Abstract
Objective:
To develop and evaluate measures of patient work system factors in medication management that may be modifiable for improvement during the care transition from hospital to home among older adults.
Design, settings, and participants:
Measures were developed and evaluated in a multi-site prospective observational study of older adults (≥65 years) discharged home from medical units of two U.S. hospitals from August 2018 to July 2019.
Main Measures:
Patient work system factors for managing medications were assessed during hospital stays using 6 capacity indicators, 4 task indicators, and 3 medication management practice indicators. Main outcomes were assessed at participants’ homes approximately a week after discharge for (a) medication discrepancies between the medications taken at home and those listed in the medical record, and (b) patient experiences with new medication regimens.
Results:
274 of the 376 recruited participants completed home assessment (72.8%). Among capacity indicators, most older adults (80.6%) managed medications during transition without a caregiver, 41.2% expressed low self-efficacy in managing medications and 18.3% were not able to complete basic medication administration tasks. Among task indicators, more than half (57.7%) had more than 10 discharge medications and most (94.7%) had medication regimen changes. Having more than 10 discharge medications, more than two medication regimen changes, and low self-efficacy in medication management increased the risk of feeling overwhelmed (odds ratio [95% CI]: 2.63[1.08-6.38], 3.16[1.29-7.74], and 2.56 [1.25-5.26], respectively). Low transportation independence, not having a home caregiver, low medication administration skills, and more than 10 discharge medications increased rhe risk of medication discrepancies (Incidence rate ratio [95% CI]: 1.39 [1.01-1.91], 1.73[1.13-2.66], 1.99 [1.37-2.89], and 1.91 [1.24-2.93], respectively).
Conclusions:
Patient work system factors could be assessed before discharge with indicators for increased risk of poor patient experience and medication discrepancies during older adults’ care transition from hospital to home.
INTRODUCTION
Medication-related harms are a significant threat to older adults and are associated with more than 12 emergency department visits annually per 1000 older adults in the United States, nearly double the rate among younger adults in a recent estimate.[1] Post-hospital discharge is a high risk period for older adults to develop adverse drug events.[2] An improved understanding of modifiable risk factors during care transitions may inform interventions.[1, 3] Human factors and systems engineering approaches have been used to study factors in the home environment that are potentially modifiable and these studies have led to the development of the patient work system model.[4–6] According to the patient work system model, patient and family self-care work is shaped by patient work system elements, such as persons, tasks, tools and context. Persons include patients, caregivers, and professionals (e.g., care transition nurse), while context refers to physical-spatial, social-cultural, and organizational characteristics in a home environment.[5] Although the patient work system model has been used in qualitative analysis of self-care work,[7–9] its potential as an assessment tool has not been explored. In this study, we developed and evaluated measures to assess potentially modifiable patient work system factors for managing medications.[10–12]
After hospitalization, older adults and home caregivers often need to learn about new medications, reconcile regimen changes made during hospitalization, manage transient medications, and develop new routines. The demands of these tasks can be overwhelming because of their quantity (e.g., number of tasks per day) and characteristics (e.g., task complexity). Task burdens may be further magnified due to limited capacity of the patient work system for performing the work of medication management (e.g., lack of a home caregiver).[13–15] From the patient perspective, self-management of medications after hospital discharge can pose demands that outpace the patient work system’s capacity.[16] It may be possible to reduce the task burdens and/or enhance the capacity of a given patient work system. These strategies are often considered in human factors redesign of work systems (termed “fitting the task to the human”).[17, 18]
In this study, we aimed to develop a set of measures of capacity, task and medication management practice factors (called indicators). Furthermore, we aimed to evaluate the potential of these indicators to predict risks for adverse drug events and poor patient experience during care transition among older adults. The data were collected as part of an initiative to redesign hospital-to-home care transition programs to better match medication management task demands and capacities.
METHODS
Study Design
We developed a set of indicators for measuring patient work system factors for managing medications, and then conducted a multi-site observational study to prospectively evaluate these indicators. We assessed patient work systems using the developed indicators through structured interviews and chart review of medications before hospital discharge. After discharge we conducted follow-up visits at patient homes to assess patient experience with medication management and medication discrepancies through structured interviews and direct observation. We evaluated the indicators for their potential in predicting poor patient experience and medication discrepancies.
Measures of Patient Work Systems for Medication Management
We used the patient work system model[5] to develop measures for assessing socio-technical factors in home settings where tasks are performed mostly by older adults and their caregivers, but influenced by collaborative work with healthcare professionals. We considered three groups of factors: (1) capacity for performing the work of medication management, as reflected by cognitive and physical function of the older adult, availability of family caregivers, resources at home, and interactions with a distributed network of professionals, (2) task amount and complexity in managing medications during transition, and (3) medication management practices in communicating about and filling prescriptions.
A multidisciplinary team including human factors specialists, health service researchers, medication safety experts, hospitalists, and primary care physicians iteratively developed indicators for the three groups of patient work system factors. The development was informed by our qualitative analyses of older adult and professional experiences in managing medications during care transition[12, 19, 20] and by existing literature for measures on medication regimen complexity,[21] medication changes,[22] medication discrepancies,[23] medication management by older adults,[24] medication-related problems,[25] and transitional care quality.[26, 27] To be applicable for preventive or ameliorative actions, we selected indicators feasible for assessment before hospital discharge. Each indicator could reflect multiple work system factors. For example, transportation independence provided by owning a car reflects older adult resource access, indicating ability to obtain medications and to attend healthcare appointments, and overall enhanced socio-economic status.
The resulting assessment instrument was piloted over a two-week period with 15 older adult patients at the planned study sites to identify issues with interview questions, including understandability and logistics for recruitment and data collection in hospitals and at patient homes. We revised the instrument and re-piloted it with 23 older adult patients over two weeks, which identified the need for only minor adjustments in data collection instructions. The final assessment instrument can be found in the Appendices.
Six capacity indicators of the patient work system factors were:
having a primary care provider (self-report),
number of prescribers (self-report),
having a home caregiver (self-report),
self-efficacy for medication management (four-item Self-Efficacy for Managing Chronic Conditions – Managing Medication and Treatment,[28] dichotomized into high - positive responses for all items and low - at least one non-positive response to identify weaknesses in any of the items),
medication administration skills (testing for skills in reading a medication label, describing how to take the medication, and opening the bottle, which were adapted from the 19 item Medication Management Instrument for Deficiencies in the Elderly[24] and assessed by a medication bottle test[29]; dichotomized into high - ability to complete all three skills versus low - failing to complete at least one of the tasks), and
transportation independence (using own cars, relying on friends, or public transportation; dichotomized into high - using own cars versus low - using other modalities).
Four task indicators were based on discharge medications (including non-prescription medications, with dichotomization based on prior studies on discharge medications[21, 22, 30]):
number of discharge medications (including as-needed medications, dichotomized into ≤10 and >10),
presence of high alert medications, based on a widely accepted list developed by the Institute for Safe Medication Practices,[31]
number of medication changes compared with home medications (dichotomized into ≤2 and >2), and
medication regimen complexity index (MRCI)[21] of the discharge medications (dichotomized into ≤30 and > 30).
Three practice indicators were:
bringing medications to hospitalisation (self-report for “bringing a list” or “medication bottles”),
picking up medications at discharge (self-report for “always been able to pick up new medications prescribed at discharge”), and
skipping prescription fills in the past year (self-report for “skipped filling your prescriptions due to problems with insurance or paying for medications”).
Main Outcome Measures
To evaluate the association between measures of patient work system factors and medication safety, we assessed medication discrepancies and self-reported experiences in managing medications after discharge. Trained pharmacy technicians used a medication discrepancy tool[23] during in-person home visits to determine discrepancies between what prescription and non-prescription medications the study participant was taking at home and what was listed in the electronic health record. All discrepancies were reviewed and confirmed by a hospital pharmacist. Although not adverse drug events (ADEs) themselves, medication discrepancies have been used to assess potential ADEs.[23, 32] Compared to ADEs or hospital readmissions, medication discrepancies provide a more direct assessment of the consequences of any patient work system factors on the medication management process. Not all medication discrepancies necessarily lead to ADEs and in most cases the adverse consequences of these discrepancies are tolerated by older adults, are not reported, or may not even be recognized. Thus, medication discrepancy was chosen as a more sensitive measure to investigate relations between patient work system factors and medication safety.
Patient experience during care transitions was assessed by a binary question (yes or no) “were you overwhelmed in the first few days after coming home with the new medication regimen?” Since the indicators were used primarily to assess capacity and task factors, we developed this overarching question to capture patient experience in performing medication management tasks. Additionally, participants were asked a set of questions about specific aspects of medication management during care transition: cost concerns, issues with insurance or filling prescriptions, experiencing unexpected side effects with newly prescribed medications, knowledge of newly prescribed medications, awareness of regimen changes made during hospitalisation, receipt of discharge instructions, and understanding of post-discharge medication plans. The patient experience questions were part of the pilot testing procedures described earlier to ensure appropriateness and clarity of wording.
Population
Johns Hopkins University institutional review board approved the study. All patients admitted to the medical and surgical units at two Mid-Atlantic hospitals were screened from August 2018 to July 2019, with three patient care units at a safety-net urban academic hospital and six patient care units at a suburban community hospital. The inclusion criteria were English-speaking patients 65 years of age or older, admitted for medical services, and with an expected length of hospital stay of at least 24 hours. We excluded patients who were discharged to inpatient or skilled nursing facilities, unable to consent due to limited cognitive capabilities (as indicated in the patient’s medical record by any level of cognitive impairment) or living more than 20 miles from the hospital. Sample sizes were based on 5% margin of error on medication discrepancy rates,[33] with a recruitment target of 350 study participants.
Data Collection
Two trained research coordinators, both certified pharmacy technicians, performed daily screening for eligible patients using the inclusion and exclusion criteria on the hospitals’ electronic health record system. The attending physicians of the eligible patients were asked to obtain patients’ verbal agreements for research contact, and then a research coordinator approached patients in their hospital rooms to obtain study participant consent. Following written consent, the research coordinator conducted structured interviews in the patient’s hospital room, usually within 48 hours of expected discharge. The interviews were to assess the capacity and practice indicators. The research coordinator reviewed the discharge medications in the patient medical record at hospital discharge to assess the task indicators. Usually within a week after discharge, the research coordinator conducted in-person structured interviews and observations at patient homes, to assess medication discrepancies, patient experience, and medication management practices at home. Caregivers, if present during interviews, were asked to be study participants and to provide consent. Study participants were compensated $25 for each data collection contact. All data were entered into REDCap (Vanderbilt University, Nashville, TN), a web-based application widely used in clinical research for building, storing, and managing questionnaires and other types of research data.
Data Analysis
We used frequencies with percentages, medians with interquartile ranges or means with standard deviations to characterize responses. To investigate association with patient work system factors, we used Poisson regression models with number of medication discrepancies and multiple logistic regression models with patient experiences in managing medications during transition. Variables with high multi-collinearity were excluded.
RESULTS
The patient work system characteristics were assessed with 376 study participants (Figure 1) among the 4046 eligible patients. Nearly half (2082) were not approached because of lack of verbal agreement to be approached or unavailability (e.g., away from room or sleeping). More than one-third (38.0%) of the 376 participants were 75 years or older and 130 (34.5%) had an annual income of <$25,000 USD (Table 1). Nearly all participants (95.5%) had Medicare insurance coverage (a US public health insurance program for individuals age 65 years and older), and about one-third (32.7%) had two or more prior hospital admissions within the last 12 months.
Figure 1.
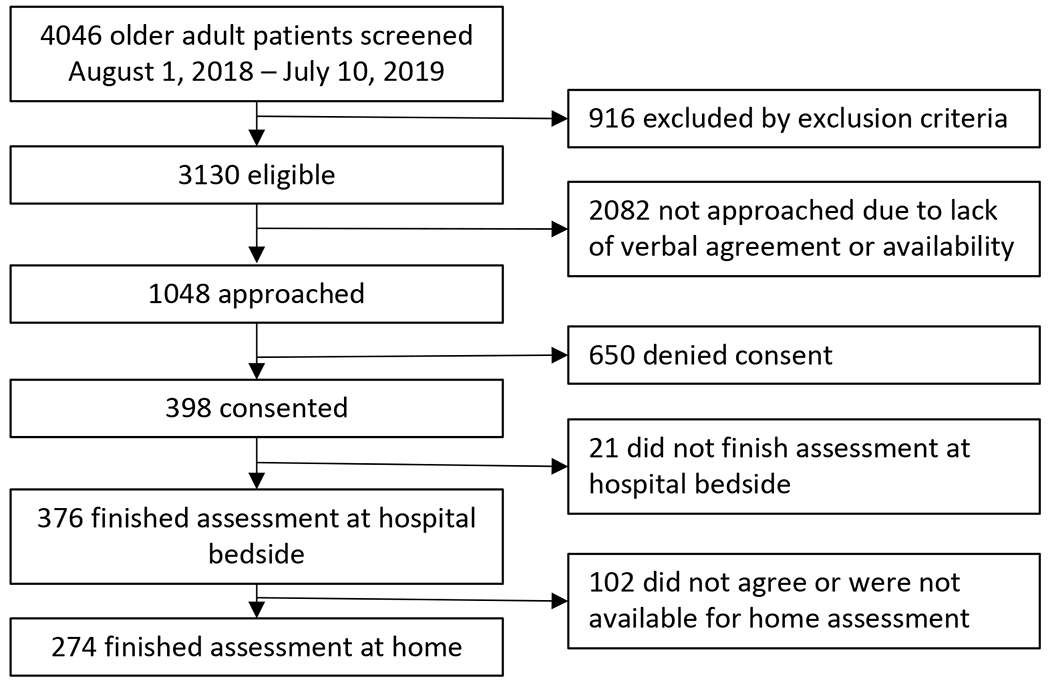
Study flow. Home assessment was targeted within 1-2 weeks of hospital discharge.
Table 1.
Characteristics of study participants. Comparison between the two hospitals was by Chi-square tests or Fisher’s exact tests.
| Total n=376 | Hospital 1 n=156 (41%) | Hospital 2 n=220 (59%) | P value | |
|---|---|---|---|---|
| Sex | ||||
| Female | 61.7 | 69.2 | 56.4 | 0.011 |
| Age (Median, IQR: 72.5, 68.5-78) | ||||
| 65-69 | 30.3 | 35.9 | 26.4 | 0.272 |
| 70-74 | 31.1 | 31.4 | 30.9 | |
| 75-79 | 17.9 | 15.4 | 19.6 | |
| 80-84 | 13.8 | 11.5 | 15.5 | |
| 85+ | 6.9 | 5.8 | 7.6 | |
| Race | ||||
| White | 73.7 | 74.4 | 73.2 | 0.030 |
| Black/African American | 21.8 | 24.4 | 20.0 | |
| Other | 4.5 | 1.3 | 6.8 | |
| Education | ||||
| Below high school | 13.6 | 24.3 | 5.9 | <0.001 |
| High school graduate | 20.7 | 29.5 | 14.5 | |
| More than high school | 65.7 | 46.2 | 79.6 | |
| Income | ||||
| Under $25K | 34.6 | 57.1 | 18.6 | <0.001 |
| $25K - $50K | 22.3 | 24.4 | 20.9 | |
| $50K+ | 39.4 | 16.0 | 55.9 | |
| Not reported | 3.7 | 2.5 | 4.6 | |
| Insurance | ||||
| With Medicaid | 17.0 | 21.8 | 13.6 | 0.082 |
| Without Medicaid | 78.5 | 75.0 | 80.9 | |
| Other | 4.5 | 3.2 | 5.5 | |
| Length of hospital stay | ||||
| 1 day | 4.3 | 8.3 | 1.4 | 0.003 |
| 2 days | 15.2 | 15.4 | 15.0 | |
| 3+ days | 80.3 | 75.7 | 83.6 | |
| Not reported | 0.2 | 0.6 | 0.0 | |
| Top 5 Chronic conditions | ||||
| Congestive heart failure | 25.5 | 34.6 | 19.1 | |
| Diabetes | 25.0 | 27.6 | 23.2 | |
| Coronary artery disease | 19.0 | 25.0 | 16.4 | |
| Chronic obstructive pulmonary disease | 18.1 | 26.3 | 12.3 | |
| Arrhythmia | 6.4 | 9.0 | 4.5 | |
Patient Work System Factors for Medication Management
Nearly one-half (48.9%) reported having three or more prescribers and almost all (97.9%) reported having a primary care provider (Table 2). Most (80.6%) did not have a caregiver at home. Among those having a caregiver at home, between 45.3-72.6% received help from the caregiver for medication-related tasks. About one-fifth (22.6%) reported skipping medications in the past year due to problems with insurance or paying for medications. More than half (53.5%) of the participants reported bringing their medication lists and/or bottle(s) to the hospital on admission. Nearly one-fifth (18.3%) had low medication administration skills. A significant minority (41.2%) expressed low self-efficacy in managing medications, with one-third (34.3%) reporting neutral or negative responses on ability to list their medications.
Table 2.
Characteristics of patient work systems for medication management (n = 376)
| n (%) | |
|---|---|
|
Capacity indicators
| |
| Having a primary care provider | 368 (97.9) |
| Number of prescribers | |
| None | 13 (3.5) |
| 1 | 86 (22.9) |
| 2 | 88 (23.4) |
| 3+ | 184 (48.9) |
| Not reported | 5 (1.3) |
| Having a caregiver at home | 73 (19.4) |
| Tasks that the caregiver helps (percentage of 73 who had a caregiver at home) | |
| Read discharge instructions | 42 (57.5) |
| Explain to you how to take your medications | 46 (63.0) |
| Create a medication schedule for when to take what medications | 40 (54.8) |
| Fill pillboxes | 41 (56.2) |
| Make changes to medications as a result of hospitalization | 33 (45.2) |
| Remind you to take your medications | 53 (72.6) |
| Update your list of medications | 50 (68.5) |
| Help you with medical appointments and other needed tasks | 63 (86.3) |
| Self-efficacy for medication management (positive responses1) | |
| I can follow directions when my doctor changes my medications | 364 (96.8) |
| I can manage my medications without help | 336 (89.4) |
| I can list my medications, including the doses and schedule | 247 (65.7) |
| I can take my medication when there is a change in my usual day (unexpected things happen) | 345 (92.5) |
| Low (at least one non-positive response with four statements) | 155 (41.2) |
| Medication administration skills | |
| Correctly read the drug name on the medication bottle | 334 (88.8) |
| Correctly tell how to take the medication | 329 (87.5) |
| Open the bottle | 335 (89.1) |
| Low (unable to perform at least one of the 3 skills) | 69 (18.3) |
| Transportation Independence | |
| High (owning a car) | 248 (66.0) |
| Low | |
| Friend | 93 (24.7) |
| Public transportation | 13 (3.5) |
| Other | 22 (5.9) |
|
| |
|
Task indicators [Median (interquartile range), range]
| |
| Number of medications on discharge > 10 [12 (8–16), 0-33] | 217 (57.7) |
| Medication regimen complex index > 30 [26 (16.5–37.8), 0-91] | 156 (41.5) |
| Number of high alert medications ≥ 1 [1 (0–2), 0-5] | 228 (60.6) |
| Number of medication changes ≥1 [4 (2–7), 0-22] | 356 (94.7) |
| New medications ≥ 1 [1 (1–3), 0-15] | 290 (77.1) |
| Medications stopped ≥ 1 [1 (0–3), 0-14] | 236 (62.8) |
| Regimen changes ≥ 1 [0 (0–1), 0-8] | 169 (44.9) |
| Formulary change ≥ 1 [0 (0–0), 0-2] | 16 (4.3) |
|
| |
| Practice indicators for medication management | |
| Patient/Caregiver brought medication list or bottles to hospital | 201 (53.5) |
| Not able to pick up new medications prescribed at discharge | 21 (5.6) |
| Skipping medications due to issues of insurance or cost | 85 (22.6) |
Response options are on a 5-point Likert scale ranging from “Strongly Disagree” to “Strongly Agree”, and positive responses were “Agree” or “Strongly Agree”
Most (94.7%) of the participants had one or more changes to their home medications recorded upon admission (Table 2), such as new prescriptions and discontinued medications, with a median of four changes. Nearly two-thirds of the participants had one or more high alert medications, with insulin and opioids as the most frequent types. At discharge, the median number of medications per participant was 12 (IQR 8-16) and 41.5% of the participants had MRCIs higher than 30 (median 26, IQR 16.5-38).
Home visits were conducted with 274 of the 376 (72.9%) study participants to assess medication discrepancies and medication management experiences during the transition from hospital to home. To manage medications at home, most participants reported using medication lists (78.8%) or pill organizers (64.2%), such as multicompartment pillboxes with markers for days or times. Most (88.0%) reported filling their prescription medications at community pharmacies; about a quarter (24.5%) used mail-order pharmacies.
Patient Experience with Medication Management
Forty-two (15.3%) of the study participants felt overwhelmed by medication management tasks (Table 3). Among the task indicators, having more than 10 discharge medications and more than two medication changes at discharge increased the risk of feeling overwhelmed (odds-ratio [range]: 2.63 [1.08-6.38] and 3.16 [1.29-7.74], respectively). Among the capacity indicators, low self-efficacy in medication management increased the risk of feeling overwhelmed (2.56 [1.25-5.26]). Nearly half of participants (43.8%) reported receiving help from hospitals or home care agencies. It was common for the participants to report worries about cost (27.3%), burdensome insurance approval processes (9.2%), difficulties with filling prescriptions (16.4%), and unexpected side effects to newly prescribed medications (18.2%). Only one-third of the 139 participants with new medications (33.8%) knew the consequences of not taking new medications. Nearly all participants reported receiving discharge instruction materials and having a clear understanding what medications were due when coming home (96.4% and 97.0%, respectively).
Table 3.
Patient experience of transitional care assessed at homes, reported by “Yes” answers over completed answers and percentages.
| Assessment items | “Yes” Answers (%) |
|---|---|
| Were you overwhelmed in the first few days after coming home with the new medication regimen? | 42/273 (15.4) |
| Are you worried about the cost of your medications? | 74/271 (27.3) |
| Did you spend a lot of time dealing with insurance approval for your medications? | 25/273 (9.2) |
| Are there prescriptions you have had trouble filling? | 44/269 (16.4) |
| Did the hospital doctors prescribe new medications? If yes | 139/274 (50.7) |
| Have you experienced unexpected side effects to the new medications? | 25/137 (18.2) |
| Appropriate answer to “What would happen if you DO NOT take the new medication(s)?” | 92/139 (66.2) |
| Did the hospital doctors make any changes to your medications? | 103/273 (37.7) |
| When being discharged from the hospital, did you receive an electronic or printed discharge instruction material? | 264/274 (96.4) |
| Was it clear to you when the next dose of your medication was DUE after coming home from the hospital? | 261/269 (97.0) |
Medication Discrepancies
Medication discrepancies were identified in 30.3% of the participants visited at home (83/274), with nutrients and supplements the most frequent types (18.7%). In a multi-variable analysis, four indicators of patient work system factors increased the risk for medication discrepancies (incident risk ratio [range], Figure 2): low transportation independence (1.39 [1.01-1.91]), not having a home helper (1.73 [1.13-2.66]), low medication administration skills (1.99 [1.37-2.89]) and more than 10 discharge medications (1.91 [1.24-2.93]). Although originally expected, along with the three practice indicators, other task indicators were not associated with increased risks for medication discrepancies: high medication regimen complexity (1.24 [0.85-1.82]), high alert medications (1.15 [0.83-1.59]) or high numbers of medication changes (0.88 [0.64-1.22]).
Figure 2.
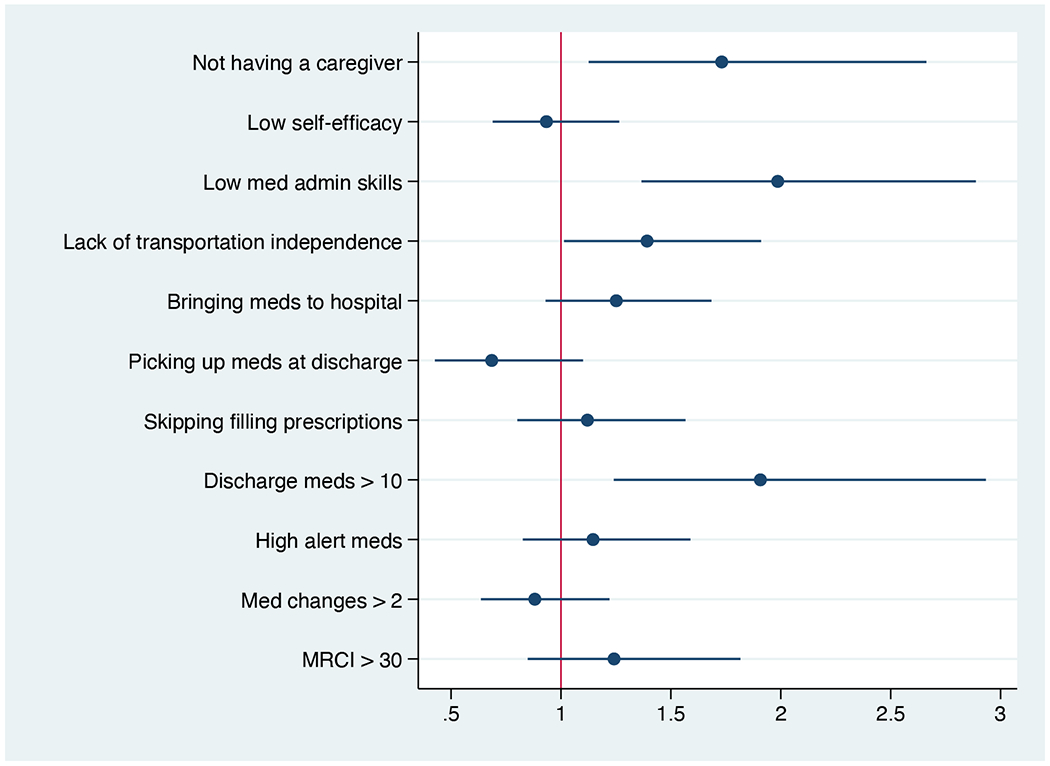
Incidence risk ratios (IRRs) for patient work system factors related to the number of medication discrepancies assessed at the study participant homes after discharge. MRCI: medication regimen complex index. Low med-admin skills: inability to complete all three medication self-management skill tests (reading sample medication labels, describing instructions on labels, and opening the bottles). Low self-efficacy: neutral or negative on responses to at least one item in short form of Self-Efficacy for Managing Chronic Conditions – Managing Medication and Treatment.[28]
DISCUSSION
Our observational study developed and evaluated a set of measures to assess patient work systems in managing medications during older adults’ transition to home following hospitalisation. This approach addressed a gap in improving medication safety in ambulatory care settings, which is a function of the patient work system, including its capacity for medication management, the tasks imposed, and medication management practices. The measures can be assessed before hospital discharge, which enables them to be used to address risks for potential adverse drug events and poor patient experiences during care transitions. The study added new concepts in assessing capacities, tasks and medication management practices during care transition, beyond the holistic assessment of healthcare task difficulty among older adults.[34] In this studied population of older adults, the burden of medication management tasks during transition of care was high in terms of number of discharge medications and medication regimen changes, similar to the finding from a prior study.[22]
Our evaluation of the 13 indicators suggests ways to reduce future assessment burdens. Among the task factor indicators, two relatively straightforward counts of discharge medications and changes predicted poor patient experience and potential adverse drug events. In comparison, MRCI was not associated with higher risks of adverse outcomes, despite the nuances of medication management tasks captured by MRCI.[21, 30] Risks associated with polypharmacy have been targeted with interventions such as deprescribing,[27] while high numbers of regimen changes or overprescribing have not been recognized as a task factor that increases risk for poor patient experiences or medication safety.
Among the capacity factor indicators, not having a caregiver and lack of transportation independence may flag meaningful home risk factors. Among the study participants, whose median age was 72.5 years, over 80% did not have a home caregiver. When compared with the four-item self-efficacy survey, testing of medication administration skills[24] is time-consuming, yet a bottle test may be needed to assess patients’ physical, vision and cognitive ability in managing medications. Many older adults have reduced cognitive and physical functions.[35, 36] A similar skills test was used in a study to identify deficiencies in medication self-management skills.[29] Finally, contrary to our expectations, higher numbers of prescribers were not associated with risks for higher numbers of medication discrepancies. While over 50% of the participants reported bringing medications or lists of medications to hospitals, this did not translate into fewer medication discrepancies in our study. Similarly, prior challenges in accessing medications were not predictive of higher numbers of medication discrepancies, as highlighted in qualitative studies.[20] Medication materials management, such as identifying optimal storage locations, were complex and idiosyncratic. Incorporating new medications into these practices indicates enduring task demands after discharge. We also identified that only one-third of the participants were able to articulate the reasons why they were prescribed a new medication at discharge, even though nearly all received discharge instructions in the hospital.
The results of our study have direct implications for medication safety improvement interventions during transitions, as well as for measuring patient experiences with medication management. Risks for medication-related harms in ambulatory care and suboptimal patient experiences are multidimensional and complex.[37, 38] Some of the challenges in studying medication use in ambulatory settings include a lack of comprehensive data, the distributed nature of multiple providers and prescribers, the volume of care episodes, and burden of chronic conditions.[39, 40] The indicators developed are novel and systematically capture risk of failures in medication management by older adults and their caregivers during the transition from hospital to home. In comparison with other assessment tools (e.g., [41]), the indicators identify potentially reversible risk factors associated with patient work systems not yet systematically targeted. One scoping review[42] identified a major gap in caregiver engagement, in line with the findings of our study. The indicators may help guide more targeted approaches in caregiver engagement, such as those with high task burden as reflected by task indicators. A systematic review[43] identified supporting evidence for interventions in older adults through self-management coaching, medication reconciliation and patient-initiated communication during transition, also in line with the findings of our study. Self-management coaching should enhance capacities of patient work systems. Medication reconciliation could be enhanced to flag patients with high numbers of discharge medications and adjustments as needing additional support. Proactive, patient-centered communication after discharge is important to address poor patient experience, such as feeling overwhelmed with new medications.
Below we outline three future strategies to redesign the support of older adults’ care transition from the hospital to home. First, health professionals should actively recruit caregivers to support older adults who have capacity and task related risk factors. Families and older adults themselves may need tools to realistically assess medication management needs during care transitions.[24] Second, community pharmacies are an important resource, given that most older adults (88%) filled discharge medications through them. Health professionals should inform patients about the role of community pharmacists who can help patients review and reconcile discharge medications.[44] This approach should complement the recommendation of working with primary care practices to improve care transitions, although growing use of mail order and online pharmacies may reduce the feasibility and effectiveness of this strategy. Third, the goal of medication reconciliation should include supporting patient work systems, both in terms of clinical outcomes of avoiding medication related harms and patient centered outcomes.[45] As assessed in this study, it was common for older adults to feel overwhelmed and struggle with tasks related to cost and insurance coverage, which may be viewed as a form of “safety hazards” to medication safety that the older adults and families have to navigate around and overcome.[20] Post-discharge support, such as those provided by hospital personnel and home health nurses, could help address patient work system factors during medication reconciliation, and identify knowledge deficits such as lack of awareness of medication changes or reasons for new medications.
This study had several limitations. It was conducted within one healthcare system in the US. Older adults in other types of communities may differ in their work system factors impacting on medication management, such as those in rural areas, those with language barriers, and those in different countries with different services available and usage patterns of such services. Capacity factor indicators should be adapted to settings and cultures. It is important to note that we intentionally recruited study participants from a suburban hospital and an inner-city hospital serving under-resourced and disadvantaged communities. The lay public was not directly involved in the development of the indicators even though they were based on qualitative studies of older adults during care transition and input from professionals with extensive experience in addressing challenges during care transition. Assessment of patient experience was limited to a binary question (“Were you overwhelmed …?”). Further validation of this question in assessing patient experiences is needed. We limited the study to measures that may be assessed during a hospital stay. The medication safety outcomes assessed were short-term and process-oriented. Data on adverse drug events, post-discharge health services utilizations, and views from community health professionals were not included. Future studies are needed to build on the measures assessed in this study with longer term outcomes in different community settings. The recruitment and follow-up home assessment may have introduced biases to study findings as we were able to approach only about half of the eligible patients for research consent, obtain consent from about 40% when approached, and conduct home assessment in about 75% of the recruited study participants. Nevertheless, the study results should provide information to reduce burdens in future deployment of similar assessment tools, and thus potentially reduce recruitment and follow-up biases. The study was conducted prior to the COVID-19 pandemic, which introduced profound changes in society, including wider uses of telehealth services. However, it is perhaps more pertinent to assess patient work systems along the indicators reported here as older adults continue to work within fragmented health systems, and professionals continue to work with electronic health record systems and medication reconciliation processes in place before the pandemic. There are increased pressures on professionals in primary care, hospitals, and pharmacies that include staffing issues that impact transitions of care.
CONCLUSION
Patient work system factors including high numbers of medications, regimen changes, low medication management efficacy and limited self-management skills were associated with increased risks of poor patient experience and medication discrepancies during the care transition from hospital to home among older adults. With public involvement and adaptation to specific settings, these indicators may be used in assessment of task and capacity related risk factors to individualize risk-reduction efforts as older adults and families take on medication management when transitioning to home. For older adults, reduction of medication management task burdens through identifying and involving caregivers, and through deprescribing and simplifying medication regimens should be emphasized as a strategy to improve medication safety during care transitions.
Supplementary Material
What is already known on this topic
Older adults are at an increased risk for adverse drug events following discharge to home after hospitalisation. Risk factors have been identified in terms of demographics and disease conditions.
What this study adds
A set of candidate indicators based on human factors work system design principles were developed and evaluated to assess capacity, task and practice factors in medication management. In older adults, several indicators were found to be associated with increased risk for adverse drug events and with poor patient experience after discharge to home.
How this study might affect research, practice or policy
Capacity factors in post-discharge medication management and task factors may support novel assessment tools for modifiable risk factors, and thus interventions to address specific capacity or task related-risk factors.
Funding.
This study was funded by the Agency for Healthcare Research and Quality (R01 HS 024436). The content is solely the responsibility of the authors and does not necessarily represent the official views of the sponsor.
Footnotes
Competing interests. None declared.
Patient consent for publication. Consent obtained from parent(s)/guardian(s).
Ethics approval. This study involves human participants and was approved by Johns Hopkins University (IRB Protocol 00086698). Participants gave informed consent to participate in the study before taking part.
REFERENCES
- 1.Budnitz DS, Shehab N, Lovegrove MC, et al. US Emergency Department Visits Attributed to Medication Harms, 2017-2019. Jama. 2021. Oct 5;326(13):1299–309. Epub 2021/10/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kanaan AO, Donovan JL, Duchin NP, et al. Adverse drug events after hospital discharge in older adults: types, severity, and involvement of Beers Criteria Medications. Journal of the American Geriatrics Society. 2013. Nov;61(11):1894–9. Epub 2013/10/15. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parekh N, Ali K, Davies JG, et al. Medication-related harm in older adults following hospital discharge: development and validation of a prediction tool. BMJ quality & safety. 2020. Feb;29(2):142–53. Epub 2019/09/19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Werner NE, Tong M, Borkenhagen A, et al. Performance-Shaping Factors Affecting Older Adults’ Hospital-to-Home Transition Success: A Systems Approach. Gerontologist. 2018. Jan 3. Epub 2018/01/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holden RJ, Schubert CC, Mickelson RS. The patient work system: an analysis of self-care performance barriers among elderly heart failure patients and their informal caregivers. Applied ergonomics 2015. Mar;47:133–50. Epub 2014/12/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holden RJ, Carayon P, Gurses AP, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics 2013;56(11):1669–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Werner NE, Ponnala S, Doutcheva N, et al. Human factors/ergonomics work system analysis of patient work: state of the science and future directions. International journal for quality in health care : journal of the International Society for Quality in Health Care / ISQua. 2021. Jan 12;33(Supplement_1):60–71. Epub 2021/01/13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kleman C, Magnus JM, Andrews M, et al. The work of managing a chronic illness: A job description. J Eval Clin Pract. 2023. Feb;29(1):166–80. Epub 2022/08/30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ozkaynak M, Valdez R, Hannah K, et al. Understanding Gaps Between Daily Living and Clinical Settings in Chronic Disease Management: Qualitative Study. J Med Internet Res. 2021. Feb 25;23(2):e17590. Epub 2021/02/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murray MD, Morrow DG, Weiner M, et al. A conceptual framework to study medication adherence in older adults. The American journal of geriatric pharmacotherapy. 2004. Mar;2(1):36–43. Epub 2004/11/24. eng. [DOI] [PubMed] [Google Scholar]
- 11.Robinson S, Howie-Esquivel J, Vlahov D. Readmission risk factors after hospital discharge among the elderly. Population health management. 2012. Dec;15(6):338–51. [DOI] [PubMed] [Google Scholar]
- 12.Xiao Y, Abebe E, Gurses AP. Engineering a Foundation for Partnership to Improve Medication Safety during Care Transitions. J Patient Saf Risk Manag. 2019. Feb 1;24(1):30–6. Epub 2019/03/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maddigan SL, Farris KB, Keating N, et al. Predictors of older adults’ capacity for medication management in a self-medication program: a retrospective chart review. J Aging Health. 2003. May;15(2):332–52. Epub 2003/06/11. [DOI] [PubMed] [Google Scholar]
- 14.Cross AJ, Elliott RA, Petrie K, et al. Interventions for improving medication-taking ability and adherence in older adults prescribed multiple medications. Cochrane Database Syst Rev. 2020. May 8;5:CD012419. Epub 2020/05/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liebzeit D, Geiger O, Jaboob S, et al. Older Adults’ Process of Collaborating with a Support Team during Transitions from Hospital to Home: A Grounded Theory Study. Gerontologist. 2023. Jul 12. Epub 2023/07/12. [DOI] [PubMed] [Google Scholar]
- 16.Shippee ND, Shah ND, May CR, et al. Cumulative complexity: a functional, patient-centered model of patient complexity can improve research and practice. Journal of clinical epidemiology. 2012. Oct;65(10):1041–51. [DOI] [PubMed] [Google Scholar]
- 17.Gurses AP, Ozok AA, Pronovost PJ. Time to accelerate integration of human factors and ergonomics in patient safety. BMJ quality & safety. 2012. Apr;21(4):347–51. Epub 2011/11/30. eng. [DOI] [PubMed] [Google Scholar]
- 18.Kroemer KHE, Kroemer KHE. Fitting the human : introduction to ergonomics. 6th ed. Boca Raton: CRC Press; 2009. xix, 437 p. p. [Google Scholar]
- 19.Hannum SM, Abebe E, Xiao Y, et al. Engineering care transitions: Clinician perceptions of barriers to safe medication management during transitions of patient care. Applied ergonomics. 2020. Nov 5;91:103299. Epub 2020/11/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xiao Y, Smith A, Abebe E, et al. Understanding Hazards for Adverse Drug Events Among Older Adults After Hospital Discharge: Insights From Frontline Care Professionals. Journal of patient safety. 2022. May 22. Epub 2022/05/27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.George J, Phun YT, Bailey MJ, et al. Development and validation of the medication regimen complexity index. The Annals of pharmacotherapy. 2004. Sep;38(9):1369–76. [DOI] [PubMed] [Google Scholar]
- 22.Harris CM, Sridharan A, Landis R, et al. What happens to the medication regimens of older adults during and after an acute hospitalization? Journal of patient safety. 2013. Sep;9(3):150–3. [DOI] [PubMed] [Google Scholar]
- 23.Coleman EA, Smith JD, Raha D, et al. Posthospital medication discrepancies: prevalence and contributing factors. Archives of internal medicine. 2005. Sep 12;165(16):1842–7. Epub 2005/09/15. eng. [DOI] [PubMed] [Google Scholar]
- 24.Orwig D, Brandt N, Gruber-Baldini AL. Medication management assessment for older adults in the community. Gerontologist. 2006. Oct;46(5):661–8. [DOI] [PubMed] [Google Scholar]
- 25.Snyder ME, Pater KS, Frail CK, et al. Utility of a brief screening tool for medication-related problems. Res Social Adm Pharm. 2015. Mar-Apr;11(2):253–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coleman EA, Mahoney E, Parry C. Assessing the quality of preparation for posthospital care from the patient’s perspective: the care transitions measure. Medical care. 2005. Mar;43(3):246–55. [DOI] [PubMed] [Google Scholar]
- 27.Hansen LO, Greenwald JL, Budnitz T, et al. Project BOOST: effectiveness of a multihospital effort to reduce rehospitalization. Journal of hospital medicine. 2013. Aug;8(8):421–7. [DOI] [PubMed] [Google Scholar]
- 28.Gruber-Baldini AL, Velozo C, Romero S, et al. Validation of the PROMIS((R)) measures of self-efficacy for managing chronic conditions. Qual Life Res. 2017. Jul;26(7):1915–24. Epub 2017/02/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Howell EH, Senapati A, Hsich E, et al. Medication self-management skills and cognitive impairment in older adults hospitalized for heart failure: A cross-sectional study. SAGE Open Med. 2017;5:2050312117700301. Epub 2017/05/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schoonover H, Corbett CF, Weeks DL, et al. Predicting potential postdischarge adverse drug events and 30-day unplanned hospital readmissions from medication regimen complexity. Journal of patient safety. 2014. Dec;10(4):186–91. Epub 2014/11/20. eng. [DOI] [PubMed] [Google Scholar]
- 31.Institute for Safe Medication Practices. High-Alert Medications in Community/Ambulatory Care Settings 2021. [Available from: https://www.ismp.org/recommendations/high-alert-medications-community-ambulatory-list.
- 32.Alqenae FA, Steinke D, Keers RN. Prevalence and Nature of Medication Errors and Medication-Related Harm Following Discharge from Hospital to Community Settings: A Systematic Review. Drug Saf. 2020. Jun;43(6):517–37. Epub 2020/03/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lindquist LA, Yamahiro A, Garrett A, et al. Primary care physician communication at hospital discharge reduces medication discrepancies. Journal of hospital medicine. 2013. Dec;8(12):672–7. Epub 2013/12/07. eng. [DOI] [PubMed] [Google Scholar]
- 34.Boyd CM, Wolff JL, Giovannetti E, et al. Healthcare task difficulty among older adults with multimorbidity. Medical care. 2014. Mar;52 Suppl 3:S118–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barbas NR, Wilde EA. Competency issues in dementia: medical decision making, driving, and independent living. J Geriatr Psychiatry Neurol. 2001. Winter; 14(4):199–212. Epub 2002/01/17. [DOI] [PubMed] [Google Scholar]
- 36.Beckman A, Bernsten C, Parker MG, et al. The difficulty of opening medicine containers in old age: a population-based study. Pharm World Sci. 2005. Oct;27(5):393–8. Epub 2005/12/13. [DOI] [PubMed] [Google Scholar]
- 37.Sarkar U, Lopez A, Maselli JH, et al. Adverse drug events in U.S. adult ambulatory medical care. Health services research. 2011. Oct;46(5):1517–33. Epub 2011/05/11. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sarkar U, Wachter RM, Schroeder SA, et al. Refocusing the lens: patient safety in ambulatory chronic disease care. Joint Commission journal on quality and patient safety / Joint Commission Resources. 2009. Jul;35(7):377–83, 41. [DOI] [PubMed] [Google Scholar]
- 39.Hochhalter AK, Basu R, Prasla K, et al. Retrospective cohort study of medication adherence and risk for 30-day hospital readmission in a Medicare Cost Plan. Managed care (Langhorne, Pa). 2014. Jan;23(1):43–7. Epub 2014/04/29. eng. [PubMed] [Google Scholar]
- 40.Sikka R, Xia F, Aubert RE. Estimating medication persistency using administrative claims data. The American journal of managed care. 2005. Jul;11(7):449–57. Epub 2005/07/28. eng. [PubMed] [Google Scholar]
- 41.Glans M, Kempen TGH, Jakobsson U, et al. Identifying older adults at increased risk of medication-related readmission to hospital within 30 days of discharge: development and validation of a risk assessment tool.. BMJ Open. 2023. Aug. Epub 2023/08/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liebzeit D, Rutkowski R, Arbaje AI, et al. A scoping review of interventions for older adults transitioning from hospital to home. Journal of the American Geriatrics Society. 2021. Oct;69(10):2950–62. Epub 2021/06/20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tomlinson J, Cheong VL, Fylan B, et al. Successful care transitions for older people: a systematic review and meta-analysis of the effects of interventions that support medication continuity. Age and ageing. 2020. Jul 1;49(4):558–69. Epub 2020/02/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.White A, Fulda KG, Blythe R, et al. Defining and enhancing collaboration between community pharmacists and primary care providers to improve medication safety. Expert Opin Drug Saf. 2022. Nov 21:1–8. Epub 2022/11/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Redmond P, Grimes TC, McDonnell R, et al. Impact of medication reconciliation for improving transitions of care. Cochrane Database Syst Rev. 2018. Aug 23;8:CD010791. Epub 2018/08/24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


