Abstract
Background
Chronic pain poses a significant public health challenge. We present the global and regional data on Prevalence, Incidence and Years Lived with Disability (YLDs) for Chronic pain from the Global burden of disease (GBD) study 2019 data and analyze their associations with Socio-demographic index (SDI), age, and gender, and the future trends from 2020 to 2035.
Methods
Regional trends in the burden of chronic pain and its association with age, gender, and SDI were assessed from 1990 to 2019. Joinpoint analysis was employed to describe trends in chronic pain burden across different SDI regions. Additionally, the Bayesian Age-Period-Cohort model (BAPC) was used for predicting future trends. Age-standardized rates (ASRs) of prevalence, incidence, and YLDs were employed to quantify the burden of chronic pain.
Results
Between 1990 and 2019, a significant increase was observed in global prevalence and YLDs rates of chronic pain. Higher rates were found among females, whereas a faster rise was noted among males. Notably, Low Back Pain (LBP) and Migraine accounted for predominant YLDs globally, particularly among those aged 75 and above. A notable prevalence of Tension-type Headache (TTH) was observed among younger populations. Furthermore, ASRs for chronic pain were highest in high-SDI regions. Projections suggest an increase in headache ASRs globally for both genders from 2020 to 2035.
Conclusion
From 1990 to 2019, the global burden of chronic pain increased significantly, with projections indicating a continued rise in headache burden over the next 15 years, underscoring the need for heightened attention to these issues.
Keywords: Bayesian age-period-cohort model, chronic pain, global burden of diseases study, headache, incidence, musculoskeletal disorders, prevalence, socio-demographic index, years lived with disability
Introduction
Chronic pain is defined as pain lasting over 3 months, which can significantly disrupt daily activities, including work, social interactions, and self-care. Chronic pain can be caused by a wide variety of reasons, such as cancer, arthritis, and rheumatic diseases. 1 It stands as the primary motive for patient visits to healthcare facilities. It can also contribute to depression, anxiety, and sleep disturbances, further exacerbating the experience of pain. 2 In 2019, the International Academy for the Study of Pain (IASP) and the World Health Organization (WHO) collaborated to revise the assessment labeling and classification diagnostic outline for Chronic pain. 3 IASP recommends that Chronic pain not be viewed as a symptom, but rather treated as a disease. 4 Despite advancements in medical care and the widespread use of various opioids in clinical practice, a significant societal burden persists in association with Chronic pain.
The inadequate scientific comprehension of the epidemiology of Chronic pain has resulted in a significant disparity in the allocation of healthcare resources, such as the dearth of statistical data and epidemiological investigations into Chronic pain. 5 Consequently, there is an imperative necessity to devise pragmatic policies aimed at addressing the epidemiology of diverse Chronic pain etiologies, rationalizing the distribution of healthcare resources, and averting the wasting of already scarce resources, all to alleviate the burden of disease associated with Chronic pain.
GBD 2019 provides a valuable resource for epidemiologic studies by reporting the burden of disease for three indicators covering 204 countries and territories. Therefore, based on data from GBD 2019 and improved methodology, we analyzed global, regional, and national trends in the Prevalence of Chronic pain and its subtypes from 1990 to 2019, to reveal the effects of the SDI, geographic location, gender, and age on the Incidence, Prevalence, and YLDs rate of Chronic pain and predict its trends in the next 15 years, to provide new insights for the development of Chronic pain prevention plans in different countries. 6
Methods
Study overview
Global Burden of Disease data for Chronic pain was derived from GBD 2019, which provides a comprehensive assessment of the burden of disease for 369 diseases and 87 risk factors from 204 countries and territories based on the most recent epidemiologic data available. All countries and territories were categorized into 21 regions based on epidemiologic similarities and geographic proximity. Additionally, the SDI was used to further group them into five categories: low SDI, low-middle SDI, middle SDI, high-middle SDI, and high SDI. The criteria for defining these five SDI categories are detailed in Table S1. The SDI is a composite indicator that is estimated based on lagged distributional income per capita, the total fertility rate for females under 25, and the average years of schooling for adults aged 15 and over. 7 The subtypes of chronic pain are classified according to the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) by the World Health Organization (WHO). These subtypes include headache disorders such as Migraine and Tension-type Headache (TTH), as well as musculoskeletal disorders like Gout, Low Back Pain (LBP), Neck Pain, Osteoarthritis, Rheumatoid Arthritis (RA), and other musculoskeletal disorders. The ICD codes for these disorders can be found in Table S2.
Data
Both crude and age-standardized prevalence, incidence, and YLD rates for headache disorders, including Migraine and TTH, as well as for musculoskeletal disorders such as Gout, LBP, Neck Pain, Osteoarthritis, RA, and other musculoskeletal disorders were extracted. For each of these estimates and rates, we also obtained their corresponding 95% uncertainty intervals (UI). The Global Burden of Disease (GBD) study collects data from a wide array of sources to provide comprehensive estimates on health loss due to diseases, injuries, and risk factors globally. To improve the robustness of estimates, GBD draws from over 90,000 unique data sources, including some less conventional ones like verbal autopsy, where interviewers gather information from the relatives of deceased individuals to determine cause of death. This methodology ensures data collection in regions lacking consistent health records. Each dataset is thoroughly vetted by specialists, and results are compiled with the collaboration of over 12,000 researchers globally. More details can be found in the Global Health Data Exchange (GHDx) (https://ghdx.healthdata.org/).
Statistical analyses
In the GBD study, uncertainty was assessed for all estimates to account for factors such as primary data source variability, modeling uncertainty, data errors, and data manipulation. Consequently, uncertainty was quantified and statistically represented at each location, reflected in the 95% UIs accompanying each estimate. The UIs were derived from 1000 plotted levels of the model’s posterior distribution, with the 95% UIs defined as the 2.5th and 97.5th percentiles of that distribution.
Temporal trends in the global burden of disease for Chronic pain were estimated with a joinpoint regression model using a joinpoint regression analysis to identify points of significant trend change and divide the overall trend into subsections based on these observed joinpoints by calculating the annual percent change (APC), average annual percent change (AAPC) and 95% confidence intervals (CI) to further assess the epidemiologic trends in each subsegment. Additionally, AAPC, as a summary measure of trend for a predefined fixed interval (1990–2019), was also calculated as a weighted average of APC for the spanwise width of the segmented intervals. The overall asymptotic significance level was maintained by Bonferroni correction using a Monte Carlo permutation method that randomized the 4499 datasets. 8 If both the APC/AAPC estimate and its lower limit of the 95% CI were >0, an increasing trend was identified over time. Conversely, if both the APC/AAPC estimate and its 95% CI upper bound were <0, a decreasing trend was identified over a period of time. Otherwise, the trend is considered unknown.
The projections of Incidence and Prevalence for 2020–2035 were carried out based on the BAPC method. The Bayesian APC model is based on the INLA (Integrated Nested Laplace Approximations) method. 9 The APC model estimates the age of the individual, the birth cohort, and the time of the event: , with an intercept of µ, the age, period, and cohort effects α i , β j and γk, i (1 ≤ i ≤ i) denotes the age cohort at the time point j (1 ≤ j ≤ j), and the cohort index k depends on the age and period indices as well as the age group and period interval widths: k = j + M (i − i). m denotes the ratio of the width of the age group to the period interval, for example, for the age group of 5 years old and for annual data, M is 5, which is the one used in this study. R package BAPC (V.0.0.36) and INLA (V.23.05.30) were used to implement a BAPC model integrated nested Laplace approximations, and R package easyGBDR (V.1.0.0.1) was used to clean and sort our data. All analyses and visualizations were performed using R software (V.4.2.3).
Results
Prevalence of headache and musculoskeletal disorders
In 2019, the estimated global prevalence of headache disorders reached 2.60 billion cases (95% UI: 2.40 to 2.80 billion), with an age-standardized prevalence rate (ASPR) of 32,717 per 100,000 people (Table 1). As presented in Table S3, females demonstrated a higher ASPR of 35,671 cases (95% UI: 32,965 to 38,392) per 100,000 people. Specifically, TTH was identified as the predominant cause of chronic pain, with an ASPR of 25,113 cases (95% UI: 22,021 to 28,316) per 100,000 people (Figure S1A, Table 1). Geographically, Western Europe exhibited the highest ASPR for headache disorders, while Eastern Sub-Saharan Africa recorded the lowest (Table S3).
Table 1.
Numbers and ASRs of YLDs, incidence and prevalence of subtypes of chronic pain disorders worldwide in 2019 and their 95% uncertainty intervals.
| Causes | Prevalence | Incidence | YLDs | |||
|---|---|---|---|---|---|---|
| Number, 2019 | ASPR, 2019 | Number, 2019 | ASIR, 2019 | Number, 2019 | ASYR, 2019 | |
| Total | 4117862020 (3829669103∼4406246338) | 51124.27 (47561.00∼54768.60) | 1116588507 (1006970401∼1231328140) | 14055.25 (12650.84∼15492.97) | 193901475 (115915958∼295214425) | 2372.61 (1407.81∼3622.20) |
| Musculoskeletal disorders | 2602898103 (2396738293∼2805119609) | 32716.78 (30148.43∼35335.04) | 793839082 (714299832∼877018808) | 10110.72 (9070.72∼11167.13) | 46619354 (9772903∼100161725) | 581.76 (119.58∼1255.58) |
| Headache disorders | 1514963916 (1432930809∼1601126728) | 18407.49 (17412.57∼19433.56) | 322749424 (292670568∼354309332) | 3944.53 (3580.13∼4325.84) | 147282120 (106143055∼195052699) | 1790.85 (1288.24∼2366.62) |
| Migraine | 1128087260 (979598830∼1298138078) | 14107.26 (12270.27∼16239.02) | 87648968 (76635688∼98654601) | 1142.54 (995.90∼1289.44) | 42077665 (6418383∼95645211) | 525.54 (78.79∼1193.99) |
| Tension-type headache | 1995172548 (1751946845∼2242204885) | 25113.49 (22020.81∼28316.24) | 706190113 (626723554∼788575302) | 8968.18 (7931.86∼9990.52) | 4541688 (1395545∼14981335) | 56.21 (17.00∼188.51) |
| Goat | 53871846 (43383204∼66342327) | 652.24 (528.56∼798.60) | 9222886 (7419132∼11521165) | 111.33 (90.01∼139.20) | 1673973 (1068061∼2393469) | 20.23 (12.91∼28.88) |
| LBP | 568444531 (505000665∼640597791) | 6972.55 (6190.47∼7860.48) | 223455640 (197710057∼252992458) | 2748.90 (2425.77∼3106.89) | 63685119 (44999198∼85192922) | 780.15 (549.34∼1046.05) |
| Neck pain | 222718452 (179236776∼281066237) | 2696.52 (2177.01∼3375.19) | 47528964 (37448843∼59936489) | 579.09 (457.90∼729.64) | 22081323 (14508244∼31726932) | 267.35 (175.53∼383.54) |
| Osteoarthritis | 527811871 (478667548∼584793490) | 6348.25 (5776.34∼7023.04) | 41467541 (36875471∼46438408) | 492.21 (438.66∼551.50) | 18948965 (9571297∼37659659) | 227.97 (115.31∼452.70) |
| Rheumatoid arthritis | 18583481 (16955383∼20433859) | 224.25 (204.94∼245.99) | 1074390 (975501∼1179332) | 13.00 (11.83∼14.27) | 2433039 (1681353∼3276916) | 29.35 (20.29∼39.51) |
| Other musculoskeletal disorders | 452588037 (390256734∼525237802) | 5479.36 (4725.98∼6353.28) | 0 (0∼0) | 0.00 (0.00∼0.00) | 38459699 (26253489∼53553785) | 465.81 (317.92∼647.83) |
Abbreviations: 95% uncertainty intervals of all regions and countries are reported in the Supplemental Table S3; ASPR: age-standardized prevalence rate (per 100,000 people); ASIR: age-standardized incidence rate (per 100,000 people); ASYR: age-standardized YLDs rate (per 100,000 people); YLDs: years of life lived with disability.
In 2019, the global prevalence of musculoskeletal disorders was estimated at 1.52 billion cases (95% UI: 1.43 to 1.60 billion), with an ASPR of 18,407 per 100,000 people. Similar to headache disorders, females exhibited a higher ASPR of 20,601 (95% UI: 19,535 to 21,706) per 100,000 people, while males showed a rising trend with an annual percentage change (AAPC) of 0.06 (95% CI: 0.05 to 0.06) over the past 30 years. LBP was identified as the primary musculoskeletal disorder, with an ASPR of 6973 cases (95% UI: 6190 to 7860) per 100,000 people. Geographically, the highest ASPRs for musculoskeletal disorders were observed in High-income North America at 29,665 (95% UI: 28,629 to 30,713) per 100,000 people (Table S3). A notable increase in the ASPR of osteoarthritis was observed starting from age 35 onwards. This led to osteoarthritis becoming the primary cause of chronic pain in the population aged 75 and above for both sexes in 2019 (Figure S1A).
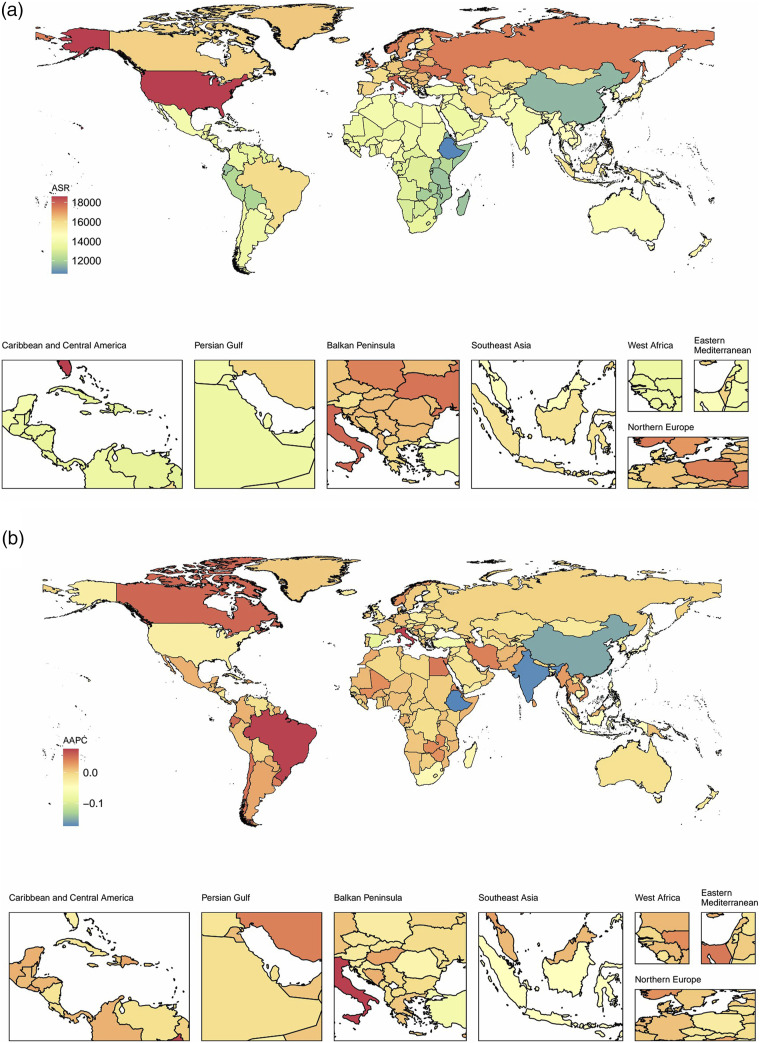
In terms of gender-specific trends, the ASPR for headache disorders in females exhibited a decrease with an AAPC of −0.02 (95% CI: −0.02 to −0.01), while in males, there was an observable upward trend with an AAPC of 0.03 (95% CI: 0.02 to 0.03) from 1990 to 2019. It is noteworthy that the regional ASPRs for all Chronic pain subtypes showed minimal changes between 1990 and 2019, with TTH emerging as the predominant cause of Chronic pain across all regions (Figure S1B). Regional trends of ASPR for chronic pain are illustrated in Figure S2. Most countries showed an increase in ASPR for chronic pain over the past three decades. Specifically, the ASPR for headache in East Asia exhibited the most substantial escalation with an AAPC of 0.11 (95% CI: 0.15 to 0.18). In contrast, the ASPR for musculoskeletal disorders in High-income North America observed a significant rise with an AAPC of 0.24 (95% CI: 0.20 to 0.27) (Table S3).
Incidence of headache and musculoskeletal disorders
In 2019, the estimated number of new headache cases worldwide was nearly 794 million (95% UI: 714 to 877 million). The global age-standardized incidence rate (ASIR) stood at 10,111 cases (95% UI: 9071 to 11,167) per 100,000 people, with a higher incidence rate observed in females (Table 1 and Table S3).
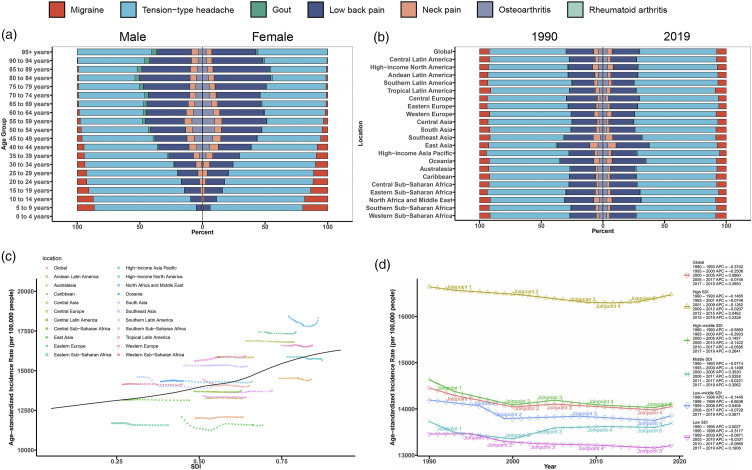
In 2019, America and Europe exhibited the highest ASIR of headaches. The TTH accounted for a significant ASIR of 8968 cases (95% UI: 7931 to 9991) per 100,000 people across all age groups. Notably, a higher incidence was observed among children and young adolescents. From 1990 to 2019, TTH emerged as the leading cause of chronic pain incidence worldwide, followed by LBP with an ASIR of 2749 cases (95% UI: 2426 to 3107) per 100,000 people, predominantly among those aged 55 and above (Figures 1 and 2, Table 1).
Figure 1.
The percentages in ASIRs of seven conditions in different age groups, regions for males and females in 1990 and 2019, the trends in ASIRs of chronic pain and SDI in 21 regions for both sexes in 2019, and the trends in ASIRs of chronic pain in five different SDI regions in 2019. (a): The percentage in ASIRs of seven conditions in 20 age groups for males and females in 2019; (b): the percentage in ASIRs of seven conditions in 21 regions for both sexes in 1990 and 2019; (c): trends in ASIRs of Chronic pain and SDI in 21 regions for both sexes in 2019; (d): trends in ASIRs of Chronic pain in five SDI group regions for both sexes in 2019 and its APC. Abbreviation: ASIR: age-standardized incidence rate; APC: annual percent change; SDI: socio-demographic index.
Figure 2.
National distribution of chronic pain ASIRs and AAPC for both genders in 2019 in 204 countries. (a): Distribution of ASIR of chronic pain; (b): distribution of AAPC of ASIR of chronic pain. Abbreviation: ASIR: age-standardized incidence rate; AAPC: average annual percent change.
In 2019, the estimated number of new cases of musculoskeletal disorders was 323 million (95% UI: 293 to 354 million), resulting in an ASIR of 3945 (95% UI: 3580 to 4326) per 100,000 people (Table 1). Limited disparity in ASIR was observed in Musculoskeletal disorders in terms of males and females. In terms of temporal trends from 1990 to 2019, the ASIRs for headache and musculoskeletal disorders showed a modest decrease, with AAPC of −0.01 (95% CI: −0.01 to 0.00) and −0.32 (95% CI: −0.34 to −0.31) respectively. This decrease was more pronounced among females, with AAPCs of −0.03 (95% CI: −0.04 to −0.03) for headache and −0.32 (95% CI: −0.34 to −0.30) for musculoskeletal disorders. However, the ASIR for headache in males showed a slight increase with an AAPC of 0.02 (95% CI: 0.02 to 0.03) (Table S3).
Over the past 30 years, most regional ASIRs for chronic pain have shown a decline. However, Latin America has witnessed a significant increase in both headache and musculoskeletal disorders. This increase is particularly pronounced in Tropical Latin America, with an AAPC of 0.08 (95% CI: 0.08 to 0.09) for headache and 0.05 (95% CI: 0.04 to 0.05) for musculoskeletal disorders, as presented in Table S3. The decline in the ASIR of chronic pain reflects the effectiveness of prevention efforts by relevant departments. Nonetheless, further measures are essential for the future. These should include targeted prevention strategies for TTH in specific regions such as Latin America, as well as measures to protect high-risk groups for musculoskeletal disorders, notably males and the 80 to 89 age cohort.
YLDs of headache and musculoskeletal disorders
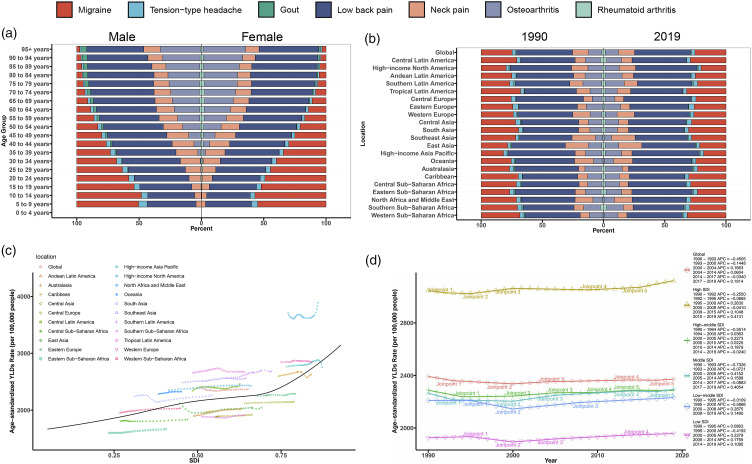
As indicated in Table 1 and Table S3, headaches accounted for 46.6 million (95% UI, 9.66 to 100 million) YLDs, with an age-standardized YLDs rate (ASYR) of 582 (120 to 1256) per 100,000 people globally in 2019. A higher ASYR was observed in females at 725 per 100,000 people, with a 95% UI ranging from 139 to 1588. Regionally, South Asia bore the largest burden of headaches with 10.7 million YLDs (1.77 to 23.5 million) in 2019. However, in terms of ASYR, Western Europe exhibited the highest rates at 749 (143 to 1638) per 100,000 people. As for subtypes of headaches, migraine caused predominate ASYR (52,6 79 to 1194) per 100,000 people globally, especially in 0 to 24 age groups in 2019 (Figure 3, Table 1).
Figure 3.
The percentages in ASYRs of seven conditions in different age groups, regions for males and females in 1990 and 2019, the trends in ASYRs of Chronic pain and SDI in 21 regions for both sexes in 2019, and the trends in ASYRs of chronic pain in five different SDI regions in 2019. (a): The percentage in ASYRs of seven conditions in 20 age groups for males and females in 2019; (b): the percentage in ASYRs of seven conditions in 21 regions for both sexes in 1990 and 2019; (c): trends in ASYRs of chronic pain and SDI in 21 regions for both sexes in 2019; (d): trends in ASYRs of chronic pain in five SDI group regions for both sexes in 2019 and its APC. Abbreviation: ASYR: age-standardized YLDs rate; APC: annual percent change; SDI: socio-demographic index.
Notably, musculoskeletal disorders accounted for a greater number of YLDs at 147 million (95% UI: 106 to 195 million) and a higher ASYR at 1791 (95% UI: 1288 to 2367) per 100,000 people in 2019. Similar to headache disorders, females exhibited a higher ASYR for musculoskeletal disorders compared to males, with an ASYR of 1505 (95% UI: 1078 to 1995) per 100,000 people. In 2019, High-income North America recorded the highest ASYR at 3212 (95% UI: 2328 to 4214), followed by High-income Asia Pacific with an ASYR of 2282 (95% UI: 1615 to 3046) per 100,000 people. In terms of different age groups, LBP presented the greatest threat, with an ASYR of 780 (95% UI: 549 to 1046) per 100,000 people, particularly among those aged 75 and above. Osteoarthritis also contributed significantly to disability, with an ASYR of 228 (95% UI: 115 to 453) per 100,000 people (Figure 3, Tables 1 and S3)
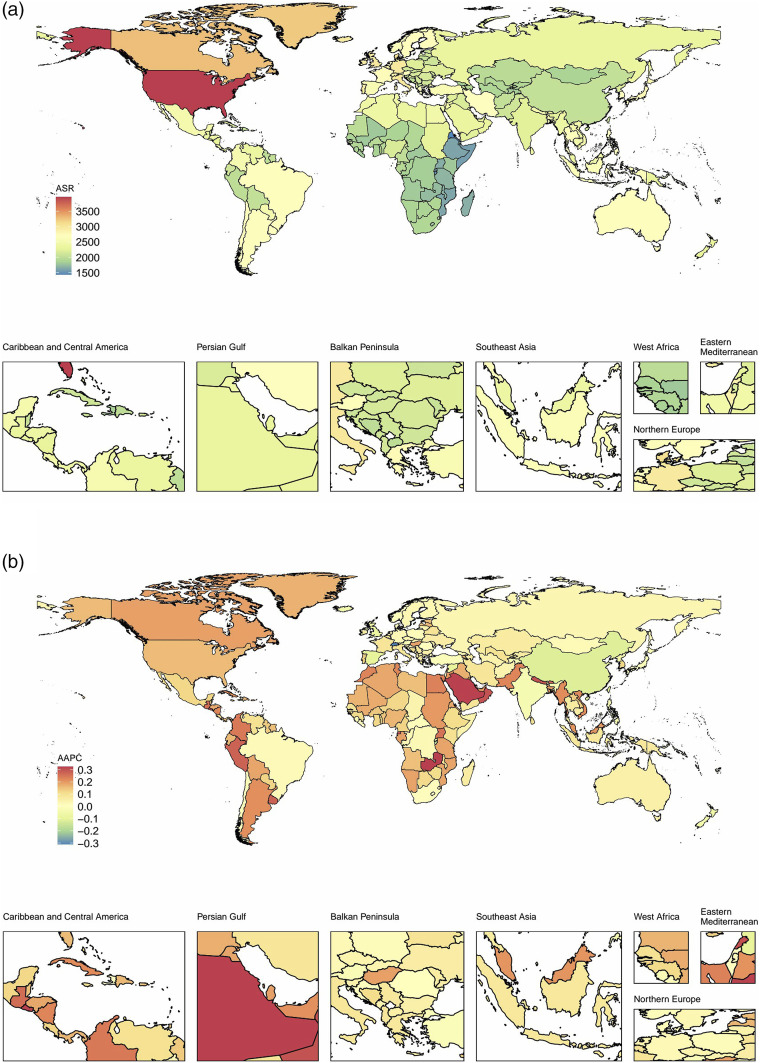
Notably, from 1990 to 2019, the global ASYR for headaches showed an increase with an AAPC of 0.04 (95% CI: 0.0 to 0.04), while that for musculoskeletal disorders declined with an AAPC of −0.05 (95% CI: −0.07 to −0.04) (Figure 4). Specifically, the most substantial increases in ASYRs for headache were observed in East Asia (AAPC: 0.22, 95% CI: 0.21 to 0.23) and Andean Latin America (AAPC: 0.2, 95% CI: 0.18 to 0.21), while for musculoskeletal disorders, significant rises were noted in Andean Latin America (AAPC: 0.24, 95% CI: 0.23 to 0.25) and Central Latin America (AAPC: 0.19, 95% CI: 0.16 to 0.22). However, it’s worth noting that the ASYRs for musculoskeletal disorders declined notably in East Asia with an AAPC of −0.22 (95% CI: −0.3 to −0.14) over the same period (Table S3).
Figure 4.
National distribution of chronic pain ASYRs and AAPC for both genders in 2019 in 204 countries. (a): Distribution of ASYR of chronic pain; (b): distribution of AAPC of ASYR of chronic pain. Abbreviation: ASYR: age-standardized YLDs rate; AAPC: average annual percent change.
Associations between SDI and ASRs of headache and musculoskeletal disorders
Analyses were conducted to investigate the associations between ASRs for chronic pain and SDI trends for each region from 1999 to 2019. The study revealed a modest positive association between global ASRs and SDI. Specifically, regions with higher SDI levels showed a greater burden of chronic pain, as evidenced by a higher ASPR (Figures 1, 3 and S1). Conversely, a limited correlation was observed between regional ASRs and SDI. This variability suggests that the relationship between ASRs and SDIs differs across regions and does not consistently reflect inequality in ASRs among countries with varying SDIs (Figures 1, 3 and S1). These findings emphasize the need for region-specific approaches to address this public health challenge.
The Joinpoint analysis was utilized to illustrate the trends of ASR in five SDI regions. Our findings revealed that high-SDI regions demonstrated the highest ASRs (ASPR, ASIR, and ASYR), and middle SDI regions exhibited a notable change in slope. Upon closer examination, during the past 30 years, the trends of ASRs were divided into no less than four segments, and the ASYRs and ASPRs in the five SDI regions remained stable, except which of ASIRs showed a modest decline across all regions. Notably, it was evident that the slopes of ASRs in most SDI regions demonstrated a significant decline from 1990 to 2000, especially from 1990 to 1993 of ASYR in the middle SDI region with APC of 0.73. Furthermore, the trends in most SDI regions demonstrated a modest increase from 2000 to 2005 and 2017 to 2019, particularly in middle SDI regions with an APC of 0.35 from 2000 to 2005, but the reasons may be conflicted (Figures 1, 3 and S1).
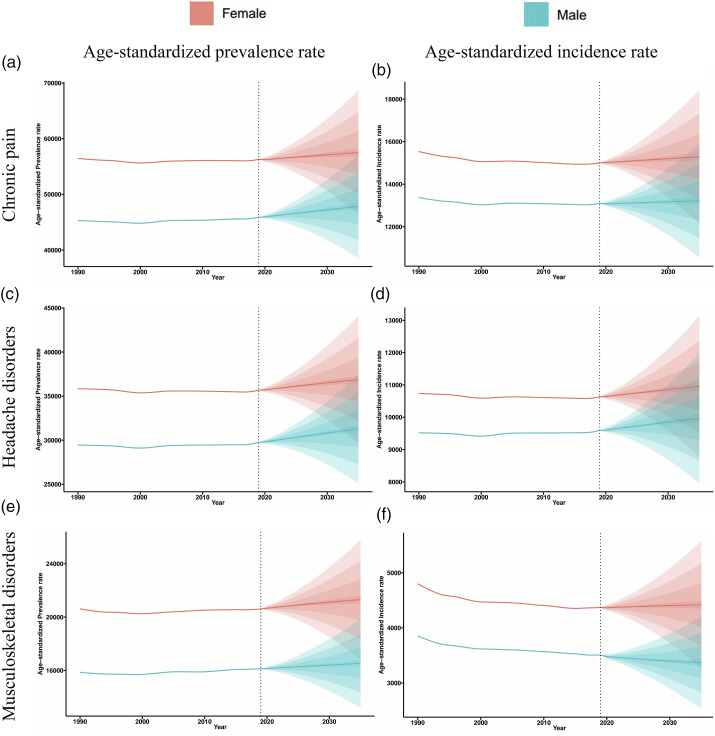
Projection for the ASRs of chronic pain
Employing the highly adaptable Bayesian APC model, we conducted projections for the global and regional incidence and prevalence of headaches and Musculoskeletal disorders for both genders from 2020 to 2035, as depicted in Figures 5 and S3. Regarding Musculoskeletal disorders, changes were difficult to observe from 2020 to 2035 in Figure 5(E) and (F), only males are projected to experience less burden of Musculoskeletal disorders. However, our analysis also revealed that headache is poised to impose a heavier burden worldwide for both genders in the next 15 years.
Figure 5.
Trends of ASPR and ASIR of chronic pain with headache and musculoskeletal disorders for males and females from 2020 to 2035. (a): Trends of ASPR of chronic pain with headache and musculoskeletal disorders for males and females from 2020 to 2035; (b): trends of ASIR of chronic pain with headache and musculoskeletal disorders for males and females from 2020 to 2035. Abbreviation: ASPR: age-standardized prevalence rate; ASIR: age-standardized incidence rate.
Between 2020 and 2035, the ASRs of Chronic pain are anticipated to remain stable in most regions for both genders. However, in South Asia, Tropical Latin America, and High-income North America, the situations are expected to gradually increase with no disparity between the two genders after 2020. For another in Southern Latin America, Australasia, and Western Europe, the ASPRs for males and ASIRs for females are projected to rise gradually, but ASPRs for females and ASIRs for males are expected to decline slowly after 2020. Furthermore, we also found severe situations in High-income North America and South Asia, which could undertake substantially heavier burdens in the future, meaning that economic levels may have limited relation with preventing these diseases. Fascinatingly, the High-income Asia Pacific region stands out as the sole area where ASRs of Chronic pain are anticipated to decrease in the future for both males and females. This suggests that local efforts in the prevention and treatment in mitigating the increasing burden of Chronic pain may be effective (Figure S3).
Discussion
In this study, utilizing GBD 2019 data, we examined the global, regional, and national epidemiological trends of chronic pain, focusing on its incidence, prevalence, and YLDs. We also explored the associations between these trends and the SDI.
Over the past three decades, there has been a discernible increase in the global ASPR and ASYR for chronic pain. However, a slight decline in ASIR has been observed. Notably, females have consistently exhibited higher rates across these metrics. Among the specific types of chronic pain, TTH has emerged as a predominant disorder globally, particularly among younger age groups. Conversely, LBP has been a leading contributor to global disability, with a significant impact on individuals aged 75 and above. Our analyses revealed that high-SDI regions have consistently reported a higher burden of chronic pain over the past 30 years. Looking forward, while the ASRs for musculoskeletal conditions are projected to remain relatively stable, an increasing prevalence of headache disorders, especially TTH, is anticipated.
Gender disparities in chronic pain prevalence were evident, with women more susceptible to conditions like LBP and migraine. This aligns with studies showing challenges faced by postmenopausal women due to age-related musculoskeletal changes.10–13 Improvements in treatment methods and therapeutic options have contributed to a recent decline in ASIRs and ASYRs for LBP and TTH.14–17 However, challenges such as medication overuse and lifestyle triggers remain significant.18,19
Regional analyses indicate that socioeconomic transitions, particularly in Andean Latin America, East Asia, and South Asia, may contribute to the rising prevalence of TTH.20–23 Additionally, TTH has been associated with neck pain and LBP.16,17 These regional disparities call for tailored approaches to chronic pain management.
Our research highlights the substantial global disability caused by LBP, particularly among individuals aged 75 and above. Older age groups are particularly susceptible to severe incapacitation from LBP, leading to reduced mobility and autonomy. Moreover, about 20% of older adult individuals with LBP face difficulties in performing daily self-care tasks and participating in social activities. 24 Comparatively, older individuals often experience inferior treatment outcomes and slower recovery rates compared to their younger counterparts. Given these challenges, there is an urgent need to develop targeted management guidelines for older adult LBP patients. These guidelines should consider age-specific clinical outcomes such as institutionalization risks, fall prevention, and mobility issues. Additionally, understanding patient preferences and the acceptability of treatments is crucial. 25
In 2019, a modest positive correlation was observed between global ASRs for chronic pain and SDI across all quintiles. High-SDI nations, in particular, bore a significant burden of chronic pain. However, this relationship was not uniformly observed across regions. The ASRs for headache disorders also showed a positive association with SDI. This could be attributed to factors prevalent in high-income countries, such as aging populations, physical inactivity, mental stress, and obesity, which increase the risk of comorbid conditions. 23 However, addressing the burden of chronic pain presents challenges in both high-income and low and middle-income countries. Firstly, treatment effectiveness data predominantly originate from high-income countries, leaving a gap in understanding the cultural suitability of guideline recommendations for lower-income nations. It is therefore crucial for developing countries to enhance their epidemiological data collection efforts to bridge this knowledge gap. Secondly, in high-income countries with well-established medical systems, it is imperative to align healthcare practices with clinical guidelines to mitigate excessive opioid use and unnecessary surgical interventions, thereby ensuring optimal patient care and resource utilization. 26
According to the projection in high-income Asian countries like Korea and Japan, the decline of burden in the next decade needs to be a focus as this decline is largely due to improved access to medical services and advancements in pain management techniques, coupled with increased public awareness through media. 27 For instance, effective interventions, including better pain education and preventive measures, have significantly reduced the burden of chronic pain, particularly among the older adults. To ensure effective pain education and prevention in Korea, a holistic strategy combining public awareness campaigns, integration into primary care, regular provider training, targeted community programs, and ongoing evaluation should be implemented. Despite these advances, a significant portion of individuals remain untreated, underscoring the need for a multidisciplinary approach to address both the physical and psychological aspects of chronic pain. 28
In previous studies, older adults from lower-income backgrounds facing higher risks due to limited access to healthcare, preventive measures, and treatments. If suffering from stress, anxiety, and depression which are known to exacerbate pain perception, these individuals may have to survive under heavier pain. In terms of lifestyle factors, physical inactivity is strongly associated with an increased risk of musculoskeletal pain, while regular exercise has been shown to alleviate chronic pain, especially in conditions like low back pain. This highlights the importance of moderate exercise as a mitigating factor for chronic pain. 29 Opioid overuse is another well-recognized factor that not only contributes to the persistence of pain but also leads to dependency and other adverse health outcomes. 30 Yet their long-term effectiveness in managing chronic pain remains controversial. Notably, the roles of researchers and health care providers could be crucial. 31 Researchers can utilize our findings to develop targeted interventions that addressing the specific metrics involved in ages, genders, SDI and symptoms, such as mobility programs for older adults with LBP, which can reduce disability and improve quality of life. 32 Additionally, health care providers can use these data to develop more socio-demographically tailored campaigns focused on increasing access to medical care of the patients with musculoskeletal disorders in lower-income areas or changing their lifestyle modifications.
Between 2020 and 2035, regional ASRs for chronic pain are expected to remain relatively stable, with headaches showing increasing trends for both genders, suggesting that despite advancements in treatment and management strategies, the overall burden remains consistent. This could reflect the limitations of existing therapeutic approaches or possibly highlight the need for more targeted interventions. Moreover, factors such as aging populations, lifestyle changes, and socioeconomic disparities across regions should be noted.31,33,34 The rising trends in headaches warrant attention, particularly considering the potential impact on individuals’ quality of life and healthcare systems. Earlier diagnosis and more effective treatment are needed to address this problem. Furthermore, tailored and targeted public health interventions may be crucial to reducing the burden of chronic pain, especially in regions where the prevalence is increasing. 35
Several limitations should be noted in this study. Firstly, it focused mainly on Migraine, TTH, and LBP due to data constraints. Future research should aim to include a broader range of chronic pain conditions. Secondly, the lack of YLDs data from 1990 to 2019 limited our projections for ASYRs from 2020 to 2035. We anticipate that future updates may address this gap. Lastly, potential risk factors for chronic pain were not fully explored due to the scope of the study, warranting further investigation in future research.
Conclusion
This study reveals a global trend in chronic pain over the past three decades, with TTH emerging as a major concern. While musculoskeletal pain is projected to remain stable, an increase in headache disorders is anticipated. These findings underscore the ongoing challenges in managing chronic pain worldwide.
Supplemental Material
Supplemental Material for Global and regional trends and projections of chronic pain from 1990 to 2035: Analyses based on global burden of diseases study 2019 by Mengyi Zhu, Jiarui Zhang, Diefei Liang, Junxiong Qiu, Yuan Fu, Zhaopei Zeng, Jingjun Han, Junmeng Zheng and Liling Lin in British Journal of Pain.
Author contributions: LL, JZ, and JH conceptualized the study and offered comprehensive guidance. MZ, JZ, and DL drafted the initial manuscript. MZ and JZ conducted data extraction. MZ, JZ, YF, and ZZ contributed to the execution of the analysis. All authors participated in interpreting the findings, meticulously reviewed the manuscript, and endorsed the final version submitted for publication.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: LL is supported by the Medical Science and Technology Research Fund of Guangdong Province (A2024010), JM is supported by National Natural Science Foundation of China (82271806), and JQ is supported by Natural Science Foundation of Guangdong Province (2022A1515110560), Basic and Applied Basic Research Project of Guangzhou Basic Research Program (202201011024), and Scientific Research Sailing Project of Sun Yat-sen Memorial Hospital, Sun Yat-sen University (YXQH2022017).
Supplemental Material: Supplemental material for this article is available online.
Ethical statement
Ethical approval
The Global Burden of Disease study obtained a waiver of informed consent, which was reviewed and approved by the Institutional Review Board at the University of Washington. Comprehensive information regarding ethical standards can be accessed through the official website (https://www.healthdata.org/gbd/2019). No additional ethics approval was required in this study.
ORCID iDs
Mengyi Zhu https://orcid.org/0009-0002-4820-868X
Junmeng Zheng https://orcid.org/0000-0002-4243-8209
Liling Lin https://orcid.org/0000-0001-5487-1758
References
- 1.Caraceni A, Martini C, Zecca E, et al. Breakthrough pain characteristics and syndromes in patients with cancer pain. An international survey. Palliat Med 2004; 18: 177–183. [DOI] [PubMed] [Google Scholar]
- 2.Alford DP, Krebs EE, Chen IA, et al. Update in pain medicine. J Gen Intern Med 2010; 25: 1222–1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perrot S, Cohen M, Barke A, et al. The IASP classification of chronic pain for ICD-11: chronic secondary musculoskeletal pain. Pain 2019; 160: 77–82. [DOI] [PubMed] [Google Scholar]
- 4.Treede RD, Rief W, Barke A, et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the international classification of diseases (ICD-11). Pain 2019; 160: 19–27. [DOI] [PubMed] [Google Scholar]
- 5.Lyng KD, Djurtoft C, Bruun MK, et al. What is known and what is still unknown within chronic musculoskeletal pain? A systematic evidence and gap map. Pain 2023; 164: 1406–1415. [DOI] [PubMed] [Google Scholar]
- 6.Safiri S, Nejadghaderi SA, Noori M, et al. The burden of low back pain and its association with socio-demographic variables in the Middle East and North Africa region, 1990–2019. BMC Muscoskel Disord 2023; 24: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 2020; 396: 1204–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang L, Zhang X, Pu Y, et al. Global, regional, and national burden of urolithiasis from 1990 to 2019: a systematic analysis for the global burden of disease study 2019. Clin Epidemiol 2022; 14: 971–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riebler A, Held L. Projecting the future burden of cancer: Bayesian age-period-cohort analysis with integrated nested laplace approximations. Biom J 2017; 59: 531–549. [DOI] [PubMed] [Google Scholar]
- 10.Wong CK, Mak RY, Kwok TS, et al. Prevalence, incidence, and factors associated with non-specific chronic low back pain in community-dwelling older adults aged 60 years and older: a systematic review and meta-analysis. J Pain 2022; 23: 509–534. [DOI] [PubMed] [Google Scholar]
- 11.Sarlani E, Greenspan JD. Gender differences in temporal summation of mechanically evoked pain. Pain 2002; 97: 163–169. [DOI] [PubMed] [Google Scholar]
- 12.Vetvik KG, MacGregor EA. Sex differences in the epidemiology, clinical features, and pathophysiology of migraine. Lancet Neurol 2017; 16: 76–87. [DOI] [PubMed] [Google Scholar]
- 13.Lu CB, Liu PF, Zhou YS, et al. Musculoskeletal pain during the menopausal transition: a systematic review and meta-analysis. Neural Plast 2020; 2020: 8842110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.GBD 2021 Low Back Pain Collaborators . Global, regional, and national burden of low back pain, 1990–2020, its attributable risk factors, and projections to 2050: a systematic analysis of the global burden of disease study 2021. Lancet Rheumatol 2023; 5: e316–e329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yoon MS, Manack A, Schramm S, et al. Chronic migraine and chronic tension-type headache are associated with concomitant low back pain: results of the German headache consortium study. Pain 2013; 154: 484–492. [DOI] [PubMed] [Google Scholar]
- 16.Ashina S, Lipton RB, Bendtsen L, et al. Increased pain sensitivity in migraine and tension-type headache coexistent with low back pain: a cross-sectional population study. Eur J Pain 2018; 22: 904–914. [DOI] [PubMed] [Google Scholar]
- 17.Ashina S, Bendtsen L, Lyngberg AC, et al. Prevalence of neck pain in migraine and tension-type headache: a population study. Cephalalgia 2015; 35: 211–219. [DOI] [PubMed] [Google Scholar]
- 18.Pellegrino ABW, Davis-Martin RE, Houle TT, et al. Perceived triggers of primary headache disorders: a meta-analysis. Cephalalgia 2018; 38: 1188–1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ashina S, Mitsikostas DD, Lee MJ, et al. Tension-type headache. Nat Rev Dis Prim 2021; 7: 24. [DOI] [PubMed] [Google Scholar]
- 20.Lederbogen F, Kirsch P, Haddad L, et al. City living and urban upbringing affect neural social stress processing in humans. Nature 2011; 474: 498–501. [DOI] [PubMed] [Google Scholar]
- 21.Pacheco-Barrios K, Velasquez-Rimachi V, Navarro-Flores A, et al. Primary headache disorders in Latin America and the Caribbean: a meta-analysis of population-based studies. Cephalalgia 2023; 43: 3331024221128265. [DOI] [PubMed] [Google Scholar]
- 22.Atun R, de Andrade LO, Almeida G, et al. Health-system reform and universal health coverage in Latin America. Lancet 2015; 385: 1230–1247. [DOI] [PubMed] [Google Scholar]
- 23.GBD 2016 Headache Collaborators . Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol 2018; 17: 954–976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dionne CE, Dunn KM, Croft PR. Does back pain prevalence really decrease with increasing age? A systematic review. Age Ageing 2006; 35: 229–234. [DOI] [PubMed] [Google Scholar]
- 25.Rundell SD, Sherman KJ, Heagerty PJ, et al. The clinical course of pain and function in older adults with a new primary care visit for back pain. J Am Geriatr Soc 2015; 63: 524–530. [DOI] [PubMed] [Google Scholar]
- 26.Chen S, Chen M, Wu X, et al. Global, regional and national burden of low back pain 1990–2019: a systematic analysis of the global burden of disease study 2019. J Orthop Translat 2022; 32: 49–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cho S-H, Kim Y-M, Lee J-H, et al. The trend of prevalence of pain in Korea from 2005 to 2016. Korean J Pain 2020; 33: 352–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Takura T, Ushida T, Kanchiku T, et al. The societal burden of chronic pain in Japan: an internet survey. J Orthop Sci 2015; 20: 750–760. [DOI] [PubMed] [Google Scholar]
- 29.Schwan J, Sclafani J, Tawfik VL. Chronic pain management in the elderly. Anesthesiol Clin 2019; 37: 547–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Volkow ND, McLellan AT. Opioid abuse in chronic pain--misconceptions and mitigation strategies. N Engl J Med 2016; 374: 1253–1263. [DOI] [PubMed] [Google Scholar]
- 31.Foster NE, Anema JR, Cherkin D, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet 2018; 391: 2368–2383. [DOI] [PubMed] [Google Scholar]
- 32.Sidiq M, Muzaffar T, Janakiraman B, et al. Effects of pain education on disability, pain, quality of life, and self-efficacy in chronic low back pain: a randomized controlled trial. PLoS One 2024; 19: e0294302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Theeler BJ, Erickson JC. Posttraumatic headache in military personnel and veterans of the Iraq and Afghanistan conflicts. Curr Treat Options Neurol 2012; 14: 36–49. [DOI] [PubMed] [Google Scholar]
- 34.Xavier MK, Pitangui AC, Silva GR, et al. Prevalence of headache in adolescents and association with use of computer and videogames. Ciência Saúde Coletiva 2015; 20: 3477–3486. [DOI] [PubMed] [Google Scholar]
- 35.Li XY, Yang CH, Lv JJ, et al. Correction: global, regional, and national epidemiology of migraine and tension-type headache in youths and young adults aged 15–39 years from 1990 to 2019: findings from the global burden of disease study 2019. J Headache Pain 2023; 24: 156. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Global and regional trends and projections of chronic pain from 1990 to 2035: Analyses based on global burden of diseases study 2019 by Mengyi Zhu, Jiarui Zhang, Diefei Liang, Junxiong Qiu, Yuan Fu, Zhaopei Zeng, Jingjun Han, Junmeng Zheng and Liling Lin in British Journal of Pain.