Abstract
Rare and common genetic variants contribute to the risk of atrial fibrillation (AF). Although ion channels were among the first AF candidate genes identified, rare loss-of-function variants in structural genes such as TTN have also been implicated in AF pathogenesis partly by the development of an atrial myopathy, but the underlying mechanisms are poorly understood. While TTN truncating variants (TTNtvs) have been causally linked to arrhythmia and cardiomyopathy syndromes, the role of missense variants (mvs) remains unclear. We report that rare TTNmvs are associated with adverse clinical outcomes in AF patients and we have identified a mechanism by which a TTNmv (T32756I) causes AF. Modeling the TTN-T32756I variant using human induced pluripotent stem cell-derived atrial cardiomyocytes (iPSC-aCMs) revealed that the mutant cells display aberrant contractility, increased activity of a cardiac potassium channel (KCNQ1, Kv7.1), and dysregulated calcium homeostasis without compromising the sarcomeric integrity of the atrial cardiomyocytes. We also show that a titin-binding protein, the Four-and-a-Half Lim domains 2 (FHL2), has increased binding with KCNQ1 and its modulatory subunit KCNE1 in the TTN-T32756I-iPSC-aCMs, enhancing the slow delayed rectifier potassium current (Iks). Suppression of FHL2 in mutant iPSC-aCMs normalized the Iks, supporting FHL2 as an Iks modulator. Our findings demonstrate that a single amino acid change in titin not only affects function but also causes ion channel remodeling and AF. These findings emphasize the need for high-throughput screening to evaluate the pathogenicity of TTNmvs and establish a mechanistic link between titin, potassium ion channels, and sarcomeric proteins that may represent a novel therapeutic target.
INTRODUCTION
Atrial fibrillation (AF), the most prevalent cardiac arrhythmia, affects more than 60 million people worldwide and is associated with increased risk for stroke, heart failure, and dementia, justifying it as a major public healthcare burden2,3. AF is characterized by irregular and often abnormally fast heart rates4,5. Over the last decade, tremendous progress has been made in understanding the genetic architecture of AF6–8. Genome-wide association studies have identified over 140 common loci associated with AF, while family-based studies have implicated rare variants primarily encoding ion channels9,10. Although AF has been traditionally classified as a ‘channelopathy’, variants in myocardial sarcomeric proteins such as titin have been increasingly associated with familial or early-onset AF11,12.
The TTN gene encodes for a massive myofilament (~4200 kDa), titin, which stretches along the Z-disk (N-terminus) to the M-band (C-terminus) region of the sarcomere13,14. Titin serves as a molecular scaffold for other muscle proteins, participates in downstream signaling, and provides passive tension to cardiac muscle15,16. Due to its large size, the rate of genetic variation in TTN is high, including both truncating (TTNtvs) and missense variants (TTNmvs)1,17. The prevalence of rare TTNtvs and TTNmvs in the general population is 2% and 5.7%, respectively18–20. While TTNtvs are the most common genetic cause (10–20%) of dilated cardiomyopathy (DCM), TTNmvs are often disregarded in clinical practice, fulfilling a stand-alone benign criterion in DCM-specific variant interpretation frameworks based on the American College of Medical Genetics (ACMG) recommendations21,22. Yet, TTNmvs may have the potential to confer disease, as a recent study in two families revealed that TTNmvs in a conserved cysteine of TTN can cause DCM23. Another study demonstrated segregation of a novel TTNmv among five individuals with atrioventricular block in a Chinese family, suggesting that TTNmvs may also be implicated in arrhythmia syndromes24. To date, a relationship between rare TTNmvs and AF has not been explored at either clinical or mechanistic levels. This has potentially heightened importance across racial and ethnic groups, in whom the likelihood of detecting variants of uncertain significance (which are predominantly TTNmvs), is higher than in individuals of European descent25.
Despite the clinical importance, the pharmacological therapy of AF is limited in part because of the incomplete understanding of the myocardial substrate for AF as human atrial tissue is rarely available and the limitations of existing in vitro and in vivo models26. However, human induced pluripotent stem cell-derived atrial cardiomyocytes (iPSC-CMs) not only possess the complex array of cardiac ion channels that make up the atrial action potential (AP) but also hold great promise for modeling AF27,28. Modeling patient-specific mutations associated with familial AF using mature human iPSC-CMs offers a powerful, naturally integrated system with distinct advantages over animal models and heterologous expression systems29. Recent reports using human iPSC-CM models have elucidated the pathophysiological mechanisms of DCM30, hypertrophic cardiomyopathy31, Brugada syndrome32, long QT syndrome33, and AF27,29,34. Human iPSC-CMs also have the potential to uncover the molecular mechanisms of AF as they can be easily modified to contain the precise genetic background of the individual patient35–37.
To examine the potential role of TTNmvs in AF, we examined the prevalence of rare TTNmvs in a single-center cohort of African-American and Hispanic/Latinx individuals with AF who underwent whole exome sequencing, compared clinical characteristics between TTNmv carriers and non-carriers, and evaluated whether TTNmvs were associated with increased risk of AF or heart failure (HF)-related hospitalizations. To explore whether the TTNmvs may be mechanistically linked to the development of AF, we introduced a rare TTNmv (TTN-T32756I) into human iPSC-aCMs using clustered regularly interspaced short palindromic repeats-associated 9 (CRISPR-Cas9). We performed electrophysiological (EP), pharmacological, and mechanistic analyses to elucidate the mechanisms by which the TTNmv causes AF. Our study showed that the TTN-T32756I iPSC-aCMs exhibited a striking AF-like EP phenotype in vitro, and transcriptomic analyses revealed that the TTNmv increases the activity of the Four-and-a-half LIM domain protein 2 (FHL2) which then modulates the slow delayed rectifier potassium current (IKs) to cause AF, possibly through a reentrant mechanism.
RESULTS
TTNmvs are associated with increased hospitalization risk in a multiethnic cohort with AF.
Clinical characteristics:
A total of 131 subjects were included (mean [SD] age at AF diagnosis 63.5 [13.8] years, 70 [53.4%] male, 38 [29%] Hispanic/Latinx, 93 [71%] non-Hispanic Black; Table 1). We identified 138 TTNmvs, most commonly in the TTN A-band (108 [78.8]%), followed by the I-band (20 [14.6%]), M-band (2 [1.5%]), near the Z-disk (6 [4.4%], and in the Z-disk (2 [1.5%]) (Figure 1A, Supplementary Table 1). Based on the REVEL in silico score, 52 (37.7%) TTNmvs variants were predicted to be deleterious. A total of 77 (58.8%) subjects carried a TTNmv, with 43 (32.8%) carrying a predicted deleterious variant. Carriers of a TTNmv had a higher QTc interval on electrocardiogram (ECG) closest to AF diagnosis (mean [SD] 466.5 [42.3] vs. 449.6 [37.7] ms, P=0.027); there were otherwise no other significant clinical or demographic differences between variant carriers and non-carriers. When stratifying by predicted deleterious TTNmv only (Supplementary Table 2), a higher proportion of variant carriers were non-Hispanic Black (36 [83.7%] vs. 57 [64.8%], P=0.026). On index ECG, carriers additionally had higher ventricular rate (mean [SD] 103.7 [31.4] vs. 90.9 [27.4] beats/min, P=0.022), QTc interval (mean [SD] 470.6 [44.0] vs. 453.9 [38.7] ms, P=0.035), and LVEDD on index echocardiogram (mean [SD] 49.8 [8.0] vs. 45.6 [9.2] mm, P=0.021). Seventeen (15.2%) subjects met criteria for left ventricular (LV) dilatation, with a higher proportion of LV dilatation in TTNmv carriers but without a significant difference compared to non-carriers (13 [20.3%] vs. 4 [8.3%], P=0.111). Twelve subjects (9.2%) met criteria for a clinical diagnosis of nonischemic DCM based on a left ventricular ejection fraction (LVEF) <50%, presence of LV dilatation, and confirmation of non-severe coronary artery disease by coronary angiography. Of those, 8 subjects carried TTNmvs of which 6 were predicted to be deleterious (Supplementary Table 3).
Table 1: Clinical characteristics of ethnic minority subjects with AF stratified by presence of rare missense TTN variants.
*Data are missing for the following variables: eGFR (1), electrocardiogram within 3 months of AF diagnosis (11), LVEDD (19), left atrial size (6), left atrial diameter (21). Left ventricular dilatation is defined as left ventricular end diastolic diameter greater than 2 standard deviations above the normal sex-specific mean value. Variants with a REVEL score ≥ 0.7 were defined as predicted deleterious. Continuous data are represented as mean (standard deviation) and categorical data are represented as count (%).
| TTN Missense Absent | TTN Missense Present | Total | ||
|---|---|---|---|---|
| (N=54) | (N=77) | (N=131) | P-value | |
| Mean age at AF diagnosis (years) | 64.3 (15.2) | 62.9 (12.9) | 63.5 (13.8) | 0.575 |
| Male sex | 30 (55.6%) | 40 (51.9%) | 70 (53.4%) | 0.724 |
| Race/ethnicity | 0.696 | |||
| Non-Hispanic Black | 37 (68.5%) | 56 (72.7%) | 93 (71.0%) | |
| Hispanic/Latinx | 17 (31.5%) | 21 (27.3%) | 38 (29.0%) | |
| BMI (kg/m2) | 33.7 (9.0) | 34.2 (10.1) | 34.0 (9.6) | 0.765 |
| Diabetes | 18 (33.3%) | 32 (41.6%) | 50 (38.2%) | 0.366 |
| Hypertension | 45 (83.3%) | 68 (88.3%) | 113 (86.3%) | 0.448 |
| Coronary artery disease | 13 (24.1%) | 20 (26.0%) | 33 (25.2%) | 0.841 |
| History of stroke/transient ischemic attack | 8 (14.8%) | 18 (23.4%) | 26 (19.8%) | 0.270 |
| Congestive heart failure | 21 (38.9%) | 33 (42.9%) | 54 (41.2%) | 0.720 |
| Nonischemic dilated cardiomyopathy | 4 (7.7%) | 8 (11.1%) | 12 (9.7%) | 0.760 |
| Estimated glomerular filtration rate (mg/dL) | 71.8 (24.4) | 67.2 (24.7) | 69.1 (24.6) | 0.297 |
| Ventricular rate | 92.1 (29.0) | 97.5 (29.6) | 95.3 (29.4) | 0.326 |
| QRS interval (ms) | 97.6 (23.7) | 100.2 (28.1) | 99.2 (26.3) | 0.593 |
| QTc interval (ms) | 449.6 (37.7) | 466.5 (42.3) | 459.6 (41.2) | 0.027 |
| Left ventricular ejection fraction (%) | 0.722 | |||
| Normal (≥50%) | 32 (59.3%) | 45 (58.4%) | 77 (58.8%) | |
| Mildly decreased (40–49%) | 7 (13.0%) | 7 (9.1%) | 14 (10.7%) | |
| Moderately decreased (30–39%) | 4 (7.4%) | 9 (11.7%) | 13 (9.9%) | |
| Severely decreased (20–29%) | 7 (13.0%) | 9 (11.7%) | 16 (12.2%) | |
| Very severely decreased (< 20%) | 4 (7.4%) | 7 (9.1%) | 11 (8.4%) | |
| Left ventricular end diastolic diameter (mm) | 45.3 (9.2) | 47.8 (9.8) | 46.7 (9.5) | 0.180 |
| Left ventricular dilatation | 4 (8.3%) | 13 (20.3%) | 17 (15.2%) | 0.111 |
| Left atrial size | 0.675 | |||
| Normal | 17 (32.7%) | 21 (28.8%) | 38 (30.4%) | |
| Mildly dilated | 15 (28.8%) | 23 (31.5%) | 38 (30.4%) | |
| Moderately dilated | 13 (25.0%) | 17 (23.3%) | 30 (24.0%) | |
| Severely dilated | 7 (13.5%) | 12 (16.4%) | 19 (15.2%) | |
| Left atrial diameter (mm) | 39.6 (7.4) | 41.2 (7.7) | 40.5 (7.6) | 0.286 |
| Number of TTN missense variants | - | |||
| 0 | 54 (100.0%) | 0 (0.0%) | 54 (41.2%) | |
| 1 | 0 (0.0%) | 37 (48.1%) | 37 (28.2%) | |
| 2 | 0 (0.0%) | 26 (33.8%) | 26 (19.8%) | |
| >2 | 0 (0.0%) | 14 (18.2%) | 14 (10.7%) | |
| Number of predicted deleterious TTN missense variants | - | |||
| 0 | 54 (100.0%) | 34 (44.2%) | 88 (67.2%) | |
| 1 | 0 (0.0%) | 34 (44.2%) | 34 (26.0%) | |
| 2 | 0 (0.0%) | 9 (11.7%) | 9 (6.9%) |
Figure 1: TTNmv prevalence and association with hospitalization in a multiethnic atrial fibrillation (AF) cohort.
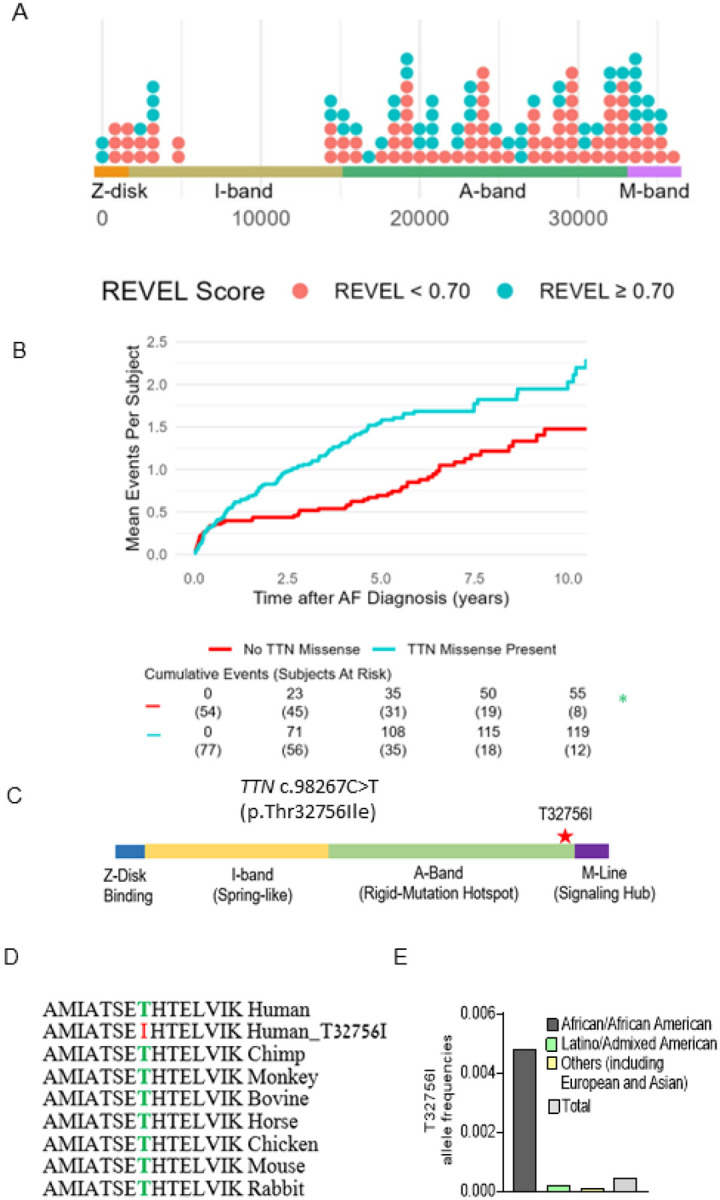
A) Distribution of TTNmv in multiethnic AF cohort based on amino acid position in the TTN gene, stratified by REVEL in silico score for prediction of deleterious effect, defined by REVEL ≥ 0.70. (B) Mean cumulative incidence of AF and heart failure (HF)-related hospitalizations in subjects with AF stratified by presence of TTNmv. Hazard ratio (HR), 95% confidence interval (CI), and P-value were obtained from univariable Cox proportional hazard modeling. (C) Diagram denoting the location of TTNmv-T23756I. (D) Sequence alignment shows that the region of the T23756I is highly conserved across vertebrate species. (E) Allele frequencies of TTN-T3265I in various ethnic groups (gnomAD).
TTNmvs are associated with higher hospitalization risk:
A total of 174 hospitalizations (64 AF-related and 110 HF-related) occurred after a median (interquartile range [IQR]) follow-up time of 4.14 (1.25–6.04) years, with 119 (68.4%) events occurring in TTNmv carriers and 55 (31.6%) of events occurring in non-TTNmv carriers. Thirty-nine (50.6%) subjects with a TTNmv experienced at least one hospitalization during the follow-up period compared to 22 (40.1%) of non-carriers, and total hospitalization incidence rate was 32.2 events per 100 person-years (p-y) in TTNmv carriers compared to 17.4 per 100 p-y in non-carriers. Mean cumulative incidence is shown in Figure 1B. The unadjusted hazard of hospitalization by 10 years was significantly higher in TTNmv carriers compared to noncarriers (hazard ratio [HR] 1.81, 95% confidence interval [CI] 1.04–3.15, p=0.036). This remained significant after partial adjustment for age and sex (HR 1.82, 95% CI 1.04–3.17, p=0.035) as well as full adjustment that additionally included ethnicity and baseline LVEF <50% (HR 1.80, 95% CI 1.03–3.15, p=0.039; Supplementary Table 4). No other covariates were significantly associated with the outcome. To assess whether baseline LVEF influenced the relationship between TTNmvs and hospitalization risk, an interaction term between LVEF<50% and presence of TTNmvs was tested and was not significant (interaction P=0.843). To assess whether prediction of deleterious effect influenced the relationship between TTNmv presence and hospitalization risk, subgroups based on high or low REVEL score were separately examined (Supplementary Table 5). Compared to non-TTNmv carriers, hospitalization risk was significantly increased in subjects carrying predicted deleterious TTNmvs (HR 1.92, 1.04–3.53, P=0.036). While subjects with TTNmvs not predicted to be deleterious also had an elevated point estimate of hospitalization risk, this difference was not significant (HR 1.60, 95% CI 0.78–3.28, P=0.198). Findings remained similar with exclusion of patients with nonischemic DCM (Supplementary Table 6). While in a previous study we identified likely pathogenic or pathogenic AF variants in 7.0% of ethnic minority probands with most (46.7%) TTNtvs12, these results suggest that TTNmvs are also linked with adverse clinical outcomes and missense variants should be considered in assessing pathogenicity in clinical and genetic contexts.
A single amino acid change in a TTNmv is potentially causative of AF.
We identified three early-onset paroxysmal AF probands from separate families harboring the same rare TTNmv (Chr 2q31.2 (GRCh38): g. 178539797G>A). The clinical characteristics of the three probands are summarized in Table 2. This missense variant localizes in the A-band of TTN and causes the substitution of a conserved residue threonine by an isoleucine (p.Thr32756Ile, NM_001267550.2 (TTN), c.98267C>T (Figure 1C–D, Supplementary Figure 1A). In the gnomAD reference population, the TTN-T32756I variant has a frequency of 0.000245 overall, at a frequency of 0.0046 within the subpopulation of African ancestry and is impartially distributed across sexes and different ages (Figure 1E, Supplementary Figure 1B–E). The TTNmv has also been described in Clinvar (NM_001267550.2(TTN):c.98267C>T (p.Thr32756Ile), Supplementary Table 7) and gnomAD v4.0.0 (SNV:2–178539798-G-A(GRCh38)) in patients with DCM and other diseases.
Table 2:
Clinical characteristics of the early-onset AF patients with TTN-T32756I variation.
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Age range at the diagnosis (years) | 51–55 | 61–65 | 36–40 |
| Sex | Male | Female | Male |
| Race/ethnicity | Hispanic | Black | Black |
| Body mass index (kg/m 2 ) | 42.2 | 26.9 | 31.4 |
| Type | Paroxysmal | Paroxysmal | Paroxysmal |
| Comorbidities | Hypertension Prostate cancer | Hypertension Hyperlipidemia Coronary artery disease Uterine/vulva cancer Severe mitral regurgitation |
Hypertension Asthma |
| Family history | No | No | No |
| Presenting symptoms | Asymptomatic, found during preoperative evaluation | Asymptomatic, in setting of gastrointestinal bleed | Palpitations, dyspnea |
| LA size (mm) | 51 | 33 | 35 |
| LVEF (%) | 55 | 50 | 60 |
| Antiarrhythmic drug | No | No | No |
| Ablation | Yes | No | No |
| Cardioversion | Yes | No | Yes |
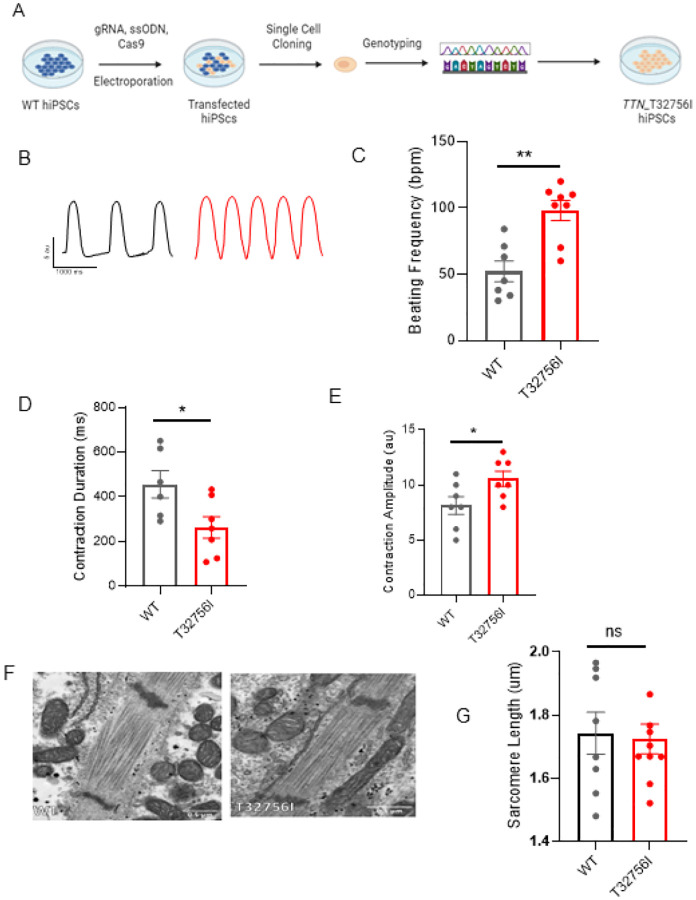
TTN-T32756I iPSC-aCMs display aberrant contractility without affecting the sarcomere integrity:
To functionally characterize the TTN-T32756I variant, we exploited wild-type (WT) human iPSC lines and introduced the point mutation c.98267C>T in the TTN allele (Figure 2A, Supplementary Figure 2A–B). The iPSC lines expressing the pluripotent markers Sox2 and Oct4 and showing normal karyotype were first differentiated into cardiomyocytes (Supplementary Figure 2C–D), and then a retinoic acid-based and comprehensive maturation protocol was applied to generate the iPSC-aCMs as we described previously26,27. Given that cardiac contractility is a key component of heart function and is linked to cardiac disorders associated with TTN38, we first assessed the contractility of the WT and mutant iPSC-aCMs and observed both reduced contraction and abnormal relaxation in TTN-T32756I-iPSC-aCMs (Figure 2B–E, Supplementary Figure 3A–B). Compared to WT, the beating frequency of the TTN-T32756I-iPSC-aCMs was significantly increased (52 ± 7.8 vs. 98 ± 7.5 beats per min, P=0.001; Figure 2C) coupled with the reduction of the contraction duration (456.5 ± 61.45 vs 262.9 ± 48.16 msec, P=0.032; Figure 2D), the peak-to-peak time (1529 ± 195.5 vs 636.6 ± 135.8 msec, P=0.004; Supplementary Figure 3B), and the relaxation (281.5 ± 42.95 vs 79.40 ± 21.14 msec, P=0.003; Supplementary Figure 3A). The contraction amplitude of the mutant was also increased (8.1 ± 0.8 vs 10.6 ± 7 au, P=0.040) without any significant changes in time-to-peak (Figure 2E, Supplementary Figure 3C), suggesting an increased contractile force by the TTN-T32756I-iPSC-aCMs. As sarcomere disorganization is often found in TTN-related cardiomyopathies and underlies contractile dysfunction39, we explored whether TTNmvs perturbed the organization of the sarcomere. Surprisingly, we did not find any disarray in the sarcomeres of either WT or TTN-32756I-iPSC-aCMs. Using transmission electron microscopy (TEM) and immunofluorescence (IF), we observed symmetrical arrays of recurring sarcomeres in the WT and the mutant atrial cardiomyocytes with no changes in the sarcomere length (Figure 2F–G, Supplementary Figure 3D–F). Although no sarcomeric perturbation by the T32756I variant was observed, the aberrant contractility displayed by the TTN-T32756I-iPSC-aCMs suggests that the TTNmv may be pathogenic.
Figure 2: Human induced pluripotent stem cell-derived atrial cardiomyocytes (iPSC-aCMs) carrying TTN-T32756I variants have atypical contractility but no sarcomere disorganization.
(A) Workflow to generate the CRISPR/Cas9-mediated iPSC line carrying TTN-T32756I missense variation. (B-E) Contraction profile of wild type (black) and TTN-T32756I (Red) iPSC-aCMs showing increased beating frequency (C), Peak-to-Peak time (D), and Contraction duration (E) in the mutant. (F) Representative sarcomeric organization of wild-type (WT) and TTN-T32756I iPSC-aCM by Transmission electron microscopy (TEM). (G) There is no significant change in the sarcomere length (H). n.s.; P>0.05; *P<0.05; **P< 0.01.
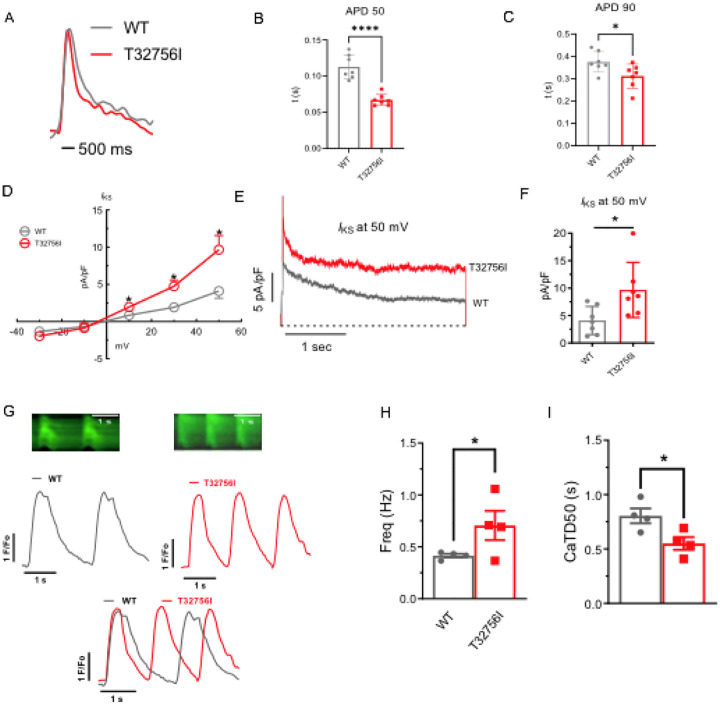
Altered cardiac potassium current and calcium handling underlies the arrhythmia phenotype in TTN-T32756I-iPSC-aCMs:
As studies have shown that abnormal atrial electrophysiology and calcium-handling underlie atrial arrhythmogenesis and contractile dysfunction40,41, we hypothesized that the TTN-T32756I variant modulates atrial APs, ion channels and intracellular calcium. We first tested the AP characteristics of the isolated WT and the TTN-T32756I iPSC-aCMs, which revealed a significant shortening of the AP duration (APD) at 10%, 50%, and 90% repolarization, however, there was no change in the peak amplitude (Figure 3A–C, Supplementary Figure 4A–B). Since increased potassium current (Ik) especially the augmented delayed rectifier potassium current (Iks) causes AF by reducing the APD27,42, we then assessed the Iks by whole-cell voltage clamping. We observed an increase in both Ik and Iks in TTN-T32756I-iPSC-aCMs when compared to the WT (Figure 3D–F, Supplementary Figure 4C–E); thus, confirming that the APD shortening is partly due to the increased Ik. To test the effect of T32756I on atrial calcium handling, we measured the intracellular calcium transients at the excitation-contraction coupling moment of the iPSC-aCMs using fluorescent (fura-2, AM) calcium imaging. Compared to the WT, TTN-T32756I-iPSC-aCMs exhibited increased arrhythmic frequency along with a significant reduction of the time to 50% and 90% decline of calcium transients (Figure 3G–I, Supplementary Figure 4F). However, TTN-T32756I-iPSC-CMs exhibited similar calcium transient amplitudes as the WT, indicating that there was no change in the availability of the intracellular calcium for each contraction (Supplementary Figure 4G). Our findings suggest that the reduced APD due to the increased potassium current and the decreased timing of the calcium transient may create a reentrant substrate for AF.
Figure 3: Effect of T32756I on action potential (AP) and calcium-handling in iPSC-aCMs.
(A-C) Representative optical AP recordings of WT and TTN-T32756I showing reduction of AP duration (APD) at the 50% (APD50) (B) and 90% (APD90) repolarization (C). (D) Current-voltage (I-V) curves of the slow delayed rectifier potassium current (Iks) in WT and TTN_T32756I iPSC-aCMs. control (n=7) (E-F) Comparison of Iks current density at 50 mV (mean ± SEM). N.s.; P>0.05; *P<0.05; **P<0.01; ***P<0.001; ****P<0.0001. (G) Representative tracings of spontaneous calcium transients of WT and TTN-T32756I iPSC-aCMs. (H-I) Calcium kinetics show that the TTN-T32756I iPSC-aCMs have increased frequency (B) and decreased transient durations (I) compared with the WT iPSC-aCMs.
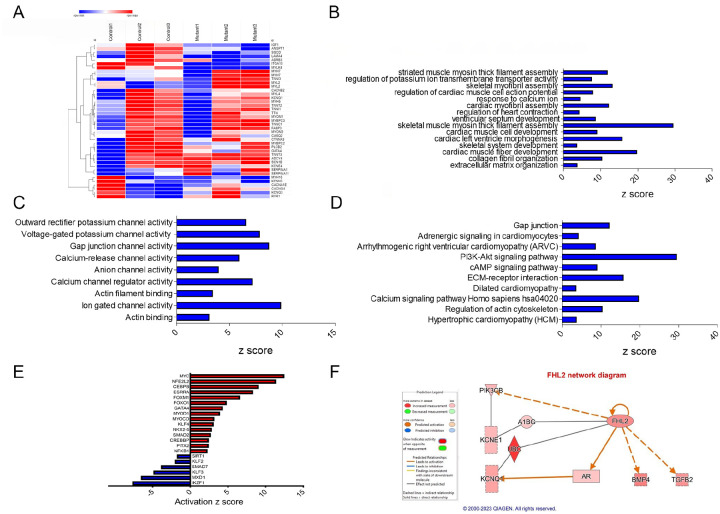
RNA sequencing analysis reveals alterations in cardiac signaling and disease pathways in TTN-T32756I-iPSC-aCMs:
To elucidate the underlying molecular mechanism by which TTN-T32756I causes contractile defects and ion channel remodeling, we performed transcriptome sequencing of the mutant iPSC-aCMs and WT. Comparison of total RNA levels in TTN-T32756-iPSC-aCMs with WT-iPSC-aCMs and differential expression analysis showed genes related to cardiac muscle contraction and calcium handling were predominantly affected (Figure 4A, Supplementary Figure 5A). Gene-ontology (GO) pathway enrichment further showed that the top significantly downregulated cardiac-related GO Biological Processes (-BP) in TTN-T32756I iPSC-aCMs included key processes such as cardiac myofibril assembly, skeletal muscle myosin thick filament assembly, extracellular matrix organization, and regulation of potassium ion transmembrane transporter assembly among others (Figure 4B). As for GO-Molecular function pathways (GO-MF), outward potassium channel activity, voltage-gated potassium channel activity, calcium channel activity, and gap junction channel activity were enriched (Figure 4C). Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis identified downregulation in critical pathways including Adrenergic signaling in cardiomyocytes, the Phosphoinositide 3-kinase (PI3K) signaling pathway, Dilated cardiomyopathy pathway, Hypertrophic cardiomyopathy pathway and Calcium signaling pathway (Figure 4D), which are crucial for normal cardiac electrophysiology and contractility. Upregulated pathways in both GO and KEGG analyses were mostly restricted to neuronal pathways including axon and neuron development, Hippo signaling pathway, and Notch signaling pathway. In the transcriptomic analysis of TTN-T32756I-iPSC-aCMs, several transcription factors (TFs) showed significant alterations, highlighting their potential roles in the mutation’s impact (Figure 4E, Supplementary Figure 5D). Top-cardiac related upregulated TFs include MYC, linked to cell growth and apoptosis, suggesting an increase in cellular proliferation. Stress-related TFs such as NFE2L2 and CEBPB are also elevated, indicating a heightened stress response. Additionally, TFs like ESRRA and FOXM1, which regulate metabolic processes and cell cycle respectively, along with FOXO1 for metabolism and stress resistance, were upregulated. Key TFs in muscle function such as MYOD1, MYOCD, KLF5, and NKX2.5 were enhanced, alongside SMAD2, CREBBP, PITX2, NFKB1, and GATA4, which are vital for diverse roles ranging from signal transduction to immune regulation (Figure 4E). Conversely, downregulated transcription factors include SIRT1, which plays a role in cellular stress resistance and mitochondrial function, pointing to potential vulnerabilities in cellular defenses. Cardiovascular-related TFs such as KLF2 and KLF3, along with SMAD7, involved in TGF-beta signaling, were reduced, possibly impacting structural and signaling integrity. Additionally, MXD1 and IKZF1, crucial for cellular differentiation and immune development, were also diminished (Figure 4E). These transcriptional changes underscore a complex network of regulatory adjustments that could contribute to the altered electrophysiological and structural properties in TTN-T32756I-iPSC-aCMs.
Figure 4: Transcriptomic profile and pathway enrichment analysis comparing TTN-T32756I iPSC-aCMs with the WT.
(A) Heatmaps of cardiac-related upregulated and downregulated differentially expressed genes (DEGs) (B) Top significantly enriched downregulated cardiac-related Gene-Ontology Biological process (GO-BP) pathways in the TTN-T32756I iPSC-aCMs. (C) Top significantly enriched downregulated cardiac-related Gene-Ontology Molecular Function (GO-MF) pathways in the TTN-T32756I iPSC-aCMs. (D) Top significantly enriched downregulated cardiac-related Kyoto Encyclopedia of Genes and Genomes (KEGG) pathways in the TTN-T32756I iPSC-aCMs.(E) Significantly enriched upregulated and downregulated transcription factors (TFs) (F) Network diagram showing the upregulation of KCNQ1 by FHL2 predicted by the Ingenuity pathway enrichment analysis (IPA).
Utilizing the KEGG and GO pathways, we performed Ingenuity Pathway Analysis (IPA) to identify novel titin-interacting proteins that could cause the increased Iks activity in the TTN-T32756I-iPSC-aCMs. The IPA suggests FHL2, which is known to transduce mechanical signaling through its interactions with titin and is enriched in the mutant iPSC-aCMs (Figure 4F). As FHL2 has also been shown to directly interact with the Iks-binding partner mink (KCNE1) and increases its current density43, we postulate that elevated FHL2 level in TTN-T32756I-iPSC-aCMs may cause enhanced binding to Iks, and thus increase its activity.
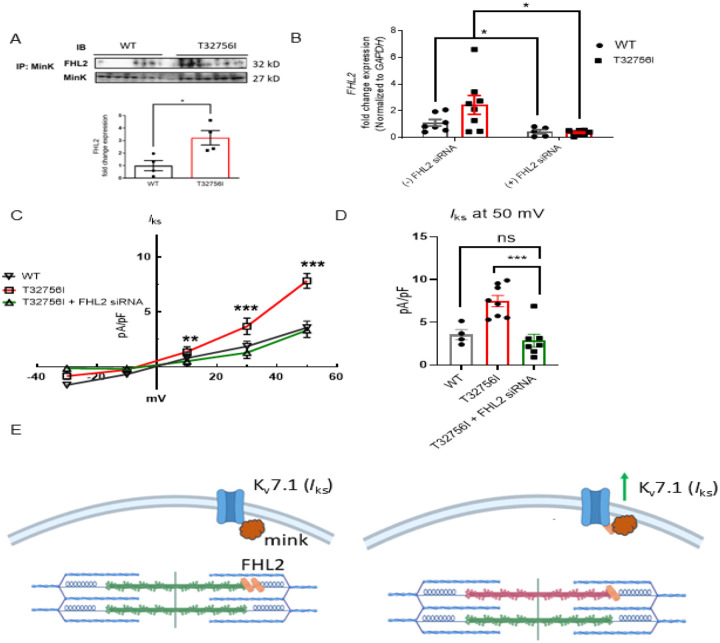
The enhanced Iks current in TTN-T32756I-iPSC-aCMs is mediated by the FHL2:
To determine if TTN-T32756I increases Iks by modulating the interaction between KCNQ1-KCNE1 and FHL2, we performed co-immunoprecipitation studies in both WT and TTN-T32756I-iPSC-aCMs. The co-localization between KCNE1 and FHL2 increased ~3 fold in TTN-T32756I-iPSC-aCMs, suggesting an increased interaction between them (Figure 5A). Since FHL2 enhances Iks activity, we then investigated whether inhibition of the FHL2 could reverse the increased Iks that was observed in the TTN-T32756I-iPSC-aCMs. To inhibit FHL2, we employed the small interfering (si) RNA to suppress the FHL2 gene and measured the Iks activity in both WT and TTN-T32756I-iPSC-aCMs. Both the WT and mutant iPSC-aCMs transfected with FHL2 specific siRNA showed a substantial decrease in FHL2 expression (Figure 5B). As shown in Figure 5C–D, voltage-clamp recordings demonstrate that the Iks in FHL2-suppressed TTN-T32756I-iPSC-aCMs is significantly reduced compared to corresponding the Iks in TTN-T32756I-iPSC-aCMs but comparable to the WT (Figure 5D). Therefore, inhibition of FHL2 by the siRNA rescues the increased Iks of the TTN-T32756I-iPSC-aCMs, which is similar to that of WT Iks. Overall, our data suggest that the TTNmv creates an EP substrate for AF by modulating the IKs activity in part by an increased interaction between the KCNQ1-KCNE1 complex and FHL2 (Figure 5E).
Figure 5:
Inhibition of FHL2 rescues enhanced Iks in TTN-T32756I iPSC-aCMs. (A) Co-immunoprecipitation revealed increased interaction between FHL2 and KCNQ1-KCNE1 (MinK) complex. (IP: KCNE1). Immunoblotting (IB) was performed with antibodies against FHL2 (32 kDa) and MinK (32 kDa) (n = 3) (B) qPCR data showing the inhibition of FHL2 gene by the siRNA in the WT and TTN-T32756I iPSC-aCMs (n=7). (C) I-V curves showing the rescue of the Iks TTN-T32756I iPSC-aCMs by the suppression of FHL2 (n=4–8). (D) Comparison of Iks current density at 50 mV (mean ± SEM). I Schematic showing the TTN-T32756I results in increased FHL2 binding with the KNCQ1-KCNE1 complex and enhanced Iks activity. *P<0.05, **P<0.01, ***P<0.001.
DISCUSSION
We identified an association between TTNmvs and clinical outcomes among a multiethnic cohort of AF patients and elucidated a causal mechanism by which a TTNmv may lead to AF. Although TTNtvs are a well-recognized cause of DCM and have been associated with early-onset AF11,44, the role of TTNmvs in either arrhythmia or cardiomyopathy pathogenesis is unknown. Here, for the first time, we show that TTNmvs are associated with increased hospitalization risk in a multiethnic AF cohort, and that a TTNmv can cause AF by impairing contractility and ion channel remodeling in atrial cardiomyocytes. Furthermore, we demonstrate that augmented Iks mediated by FHL2 can create a substrate for AF. Together, these findings establish a potential causal role of TTNmvs in AF and support Iks and FHL2 as potential therapeutic targets for TTN-related AF.
The genetic architecture of AF is complex, with both monogenic and polygenic contributions that intersect with age and comorbidities to define an individual’s risk. Despite AF being traditionally considered an ion channelopathy, the sarcomeric gene, TTN, is the most common in which rare loss-of-function variants have been associated with AF11,45, and penetrance of such variants was found to be even greater for AF than for heart failure in the UK Biobank46. As rare TTN variants comprise the strongest monogenic contribution to AF risk, we sought to explore whether TTNmvs may similarly have implications in AF development or outcomes. A study of 147 probands with DCM identified 44 severe TTNmvs in 37 probands, which clustered in the A-band region1. There were no differences in heart transplant-free survival between carriers and noncarriers. In a more recent study of 530 subjects with DCM using more stringent allele frequency criteria, 31 predicted deleterious variants were identified, also predominantly located in the A-band19. However, these TTNmvs were found with similar frequency to reference populations. Finally, a study of two families with DCM demonstrated segregation of TTNmvs affecting the same highly conserved cysteine residue in the I-band, which showed impaired contraction and folding at physiological temperatures in a homozygous iPSC model, demonstrating that a TTNmv can cause DCM23.
We identified TTNmvs in 58% of subjects in our cohort, and 33% carried a potentially deleterious variant by REVEL in silico prediction. This frequency was higher than the 37/147 (25.2%) of TTNmv carriers in a DCM cohort17, understanding that differing methods of bioinformatic filtering may limit ability for direct comparison. Aligning with prior studies, most deleterious variants in our study were found in the A-band47,48, where TTNtvs have been linked most strongly to disease. Presence of predicted deleterious TTNmvs was associated with higher LV end diastolic diameter but without statistically significant differences in LVEF, potentially suggesting overlap between a subclinical left ventricular cardiomyopathy and AF in these subjects. We additionally noted higher ventricular rate and QTc interval on index ECGs in these subjects. Rare deleterious variants in TTN have previously been associated with changes in the QT interval49, but the mechanism for this remains unclear. Finally, evidence on the relationship between TTNmvs and clinical outcomes is sparse and limited to examining event-free survival in DCM patients. We observed a significant association between TTNmv presence and increased cumulative incidence of AF or HF-related hospitalizations, which remained unchanged in multivariable adjustment and in sensitivity analyses. This importantly suggests that TTNmvs may correlate with disease severity. Further study exploring these associations in larger validation cohorts and examining AF-specific measures such as arrhythmia burden or treatment response will be necessary to fully understand the clinical importance of TTNmvs in AF.
Prediction of missense variant impact using in silico tools and algorithms can be limited by low specificity, contributing to challenges in clinical interpretation50. Functional studies are often helpful in these cases to confirm or support variant pathogenicity. As existing in vitro or in vivo models do not adequately replicate the complexity of AF, human iPSC-aCMs possess the complex array of cardiac ion channels that make up the atrial AP and provide an adequate model to establish causal relationships in AF26. We identified the missense variant TTN-T32756I in three unrelated subjects in our multiethnic AF registry and studied this variant in an iPSC-aCM model. Remarkably, the single amino acid change in this giant protein titin results in aberrant contractility and EP remodeling without affecting the sarcomeric integrity. Although we did not observe any defects in the sarcomere, in a separate study we showed that deletion of nine amino acids including the T32756I in the same area caused significant perturbation in the sarcomere assembly37. T32756 corresponds to a conserved Threonine of the Ig139 domain (UniProt# Q8WZ42, predicted Ig155 by TITINdb2) and the replacement of a conserved hydrophilic residue (Thr) in WT with a hydrophobic residue (Ile) may cause thermal instability and destabilize the domain. It is now well recognized that point mutations may drastically disrupt the Ig domains and could possibly unfold under pathological conditions51. Such mutations have been proposed to modify titin-based passive stiffness and may lead to cardiomyopathy.
Missense mutations such as T2850I, R57C, S22P in the I-band titin have been reported to significantly destabilize Ig domains and display a higher tendency for unfolding52,53. Likewise, T32756I may unfold under the physiological settings and increase susceptibility to protein loss (haploinsufficiency) or degradation (poison peptide effect), leading to impaired sarcomere function. Furthermore, as titin acts as a crucial signaling hub that transduces mechanical forces to downstream signaling pathways within cardiomyocytes and interacts with various sarcomeric proteins and signaling molecules14,54, subtle destabilization of Ig139 domain by the T32756I could alter the biochemical signals that regulate various downstream signaling pathways involved in cardiac function and adaptation. Hence, the contractile and ion channel dysfunction caused solely by the homozygosity of T32756I in the iPSC-aCMs provide strong evidence that the AF is exclusively caused by the TTN-T32756I missense variant.
Although several studies have identified possible pathways associated with TTNtvs and AF, the pathogenic mechanisms of TTNmv-associated AF remain unclear. We show for the first time that the T32756I creates an EP substrate for AF by ion channel remodeling with an enhanced IKs, which is mediated by a titin interacting protein FHL2. FHL2 is enriched in cardiac muscle and is a multifunctional protein that regulates cardiac myocyte signaling and function55. FHL2 interacts with KCNE1 that binds to the outer face of the KCNQ1 channel pore domain and may modify the interactions between the voltage sensor, S4-S5 linker, and the pore domain to augment the channel current43. It has been suggested that FHL2 interacts with titin N2B segment, titin kinase domain and forms a complex with other proteins, such as MURF1 and MURF2, calmodulin, and Nbr1, playing a role in hypertrophy signaling and the atrophy response56,57. It also binds to the edge of titin (M-line), which is in close proximity to T32756I, and interacts with myospryn and obscurin58. It is tempting to postulate that T32756I may interfere with FHL2’s ability to interact with titin, which could then disrupt with subsequent mechano-biochemical signaling and increase FHL2’s availability for binding with the KCNQ1-KCNE1 complex. While our study provides mechanistic insights into the role of the TTN-32756I missense variant in AF, TTNmvs may be involved in the regulation of ion channel modulation and atrial rhythmicity through a multitude of interrelated signaling pathways. Further studies are needed to fully uncover the molecular basis of this regulation and its implications for AF pathophysiology and potential therapeutic interventions.
In summary, this study supports a causal relationship between a TTNmv and AF and suggests that TTNmvs may be associated with adverse outcomes in patients with AF. The study also unveils the critical role of FHL2 in modulating the atrial action potential via binding to Kv7.1-KCNE1 and enhancing the IKs in TTN-T32756I-iPSC-aCMs. Importantly, we found that the increased IKs can be rescued by FHL2 suppression. This suggests that targeting IKs or FHL2 may restore and maintain sinus rhythm and improve atrial contractility. Further study is needed to determine if TTNmvs in other regions are associated with AF by a similar mechanism. Our data indicate that AF-associated TTNmv can cause arrhythmia, provide new insight into the mechanisms underlying AF and suggest that targeting KCNQ1 or FHL2 could represent a new therapeutic strategy for improving cardiac function. Our findings may also have broader implications for the treatment of patients harboring disease-causing rare variants in sarcomeric proteins and suggest that genomic analyses that encompass TTNmvs should also consider experimental evidence in advancing our understanding of AF etiology and improving patient care in the era of precision medicine.
METHODS
Study population
The UIC Multi-Ethnic AF Biorepository was established in 2015 to explore the genetic basis of AF across race and ethnicity. This study was approved by the UIC Institutional Review Board (#2015–0681). Subjects are prospectively enrolled from outpatient and inpatient sites within the University of Illinois Health (UIH) healthcare system. Subjects must have a documented history of AF by electrocardiogram, Holter/event monitor, or implantable cardiac device, with confirmation by an attending cardiologist. At time of enrollment, blood is drawn for DNA extraction and genetic analysis. Baseline demographics are obtained through provider notes in the electronic health record (EHR) and confirmed with the patient at the time of enrollment as necessary. Longitudinal clinical outcomes are followed through serial EHR review. Written informed consent was obtained from all participants. Adults 18 years of age or older at time of AF diagnosis were prospectively enrolled between August 25, 2015, and May 19, 2019. Samples from 161 subjects who identified as non-Hispanic Black (NHB) or Hispanic/Latinx (HL) and had an echocardiogram performed within 3 months of enrollment date underwent whole exome sequencing. A total of 27 subjects with congenital or rheumatic disease, severe mitral stenosis, and end stage renal disease on dialysis were excluded. Three subjects who carried a predicted loss-of-function frameshift or stop-gain TTN variant were additionally excluded. The primary exposure was the presence of one or more missense TTN variants. The primary outcome was time from initial AF diagnosis to hospitalizations with a primary diagnosis of either AF or acute decompensated HF recorded in the clinical discharge summary, captured as repeating events. Clinical data was obtained through manual review of EHR and comorbidities were defined if present in clinical notes on or prior to AF diagnosis date. Subjects were censored on date of death, last known clinical encounter (up to August 26, 2023), or at 10 years after AF diagnosis. Echocardiographic criteria for left ventricular dilatation was defined as left ventricular end diastolic diameter (LVEDD) > 2 standard deviations (SD) above sex-specific mean according to standard guidelines59. Subjects meeting echocardiographic criteria for left ventricular dilatation fulfilled clinical criteria for nonischemic dilated cardiomyopathy if left ventricular ejection fraction (LVEF) < 50% and ischemic cardiomyopathy was ruled out by coronary angiogram.
Whole exome sequencing
Samples were sequenced with support of the National Human Genome Research Institute (NHGRI) Centers for Common Disease Genetics (CCDG) program. Sequencing was performed at the Broad Institute following methods established by the National Heart, Lung, and Blood Institute (NHLBI) Trans-Omics for Precision Medicine (TOPMed) Atrial Fibrillation Study (available under TOPMed Whole Genome Sequencing Methods: Freeze 9 at https://www.ncbi.nlm.nih.gov/projects/gap/cgi-bin/study.cgi?study_id=phs001062.v5.p2). Samples underwent WES using an Illumina HiSeq X system with 150bp paired-end read length, at 20x depth for at least 85% of targets Alignment to human genome reference GRCh38/hg38 was performed using BWA-MEM (Burrows-Wheeler Aligner, v0.7.15.r1140). TTN variant calls were filtered to select those with read depth of ≥20X, genotype quality ≥20, minor allele frequency (MAF) ≤1% across gnomAD subpopulations, and excluding intronic, regulatory or UTR 3’/5’ variants. Synonymous variants, homozygous reference calls, non-canonical variants, and any variants with percent spliced in (PSI) index <90 were excluded. Missense variants predicted to be deleterious were identified using REVEL score of ≥0.7, a previously proposed cutoff to predict deleterious effect in dilated cardiomyopathy60,61. Because of the uncertain role of missense TTN variants across AF and other cardiac diseases, we examined all TTN missense variants regardless of REVEL score. Variant annotation data were obtained from Ensembl Variant Effect Predictor62, downloaded January 11, 2024, and CardioDB (https://cardiodb.org/titin) for TTN region and percent spliced in (PSI)63, downloaded November 16, 2023.
Human iPSC culture and human iPSC-aCM differentiation
Human iPSC-CMs were derived from reprogrammed peripheral blood mononuclear cells (PBMCs) as previously described29. 80–90% confluent iPSC-CMs was differentiated using the Cardiomyocyte Differentiation Kit (Gibco) and guided toward the atrial subtype using all-trans RA64. The cellular population was purified through glucose starvation and lactate replacement, resulting in contracting monolayers of iPSC-aCMs. Our protocol typically yields ~80 to 90% pure iPSC-aCMs and <6% fibroblasts based on immunostaining analysis as we have previously described29,64. Human iPSC-aCMs were then matured following dissociation and replating on fibronectin-coated plates and maintained in Cardiomyocyte Maintenance Media supplemented with T3, insulin-like growth factor-1, and dexamethasone as previously described27.
Generation of TTN-T32756I hiPSCs using CRISPR-Cas9
We edited the genome of WT iPSCs to introduce the T32756I using CRISPR-Cas9 technique29. The TTN-T32756I CRISPR-Cas9 was designed from WT allele sgRNA and two ssODN that target the TTN genomic locus: 31111–31119 and genomic DNA location: chr2:178539785–178539811 (GRCh38.p13). Amplification in the exon 352 cDNA donor RNP was constructed and electroporated into the TTN gene WT hiPSCs. Gene-editing efficiency was confirmed with next-generation sequencing (NGS). Karyotype analysis was carried out by the Cytogenetics laboratory at WiCell Research Institute Inc. Cells were collected and chromosome were evaluated using the giemsa trypsin wright (GTW) banding method. Metaphase cells were analyzed, all of which were concluded to have a normal karyotype (46, XY)
Contraction analysis and optical voltage mapping
Contractility of hiPSC-aCMs was performed with a versatile open-source software, MUSCLEMOTION65. MUSCLEMOTION is ab ImageJ plugin that utilizes a video-based system to assess contractile functions. Optical voltage mapping recordings were performed on the IonOptix system myopacer system using the fluovolt membrane potential kit (Thermo Fisher). HiPSC-aCMs were cultured in confocal dishes were incubated with Tyrode’s solution (140 mM NaCl, 4.56 mM KCl, 0.73 mM MgCl2, 10 mM HEPES, 5.0 mM dextrose, 1.25 mM CaCl2) plus 1x Fluovolt (Sigma/Aldrich) for 15–20 minutes. Cells were then rinsed with normal Tyrode’s solution and recorded APDs on the IonOptix system. These experiments were performed at the room temperature (25°C).
Electrophysiology
Whole-cell patch clamping on hiPSC-aCMs IK recordings was performed according to previously published protocols27,29. Briefly, voltage-clamps were achieved by using an Axopatch 200B amplifier controlled by pClamp10 software through an Axon Digidata 1440A. External solution for IK recordings contained: 140 mM NaCl, 4 mM KCl, 1.8 mM CaCl2, 1.2 mM MgCl2, 10 mM glucose, 10 mM HEPES, and 0.01 mM nifedipine, adjusted to pH 7.4 with NaOH. IKs recordings were isolated as 1 μM HMR-1556–sensitive current. The intracellular solution contained 100 mM potassium aspartate, 2 mM MgCl2, 20 mM KCl, 5 mM Mg-ATP, 5 mM EGTA, and 10 mM HEPES adjusted to 7.2 with KOH. IKs currents were elicited by using 3-second voltage-clamp steps to test potentials of −60 to +60 mV from holding potential of –40 mV and with 20 mV increments.
Calcium Handling
Calcium transients were measured using Fluo-4-AM (Invitrogen) dye dissolved in 2.5% Pluronic F-127 (MilliporeSigma). To get a working concentration of 5 μM, the dye solution was added to Tyrode’s solution (1 mM Ca2+). The cells were treated with Fluo-4-AM in 1 mM Ca2+ Tyrode’s solution, and then allowed to sit at room temperature for 20 minutes in the dark. Tyrode’s solution without indicators and containing 2 mM calcium was used to wash the cells. Using a 40× objective and the Zeiss LSM 710 confocal equipped with a BiG module, line scans were acquired and examined using ImageJ. The corrected minimum and maximum fluorescence values were determined by normalizing the fluorescence using a baseline background region that was unique to each cell. Fluorescence signals were normalized to basal cell fluorescence after fluo-4 loading (F0). Estimations of intracellular Ca2+ are reported as changes in ΔF/F0, where ΔF = F-F0.
Transmission electron microscopy (TEM)
iPSC-aCMs were fixed with 2.5% glutaraldehyde in 0.1M Sorenson’s Buffer for 60 minutes at room temperature. The cells are then carefully collected into a microcentrifuge tube pre-filled with same the fixation buffer. The samples were then centrifuged at 2500xg for 10 min at room temperature. The pellet was then removed and inverted with a hypodermic needle to ensure fixative solution thoroughly permeates the sample. The pellet is then allowed to incubate at room temperature to fix for an additional 60 minutes at room temperature. The fixation solution was then removed and substituted with 1% glutaraldehyde + 4% paraformaldehyde in 0.1M Sorenson’s buffer and stored in 4°C. Fixed samples were embedded in resin and microtome sections were imaged on a JEOL JEM-1400 Flash TEM.
Immunofluorescence
Cells were cultured on Matek(R) glass bottom dishes that were coated with vitronectin. The cells were then allowed to grow for a period of 2 days. The cells were then fixed with 4% paraformaldehyde (PFA) for 10 minutes and permeabilized with phosphate-buffered saline (PBS) containing 0.1% Triton X-100 for 10 minutes. After that, the cells were blocked with 3% bovine serum albumin (BSA) in PBS for 1 hour at room temperature. The staining procedure was carried out overnight at 4°C using primary antibodies that were diluted in 3% BSA in PBS. The cells were rinsed three times with PBS and then exposed to secondary antibodies (anti-mouse-FITC or anti-rabbit-PE, Santacruz, 1:1000) for one hour at room temperature. Subsequently, the cells were rinsed 3x with PBS and co-stained with 1μg/ml of DAPI. The antibodies Anti-SOX2 (Abcam, 1:200) and anti-OCT4 (Santacruz, 1:200) were used to assess the generation of iPSCs, while anti-cTnT (Invitrogen, 1:300) and anti-Kv1.5 (Alomone labs, 1:200) were utilized to confirm the differentiation of atrial cardiomyocytes. The samples were visualized using an LSM710 Meta Confocal Microscope manufactured by Zeiss.
Protein isolation, western blotting, and co-immunoprecipitation
We performed Western blots as previously described27,29. For western blots, cells on 6-well plates were washed with ice cold DPBS without Ca2+ and Mg2+, after which 250 μL of 1X RIPA with protease and phosphatase inhibitors was added per well. Lysate concentrations were measured using BCA Assay, and diluted with 4X Laemmli buffer with 10% 2-Mercaptoethanol. Per sample, 25 μg of protein was then run on an SDS-polyacrylamide gel to separate, and resolved gels were electro-transferred on 0.2 μm PVDF membranes. Membranes were blocked with 5% BSA for 1 hour, and then probed with corresponding antibodies of target proteins (anit-FHL2 antibody, Abcam#ab202584). The blots were developed using either anti-rabbit HRP or anti-mouse HRP and scanned on C280 imaging systems (Azure Biosystems). Protein signal densities were determined using ImageJ and normalized to corresponding β-actin signal densities.
For co-immunoprecipitation experiments, cells are rinsed with ice cold DPBS without Ca2+ and Mg2+, after which 500 μL of 1X RIPA with protease and phosphatase inhibitors was added each well of a 6-well plate. Lysates are sonicated on ice 3×5 seconds, then centrifuged for 10 min at 14,000xg at 4°C. 100μL of Protein A/G agarose bead slurry was added to the lysate and incubated at 4°C on a rotator for 60 minutes. The cell lysate with bead slurry was centrifuged for 10 minutes at 1000xg at 4°C and the supernatant was transferred to a fresh Eppendorf tube. 2μg of primary antibody (KCNE1 [Alomone# APC-168]: 2.5μL) was added to 500μg of precleared cell lysate, and the mixture was incubated with gentle rotation overnight at 4°C for a day. 40μL of Protein A/G bead slurry was the washed 3x with RIPA, and the precleared cell lysate with the primary antibody was added to the bead slurry, and then followed by incubation for 3 hours at 4°C. The mixture is centrifuged for 10 min at 1000xg at 4°C, and the flow through was saved to verify the immunoprecipitation. The bead pellet was rinsed with 5×500 μL RIPA and resuspended in 30μL 4X Laemmli sample buffer, vortexed, then centrifuged for 30 seconds. The sample was then boiled for 5 min, then centrifuged at 14,000xg for 5 min, representing the IP sample. 15 μL of supernatant and immunoprecipitate samples were loaded onto a 10% SDS-PAGE gel and analyzed by western blotting.
RNA-Sequencing
The RNA was isolated using the Maxwell® RSC simplyRNA Cells Kit (Promega AS1390) according to the instructions provided by the manufacturer. Library preparation was carried out using the Universal Plus mRNA-Seq kit (NuGen 0520-A01). Briefly, RNA underwent poly-A selection, enzymatic fragmentation, and generation of double-stranded cDNA using a mixture of Oligo (dT) and random priming. The cDNA was subjected to end repair, ligation of dual-index adaptors, strand selection, and 15 cycles of PCR amplification. The concentrations of the purified library were determined using the Qubit 1X dsDNA HS Assay Kit (Invitrogen Q33231). The libraries were then combined in equal amounts, considering the Qubit concentration and the average size determined by TapeStation. The pooled libraries were subsequently run on the MiniSeq instrument for index balancing. The ultimate, refined pool was measured using quantitative polymerase chain reaction (qPCR). The raw reads were aligned to the reference genome hg38 using the STAR alignment tool. The quantification of ENSEMBL gene expression was performed using FeatureCounts. The edgeR package was used to calculate normalized and differential expression statistics. To account for multiple testing, p-values were adjusted using the false discovery rate (FDR) correction method. We detected differentially expressed genes (DEGs) with a q value of less than 0.05 and a log 2 fold change of at least 2 between the Control and AF iPSC-aCMs. We conducted unsupervised hierarchical clustering of all genes that showed differential expression using the Euclidean distance and complete linkage method. Additionally, we created volcano plots using the R programming language. The up- and down-regulated genes were analyzed individually using the DAVID functional annotation tool against the Gene Ontology Biological Process (GO BP) database.
qPCR
Total RNA was isolated from hiPSC-aCMs using TRIzol reagent (Invitrogen), following the manufacturer’s instructions to ensure the extraction of high-quality RNA. The concentration and purity of the isolated RNA were carefully assessed using a NanoDrop 2000 spectrophotometer (Thermo Fisher Scientific), with 1 μg of total RNA utilized for each reverse transcription reaction. Reverse transcription to synthesize cDNA was conducted using SuperScript III Reverse Transcriptase (Thermo Fisher Scientific). For the analysis, specific assays and primers were selected for target gene FHL2 (Forward sequence: GTGGTGTGCTTTGAGACCCTGT, Reverse sequence: GAGCAGTGGAAACAGGCTTCATG) with glyceraldehyde 3-phosphate dehydrogenase (GAPDH) serving as the normalization reference gene. qPCR reactions were performed on an ABI QuantStudio 5 system (Applied Biosystems), using SYBR Green PCR Master Mix to accurately detect and quantify PCR amplification products. Relative expression levels of the target genes were calculated employing the ΔΔCt method, by the quantification of gene expression changes in the experimental samples relative to control. For the ΔCT Calculation, the cycling time (CT) value of the target gene was subtracted from the CT value of GAPDH in the same sample using ΔCT=CTtarget gene − CTreference gene . The ΔΔCT value was then calculated using ΔΔCT= ΔCTExperimental – ΔCTControl. The relative expression for the gene was in turn calculated using Relative gene expression= 2−ΔΔCT.
siRNA experiments
FHL2-specific siRNAs (#SR301594) or scrambled siRNAs were applied to mature hiPSC-aCMs using Lipofectamine RNAiMAX (Invitrogen, Carlsbad, CA). Opti-MEM medium was used to dilute stock solutions of lipofectamine and siRNA, each prepared at a concentration of 10 μM. The siRNA-lipid complex was then made by mixing these solutions in a 1:1 ratio and incubated for five minutes. After adding this complex to the cells dropwise, the media was changed, and the cells were allowed to incubate for a further two days.
Data Analysis and Statistics
For clinical data, categorical variables are represented as count and percentage (%) and tested by Fisher’s exact test. Continuous variables are reported as mean (standard deviation [SD]) or median and interquartile range (IQR) where specified and tested with Mann-Whitney U and Kruskal-Wallis tests. Ordinal variables were tested with Kruskal-Wallis test. Univariable and multivariable Cox proportional hazards models were used to evaluate risk of the primary outcome as recurring events, related to presence of TTN missense variants. A partially adjusted model was first tested using covariates of age and sex, followed by a fully adjusted model which additionally incorporated covariates of ethnicity and baseline LVEF <50%. Interaction between TTN missense variants and LVEF was additionally evaluated. To identify whether associations were limited to variants with predicted deleterious effect, analysis was repeated stratifying subjects according to presence and predicted impact of TTNmv: presence of one or more predicted deleterious (REVEL≥0.7) variants, presence of predicted benign (REVEL <0.7) variants only, or no TTNmv present. Additional sensitivity analyses were performed excluding subjects with multiple TTNmvs and with nonischemic dilated cardiomyopathy. Analysis was performed in R (version 4.2.1, packages: arsenal, ggplot2, ggsurvfit, gtsummary, reda, survival).
Experiments were performed at least two times (biological replicates) to ensure reproducibility. Unless otherwise noted, experimental data on hiPSCs are shown as mean ± SD. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001 indicate significance, while P > 0.05 is regarded as non-significant. Statistical analyses include unpaired nonparametric and 2-tailed Mann-Whitney U test for data with normal distribution, and either 1-way or 2-way ANOVA with post hoc Bonferroni’s corrections for several groups. The first and third quartiles of a median are used to express skewed data. Fisher’s Exact test is used to compare categorical data, and unpaired Student’s t-test or ANOVA are applied to assess continuous variables.
Supplementary Material
ACKNOWLEDGEMENT
This work was in part supported by NIH grants R01 HL150586 (DD), R01 HL148444 (DD), NIH T32 HL139439 and AHA 23POST1019044 (MH), UL1 TR002003 (The University of Illinois Chicago Center for Clinical and Translational Science (CCTS)), and UIC seed funding (MAP).
Footnotes
CODE AVAILABILITY
R version 4.2.1 and packages (arsenal, ggplot2, ggsurvfit, gtsummary, reda, survival, tidycmprsk) are available at https://cran.r-project.org/. Variants are annotated with Ensembl Variant Effect Predictor (https://www.ensembl.org/info/docs/tools/vep/index.html) and CardioDB (https://cardiodb.org/titin) for TTN region and percent spliced in (PSI).
COMPETING INTERESTS
The authors declare no competing interests.
DATA AVAILABILITY
Whole genome sequencing data of the patients are subject to conditions of the IRB protocols and UIC policies under which the data was generated, and therefore the raw sequencing data is unavailable. The ClinVar accession number for the variant studied is VCV000178164.47. Data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1.Brundel B. J. J. M. et al. Atrial fibrillation. Nature Reviews Disease Primers 2022 8:1 8, 1–23 (2022). [DOI] [PubMed] [Google Scholar]
- 2.Elliott A. D., Middeldorp M. E., Van Gelder I. C., Albert C. M. & Sanders P. Epidemiology and modifiable risk factors for atrial fibrillation. Nature Reviews Cardiology 2023 20:6 20, 404–417 (2023). [DOI] [PubMed] [Google Scholar]
- 3.Schotten U., Verheule S., Kirchhof P. & Goette A. Pathophysiological mechanisms of atrial fibrillation: A translational appraisal. Physiol Rev 91, 265–325 (2011). [DOI] [PubMed] [Google Scholar]
- 4.Markides V. & Schilling R. J. Atrial fibrillation: classification, pathophysiology, mechanisms and drug treatment. Heart 89, 939 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee D. S. M., Damrauer S. M. & Levin M. G. Genetics of atrial fibrillation. Curr Opin Cardiol 38, 162–168 (2023). [DOI] [PubMed] [Google Scholar]
- 6.Feghaly J., Zakka P., London B., MacRae C. A. & Refaat M. M. Genetics of Atrial Fibrillation. J Am Heart Assoc 7, (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sagris M. et al. Atrial Fibrillation: Pathogenesis, Predisposing Factors, and Genetics. Int J Mol Sci 23, (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roselli C., Roselli C., Rienstra M., Ellinor P. T. & Ellinor P. T. Genetics of Atrial Fibrillation in 2020: GWAS, Genome Sequencing, Polygenic Risk, and Beyond. Circ Res 127, 21–33 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roselli C. et al. Multi-ethnic genome-wide association study for atrial fibrillation. Nature Genetics 2018 50:9 50, 1225–1233 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Choi S. H. et al. Association between titin loss-of-function variants and early-onset atrial fibrillation. JAMA 320, 2354 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chalazan B. et al. Association of Rare Genetic Variants and Early-Onset Atrial Fibrillation in Ethnic Minority Individuals. JAMA Cardiol (2021) doi: 10.1001/jamacardio.2021.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.S Labeit B. K. Titins: giant proteins in charge of muscle ultrastructure and elasticity. Science (1979) 270, 293–296 (1995). [DOI] [PubMed] [Google Scholar]
- 13.Granzier H. L. & Labeit S. The Giant Protein Titin: A Major Player in Myocardial Mechanics, Signaling, and Disease. Circulation Research vol. 94 284–295 Preprint at 10.1161/01.RES.0000117769.88862.F8 (2004). [DOI] [PubMed] [Google Scholar]
- 14.MM LeWinter Y. W. S. L. H. G. Cardiac titin: structure, functions and role in disease. Clin. Chim. Acta 375, 1–9 (2007). [DOI] [PubMed] [Google Scholar]
- 15.Linke W. A. & Hamdani N. Gigantic business: Titin properties and function through thick and thin. Circulation Research vol. 114 1052–1068 Preprint at 10.1161/CIRCRESAHA.114.301286 (2014). [DOI] [PubMed] [Google Scholar]
- 16.Schafer S. Titin-truncating variants affect heart function in disease cohorts and the general population. Nat. Genet. 49, 46–53 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Begay R. Role of titin missense variants in dilated cardiomyopathy. J. Am. Heart Assoc. 4, (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vissing C. R. et al. Dilated cardiomyopathy caused by truncating titin variants: long-term outcomes, arrhythmias, response to treatment and sex differences. J Med Genet 58, 832–841 (2021). [DOI] [PubMed] [Google Scholar]
- 19.Akinrinade O. et al. Relevance of Titin Missense and Non-Frameshifting Insertions/Deletions Variants in Dilated Cardiomyopathy. Sci Rep 9, (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weston T. G. R., Rees M., Gautel M. & Fraternali F. Walking with giants: The challenges of variant impact assessment in the giant sarcomeric protein titin. WIREs Mechanisms of Disease e1638 (2023) doi: 10.1002/WSBM.1638. [DOI] [PubMed] [Google Scholar]
- 21.Martínez‐barrios E. et al. Discerning the Ambiguous Role of Missense TTN Variants in Inherited Arrhythmogenic Syndromes. J Pers Med 12, (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Richards S. et al. Standards and Guidelines for the Interpretation of Sequence Variants: A Joint Consensus Recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17, 405 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Domínguez F. et al. Titin Missense Variants as a Cause of Familial Dilated Cardiomyopathy. Circulation 147, 1711–1713 (2023). [DOI] [PubMed] [Google Scholar]
- 24.Liu G. et al. Novel missense variant in TTN cosegregating with familial atrioventricular block. Eur J Med Genet 63, (2020). [DOI] [PubMed] [Google Scholar]
- 25.Chen E. et al. Rates and Classification of Variants of Uncertain Significance in Hereditary Disease Genetic Testing. JAMA Netw Open 6, E2339571 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ly O. T., Brown G. E., Han Y. D., Darbar D. & Khetani S. R. Bioengineering approaches to mature induced pluripotent stem cell-derived atrial cardiomyocytes to model atrial fibrillation. Exp Biol Med 246, 1816–1828 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ly O. T. et al. Mutant ANP induces mitochondrial and ion channel remodeling in a human iPSC–derived atrial fibrillation model. JCI Insight 7, (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nicholson M. W. et al. Utility of iPSC-Derived Cells for Disease Modeling, Drug Development, and Cell Therapy. Cells 11, (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hong L. et al. Human induced pluripotent stem cell-derived atrial cardiomyocytes carrying an SCN5A mutation identify nitric oxide signaling as a mediator of atrial fibrillation. Stem Cell Reports 16, 1542–1554 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Poetsch M. S. & Guan K. iPSCs for modeling of sarcomeric cardiomyopathies. Recent Advances in iPSC Disease Modeling, Volume 1 237–273 (2020) doi: 10.1016/B978-0-12-822227-0.00012-0. [DOI] [Google Scholar]
- 31.Li S. et al. Mitochondrial Dysfunctions Contribute to Hypertrophic Cardiomyopathy in Patient iPSC-Derived Cardiomyocytes with MT-RNR2 Mutation. Stem Cell Reports 10, 808–821 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nijak A. et al. iPSC-Cardiomyocyte Models of Brugada Syndrome—Achievements, Challenges and Future Perspectives. International Journal of Molecular Sciences 2021, Vol. 22, Page 2825 22, 2825 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moretti A. et al. Patient-Specific Induced Pluripotent Stem-Cell Models for Long-QT Syndrome. New England Journal of Medicine 363, 1397–1409 (2010). [DOI] [PubMed] [Google Scholar]
- 34.Benzoni P. et al. Human iPSC modelling of a familial form of atrial fibrillation reveals a gain of function of If and ICaL in patient-derived cardiomyocytes. Cardiovasc Res 116, 1147 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Simons E., Loeys B. & Alaerts M. iPSC-Derived Cardiomyocytes in Inherited Cardiac Arrhythmias: Pathomechanistic Discovery and Drug Development. Biomedicines 11, (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brown G. E. et al. Engineered cocultures of iPSC-derived atrial cardiomyocytes and atrial fibroblasts for modeling atrial fibrillation. Sci Adv 10, (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jiang X. et al. Transient titin-dependent ventricular defects during development lead to adult atrial 1 arrhythmia and impaired contractility 2 3 Corresponding Authors 25. Iscience (In press) (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schick R. et al. Functional abnormalities in induced Pluripotent Stem Cell-derived cardiomyocytes generated from titin-mutated patients with dilated cardiomyopathy. PLoS One 13, (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hinson J. T. et al. Titin Mutations in iPS cells Define Sarcomere Insufficiency as a Cause of Dilated Cardiomyopathy. Science 349, 982 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nattel S., Heijman J., Zhou L. & Dobrev D. Molecular Basis of Atrial Fibrillation Pathophysiology and Therapy. Circ Res 51–72 (2020) doi: 10.1161/CIRCRESAHA.120.316363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McCauley M. D. et al. Ion Channel and Structural Remodeling in Obesity-Mediated Atrial Fibrillation. Circ Arrhythm Electrophysiol 13, 8296 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Menon A. et al. Electrophysiologic and molecular mechanisms of a frameshift NPPA mutation linked with familial atrial fibrillation. J Mol Cell Cardiol 132, 24–35 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kupershmidt S. et al. Cardiac-enriched LIM domain protein fhl2 is required to generate IKs in a heterologous system. Cardiovasc Res 56, 93–103 (2002). [DOI] [PubMed] [Google Scholar]
- 44.Goodyer W. R. et al. Broad Genetic Testing in a Clinical Setting Uncovers a High Prevalence of Titin Loss-of-Function Variants in Very Early Onset Atrial Fibrillation. Circ Genom Precis Med 12, 526–528 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yoneda Z. T. et al. Early-Onset Atrial Fibrillation and the Prevalence of Rare Variants in Cardiomyopathy and Arrhythmia Genes. JAMA Cardiol 6, 1371–1379 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Choi S. H. et al. Monogenic and Polygenic Contributions to Atrial Fibrillation Risk: Results from a National Biobank. Circ Res 126, 200 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Roberts A. M. et al. Integrated allelic, transcriptional, and phenomic dissection of the cardiac effects of titin truncations in health and disease. Sci Transl Med 7, (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Akinrinade O., Alastalo T. P. & Koskenvuo J. W. Relevance of truncating titin mutations in dilated cardiomyopathy. Clin Genet 90, 49–54 (2016). [DOI] [PubMed] [Google Scholar]
- 49.Kapoor A. et al. Rare coding TTN variants are associated with electrocardiographic QT interval in the general population. Sci Rep 6, (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Richards S. et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genetics in Medicine 17, 405–424 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li H., Carrion-Vazquez M., Oberhauser A. F., Marszalek P. E. & Fernandez J. M. Point mutations alter the mechanical stability of immunoglobulin modules. Nat Struct Biol 7, 1117–1120 (2000). [DOI] [PubMed] [Google Scholar]
- 52.Zuo J., Zhan D., Xia J. & Li H. Single-Molecule Force Spectroscopy Studies of Missense Titin Mutations That Are Likely Causing Cardiomyopathy. Langmuir 37, 12128–12137 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Anderson B. R., Bogomolovas J., Labeit S. & Granzier H. Single Molecule Force Spectroscopy on Titin Implicates Immunoglobulin Domain Stability as a Cardiac Disease Mechanism. J Biol Chem 288, 5303 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Krüger M. & Linke W. A. The giant protein titin: A regulatory node that integrates myocyte signaling pathways. Journal of Biological Chemistry vol. 286 9905–9912 Preprint at 10.1074/jbc.R110.173260 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tran M. K., Kurakula K., Koenis D. S. & de Vries C. J. M. Protein–protein interactions of the LIM-only protein FHL2 and functional implication of the interactions relevant in cardiovascular disease. Biochimica et Biophysica Acta (BBA) - Molecular Cell Research 1863, 219–228 (2016). [DOI] [PubMed] [Google Scholar]
- 56.Sun Y., Liu X., Huang W., Le S. & Yan J. Structural domain in the Titin N2B-us region binds to FHL2 in a force-activation dependent manner. Nature Communications 2024 15:1 15, 1–14 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Liang Y., Bradford W. H., Zhang J. & Sheikh F. Four and a half LIM domain protein signaling and cardiomyopathy. Biophys Rev 10, 1073 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Henderson C. A., Gomez C. G., Novak S. M., Mi-Mi L. & Gregorio C. C. Overview of the Muscle Cytoskeleton. Compr Physiol 7, 891 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lang R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28, 1–39.e14 (2015). [DOI] [PubMed] [Google Scholar]
- 60.Ioannidis N. M. et al. REVEL: An Ensemble Method for Predicting the Pathogenicity of Rare Missense Variants. Am J Hum Genet 99, 877 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Morales A. et al. Variant Interpretation for Dilated Cardiomyopathy: Refinement of the American College of Medical Genetics and Genomics/ClinGen Guidelines for the DCM Precision Medicine Study. Circ Genom Precis Med 13, E002480 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McLaren W. et al. The Ensembl Variant Effect Predictor. Genome Biol 17, 1–14 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Roberts A. M. et al. Integrated allelic, transcriptional, and phenomic dissection of the cardiac effects of titin truncations in health and disease. Sci Transl Med 7, (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Argenziano M. et al. Electrophysiologic Characterization of Calcium Handling in Human Induced Pluripotent Stem Cell-Derived Atrial Cardiomyocytes. Stem Cell Reports 10, 1867 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sala L. et al. Musclemotion: A versatile open software tool to quantify cardiomyocyte and cardiac muscle contraction in vitro and in vivo. Circ Res 122, e5–e16 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Whole genome sequencing data of the patients are subject to conditions of the IRB protocols and UIC policies under which the data was generated, and therefore the raw sequencing data is unavailable. The ClinVar accession number for the variant studied is VCV000178164.47. Data that support the findings of this study are available from the corresponding author upon reasonable request.