ABSTRACT
Introduction:
Type 2 Diabetes Mellitus (T2DM) patients often exhibit gaps in knowledge and improper practices regarding insulin injection techniques. This quasi-experimental study aimed to assess the effectiveness of tailored health education in bridging these gaps and improving insulin injection practices among T2DM patients.
Objectives:
The study aimed to evaluate baseline knowledge and practices related to insulin injection techniques among T2DM patients, implement a tailored health education intervention, and assess the impact of this intervention on knowledge and practices.
Methodology:
Participants included T2DM patients attending rural health centers. A structured questionnaire was utilized to assess baseline knowledge and practices. Tailored health education sessions were then conducted, incorporating video-based teaching, mock demonstrations, and handouts in the local language. Post-intervention assessments were performed using the same questionnaire. Data were analyzed using appropriate statistical methods.
Results:
At baseline, a significant knowledge gap and improper insulin injection practices were identified among participants. Following the tailored health education intervention, a substantial improvement in participants’ knowledge of insulin storage, handling, and administration was observed. The intervention also positively impacted insulin injection practices, emphasizing key areas such as handwashing, site cleansing, and needle disposal.
Conclusion:
This quasi-experimental study highlights the effectiveness of tailored health education in enhancing insulin injection practices among T2DM patients. The findings emphasize the potential for structured health education programs to address knowledge gaps, improve healthcare standards, and enhance the overall quality of life for individuals with T2DM. The study underscores the importance of individualized educational approaches to meet patient needs better.
Keywords: Healthcare standards, insulin injection practices, knowledge enhancement, quasi-experimental study, tailored health education, type 2 diabetes mellitus
Introduction
Diabetes mellitus (DM) is one of the leading causes of mortality and morbidity. Globally the incidence, prevalence, death, and disability-adjusted life-years (DALYs) associated with diabetes were 22.9 million, 476.0 million, 1.37 million, and 67.9 million in the year 2017.[1] In India, 74.2 million are affected with type 2 diabetes mellitus (T2DM).[2] Uncontrolled diabetes is associated with increased mortality from infections, cardiovascular disease, stroke, chronic kidney disease, chronic liver disease, and cancer.[3] Oral hypoglycemic agents are the first line of management of Type 2 DM. Insulin is indicated in patients with uncontrolled hyperglycaemia and in special circumstances like surgery, severe infection, and pregnancy.[4] In India, 3.2 million DM patients are using insulin for disease control.[5]
Proper insulin injection technique is necessary to ensure complete benefit of insulin use. Studies have highlighted the consequences of faulty practices in insulin storage, handling, and injection techniques among patients with Type 2 DM.[6,7] If vials are not stored at appropriate temperature, the potency and efficacy of insulin is affected.[8] Poor insulin injection technique leads to inadequate control of blood sugar level.[9,10] Pain associated with improper injection technique is an important barrier to adherence to insulin therapy.[11] There are several national and international guidelines on storage, mixing, and administration of insulin.[12,13] However, there exists a gap between recommendations and the actual practice of insulin injection technique.[14,15,16]
To prevent faulty insulin injection technique, patients have to be provided with adequate information about the insulin storage, site selection and rotation, dosing, administration, and safe disposal methods of sharps.[17,18] This can be done through educational interventions targeting commonly encountered errors.[19,20,21] Studies on effectiveness of health education on appropriate insulin injection techniques are limited especially in rural areas. Hence in this study, we developed a health education material on insulin injection technique and assessed its effectiveness in a rural setting. The objectives of this study are to evaluate the knowledge and practice of insulin injection techniques in patients with T2DM and to assess the effectiveness of health education programs on insulin injection techniques.
Subjects and Methods
This was a quasi-experimental study using a pre- and post-test design. The study was conducted among DM patients attending healthcare centers in the Karaikal district. Karaikal is one of the four districts in Puducherry’s union territory. Karaikal has 11 Primary Health Centres (PHC) and one Community Health Centre (CHC). Five PHCs and one CHC were chosen purposively. Type 2 DM patients aged 18 years and above, and who were on self-injected insulin for one month and above were included in the study. Patients using insulin pens and pregnant women were excluded. The duration of the study was 2 months (August 2022-October 2022). Considering the practice of correct insulin injection technique as 14%[19,22] and assuming 30% improvement in appropriate insulin injection technique after the health education program, with 80% power and 95% confidence interval, a minimum sample size of 84 individuals was needed for the study. The sample size was calculated using OpenEpi software version 3.01.
Study instrument
An interviewer-assisted structured Questionnaire was developed. It had two parts: the first part collected details on socio-demographic characteristics, duration of Type 2 DM, duration of insulin use, type of insulin used, number of insulin injections per day, and length of the needle. The second part of the questionnaire was based on the Forum for Injection Technique and Therapy Expert Recommendations (FITTER) India.[13] It was translated into Tamil and back-translated, pretested, and modified. The knowledge of insulin use, insulin storage, handling techniques, and complications associated with improper insulin injection techniques was evaluated using 12 close-ended questions. Each correct response was given a score of “1.” The overall knowledge score ranged between 0 and 12 and was graded as adequate (>9), moderately adequate (7–8), and inadequate (≤6) knowledge. The practice of insulin injection technique was evaluated using the 10-step checklist (FITTER).[13] A score of “1” was given if the patient correctly performed a critical step of the insulin injection technique. The overall practice score ranged between 0 and 10 and was graded as poor (≤5), fair (6–7.5), and good practice (>7.5).
Pre-test
Initially, the questionnaire was used to assess the study participant’s knowledge of insulin use and injection technique. Then they were asked to demonstrate the insulin injection technique on an injection model using dummy medication and an insulin syringe. The participant’s practice of insulin injection technique was observed by the study investigators and assessed using the checklist developed.
Health education program
A health education module was developed [Table 1]. Following the pre-test, the health education (Intervention) was provided by the investigators through PowerPoint presentation and demonstration. The intervention was delivered by the student researcher under the guidance of faculty members. The intervention was provided individually in a learner-to-instructor ratio of 1:1. The sessions were conducted on Non-Communicable Disease Clinic (NCD) days, which happen once a week at Primary Health Centres (PHC) and daily at Community Health Centre (CHC). The teaching/learning occurred in the outpatient department of the health centre after the patient had completed their consultation with the doctors. Each session lasted 30–40 minutes. Initially, it was planned to conduct the PowerPoint session using a projector. However, due to logistical reasons at primary health centres, the PowerPoint presentation was shown individually to the participants using a Tablet phone (iPad) and a laptop. This adaptation was convenient for the participants. There was no other modification during the study.
Table 1.
Health Education Module for Insulin Injection
| Teaching Learning Method | Sequence/steps | Duration (minutes) |
|---|---|---|
| Powerpoint presentation | Contents | 10-15 |
| Insulin | ||
| 1.Storage of insulin | ||
| 2.Pre-injection readiness | ||
| 3.Cleansing | ||
| 4.Resuspension of cloudy insulin | ||
| 5.Mixing insulins | ||
| 6.Injection–mealtime gap | ||
| Injection Technique | ||
| 1.Injection site & rotation. | ||
| 2.Single use of insulin syringe & needle | ||
| 3.Disadvantages of reuse of needles | ||
| 4.Missing a dose | ||
| 5.Adverse events of faulty technique (pain, lipohypertrophy, hypoglycemia) | ||
| 6.Injection device disposal | ||
| Video | Injection Technique using Seven golden rules | 5 |
| 1.The hands of the patient and the injection site should be clean | ||
| 2.6 mm syringe needles are recommended for all adults | ||
| 3.Recommended sites are the abdomen, upper thighs, upper arms, and upper buttocks. | ||
| 4.Persons using insulin should self-inspect their injection sites and screen for LH. | ||
| 5.Needles should not be reused. Insulin syringes and needles should not be shared | ||
| 6.Safe disposal of insulin needles and ancillaries should be ensured | ||
| 7.Injection sites should be inspected and palpated by health care professionals at least once a year, and more frequently if LH is detected | ||
| Demonstration-mannequin | Injection Technique based on FITTER guidelines | 10-15 |
| Teach-back | To check patient understanding of information | 5 |
| Handout | Patient education material in Tamil | - |
During the face-to-face demonstration, the investigators explained the procedure in the local language, using a dummy medication and insulin syringe on an injection model developed for this study. An insulin injection technique video was also played after the face-to-face demonstration. To check the understanding, patients were asked to teach back the procedure. Corrections were given and doubts were clarified. All participants were given a Tamil language hand-out on safe insulin injection technique and storage of insulin. No incentives or reimbursements were provided to the learners. All participants were informed about their visit after one month for post-test assessment. It was planned according to their routine monthly review visit at PHC.
Post-test
One month after this health education session, the patients were asked to visit the primary health care centre, and the participant’s knowledge of insulin use and injection technique was assessed again using the interviewer-assisted structured questionnaire. The patients were asked to re-demonstrate the insulin injection technique using dummy medication and insulin syringes on the subcutaneous injection model. The investigator observed and re-assessed the participant’s practice of insulin injection technique using the checklist
Statistical analysis
Data on continuous and categorical variables were summarized as mean ± standard deviation and proportions, respectively. Shapiro–Wilk test was used to test the normality of distribution. The data on overall knowledge and practice scores followed a skewed distribution, summarized as median and interquartile range. The difference in knowledge and practice before and after intervention was compared using the Wilcoxon signed-rank test. P-value <0.05 was considered as statistically significant. Statistical analysis was done by using IBM SPSS software version 25.
Ethical approval
Ethical clearance was obtained from the Institution Ethical Committee (IEC/OS/2022/254). A written informed consent was obtained from all the participants. Adequate privacy was provided. Confidentiality of the participants was ensured and maintained throughout the study.
Results
During the study period of two months, after fulfilling the inclusion and exclusion criteria a total of 90 patients were approached for participating in the study. Out of which 75 patients consented to participate in the study and written informed consent was obtained from them.
Patient characteristics
The mean (SD) age of the participants age was 48.2 (7.9) years, the duration of diabetes was 4.7 (3.1) years, and the duration of insulin use was 2.3 (1.8) years. The majority of the patients 65 (86.6%) were on premixed insulin and the rest were on short-acting insulin. About 80% of the patients were not aware of the needle length used by them for administering insulin, and 6 mm was the length of the needle used by the other patients. The other socio-demographic characteristics of the study population are described in Table 2.
Table 2.
Characteristic of participants using Insulin, n=75
| Characteristic | Frequency | Percentage |
|---|---|---|
| Age Category | ||
| 20–30 | 3 | 4.0 |
| 31–40 | 7 | 9.3 |
| 41–50 | 31 | 41.3 |
| 51–60 | 31 | 41.3 |
| 61–70 | 3 | 4.0 |
| Employment Status | ||
| Employed | 47 | 62.7 |
| Unemployed | 28 | 37.3 |
| Gender | ||
| Male | 44 | 58.7 |
| Female | 31 | 41.3 |
| Socioeconomic Status | ||
| Lower | 23 | 30.7 |
| Lower Middle | 38 | 50.7 |
| Middle | 14 | 18.7 |
| Upper Middle | 1 | 1.3 |
| Upper | 0 | 0.0 |
| Marital Status | ||
| Married | 62 | 82.7 |
| Widowed | 10 | 13.3 |
| Divorced | 3 | 4.0 |
| Education | ||
| Illiterate | 19 | 25.3 |
| Primary | 37 | 49.3 |
| Secondary | 14 | 18.7 |
| Higher Secondary | 4 | 5.3 |
| Degree | 1 | 1.3 |
| Source of Instruction of Insulin usage | ||
| Nurse | 44 | 58.7 |
| Doctor | 19 | 25.3 |
| Other patients | 7 | 9.3 |
| Pharmacists | 5 | 6.7 |
| Insulin Doses per day | ||
| 1 | 2 | 2.7 |
| 2 | 61 | 81.3 |
| 3 | 12 | 16.0 |
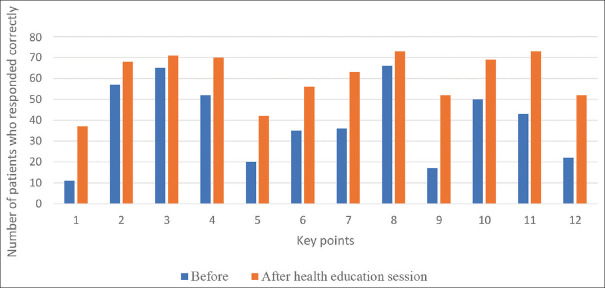
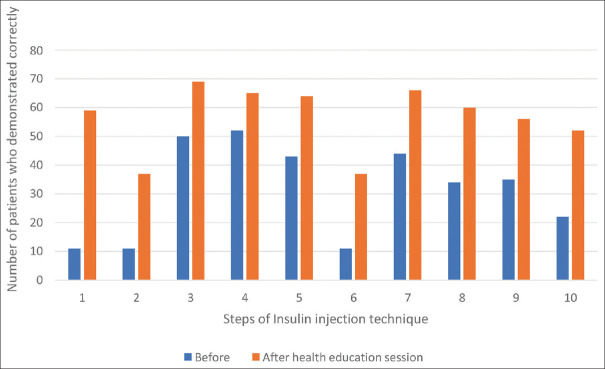
Figures 1 and 2 depict the assessment of knowledge of insulin use, handling storage, and practice of insulin injection technique among the study participants, respectively.
Figure 1.
Assessment of knowledge of insulin use, handling storage, and injection technique (n = 75). Key points assessing the awareness and importance of: 1. washing hands and cleaning the injection site before insulin injection, 2. ideal time interval between insulin injection and meal, 3. insulin injection sites, 4. rotation of the insulin injection sites, 5. reuse of insulin needle and its consequences, 6. holding the needle at site for some time after injecting insulin, 7. not massaging the site after insulin injection, 8. ideal place to store insulin vial at home, 9. ideal method of carrying an insulin vial during travel, 10. keeps the insulin vial at room temperature before injecting, 11. does not inject insulin in the lumps present near injection sites, 12. disposing of the used insulin needle
Figure 2.
Assessment of practice of insulin injection technique (n = 75). 1. Check the expiry date of the insulin vial and the type of insulin, 2. Wash hands, 3. Bring insulin to room temperature, 4. Selecting insulin dose and loading the syringe, 5. Select the site (upper arm, abdomen, and thigh). Inspects for scars, wounds, lumps, 6. Clean the injection site before injection and lift the skin fold, 7. Insert the needle at a 90-degree angle into the skin, 8. Administer insulin slowly, 9. Hold the needle under the skin for at least 10 seconds after injecting and release of skin fold, 10. Safely dispose of the needle and syringe
Pre-health education session
The overall median pre-knowledge score of the study participants about insulin use, storage, handling, and injection technique was 6 (3–10). About 41 (54.7%) of them had inadequate knowledge, 15 (20%) patients had moderately adequate knowledge, and the rest of them 19 (25.3%) had adequate knowledge.
The participant’s overall median pre-practice score of the insulin injection technique was 5 (2–6). About 54 (72%) of them followed poor practice, 17 (22.7%) and 4 (5.3%) had fair and good practice of insulin injection technique, respectively.
About 55 (73.3%) patients were reusing the needle, and the average reuse of a needle was six times. Injection site pain, swelling, and bruising were reported by 35 (46.7%) patients. Most of the patients 53 (70.6%) were not aware of the safe disposal of insulin needles and syringes. They were throwing it in the garbage and sewer. Only 22 (29.3%) of them collected the needle in a puncture-proof box with a lid at the top and syringes in a plastic bag, and handed over them to the nearby health centre for safe disposal.
Post-health education session
The overall median post-knowledge score of the study participants about insulin use, storage, handling, and injection technique was 10 (9–11). About 49 (65.3%) of them had adequate knowledge, 18 (24%) had moderately adequate knowledge, and the rest 8 (10.6%) of them had inadequate knowledge.
The overall median post-practice score of the study participants’ insulin injection technique was 8 (7–9). About 38 (50.7%) of them followed good practice, 31 (41.3%) and 6 (8%) had fair and poor practice of insulin injection technique, respectively.
A statistically significant (P < 0.001) improvement in knowledge and practice scores was noted after the health education session [Table 3].
Table 3.
Comparison of the total median score of knowledge and practice pre- and post-health education sessions of insulin injection technique
| Domain | Total median score (IQR) | *P | |
|---|---|---|---|
|
| |||
| Pre Session | Post Session | ||
| Knowledge | 6 (3–10) | 10 (9–11) | <0.001 |
| Practice | 5 (2–6) | 8 (7–9) | <0.001 |
*Wilcoxon signed rank test; IQR, Interquartile range
The knowledge and practice of insulin injection technique participants increased after the education session for the following key points: checking the expiry date of insulin vials 59 (78.7%), handwashing and site cleansing 37 (49.3%), awareness of the necessity to hold the needle for 6–10 seconds after injecting insulin 56 (74.7%), ideal method of carrying an insulin vial during travel 52 (69.3%), and safe disposal of insulin needle and syringes 52 (69.3%)
Discussion
This study aimed to assess the impact of tailored health education sessions on the knowledge and practice of insulin injection techniques among type 2 diabetic patients in rural health centres. The findings indicate that most patients’ baseline knowledge and practice of insulin injection techniques were inadequate. However, significant improvements were observed after the implementation of health education sessions.
Previous studies have identified errors and knowledge gaps related to insulin injection techniques, including lack of handwashing, improper site cleansing, needle reuse, improper insulin storage, and inappropriate needle disposal.[6,7,9,10] Consistent with these findings, our study also identified similar issues. However, the tailored health education sessions successfully addressed these gaps and emphasized the detrimental consequences of needle reuse. In addition, the intervention aimed to increase awareness of recommended practices, including checking for air bubbles in the syringe and ensuring adequate insulin absorption by holding the needle under the skin after injection.
The prevalence of needle reuse was high, corroborating findings from other national and international studies.[23,24,25] Educating patients about the risks associated with needle reuse and promoting proper disposal methods to prevent environmental hazards and needle stick injuries among sanitation workers is crucial. Our study provided education on safe disposal techniques, emphasizing using puncture-proof containers with lids.
The tailored health education intervention significantly improved participants’ knowledge of insulin storage, handling, and administration. Previous studies have used various teaching techniques, such as lectures, PowerPoint presentations, films, and take-home booklets.[21,26] In our research, we chose a customized strategy utilizing handouts in the local language, mock demonstrations, and video-based teaching techniques. This personalized method proved effective in improving patients’ insulin injection technique.
While our study primarily focused on assessing the knowledge and practice of insulin injection techniques, we acknowledge some limitations. We did not monitor HbA1c levels to determine the impact of the educational intervention on glycemic management. Moreover, our study had a short duration and a small sample size. Future research should include larger sample sizes and examine the long-term effects of interventions on glycemic control, medication adherence, and patient outcomes. We recommend conducting cost-effectiveness analyses of health education programs in diabetes self-management. Such research would provide valuable insights into these programs’ economic impact and benefits.
Conclusion
Patients with type 2 DM have a knowledge gap and exhibit improper practice of insulin injection techniques. Health education interventions significantly improve participants’ knowledge of insulin storage, handling, and administration. Therefore, healthcare providers can develop tailored and effective health education programs to address the specific needs of patients, leading to enhanced benefits of insulin therapy, improved healthcare standards, and an overall better quality of life for individuals with type 2 DM.
Financial support and sponsorship
Short-term student project 2022 under ICMR.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: An analysis from 1990 to 2025. Sci Rep. 2020;10:14790. doi: 10.1038/s41598-020-71908-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.International Diabetes Federation. IDF Diabetes Atlas. 10th ed. Brussels, Belgium: 2021. [[Last accessed on 2023 Dec 19]]. Available from: https://www.diabetesatlas.org . [Google Scholar]
- 3.Pradeepa R, Mohan V. Epidemiology of type 2 diabetes in India. Indian J Ophthalmol. 2021;69:2932–8. doi: 10.4103/ijo.IJO_1627_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Netere AK, Ashete E, Gebreyohannes EA, Belachew SA. Evaluations of knowledge, skills and practices of insulin storage and injection handling techniques of diabetic patients in Ethiopian primary hospitals. BMC Public Health. 2020;20:1537. doi: 10.1186/s12889-020-09622-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mohan V, Shah SN, Joshi SR, Seshiah V, Sahay BK, Banerjee S, et al. Current status of management, control, complications and psychosocial aspects of patients with diabetes in India: Results from the DiabCare India 2011 Study. Indian J Endocrinol Metab. 2014;18:370–8. doi: 10.4103/2230-8210.129715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patil M, Sahoo J, Kamalanathan S, Selviambigapathy J, Balachandran K, Kumar R, et al. Assessment of insulin injection techniques among diabetes patients in a tertiary care centre. Diabetes Metab Syndr. 2017;11:S53–6. doi: 10.1016/j.dsx.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 7.Poudel RS, Shrestha S, Piryani RM, Basyal B, Kaucha K, Adhikari S. Assessment of insulin injection practice among diabetes patients in a tertiary healthcare centre in Nepal: A preliminary study. J Diabetes Res. 2017;2017:8648316. doi: 10.1155/2017/8648316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vimalavathini R, Gitanjali B. Effect of temperature on the potency and pharmacological action of insulin. Indian J Med Res. 2009;130:166–9. [PubMed] [Google Scholar]
- 9.Nasir BB, Buseir MS, Muhammed OS. Knowledge, attitude and practice towards insulin self-administration and associated factors among diabetic patients at Zewditu Memorial Hospital, Ethiopia. Lebina L, editor. PLoS One. 2021;16:e0246741. doi: 10.1371/journal.pone.0246741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Choudhary A, Chouhan J, Gulati S, Vishandasani JK. Practice of insulin injection techniques among persons with diabetes in central India: An observational survey. Int J Adv Med. 2021;8:648–52. [Google Scholar]
- 11.Grassi G, Scuntero P, Trepiccioni R, Marubbi F, Strauss K. Optimizing insulin injection technique and its effect on blood glucose control. J Clin Transl Endocrinol. 2014;1:145–50. doi: 10.1016/j.jcte.2014.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bahendeka S, Kaushik R, Swai AB, Otieno F, Bajaj S, Kalra S, et al. EADSG Guidelines: Insulin storage and optimisation of injection technique in diabetes management. Diabetes Ther. 2019;10:341–66. doi: 10.1007/s13300-019-0574-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tandon N, Kalra S, Balhara YS, Baruah M, Chadha M, Chandalia H, et al. Forum for injection technique and therapy expert recommendations, India: The Indian recommendations for best practice in insulin injection technique, 2017. Indian J Endocr Metab. 2017;21:600–17. doi: 10.4103/ijem.IJEM_97_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strauss K, Gols HD, Hannet I, Partanen TM, Frid A. A pan-European epidemiologic study of insulin injection technique in patients with diabetes. Pract Diabetes Int. 2002;19:71–6. [Google Scholar]
- 15.Berard L, Cameron B. Injection technique practices in a population of Canadians with diabetes: Results from a recent patient/diabetes educator survey. Can J Diabetes. 2015;39:146–51. doi: 10.1016/j.jcjd.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 16.De Coninck C, Frid A, Gaspar R, Hicks D, Hirsch L, Kreugel G, et al. Results and analysis of the 2008-2009 insulin injection technique questionnaire survey. J Diabetes. 2010;2:168–79. doi: 10.1111/j.1753-0407.2010.00077.x. [DOI] [PubMed] [Google Scholar]
- 17.Majumdar A, Sahoo J, Roy G, Kamalanathan S. Improper sharp disposal practices among diabetes patients in home care settings: Need for concern? Indian J Endocrinol Metab. 2015;19:420–5. doi: 10.4103/2230-8210.152792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang MC, Hung CH, Huang YW, Yang SC. Predictors of Self-Efficacy in Administering Insulin Injection. Clin Nurs Res. 2021;30:120–6. doi: 10.1177/1054773819858484. [DOI] [PubMed] [Google Scholar]
- 19.Ahmad S, Osman MT, Jaffar A, Rashid MRA, Hassan MR, Supian ZA. Education of correct insulin injection technique amongst diabetic patients: Outcome study from Malaysia. Int J Med Res Health Sci. 2016;5:198–205. [Google Scholar]
- 20.Gorska-Ciebiada M, Masierek M, Ciebiada M. Improved insulin injection technique, treatment satisfaction and glycemic control: Results from a large cohort education study. J Clin Transl Endocrinol. 2020;19:100217. doi: 10.1016/j.jcte.2020.100217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nakatani Y, Matsumura M, Monden T, Aso Y, Nakamoto T. Improvement of glycemic control by re-education in insulin injection technique in patients with diabetes mellitus. Adv Ther. 2013;30:897–906. doi: 10.1007/s12325-013-0066-8. [DOI] [PubMed] [Google Scholar]
- 22.Chu LT, Nguyen TQ, Pham PTT, Thai TT. The Effectiveness of health education in improving knowledge about hypoglycemia and insulin pen use among outpatients with type 2 diabetes mellitus at a primary care hospital in Vietnam. J Diabetes Res. 2021;2021:9921376. doi: 10.1155/2021/9921376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kamrul-Hasan A, Paul AK, Amin MN, Gaffar MAJ, Asaduzzaman M, Saifuddin M, et al. Insulin Injection Practice and Injection Complications –Results from the Bangladesh Insulin Injection Technique Survey. Eur Endocrinol. 2020;16:41–8. doi: 10.17925/EE.2020.16.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bari B, Corbeil MA, Farooqui H, Menzies S, Pflug B, Smith BK, et al. Insulin Injection practices in a population of Canadians with diabetes: An observational study. Diabetes Ther. 2020;11:2595–609. doi: 10.1007/s13300-020-00913-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ji J, Lou Q. Insulin pen injection technique survey in patients with type 2 diabetes in mainland China in 2010. Curr Med Res Opin. 2014;30:1087–93. doi: 10.1185/03007995.2014.895711. [DOI] [PubMed] [Google Scholar]
- 26.Selvadurai S, Cheah KY, Ching MW, Kamaruddin H, Lee XY, Ngajidin RM, et al. Impact of pharmacist insulin injection re-education on glycemic control among type II diabetic patients in primary health clinics. Saudi Pharm J. 2021;29:670–6. doi: 10.1016/j.jsps.2021.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]