Abstract
The information needs of practicing clinicians are distinct from the needs of students, researchers, or nonclinical personnel. Clinicians seek information to stay current with new relevant medical developments and to find answers to patient-specific questions. The volume of available information makes clinicians' tasks of rapidly identifying high-quality studies daunting. New tools evaluate the rigor and relevance of information and summarize it in the form of synthesized clinical answers. These sources have the opposite focus of many other information tools in that they strive to provide less information rather than more. With the development of these sources of validated and refined information, a new search approach is needed to locate clinical information in which speed is the benchmark. The existing medical literature, including these new refinement tools, can be conceptualized as a pyramid, with the most useful information, based on validity and relevance, placed at the apex. Use of this hierarchy allows searchers to drill down through progressive layers until they find their answers. Librarians can play a significant role in evaluating the ever-increasing variety of these synthesized resources, placing them into the searching hierarchy, and training clinicians to search from the top down.
INTRODUCTION
The type, format, and sources of information in medicine are undergoing significant and rapid change. The increasing number and diversity of useful medical electronic databases and Internet sites owe their existence in large part to the growing body of evidence-based literature that seeks to connect clinicians with systematic observations from medical research. Medical librarians, in addition to their role in archiving information, are now focusing on providing more effective methods of information retrieval, usually through electronic means.
To meet the growing demand for electronic “just-in-time” information, many librarians are encouraging their users to build their own personalized portals to library home pages for quick access to the resources and services they use the most. Librarians are also looking to handheld computers to provide this information in a clinical setting.
These new retrieval systems also have the potential to provide new types of information, information that synthesizes “raw” information originating from original research findings into summaries and conclusions. Librarians are increasingly being asked to provide information that is filtered by scientific rigor and relevance to the clinical practice of medicine [1–4]. Information sources that evaluate the rigor and relevance of information and then summarize it in the form of synthesized answers to clinical questions can be very helpful in meeting this goal.
Summary sources of information have existed for some time, usually in the form of books, reviews, consensus reports, and expert statements from professional organizations. This new type of information differs from these older sources in that it strives to provide information that is more useful to clinicians in the day-to-day care of patients.
The needs of clinicians in practice are quite distinct from the needs of students, researchers, or nonclinical hospital or university personnel [5]. Clinicians usually seek information for two reasons: to stay current with new developments in medicine relevant to their practice or to find answers to patient-specific questions [6]. Different tools and methods are required for these different information needs. Clinicians need to be told about new information but also need a tool for quickly finding the information again when they need it.
Due to the time constraints imposed by medical practice, the usefulness of information retrieval systems and the information they provide are critical to busy clinicians. Clinicians generate highly specific patient-related questions at a rate of about one to three questions for every three patient visits [7, 8]. Of every ten questions posed, they only look up the answers to four and only find the answers to three [9]. Of those they do not look up, they estimate at least half are important. Thus, clinicians are guessing at seven of ten questions, due in large part to the amount of work it takes to find valid and reliable information that applies to their patients.
The traditional evidence-based medicine (EBM) approach focuses mainly on the critical evaluation of original research and other sources of primary information. Over the past several years, many librarians have become active partners in the EBM process by expanding their skills to include a better understanding of clinical research and its resulting literature [10]. Librarians are now teaching targeted searching techniques, quality filtering, and critical appraisal skills in their organizations [11]. However, this approach—the evaluation of the validity of medical information by individuals using it, whether by librarians or clinicians—is not as useful as it could be because of the excessive time involved and difficulty of integrating it into clinical medical practice at the point of need. Original research, as typically published, is not useful in the care of patients until it has been transformed in some manner.
The “usefulness” of any information source rests on the three characteristics outlined in this equation [12]:
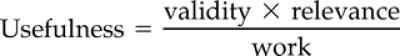 |
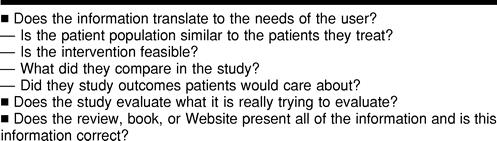
The validity of information refers to its scientific rigor (Table 1). A hierarchy exists of research study design, with some methodologies having greater scientific strength. The randomized controlled trial is the strongest type of design in clinical medicine. Even randomized trials may have design faults, and critical appraisal techniques have been developed to evaluate the validity of this type of research [13].
Table 1 Assessing the validity of information sources
Information in the medical literature also has various levels of relevance to practitioners of clinical medicine. The goal of medical practice is to help patients live long, healthy, functional, and symptom-free lives [14]. The most relevant information is research that directly evaluates the effectiveness of medical care on these outcomes that matter the most to patients.
This type of information is called “patient-oriented evidence that matters” (POEMs) [15]. This type of evidence evaluates the effectiveness of interventions that patients care about and that, as a result, clinicians care about as well. Most information in medicine, including most research, is preliminary in that it does not directly address the question of whether a particular medical approach is in the best interest of patients. POEMs contains information that directly tells clinicians that what they do for patients has been shown to make them live longer or live better.
For example, for many years anti-arrhythmic drugs were used to treat patients with asymptomatic cardiac ventricular arrhythmias because of their demonstrated effect on diminishing the frequency of arrhythmia. The supposition was that decreasing these arrhythmias would decrease patients' risk of sudden death, frequently the result of uncontrolled arrhythmic activity. After six years of use, the first study was performed to determine whether mortality was decreased in these patients. Much to everyone's surprise, mortality was actually significantly increased compared with untreated patients. This study was replicated several times, with the same results, and these drugs are used much less today.
This is just one example in which the preliminary information is not supported by research evaluating patient-oriented outcomes. There are many instances in which the early, “makes sense” data did not translate into benefits to patients. While this preliminary information is necessary to increase our knowledge of disease, it is “not ready for prime time” in the sense that clinicians should not base changes in practice on it. While this type of disease-oriented evidence (DOE) research is crucial to the development of better medical practice, it is not sufficient, in itself, for clinical decision making.
The goal of this new approach to medical information is to provide highly valid and relevant information while requiring the least amount of time and effort to locate and apply it to practice. To meet this goal, these new information sources have the opposite focus of many other information tools in that they strive to provide less information rather than more.
NEW INFORMATION SOURCES
Even with the development of electronic archiving and searching, the corpus of the medical literature is still so large as to effectively prevent its integration into clinical medicine. Since its inception, MEDLINE has been the database of choice for clinicians and librarians seeking medical information. One of this comprehensive biomedical database's strengths is its size, with over eleven million journal citations, but this size also makes it more challenging to search, and the burden of determining the validity and relevance of its articles is up to users.
In 1996, the National Library of Medicine addressed the need for clinicians to refine their MEDLINE search retrieval in PubMed by applying proven clinical filters. Clinical Queries [16] provide a way to limit search retrieval to articles about the four types of clinical research: diagnosis, etiology, therapy, and prognosis, as well as options to direct the emphasis of the search to be more sensitive or more specific.
Even information that can be rapidly retrieved must be evaluated for validity, and irrelevant information must be removed. Following retrieval and evaluation for relevance and validity, research findings must be compared and combined in ways that can be used to influence patient care.
Methods have been developed for combining research findings in an explicit and reproducible manner. Systematic review and meta-analysis are two such methods. Research findings are obtained in a comprehensive manner, evaluated for scientific rigor, and combined in a way that makes both clinical and scientific sense. In this way, a vast amount of medical literature can be summarized in a single document, “refining” the raw information into a finished product ready for clinical application.
“REFINED” SOURCES OF INFORMATION
In 1972, Archie Cochrane, a British epidemiologist, decried the unorganized way in which research findings were communicated to clinicians and stimulated thinking about ways to sift through the medical literature to find the nuggets of clinically relevant information and synthesize them [17]. In honor of his pioneering efforts, the Cochrane Collaboration [18] was set up in 1992 to make his vision real.
The Cochrane Collaboration is a mixture of volunteer and supported efforts from around the world. Its aim is to provide a clearinghouse for the best clinically relevant research information. By putting this information all in one spot, clinicians can quickly access this information to make decisions based on the best available evidence.
The Cochrane Database of Systematic Reviews is the flagship of the Cochrane Library [19]. Each of the reviews is aimed at answering a particular question (e.g., “are antibiotics effective in the treatment of otitis media in children?”). The methods used to identify all relevant research on a question are outlined in the review. Only results of randomized controlled trials, the most rigorous type of research, are used in the reviews. If possible, the authors of studies try to combine all of the study results (meta-analysis), trying to treat all of the separate studies as one big study to answer the question. The results and an answer to the question are provided in the review. These reviews are updated regularly.
Another approach to refining medical information is The Database of Abstracts of Reviews of Effectiveness (DARE) [20]. DARE, prepared by the National Health Centre for Reviews and Dissemination (CDR) at the University of York, England, United Kingdom, complements the Cochrane Database of Systematic Reviews by offering an annotated bibliography of quality-assessed reviews, primarily meta-analyses, in those subjects for which there is currently no Cochrane Review.
Practice guidelines are also designed to refine medical information into practical ways that can be used by clinicians. Not all practice guidelines, though, are based on the best clinical evidence. Guidelines can be categorized as either consensus-based (e.g., the National Institutes of Health Consensus Guidelines on osteoporosis prevention, diagnosis, and therapy [21]), evidence-based (American Heart Association Guidelines on pacemaker implantation [22]), or evidence-linked (e.g., American Gastroenterology Association Guidelines on management of intestinal ischemia [23]) [24]. The last group is the most useful, because the guidelines are stated and recommendations are linked in the guidelines to specific, graded evidence supporting the evidence. In this way, readers can see for themselves the strength of the evidence, rather than relying on the opinion of the authors of the guidelines for interpretation.
NEW APPROACHES TO INFORMATION RETRIEVAL
With the development of these sources of validated and refined information, a new approach is needed to access clinical information in which speed is the new benchmark. The existing medical literature, including these new refinement tools, can be conceptualized as a pyramid, with the most useful information, based on validity and relevance, placed at the apex (Figure 1). The Cochrane Library is placed at the top of the pyramid, because it provides the best evidence, synthesized and presented in a highly usable format. At the bottom of the pyramid are sources that are either expert based, and thus difficult to validate, or raw information that has not yet been synthesized into usable forms [25].
Figure 1.
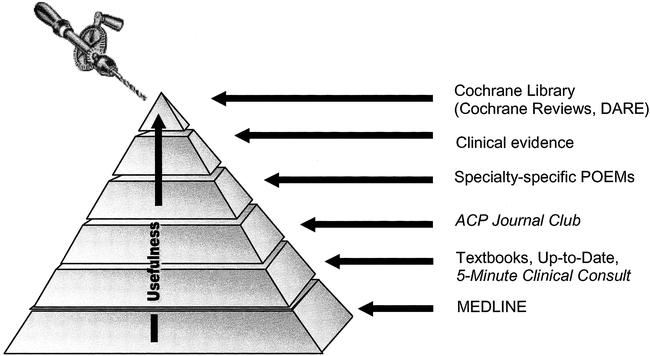
Drilling down for information
Use of this hierarchy allows searching to begin at the level of information with the highest usefulness. Starting at the top, searchers “drill down” through the progressive layers, encountering information along the way that is either less valid, less relevant, or harder to use. Rather than focusing on comprehensiveness, which would be the goal when preparing for a grant or clinical trial approval, searchers search only until finding the answer to a specific clinical question. The value of the hierarchy is that the best information is searched first, reducing the need for comprehensiveness.
This approach to the medical literature is similar to the tertiary-secondary-primary literature pyramid used by information specialists. What is different, though, is that searchers more sharply focus on information of greater usefulness (both valid and relevant), rather than treating each gradation of literature as being essentially equivalent.
CURRENT AWARENESS AND SEARCHING TOOLS FOR INFORMATION MASTERY
To help clinicians efficiently navigate the information pyramid and identify information of high relevance and validity, two specific tools are needed. Clinicians need a “first alert” method, a specialty-specific “POEM Bulletin Board,” for relevant new patient-oriented information as it becomes available. The myriad newsletters, Web-based systems, and other “current awareness” services attempt to fill this need. One recently released Daily POEM newsletter sends primary care based POEMs from a monthly database to subscribers via email. With few exceptions [26], these sources do not filter information based on relevance and validity and thus may not provide clinically useful information.
Clinicians also need a source for rapid retrieval of the information to which they have been alerted but that has not yet been integrated into their daily medical practice [27]. Computer-based sources are available that can provide information in less than thirty seconds [28]. Medical InfoRetriever is a tool developed by a family practice physician to meet the needs of busy clinicians in practice. It is a search engine with eight databases of information available on platforms for Web, desktop, and handheld computer access.
The aim of InfoRetriever is to provide “just-in-time” information to clinicians that they can retrieve while practicing, rather than putting off their information search for another time. The goal is to provide answers to search queries in less than one minute. All the information presented by InfoRetriever is highly filtered for relevance and validity. In addition, using InfoRetriever to answer questions forces clinicians to search the information pyramid from the “top down,” thus resulting in the highest-quality, evidence-based answer to each specific question. The databases searched by InfoRetriever are:
The Cochrane Database of Systematic Reviews presents only the abstracts and not the complete reviews.
POEMs abstracts from the Journal of Family Practice [29] are 700-word, structured, critically appraised abstracts and commentaries of original research articles published in 102 clinical medicine journals. Only research that provides patient-oriented evidence that matters is abstracted; preliminary research or research not meeting the criteria for validity from the Evidence-Based Medicine Working Group is not included.
Synopses from Evidence-Based Practice [30] is a monthly abstracting service that includes only articles meeting the POEMs criteria outlined above. These synopses are short (fewer than 300 words) and present unstructured abstracts and commentaries. This database presents information highly filtered for validity and clinical relevance [31]. This culled information is much more valuable than unfiltered sources of information, because the useless information has been removed.
Monographs from Griffith's 5-Minute Clinical Consult [32] present brief overviews of the diagnosis and management of about 1,000 topics. While not an evidence-based resource, it provides basic information that can be used to supplement the better sources of information also included in the database and allows clinicians to find an answer to almost all of their clinical questions.
Practice Guidelines: Summaries of evidence-linked and validated practice guidelines are provided in the guidelines. The desktop and Web-based versions also include links to “evidence-linked” practice guidelines available on the Internet.
Family Practice Inquiries Network (FPIN) Answers is a nationwide project designed to develop a database of questions arising in primary care with evidence-based answers supplemented with expert commentary.
Clinical Rules and Calculators provides clinical prediction calculators based on published research data. For example, one clinical rule allows clinicians to estimate the probability of a deep venous thrombosis based on the clinical symptoms of the patient [33].
History and Physical Exam Diagnostic Calculator presents calculators to determine the sensitivity, specificity, predictive values, and likelihood ratios of various history and physical examination findings. Clinicians can enter the pretest probability, and the calculations will automatically be updated.
Diagnostic Test Calculators determine the test characteristics of laboratory and imaging procedures. Clinicians can change the pretest probability to determine how the predictive values of the test will change.
Drug Database lists more than 1,300 drugs with basic information, such as adult and pediatric doses, safety in pregnancy and lactation, relative price, and managed care formulary inclusion.
InfoRetriever places highly valid, highly relevant information “at the fingertips” of clinicians, while they practice. Searches can be performed simultaneously on all eight databases, searching by text word or keyword (general clinical categories based on the International Classification of Diseases). Each database also can be browsed separately.
The search results screen presents a list of “hits.” The search findings are organized in order of decreasing quality of the evidence, based on criteria outlined by the Evidence-Based Medicine Working Group. In this way, clinicians can determine quickly what the information is and the degree of certainty.
Other tools are also being made available to provide clinicians with highly valid information. Ovid Technologies has developed an evidence-based medicine library that includes, in separate databases, the Cochrane Database of Systematic Reviews and Controlled Trials, the Database of Abstracts of Reviews of Effectiveness, and ACP Journal Club [34]. The BMJ Publishing Group produces Clinical Evidence, an updated paper, Web, or CD-ROM compilation of current evidence on the prevention and treatment of many common clinical conditions [35]. Clinical Evidence, also available by subscription from Ovid, is unique in that it details the gaps and uncertainties in the current medical knowledge. Knowing where the “holes” are in the evidence on a given subject is just as important as knowing what evidence is available.
THE LIBRARIAN'S ROLE
The growing number of evidence-based information sources, initially developed to streamline the information-gathering process for clinical decision making, are now in need of being managed themselves. Librarians—by virtue of their traditional roles in collection development, literature searching, and end-user training—are in a wonderful position to study the strengths and weaknesses of these new tools to determine whether they are truly evidence based and present patient-oriented evidence that matters.
If resources meet these criteria, librarians can place them into the proper level of the searching hierarchy. The placement of a resource into the EBM searching hierarchy is an attempt to balance the “usefulness equation” for that resource when compared to another. Librarians are uniquely aware of the intricacies of a broad range of search systems, allowing them to rank their usefulness more easily. For example, the simultaneous search feature in Ovid's evidence-based medicine library for searching Cochrane, DARE, and ACP Journal Club with one strategy enhances the overall usefulness of these products by lowering the work part of the equation.
Clinicians, who may not be aware of the variety of refined information sources and timesaving search features that exist, will benefit from librarians' organization of searching hierarchies. With such a framework in place, librarians can emphasize the location of relevant retrieval with minimal time and effort by training clinicians to search the usefulness pyramid from the top down
INFORMATION MASTERY
All information in medicine is not created equal; most of the currently available medical information either is too preliminary to warrant a change in clinical medicine or is otherwise not relevant to clinical medicine. The goal of clinicians is to rapidly identify and use high-quality information in the course of their practice. Unfortunately, the volume of information available to them makes this task daunting without specific tools. Further, information that is presented in its raw (i.e., originally published) form is not useful to clinicians, until they or someone else can evaluate and summarize it. A growing number and variety of new tools that are sources of highly filtered, highly relevant information are available. Librarians can play a significant role in helping clinicians evaluate the clinical value of these resources. These new tools, placed within a searching framework based on the usefulness equation, offer the promise that all clinicians can use resources that retrieve information with the highest relevance and validity with the lowest work, thereby becoming “information masters.”
Contributor Information
Karen K. Grandage, Email: kgrandage@virginia.edu.
David C. Slawson, Email: dslawson@virginia.edu.
Allen F. Shaughnessy, Email: ashaughnessy@pinnaclehealth.org.
REFERENCES
- Eldredge JD. Evidence-based librarianship: an overview. Bull Med Libr Assoc. 2000 Oct; 88(4):289–302. [PMC free article] [PubMed] [Google Scholar]
- Rader T, Gagnon AJ. Expediting the transfer of evidence into practice: building clinical partnerships. Bull Med Libr Assoc. 2000 Jul; 88(3):247–50. [PMC free article] [PubMed] [Google Scholar]
- Scherrer CS, Dorsch JL. The evolving role of the librarian in evidence-based medicine. Bull Med Libr Assoc. 1999 Jul; 87(3):322–8. [PMC free article] [PubMed] [Google Scholar]
- McKibbon KA. Evidence-based practice. Bull Med Libr Assoc. 1998 Jul; 86(3):396–401. [PMC free article] [PubMed] [Google Scholar]
- Gruppen LD. Physician information seeking: improving relevance through research. Bull Med Libr Assoc. 1990 Apr; 78(2):165–72. [PMC free article] [PubMed] [Google Scholar]
- Thompson ML. Characteristics of information resources preferred by primary care physicians. Bull Med Libr Assoc. 1997 Apr; 85(2):187–92. [PMC free article] [PubMed] [Google Scholar]
- Covell DG, Uman GC, and Manning PR. Information needs in practice: are they being met? Ann Intern Med. 1985 Oct; 103(4):596–9. [DOI] [PubMed] [Google Scholar]
- Osheroff JA, Forsythe DE, Buchanan BG, Bankowitz RA, Blumenfeld BH, and Miller RA. Physicians' information needs: analysis of questions posed during clinical teaching. Ann Intern Med. 1991 Apr 1; 114(7):576–81. [DOI] [PubMed] [Google Scholar]
- Ely JW, Osheroff JA, Ebell MH, Bergus GL, Levy BT, Chambliss ML, and Evans ER. Analysis of questions asked by family doctors regarding patient care. Br Med J. 1999 Aug 7; 319(7206):358–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKibbon KA. Evidence-based practice. Bull Med Libr Assoc. 1998 Jul; 86(3):396–401. [PMC free article] [PubMed] [Google Scholar]
- Scherrer CS, Dorsch JL. The evolving role of the librarian in evidence-based medicine. Bull Med Libr Assoc. 1999 Jul; 87(3):322–8. [PMC free article] [PubMed] [Google Scholar]
- Shaughnessy AF, Slawson DC, and Bennett JH. Becoming an information master: a guidebook to the medical information jungle. J Fam Pract. 1994 Nov; 39(5):489–99. [PubMed] [Google Scholar]
- Oxman AD, Sackett DL, and Guyatt GH. Users' guides to the medical literature. I. how to get started. JAMA. 1993 Nov 3; 270(17):2093–5. [PubMed] [Google Scholar]
- Slawson DC, Shaughnessy AF, and Bennett JH. Becoming a medical information master: feeling good about not knowing everything. J Fam Pract. 1994 May; 38(5):505–13. [PubMed] [Google Scholar]
- Shaughnessy AF, Slawson DC, and Bennett JH. Becoming an information master: a guidebook to the medical information jungle. J Fam Pract. 1994 Nov; 39(5):489–99. [PubMed] [Google Scholar]
- Haynes RB, Wilczynski N, McKibbon KA, Walker CJ, and Sinclair JC. Developing optimal search strategies for detecting clinically sound studies in MEDLINE. J Am Med Inform Assoc. 1994 Nov–Dec; 1(6):447–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochrane A. 1931–1971: a critical review, with particular reference to the medical profession. In: Medicines for the year 2000. London, U.K.: Office of Health Economics, 1979:1–11. [Google Scholar]
- General information. [Web document]. The Cochrane Library, 1999. [rev. 1 Feb 2000; cited 20 Feb 2002]. <http://www.update-software.com/ccweb/cochrane/general.htm>. [Google Scholar]
- The Cochrane Library. [Web document]. Update Software, 2002. [cited 20 Feb 2002]. <http://www.updateusa.com/clibhome/clib.htm>. [Google Scholar]
- Centre for Reviews and Dissemination, National Health Service. Searching CRD databases. [Web document]. York, U.K.: University of York. [cited 6 Aug 2001]. <http://144.32.228.3/scripts/WEBC.EXE/NHSCRD/start/>. [Google Scholar]
- Osteoporosis prevention, diagnosis, and therapy. NIH Consens Statement. 2000 Mar 27–29; 17(1):1–36. [PubMed] [Google Scholar]
- Gregoratos G, Cheitlin MD, Conill A, Epstein AE, Fellows C, Ferguson TB Jr.,, Freedman RA, Hlatky MA, Naccarelli GV, Saksena S, Schlant RC, Silka MJ, Ritchie JL, Gibbons RJ, Eagle KA, Gardner TJ, Lewis RP, O'Rourke RA, Ryan TJ, and Garson A Jr. ACC/AHA guidelines for implantation of cardiac pacemakers and antiarrhythmia devices: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Pacemaker Implantation). J Am Coll Cardiol. 1998 Apr; 31(5):1175–209. [DOI] [PubMed] [Google Scholar]
- American Gastroenterological Association medical position statement: guidelines on intestinal ischemia. Gastroenterology. 2000 May; 118(5):951–3. [DOI] [PubMed] [Google Scholar]
- Becker LA, Slawson DC, and Shaughnessy AF. Practice guidelines: the good, the questionable, the ugly. J Fam Pract 2002:submitted for publication. [Google Scholar]
- Oxman AD, Guyatt GH. The science of reviewing research. Ann N Y Acad Sci. 1993 Dec 31; 703:125–33. [DOI] [PubMed] [Google Scholar]
- Nutting PA. Tools for survival in the information jungle. J Fam Pract 1999;48(5):339–40. [Google Scholar]
- Jacobson LD, Edwards AG, Granier SK, and Butler CC. Evidence-based medicine and general practice. Br J Gen Pract 1997;47:449–52. [PMC free article] [PubMed] [Google Scholar]
- Straus SE. Bringing evidence to the point of care [EBM note]. Evidence-Based Medicine. 1999 May–Jun; 4:70–1. [Google Scholar]
- The Journal of Family Practice POEMs. [Web document]. [cited 6 Aug 2001]. <http://www.jfponline.com/display_archives.asp?YEAR=POEMs>. [Google Scholar]
- Evidence-based practice. [Web document]. Dowden Health Media, 2001. [cited 6 Aug 2001]. <http://www.ebponline.net>. [Google Scholar]
- Validity and relevance: how do we evaluate validity and relevance? [Web document]. InfoPOEMs. [cited 6 Aug 2001]. <http://www.medicalinforetriever.com/validity.cfm>. [Google Scholar]
- Dambro MR. ed. Griffith's 5-Minute clinical consult. 9th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2001. [Google Scholar]
- Wells PS, Anderson DR, Bormanis J, Guy F, Mitchell M, Gray L, Clement C, Robinson KS, and Lewandowski B. Value of assessment of pretest probability of deep-vein thrombosis in clinical management. Lancet. 1997 Dec 20–27; 350(9094):1795–8. [DOI] [PubMed] [Google Scholar]
- Products & services: evidence-based medicine reviews. [Web document]. New York, NY: Ovid Technologies. [cited 6 Aug 2001]. <http://www.ovid.com/products/clinical/ebmr.cfm>. [Google Scholar]
- Clinical evidence. [Web document]. London, U.K.: BMJ Publishing Group [cited 6 Aug 2001]. <http://www.clinicalevidence.org>. [Google Scholar]


