Abstract
Background
Acquired brain injury (ABI) is a major cause of disability. Timely access to inpatient ABI rehabilitation is associated with improved outcomes at the patient, system, and societal levels.
Problem
Wait times to access the inpatient ABI rehabilitation programme at the local regional rehabilitation centre by patients referred from community hospitals were consistently greater than provincial targets and benchmarks.
Objective
This initiative aimed to reduce the mean wait times from referral to admission by 30% (from 27 to 19 days) during the 12-month project period. The secondary aim was to concurrently achieve a reduction in the mean wait times for decisions from 9.5 to 5 days during the same period.
Methods
A non-randomised time-series design was undertaken. Baseline and postintervention wait times were obtained from patient intake charts. Process mapping, value analysis and five-why analysis were used to identify root causes for delays in the intake process. Referring hospital staff and the ABI Rehab interdisciplinary team members were engaged in change idea development and refinement. Iterative Plan-Do-Study-Act cycles were used to improve the change ideas’ usability and uptake. Data analysis was performed using the QI Macros package in Microsoft Excel.
Results
Root causes for delays included frequent incomplete referrals, variability in the intake process and limitations in rehab bed availability. Two change ideas were introduced: (1) a standardised intake protocol and (2) a referral checklist. Within 3 months, the mean decision wait times were reduced to 4 days (58% reduction), and the mean admission wait times were reduced to 12 days (54% reduction).
Conclusion
This initiative led to the systematic standardisation of the intake process for the local regional ABI rehab programme. Wait time improvements surpassing the initial aims were observed and may inform future benchmarks.
Keywords: Quality improvement, Checklists, Health services research, Healthcare quality improvement
WHAT IS ALREADY KNOWN ON THIS TOPIC
Acquired brain injury (ABI) is a major cause of disability. Timely access to inpatient ABI rehabilitation is associated with improved outcomes at the patient, system and societal levels.
WHAT THIS STUDY ADDS
In this initiative, checklists and standardisation were implemented at the regional brain injury rehabilitation centre to reduce admission wait times by an average of 2 weeks for inpatients referred from community hospitals. This result surpassed the initial aims.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
To the authors’ knowledge, this is the first initiative targeting wait times in this patient population using rigorous quality improvement methodology, including process mapping, five-why analysis, value analysis, Plan-Do-Study-Act cycles and standardisation. These successful approaches may be adapted to other rehabilitation programmes and may inform future benchmarks and targets for access to ABI inpatient rehabilitation. Associated cost savings are expected with the implementation of these approaches.
Introduction
Problem description and aim
Patients with acquired brain injury (ABI) referred from community hospitals to the local inpatient ABI rehab programme waited an average of 9.5 days for an admission decision and 26.7 days for an admission from 1 August 2021 to 16 March 2022. This surpassed the 3-day 90th percentile provincial target set by the Rehabilitative Care Alliance for patients designated as alternate level of care (ALC) from referral to admission to an inpatient rehab programme.1
Therefore, the aim of this initiative was to achieve a 30% reduction in the average wait times from referral to admission (from 26.7 to 19 days) by 1 July 2022 for patients referred from community hospitals. The secondary aim was to achieve a reduction in the average wait times for admission decisions from 9.5 to 5 days by 1 July 2022.
Available knowledge
ABI is a major cause of disability, with incidence rates of moderate to severe ABI as high as 500 per every 100 000 individuals.2 The most common causes of brain injury include traumatic brain injury (TBI) from motor vehicle collisions or falls.2
Timely access to inpatient ABI rehabilitation is associated with improved outcomes at the patient, system and societal levels. For individual patients, long wait times increase the risk of medical complications such as pressure injuries3 and joint contractures4 and can limit future independence.5 At the system level, patient flow issues arise, such as when individuals occupy beds above their care needs.5 At the societal level, delays in accessing rehabilitation can result in participation restriction in the workforce and negative economic consequences.5 Scientific literature suggests that inpatient rehabilitation within 35 days post-ABI is associated with better outcomes.2
Methods
Team and Stakeholders
This improvement initiative was a year-long process involving biweekly team meetings.
The improvement team included the team leader (corresponding author), the director of the rehabilitation centre, ABI managers, ABI physicians, ABI allied health professionals and intake coordinators, who performed extensive case management and communication for referrals prior to admission.
Referring community hospital representatives were engaged via email, telephone and virtual meetings in the change idea development and testing Plan-Do-Study-Act (PDSA) cycles.
Patient and public involvement
Patient cognitive status following brain injury, as well as the lack of direct interaction with the internal intake process logistics, did not allow for regular patient involvement in this initiative.
Design
A non-randomised time-series design was chosen. Wait times for patients referred from community hospitals to the regional inpatient ABI rehab programme were obtained from the intake coordinators for the baseline period of August 2021 to March 2022 and the postintervention period of March 2022 to June 2022. The QI Macros program in Microsoft Excel was used to analyse wait time variations in the baseline and postintervention periods. All data analyses were performed by 30 June 2022 and included all referrals for which a decision was made by that date.
Diagnostics
To understand the referral and intake process, a process map was constructed (online supplemental figure S2). A simplified process map is shown in online supplemental figure S2. The process step durations were estimated by the intake coordinators and validated by a retrospective chart review for 11 patients. Each process step duration is under 2 hours and does not significantly contribute to wait times; however, the durations between process steps are highly variable. A value analysis was performed by labelling process steps as value-added or non-value-added from the perspective of the patient. Overall, there were many non-value-added steps in the process, such as waiting for clarifying information from the referring hospitals. A five-why analysis was then performed on the bottlenecks to identify root causes for long wait times (online supplemental figure S3).
Three main contributors to long wait times in the local setting were identified:
-
Referral process inefficiencies
Region-specific mandated generic referral forms did not allow for adequate and efficient assessment of patient eligibility and readiness for ABI inpatient rehab.
Admission criteria were not clearly outlined or readily available for referring hospitals.
-
Intake process inconsistencies
The admission criteria lacked standardised definitions and were inconsistently used in the intake process.
Delays and variability in the referral review process (1–7 days), intake assessment scheduling and case review with the ABI physician led to bottlenecks in the process.
-
Limited resource availability
After receiving an acceptance to the ABI inpatient rehab programme, patients may be placed on a waitlist until a rehab bed becomes available, lasting 1 day to 4 weeks.
Rehab bed availability was influenced by inpatient length of stay, bed reallocations to acute care designations and staff redeployment during the COVID-19 pandemic.
The first two contributors affected the wait times from referral to decision, while the latter affected the wait times from decision to admission. These local contributors were consistent with those reported in literature.
Change idea generation
Two change ideas were designed to decrease wait times from referral to decision:
-
A one-page referral checklist based on updated admission criteria, to be appended with the referral form (see online supplemental material titled ‘Referral Checklist’).
Hypothesised to address inefficiencies in the referral process and to result in a higher proportion of complete referral forms, ultimately facilitating an earlier admission decision by reducing the frequency of clarifying communication.
-
Standardisation of the intake process (see online supplemental material titled ‘STANDARD WORK: ABI Inpatient Intake).
Hypothesised to reduce the variability and overall duration of each process step, particularly for the bottlenecks identified in the diagnostics phase.
-
The targets for the bottlenecks were set as follows:
Referrals are to be reviewed within 1 business day of receipt.
Intake assessments are to be completed within 5 business days from the referral review.
Referrals are to be reviewed between the intake coordinator and ABI physician within 2 business days from the intake assessment completion.
The reasons for limited resource availability were multifactorial and addressing this contributor was not deemed to be in scope for this initiative.
These change ideas are supported by literature on initiatives with similar root causes for long wait times for health services delivery. For example, recommendations to improve access to stroke rehabilitation include setting wait time standards from stroke onset to inpatient rehab and providing training on standardising referral and transfer processes from acute care to meet the targets.6 Standardisation of referral processes to meet targets and lean-inspired methodology (eg, eliminating non-value-added steps) have demonstrated the ability to improve wait times and intake processes. They use the inherent strengths of the existing system and are more cost-effective than wide system redesigns.7
Measures
Table 1 outlines the measures and associated methods of data collection. The measures were chosen based on the change ideas described above.
Table 1. Family of measures.
| Measure type | Measure | Method of data collection |
| Target (outcome) | Average number of days from referral to rehab admission | Obtained for each referral from an internal database and were verified for reliability from audits of patient intake charts |
| Target (high-level process) | Average number of days from referral to decision | |
| Balancing | Intake coordinator’s workload (number of hours spent on the intake process per patient referral) | Self-tracked and documented by the intake coordinators |
| Average satisfaction level of intake coordinators | Reported on a 1–5 scale (5=very satisfied and 1=very dissatisfied) via a 1-question survey for each referral after a rehab decision is communicated | |
| Average satisfaction level of community hospital with the intake process | Self-reported on a 1–5 scale (5=very satisfied and 1=very dissatisfied) | |
| Fidelity (referral checklist) | % Referrals in which checklist was completed by the referring hospitals | Collected by the intake coordinators, who reviewed the referral checklist for completeness and accuracy during the intake process. |
| % Referrals that were appropriate for ABI rehab | ||
| Fidelity (standard work) | % Referrals for which standard work was followed | Collected on a tracking sheet completed by the intake coordinators for each referral from community hospitals. |
| % Referrals reviewed ≤1 business day of receipt | ||
| % Intake assessment completion ≤5 business days from the referral review | ||
| % Case review between intake coordinator and ABI physician ≤2 business days from the intake assessment completion |
Fidelity measures were reported as a percentage of referrals received per month. Balancing measures were collected once before the change ideas were introduced and monthly afterwards.
ABIacquired brain injury
Strategy
The PDSA cycles for the referral checklist and intake process standardisation are outlined below:
Referral checklist
PDSA 1
Plan: Refine ABI admission criteria.
Do: Consulted ABI MDs and Allied health staff.
Study: Consensus was achieved on criteria during several group discussions.
Act: Feedback was incorporated into the one-page referral checklist.
PDSA 2
Plan: Obtain feedback from referring community hospitals to refine checklist.
Do: Met with two contacts from community hospitals for feedback on usability (no other contacts were interested or available to meet).
Study: Feedback was positive, no major changes to checklist.
Act: Refined checklist and posted checklist on the ABI rehab institutional website.
PDSA 3
Plan: Ascertain whether checklist is being used by referring hospitals.
Do: Measured proportion of referrals that had the checklist attached and completed.
Study: Low awareness of the checklist was noted (only one referring hospital had used the checklist as intended for one referral (in May 2022).
Act: telephone calls and informational emails to known referring contacts.
PDSA 4
Plan: Understand barriers to usage of the checklist.
Do: Follow-up with referring hospitals.
Study: There was general lack of awareness to use the checklist. Those who were aware of the checklist referred to the eligibility criteria for more complex referrals but did not use it alongside the referral form as intended, as it was felt to be too cumbersome to use for all referrals, particularly those that were not deemed complex. There were no specific suggestions on how to make the referral checklist less complex. Unfortunately, the referral form content and format were regionally mandated and could not be modified as part of this initiative.
Act: At this point, the checklist PDSAs were put on pause as the intervention was not being used as intended, it was difficult to optimise the intervention, and was not affecting referral appropriateness. The team then focused on the standardisation PDSAs as the main change intervention.
Intake process standardisation
PDSA 1
Plan: Set order of steps and duration targets for main process bottleneck steps.
Do: Consulted intake coordinators, ABI MDs, managers.
Study: There were several intake process steps that some team members did not feel were necessary for all referrals, such as the intake assessment and case review with the ABI physician for all referrals. However, ultimately, it was felt that removing or rearranging these steps would result in too large a change in the intake process. Instead, standardisation to reduce variability was the preferred approach by the team members.
Act: Refined future-state process map and target bottleneck durations (modified the previous workflow such that the intake office administrator notifies the intake coordinator on the date of referral receipt instead of at the weekly intake meeting).
PDSA 2
Plan: Develop and refine standard work for the intake process.
Do: Typed document with step-by-step instructions of the intake process, including maximum target wait times for steps.
Study: Obtained feedback from the intake coordinators on optimal wording and order of instructions.
Act: Developed the first version of the standard work document available to all intake coordinators, encouraged use of standard work.
PDSA 3
Plan: Identify effects and deviations from standardised protocol.
Do: Surveyed the intake coordinators on usability and barriers to usage.
Study: Wait time variability decreased from 1 to 5 business to 1 day after the introduction of the standard work. The standard work addressing the remaining bottlenecks (intake assessment completion and case review with the ABI physician) did not show consistent fidelity to their target timelines.
Act: Continue to refine standard work by focusing on decreasing wait times for the remaining bottlenecks.
Results
Outcome measures
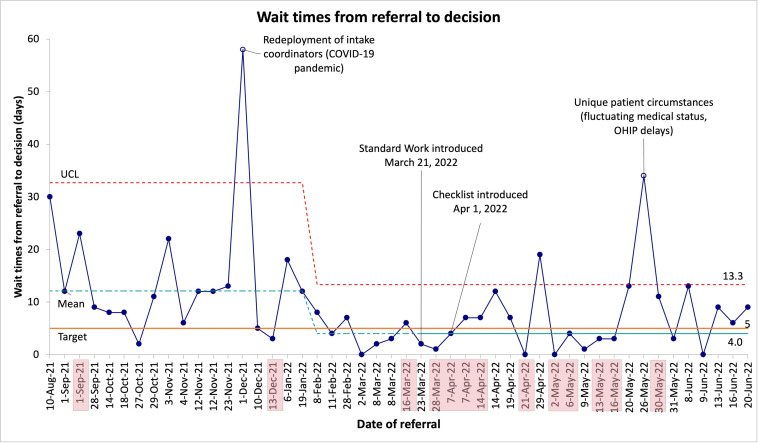
The mean wait times from referral to decision were reduced by 58% from 9.5 to 4.0 days. This was below the target mean of 5 days by 1 July 2022. Furthermore, there was less variability in the wait times (manifested by tighter control limits) after the introduction of the change ideas.
Figure 1 shows a statistical process control I-chart for decision wait times for all referrals from 10 August 2021 to 20 June 2022. The baseline included 25 referrals from 10 August 2021 to 16 March 2022 with a mean wait time to decision of 9.5 days. In the postintervention period, there were 23 referrals from 23 March 2022 to the end of the observation period (20 June 2022).
Figure 1. Statistical process control I-chart for wait times from referral to decision. Each data point represents a referral, with the date of each referral depicted on the x-axis. The referral dates for cases that were declined admission are shaded. The astronomical point on 1 December 2021 is labelled and attributed to redeployment of staff. UCL, upper control limit. OHIP, Ontario Health Insurance Plan.
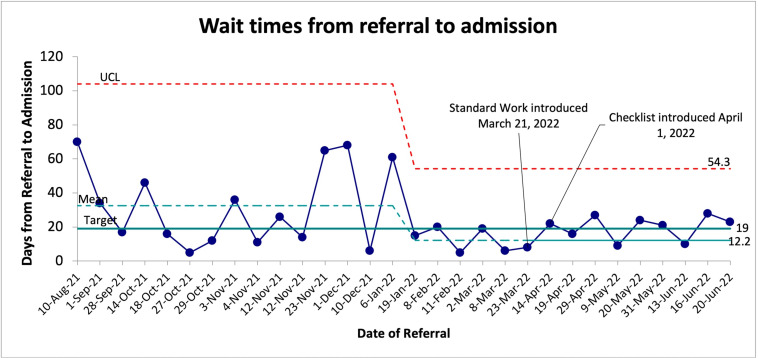
The mean wait times from referral to admission were reduced by 54% from 26.7 to 12.2 days. This was below the target mean of 19 days by 1 July 2022. Furthermore, there was less wait time variability (manifested by tighter control limits) after the change ideas.
Figure 2 shows a statistical process control I-chart for admission wait times for all referrals from 10 August 2021 to 13 June 2022. The baseline included 20 admissions from 10 August 2021 to 8 March 2022 with a mean wait time to admission of 26.7 days. In the postintervention period, there were 10 admissions from 23 March 2022 to the end of the observation period (20 June 2022).
Figure 2. Statistical process control I-chart for wait times from referral to admission for patients who were accepted to the regional ABI Inpatient Rehab Programme. Each data point represents a referral, with the date of each referral depicted on the x-axis. ABI, acquired brain injury; UCL, upper control limit.
For both the decision and admission wait times, the special cause variation of 8 or more points below the baseline mean occurred in February 2022, which was 1–2 months prior to the introduction of the change ideas. This temporal relationship suggests that other factors may have played a role in the wait time improvements. Since the process of designing the change ideas occurred January to February 2022, it is likely that the intake coordinators were implementing some of the principles and targets of the standard work prior to its official introduction into the intake process, as the coordinators were heavily involved in drafting and refining the standard work in the months prior to its introduction.
It is possible that the shorter decision times correlate with a higher proportion of rejected referrals during the postintervention period. (Postintervention, the admission rate dropped from 80% to 43%.) By having updated the admission criteria as part of the referral checklist, the intake coordinators could apply the admission criteria more consistently on referral review and subsequently decline those patients who did not meet the readiness criteria for rehab. Hence, it is plausible that the checklist contributed to more referral rejections and ultimately more re-referrals when the patients became rehab ready. This could also explain the increased number of referrals per month from March 2022 to June 2022, as each re-referral was considered a new referral for data analysis purposes. In contrast, prior to the introduction of the change ideas, patients who were not rehab-ready were deemed ‘pending’ for days to weeks instead of being declined; therefore, the wait times from referral to admission did not represent wait times from rehab readiness for next stage of rehabilitation to rehab service initiation, as is recommended in the 2021 Ontario TBI Report Card8 for mandated wait time data collection. In this way, the overall wait times after the change ideas were implemented were more likely to reflect the true duration to admission from when the patient was rehab ready.
Fidelity measures
Assessing the fidelity of the change ideas reveals the overall adherence to the standard work consistently remained above 70% from March 2022 to June 2022 inclusive, which was considered good uptake. This suggests that the introduction of the standard work contributed to the wait time improvements.
On the other hand, there was low fidelity for the referral checklist: only one referring hospital had used the checklist as intended for one referral (in May 2022). For the remaining referrals, the main reason cited for not using the checklist included a general lack of awareness of the referral checklist from the referring hospitals. Those who were aware of the checklist referred to the eligibility criteria for more complex referrals but did not use it alongside the referral form as intended, as it was felt to be too cumbersome to use for all referrals, particularly those that were not deemed complex. Therefore, the reported results of the initiative could not be attributed to the referral checklist, as education efforts for this change idea continue to be optimised to achieve an adequate fidelity.
Of note, the median monthly percentage of referrals deemed appropriate for rehab was 47%, with June 2022 showing 100% appropriate referrals.
Balancing measures
The intake coordinator’s workload did not increase with the introduction of the change ideas. The satisfaction level with the intake process remained stable or slightly increased for both the intake coordinators and the community hospitals with the new change ideas, though they reported that it was difficult to quantify as originally intended on a 1–5 Likert scale.
Strengths and limitations
Strengths
The strengths of this initiative included the thorough diagnostic process and PDSA cycles performed with key stakeholders (intake coordinators, ABI physicians, clinical managers, community hospital contacts), which led to confidence in the root causes, change theories and change ideas. Standardisation and checklists have been well documented in the literature to result in improvements in efficiency and timeliness in healthcare settings.7 Optimising these change ideas through further iterative PDSA cycles will likely lead to further improvements and are readily generalisable to other settings and populations.
Data collection and analysis
Limitations of this initiative included the lack of infrastructure to support automated collection of fidelity and outcome measures, which made data collection cumbersome. Efforts to remove barriers to data collection included writing standard work for wait time definitions that were manually inputted into an internal database and using a visual tracking system for fidelity measures.
Other factors that may have limited internal validity included the low monthly referral frequency from community hospitals, leading to relatively sparse data for analysing fidelity measures. Aggregating the measures into quarterly periods may improve the analysis.
Overall, the number of data points was sufficient for application of the control chart analysis for special cause variation to analyse the effectiveness of the interventions. In particular, the number of data points for decision wait times was similar for preintervention and postintervention periods (25 vs 23, respectively), which allowed for a reliable analysis of the effectiveness and sustainability of the interventions. However, the number of data points for admission wait times in the postintervention period was limited to 10 (compared with 20 baseline data points) in the context of the admission rate drop from 80% preintervention to 43% postintervention. The constraint of only 10 observations to evaluate the sustainability of the interventions impacting admission wait times is a limitation of this project. Unfortunately, it was not feasible to measure more than 10 postintervention admission wait times due to several factors, including low monthly referral frequency from community hospitals, staffing changes after June 2022, and new organisational priorities including the launch of a new electronic medical health record system.
Referral checklist
Barriers to the uptake of the referral checklist for referring hospitals included low awareness of the checklist, despite posting it on the regional ABI Rehab website beside the link to the referral form. Education efforts were limited to telephone calls and informational emails to known referring contacts, as there is no centralised communication system with all possible referring hospitals in the province. Furthermore, there may have been better uptake had the checklist been able to be included as part of the referral form itself, to minimise paperwork and cognitive load for referring hospitals.
Standardisation of the intake process
The standard work had the largest wait time reduction impact on the step between referral receipt and referral review. This was achieved by modifying the previous workflow such that the intake office administrator notifies the intake coordinator on the date of referral receipt instead of at the weekly intake meeting. This change decreased the variability from 1 to 5 business days prior to the introduction of the standard work to 1 day after the introduction of the standard work. The standard work addressing the remaining bottlenecks (intake assessment completion and case review with the ABI physician) did not show consistent fidelity to their target timelines. They were addressed in the standard work by the intake coordinators proactively scheduling these events within the target timelines; however, this did not prove effective, as these steps were heavily dependent on the other party’s schedules (referring hospitals and ABI physicians, respectively). Therefore, the standard work for these steps would have likely benefited from stronger interventions such as forcing functions and automation to ensure higher fidelity. Their fidelity was lowest in June 2022, which coincided with the hospital-wide introduction of a new electronic medical record system. This may have been a confounding factor.
Scoping
There were few applicable or consistent wait time indicators and benchmarks on which to anchor the aim and outcome measures. The wait time indicators from the literature were not standardised across regions or organisations and ranged from the median number of days from brain injury onset to rehab admission,8 to the 90th percentile benchmark for ALC patients from referral to rehab admission (for any type of inpatient rehab, not only for brain injury),1 to the distribution of the number of days from acceptance to rehab admission.9
The wait times that were chosen as outcome measures included times from patient referral to rehab, not from the onset of brain injury, as this was the portion of the process that the team felt was within their control and influence.
Future directions in refining this initiative will consider tracking patient outcomes as the primary outcome measures (and tracking wait times as high-level process measures), tracking time from ABI onset to transfer to rehab (rather than from referral to rehab) to align with suggested targets from scientific literature, and considering to use an alternate wait time metric such as the median or 90th percentile wait times, for consistency with other benchmarks.
Conclusion
This initiative led to the systematic standardisation of the admission criteria and intake process for the ABI rehab programme at the regional institution. These change ideas addressed the two main root causes of long wait times: (1) incomplete referral information and (2) intake process variability; they did not address the third root cause of limited resources as this was multifactorial and out of scope for this initiative. Despite this, wait time improvements were observed for decision and admission durations. The mean wait times from referral to decision were reduced by 58% from 9.5 to 4.0 days, and the mean wait times from referral to admission were reduced by 54% from 26.7 to 12.2 days, in addition to manifesting less data variability.
These results surpassed the initial aims of this initiative. Although there are no national or provincial targets specifically for ABI rehab wait times, the results of this initiative may inform future benchmarks. This study’s approaches may also inform wait time reductions for other healthcare services.
Furthermore, associated cost savings attributed to decreased acute care occupancy while waiting for rehab are expected, as improvements in wait times to access rehabilitative care have been reported to correlate with cost savings.5 Assuming a cost of approximately CAD$1000 per patient per day of acute care bed occupancy while awaiting rehab,10 this initiative translates into an estimated CAD$14 500 of savings per referral based on the 14.5- day reduction from referral to admission. A full cost analysis was not part of the scope of this paper.
The sustainability and spread of this initiative will continue to be dependent on factors such as staffing consistency and training on the standard work, and modification of the standard work to be integrated into the newly implemented electronic medical record. Ongoing education about the admission criteria will also be important to guide referring hospitals towards preparing appropriate referrals.
supplementary material
Acknowledgements
The authors would like to acknowledge the ABI Rehab intake coordinators, managers, physicians and allied health professionals for advancing this initiative.
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: As per the TCPS2 (2018) Article 2.5, an exemption from ethics review by the Hamilton Integrated Research Ethics Board (HiREB) was granted, as this work aligned with quality improvement activity.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Contributor Information
Ramona Neferu, Email: ramona.neferu@medportal.ca.
Rebecca Fleck, Email: rebecca.fleck@sjhc.london.on.ca.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
References
- 1.Gargaro J, Reilly K, Habib Perez O, et al. Ontario Neurotrauma Foundation - Brain Injury Guidelines; 2021. Ontario and sub regional traumatic brain injury (TBI) care report cards and provincial and regional trends in TBI care.https://braininjuryguidelines.org/onf/wp-content/uploads/2021/11/TBI-Report-Card_Oct-2021-Final.pdf Available. [Google Scholar]
- 2.Rehabilitative Care Alliance 2019-20 system performance report: summary report. 2021 http://rehabcarealliance.ca/uploads/File/Initiatives_and_Toolkits/System_Evaluation/2019-2020_System_Evaluation_Summary_Report.pdf Available.
- 3.Teasell R, Mehta S, Faltynek P, et al. Evidence-based review of moderate to severe acquired brain injury. Epidemiology and long-term outcomes following acquired brain injury. 2019. https://erabi.ca/modules/module-2/ Available.
- 4.Colantonio A, Gerber G, Bayley M, et al. Who waits for inpatient rehabilitation services in Canada after neurotrauma? A population based-study. J Rehabil Med. 2010;42:773–9. doi: 10.2340/16501977-0582. [DOI] [PubMed] [Google Scholar]
- 5.Osis SL, Diccini S. Incidence and risk factors associated with pressure injury in patients with traumatic brain injury. Int J Nurs Pract. 2020;26:e12821. doi: 10.1111/ijn.12821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marshall S, Janzen S, Faltynek P, et al. Evidence-based review of moderate to severe acquired brain injury. Motor and sensory impairment rehabilitation post acquired brain injury. 2019. https://erabi.ca/modules/module-4/ Available.
- 7.Rehabilitative Care Alliance Patient and system-level benefits of rehabilitative care - a primer to support planning by OHTs and Ontario health. 2020. http://www.rehabcarealliance.ca/uploads/File/Initiatives_and_Toolkits/Ontario_Health_Teams/Primer/RCA_Primer_on_Rehab_for_OHTs.pdf Available.
- 8.Jin A, Bagg S, Martin C, et al. Stroke Network of Southeastern Ontario; 2013. Leveraging rehabilitation to improve patient flow and quality outcomes in Southeastern Ontario: using stroke care as a model. Summary report.https://www.strokenetworkseo.ca/sites/strokenetworkseo.ca/files/rehab_forum_report_jan25_2013_final.pdf Available. [Google Scholar]
- 9.Valsangkar NP, Eppstein AC, Lawson RA, et al. Effect of Lean Processes on Surgical Wait Times and Efficiency in a Tertiary Care Veterans Affairs Medical Center. JAMA Surg. 2017;152:42–7. doi: 10.1001/jamasurg.2016.2808. [DOI] [PubMed] [Google Scholar]
- 10.Canadian Institute for Health Information . Ottawa, ON: CIHI; 2016. Care in Canadian ICUs.https://secure.cihi.ca/free_products/ICU_Report_EN.pdf Available. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information.