Abstract
Our descriptive study examined current associations (2022–2024) between US state-level health outcomes and 4 US state-level political metrics: 2 rarely used in public health research (political ideology of elected representatives based on voting records; trifectas, where 1 party controls the executive and legislative branches) and 2 more commonly used (state policies enacted; voter political lean). The 8 health outcomes spanned the life course: infant mortality, premature mortality (death at age <65), health insurance (adults aged 35–64), vaccination for children and persons aged ≥65 (flu; COVID-19 booster), maternity care deserts, and food insecurity. For the first 3 outcomes, we also examined trends in associations (2012–2024). For all political metrics, higher state-level political conservatism was associated with worse health outcomes, especially for the metrics for political ideology and state trifectas. For example, in 2016, the premature mortality rate in states with Republican vs Democratic trifectas was higher by 55.4 deaths per 100 000 person-years (95% CI: 7.7, 103.1), and the slope of the rate of increase to 2021 was also higher, by 27.0 deaths per 100 000 person-years (95% CI: 24.4, 29.7). These results suggest elections, political ideology, and concentrations of political power matter for population health.
Keywords: childhood vaccination, COVID-19 boosters, electoral politics, health insurance, infant mortality, food insecurity, maternity care deserts, political polarization, political conservatism, political determinants of health, political liberalism, poverty, premature mortality, state policies, state trifecta
To date, most US research on political determinants of health has focused on analyzing health impacts of proposed or enacted legislation or voter political lean (which neglects how voting is affected by both gerrymandering and voter suppression). We expand the focus by including 2 political metrics pertaining to elected officials’ political ideology (based on voting records) and partisan concentrations of political governance. Our state-level analyses focus on 8 current health outcomes (2022–2024) that span the life course: infant mortality, premature mortality, health insurance (adults aged 35–64), vaccination for children and persons aged ≥65 (flu; COVID-19 booster), maternity care deserts, and food insecurity. For the first 3 outcomes, we also examined trends over time (2012–2024). Across all political metrics, higher state-level political conservatism was associated with (1) worse health outcomes in the current period and (2) higher burdens of both premature mortality and percentage of adults ages 35–64 lacking health insurance in every presidential election year. Additionally, the sharp post-2018 rise of premature mortality rates that extended through 2021 started at higher levels and was greater in the more conservative vs more liberal states. This quantitative descriptive evidence offers important insights into how elections matter for population health.
Introduction
Elections are crucial to democratic governance, with results shaping political priorities, policies, programs, resources, and—often underappreciated—population health.1-10 At issue is who is elected, with what political agendas, both individually and as tied to political party affiliations and governing coalitions. Such statements might seem to be truisms, but US population health research engaged with issues of governance and health has primarily focused on policies proposed or enacted8-13—and also more recently, voter political lean (as spurred by the impact of political polarization on responses to and the harms of the COVID-19 pandemic)14-23—and not on who enacts the policies and their power to do so.1-7,21-25 Consequently, limited US empirical evidence documents links between political ideologies, political power, and population patterns of health and health inequities.1-8,22-25
How and why politics affects population health, including the magnitude of health inequities, is at core an interdisciplinary query.1-8,22-25 In our descriptive social epidemiologic study, we draw on political science and political sociology scholarship to address gaps in political metrics used in US public health research,1-8,21,22 while also foregrounding critical epidemiologic concerns, not typically addressed in social science literature, regarding etiologic period (ie, the time it takes for an exposure to become biologically embodied and manifested as a health outcome) and the need to analyze risk in relation to both baseline rates and changes in rates over time.3,24,26
Our a priori hypothesis is that more conservative political ideologies—that is, politics that prioritize the private sector and cultural traditionalism over government programs, policies, and regulations that prioritize social equity and collective goods1-11,25,27—are associated both with poorer current public health outcomes and worse trends in population health improvements over time. Numerous pathways are postulated to link political ideologies to population health outcomes and health inequities, variously involving the power of the state to shape living, working, and economic conditions and the rights needed to attain equity in these conditions; access to and quality of health care; and protection of the biophysical resources and environs necessary to thrive.1-11,24-27 Also crucial is who holds what power to implement the specified political ideology, as shaped by laws affecting who can vote, voter turnout and voter suppression, demarcation of political district boundaries (including gerrymandering), political donations, and who is declared to be an election winner.1-5,22,28 A lack of public health research addressing political ideology and concentrations of political power is thus worrisome.
Our observational cross-sectional state-level analysis accordingly seeks to expand knowledge about the social patterning of population health in relation to a range of political metrics, taking advantage of heterogeneities in state political profiles and health status across US states and over time, spanning 4 US presidential elections (2012–2024) during a time of increasing political polarization.1,4,5 With regard to exposures, we include not only the 2 more commonly used measures employed in public health research pertaining to state policies and voter political lean6,8,10-23 but also 2 measures commonly used in political science and political sociology research but rarely used in public health studies, regarding elected representatives’ political ideology (based on their voting records) and the concentration of party political power via state trifectas (ie, 1 party controls both the executive and legislative branches of government).1-3,22,23 We consider the associations of these political metrics with 8 health outcomes, chosen because they (1) span the life course, (2) are important public health indicators, and (3) are quickly temporally responsive to changes in societal conditions (ie, have a short etiologic period).3,24,26,29,30 In Table 1, we summarize the theoretical rationale for each study variable. By considering the patterns of relationships observed, we aimed to generate both questions and information about relationships between political ideology, power, and population health that can be useful to health and policy researchers, health professionals, policymakers, elected officials, civil society groups, and the broader electorate.
Table 1.
Theoretical justification for the US state-level variables: political metrics, health outcomes, and socioeconomic covariates.
| State-level variable | Theoretical justification | Additional considerations |
|---|---|---|
| Political metrics | 1. Political ideology of elected representatives. Elected officials campaign to win positions of power and legislate based on their political ideology. Political ideologies, while complex, in the United States typically are categorized as ranging from conservative to liberal, in relation to both social and economic positions. Political ideologies can affect population health and health inequities via their material impacts on people's living and working conditions and on their economic, social, political, civil, and cultural rights. | Politicians’ legislative voting records (ie, roll-call votes) provide public data on their political positions and can reflect their willingness to use state power to implement their political ideology. In the United States, members of Congress (US House and Senate) legislate to shape federal policy, including its impact on states and resources for constituents in their states. A political ideology score based on roll-call votes of US members of Congress is available (DW-Nominate) and is used in numerous social science studies, but rarely in population health studies.23,31 |
| 2. Political party concentration of power. Political parties provide the resources and organizational means for politicians with a similar political ideology to enact their legislative agenda. Achieving political party concentration of power, in order to have a sufficient number of votes to pass legislation and override any vetoes, is a core objective. The likelihood of particular policies to impact population health depends, in part, on the power of political parties to enact the legislation they advocate. | In the US political system, political party concentration of power can be measured in relation to whether a single party controls the executive and legislative branches of government. At the US state level, this involves control of 3 seats of power (also referred to as a “trifecta”): governor (executive) and each component of their bicameral legislatures (eg, House and Senate), with the 1 exception of Nebraska (which has a unicameral legislature).32 Trifecta data are used in numerous social science studies, but rarely in population health studies.23,32,33 | |
| 3. State policy index. State policies are the political enactment of elected officials’ political ideologies and the government agencies they control and whose budgets they set. These policies, enacted over time, singly and together, shape the conditions of life for people and ecosystems within their state (and sometimes neighboring states, as per the case of environmental pollution), thereby affecting people's health. | Beyond the direct health impacts of specific policies (eg, Medicaid expansion), both public health and social science studies increasingly are investigating impacts of policy “bundles,” which reflect a shared underlying political ideology and base of support.2,10,27,34-36 Some indices of state policies focus on multiple policies in a specific policy domain (eg, health care) and others consider policies across multiple domains (eg, social and economic policies); while many are cross-sectional and cover a limited set of years, some include decades of policy data to create dynamic measures of state policy indices.27,37 | |
| 4. Voter political lean. Voters’ political ideologies can affect which political parties and politicians they vote for and hence which state policies are or are not enacted. The partisan identification of voters is the basis for measuring voter political lean, which typically is measured as the percentage difference between the vote for a particular party in a particular area (eg, state or political district) vs in the national vote. Voter political lean is often interpreted as being a measure of voter political ideology. One impact of voter political lean on health is via the politicians (and other elected officials) who are elected vs defeated, as well as the ballot initiatives passed vs defeated; others may be via pathways involving interpersonal relationships between members of the electorate. | Voter political lean is a metric increasingly used in public health research since 2020, in research focused on COVID-19 pandemic and political polarization.14-23 Key caveats are that voter political lean (1) is based solely on who votes, noting that only 66% and 46% of US eligible voters, respectively, voted in the 2020 presidential election and the 2022 midterm elections,38 and persons least likely to vote are concentrated among politically, socially, and economically marginalized sectors of society who also are at higher risk of poor health1-3,38,39; (2) does not reflect views of persons legally not permitted to vote (eg, ex-felons, noncitizens, young people aged <18); and (3) ignores gerrymandering (ie, legislators’ manipulation of district boundaries to give unfair advantage to population groups deemed likely to elect them), which deliberately diminishes the votes of those targeted adversely by gerrymandering and affects which policies are enacted.5,28,40,41 | |
| Health outcomes | Guiding selection of 8 chosen health outcomes is that they (1) span the life course, enabling detection of associations with political metrics across all age groups; (2) are quickly responsive to contemporaneous exposures (ie, have a short etiologic period); and (3) are important public health indicators, with all except 1 (vaccination for the newly emergent disease COVID-19) designated as either “leading health indicators” or “objectives” in 1 or both of the US Department of Health and Human Services agenda-setting national initiatives Healthy People 2020 and Healthy People 2030.29,30 | All health outcomes but one were based on state-level data for the entire population; the exception was the state-representative survey data on percentage of adults without health insurance. The specific outcomes selected involve both health status and access to health care. They comprised infant mortality, premature mortality (death before age 65), lack of health insurance among working-age adults (ages 35–64), childhood immunization, flu vaccination among adults aged ≥65, COVID-19 vaccination among adults aged ≥65, food insecurity, and maternity care deserts. |
| Socioeconomic covariates | We opted to adjust for state poverty rates as a potential confounder, since (1) poverty is associated with the selected exposures and health outcomes and poverty rates vary by state and (2) poverty rates (unlike other socioeconomic metrics, such as educational level or wealth) are rapidly responsive to changes in fiscal policies.42-48 | We focused on poverty rates among children (<18 years) and adults aged ≥65 because numerous US safety net programs focus on these age groups and use the Federal Poverty Level to determine eligibility.42-51 We recognize that adjusting for poverty may result in attenuated estimates of association, since it may be on the causal pathway between state policies and health outcomes. |
Social epidemiologic, political science, and political sociology theories inform the justifications for the variables selected; for supporting scholarship, see citations 1-8, 21-28. Descriptions of the specific variables used are presented in the Data and methods section, and details on how to access these data and how to construct the variables used are provided in Table S1 and Textbox S1, respectively.
Data and methods
Study design
Our repeated cross-sectional, descriptive, population-based study included US state-level data, by year, for all 50 US states plus the District of Columbia (DC). Due to unavailable data for both health outcomes as well as most of the political metrics, we did not include US territories.52,53
Variables
Our study included 3 types of annual state-level variables chosen with the theoretical justifications provided in Table 1: (1) political metrics, (2) health outcomes, and (3) socioeconomic covariates. Details on how to access these data and how to construct the variables used are presented in Table S1 and Textbox S1, respectively.
State-level political metrics: political ideology, power, policies, and voter political lean
Political ideology: DW-Nominate (2012–2024)
We used data on the first dimension of the DW-Nominate scale, which measures political ideology based on roll-call votes (especially regarding the economy and government regulation) of every member of US Congress, using data spanning from the 112th through the 118th Congress.31 Given the variable number of US House representatives by US state (current median: 6; average: 8.7; range: 1–52) and also 2 US senators per state,54 we generated annual state-level measures of DW-Nominate political polarization, based on tercile cut points for the full study period (2012–2024), using the Index of Concentration at the Extremes (ICE).55-59 We scored the ICE to range from −1 (most conservative) to 1 (most liberal).
Political party concentrations of power (2012–2024)
For each time period under consideration (as demarcated in Table S2), we assessed each state's annual trifecta status (ie, state governor and legislature controlled by the same political party)32 and categorized states in relation to whether they were (1) consistently a Republican trifecta, (2) consistently a Democratic trifecta, or (3) “mixed” (neither consistently a Republican or Democratic trifecta).
State liberalism index (2012–2020)
This metric, developed by Caughey and Warshaw, assigns scores derived from “a dynamic latent-variable model” based initially on “data on 148 [social and economic] policies collected over eight decades (1936–2014)” and extended to 202027,37 (see detailed description in Textbox S1). Of note, this index captures domains of policy relevant to structural racism.3,24-26,59 We coded this metric as ranging from −1 (most conservative) to 1 (most liberal).
Voter political lean (2022)
The Cook Partisan Voting Index (PVI) uses people's votes to quantify “how partisan a district or state is compared to the nation as a whole.”60 This variable is available at the state level only for 2022, and its range was from R+25 to D+43,61 which we coded as ranging from −25 (most Republican) to 43 (most Democratic).
State-level public health outcomes: critical temporally-responsive indicators spanning the life course
Infant mortality rates (2012–2024)
We obtained the annual infant mortality rate data (deaths per 1000 live births)62-64 from CDC WONDER65 for January 1, 2012, to May 31, 2024.
Premature mortality rates (2012–2024)
We generated data on premature mortality (death before age 65 years34,66-70) using annual age-specific mortality data from CDC WONDER65 for January 1, 2012, through May 31, 2024, and age-standardized the rates (deaths per 100 000 person-years) via direct standardization using the Year 2000 Standard Million.71
Health insurance (2012–2022)
We accessed annual 1-year state-level estimates for the percentage of adults aged 35 to 64 years lacking health insurance using US Census American Community Survey data for January 1, 2012, through December 31, 2022.72 This age group is ineligible for programs directed to children or adults aged ≥65 years,68,73 and is the sole age bracket for working-age adults consistently available for 2012–2022.72
Childhood immunization (2022)
We obtained state-level data on the percentage of children aged 24 months who had completed the series of 7 recommended shots.74-77 The data are from the Centers for Disease Control and Prevention’s (CDC's) ChildVaxView website75 for the time period January 1, 2022, through December 31, 2022.
Older-adult flu vaccination (2022)
We obtained state-level data on the percentage of US adults aged ≥65 years who reported receiving a seasonal flu vaccine78-80 during the past 12 months (January 1–December 31, 2022).81
Older-adult COVID-19 booster uptake (2023–2024)
We obtained state-level data from CDC's CovidVaxView on the percentage of adults aged ≥65 years who received a 2023–2024 COVID-19 vaccine dose82 between September 24, 2023, and May 25, 2024, among those already vaccinated with ≥1 dose.83
Food insecurity (2020–2022)
We obtained US Department of Agriculture state-level data84 on food insecurity85-88 for 2020–2022 (3-year estimate).89
Maternity care deserts (2021–2022)
We obtained data on the percentage of women aged 15–44 years in each state living in counties categorized as maternity care deserts90-92 from America Health Rankings for 2021–2022 (2-year estimates).93
State-level socioeconomic covariates: child and senior poverty rates
We included data on poverty among children (aged <18 years) and adults aged ≥65 years (2012–2022), given poverty's well-documented contributions to health inequities,42-44 its rapid responsiveness (including as compared with educational levels and wealth) to fiscal policy changes,45-48 and the numerous US safety programs using the Federal Poverty Level to determine eligibility.43,49-51 We used state-level data, spanning January 1, 2012, through December 31, 2022, based on American Community Survey estimates.72,94-96
Statistical analysis
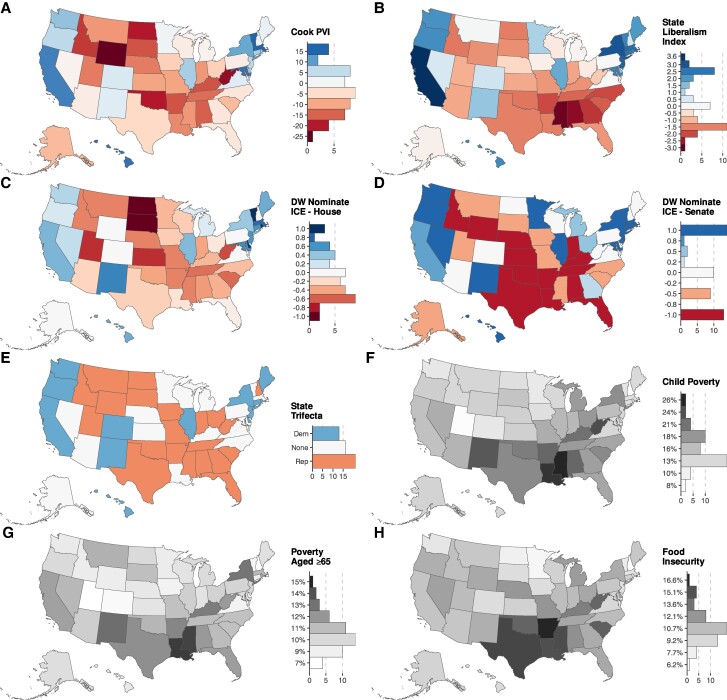
We first tabulated the distribution of each of the state-level political, health, and poverty metrics across 4 time periods demarcated by the past 3 and current presidential election years (2012, 2016, 2020, and 2024; see Table S2), and mapped each state's value for the current period (2022–2024) (Figure 1). All analyses used the observed data, given no missing data for any variables; analyses using DW-Nominate and state trifecta data, however, excluded DC, since they are not applicable to DC's governance structure. Correlations among the study variables are provided in Figure S1.
Figure 1.
Maps of current state-level data for the political exposures, health outcomes, and covariates (2022–2024): political metrics (A-E), poverty (F-G), and health outcomes (H-O). Darker colors denote higher values. Adverse health outcomes are shown in grayscale (darker color, worse health outcome); beneficial outcomes use a purple color scale (darker color, better health outcome). Abbreviations: Cook PVI, Cook Partisan Voting Index; ICE, Index of Concentration at the Extremes.
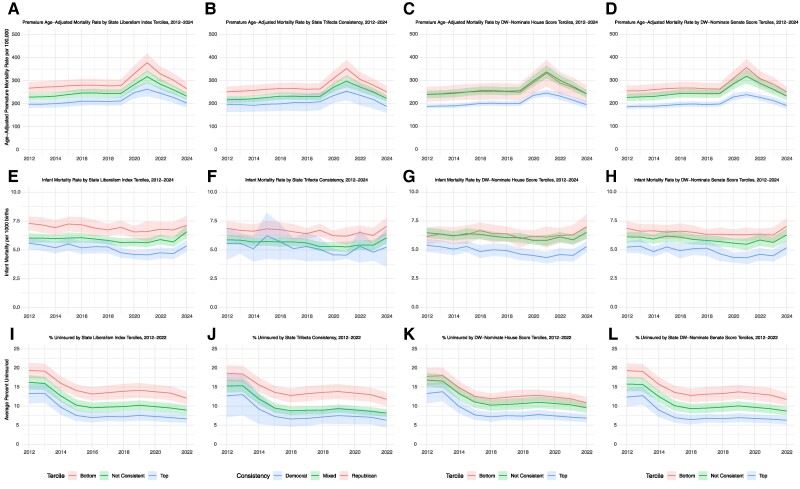
We then used linear regression to quantify the current (2022–2024) cross-sectional standardized associations97,98 (which allow for comparison of estimates for metrics with different scales97,98) between the state-level political exposures and health outcomes, overall and adjusted for the poverty variables (Table 2, Table S3). Sensitivity analyses weighted for state population size99,100 (Table S4). Supplemental analyses stratified by racialized groups for infant mortality and premature mortality rates, the only outcomes for which data were publicly available by these social groups (Table S5); none of the health outcomes were available stratified by any socioeconomic metrics.
Table 2.
Cross-sectional standardized associations of the state-level current political exposures with the current health outcomes, adjusted for child and elderly poverty, for 50 US states and the District of Columbia, 2022–2024.
| Variable: health outcomes | Political exposure: standardized effect estimate (95% CI) and P value (for different from 0) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cook PVI | P | State liberalism index | P | State trifecta | US House | US Senate | ||||||
| DW-Nominate | P | DW-nominate | P | |||||||||
| D vs R | P | Mixed vs R | P | |||||||||
| Infant mortality: deaths per 1000 live births | −0.32 (−0.62, −0.02) | * | −0.56 (−0.84, −0.29) | *** | −0.94 (−1.57, −0.30) | ** | −0.24 (−0.83, 0.35) | **** | −0.43 (−0.68, −0.18) | *** | −0.46 (−0.72, −0.21) | *** |
| Premature mortality rate (age-standardized death rate for persons under age 65 per 100 000 persons) | −10.53 (−20.21, −0.84) | * | −12.42 (−22.18, −2.65) | * | −25.49 (−46.62, −4.35) | * | −13.00 (−32.46, 6.47) | **** | −8.87 (−17.53, −0.20) | * | −10.83 (−19.65, −2.02) | * |
| Percentage adults without health insurance (ages 35–64) | −1.54 (−2.51, −0.58) | ** | −1.96 (−2.89, −1.02) | *** | −2.76 (−4.90, −0.61) | * | −2.33 (−4.31, −0.36) | * | −1.05 (−1.94, −0.16) | * | −1.53 (−2.41, −0.66) | *** |
| Childhood immunization: % children aged 24 months who have received full set of vaccines | 2.35 (0.38, 4.32) | * | 2.60 (0.60, 4.61) | * | 3.06 (−1.56, 7.67) | **** | −0.07 (−4.32, 4.18) | **** | 2.78 (1.06, 4.49) | ** | 2.70 (0.95, 4.46) | ** |
| Flu vaccinations: % adults aged ≥65 vaccinated | 2.85 (1.60, 4.09) | *** | 2.44 (1.08, 3.81) | *** | 4.35 (1.36, 7.34) | ** | 3.23 (0.47, 5.98) | * | 1.71 (0.48, 2.95) | ** | 1.86 (0.59, 3.13) | ** |
| COVID-19 vaccination: % adults aged ≥65 vaccinated who received booster | 3.72 (2.39, 5.05) | *** | 3.73 (2.35, 5.12) | *** | 5.95 (2.77, 9.13) | *** | 4.03 (1.10, 6.96) | ** | 2.62 (1.35, 3.88) | *** | 3.26 (1.99, 4.52) | *** |
| Food insecurity: % of households | −0.39 (−0.79, 0.01) | **** | −0.37 (−0.78, 0.05) | **** | −0.68 (−1.58, 0.23) | **** | −0.68 (−1.51, 0.15) | **** | −0.22 (−0.59, 0.15) | **** | −0.56 (−0.90, −0.21) | ** |
| Maternity care deserts: % of female population aged 15–44 living in counties designated as a maternity care desert | −4.75 (−4.87, −2.43) | *** | −2.93 (−4.36, −1.51) | *** | −6.21 (−9.31, −3.11) | *** | −3.43 (−6.29, −0.57) | * | −3.17 (−4.29, −2.05) | *** | −2.24 (−3.58, −0.89) | ** |
For the current analyses, we include the most recent data available, as follows: for DW-Nominate, 2022–2024; for Cook PVI, 2022; for state liberalism index, 2020; for state trifecta, 2022–2024; for infant mortality rates, 2022–2024; for premature mortality rates, 2022–2024; for % of adults without health insurance, 2022; for childhood immunization, 2022; for flu vaccinations among adults ≥65, 2022; for COVID-19 vaccinations among adults ≥65, 2023–2024; for food insecurity, 2020–2022; for maternity care deserts, 2021–2022; for child and elderly poverty, 2022. P values: *.01 to <.05; **.001 to <.01; ***<.001; ****>.05.
Abbreviations: Cook PVI, Cook Partisan Voting Index; D, Democratic; R, Republican.
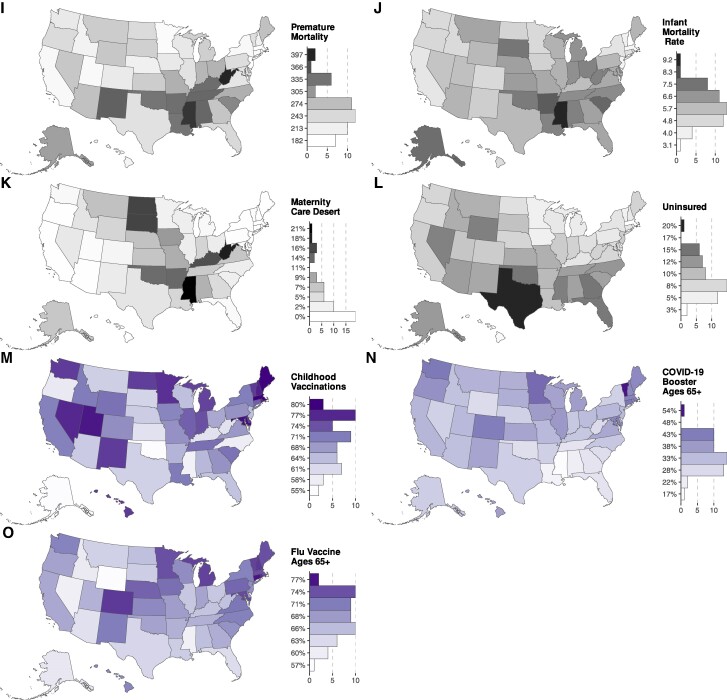
For the trend analyses (2012–2024), we first plotted the annual data for each health outcome stratified by states grouped by level of political conservatism (Figure 2). Next, we conducted joinpoint analyses,101-103 using these same state groupings, to identify key inflection points in the temporal trends (Table 3). We then fit spline regression models, which used state-level random effects to account for possible unobserved heterogeneity between states and also adjusted for poverty, to (1) test for the significance of these joinpoints, (2) estimate the slope between the identified joinpoints, and (3) estimate the absolute difference in health outcomes, comparing the bottom and middle categories to the top category for each political metric, for each presidential election year.
Figure 2.
Trends in state-level health outcomes by stratified by state-level political metrics (state liberalism; state trifecta; DW-Nominate House; DW-Nominate Senate), for the 50 US states and the District of Columbia (2012–2024): premature mortality (A-D), infant mortatliy (E-H), and percent uninsured (I-L).
Table 3.
Baseline rates, joinpoint regression analysis of trends in health outcomes stratified by state-level political metrics, and rate differences, adjusted for poverty, for 50 US states and the District of Columbia (2012–2024).
| Health outcome | Political metric | Baseline health outcome (2012), value (95% CI) | Inflection points (year, 95% CI) and slope (95% CI) | Comparison of absolute rate differences during presidential election years, adjusted for poverty, rate difference (95% CI) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Interval 1 | Interval 2 | Interval 3 | 2012 | 2016 | 2020 | 2024 | ||||||
| Estimate | Slope | Inflection point | Slope | Inflection point | Slope | |||||||
| Premature mortality rate (age-standardized death rate for persons <65 years per 100 000 persons) | State liberalism index | Most liberal: consistently in top tercile | 135.9 (107.4, 164.3) | 2.8 (1.3, 4.4) | 2018 (2015, 2018) | 17. 6 (14. 9, 20.3) | 2021 (2021, 2022) | −19.4 (−22.6, −16.3) | [referent] | [referent] | [referent] | [referent] |
| Not consistently in either top or bottom tercile | 172.3 (146.4, 198.2) | 2.9 (1. 6, 4.2) | 2018 (2015, 2018) | 21.8 (19.4, 24.2) | 2021 (2021, 2022) | −26.2 (−28.8, −23.5) | 36.4 (11.9, 61.0) | 36.5 (12.6, 60.5) | 104.0 (79.9, 128.1) | 29.1 (−15.7, 73.9) | ||
| Most conservative: consistently in bottom tercile | 175.9 (142. 9, 208.8) | 12.5 (11.4, 13.6) | 2018 (2015, 2018) | 29.0 (25.6, 32.4) | 2021 (2021, 2022) | −29.5 (−32.9, −26.2) | 40.0 (12.0, 68.1) | 78.6 (51.1, 106.2) | 120.8 (91.9, 149.8) | 102.0 (72.2, 131.8) | ||
| State trifecta | Consistently Democratic | 173.7 (126.3, 221.1) | 1.5 (−1.1, 4.1) | 2018 (2016, 2018) | 17.7 (12.8, 22.7) | 2021 (2021, 2021) | −19.8 (−25.6, −14.0) | [referent] | [referent] | [referent] | [referent] | |
| Mixed | 195.6 (168.3, 222.9) | 2.2 (1.1, 3.4) | 2018 (2015, 2018) | 21.9 (19.9, 23.9) | 2021 (2021, 2022) | −22.7 (−24.9, −20.5) | 21.9 (−23.8, 67.7) | 24.9 (−20.1, 69.8) | 99.5 (54.4, 144.7) | 30.1 (−53.3, 113.5) | ||
| Consistently Republican | 229.5 (196.0, 263.0) | 1.4 (−0.1, 2.9) | 2018 (2015, 2018) | 27.0 (24.4, 29.7) | 2021 (2021, 2022) | −29.9 (−32.9, −26.9) | 55.8 (7.7, 103.1) | 55.4 (7.7, 103.1) | 73.8 (26.0, 121.6) | 52.8 (3.7, 101.9) | ||
| US House: DW-Nominate index | Most liberal: consistently in top tercile | 161.3 (128.8, 193.9) | 1.5 (−0.5, 3.5) | 2018 (2015, 2018) | 15.6 (12.7, 18.6) | 2021 (2021, 2022) | −16.6 (−20.0, −13.1) | [referent] | [referent] | [referent] | [referent] | |
| Not consistently in either top or bottom tercile | 213.0 (185.2, 240.7) | 1.9 (0.8, 3.0) | 2018 (2015, 2018) | 26.0 (24.0, 28.0) | 2021 (2021, 2022) | −28.6 (−30.8, −26.4) | 51.6 (22.3, 80.9) | 49.6 (20.8, 78.5) | 122.2 (93.3, 161.2) | 43.5 (−7.3, 94.4) | ||
| Most conservative: consistently in bottom tercile | 213.2 (174.5, 251.8) | 2.4 (0.8, 4.0) | 2018 (2015, 2018) | 24.0 (20.3, 27.6) | 2021 (2021, 2022) | −26.0 (−30.2, −21.9) | 51.8 (12.7, 91.0) | 48.3 (9.8, 86.7) | 63.1 (24.5, 101.7) | 43.1 (3.5, 82.7) | ||
| US Senate: DW-Nominate index | Most liberal: consistently in top tercile | 160.4 (125.6, 195.1) | 2.1 (0.3, 3.4) | 2018 (2015, 2018) | 14.8 (11.4, 18.1) | 2021 (2021, 2022) | −15.3 (−19.2, −11.3) | [referent] | [referent] | [referent] | [referent] | |
| Not consistently in either top or bottom tercile | 198.6 (171.2, 226.0) | 2.6 (1.5, 3.8) | 2018 (2015, 2018) | 24.0 (21.9, 26.0) | 2021 (2021, 2022) | −25.9 (−28.2, −23.6) | 38.3 (5.2, 71.4) | 40.5 (8.0, 73.1) | 110.8 (78.1, 143.5) | 37.2 (−20.5, 95.0) | ||
| Most conservative: consistently in bottom tercile | 225.2 (191.7, 258.7) | 1.0 (−0.5, 2.5) | 2018 (2015, 2018) | 27.5 (24.7, 30.3) | 2021 (2021, 2022) | −30.4 (−33.5, −27.2) | 64.8 (27.9, 101.8) | 60.7 (24.3, 97.0) | 84.1 (47.6, 120.5) | 51.4 (14.1, 88.8) | ||
| Infant mortality: deaths per 1000 live births | State liberalism index | Most liberal: consistently in top tercile | 4.6 (3.9, 5.4) | 0.4 (0.2, 0.5) | 2022 (2014, 2022) | 0.3 (0.1, 0.4) | — | — | [referent] | [referent] | [referent] | [referent] |
| Not consistently in either top or bottom tercile | 5.2 (4.4, 5.9) | −0.0 (−0.1, 0.0) | 2022 (2015, 2022) | 0.4 (0.2, 0.5) | — | — | 0.5 (−0.0, 1.1) | 0.8 (0.2, 1.3) | 1.0 (0.4, 1.5) | 1.6 (0.9, 2.3) | ||
| Most conservative: consistently in bottom tercile | 6.1 (5.2, 7.0) | −0.0 (−0.1, −0.0) | 2021 (2014, 2022) | 0.1 (0.0, 0.2) | — | — | 1.5 (0.8, 2.1) | 1.6 (1.0, 2.2) | 1.7 (1.1, 2.3) | 1.6 (−0.5, 3.8) | ||
| State trifecta | Consistently Democratic | 5.1 (3.9, 6.3) | −0.1 (−0.1, −0.0) | 2022 (2014, 2022) | 0.2 (−0.2, 0.5) | — | — | [referent] | [referent] | [referent] | [referent] | |
| Mixed | 5.2 (4.4, 6.0) | −0.1 (−0.1, −0.0) | 2021 (2017, 2022) | 0.2 (0.1, 0.3) | — | — | 0.1 (−0.9, 1.2) | 0.2 (−0.8, 1.2) | 0.3 (−0.7, 1.3) | 0.6 (−0.5, 1.7) | ||
| Consistently Republican | 5.9 (4.9, 7.0) | 0.0 (−0.1, 0.1) | 2016 (2014, 2017) | −0.1 (−0.2, −0.0) | 2020 (2019, 2022) |
0.1
(0.0, 0.2) |
0.9 (−0.3, 2.0) | 1.3 (0.2, 2.3) | 1.2 (0.1, 2.2) | 1.4 (0.3, 2.6) | ||
| US House: DW-Nominate index | Most liberal: consistently in top tercile | 4.3 (3.5, 5.2) | −0.1 (−0.1, −0.0) | 2022 (2014, 2022) | 0.3 (0.1, 0.5) | — | — | [referent] | [referent] | [referent] | [referent] | |
| Not consistently in either top or bottom tercile | 5.3 (4.5, 6.1) | −0.1 (−0.1, −0.0) | 2021 (2014, 2022) | 0.1 (0.1, 0.2) | — | — | 1.0 (0.4, 1.6) | 1.1 (0.5, 1.7) | 1.2 (−0.7, 3.2) | 1.1 (0.4, 1.8) | ||
| Most conservative: consistently in bottom tercile | 4.9 (3.9, 5.9) | 0.1 (0.0, 0.2) | 2016 (2015, 2017) | −0.1 (−0.2, −0.0) | 2021 (2019, 2022) |
0.3
(0.1, 0.4) |
0.6 (−0.3, 1.4) | 1.5 (0.7, 2.3) | 1.4 (0.6, 2.2) | 1.7 (0.8, 2.6) | ||
| US Senate: DW-Nominate index | Most liberal: consistently in top tercile | 4.7 (3.8, 5.6) | −0.1 (−0.1, −0.0) | 2022 (2014, 2022) | 0.3 (0.0, 0.5) | — | — | [referent] | [referent] | [referent] | [referent] | |
| Not consistently in either top or bottom tercile | 5.5 (4.7, 6.4) | −0.1 (−0.1, −0.0) | 2021 (2014, 2022) | 0.2 (0.1, 0.3) | — | — | 0.8 (0.1, 1.5) | 0.9 (0.2, 1.6) | 1.0 (−0.6, 2.6) | 1.1 (0.3, 1.9) | ||
| Most conservative: consistently in bottom tercile | 6.0 (5.0, 7.0) | −0.0 (−0.1, 0.1) | 2016 (2014, 2017) | −0.1 (−0.2, 0.0) | 2020 (2018, 2022) | 0.1 (0.0, 0.2) | 1.2 (0.4, 2.1) | 1.5 (0.7, 2.3) | 1.5 (0.7, 2.3) | 1.6 (0.8, 2.5) | ||
| Percentage lacking health insurance (adults aged 35–64) | State liberalism index | Most liberal: consistently in top tercile | 11.8 (9.4, 14.3) | −2.0 (−2.2, −1.7) | 2015 (2014, 2016) | 0.0 (−0.1, 0.2) | — | — | [referent] | [referent] | [referent] | [referent] |
| Not consistently in either top or bottom tercile | 14.6 (12.4, 16.9) | −2.1 (−2.3, −1.9) | 2015 (2014, 2017) | 0.0 (−0.1, 0.1) | — | — | 2.8 (0.7, 4.8) | 2.2 (0.1, 4.2) | 1.6 (−1.2, 4.3) | 2.0 (−0.5, 4.6) | ||
| Most conservative: consistently in bottom tercile | 17.2 (14.3, 20.1) | −1.9 (−2.2, −1.6) | 2015 (2014, 2020) | 0.0 (−0.1, 0.1) | — | — | 5.4 (3.0, 7.7) | 5.7 (3.3, 8.1) | 6.0 (2.8, 9.1) | 5.4 (3.0, 7.8) | ||
| State trifecta | Consistently Democratic | 10.8 (7.3, 14.4) | −2.0 (−2.4, −1.5) | 2015 (2014, 2016) | 0.1 (−0.1, 0.3) | — | — | [referent] | [referent] | [referent] | [referent] | |
| Mixed | 13.0 (10.7, 15.2) | −2.1 (−2.3, −1.9) | 2015 (2014, 2017) | 0.0 (−0.1, 0.1) | — | — | 2.1 (−1.2, 5.4) | 1.7 (−1.6, 5.1) | 1.3 (−3.0, 5.7) | 1.6 (−2.6, 5.7) | ||
| Consistently Republican | 15.6 (12.8, 18.3) | −1.7 (−1.9, −1.4) | 2015 (2014, 2019) | 0.0 (−0.1, 0.2) | — | — | 4.7 (1.2, 8.2) | 5.9 (2.4, 9.5) | 7.2 (2.5, 11.8) | 5.7 (2.1, 9.4) | ||
| US House: DW-Nominate index | Most liberal: consistently in top tercile | 11.8 (9.1, 14.5) | −1.7 (−2.1, −1.4) | 2015 (2014, 2016) | 0.1 (−0.1, 0.2) | — | — | [referent] | [referent] | [referent] | [referent] | |
| Not consistently in either top or bottom tercile | 14.5 (12.1, 16.9) | −2.1 (−2.2, −1.9) | 2015 (2014, 2017) | 0.0 (−0.0, 0.2) | — | — |
2.7
(0.4, 5.0) |
2.4 (0.1, 4.7) | 2.2 (−0.8, 5.1) | 2.3 (−0.5, 5.1) | ||
| Most conservative: consistently in bottom tercile | 15.2 (12.0, 18.4) | −2.0 (−2.3, −1.7) | 2015 (2014, 2019) | 0.0 (−0.1, 0.2) | — | — | 4.7 (1.6, 7.8) | 4.6 (1.5, 7.6) | 5.7 (1.8, 9.7) | 4.4 (1.2, 7.5) | ||
| US Senate: DW-Nominate index | Most liberal: Consistently in top tercile | 11.5 (8.8, 14.2) | −2.0 (−2.3, −1.7) | 2015 (2014, 2016) | 0.1 (−0.0, 0.2) | — | — | [referent] | [referent] | [referent] | [referent] | |
| Not consistently in either top or bottom tercile | 14.3 (12.0, 16.6) | −2.1 (−2.3, −1.7) | 2015 (2014, 2018) | 0.0 (−0.0, 0.2) | — | — | 2.7 (0.3, 5.1) | 2.3 (−0.1, 4.7) | 1.8 (−1.4, 5.0) | 2.0 (−0.9, 5.0) | ||
| Most conservative: consistently in bottom tercile | 17.5 (14.7, 20.2) | −1.7 (−2.1, −1.4) | 2015 (2014, 2020) | 0.0 (−0.1, 0.2) | — | — | 5.9 (3.2, 8.6) | 5.6 (2.9, 8.4) | 5.4 (1.8, 8.9) | 5.3 (2.5, 8.0) | ||
Values were adjusted for both childhood poverty and poverty among persons aged ≥65 years; for the rate comparisons, the referent group for the rate difference is most liberal or Democratic trifecta, indicated by a value of [referent] for rate difference; DC (District of Columbia) is included solely for the state liberalism index analyses; and slopes and rate differences whose 95% CIs exclude 0 are shown in bold type.
We conducted all statistical analyses other than the joinpoint analyses104 in R (version 4.3.3; R Project for Statistical Computing, Vienna, Austria)105; information on how to access the analytic code is provided in Table S1.
Ethics approval
No institutional review board approval was required, because the study involved secondary analysis of publicly available de-identified data (Harvard Longwood Campus IRB decision tool, July 20, 2024).
Results
State political and health profiles
Current values for the state-level political metrics, health outcomes, and poverty metrics are mapped in Figure 1, which displays the geographic patterning of these measures. In these maps, higher values are shown in darker colors, adverse health outcomes are shown in grayscale (for which a higher value is a worse outcome), and beneficial health outcomes use a purple scale (for which a higher value is a better outcome). Detailed data on the distribution of these variables are provided in Table S2 for both the current period (2022–2024) and over time (2012–2024). Similar patterns of state heterogeneity are evident for all of these variables in each time period (Figure 1, Table S2).
Current cross-sectional analyses
Table 2 presents the standardized regression coefficients (ie, for change in the health outcome associated with 1-SD change in the political exposure variable) for the current period (2022–2024), adjusted for the poverty metrics. Table S3 presents the unadjusted and adjusted results. For all outcomes and all political metrics, higher exposure to state conservatism was associated with poorer health outcomes, even after adjusting for poverty, which attenuated estimates (Table 2, Table S3). Sensitivity analyses weighted for state population size yielded similar results (Table S4).
Considering first the outcomes for which higher values indicate worse health (infant mortality, premature mortality, percentage uninsured, maternity care desert, and food insecurity), states with lower political conservatism had lower values (ie, better health outcomes) than states with higher political conservatism, as indicated by the negative estimates shown in Table 2. The largest standardized regression estimates were observed for the political ideology and the state trifecta metrics, as follows—(1) infant mortality: Democratic vs Republican trifecta (−0.94 infant deaths per 1000 live births; 95% CI: −1.57, −0.30); (2) premature mortality: US House DW-Nominate ICE score (−8.87 deaths per 100 000 person-years; 95% CI: −17.53, −0.20); (3) percentage uninsured: Democratic vs Republican trifecta (−2.76%; 95% CI: −4.90%, −0.61%); (4) maternity care desert: Democratic vs Republican trifecta (−6.21%; 95% CI: −9.31%, −3.11%); and (5) household food insecurity: US Senate DW-Nominate ICE score (−0.56%; 95% CI: −0.90%, −0.21%). In supplemental analyses for infant and premature mortality, the same patterns held for the White non-Hispanic population; however, among the Black non-Hispanic and Hispanic populations, the associations were not significant (with wide 95% CIs indicating low precision of estimates due to smaller population size; see Table S5).
Next, considering the health outcomes where a higher value is a better outcome (ie, the 3 outcomes pertaining to percentage vaccinated), positive estimates indicated better outcomes in states with lower political conservatism (Table 2). The largest standardized regression coefficients again occurred for the metrics for political ideology and state trifecta, as follows—(1) childhood vaccination: US House DW-Nominate ICE score (+2.78%; 95% CI: 1.06%, 4.49%); (2) flu vaccination among adults aged ≥65: Democratic vs Republican trifecta (+4.35%; 95% CI: 1.36%, 7.34%); and (3) COVID-19 booster among adults aged ≥65: Democratic vs Republican trifecta (+5.95%; 95% CI: 2.77%, 9.13%). Hence, for all health outcomes, the strongest associations with health among the political metrics was observed for the 2 metrics least commonly used in population health research, pertaining to political ideology of elected officials and state concentrations of political power.
Trend analyses
Figure 2 displays temporal trends, by year (for 2012–2024), in state-level health outcomes (and 95% CIs) stratified by states grouped by their level of political conservatism. For virtually all outcomes, the extreme groups (eg, comparing the top and bottom tercile, or Republican vs Democratic trifecta) and their 95% CIs do not overlap, with states in the most conservative stratum consistently having worse health than those in the most liberal stratum. Figure S2 shows these results by state within each tercile or trifecta grouping.
Table 3 presents data stratified by the political metrics and adjusted for the poverty variables, for (1) the slope for the rate of change of the state-level health outcomes and the temporal inflection points and (2) the rate differences across the political metrics in each presidential election year. Differences in baseline values and in trends, comparing states in the most conservative vs liberal strata for each political metric, were most apparent for premature mortality and for percentage of persons lacking health insurance; no consistent patterns were evident for infant mortality.
For premature mortality, the sharp rise in premature mortality in 2018–2021 was greatest in the states in the most conservative political strata for all 4 political metrics, with this steep rise compounding already higher baseline rates (Table 3). Contrasts in these slopes, comparing states in the most conservative vs most liberal strata, were similar across political metrics for age-standardized deaths per 100 000 person-years—(1) for state liberalism index: 29.0 (95% CI: 25.6, 32.4) vs 17.6 (95% CI: 14.9, 20.3); (2) for state trifecta: 27.0 (95% CI: 24.4, 29.7) vs 17.7 (95% CI: 12.8, 22.7); (3) for US House DW-Nominate Index: 24.0 (95% CI: 20.3, 27.6) vs 15.6 (95% CI: 12.7, 18.6); and (4) for US Senate DW-Nominate Index: 27.5 (95% CI: 24.7, 30.3) vs 14.8 (95% CI: 11.4, 18.1). These slopes built on the 2016 absolute age-standardized rate difference (per 100 000 person-years), between the more conservative vs more liberal states, as follows—(1) for state liberalism index: 78.6 (95% CI: 51.1, 106.2); (2) for state trifecta: 55.4 (95% CI: 7.7, 103.1); (3) for US House DW-Nominate Index: 48.3 (95% CI: 9.8, 86.7); and (4) for US Senate DW-Nominate Index: 60.7 (95% CI: 24.3, 97.0). These absolute gaps persisted in 2024 for (1) state liberalism index: 102.0 (95% CI: 72.2, 131.8); (2) state trifecta: 52.8 (95% CI: 3.7, 101.9); (3) US House DW-Nominate Index: 43.1 (95% CI: 3.5, 82.7); and (4) US Senate DW-Nominate Index: 51.4 (95% CI: 14.1, 88.8).
For the percentage of persons lacking health insurance (adults aged 35–64 years), for all political metrics, the point estimate for the slope for the rate of decline after 2015 was consistently smaller in states in the more conservative vs liberal strata (albeit with overlapping 95% CIs). Moreover, the percentage of those without health insurance was consistently higher in the states in the more conservative vs more liberal strata in every presidential election year. The highest absolute difference occurred in 2020 for state trifecta (7.2%; 95% CI: 2.5%, 11.8%).
Discussion
Our descriptive analyses document that US states with more conservative political metrics had worse health profiles in 2022–2024 compared with those with more liberal political metrics. These relationships held across all 4 political metrics and a range of health outcomes spanning the life course, with the selected outcomes chosen because they are quickly responsive to contemporaneous exposures. From 2012 to 2024, moreover, burdens of both premature mortality and the percentage of adults aged 35–64 years lacking health insurance were consistently higher in more conservative vs more liberal states in every presidential election year, and the sharp post-2018 rise of premature mortality rates extending through 2021 started at higher levels and was greater in the more conservative vs more liberal states. Moreover, for most, but not all, analyses, we observed stronger associations for the 2 political metrics not typically used in public health studies: political ideology of elected officials and state trifectas. Together, the observed patterns of association indicate that elections, political ideology, and concentrations of political power matter for population health.
Before interpreting study results, it is important to consider the study’s limitations. First, as noted above, our state-level study is a correlational, not causal, analysis; other state-level factors could be associated with the political metrics and confound the observed associations. Second, adjusting for poverty may result in attenuated estimates of association, since poverty arguably could be on the causal pathway between the political metrics and the health outcomes; supporting this view, adjusting for poverty attenuated estimates of the associations between the political metrics and health outcomes (Table S3). Third, we were unable to analyze the health outcomes stratified by poverty, education, or other socioeconomic metrics due to lack of publicly accessible, state-level health data for these metrics; similar data limitations precluded stratifying analyses by racialized groups, except for infant and premature mortality (Table S5). Due to our focus on outcomes with short etiologic periods, we did not test for lagged associations, even as current and past political exposures might jointly affect state health profiles. Of note, the bulk of premature deaths during the study time period were due to external causes (which have short etiologic periods) and, since 2020, COVID-19, not chronic diseases.106,107
Our findings are consistent with the recent wave of public health and social science research, since 2020, on the health impacts of political polarization and partisanship on government and individual responses to the COVID-19 pandemic on COVID-19 outcomes and overall mortality rates.14-23,108 In these studies, more voter support for conservative or right-leaning politics typically was associated with worse health.14-23 Other studies have found that governors’ conservative opposition to public health regulations was associated with worse COVID-19 outcomes,14,108-110 with the party affiliations of state governors associated with the timing and content of state's COVID-19 policies regarding population mobility, evictions, and masking109,110; people's response to these policies and to their governor's recommendations14; and COVID-19 mortality.108 Only 1 study additionally used the political ideology and trifecta metrics we used, and found that these metrics and also voter political lean were associated with COVID-19 mortality rates and that stress on hospital intensive care unit capacity was most strongly associated with Republican trifectas and US Senator political ideology scores.23 The only other population health study to our knowledge including data on state trifectas found that they were associated with the types of obesity-related health policies enacted between 2009 and 2015.33 Together, this body of research lends support to the hypothesis that who is elected, the power they wield, and their incumbency matters for population health.
Our repeated cross-sectional trend analyses likewise support the hypothesis that political context shapes population health. For example, in the case of the percentage of adults aged 35–64 years who lack health insurance, the finding that the key inflection point in 2015 had tighter CIs for the more liberal vs more conservative states, along with the persistence of higher proportions of uninsurance in every presidential election year in the more conservative vs more liberal states, is consistent with (1) the 2013–2014 policy changes regarding Medicaid expansion and the subsequent state dynamics of adoption of Medicaid expansion111 and (2) research documenting links between conservative ideology, racial resentment, and views about state support for Medicaid (and also the Supplemental Nutrition Assistance Program [SNAP]).112 The results for the higher and greater acceleration in premature mortality during the first years of the COVID-19 pandemic in more conservative vs more liberal states are also consistent with prior US research on political conservatism and COVID-19 policies and mortality, and likely reflect the political as well as epidemiological dynamics of the onset of the COVID-19 pandemic.4,10,14-23 Use of joinpoint analysis101-104 notably allowed for considering not only possible temporal “shocks” (eg, as tied to election years) but also rates of change in relation to baseline rates, which both matter for appraising population health burdens and trends.24,26,113
The observed relationship between greater state conservatism and poorer state health profiles could reflect causal pathways (see Table 1) and also diverse biases—for example, shared common causes,114,115 selection bias,115(p. 396) and conditioning on a shared effect.114(p. 463) For example, individuals could move to states that they view as having politics—and politicians—more compatible with their political views.2,4 Two lines of evidence suggest that such moves would not lead to worse health in conservative states. First, people who change their state of residence typically are more affluent than those who do not move116,117 and thus likely to have better health.118,119 Second, if people move to states to obtain more social welfare benefits (eg, because they have worse health or lack health insurance118,119), this would presumably imply moving to more liberal states.2-5,9,10 Moreover, the existence of a shared common cause, such as states’ past histories of structural racialized, economic, and political inequality (eg, past histories of Jim Crow)—whereby such history leads to both contemporary greater conservatism and poorer health among states’ residents—would bolster the hypothesis that conservatism adversely affects population health.3,5,7-10,24-26,34,112,113 Future research could thus reasonably pursue investigating the causal basis of the descriptive associations we report.
Conclusion
In summary, our descriptive population-based study provides timely and novel insights into patterns of associations, for the time period 2012–2024, between diverse measures of state-level conservatism and a wide range of temporally-responsive US state-level population health outcomes. We also provide suggestive evidence that 2 key political metrics rarely used in public health research often are most strongly associated with population health: political ideology of elected officials and state trifectas. In our view, these results comprise the “bodily evidence that links the ‘body natural’ to the ‘body politic’”24(p.10) and can usefully inform future research questions and also health professionals, policymakers, elected officials, civil society groups, and the broader electorate. Especially relevant in an election year, our results suggest that current levels and trajectories of health outcomes are sensitive to political contexts, which are themselves changeable by elections.1-10 Our results likewise suggest that analyses concerned with political determinants of health are likely incomplete if they focus solely on voter political lean or state policies enacted, without also including data on the politicians, their votes, and partisan concentrations of power.
We close by acknowledging the context in which we have conducted our analyses, which underscores the relevance of our descriptive findings. We commenced work on this study in the spring of 2024, amidst the campaigning for the November 2024 US presidential, congressional, and state and local elections. Mindful of the study's relevance to these elections,120 we wrote this final paragraph in the aftermath of the US elections, which has resulted in a Republican trifecta at the national level, and at the state level there are now 23 Republican trifectas (same as before the election), 15 Democratic trifectas (down 2, compared with before the election), and 12 divided state governments (up 2, compared with before the election).121 Data on the Cook PVI metric for voter political lean have yet to be calculated, although preliminary results indicate that, among the 30 states whose electoral votes went to the Republican ticket, the margin of Republican victory ranged from 0.9% (Wisconsin) to 45.8% (Wyoming) of the vote, and among the 19 states whose electoral votes went to the Democratic ticket, the margin of Democratic victory ranged from 2.7% (New Hampshire) to 31.8% (Vermont); the margin for DC (with no electoral votes) equaled 85.8%.121 If indeed political conservativism is causally associated with worse health outcomes and reduced access to health care, the election results may foretell (1) worsening health profiles in states with high or rising conservatism and (2) potential challenges to maintaining or improving the better health outcomes in more liberal states, given the national Republican trifecta.122-125 What actually transpires, however, will, of course, depend on the actions of elected officials, judges, government agencies, civil society organizations, and social movements, at the national, state, and local levels.1-3,5-11,24,122-125 A sobering question to consider is: If state health profiles worsen, who will be blamed, by whom?
Supplementary Material
Contributor Information
Nancy Krieger, Department of Social and Behavioral Sciences, Harvard T.H. Chan School of Public Health, Boston, MA 02115, United States.
Soroush Moallef, Department of Social and Behavioral Sciences, Harvard T.H. Chan School of Public Health, Boston, MA 02115, United States; FXB Center for Health and Human Rights, Harvard University, Boston, MA 02115, United States.
Jarvis T Chen, Department of Social and Behavioral Sciences, Harvard T.H. Chan School of Public Health, Boston, MA 02115, United States.
Ruchita Balasubramanian, Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, MA 02115, United States; Center for Communicable Disease Dynamics, Harvard T.H. Chan School of Public Health, Boston, MA 02115, United States.
Tori L Cowger, FXB Center for Health and Human Rights, Harvard University, Boston, MA 02115, United States.
Rita Hamad, Department of Social and Behavioral Sciences, Harvard T.H. Chan School of Public Health, Boston, MA 02115, United States.
Alecia J McGregor, Department of Health Policy and Management, Harvard T.H. Chan School of Public Health, Boston, MA 02115, United States.
William P Hanage, Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, MA 02115, United States; Center for Communicable Disease Dynamics, Harvard T.H. Chan School of Public Health, Boston, MA 02115, United States.
Loni Philip Tabb, Department of Biostatistics, Dornsife School of Public Health, Drexel University, Philadelphia, PA 19104, United States.
Mary T Bassett, Department of Social and Behavioral Sciences, Harvard T.H. Chan School of Public Health, Boston, MA 02115, United States; FXB Center for Health and Human Rights, Harvard University, Boston, MA 02115, United States.
Supplementary material
Supplementary material is available at Health Affairs Scholar online.
Funding
S.M. is supported by a Canadian Institutes of Health Research (CIHR) Doctoral Award (FRN #193216). The CIHR played no role in the writing of the manuscript or the decision to submit it for publication.
Notes
- 1. McGuire JW. Democracy and Population Health. Cambridge, UK: Cambridge University Press; 2020. [Google Scholar]
- 2. Fafard P, Cassola A, de Leeuw E. Integrating Science and Politics for Public Health. Cham, Switzerland: Springer International; 2022. [Google Scholar]
- 3. Beckfield J. Political Sociology and the People's Health. New York: Oxford University Press; 2018. [Google Scholar]
- 4. Oberlander J. Polarization, partisanship, and health in the United States. J Health Polit Policy Law. 2024;49(3):329–350. [DOI] [PubMed] [Google Scholar]
- 5. Keena A, Latner M, McGann AJM, Smith CA. Gerrymandering the States: Partisanship, Race, and the Transformation of American Federalism. Cambridge, UK: Cambridge University Press; 2021. [Google Scholar]
- 6. Oliver TR. The politics of public health policy. Annu Rev Publ Health. 2006;27(1):195–233. [DOI] [PubMed] [Google Scholar]
- 7. Navarro V, Shi L. The political context of social inequalities and health. Soc Sci Med. 2001;52(3):481–491. [DOI] [PubMed] [Google Scholar]
- 8. Dawes D, Gonzalez J. The politics of population health. Milbank Q. 2023;101(S1):224–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Falkenbach M, Bekker M, Greer SL. Do parties make a difference? A review of partisan effects on health and the welfare state. Eur J Public Health. 2020;30(4):673–682. [DOI] [PubMed] [Google Scholar]
- 10. Montez JK, Grumbach JM. US state policy contexts and population health. Milbank Q. 2023;101(S1):196–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Montez JK, Beckfield J, Cooney JK, et al. US state policies, politics, and life expectancy. Milbank Q. 2020;98(3):668–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Riley AR, Collin D, Grumbach JM, Torres JM, Hamad R. Association of US state policy orientation with adverse birth outcomes: a longitudinal analysis. J Epidemiol Community Health. 2021;75(7):689–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kemp B, Grumbach JM, Montez JK. U.S. state policy contexts and physical health among midlife adults. Socius. 2022;8. 10.1177/23780231221091324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Grossman G, Kim S, Rexer JM, Thirumurthy H. Political partisanship influences behavioral responses to governors’ recommendations for COVID-19 prevention in the United States. Proc Natl Acad Sci USA. 2020;117(39):24144–24153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kerr J, Panagopoulos C, van der Linden S. Political polarization on COVID-19 pandemic response in the United States. Pers Individ Dif. 2021;179:110892. 10.1016/j.paid.2021.110892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Williams CYK, Ferreira AF. Impact of political partisanship on public interest in infection prevention measures in the United States: an infodemiological study. Prev Med Rep. 2021;23:101493. 10.1016/j.pmedr.2021.101493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kaashoek J, Testa C, Chen JT, et al. The evolving roles of US political partisanship and social vulnerability in the COVID-19 pandemic from February 2020–February 2021. PLOS Glob Public Health. 2022;2(12):e0000557. 10.1371/journal.pgph.0000557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schnake-Mahl A, Bilal U. Disaggregating disparities: a case study of heterogenous COVID-19 disparities across waves, geographies, social vulnerability, and political lean in Louisiana. Prev Med Rep. 2022;28:101833. 10.1016/j.pmedr.2022.101833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Warraich HJ, Kumar P, Nasir K, Joynt Maddox KE, Wadhera RK. Political environment and mortality rates in the United States, 2001-19: population based cross sectional analysis. BMJ. 2022;377:e069308. 10.1136/bmj-2021-069308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Nayak SS, Fraser T, Aldrich DP, Panagopoulos C, Kim D. County-level political group density, partisan polarization, and individual-level mortality among adults in the United States: a lagged multilevel study. SSM Popul Health. 2024;26:101662. 10.1016/j.ssmph.2024.101662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bambra C, Lynch J, Smith K. The Unequal Pandemic: COVID-19 and Health Inequalities. Bristol, UK: Policy Press; 2021. [Google Scholar]
- 22. Lynch J. The political economy of health: bringing political science in. Annu Rev Polit Sci. 2023;26(1):398–410. [Google Scholar]
- 23. Krieger N, Testa C, Chen JT, Hanage WP, McGregor AJ. Relationship of political ideology of US federal and state elected officials and key COVID pandemic outcomes following vaccine rollout to adults: April 2021-March 2022. Lancet Reg Health Am. 2022;16:100384. 10.1016/j.lana.2022.100384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Krieger N. Ecosocial Theory, Embodied Truths, and the People's Health. New York: Oxford University Press; 2021. [Google Scholar]
- 25. Heller JC, Givens ML, Johnson SP, Kindig DA. Keeping it political and powerful: defining the structural determinants of health. Milbank Q. 2024;102(2):351–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Krieger N. Analyzing structural racism and its health impacts: it's about time. Am J Epidemiol. 2024:kwae392. Epub ahead of print. 10.1093/aje/kwae392 [DOI] [PubMed] [Google Scholar]
- 27. Caughey D, Warshaw C. The dynamics of state policy liberalism index, 1936-2014. Am J Polit Sci. 2016;60(4):889–913. [Google Scholar]
- 28. Caughey D, Tausanovitch C, Warshaw C. Partisan gerrymandering and the political process: effects on roll-call voting and state policies. Election Law J. 2017;16(4):453–469. [Google Scholar]
- 29. US Department of Health and Human Services . Healthy People 2020. Last reviewed December 14, 2020. Accessed August 3, 2024. https://www.cdc.gov/nchs/healthy_people/hp2020.htm
- 30. US Department of Health and Human Services . Healthy People 2030. Last reviewed: August 18, 2020. Accessed August 3, 2024. https://www.cdc.gov/nchs/healthy_people/hp2030/hp2030.htm
- 31. Voteview.com. About the project. Accessed July 24, 2024. https://voteview.com/about
- 32. Ballotpedia . State government trifectas. Accessed July 24, 2024. https://ballotpedia.org/State_government_trifectas
- 33. Pomeranz JL, Siddiqi A, Bolanos GJ, Shor JA, Hamad R. Consolidated state political party control and the enactment of obesity-related policies in the United States. Prev Med. 2017;105:397–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Montez JK, Mehri N, Monnat SM, et al. U.S. state policy contexts and mortality of working-age adults. PLoS One. 2022;17(10):e0275466. 10.1371/journal.pone.0275466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Matthay EC, Gottlieb LM, Rehkopf D, Tan ML, Vlahov D, Glymour MM. What to do when everything happens at once: analytic approaches to estimate the health effects of co-occurring social policies. Epidemiol Rev. 2022;43(1):33–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Montez JK. US state polarization, policymaking power, and population health. Milbank Q. 2020;98(4):1033–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Caughey D. Updated estimates of state policy and mass ideology, 1936-2020. Accessed July 24, 2024. https://www.dropbox.com/t/MRDUHsLpFAzNBDhu
- 38. Hartig H, Daniller A, Keeter S, Van Green T. Voter Turnout, 2018-2022. Pew Research Center; July 12, 2023. Accessed July 23, 2024. https://www.pewresearch.org/politics/2023/07/12/voter-turnout-2018-2022/ [Google Scholar]
- 39. Barber M, Holbein JB. 400 Million voting records show profound racial and geographic disparities in voter turnout in the United States. PLoS One. 2022;17(6):e0268134. 10.1371/journal.pone.0268134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Syed Q, Schmidt S, Powell RE, et al. Gerrymandering and political determinants of health. Popul Health Manag. 2022;25(4):568–570. [DOI] [PubMed] [Google Scholar]
- 41. Rushovich T, White A, Nethery RC, Krieger N. Gerrymandering and the packing and cracking of medical uninsurance in the United States. J Public Health Manage Policy. 2024;30(6):832–834. 10.1097/PHH.0000000000001916 [DOI] [PubMed] [Google Scholar]
- 42. Duncan GJ, Kalil A, Ziol-Guest KM. Parental income and children's life course: lessons from the panel study of income dynamics. Ann Am Acad Pol Soc Sci. 2018;680(1):82–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Pilkauskas NV. Child poverty and health: the role of income support policies. Milbank Q. 2023;101(S1):379–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Agarwal SD, Cook BL, Liebman JB. Effect of cash benefits on health care utilization and health: a randomized study. JAMA. 2024;332:1455–1463. 10.1001/jama.2024.13004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Saunders P. Inequality and poverty. In: Béland D, Morgan KJ, Obinger H, Pierson C, eds. Oxford Handbook of the Welfare States. 2nd ed. Oxford, UK: Oxford University Press; 2021:717–732. [Google Scholar]
- 46. Hamad R, Yeb J, Jackson K, Gosliner W, Fernald LCH. Potential mechanisms linking poverty alleviation and health: an analysis of benefit spending among recipients of the U.S. earned income tax credit. BMC Public Health. 2023;23(1):1385. 10.1186/s12889-023-16296-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Parolin Z, Filauro S. The United States’ record-low child poverty rate in international and historical perspective: a research note. Demography. 2023;60(6):1665–1673. [DOI] [PubMed] [Google Scholar]
- 48. Trisi D. Expiration of Pandemic Relief Led to Record Increases in Poverty and Child Poverty in 2022. Center on Budget and Policy Priorities, June 10, 2024. Accessed August 15, 2024. https://www.cbpp.org/research/poverty-and-inequality/expiration-of-pandemic-relief-led-to-record-increases-in-poverty
- 49. US Department of Health and Human Services . Programs that use the poverty guidelines as part of eligibility determination. Content last reviewed November 5, 2019. Accessed July 26, 2024. https://www.hhs.gov/answers/hhs-administrative/what-programs-use-the-poverty-guidelines/index.html
- 50. Roming K. Social Security Lifts More People Above the Poverty Line Than Any Other Program. Washington, DC: Center on Budget and Policy Priorities; January 31, 2024. Accessed July 26, 2024. https://www.cbpp.org/research/social-security/social-security-lifts-more-people-above-the-poverty-line-than-any-other
- 51. US Department of Health and Human Services . Healthy People 2030. Objective SDOH-01: reduce the proportion of people living in poverty. Accessed July 26, 2024. https://health.gov/healthypeople/objectives-and-data/browse-objectives/economic-stability/reduce-proportion-people-living-poverty-sdoh-01
- 52. Lewallen J. From rules to representation: teaching about the territories and their delegates in the US Congress. PS: Political Science & Politics. 2017;50(2):497–500. [Google Scholar]
- 53. Ballotpedia . U.S. territories. Accessed July 25, 2024. https://ballotpedia.org/U.S._Territories
- 54. Ballotpedia . List of current members of the U.S. Congress. Accessed July 24, 2024. https://ballotpedia.org/List_of_current_members_of_the_U.S._Congress#Congressional_delegations_by_state
- 55. Massey DS. The prodigal paradigm returns: ecology comes back to sociology. In: Booth A, Crouter A, eds. Does It Take a Village? Community Effects on Children, Adolescents, and Families. Mahwah, NJ: Lawrence Erlbaum Associates; 2001:41–48. [Google Scholar]
- 56. Krieger N, Waterman PD, Gryparis A, Coull BA. Black carbon exposure, socioeconomic and racial/ethnic spatial polarization, and the Index of Concentration at the Extremes (ICE). Health Place. 2015;34:215–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Krieger N, Waterman PD, Spasojevic J, Li W, Maduro G, Van Wye G. Public health monitoring of privilege and deprivation with the Index of Concentration at the Extremes. Am J Public Health. 2016;106(2):256–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Larrabee Sonderlund A, Charifson M, Schoenthaler A, Carson T, Williams NJ. Racialized economic segregation and health outcomes: a systematic review of studies that use the Index of Concentration at the Extremes for race, income, and their interaction. PLoS One. 2022;17(1):e0262962. 10.1371/journal.pone.0262962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Tabb LP, Bayliss R, Xu Y. Spatial and spatio-temporal statistical implications for measuring structural racism: a review of three widely used residential segregation measures. Spatial Spatio-temporal Epidemiol. 2024;50:100678. 10.1016/j.sste.2024.100678 [DOI] [PubMed] [Google Scholar]
- 60. The Cook Political Report . The Cook Partisan Voting Index (Cook PVISM). Accessed July 24, 2024. https://www.cookpolitical.com/cook-pvi
- 61. The Cook Political Report . 2022 Cook PVISM: State Map and List. Accessed July 24, 2024. https://www.cookpolitical.com/cook-pvi/2022-partisan-voting-index/state-map-and-list
- 62. US Centers for Disease Control and Prevention . Infant mortality. Accessed July 25, 2024. https://www.cdc.gov/maternal-infant-health/infant-mortality/index.html
- 63. Reidpath DD, Allotey P. Infant mortality rate as an indicator of population health. J Epidemiol Community Health. 2003;57(5):344–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Gonzalez RM, Gilleskie D. Infant mortality rate as a measure of a country's health: a robust method to improve reliability and comparability. Demography. 2017;54(2):701–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Centers for Disease Control and Prevention . CDC WONDER. Accessed July 24, 2024. https://wonder.cdc.gov/
- 66. Fastrup J, Vinkenes M, O’Dell M. Public Health: A Health Status Indicator for Targeting Federal Aid to States. Washington, DC: US General Accounting Office; 1996. [Google Scholar]
- 67. Krieger N, Rehkopf DH, Chen JT, Waterman PD, Marcelli E, Kennedy M. The fall and rise of US inequities in premature mortality: 1960-2002. PLoS Med. 2008;5(2):e46. 10.1371/journal.pmed.0050046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. US Federal Government . Aging well: government benefits for older adults. Accessed July 25, 2024. https://www.benefits.gov/news/article/502
- 69. National Academies of Sciences, Engineering, and Medicine; Division of Behavioral and Social Sciences and Education; Committee on National Statistics; Committee on Population; Committee on Rising Midlife Mortality Rates and Socioeconomic Disparities . In: Becker T, Majmundar MK, Harris KM, eds. High and Rising Mortality Rates Among Working-Age Adults. National Academies Press (US); 2021. [PubMed] [Google Scholar]
- 70. Dowd JB, Doniec K, Zhang L, Tilstra A. US exceptionalism? International trends in midlife mortality. Int J Epidemiol. 2024;53(2):dyae024. 10.1093/ije/dyae024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. CDC, National Center for Health Statistics . Age adjustment. Accessed July 24, 2024. https://www.cdc.gov/nchs/hus/sources-definitions/age-adjustment.htm
- 72. US Census Bureau . American Community Survey data. Accessed July 24, 2024. https://www.census.gov/programs-surveys/acs/data.html
- 73. US Centers for Medicare and Medicaid Servies . InsureKidsNow.gov. Accessed July 25, 2024. https://www.insurekidsnow.gov/
- 74. Centers for Disease Control and Prevention . Vaccines for your child: why vaccinate your child. Accessed December 3, 2024. https://www.cdc.gov/vaccines-children/?CDC_AAref_Val=https://www.cdc.gov/vaccines/parents/why-vaccinate/index.html
- 75. Centers for Disease Control and Prevention . ChildVaxView. Accessed December 3, 2024. https://www.cdc.gov/childvaxview/?CDC_AAref_Val=https://www.cdc.gov/vaccines/imz-managers/coverage/childvaxview/index.html
- 76. Nandi A, Shet A. Why vaccines matter: understanding the broader health, economic, and child development benefits of routine vaccination. Hum Vaccin Immunother. 2020;16(8):1900–1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Hill HA, Yankey D, Elam-Evans LD, Chen M, Singleton JA. Vaccination coverage by age 24 months among children born in 2019 and 2020—National Immunization Survey-Child, United States, 2020–2022. MMWR Morb Mortal Wkly Rep. 2023;72(44):1190–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Centers for Disease Control and Prevention . Flu & people 65 years and older. Accessed July 25, 2024. https://www.cdc.gov/flu/highrisk/65over.htm
- 79. Roller-Wirnsberger R, Lindner S, Kolosovski L, et al. The role of health determinants in the influenza vaccination uptake among older adults (65+): a scope review. Aging Clin Exp Res. 2021;33(8):2123–2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Conrad A, Valour F, Vanhems P. Burden of influenza in the elderly: a narrative review. Curr Opin Infect Dis. 2023;36(4):296–302. [DOI] [PubMed] [Google Scholar]
- 81. America's Health Rankings . 2024 Senior Report. Flu vaccination—age 65+ in United States, 2022. Accessed July 25, 2024. https://www.americashealthrankings.org/explore/measures/flu_vaccine_sr
- 82. Panagiotakopoulos L, Godfrey M, Moulia DL, et al. Use of an additional updated 2023-2024 COVID-19 vaccine dose for adults aged ≥65 years: recommendations of the Advisory Committee on Immunization Practices—United States, 2024. MMWR Morb Mortal Wkly Rep. 2024;73(16):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Centers for Disease Control and Prevention . COVIDVaxView. Accessed December 3, 2024. https://www.cdc.gov/covidvaxview/?CDC_AAref_Val=https://www.cdc.gov/vaccines/imz-managers/coverage/covidvaxview/index.html
- 84. Rabbitt MP, Hales LJ, Burke MP, Coleman-Jensen A.. Household Food Security in the United States in 2022. Report No. ERR-325. US Department of Agriculture, Economic Research Service; 2023. 10.32747/2023.8134351.ers [DOI]
- 85. Thorndike AN, Gardner CD, Kendrick KB, et al. Strengthening US food policies and programs to promote equity in nutrition security: a policy statement from the American Heart Association. Circulation. 2022;145(24):e1077–e1093. 10.1161/CIR.0000000000001072 Erratum in: Circulation 2022; 146(9):e137. doi: 10.1161/CIR.0000000000001091. [DOI] [PubMed] [Google Scholar]
- 86. Abraham S, Breeze P, Sutton A, Lambie-Mumford H. Household food insecurity and child health outcomes: a rapid review of mechanisms and associations. Lancet. 2023;402(Suppl 1):S16. 10.1016/S0140-6736(23)02139-6 [DOI] [PubMed] [Google Scholar]
- 87. Gregory CA, Colman-Jensen A, eds. Food Insecurity, Chronic Disease, and Health among Working Age Adults. Economic Research Service Report no. 235.Washington, DC: US Department of Agriculture, Economics Research Service; 2017. [Google Scholar]
- 88. Mavegam Tango Assoumou BO, Coughenour C, Godbole A, McDonough I. Senior food insecurity in the USA: a systematic literature review. Public Health Nutr. 2023;26(1):229–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. US Department of Agriculture, Economic Research Service . Food security in the U.S. Key statistics and graphics. Last updated October 25, 2023. Accessed July 25, 2024. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/key-statistics-graphics/
- 90. March of Dimes . Nowhere to go: maternity care deserts across the U.S., 2018. Accessed July 26, 2024. https://www.marchofdimes.org/sites/default/files/2022-10/2018_Maternity_Care_Report.pdf
- 91. McGregor AJ, Addo NK, Amutah-Onukagha NN, Arroyo J. “I feel like that was the only option I had”: a qualitative study of structural inequities in obstetric hospital choice in Trenton, New Jersey. J Health Care Poor Underserved. 2022;33(4):1772–1792. [DOI] [PubMed] [Google Scholar]
- 92. Sonenberg A, Mason DJ. Maternity care deserts in the US. JAMA Health Forum. 2023;4(1):e225541. 10.1001/jamahealthforum.2022.5541 [DOI] [PubMed] [Google Scholar]
- 93. America's Health Rankings . Health of Women and Children Report Measures, 2023: Maternity Care Desert in United States (2021-2022). Accessed July 26, 2024. https://www.americashealthrankings.org/explore/measures/maternity_care_desert
- 94. Annie E. Casey Foundation, KIDS COUNT Data Center . Children in poverty in the United States. Accessed July 26, 2024. https://datacenter.aecf.org/data/tables/43-children-in-poverty
- 95. US Census Bureau . 2020 ACS 1-year experimental data release. Accessed July 24, 2024. https://www.census.gov/programs-surveys/acs/data/experimental-data.html
- 96. Krieger N, LeBlanc M, Waterman PD, Reisner SL, Testa C, Chen JT. Decreasing survey response rates in the time of COVID-19: implications for analyses of population health and health inequities. Am J Public Health. 2023;113(6):667–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Kutner MH, Nachtsheim C, Neter J, Li W. Applied Linear Statistical Models. 5th ed. New York: McGraw-Hill Irwin; 2005. [Google Scholar]
- 98. Gelman A. When to standardize regression inputs and when to leave them alone. July 11, 2009. Accessed July 28, 2024. https://statmodeling.stat.columbia.edu/2009/07/11/when_to_standar/
- 99. Miratrix LW, Sekhon JS, Theodoridis AG, Campos LF. Worth weighting? How to think about and use weights in survey experiments. Polit Anal. 2018;26(3):275–291. [Google Scholar]
- 100. Solon G, Haider SJ, Woolridge JM. What are we weighting for? J Human Resources. 2015;50(2):301–316. [Google Scholar]
- 101. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. Published correction appears in Stat Med. 2001;20(4):655. [DOI] [PubMed] [Google Scholar]
- 102. Kim HJ, Chen HS, Byrne J, Wheeler B, Feuer EJ. Twenty years since joinpoint 1.0: two major enhancements, their justification, and impact. Stat Med. 2022;41(16):3102–3130. [DOI] [PubMed] [Google Scholar]
- 103. US National Institutes for Health, National Cancer Institute . Joinpoint regression: basic method. Accessed July 28, 2024. https://surveillance.cancer.gov/help/joinpoint/references
- 104. US National Institutes for Health, National Cancer Institute . Joinpoint trend analysis software. Version 5.2.0 (June 3, 2024). Accessed July 28, 2024. https://surveillance.cancer.gov/joinpoint/
- 105. The R Project for Statistical Computing . R version 4.3.3. Released 2024-02-29. Accessed July 31, 2024. https://www.r-project.org/
- 106. Heron M. Deaths: leading causes for 2019. Natl Vital Stat Rep. 2021;70(9):1–114. 10.15620/cdc:107021 [DOI] [PubMed] [Google Scholar]
- 107. Curtin SC, Tejada-Vera B, Bastian BA. Deaths: leading causes for 2020. Natl Vital Stat Rep. 2023;72(13):1–115. 10.15620/cdc:133059 [DOI] [PubMed] [Google Scholar]
- 108. Lhila A, Alghanem F. Along party lines: examining the gubernatorial party difference in COVID-19 mortality rates in U.S. counties. Prev Med Rep. 2023;32:102142. 10.1016/j.pmedr.2023.102142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Michener J. Race, power, and policy: understanding state anti-eviction policies during COVID-19. Policy Soc. 2022;41(2):231–246. [Google Scholar]
- 110. Murray GR, Murray SM. Following the science? Examining the issuance of stay-at-home orders related to COVID-19 by U.S. governors. Am Polit Res. 2023;51(2):147–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Kaiser Family Foundation (KFF) . Status of state medicaid expansion decisions: interactive map. Published May 8, 2024. Accessed August 9, 2024. https://www.kff.org/affordable-care-act/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/
- 112. Haeder SF, Moynihan D. Race and racial perceptions shape burden tolerance for Medicaid and the supplemental nutrition assistance program. Health Aff (Millwood). 2023;42(10):1334–1343. [DOI] [PubMed] [Google Scholar]
- 113. Shaw M, Dorling D, Gordon D, Davey Smith G. The Widening Gap: Health Inequalities and Policy in Britain. Bristol, UK: The Policy Press; 1999. [Google Scholar]
- 114. Glymour MM. Using causal diagrams to understand common problems in social epidemiology. In: Oakes JM, Kaufman JS, eds. Methods in Social Epidemiology. 2nd ed. San Francisco, CA: Jossey-Bass; 2017:458–492. [Google Scholar]
- 115. Glymour MM. Using causal diagrams to understand common problems in social epidemiology. In: Oakes JM, Kaufman JS, eds. Methods in Social Epidemiology. 1st ed. San Francisco, CA: Jossey-Bass; 2006:393–428. [Google Scholar]
- 116. Jia N, Molloy R, Smith C, Wozniak A. The economics of internal migration: advances and policy questions. J Economics Lit. 2023;61(1):144–180. [Google Scholar]
- 117. Huang P, Butts CT. Rooted America: immobility and segregation of the intercounty migration network. Am Sociol Rev. 2023;88(6):1031–1065. [Google Scholar]
- 118. Spring A, Gillespie BJ, Mulder CH. Internal migration following adverse life events: assessing the likelihood of return migration and migration toward family. Popul Space Place. 2024;30(3):e2711. 10.1002/psp.2711 [DOI] [PubMed] [Google Scholar]
- 119. Vu C, Arcaya MC, Kawachi I, Williams DR. Moving to opportunity? Low birth weight outcomes among southern-born black mothers during the great migration. Soc Sci Med. 2023;328:115983. 10.1016/j.socscimed.2023.115983 [DOI] [PubMed] [Google Scholar]
- 120. Krieger N, Moallef S, Chen JT, et al. Politicians, power, and the people's health: US elections and state health outcomes, 2012-2024. Harvard Center for Population and Development Studies, Working Paper, Volume 24, Number 1, September 12, 2024. Accessed November 14, 2024. https://www.hsph.harvard.edu/population-development/wp-content/uploads/sites/2623/2024/09/24_krieger-et-al_electionshealth_HCPDS_msstablesfigssuppl_final_with-cover_noedits.pdf
- 121. Ballotpedia . Election results, 2024. Accessed November 14, 2024. https://ballotpedia.org/Election_results, _2024
- 122. Glenza J. Why the Trump administration will be bad for Americans’ health. The Guardian, November 12, 2024. Accessed November 14, 2024. https://www.theguardian.com/us-news/2024/nov/12/trump-adminstration-health-policy
- 123. Rodriguez A. How will a Trump presidency reshape US public health? A look at his plans. USA Today, November 13, 2024. Accessed November 14, 2024. https://www.usatoday.com/story/news/health/2024/11/13/trump-health-abortion-rfk-aca/76088963007/
- 124. Friedman L. Biden and environmental groups try to protect climate policies from Trump. New York Times, November 9, 2024. Accessed November 14, 2024. https://www.nytimes.com/2024/11/09/climate/biden-environmental-groups-climate-policies-trump.html
- 125. Baron Z, Twinamatsiko A, Ranganathan S. The impact of the election on health policy and the courts. Health Aff Forefront, November 14, 2024. Accessed November 14, 2024. https://www.healthaffairs.org/content/forefront/impact-election-health-policy-and-courts
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.