Abstract
Purpose
The use of mobile phone applications (apps) in the health sector, including in eye care, is increasing. This study aimed to compare interpupillary distance (IPD) measurements using common clinical techniques (pupillometer, PD ruler, and autorefractor), which are contact procedures, with measurements from a non-contact mobile phone application.
Methods
Forty participants were recruited (mean age 25.65±3.72 years, 21 male and 19 female). Binocular distance and near IPD measurements from four instruments were compared: pupillometer (TOPCON PD-5, Japan), PD ruler, auto-refractor (KR-8100P, TOPCON, Japan), and Mobile Application (Eye Measure, 1.22). Two consecutive measurements were performed. The pupillometer measurement was used as the gold standard measurement for the Bland-Altman analysis, and two analyses were conducted: repeated measures ANOVA and Bland- Altman plots to analyze mean differences (MD) and 95% confidence intervals (CI) calculated as MD±1.96* standard deviation (SD).
Results
The measurement method affected IPD distance (F(3, 117)=15.74, p<0.01). The mobile apps resulted in significantly smaller distance IPD measurements than other methods. The PD ruler method yielded significantly larger distance IPD measurements than the pupillometer. For binocular near IPD, there was a significant difference among the methods (F(2, 78)=15.06, p<0.01). Pairwise comparison revealed that IPD ruler measurement was greater than with the other two methods (pupillometer and mobile application), while no difference was found between the pupillometer and mobile application. For consistency of measurement, correlation of two consecutive measurements was carried out, and it was found to be strongly correlated for all methods (r=0.9; p.<01).
Conclusion
Measurement by different tools showed difference of IPD measurement although induced prism due to discrepancy were within the allowed tolerance of less than 0.33 prism diopter (ISO 16034:2002) for all methods. Therefore, mobile App can be efficiently used for screening purposes for many people where limited services are available. However, caution should be exercised when mobile apps are used, such as in complex and for eyes which are misaligned.
Keywords: interpupillary distance, mobile application, non-contact, PD ruler
Introduction
Following the outbreak of the COVID-19 pandemic, non-contact healthcare procedures have been preferred with the aim of protecting patients and health care staff from the spread of infectious diseases.1 For example, telehealth services have been used by optometrists during the COVID-19 pandemic to address eye and vision concerns of patients remotely, with in-clinic visits offered after telehealth triaging.2 During COVID-19, mobile applications have become normalized as valuable aids for individuals and health professionals for the purposes of self-care, accessing information, managing crises, and to monitor health.3 Within the optometry and eyecare space, mobile applications exist for assessing vision, tracking eye health, providing information about eye conditions, and eye exercises.4 One study documented 475 Android mobile phone application; the majority were aimed for use by the general public (60.84%), followed by ophthalmology (15.15%) then optometry (7.78%).4 Optometrists are increasingly using mobile apps in clinic to conduct measurements of visual acuity, colour vision, vision therapy (eye exercise) and interpupillary (IPD) distances. Measuring interpupillary distances (IPD), the distance between the pupils of the eyes, is a routine and essential part of optometric practice. Precise IPD measurement is critical for accurate refraction so that the patient views through the trial lens optical center, and in the making of spectacles to suit an individual’s unique facial anatomy. In optical dispensing, misalignment between IPD and the optical center of the lenses will cause prismatic effects which if are of significant magnitude can lead to visual disturbances such as double vision (diplopia), distortion of images, and discomfort5,6 potentially impacting daily activities and visual function.7 In addition, IPD plays an important role in stereoacuity because it determines the convergence angle of the eyes and the corresponding retinal disparity between corresponding points in the visual field: Arshad et al, demonstrated that significant reduction of stereo-acuity (range of 20~100 min arc) was found with 1.49 prismatic effect due to misaligned IPD and the spectacles.8 In the context of virtual and augmented reality, Stanney et al,9 demonstrated that improper IPD settings in virtual reality (VR) devices can result in visual discomfort and nausea, called cybersickness. Consequently, precise measurement of IPD is important not only for conventional vision correction practice but also for modern immersive VR technologies. There are technical challenges to measure IPD which are heightened for patients who may not be able to carry out instructions, including patients who only provide limited cooperation, have developmental delays, cognitive issues, developmental delay, misaligned eyes or the inability to fixate and remain still during IPD measurement or have very different sizes of IPD compared to the examiner (eg children and infants).10 Involuntary eye movements such as nystagmus also interfere with IPD measurement leading to potential inaccuracies.11
Interpupillary distance (IPD) can be measured using various methods, each with its own advantages and disadvantages. IPD measurement traditionally requires varying levels of contact, such as the clinician leaning a millimeter ruler or hand on the patient’s face using the ruler technique to minimize shake and parallax error, or resting the nose pads and forehead rest on the patient’s nose and forehead (pupillometer) or the patient resting their chin on a chinrest and their forehead against a forehead rest (autorefractor). As these are contact procedures, the clinician should wash their hands in front of the patient and disinfect the equipment before use. While simple and cost-effective, manual measurement with a millimeter ruler is prone to inaccuracies due to human error such as parallax error in alignment and reading.12 A pupillometer, also known as a PD meter, is a specialized device designed specifically for measuring IPD. Pupillometers offer greater accuracy and precision compared to manual measurement with a ruler and are commonly used in optometry and spectacle fitting. Autorefractors are diagnostic instruments used to assess refractive errors, that may include built- in IPD measurement functionality, allowing for simultaneous measurement of refractive error and IPD. Mobile phone applications have the advantages of being non-contact and portable These apps typically guide users through the process of capturing images of their face and detecting the positions of the pupils to calculate IPD. Mobile apps potentially provide a low-cost and accessible solution for obtaining IPD measurements, which may eliminate the need for specialized equipment or professional assistance and could be a useful option for patients living in remote or underserved areas where access to eyecare services may be limited. Therefore, this study aims to compare measures using mobile applications with those of conventional methods.
Methods
Participants
Forty Participants for this study were recruited from the university population (mean age 25.65±3.72 years, 21 male and 19 female). Individuals with tropia and abnormal ocular alignment in the cover test were excluded from the study. The participants were informed about the purpose of the study and written consent was obtained from each participant before participation in the study. This study was conducted in accordance with the principles of the Declaration of Helsinki. The research protocol was approved by the Daegu Catholic University Institutional Review Board.
Instruments
Four different instruments were used for measuring interpupillary distance. (1) Pupillometer (TOPCON PD-5, Japan). This is a digital pupillometer designed to measure IPD using a corneal reflection system, aligning line markers with the corneal light reflex for precise measurements. The examiner only needs to use one eye to take measurement. It is a contact method as the device rests against the patient’s forehead and nose. In addition to IPD, it provides monocular measurements. It accommodates measurements for viewing distances ranging from 30 cm to infinity. This is the gold standard instrument. (2) A traditional PD ruler. This is traditionally made as a plastic ruler and is designed to lean against the forehead. The ruler markings are aligned with landmarks on the iris, typically the centre of the pupil (pupillary axis). The examiner must view using one eye at a time to avoid parallax error so is logistically difficult for the examiner. Variations of this method may use a pen torch aligned with the distant target to approximate the visual axis, but the placement of pen torch is difficult logistically for the examiner. It is a contact method as the device rests against the patient’s forehead and the examiner’s hand rests on the patient’s face. (3) Auto- refractor (KR-8100P, TOPCON, Japan). Autorefractors vary in design. The autorefractor used in this study is a kerato-refractometers that measures refraction, keratometry and automated IPD measurement. It is a contact method as the device rests against the patient’s forehead and the examiner’s hand rests on the patient’s face. (4) Mobile Application (Eye Measure 1.22). This App utilizes the front-facing camera to scan a face and calculate the IPD. It is a non-contact procedure. In addition to IPD, it provides segment height (SH) measurements.
The mobile application was selected using the following procedure: The search term “pupillary distance” was used in the South Korean Apple Store search bar, resulting in 15 applications. Out of 15, six were free to download. Out of the six, the App called “Eye Measure 1.22(Oct 6, 2021, Bonlook Inc)” provided the greatest number of measurements (near and distance IPD and segment height), was easy to use, and had the heights ratings and reviews of the apps in the Apple Store, so was selected for the study to measure IPD. The app works on iPhones, requiring iOS 12.0 or later and had a download size of 6.5MB.
Measurement Conditions
Four licensed optometrists with at least 3 years of practice experience in measuring PD conducted the IPD measurements. Each practitioner was randomly assigned to use one of the techniques and took measurements of all participants with that technique. In this study, IPD was assessed, which was a binocular PD. Monocular PD measurement was considered but was not compared as the autorefractor did not provide monocular PD measurements. IPD was assessed twice for each technique for each participant, and the averaged measurement for each technique was used for the analysis. The pupillometer was used with the setting of infinity fixation distance for distance IPD and 40cm fixation distance for near IPD. For the PD ruler measurement technique, each participant was asked to fixate a target 6m away for distance IPD and the near PD was measured when participants were fixating the optometrists’ nose at a fixation distance of 40cm. The autorefractor could only measure distance PD. The mobile application was used while iPhone was positioned approximately 40cm away and it provided distance IPD and near IPD measurements simultaneously.
The sample size was calculated to determine the minimum number of participants required to achieve statistical significance with adequate power. Assuming a medium effect size of 0.5, a significance level (α) of 0.05, and a power (1-β) of 80%, it was determined that 40 participants would be sufficient to detect differences in this study. For data analysis, the normality of the data was checked using the Shapiro–Wilk test. Significance level of p=0.05 was used to evaluate normality. Based on the results, data were found to be normally distributed, parametric tests were used for data analysis. After checking for normality, ANOVA was performed. Test-retest reliability was calculated using the Pearson Correlation Coefficient, to quantify the linear relationship between the measurements obtained from the devices where a correlation of more than 0.9 would indicate a very high correlation and less than 0.1 indicate a very low reliability. For agreement between PD measurements, pupillometer measurements were used as a gold standard measurement, as McMahon et al demonstrated that digital meters provide measurements that are closely aligned with the true anatomical PD, supporting their use as a reference standard in optometric practice.13 Bland-Altman plots were used with mean difference (MD) and 95% confidence intervals (CI) calculated as MD ± 1.96* standard deviation (SD).
Results
Forty university students participated for this study (mean 25.65±3.72, 21 male and 19 female). The means of the binocular and near IPD are presented in Table 1. Measurement method significantly affected distance IPD measurements: Pairwise comparisons revealed that the IPD measurements from the mobile application were statistically significantly shorter than the pupillometer, PD ruler and autorefractor measurements. In addition, the pupillometer IPD measurements were statistically significantly smaller than those with a PD ruler. However, there were no differences in IPD measurements between the Pupillometer and Autorefractor. For near IPD, there was a significant difference between methods. Pairwise comparison revealed that PD measurement with the PD ruler was greater than that with the pupillometer and the mobile application, while no difference was found between the pupillometer and mobile application.
Table 1.
Mean of Binocular Distance and Near PD Measured by Different Methods
| Type of PD | Methods to Measure PD | Mean ± SD (mm) | ANOVA, p value |
|---|---|---|---|
| Binocular Distance PD |
Pupillometer (A) | 64.2±3.5 | F(3, 117)=15.74, p<0.01A<B, C<A, B, D |
| PD ruler (B) | 64.8±3.6 | ||
| Mobile Application (C) | 63.6±3.5 | ||
| Autorefractor (D) | 64.4±3.8 | ||
| Binocular Near PD |
Pupillometer (A) | 61.1±3.6 | F(2, 78)=15.06, p<0.01A, C<B |
| PD ruler (B) | 62.1±3.5 | ||
| Mobile Application (C) | 61.5±3.4 |
Test-Retest Reliability
For consistency, the first and second PD measurements were assessed using each method. For all methods, the first and second PD measurements were strongly correlated (r=0.9, p.<01). The Pearson correlation coefficients are listed in Table 2. The correlation between distance PD and near PD for each device was r(38) = 0.97, p = < 0.05 (Pupillometer), r(38) = 0.99 p = < 0.05 (PD ruler), and r(38) = 0.99, p = < 0.05 (Mobile App).
Table 2.
Pearson’s Correlation Coefficient for 1st and 2nd Measurements for Each Method
| Type of PD | Methods to Measure PD | Pearson’s Correlation Coefficient, p value |
|---|---|---|
| Binocular Distance PD |
Pupillometer (A) | r(38)=0.98, p<0.01 |
| PD ruler (B) | r(38)=0.96, p<0.01 | |
| Mobile Application (C) | r(38)=0.96, p<0.01 | |
| Autorefractor (D) | r(38)=0.97, p<0.01 | |
| Binocular Near PD |
Pupillometer (A) | r(38)=0.98, p<0.01 |
| PD ruler (B) | r(38)=0.95, p<0.01 | |
| Mobile Application (C) | r(38)=0.96, p<0.01 |
Agreement Between Pupillometer and Other Methods
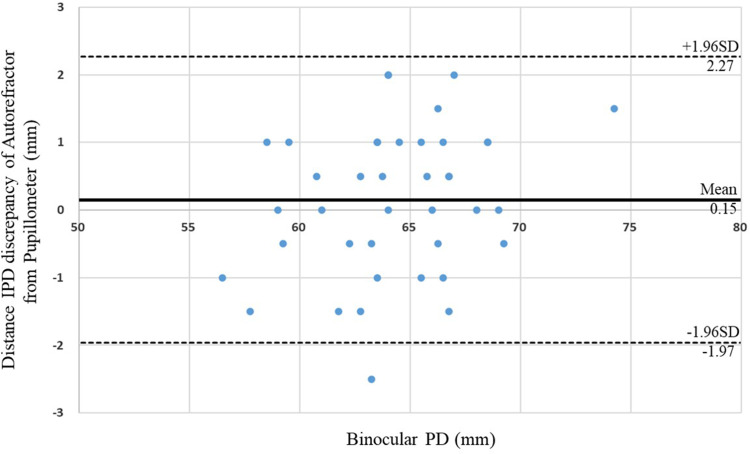
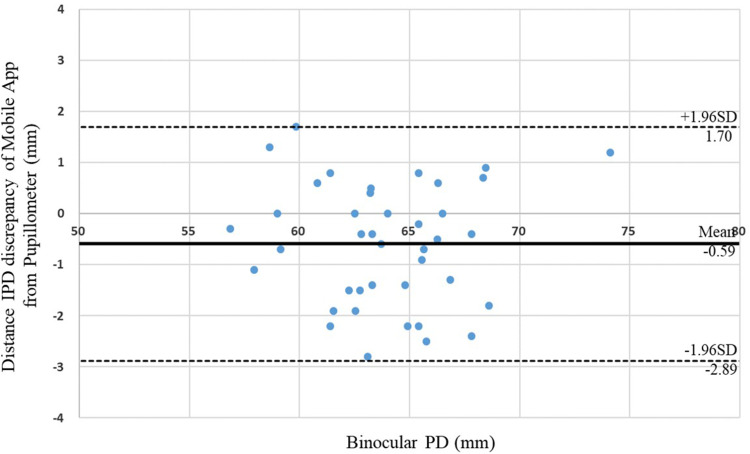
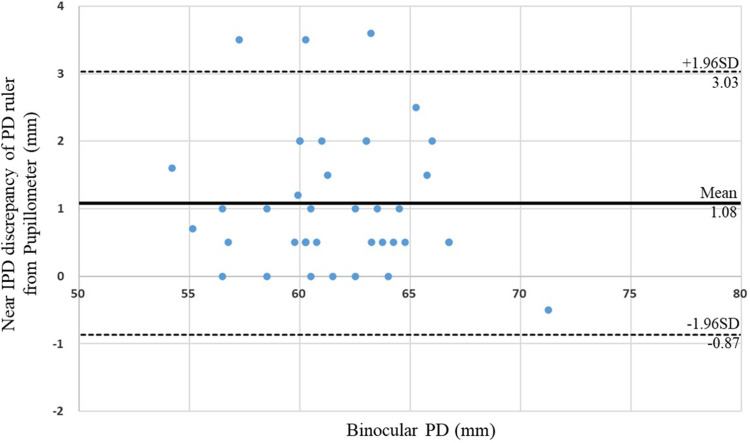
Considering Distance PD measurement using Pupillometer is a gold standard, the mean difference between Pupillometer and PD ruler was calculated to be 0.54 ± 0.74 mm (95% CI). The limits of agreement for ±1.96SD were −0.91 mm to 1.98 mm. The mean difference between the pupillometer and autorefractor was 0.15 ± 1.08 mm (95% CI). The limits of agreement for ±1.96SD were −1.97 mm to 2.27 mm (Figure 1). The mean difference between the Pupillometer and Mobile Application was −0.59 ± 1.17 mm (95% CI). The limits of agreement for ±1.96SD were −2.89 mm to 1.70 mm (Figure 2). For near PD measurement, the mean difference between Pupillometer and PD ruler was 1.08 ± 0.99 mm (95% CI). The limits of agreement for the ±1.96SD were −0.87 mm in 3.03 mm to −0.87 mm (Figure 3). The mean difference between the Pupillometer and Mobile Application was 0.52 ± 1.16 mm (95% CI). The limits of agreement for the ±1.96SD were −1.76 mm to 2.80 mm.
Figure 1.
Bland and Altman plots for difference of distance IPD measurement between Pupillometer and Autorefractor.
Figure 2.
Bland and Altman plots for difference of distance IPD measurement between Pupillometer and Mobile Application.
Figure 3.
Bland and Altman plots for difference of near IPD measurement between Pupillometer and PD ruler.
Discussion
This study indicated statistically significant differences in the distance and near IPD measurements among the methods. This study used the pupillometer as a reference measurement because many previous studies have validated the accuracy and reliability of digital PD meters in clinical settings.13,14 Therefore, the PD ruler IPD was an overestimate compared with the pupillometer. This is expected as compared to the pupillometer, the IPD with the PD ruler was overestimated in this study. One of the reasons for this finding is the Angle Kappa, which is the difference between the pupillary and visual axes. While the pupillometer measures the visual axis, which is slightly nasal from the centre of the pupil, the PD ruler without penlight torch measures from the pupil centre, which is the pupillary axis.15 PD ruler measurement also rely on solely human observation could lead human errors called parallax error and error could be from the different distance gap between the ruler and eye. When the line of sight is not perpendicular to the ruler, it can cause a shift in the perceived centre of the pupils, leading to overestimation. In addition, the variation in PD between the examiner and patient can be a factor for overestimation when the examiner’s PD is larger than the patient’s. In Gantz’s study, average distance IPD with manual PD was 60.69 while pupillometer measurement was 59.14, showing 1.55 mm difference and 0.78 mm overestimated measurements for near PD with PD ruler.14 Although Nehaapriya et al, showed different results that mean IPD measured with a PD ruler was 57.04 ± 3.46 mm, while the mean IPD measured with the autorefractometer was 60 ± 3.74 mm, their study also indicated no significant differences.16 In the present study, the distance IPD measurement with a mobile app 0.59 mm less on average than the pupillometer. Incorrect PD may cause eyestrain, fatigue, and blurred vision owing to unwanted prismatic effects, for lenses that do not have prescribed prism correction. The amount of prisms induced by an incorrect PD can be calculated using Prentices rule: For example, −3.00D lens with 0.6 mm incorrected PD can induce 0.18 prism diopters. According to ISO 16034:2002, the tolerance of the horizontally induced prism is a 0.33 prism diopter,17 therefore, the induced 0.18 prism diopters from 0.6 mm discrepancy (−3.00D) is still within an acceptable tolerance. Near PD measurement indicated that there was one data point outside the limit of agreement, but there were still much fewer outliers than other methods to measure IPD. Husna and Fitriani tested different mobile application called Galssify me, and indicated no difference between mobile App and Auto-refractometer with 0.2 mm of mean difference.12 Shin et al, used mobile App to assess pupillary light reflex and compared with measurement of manual penlight, but no significant difference found. They commented that mobile apps have several advantages for use in clinical settings, such as portability, objectivity, and records of medical evidence.18 This study could suggest that they can be easily used for mass vision screening purposes, such as in schools, workplaces, and community health initiatives, where large groups need to be screened efficiently. This study did not measure the speed of use for each device however, the mobile application stood out for speed and portability.19 The pupillometer and auto-refractor are reliable but require greater setup, professional handling20 while the PD ruler is simple but less precise and operator-dependent.21 This study has determined the agreement and discrepancy between a non-contact method of assessing IPD in comparison with the gold standard in people with normally aligned eyes. Considering that the difference is within tolerance for spectacle manufacture, the mobile application may be used to assess IPD in persons with normally aligned eyes in circumstances where it is necessary to prevent the spread of illness and efficient screening tool for remote area or underserved areas where access to professional eye care is limited. Alternatively, the results suggest calibration of the output of the mobile app for all measurements to fall within agreement, which suggests that further work by app developers with target populations will be able to address this issue. While mobile apps for measuring IPD offer convenience, caution needs to be exercised for complex prescriptions or detailed eye health assessments for diagnostic purposes. As a study limitation, this study evaluated the performance of one App out of fifteen available in this study. Consequently, the findings of this study are specific to the tested mobile application and may not fully generalize to other applications. In addition, this study did not measure monocular PD due to the lack of measurement of monocular PD in App; therefore, if there is any difference in monocular PD between the eyes, measurement of PD should not be used for clinical purposes.
Conclusion
This study investigated agreement in IPD measurements among different methods, including one mobile app. Measurements using different tools showed differences in IPD, although the majority of measurements were within spectacle manufacture tolerances. The mobile application measurements also showed consistent and precise results and with further research and work by the developers, a correction factor may be applied, ie add 0.6 mm to the specific mobile app measurement used in this study for distance IPD measurements.
Acknowledgment
This work was supported by research grants from Daegu Catholic University in 2022.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Kim S, Kim JA, Lee JY. International trend of non-contact healthcare and related changes due to COVID-19 pandemic. Yonsei Med J. 2022;63:S22–S33. doi: 10.3349/ymj.2022.63.S22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pidgeon JH, Bhardwaj MK, Titterington P, Latulippe K, Roh S, Ramsey DJ. Assessing optometric care delivered by telehealth during the COVID-19 public health emergency. Ther Adv Ophthalmol. 2022;14:25158414221123526. doi: 10.1177/25158414221123526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3..Galindo Neto NM, Sá GG, Barbosa LU, Pereira JD, Henriques AH, Barros LM. COVID-19 and digital technology: mobile applications available for download in smartphones. Texto Contexto-Enfermagem. 2020;29. doi: 10.1590/1980-265x-tce-2020-0150. [DOI] [Google Scholar]
- 4.Karthikeyan SK, Thangarajan R, Theruvedhi N, Srinivasan K. Android mobile applications in eye care. Oman J Ophthalmol. 2019;12(2):73–77. doi: 10.4103/ojo.OJO_226_2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Madrolu VSK, Male SR, Bhardwaj R, Theagarayan B. Influence of prismatic effect due to decentration of optical center in ophthalmic lens. Health Sci Rep. 2023;6(8):e1472. doi: 10.1002/hsr2.1472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holland BJ, Siderov J. Repeatability of measurements of inter- pupillary distance. Ophthalmic Physiol Opt. 1999;19(1):74–78. doi: 10.1046/j.1475-1313.1999.00400.x [DOI] [PubMed] [Google Scholar]
- 7.Moodley V, Kadwa F, Nxumalo B, Penciliah S, Ramkalam B, Zama A. Induced prismatic effects due to poorly fitting spectacle frames. Afr Vis Eye Health. 2011;70(4):168–174. doi: 10.4102/aveh.v70i4.115 [DOI] [Google Scholar]
- 8.Arshad A. Effect of Spectacle Centration on Stereoacuity. J Rawalpindi Med College. 2017;21(2):117–121. [Google Scholar]
- 9.Stanney K, Fidopiastis C, Foster L. Virtual reality is sexist: but it does not have to be. Front Robot AI. 2020;7:4. doi: 10.3389/frobt.2020.00004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Royal College of Ophthalmologists. Concise Practice Points, Managing Nystagmus in Childhood. 2023:1–13 [Google Scholar]
- 11.Self JE, Dunn MJ, Erichsen JT, et al. Management of nystagmus in children: a review of the literature and current practice in UK specialist services. Eye. 2020;34(9):1515–1534. doi: 10.1038/s41433-019-0741-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Husna HN, Fitriani N. Evaluation of pupillary distance (PD) measurement using smartphone-based pupillometer. J Phys Conf Ser. 2022;2243:012001. doi: 10.1088/1742-6596/2243/1/012001 [DOI] [Google Scholar]
- 13.McMahon TT, Irving EL, Lee C. Accuracy and repeatability of self-measurement of interpupillary distance. Optom Vis Sci. 2012;89(6):901–907. doi: 10.1097/OPX.0b013e318257f37b [DOI] [PubMed] [Google Scholar]
- 14.Gantz L, Shneor E, Doron R. Agreement and inter-session repeatability of manual and automatic interpupillary distance measurements. J Optom. 2021;14(4):299–314. doi: 10.1016/j.optom.2020.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moshirfar M, Hoggan RN, Muthappan V. Angle Kappa and its importance in refractive surgery. Oman J Ophthalmol. 2013;6(3):151–158. doi: 10.4103/0974-620X.122268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nehaapriya R, Bindu B, Sadiya I, Divya N, Panimalar V, Veeramani A. A study to compare the accuracy of interpupillary distance measured using interpupillary distance ruler with that of neidek autorefractometer. Int J Pharm Sci Res. 2020;11:2336–2339. doi: 10.26452/ijrps.v11iSPL4.4465 [DOI] [Google Scholar]
- 17.International Organization for Standardization. Ophthalmic optics – specifications for single–vision ready–to–wear near– vision spectacles. ISO 16034:2002(en); 2002. [Google Scholar]
- 18.Shin YD, Bae JH, Kwon EJ, Kim HT, Lee TS, Choi YJ. Assessment of pupillary light reflex using a smartphone application. Exp Ther Med. 2016;12(2):720–724. doi: 10.3892/etm.2016.3379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Han KD, Jaafar M, Stoakes IM, et al. Comparing the effectiveness of smartphone applications in the measurement of interpupillary distance. Cureus. 2023;15(7):e42744. doi: 10.7759/cureus.42744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mallen EA, Gilmartin B, Wolffsohn JS, Tsujimura S. Clinical evaluation of the Shin-Nippon SRW-5000 autorefractor in adults: an update. Ophthalmic Physiol Opt. 2015;35(6):622–627. doi: 10.1111/opo.12254 [DOI] [PubMed] [Google Scholar]
- 21.Wesemann W. Comparison of PD measuring devices Part 1. Optician. 2012;2012:22–28. [Google Scholar]