings of the American Medical Informatics Association Symposium 2000:453‐6. [PMC free article] [PubMed] [Google Scholar]
Liederman 2003
- Liederman EM, Morefield CS. Web messaging: a new tool for patient‐physician communication. Journal of the American Medical Informatics Association 2003;10(3):260‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liederman 2005
- Liederman EM, Lee JC, Baquero VH, Seites PG. The impact of patient‐physician Web messaging on provider productivity. Journal of Healthcare Information Management 2005;19(2):81‐6. [PubMed] [Google Scholar]
Mandl 1998
- Mandl KD, Kohane IS, Brandt AM. Electronic patient‐physician communication: problems and promise. Annals of Internal Medicine 1998;129(6):495‐500. [DOI] [PubMed] [Google Scholar]
McGeady 2007
- McGeady D, Kujala J, Ilvonen K. The impact of patient‐physician web messaging on healthcare service provision. International Journal of Medical Informatics 2008;77(1):17‐23. [DOI] [PubMed] [Google Scholar]
Medem 2007
- Medem Inc. eRisk Working Group for Healthcare's Guidelines for Online Communication. http://www.medem.com/phy/phy_eriskguidelines.cfm 2007.
Meyer 2012
- Meyer B, Atherton H, Sawmynaden P, Car J. Email for communicating results of diagnostic medical investigations to patients. Cochrane Database of Systematic Reviews 2012, Issue 8. [DOI: 10.1002/14651858.CD007980.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moyer 1999
- Moyer CA, Stern DT, Katz SJ, Fendrick AM. "We got mail": electronic communication between physicians and patients. American Journal of Managed Care 1999;5(12):1513‐22. [PubMed] [Google Scholar]
Moyer 2002
- Moyer CA, Stern DT, Dobias KS, Cox DT, Katz SJ. Bridging the electronic divide: patient and provider perspectives on e‐mail communication in primary care. American Journal of Managed Care 2002;8(5):427‐33. [PubMed] [Google Scholar]
Neville 2004
- Neville RG, Marsden W, McCowan C, Pagliari C, Mullen H, Fannin A. Email consultations in general practice. Informatics in Primary Care 2004;12(4):207‐14. [DOI] [PubMed] [Google Scholar]
OECD 2006
- Organisation for Economic Co‐operation and Development (OECD). OECD Factbook 2006 ‐ Economic, Environmental and Social statistics. http://masetto.sourceoecd.org/vl=3129664/cl=11/nw=1/rpsv/factbook/ 2006 [Accessed 01/07/2012].
Pappas 2012
- Pappas Y, Atherton H, Sawmynaden P, Car J. Email for clinical communication between healthcare professionals. Cochrane Database of Systematic Reviews 2012, Issue 9. [DOI: 10.1002/14651858.CD007979.pub2] [DOI] [PubMed] [Google Scholar]
Patt 2003
- Patt MR, Houston TK, Jenckes MW, Sands DZ, Ford DE. Doctors who are using e‐mail with their patients: a qualitative exploration. Journal of Medical Internet Research 2003;5(2):e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Perlemuter 2002
- Perlemuter L, Yomtov B. Feasibility and usefulness of dedicated software and e‐mail for self‐monitoring blood glucose in treating diabetes. Diabetic Medicine 2002;19(8):701‐2. [DOI] [PubMed] [Google Scholar]
Pondichetty 2004
- Pondichetty V, Penn D. The progressive roles of electronic medicine: benefits, concerns, and costs.. The American Journal of the Medical Sciences 2004;328(2):94‐9. [DOI] [PubMed] [Google Scholar]
Potts 2002
- Potts HW, Wyatt JC. Survey of doctors' experience of patients using the internet. Journal of Internet Medical Research 2002;4(1):e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ryan 2007
- Ryan R, Hill S, Broclain D, Horey D, Oliver S, Prictor M, Cochrane Consumers and Communication Review Group. Study Quality Guide. www.latrobe.edu.au/cochrane/resources.html (accessed December 2008) 2007.
Sawmynaden 2012
- Sawmynaden P, Atherton H, Majeed A, Car J. Email for the provision of information on disease prevention and health promotion. Cochrane Database of Systematic Reviews 2012, Issue 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schulz 2010
- Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sittig 2001
- Sittig DF, King S, Hazlehurst BL. A survey of patient‐provider e‐mail communication: what do patients think?. International Journal of Medical Informatics 2001;61(1):71‐80. [DOI] [PubMed] [Google Scholar]
TechWeb Network 2008
- TechWeb Network 2008. TechWeb Encyclopedia. http://www.techweb.com/encyclopedia 2008 [Accessed 01/07/2012].
Virji 2006
- Virji A, Yarnall KS, Krause KM, Pollak KI, Scannell MA, Gradison M, et al. Use of email in a family practice setting: opportunities and challenges in patient‐ and physician‐initiated communication. BMC Medicine 2006;4:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vodopivec‐Jamsek 2008
- Vodopivec‐Jamsek V, Jongh T, Gurol‐Urganci I, Atun R, Car J. Mobile phone messaging for preventive health care. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD007457] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wallwiener 2009
- Wallwiener M, Wallwiener CW, Kansy JK, Seeger H, Rajab TK. Impact of electronic messaging on the patient‐physician interaction. Journal of Telemedicine and Telecare 2009;15(5):243‐50. [DOI] [PubMed] [Google Scholar]
Wedderburn 1996
- Wedderburn AW, Dodds SR, Morris GE. A survey of post‐operative care after day case surgery. Annals of the Royal College of Surgeons of England 1996;78(2 Suppl):70‐1. [PubMed] [Google Scholar]
White 2004
- White CB, Moyer CA, Stern DT, Katz SJ. A content analysis of e‐mail communication between patients and their providers: patients get the message. Journal of the American Medical Informatics Association 2004;11(4):260‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ye 2010
- Ye J, Rust G, Fry‐Johnson Y, Strothers H. E‐mail in patient‐provider communication: A systematic review. Patient Education and Counseling 2010;80(2):266‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhou 2010
- Zhou YY, Kanter MH, Wang JJ, Garrido T. Improved quality at Kaiser Permanente through e‐mail between physicians and patients. Health Affairs 2010;29(7):1370‐5. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Atherton 2010
- Atherton H, Car J, Meyer B. Email for clinical communication between patients/caregivers and healthcare professionals. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD007978] [DOI] [Google Scholar]


