Abstract
A 27-year-old man sustained right ring and little finger proximal interphalangeal joint fracture dislocations. He subsequently underwent bilateral hemi-hamate autograft to treat these intra-articular injuries. The patient was followed periodically and demonstrated return of normal grip strength and radiographic union of the hemi-hamate reconstruction arthroplasties. This is the first reported case of a patient who underwent bilateral hamates as donor grafts for two proximal interphalangeal joint fracture dislocations. When patients present with multiple unrepairable proximal interphalangeal joint fracture dislocations, surgeons can consider bilateral hemi-hamate reconstruction arthroplasty as a consideration to restore normal function.
Key words: Autograft, Fracture dislocation, Hemi-hamate, PIPJ
The proximal interphalangeal (PIP) joint is critical for normal hand function, as it accounts for approximately 85% of the motion required in functional grip.1 Hyperextension or axial loading during joint flexion can result in a fracture dislocation of the PIP joint.2 Proximal interphalangeal joint fractures are particularly difficult to treat because of their predilection for stiffness.3 Whether nonsurgical or surgical management is utilized, the goals of treatment remain the same: restore concentric reduction of the joint to provide the patient the ability to resume normal, active range-of-motion as soon as possible.4
Available treatment options for PIP joint fracture dislocations include initial reduction followed by immobilization, protected motion, open reduction with internal fixation, percutaneous fixation, dynamic external fixation, extension-block pinning, and hemi-hamate reconstruction arthroplasty (HHRA).5, 6, 7, 8, 9 Hemi-hamate reconstruction arthroplasty is one option that is particularly appealing for treating highly comminuted PIP joint fracture dislocations or those with joint involvement greater than 50%.10 This procedure exploits the similarity in articular surface contours between the volar base of the middle phalanx and dorsal hamate at the location where it articulates with the base of the fourth and fifth metacarpals and is supported by strong postoperative clinical outcomes, especially when considering the severity of the initial injury.10,11
In this case report, we discuss a surgical case in which a patient had two PIP joint fracture dislocations treated with HHRA using portions of his bilateral hamates as donor sites. At the time of conception of this article, there were no published reports featuring patients who underwent HHRA for multiple digits using bilateral hamates.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Case Presentation
A 27-year-old right-hand-dominant man without relevant medical history presented to the emergency department with right ring and small finger pain after punching a wall. On physical examination, there was tenderness to palpation, swelling, and a severe lack of motion to the ring and small finger PIP joints. Radiographs were remarkable for right ring and small finger middle phalanx base fractures involving approximately 40% to 50% of both joint surfaces with well-aligned fractures and joint surfaces (Fig. 1). The patient was placed in an ulnar-gutter dorsal blocking splint and planned for nonsurgical care. He returned to the clinic 2 weeks later with radiographs demonstrating loss of reduction with dorsal subluxation/dislocation of his right ring and small finger PIP joints (Fig. 2). The original evaluation and first follow-up were at an outside facility. He was then recommended to see our practice for another opinion on care and he did not present until around the 6-week mark from injury.
Figure 1.
Orthogonal radiographs taken at the time of injury demonstrating right ring and little finger base of the middle phalanx fracture dislocations.
Figure 2.
Orthogonal radiographs taken at 2 weeks from injury showing right ring and little finger base of the middle phalanx fracture dislocations with loss of acceptable alignment.
Radiographs at that time showed continued dorsal subluxation/dislocation of both fingers with signs of healing in a mal-united position (Fig. 3). A computerized tomography scan was performed to better evaluate the bone and joint surface, and these images confirmed the size of the fractures and the middle phalanx articular surface impaction with comminution. After careful discussion regarding the risks, benefits, and alternatives, the patient agreed to proceed with surgical intervention for possible open reduction internal fixation versus hemi-hamate arthroplasty for one or both fractures.
Figure 3.
Orthogonal radiographs taken near 6 weeks after the initial injury demonstrating loss of acceptable alignment of the middle phalanx fractures with continued PIP joint dorsal subluxation, worsened middle phalanx impaction, and healing in a mal-united position.
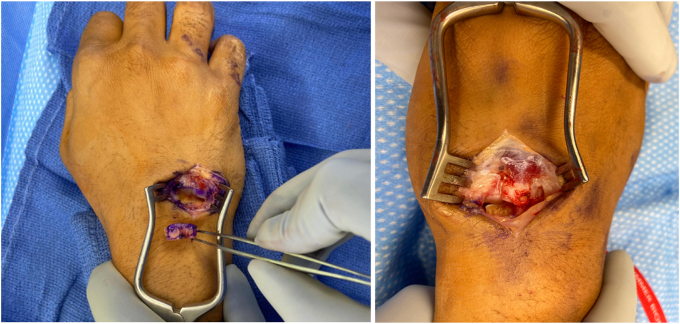
Volar approaches to both PIP joints using Brunner incisions were utilized, the flexor tendons were retracted, and a volar plate flap was made to allow visualization of the PIP joint. Both ring and little finger PIP joints had extensive comminution and thus were not amenable to fixation (Fig. 4). At this point, the decision was made to perform bilateral hemi-hamate arthroplasty. The defect of the PIP joint was resurfaced and measured prior to the preparation of the donor site graft in each finger.
Figure 4.
Intraoperative visualization of the two bases of the middle phalanx fractures demonstrating intra-articular fractures that comprise approximately 50% of the articular surface.
Attention was then turned to the dorsum of the ipsilateral hand. A longitudinal incision over the hamate was made, and dissection down the capsule between the extensor digitorum communis and extensor digiti minimi tendons was performed, being careful to leave an appropriate cuff of capsule to repair. The hamate was exposed and an osteotome was used to harvest the amount measured for the proximal phalanx defect of the small finger. The contralateral upper extremity had already been prepped and draped and now a similar approach was utilized to approach and harvest the contralateral hamate autograft (Fig. 5).
Figure 5.
Intraoperative visualization of the right and left hamate donor graft/sites that were harvested at the point where the hamate articulates with the base of the fourth and fifth metacarpals.
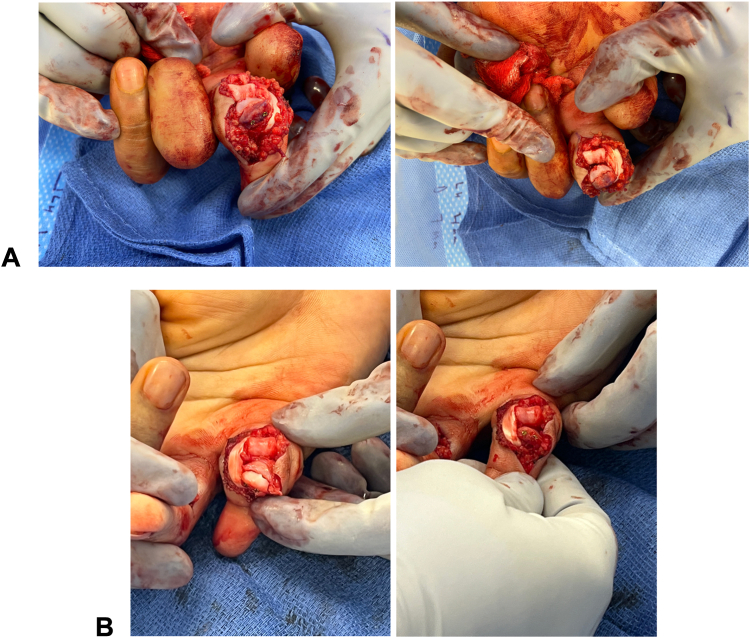
After both hamate grafts were obtained, attention was turned to fixation of the grafts to each middle phalanx base defect. A 0.028 Kirschner wire was used to provisionally fixate the grafts and assess graft fit and stability through range-of-motion using fluoroscopy. Once accepted, a lag by technique method was used for fixation, overdrilling the graft with a 1.2-mm drill and the far cortex with a 1.0-mm drill. Three screws were used for the ring finger (two size 1.2 mm and one 1.7 mm) and two screws for the small finger (two size 1.2 mm). Visual inspection and fluoroscopy were used to assess stability through range-of-motion and graft fit (Fig. 6). He was placed in a dorsal blocking splint with the PIP joint held in approximately 20° of flexion for 1 to 2 weeks prior to starting with outpatient occupational therapy. He was instructed on flexion exercises in the splint prior to therapy.
Figure 6.
A Intraoperative placement of ring finger hemi-hamate graft. B Intraoperative placement of small finger hemi-hamate graft.
At the 14-month follow-up, he maintained painless motion and was without any tenderness to palpation or instability. Visual analog scale score was 1/10 at worst with some heavy lifting activity. His active range-of-motion was as follows: ring finger flexion-extension arc of 45–95 degrees and little finger of 40–100 degrees (Fig. 7A). He had good pulp to palm motion and reported subjective confidence in making a fist and gripping objects normally. Radiographs revealed fully healed hamate grafts and stable joint surfaces with remodeling (Fig. 7B). The patient returned to office-type work at 4 weeks postsurgery and returned to full activity of recreational sports, weight lifting and kick boxing by 3–4 months postsurgery. His grip strength was 91 lbs on the injured side and 122 on the uninjured side. No complications were encountered during surgery or postoperative care for either hand.
Figure 7.
A Clinical photographs on final follow-up. B Orthogonal radiographs demonstrating union of the hamate grafts to the middle phalanges and continued reduction of the PIP joint surface with remodeling.
Discussion
In general, the success of surgical treatment for PIP joint fracture dislocations hinders joint stability following reduction.5,12 Although achieving an anatomic reduction of the articular surface is ideal, several studies have demonstrated that failure to obtain a smooth articular surface following reduction is not correlated with posttraumatic arthritic changes or poor clinical outcomes.13,14
Although uncommon, these HHRA procedures have yielded satisfactory patient outcomes. In a case series of 12 patients, Williams et al15 reported a 91.7% and 100% patient satisfaction and bony union rate, respectively. Calfee et al11 also found HHRA to be relatively successful, as the mean grip strength of hands that underwent HHRA was 95% of the contralateral, unaffected side. These positive outcomes have been sustained with longer patient follow-up, as a study by Afendras et al16 reported a mean visual analog scale pain score of 1 (of 10) at an average follow-up period of 5 years. Moreover, these outcomes do not come at the expense of significant donor site morbidity.16
Bilateral HHRA was chosen in our patient for several reasons. Open reduction internal fixation was hindered by the extent of comminution about the fracture and chronicity of the fracture. Since the fracture encompassed the volar buttress of the middle phalanx, an early range-of-motion about the joint would likely have resulted in continued dorsal subluxation and instability.9,10 Furthermore, male patients up to their third decade of life without prior evidence of PIP joint arthrosis have experienced the most consistent positive results with HHRA across previous studies.11,17
In evaluating the outcomes clinically and radiographically, one should be critical. Radiographs show a concentric and remodeled joint surface 1 year from surgery, and clinical examination reveals a 50° arc of motion at the PIP joint of the ring finger and a 60° arc of motion at the little finger. Grip strength of the injured dominant hand was at 75% of the uninjured hand. Our patient had two reconstructed joints, and it may be postulated that this is the cause of a lower grip strength than other reports.6,16,18 These motion results are some of the existing literature on HHRA with an average arc of motion at the PIP joint of 63° in chronic injuries and less than others of motion in 70% to 85%. This patient did enter therapy soon after surgery; however, he did not complete the course as our team would have preferred and was lost to follow-up for close to a year. Finger flexion with pulp to palm has been acceptable for this patient, and his main deficit in motion is extension. He did report being able to extend more at times later in the day with use.
This case report demonstrates the ability of HHRA to restore congruent PIP joint motion and subsequently provide symptomatic relief in patients who sustain certain intra-articular fractures of the middle phalanx base. Furthermore, this is the first reported case of a patient who underwent bilateral hamates as donor grafts for two PIP joint fracture dislocations. When patients present with multiple unrepairable PIP joint fracture dislocations, surgeons can consider bilateral HHRA as a consideration to restore normal function.
Conflicts of Interest
No benefits in any form have been received or will be received related directly to this article.
References
- 1.Leibovic S.J., Bowers W.H. Anatomy of the proximal interphalangeal joint. Hand Clin. 1994;10(2):169–178. [PubMed] [Google Scholar]
- 2.Jones N.F., Jupiter J.B., Lalonde D.H. Common fractures and dislocations of the hand. Plast Reconstr Surg. 2012;130(5):722e–736e. doi: 10.1097/PRS.0b013e318267d67a. [DOI] [PubMed] [Google Scholar]
- 3.Bindra R., Colantoni Woodside J. Treatment of proximal interphalangeal joint fracture-dislocations. JBJS Rev. 2015;3(12) doi: 10.2106/JBJS.RVW.O.00019. [DOI] [PubMed] [Google Scholar]
- 4.Kamnerdnakta S., Huetteman H.E., Chung K.C. Complications of proximal interphalangeal joint injuries: prevention and treatment. Hand Clin. 2018;34(2):267–288. doi: 10.1016/j.hcl.2017.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Freiberg A. Management of proximal interphalangeal joint injuries. Can J Plast Surg. 2007;15(4):199–203. doi: 10.1177/229255030701500407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams R.M.M., Hastings H., Kiefhaber T.R. PIP fracture/dislocation treatment technique: use of a hemi-hamate resurfacing arthroplasty. Tech Hand Up Extrem Surg. 2002;6(4):185–192. doi: 10.1097/00130911-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Newington D.P., Davis T.R., Barton N.J. The treatment of dorsal fracture-dislocation of the proximal interphalangeal joint by closed reduction and Kirschner wire fixation: a 16-year follow up. J Hand Surg Br. 2001;26(6):537–540. doi: 10.1054/jhsb.2001.0698. [DOI] [PubMed] [Google Scholar]
- 8.Lee L.S., Lee H.M., Hou Y.T., Hung S.T., Chen J.K., Shih J.T. Surgical outcome of volar plate arthroplasty of the proximal interphalangeal joint using the Mitek micro GII suture anchor. J Trauma. 2008;65(1):116–122. doi: 10.1097/TA.0b013e3181454ad4. [DOI] [PubMed] [Google Scholar]
- 9.Capo J.T., Hastings H., Choung E., Kinchelow T., Rossy W., Steinberg B. Hemicondylar hamate replacement arthroplasty for proximal interphalangeal joint fracture dislocations: an assessment of graft suitability. J Hand Surg Am. 2008;33(5):733–739. doi: 10.1016/j.jhsa.2008.01.012. [DOI] [PubMed] [Google Scholar]
- 10.Elfar J., Mann T. Fracture-dislocations of the proximal interphalangeal joint. J Am Acad Orthop Surg. 2013;21(2):88–98. doi: 10.5435/JAAOS-21-02-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Calfee R.P., Kiefhaber T.R., Sommerkamp T.G., Stern P.J. Hemi-hamate arthroplasty provides functional reconstruction of acute and chronic proximal interphalangeal fracture-dislocations. J Hand Surg Am. 2009;34(7):1232–1241. doi: 10.1016/j.jhsa.2009.04.027. [DOI] [PubMed] [Google Scholar]
- 12.Haase S.C., Chung K.C. Current concepts in treatment of fracture-dislocations of the proximal interphalangeal joint. Plast Reconstr Surg. 2014;134(6):1246–1257. doi: 10.1097/PRS.0000000000000854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agee J.M. Unstable fracture dislocations of the proximal interphalangeal joint. Treatment with the force couple splint. Clin Orthop Relat Res. 1987;(214):101–112. [PubMed] [Google Scholar]
- 14.Kiefhaber T.R., Stern P.J. Fracture dislocations of the proximal interphalangeal joint. J Hand Surg Am. 1998;23(3):368–380. doi: 10.1016/S0363-5023(05)80454-X. [DOI] [PubMed] [Google Scholar]
- 15.Williams R.M.M., Kiefhaber T.R., Sommerkamp T.G., Stern P.J. Treatment of unstable dorsal proximal interphalangeal fracture/dislocations using a hemi-hamate autograft. J Hand Surg Am. 2003;28(5):856–865. doi: 10.1016/s0363-5023(03)00304-6. [DOI] [PubMed] [Google Scholar]
- 16.Afendras G., Abramo A., Mrkonjic A., Geijer M., Kopylov P., Tägil M. Hemi-hamate osteochondral transplantation in proximal interphalangeal dorsal fracture dislocations: a minimum 4-year follow-up in eight patients. J Hand Surg Eur Vol. 2010;35(8):627–631. doi: 10.1177/1753193410373311. [DOI] [PubMed] [Google Scholar]
- 17.Korambayil P.M., Francis A. Hemi-hamate arthroplasty for pilon fractures of finger. Indian J Plast Surg. 2011;44(3):458–466. doi: 10.4103/0970-0358.90822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Calfee R.P., Sommerkamp T.G. Fracture-dislocation about the finger joints. J Hand Surg Am. 2009;34(6):1140–1147. doi: 10.1016/j.jhsa.2009.04.023. [DOI] [PubMed] [Google Scholar]