Abstract
The diseases of the central nervous system (CNS) often cause irreversible damage to the human body and have a poor prognosis, posing a significant threat to human health. They have brought enormous burdens to society and healthcare systems. However, due to the complexity of their causes and mechanisms, effective treatment methods are still lacking. Vagus nerve stimulation (VNS), as a physical therapy, has been utilized in the treatment of various diseases. VNS has shown promising outcomes in some CNS diseases and has been approved by the Food and Drug Administration (FDA) in the United States for epilepsy and depression. Moreover, it has demonstrated significant potential in the treatment of stroke, consciousness disorders, and Alzheimer’s disease. Nevertheless, the exact efficacy of VNS, its beneficiaries, and its mechanisms of action remain unclear. This article discusses the current clinical evidence supporting the efficacy of VNS in CNS diseases, providing updates on the progress, potential, and potential mechanisms of action of VNS in producing effects on CNS diseases.
Keywords: vagus nerve stimulation, central nervous system, clinical application, mechanisms, neurophysiotherapy
1. Introduction
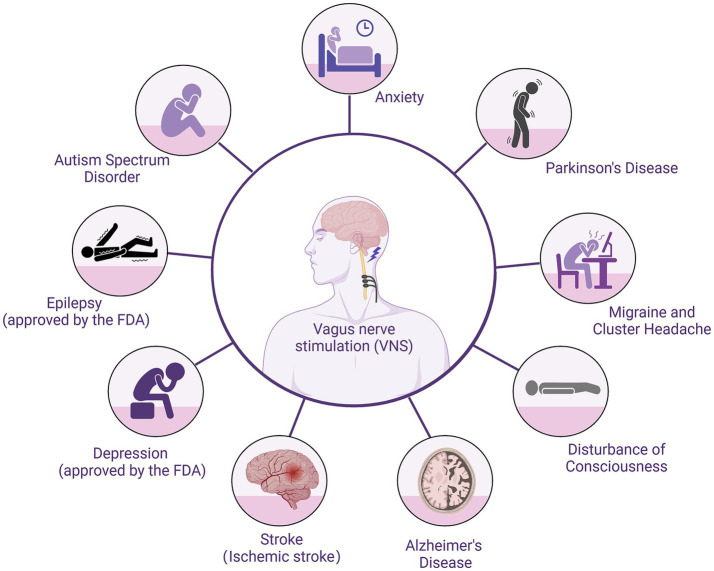
The introduction of vagus nerve stimulation into clinical applications has been a long and convoluted process. VNS was initially proposed by American neurologist James Corning in the late 19th century in an attempt to treat epilepsy. Due to his misconceptions about epilepsy, VNS was abandoned (1). It wasn’t until 1988 that the first implantation of VNS was reported (2), leading to an increase in research on vagus nerve stimulation. After years of study, the efficacy and safety of VNS were confirmed, and diseases it could potentially treat gradually emerged. VNS was first approved by the U.S. Food and Drug Administration for treating drug-resistant epilepsy (3). Subsequently, it was later approved for treating refractory depression, obesity, refractory migraines, and cluster headaches (4, 5). With advancements in the technology of implantable vagus nerve stimulation (iVNS) and its associated high surgical costs and side effects, non-invasive vagus nerve stimulation (nVNS) was proposed and implemented. Meanwhile, the clinical applications and effects of iVNS and nVNS also differ. Vagus nerve stimulation is a relatively newer therapeutic approach, and besides its explicitly approved clinical uses, there exist numerous potential applications (Figure 1). This article will provide an overview of the applications, potential, side effects, and mechanisms of action of vagus nerve stimulation in central nervous system diseases.
Figure 1.
Use of VNS in central nervous system diseases.
2. Vagus nerve stimulation
2.1. Invasive vagus nerve stimulation
Invasive Vagus Nerve Stimulation (iVNS) involves surgically implanting a vagus nerve stimulation device into the human body. The vagus nerve stimulator consists of stimulating electrodes implanted around the vagus nerve through a small cervical incision and a pulse generator implanted in the subclavian region (6, 7). The device delivers electrical stimulation every few minutes. Additionally, patients can use a wristband magnet to trigger the pulse generator, providing an extra dose of stimulation. Over several weeks following implantation, the current is gradually adjusted to the target level based on patient tolerability (7). The electrode types include helical electrodes that wrap around the vagus nerve and intravascular electrodes placed within the internal jugular vein. Helical electrodes are commonly used for broad nerve activation, while intravascular electrodes are designed to reduce off-target effects and enhance stimulation specificity (8). The complications of VNS include those related to surgery and those associated with the device and nerve stimulation. During VNS implantation, the implanted device is typically tested using one pulse train lasting 1 min with specific parameters (1 mA, 550 μs, 20 Hz). This phase may result in bradycardia or even cardiac arrest (6, 9). Surgical complications such as peritracheal hematoma, infection, and vagus nerve injury have also been reported (10). Complications associated with the device and nerve stimulation include delayed arrhythmias (bradycardia, cardiac arrest), laryngopharyngeal dysfunction (hoarseness, dyspnea, and coughing) due to stimulation of the recurrent laryngeal nerve, obstructive sleep apnea, phrenic nerve stimulation caused by proximity, tonsillar pain resembling glossopharyngeal neuralgia, and sternocleidomastoid muscle spasms (6, 11–13). The iVNS therapy system is indicated for stimulating the left vagus nerve located within the carotid sheath, specifically below the point where the superior and inferior cervical cardiac branches diverge from the vagus nerve (14). Typically, the left-sided cervical vagus nerve is chosen as the implantation site for the stimulating electrodes because stimulating the right-sided vagus nerve can lead to severe adverse reactions. The right vagus nerve innervates the sinoatrial node and parts of the myocardium, and nerve stimulation can cause various cardiac side effects, such as cardiac arrest. In comparison to the right-sided vagus nerve, the left-sided vagus nerve innervates the atrioventricular node, resulting in relatively milder adverse reactions (7). Furthermore, studies have shown that stimulation frequencies of 50 Hz or higher during VNS can cause significant and irreversible damage to the vagus nerve. To minimize adverse events associated with direct stimulation of the carotid sheath, stimulation frequencies were randomly selected within the range of 20–30 Hz (14, 15). AspireSR is a pulse generator that detects heart rate through specific detection algorithms, recommended for use in cardiac patients due to the cardiac side effects of VNS (16). Additionally, SenTiva VNS has a cardiac detection feature that not only detects heart activity but also allows for changes in VNS output parameters, making VNS therapy more tailored and safe. The SenTiva device is smaller in size compared to AspireSR. For pediatric patients whose development is not yet complete, having an appropriately sized implantable pulse generator is particularly crucial. Moreover, for those seeking smaller surgical incisions and aesthetic considerations, SenTiva represents a favorable choice. Despite being withdrawn from clinical use by the U.S. Food and Drug Administration in 2020 due to reset errors, SenTiva regained approval in 2022 (16, 17).
2.2. Non-invasive vagus nerve stimulation
Invasive Vagus Nerve Stimulation requires surgical implantation, while non-invasive Vagus Nerve Stimulation avoids trauma and is more cost-effective. nVNS devices stimulate the VN at specific body surface sites to achieve therapeutic effects. nVNS comprises transcutaneous auricular Vagus Nerve Stimulation (taVNS) and transcutaneous cervical Vagus Nerve Stimulation (tcVNS), relying on the distribution of vagal afferents in the ear and neck, respectively (18). taVNS transmits signals by stimulating the auricular branch of the vagus nerve (ABVN). Peuker and Filler found anatomical structures in the ear—such as parts of the ear canal and auricle—that send their afferent information via vagal branches. The optimal site for stimulation is the cymba conchae, as ABVN primarily exists in the skin surrounding the cymba conchae (19, 20). tcVNS involves stimulation of the vagus nerve within the carotid sheath, with the stimulation signals activating the VN through the skin and other tissues near the carotid sheath, thereby inducing vagus nerve action potentials. tVNS can be administered using various devices, such as the transcutaneous Vagus Nerve Stimulation device NEMOS and the neck-stimulating gammaCore (21). The use of VNS is restricted to the left vagus nerve, while tVNS might not have this limitation. Research by Chen et al. suggests that unilateral VN stimulation transmits only on one side, while unilateral ABVN stimulation integrates within the nucleus tractus solitarii and then transmits bilaterally via the vagus nerve. Results indicate that right transcutaneous vagus nerve stimulation is as safe as left transcutaneous vagus nerve stimulation (22). Studies by He et al. and Hein E et al. respectively employed bilateral transcutaneous vagus nerve stimulation in clinical trials involving children and adults. No adverse cardiac-related reactions were observed in these experiments (23, 24). Although nVNS is relatively safe, it is not without side effects, which include localized skin irritation caused by electrode placement, headaches, nasopharyngitis, gastrointestinal reactions, palpitations, and vocal cord hoarseness (14). Different devices have varying stimulation methods, frequencies, durations, and other parameters. Currently, there are no standardized optimal stimulation parameters, nor is there literature establishing superiority between taVNS and tcVNS stimulation methods.
3. Clinical and potential applications in central nervous system diseases
3.1. Epilepsy
Since the 1990s, numerous studies have evidenced the favorable effects of VNS in reducing seizure frequency in epilepsy patients (25, 26). In 1997 and 1999, the American Academy of Neurology (AAN) Therapeutics and Technology Assessment Subcommittee conducted two evaluations of VNS therapy for epilepsy. The committee concluded that VNS is suitable for adults and adolescents aged 12 and above with refractory partial-onset seizures (excluding those suitable for potentially curative surgical resection) (27, 28). Due to the infrequent occurrence of complete seizure remission with VNS and its invasiveness and high cost, VNS is deemed more appropriate for individuals intolerant to or not benefiting from antiseizure medication (ASMs) (28). Subsequently, the feasibility and safety of VNS were further acknowledged, with observed reductions in seizure frequency over time (29, 30). Moreover, during the use of invasive VNS in epilepsy patients, the blood concentrations of ASMs remained unaffected by VNS and could even reduce the dosage of ASMs (31, 32). Currently, invasive Vagus Nerve Stimulation has been approved for epilepsy treatment in numerous countries and regions, including the European Union, the USA, Canada, China, and Japan (33). In recent years, although iVNS has shown promising results in the treatment of drug-resistant epilepsy, it is still chosen only after antiseizure medications and surgical options have been ruled out, primarily due to its invasive nature and cost-effectiveness concerns. This is largely due to its invasive nature and cost-effectiveness concerns. Studies on the cost-effectiveness of iVNS have demonstrated a significant reduction in epilepsy-related direct medical expenses following VNS implantation compared to pre-implantation costs (34–36). Evans et al. (37) included the cost of device implantation in their analysis and obtained similar results. However, the reduction in costs is observed only when the treatment is effective and not prematurely discontinued due to ineffectiveness or severe side effects. Additionally, surgical and other medical costs vary across countries, leaving the cost-effectiveness of VNS still uncertain (33).
Further research has found that VNS is effective for various types of epilepsy and can serve as an adjunctive therapy for both focal and generalized seizures. However, in clinical practice, iVNS is more commonly used for patients with focal seizures. Some researchers suggest this could be because focal seizures may develop a higher likelihood of drug resistance, or it might relate to the relatively lower incidence of refractory generalized seizures in adults (33). Recent studies have also discovered positive effects of VNS on drug-resistant generalized seizures, particularly in cases of genetic generalized epilepsy, significantly reducing seizure frequency and epilepsy-related hospitalizations among these patients (38).
Invasive Vagus Nerve Stimulation can also be used as adjunctive therapy for pediatric epilepsy, with abundant research confirming its effectiveness and safety (12, 39). Children’s response to invasive VNS (reduction in seizure rate by ≥50%) is similar to that of adults, and seizure frequency tends to decrease with prolonged treatment (12, 40). Besides reducing seizure rates, iVNS has shown favorable outcomes in seizure duration, severity, post-seizure severity, quality of life, and overall clinical improvement (39–41). iVNS is similarly effective for pediatric or adolescent epilepsy syndromes, including Dravet syndrome (DS), Lennox–Gastaut syndrome (LGS), hypothalamic hamartomas, epileptic encephalopathies, Rett syndrome, and tuberous sclerosis complex (TSC) (39, 42–49). Initially, the FDA approved iVNS for patients aged 12 and older. However, Elliott et al. found no significant differences in treatment efficacy or complications between children under 12 and older children (12 to under 18 years old) (50). The American Academy of Neurology guideline development subcommittee suggested that for children with partial and generalized seizures who are not suitable for brain surgery, iVNS could be considered (29). Subsequent clinical studies reported the use of iVNS in children around 5 years old, revealing more pronounced improvements in quality of life and cognitive outcomes in the younger age group (under 5 years old) (41). Thus, for children with drug-resistant epilepsy, considering VNS implantation early on could mitigate the adverse effects of epilepsy on their development.
Studies have suggested that Vagus Nerve Stimulation can serve as an adjunctive therapy to control seizures during pregnancy for women with epilepsy (51, 52). There are reported cases where expectant mothers undergoing iVNS treatment for epilepsy during pregnancy led to fetal anomalies, including unilateral congenital glaucoma, mild malformations, and heart murmurs (52, 53). However, in these cases of neonatal anomalies, these pregnant women were also on multiple antiseizure medications in addition to VNS therapy. Ding et al. (54) reviewed and analyzed past relevant literature, concluding that VNS during pregnancy is relatively safe and effective for both the fetus and the mother, suggesting there’s no need to deactivate VNS during pregnancy. However, clinical trials involving VNS therapy for pregnant women with epilepsy are scarce, and the sample sizes in existing case reports are small. Additionally, VNS is often used in conjunction with ASMs, making it challenging to distinguish whether adverse reactions are solely attributable to VNS as an isolated factor. Therefore, further relevant experiments are necessary to determine the suitability of VNS for pregnant women.
Determining the optimal stimulation parameters for patients of different ages and those with specific seizure types or syndromes remains uncertain. The side effects and stimulation levels in invasive Vagus Nerve Stimulation might be closely related. Higher stimulation levels tend to result in higher rates and severity of side effects compared to lower stimulation levels (32). The settings recommended by manufacturers for VNS therapy in epilepsy are typically 1.5–2.25 mA with a pulse width of 250 μs and a frequency of 20 Hz. However, manufacturers only provide recommendations for therapeutic dosing and titration rather than definitive guidelines (55). Fahoum et al. attempted to explore target dosing for drug-resistant epilepsy (DRE) and inferred overall target output current and duty cycle for VNS therapy in epilepsy to be 1.61 mA and 17.1% duty cycle, respectively. Their analysis suggested that patients with longer durations of VNS therapy were more likely to respond to treatment, implying that patients with inadequate sustained dosing might still benefit from achieving target dosing. Therefore, improvements in VNS outcomes might be achieved through appropriately implementing evidence-based dosing and titration guidelines (55). Additionally, rapid titration in DRE patients results in faster clinical benefits regardless of age, and children demonstrate greater tolerance to rapid titration (56, 57). However, most of these reports assess efficacy based on response rates. In practice, while considering efficacy, it’s essential to tailor parameters differently for individuals based on their unique constraints (such as age, physique, etc.) and side effects.
Based on existing clinical trials targeting transcutaneous Vagus Nerve Stimulation (tVNS) for treating drug-resistant epilepsy, the majority of scholars widely acknowledge tVNS as an effective, cost-efficient, and relatively safe adjunct therapy for such patients (58–63). These studies assessed the effectiveness of tVNS in terms of seizure frequency, severity, quality of life, and epilepsy rating scales. Additionally, compared to invasive Vagus Nerve Stimulation, research indicates that transcutaneous Vagus Nerve Stimulation exhibits milder adverse reactions (60, 61, 63, 64). tVNS has also shown positive clinical outcomes for post-stroke epilepsy (65). Furthermore, studies have clinically validated the safety and efficacy of transcutaneous auricular Vagus Nerve Stimulation in treating childhood epilepsy (24). These findings suggest that tVNS represents a highly promising adjunct therapy for drug-resistant epilepsy applicable to both adults and children. However, differences exist in the devices used, stimulation parameters, and duration of studies in these clinical trials, hence the optimal stimulation parameters for tVNS remain unclear (66, 67), necessitating further research and exploration. tVNS holds significant potential in epilepsy treatment, given its non-invasive nature and relatively high safety profile, making it more acceptable to patients. However, there is currently no research indicating how to choose between tVNS or iVNS for patients with drug-resistant epilepsy. Apart from their efficacy in treating epilepsy, the choice between iVNS and tVNS in practice also involves cost-effectiveness considerations, which require further supporting evidence.
3.2. Depression
In clinical trials of Vagus Nerve Stimulation for epilepsy treatment, an unexpected discovery emerged regarding VNS’s regulatory effect on human emotions, suggesting a sustained improvement in mood (68, 69). These studies revealed the potential of VNS in treating depression. Early studies predominantly involved treatment-resistant depression patients (those unresponsive to various antidepressant therapies, including medications and electroconvulsive therapy). Following VNS treatment, these patients exhibited notable improvements in their 28-item Hamilton Rating Scale for Depression (HRS-D-28), Montgomery-Åsberg Depression Rating Scale (MADRS), and Clinical Global Impression Improvement score (CGI-I1 or 2) (70, 71). Additionally, these patients showed good tolerance to the treatment (72, 73). In subsequent randomized controlled trials, treatment-resistant depression patients receiving adjunctive VNS showed better performance on depression-related assessment scales compared to those undergoing conventional therapy alone, indicating the positive effects of adjunctive VNS (74, 75). Furthermore, apart from clinical efficacy, VNS also enhanced their quality of life, reduced mortality, and suicide rates (5, 75, 76). However, John et al. found in their experiments that the short-term efficacy (10 weeks) of VNS as an adjunctive treatment for treatment-resistant depression was not significant (77). Moreover, other experiments have shown that VNS-induced improvement in symptoms of depression accumulates over time in the short term and persists (5, 75, 78), suggesting that longer treatment durations might be necessary to achieve the desired effects when using VNS for depression. In 2005, VNS was approved for depression treatment. The National Institute for Health and Care Excellence (NICE) released guidelines for the use of invasive Vagus Nerve Stimulation in treating treatment-resistant depression, suggesting its consideration when patients have failed multiple antidepressants and psychological therapies, including electroconvulsive therapy or other forms of neurostimulation, such as VNS. Current studies mostly demonstrate iVNS as an effective anti-depression treatment, although the evidence literature is limited and requires further substantiation of its efficacy and safety.
Additionally, VNS might offer promising prospects for pregnant women and children with depression. Antidepressants have a range of effects on pregnant women, such as miscarriage, premature birth, fetal malformations, and neonatal adaptation syndrome (79). In this context, VNS as a treatment approach provides a new avenue. A case report from 2005 detailed significant relief from pregnancy-related depression in a patient receiving a combination of antidepressants and VNS therapy (80). There have been noticeable improvements in emotional and depression-related assessment scores among pediatric patients as well (81). However, the effectiveness and safety of VNS therapy for treatment-resistant depression in children and pregnant women have not been well elucidated. Therefore, more research is needed to determine specific criteria for selecting candidates for iVNS treatment within depression.
Transcutaneous Vagus Nerve Stimulation is also effective in treating depression. Several clinical trials using tVNS for treatment-resistant depression have demonstrated its effectiveness and safety. Combining tVNS with standard treatment offers greater benefits to patients (23, 82–85). Furthermore, the efficacy of tVNS in treating depression is comparable to that of citalopram (an antidepressant), suggesting that tVNS could not only serve as an adjunctive therapy but also potentially as an alternative treatment (86). However, there is still a lack of high-quality evidence regarding the effectiveness of tVNS for different types and severity levels of depression (87).
3.3. Stroke
Ischemic stroke and hemorrhagic stroke are two types of strokes, both with serious consequences that lead to a range of lingering effects impacting patients’ daily lives and social interactions. Vagus Nerve Stimulation serves as an auxiliary method in conventional rehabilitation treatments, displaying promising outcomes in the treatment of ischemic strokes. In recent years, there has been a growing number of animal experiments and clinical trials investigating VNS treatment for ischemic strokes. However, the application of VNS therapy is excluded for hemorrhagic strokes.
3.3.1. Limb motor function
Stroke often leads to loss of limb motor function. Studies indicate that about 60% of patients still experience upper limb movement impairments 6 months after surgery, significantly impacting their quality of life (88). VNS has been widely used in clinical settings for the recovery of upper limb function after ischemic stroke. Numerous clinical trials suggest that VNS in conjunction with rehabilitation (a home exercise program) has a positive impact on upper limb recovery in patients. Measurements such as the Fugl-Meyer Upper Extremity Assessment (FMA-UE), Wolf Motor Function Test (WMFT), Box and Block Test, Nine-Hole Peg Test, Stroke Impact Scale, and Motor Activity Log (MAL) all show positive changes (89–91).
Research has also emerged on tVNS for upper limb function recovery in stroke patients. Compared to a sham-VNS combined with upper limb movement therapy group, the Fugl-Meyer (UFM) scores significantly improved in the non-invasive vagus nerve stimulation combined with upper limb movement therapy group. This demonstrates the feasibility and effectiveness of tVNS in upper limb function recovery (92, 93). Motor-activated auricular vagus nerve stimulation (MAAVNS) is a closed-loop vagus nerve stimulation system that combines electromyography (EMG) and taVNS. Initially, EMG sensors detect movement in a specific muscle, and the EMG signal is then processed to activate the nerve stimulator, pairing muscle movement with tVNS (94). In a recent study, Badran et al. found that MAAVNS was more beneficial for upper limb function recovery (twice as effective as taVNS alone), and the total stimulation pulses received by the MAAVNS group were also fewer than those in the taVNS group (95).
3.3.2. Sensory function
Besides the impairment in limb movement, sensory loss after a stroke is also quite common, and successful movement often relies on the integration of sensory and motor functions (96). In a clinical study focusing on VNS treatment for upper limb movement impairments, a patient experiencing both motor and sensory issues underwent VNS therapy, resulting in significant recovery in limb movement while the sensory problems persisted. Subsequently, this patient received VNS combined with sensory therapy, leading to a marked improvement in sensory function (97). VNS holds promise as a new approach to treating sensory impairments, yet further evidence is needed to support this.
3.3.3. Dysphagia
Stroke patients commonly experience difficulty swallowing, which can lead to several complications such as pneumonia, dehydration, and malnutrition, with pneumonia being a severe complication that can cause fatalities. Yuan et al. reported a case where a patient’s oral swallowing function significantly improved after 6 weeks of using ta-VNS for treating swallowing difficulties (98). A recent double-blind, placebo-controlled, parallel study involving 40 acute stroke patients arrived at similar conclusions (99). tVNS holds promise as a complementary therapy for post-stroke swallowing difficulties, yet further research is needed.
3.4. Disorders of consciousness
Disorders of consciousness (DOC) refer to impaired consciousness following severe brain or neurological injury. Based on their neurological behavioral functions, DOC can be classified into four categories: coma, vegetative state/unresponsive wakefulness syndrome (VS/UWS), minimally conscious state (MCS), and emergence from MCS to higher levels of consciousness (eMCS) (100). In recent years, the utilization of vagus nerve stimulation (VNS) techniques has sparked considerable interest among neuroscientists for treating disorders of consciousness. These techniques offer a promising neuroregulatory treatment method for the rehabilitation of DOC patients.
Studies investigating the use of vagus nerve stimulation in treating disorders of consciousness have explored various etiologies, including traumatic brain injury (TBI) (101), stroke (102), hypoxic–ischemic encephalopathy (HIE) (103), and intracerebral hemorrhage (104). Vagus nerve stimulation, whether invasive VNS (105) or non-invasive VNS (101, 103, 106), has shown favorable outcomes in treating DOC. In these studies, assessment of consciousness disorders includes behavioral assessment and brain function evaluation. Behavioral assessment of DOC patients primarily utilizes the revised Coma Recovery Scale-Revised (CRS-R). Nearly all studies using CRS-R as a primary outcome measure reported significant improvements in scores post-intervention (101, 103, 105–107), except for Wang et al.’s study (which did not find significant changes in the scale) (108). Additionally, efficacy might increase over extended periods of time (109). Brain function assessment via scale scoring includes electroencephalograms (EEG) (105), positron emission tomography (PET) (105), and functional magnetic resonance imaging (observed changes in default mode networks and cerebral blood flow) (103, 104), providing evidence of cerebral changes post-stimulation. Yu et al. (104) found that individuals who responded to auditory stimulation (RtAS) had demonstrated better therapeutic outcomes following tVNS compared to those who did not respond, suggesting that preserved auditory function might be a key preexisting factor for tVNS responders among DOC patients.
Research on VNS has primarily focused on patients classified as VS/UWS or MCS. Wang observed significant alterations in cortical connectivity in specific brain regions through electroencephalographic observation in MCS patients, with noticeable changes in interbrain connectivity in MCS patients (108). Noe et al. also found a significant improvement in CRS-R scores in MCS patients with tVNS, while VS/UWS patients did not significantly benefit (101). However, other studies have indicated that VS/UWS patients also benefit from vagus nerve stimulation (104). In summary, the specific target population for the application of VNS in DOC remains inconclusive. In a review of VNS treatment for DOC, the author concluded that existing studies had insufficient sample sizes, low quality (lack of strict adherence to methodology, inadequate sample size selection, reliance on single outcome indicators to assess consciousness levels, and short monitoring follow-up), thus preventing definitive conclusions or recommendations (110).
3.5. Alzheimer’s disease
Alzheimer’s disease (AD) typically starts subtly and gradually progresses, manifesting as declining cognitive abilities and memory impairments, eventually affecting normal life (111). There is not extensive research on iVNS (implantable vagus nerve stimulation) for treating Alzheimer’s disease, but the existing reports show promising outcomes. Two reports involving 27 AD patients revealed improvements or stability in Alzheimer’s disease assessment scales such as the Alzheimer’s Disease Assessment Scale-Cognitive Subscale (ADAS-cog), the Mini-Mental State Examination (MMSE), and Clinician’s Interview-Based Impression of Change plus Caregiver Input (CIBIC+) (112, 113). Additionally, patients did not experience a significant decline in mood, behavior, or quality of life 1 year post-treatment (113). Apart from enhancing cognitive capabilities, iVNS demonstrates a positive impact on memory loss, effectively ameliorating Alzheimer’s disease symptoms. Studies indicate that iVNS enhances word recognition memory, working memory, and memory retention in language learning (114, 115). In summary, iVNS may delay AD progression and improve its symptoms. However, reports on iVNS treatment for AD are limited and have garnered little attention. This might be attributed to the fact that AD patients are mostly elderly, and the high risk of invasive vagus nerve stimulation in the elderly population cannot be overlooked.
The impact of tVNS on Alzheimer’s disease is currently under exploration in human trials (NCT04908358, NCT04877782). One study involving 140 elderly individuals will divide participants into tVNS and sham stimulation groups, receiving percutaneous vagus nerve stimulation-breathing controlled auricular electrical stimulation for 10 min (twice, with a 4-week interval). The efficacy of VNS will be determined through the Face-Name Associative Memory Exam (FNAME) and Alzheimer’s disease-related biomarkers in blood. Another study aims to explore the impact of tVNS on memory and attention by monitoring its effects on Alzheimer’s disease.
Research on the effects of tVNS on memory has also emerged. Early findings suggested that tVNS could alter associative memory performance in older individuals (116). In an experiment involving 60 healthy volunteers, tVNS did not impact word processing or overall emotional memory recognition. However, compared to sham stimulation, tVNS increased the hit rate percentage for high confidence memory words, suggesting an impact on recollective memory performance (117). Sun et al. proposed that tVNS has beneficial effects on offline working memory in healthy individuals (118). Mertens attempted to replicate the positive effects of iVNS on word recognition memory using tVNS but found no improvement in word recognition memory in healthy individuals (119). Researchers speculated that this outcome might be related to the parametric design of the stimulation. Mariana compared Mertens’ parameter settings with those used in other papers that measured successful memory outcomes, indicating that the standard “off” interval length might be critical for modulating successful memory (120). Recent studies also suggest that tcVNS can improve attention, performance, and working memory (121).
There’s substantial research on the effects of tVNS on cognition, demonstrating that electrical stimulation can enhance cognitive abilities and increase cognitive control in healthy volunteers (122–124). Studies found that tVNS modulates conflict-induced cognitive control and action execution in behavioral and electroencephalogram data (125). There are varying perspectives on the impact of tVNS on cognitive flexibility. Tona et al. suggested that tVNS does not influence working flexibility (126). However, Borges remains optimistic about the potential of tVNS to influence cognitive flexibility. In his study, he compared the effects of tVNS on core executive functions, including inhibitory control and cognitive flexibility, and suggested that tVNS might have a stronger impact on cognitive flexibility than on inhibitory control (127). In recent research, tVNS has shown promising implications for neurocognitive functional recovery in elderly patients, effectively reducing the occurrence of delayed neurocognitive recovery (dnCR) after total joint arthroplasty (TJA) in the elderly (128). Effective results were observed in cognitive impairment patients by stimulating two ear acupoints related to the heart (auricle CO15) and kidney (CO10) (129). This provides evidence for tcVNS in slowing cognitive decline in the elderly and preventing dementia.
As Alzheimer’s disease is common among the elderly, the risk of carotid atherosclerotic plaques is relatively higher due to its specific nature (111). Vargas-Caballero et al. (120) mentioned in their article that the surgical implantation of iVNS devices into the cervical vagus nerve would involve manipulating the carotid arteries, increasing the risk of plaque rupture and leading to severe complications like cerebrovascular disease. While invasive vagus nerve stimulation and its potential for greater closed-loop interventions might be preferable clinically, non-invasive vagus nerve stimulation may be a better choice for treating Alzheimer’s disease (120). tVNS demonstrates certain effects on memory capabilities and cognition, has low costs, and high safety, making it a very promising treatment for Alzheimer’s disease, which mainly affects elderly patients. However, the effectiveness of tVNS as a treatment method requires further clinical trials.
3.6. Anxiety
VNS has been shown to alleviate anxiety symptoms, a finding initially observed in epilepsy patients. In addition to improving epilepsy and depression, iVNS has been found to significantly reduce anxiety levels (130). George et al. (131) reported that iVNS demonstrated notable efficacy in treatment-resistant obsessive-compulsive disorder (OCD), panic disorder, and post-traumatic stress disorder (PTSD) based on Hamilton Anxiety Rating Scale (HAM-A) scores. Furthermore, OCD patients showed significant improvements in Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) scores. Additionally, iVNS has been found beneficial in alleviating PTSD symptoms, effectively enhancing the extinction of conditioned fear (132, 133). The anxiolytic effects of iVNS appear to be frequency-dependent (134). In studies by Burger et al. (135), tVNS also accelerated fear extinction but did not lead to better retention of extinction memory after 24 h. However, Genheimer et al. (136) presented contrasting findings, as her study did not observe significant anxiety reduction with tVNS. Therefore, further research is necessary to clarify these effects.
3.7. Autism spectrum disorder
Initially, VNS was found to alter the behavior of children with epilepsy and ASD, including changes in alertness, mood, and communication styles. It also significantly improved various aspects of quality of life (137–139). Moreover, these behavioral and developmental improvements were found to be independent of epilepsy control, further demonstrating the potential of VNS in treating ASD (140). However, research related to ASD remains highly limited, and whether VNS provides benefits for children with ASD is still an open question.
3.8. Parkinson’s disease
In a study using nVNS to treat gait disturbances associated with Parkinson’s disease (PD), tcVNS improved gait parameters and alleviated freezing of gait (FOG) symptoms in PD patients. Significant reductions were observed in UPDRS III scores, with notable improvements in gait parameters such as walking speed, stride length, and step velocity (141). The number of steps required for turning was particularly reduced. Additionally, Farrand et al. (142) found that higher VNS frequencies contributed to behavioral improvements and attenuation of pathological markers in PD models. These findings suggest that VNS may be a potential therapeutic option for PD, although further studies are required to validate and optimize its application in PD treatment.
3.9. Migraine and cluster headache
Since some epilepsy patients also experience migraine symptoms, iVNS was initially found to improve migraine symptoms while alleviating epilepsy (143). Hord et al. (144) followed up with epilepsy patients undergoing iVNS treatment and similarly received positive feedback regarding iVNS’s efficacy in relieving migraine. Subsequently, iVNS was further demonstrated to be effective in alleviating chronic refractory migraine and cluster headache, although these studies involved small sample sizes (145, 146). Compared to iVNS, nVNS has attracted more attention. Both tcVNS and taVNS have been found to significantly relieve acute migraine, reduce headache days and attack frequency, lower pain intensity, and improve pain-free rates (147, 148). Studies on chronic cluster headache have shown that tcVNS can terminate pain within 11 ± 1 min (149). Additionally, nVNS has shown promising results in relieving acute cluster headaches, with sustained treatment potentially providing further benefits. However, in chronic cluster headache cohorts, tcVNS has not demonstrated significant advantages (150). Although increasing evidence suggests that VNS could bring significant benefits to patients with migraine or cluster headache, further high-quality studies are urgently needed.
4. Mechanisms of VNS in CNS disorders
Vagus nerve stimulation therapy demonstrates intricate mechanisms in its application for treating central nervous system disorders. Presently, the mechanisms of VNS in central nervous system disorders remain inconclusive, and research into its mechanisms is an ongoing exploration. This holds significant importance in expanding VNS applications within the central nervous system clinically. The mechanisms of VNS are associated with the anatomy of the vagus nerve. Vagus nerve fibers have four projection areas in the brainstem, including the nucleus ambiguus (NA) and dorsal motor nucleus (DMV) for the efferent branches of the vagus nerve, along with the nucleus tractus solitarii (NTS) and spinal trigeminal nucleus for incoming fibers (151). NTS acts as the primary relay station for vagus nerve input in the brain, receiving the most incoming vagus nerve signals. Moreover, this nucleus projects to various structures, such as periventricular gray matter, dorsal raphe nucleus, paraventricular nucleus of the thalamus, amygdala, and septum. When the vagus nerve receives external electrical stimulation, the incoming fibers get excited, and the incoming signal spreads from peripheral nerves to the NTS and locus coeruleus (LC), eventually propagating to subcortical structures (mainly the hippocampal region) and cortical structures (including the insular cortex, prefrontal cortex, and motor cortex) (152). Previous research analyses suggest that VNS primarily functions by inhibiting central inflammation, promoting neuroprotection, and enhancing cortical plasticity integrity.
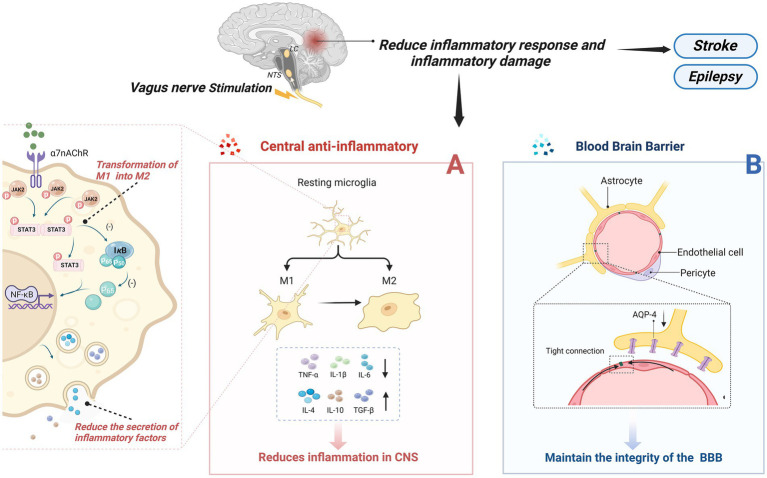
4.1. Suppression of central inflammation
Inflammation is a protective response of the body to external stimuli; however, excessive inflammation can lead to structural damage in brain function. Neuroinflammation is triggered by activated and proliferating microglia, astrocytes, and other myeloid cells, which produce pro-inflammatory cytokines, chemokines, and other inflammatory mediators, ultimately leading to neuronal damage (153). When a stroke occurs, a severe inflammatory response in the central nervous system damages neurons, and VNS’s central anti-inflammatory mechanism can alleviate this process. Several central nervous system diseases are closely associated with the occurrence of excessive inflammation, such as epilepsy and depression (154–156). The central anti-inflammatory effect of VNS has drawn significant attention and research from many scholars, with abundant and compelling evidence demonstrating its inhibitory role in inflammation. Its mechanisms primarily encompass three aspects (Figure 2): firstly, it can alter the phenotype of microglia cells; secondly, it reduces the secretion of inflammatory cytokines by activating the widespread α7nAchR receptors present in the CNS; and finally, it maintains the integrity of the blood–brain barrier, preventing inflammatory factors from damaging the central nervous system. The α7nAchR receptor is a crucial anti-inflammatory participant in the human body and is extensively expressed in the brain, including neurons, neuroglial cells, and endothelial cells. Activation of these receptors enhances the neurons’ resistance to ischemic or other types of injuries (157). Moreover, research indicates that VNS can induce an endogenous cholinergic anti-inflammatory pathway by increasing acetylcholine release through vagus nerve activation, subsequently activating α7nAchR receptors upon binding with acetylcholine (158).
Figure 2.
Central anti-inflammatory effect of VNS. (A) VNS changed microglia phenotype from M1 phenotype to M2 type; On the other hand, by activating the a7nAchR receptor, which is widely present in the CNS, the inflammatory cytokines secreted by pro-inflammatory cells are reduced. (B) Maintain the integrity of the blood-brain barrier and prevent the destruction of the central nervous system by inflammatory factors or other substances.
4.1.1. Alteration of microglial cell phenotype
As part of the homeostasis of the central nervous system, resting microglia maintain immune surveillance under physiological conditions. They have the ability to engulf pathogens and cellular debris that invade the brain and, under certain stimuli, transform into an activated phenotype to perform their function (159). Activated microglia undergo morphological changes and primarily exist in two phenotypes: the M1 phenotype, which secretes pro-inflammatory factors and induces self-perpetuating damage to neurons; and the M2 phenotype, which protects neurons and promotes recovery (160). Chen et al. found that tVNS induces a shift in the phenotype of microglial cells from the M1 polarized Iba-1/CD86 microglia to the M2 polarized Iba-1/CD206 microglia (161), enhancing the anti-inflammatory capacity of microglial cells. Additionally, the α7nAchR is identified as a critical target for altering the phenotype of microglial cells. In an Alzheimer’s disease model, tcVNS significantly shifted the phenotype of microglial cells from neurodestructive to neuroprotective, increasing the release of BDNF, basic fibroblast growth factor (bFGF), anti-inflammatory cytokines (IL-4, IL-10, TGF-β), and decreasing the release of pro-inflammatory cytokines (IL-1β, IL-6, TNF-α), ultimately delaying cognitive decline (162). Zhang et al.’s research (163) suggests that the JAK2/STAT3 pathway might be a downstream pathway of α7nAChR. Activation of α7nAChR by ACh through this pathway promotes the transformation of M1 microglial cells into the M2 phenotype.
4.1.2. Reduction of the secretion of inflammatory cytokines
Reducing Inflammatory Factors with VNS is also related to the activation of α7nAchR on microglial cells. The activation of α7nAchR on microglial cells may provide neuronal protection in vitro under conditions of hypoxia and glucose deprivation, reducing the inflammatory response to ischemic damage (164). Studies have shown that after 24 h of vascular occlusion in I/R mice, VNS activated α7nAchR on microglial cells, reducing levels of inflammatory cytokines (TNF-α, IL-1β, and IL-6), while accompanied by an increase in anti-inflammatory cytokines (IL-4, IL-10, TGF-β), thus safeguarding neuronal functional recovery following acute brain injury (162, 165, 166). Lu et al. (167) suggested that VNS’s post-stroke anti-inflammatory effect might involve the activation of α7nAChR on microglial cells, amplifying the levels of phosphorylated signal transducer and activator of transcription 3 (p-STAT3) and Janus kinase 2 (JAK2). Increased phosphorylation of both inhibits the NF-κB pathway, reducing the production of pro-inflammatory cytokines (168). In a mouse model of brain ischemia, Jiang et al. found that VNS might upregulate the expression of peroxisome proliferator-activated receptor gamma [PPARγ, a ligand-activated transcription factor that plays a positive anti-inflammatory and neuroprotective role during CNS inflammation (169)] by activating α7nAChR, thereby suppressing inflammatory factors in the CNS and exerting an anti-inflammatory effect (170). Further evidence supports the crucial role of α7nAChR in VNS’s reduction of inflammatory factors. Similarly, tVNS can upregulate the expression of α7nAchR on hippocampal microglial cells. α7nAchR prevents the expression of phosphorylated-p65 and nuclear translocation of the NF-κB pathway, thereby regulating the expression of pro-inflammatory cytokines, alleviating depressive symptoms (171).
4.1.3. Maintenance of blood–brain barrier integrity
Maintaining the integrity of the blood–brain barrier (BBB) is crucial for the stability of the central nervous system (CNS) as it effectively prevents certain substances, mostly harmful, from entering the brain from the bloodstream, thus playing a pivotal role in mitigating CNS inflammatory reactions post-stroke (172). Additionally, increased BBB permeability is often associated with inflammation-related neurodegenerative changes (173). Current research suggests that Vagus Nerve Stimulation can improve the integrity of the BBB, reducing its permeability, thereby preventing inflammatory factors from entering the CNS, effectively alleviating symptoms in mice with cortical microinfarcts (CMI) (174). However, the specific mechanisms by which VNS regulates BBB permeability remain unclear. Some researchers suggest that Vagus Nerve Stimulation lowers brain vascular permeability, possibly by preventing the upregulation of Aquaporin-4 (AQP-4) around blood vessels (175). Others propose the presence of nerve terminals around the BBB (potentially including cholinergic and noradrenergic terminals), and activation of α7nAchR may reduce BBB permeability. This suggests that VNS might transmit signals to the BBB through these peripheral cholinergic and noradrenergic terminals (176). Another potential mechanism involves immune regulation in the brain microenvironment. VNS could reduce the expression of Matrix Metalloproteinases-2/9 (MMP-2/9) in astrocytes while safeguarding vascular endothelial cadherin from microvascular damage (177). Jin et al. (178) proposed a new hypothesis stating that VNS enhances the concentration of neurotrophic factors within the brain (such as BDNF), potentially serving as a protective mechanism for the BBB.
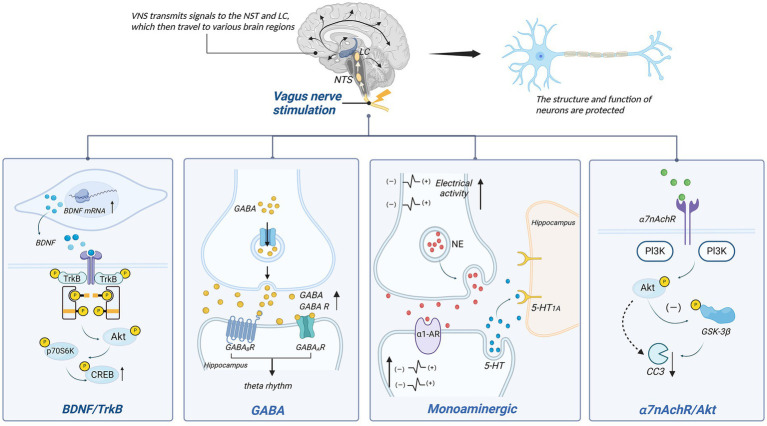
4.2. Promotion of neuroprotection
Previous research indicates that the vagus nerve plays a significant role in neuroprotection (Figure 3). Various neuroprotective pathways of Vagus Nerve Stimulation (VNS) have been discovered, including the release of neurotrophic factors, modulation of neurotransmitters, and improvement in cerebral vascular regeneration.
Figure 3.
Neuronal protection of VNS. p70S6K, p70 ribosomal protein S6 kinase kinases; CREB, cAMP-responsive element-binding protein; PI3K, phosphatidylinositol 3-kinase; NE, norepinephrine; α1-AR, α1-norepinephrine receptors; GSK-3β, glycogen synthase kinase-3β; CC3, cleaved caspase 3.
4.2.1. BDNF/TrkB
Vagus Nerve Stimulation therapy for depression is closely linked to the BDNF/TrkB signaling pathway. BDNF, a brain-derived neurotrophic factor, protects neurons by enhancing synaptic plasticity, inhibiting cell apoptosis, and promoting nerve regeneration. Tyrosine receptor kinase B (TrkB) serves as the primary receptor for BDNF. The BDNF/TrkB signaling pathway has been shown to be closely associated with the occurrence and development of various brain disorders (179). In individuals with mood disorders, notably, BDNF levels are significantly reduced, while antidepressants can increase BDNF expression and signaling (180). The mechanism behind VNS’s effect on depression may be linked to this signaling pathway.
Studies have indicated a close relationship between the vagus nerve and BDNF. When the vagus nerve is severed, hippocampal BDNF mRNA expression decreases, leading to diminished neuronal changes (181). Research by Follesa et al. (182) demonstrated increased BDNF expression in the hippocampus and cerebral cortex of rats after just 3 h of VNS. This effect is also observed in chronic VNS, where the hippocampal cell proliferation increases, and there are sustained alterations in neuronal dendritic complexity (183). Recent findings suggest that when α7nAchR is blocked, the activity in the BDNF pathway is inhibited, supporting the notion that α7nAchR might mediate VNS’s effects on BDNF (184).
TrkB also plays a role in this context. Following vagus nerve stimulation, phosphorylation occurs at tyrosine 705, 816, and 515 on the hippocampal TrkB receptor. Blocking the TrkB receptor significantly diminishes or even eliminates the therapeutic effects of VNS (185). Phosphorylation at tyrosine 705 facilitates the regulation of other tyrosines and their activation (186). Phosphorylation at tyrosine 515 leads to the activation of Ras/MAPK and PI3K signaling pathways, while phosphorylation at tyrosine 816 induces survival signal transduction mediated by phospholipase C-γ1 (PLC-γ1), inducing neuroprotection (187). Carreno et al. (188) further identified downstream factors of Y515, including Akt and p70 ribosomal protein S6 kinase (p70S6k), ultimately resulting in the phosphorylation of cAMP-response element-binding protein (CREB). Additionally, experimental evidence has confirmed the ligand-dependent activation of TrkB (189). This indicates that both BDNF and TrkB are indispensable components in the VNS mechanism for treating depression, and the BDNF/TrkB signaling pathway plays a crucial role in VNS’s antidepressant effects.
4.2.2. Monoaminergic neurotransmitter
Monoamine neurotransmitters encompass norepinephrine (NE), dopamine (DA), and serotonin (5-HT). The mechanism by which VNS improves treatment-resistant depression might be associated with increased baseline discharge activity of norepinephrine (NE) neurons in the LC, enhancing noradrenergic output (190). It’s also related to the increase in 5-HT in the dorsal raphe nucleus (DRN) after 14 days (191). This effect is similar to the desensitization of the 5-HT1A autoreceptor observed after antidepressant use, which restores the normal firing rate of 5-HT neurons in the DRN (192). Moreover, VNS’s anti-anxiety and antidepressant effects rely mainly on 5-HT neurons (193). However, changes in 5-HT1A autoreceptor sensitivity have not been observed after VNS, suggesting that its impact on 5-HT neuron discharge is indirect (154).
Studies suggest that NE might act as an intermediary, enhancing 5-HT neuron discharge by increasing excitability via α1-adrenergic receptor stimulation in the DRN (154). Liu et al. observed diminished efficacy of VNS when noradrenergic neurons were inactivated, further supporting the role of NE as an intermediary (194). Although VNS notably increases extracellular 5-HT levels in the DRN, similar changes were not observed in two postsynaptic structures, the hippocampus and prefrontal cortex (195). Nonetheless, VNS has been shown to enhance the straight activation of 5-HT1A postsynaptic receptors in these regions, likely contributing to augmented serotonergic neurotransmission in the forebrain (154). Research indicates that VNS exhibits antidepressant effects by increasing NE concentrations in the periphery, thalamus, and cortical regions (196). Manta et al. (195) found that long-term VNS not only affects extracellular 5-HT levels but also increases extracellular DA levels detected in the prefrontal cortex (PFC) and nucleus accumbens (NAc), potentially aiding in alleviating depressive symptoms.
VNS’s inhibition of epileptic seizures is also linked to hippocampal and cortical NE concentrations (197). By activating NE neuron excitability, VNS significantly increases NE release in LC projection areas (including the hippocampus and prefrontal cortex) (182), impacting the diminished VNS-induced seizure inhibition. Recent studies corroborate this view, demonstrating that VNS, by increasing activity in noradrenergic neurons in the LC, elevates arousal and causes widespread, uneven cortical activation in epilepsy patients, influencing their sleep–wake states (198). This NE-dependent modulation is likely mediated by α-adrenergic receptors since their activation can suppress epileptiform activity. In a model of pentylenetetrazole-induced seizures in rats, blockade of α2-adrenergic receptors in the hippocampus reversed VNS’s attenuating effect on seizures (197). Recent mouse experiments also underscore the importance of α-adrenergic receptors in inhibiting seizures (199).
4.2.3. GABA
GABA, an inhibitory neurotransmitter, plays a crucial role in the overall control and fine-tuning of excitatory transmission and is associated with various brain disorders (200). It is primarily distributed in the nucleus tractus solitarii (NTS), dorsal motor nucleus of the vagus nerve (DMV), medial septum (MS), and hippocampus (200, 201).
The NTS is a primary medullary site where vagus nerve afferents terminate. Vagus nerve stimulation can enhance GABA release by activating the NTS (202). The GABA system plays a significant role in epilepsy treatment, as observed in patients receiving VNS, where there is a notable increase in total GABA and free GABA levels in the cerebrospinal fluid (203). Within the NTS, γ-aminobutyric acid operates through GABA receptors for inhibitory control. VNS increases inhibition of NTS output via GABA transmission, reducing susceptibility to chemically induced reflex epileptic seizures (204). Marrosu et al. (205) suggested that VNS plays a role in modulating cortical excitability related to epilepsy, associated with the normalization of cortical GABAA receptor density.
Vagus nerve stimulation might impact memory by enhancing neuroplasticity in brain structures associated with memory storage (206). Studies link this memory processing to increased excitability in hippocampal neuron networks and the presence of local theta rhythms (207, 208). Broncel’s research indicated that GABAA and GABAB receptors in the MS (medial septum, a candidate for vagus nerve input from the NTS to hippocampal structures) are involved in regulating hippocampal theta rhythms induced by VNS, closely associated with anxiety behaviors and learning-memory capabilities (208).
Thus, vagus nerve stimulation influences the central nervous system through the GABA system. Additionally, consistently low GABA levels have been found in brain regions responsible for emotional cognitive processes in depression patients, such as the prefrontal cortex, posterior cingulate cortex, anterior cingulate cortex, and amygdala (209). Therefore, it’s speculated that part of VNS’s therapeutic effects on depression might involve the GABA system.
4.2.4. α7nAchR/Akt
Akt, also known as protein kinase B, has diverse roles in the nervous system, playing a crucial part in cell development, function, and survival processes. Phosphorylated Akt (p-Akt) can activate downstream cysteine aspartate-specific proteases, reducing cleaved caspase-3 (CC3), thereby exerting a cell-protective effect (210). Studies by Krafft et al. (211) demonstrated that in a mouse model of cerebral hemorrhage, activation of α7nAchR reduces neuronal cell death by increasing p-Akt and lowering CC3 expression. Moreover, in a mouse model of cerebral ischemia, VNS-induced α7nAchR activation increased p-Akt while reducing cleaved caspase expression in the brain, ultimately reducing neuronal cell death (165). Furthermore, Akt phosphorylation depends on the phosphoinositide 3-kinase (PI3K) signaling pathway (212). Vagus nerve stimulation has been shown to decrease cardiomyocyte apoptosis through the PI3K/Akt signaling pathway (213), indirectly indicating that PI3K may serve as an intermediary in the α7nAchR/Akt pathway. However, further related research is required to confirm this relationship.
4.3. Increase of cortical plasticity
Vagus nerve stimulation has been confirmed to produce widespread excitatory effects in various cortical regions, prompting exploration into induced cortical neuroplasticity. In the sensory and motor systems, temporarily pairing VNS with sensory stimulation or movement reorganizes neural circuits associated with sensation and movement networks (214). The cholinergic system in the basal forebrain (214, 215) and activation of the noradrenergic system in the locus coeruleus (216) may play important roles in this neural circuitry reshaping. This involves increased activity in noradrenergic neurons in the LC and cholinergic neurons in the basal forebrain (BF), which are a source of cortical-projecting cholinergic neurons (198, 217). VNS induces acetylcholine release in the basal forebrain and modulates neural activity in the BF, playing a critical role in the cortex (215). Impaired cholinergic projection in the basal forebrain cortex leads to a loss of motor network plasticity (218), while excitability and synchrony in the auditory cortex are disrupted upon blocking muscarinic receptors in the auditory cortex (219).
The sensory system comprises two pathways: the feedback (FB) and feedforward (FF) pathways. The superficial layers of the primary sensory cortex act as the hub for the feedforward (FF) pathway, while the deeper layers serve as the hub for the feedback (FB) pathway. Acetylcholine and norepinephrine, respectively, modulate the FF and FB pathways (220, 221). In the study by Kumagai et al. (199), VNS primarily activated the FF pathway within the sensory system rather than the FB pathway. This indicates that VNS-induced neural regulation can alter the FF-FB balance in the auditory cortex, known as neural gain, and the regulation of FF-FB balance induced by VNS may contribute to various clinical outcomes.
5. Pupil dilation may be a sensitive readout of VNS effects on brain states
In the cortex, the activity of basal forebrain cholinergic and local noradrenergic axons can be sensitively tracked by pupillary dilation (222). Furthermore, under constant brightness, pupillary dilation can read out the brain state characteristics of the mouse cortex and hippocampus sensitively and non-invasively (223). As a result, some scholars propose pupillary dilation as a sensitive biosensor for the titration effects of VNS-induced brain neuromodulation states. The amplitude of VNS-induced pupillary dilation corresponds to its stimulation parameters, and this VNS-induced pupillary dilation is mediated by acetylcholine released from the basal forebrain to the neocortex network, interacting nonlinearly with the current momentary brain state (214). However, there is still limited research in this area, and whether pupillary dilation is the most suitable representation of VNS stimulation is yet to be determined. Nevertheless, it’s a promising avenue to explore and provides direction for research on vagus nerve stimulation.
6. Conclusion
In conclusion, VNS is a promising therapeutic approach for central nervous system disorders. In addition to its officially approved applications for the treatment of refractory epilepsy and depression, accumulating evidence suggests that VNS may also provide benefits to patients with Alzheimer’s disease, stroke, disorders of consciousness, anxiety, Parkinson’s disease, autism spectrum disorder, migraines, and cluster headaches. Both iVNS and tcVNS can stimulate the vagus nerve (VN) at the carotid sheath and have demonstrated promising results in the treatment of various CNS diseases. However, the effects of taVNS, such as in anxiety disorders, remain controversial and certainly require further research for validation. Furthermore, research should be refined and personalized to address the specific pathological mechanisms of different CNS diseases. Each patient’s bio-psycho-social background should be considered, as this helps provide a more comprehensive and effective treatment strategy. Recent studies indicate that VNS predominantly affects the CNS by inhibiting central inflammation, promoting neuroprotection, and enhancing cortical plasticity. Altering the phenotype of CNS microglial cells, reducing pro-inflammatory factors, and maintaining blood–brain barrier permeability can suppress the intensity of CNS inflammation, thereby reducing damage to brain tissues. Protection of neurons is mainly mediated through modulation of neurotrophic factors or neurotransmitters. However, there are still several challenges in this field. Firstly, VNS often serves as an adjunct or complementary therapy for CNS diseases, and the quality of related literature varies significantly, including differences in sample size and observed indicators. Moreover, optimal stimulation protocols for specific CNS diseases or diverse populations are scarce, limiting its broader application and clinical efficacy. Expanding the indications for VNS and determining the best stimulation protocols require more high-quality research. Secondly, predicting the effectiveness of VNS for various CNS diseases is in its infancy, which poses barriers to targeted treatment. Finally, the precise mechanism of VNS’s therapeutic effect remains unclear. Existing research mostly focuses on the factors influenced by VNS rather than investigating its primary action, severely limiting the expansion of VNS into other CNS diseases. Understanding how VNS interacts with neural circuits could identify new stimulation targets. Therefore, future VNS research will prioritize addressing these issues.
Glossary
Glossary
- α7nAChR
α7 Nicotinic Acetylcholine Receptor
- ABVN
Auricular Branch of the Vagus Nerve
- AD
Alzheimer’s Disease
- ADAS-cog
Alzheimer’s Disease Assessment Scale-Cognitive Subscale
- Akt
Protein Kinase B
- AQP-4
Aquaporin-4
- ASD
Autism Spectrum Disorder
- ASMs
Antiseizure Medications
- BBB
Blood–brain barrier
- BDNF
Brain-Derived Neurotrophic Factor
- bFGF
Basic Fibroblast Growth Factor
- CGI
Clinical Global Impression
- CIBIC+
Clinician’s Interview-Based Impression of Change
- CNS
Central Nervous System
- CRS-R
Coma Recovery Scale-Revised
- DA
Dopamine
- DOC
Disorders of Consciousness
- DRN
Dorsal Raphe Nucleus
- DRE
Drug-resistant Epilepsy
- EEG
Electroencephalograms
- FDA
Food and Drug Administration
- FNAME
Face-Name Associative Memory Exam
- FOG
Freezing of Gait
- HAM-A
Hamilton Anxiety Rating Scale
- HRS-D-28
28-item Hamilton Rating Scale for Depression
- JAK2
Janus Kinase 2
- LC
Locus Coeruleus
- MADRS
Montgomery-Åsberg Depression Rating Scale
- MCS
Minimally Conscious State
- eMCS
Emergence from MCS to higher levels of consciousness
- MMP
Matrix Metalloproteinases
- MMSE
Mini-Mental State Examination
- MS
Medial Septum
- NAc
Nucleus Accumbens
- NE
Norepinephrine
- NICE
National Institute for Health and Care Excellence
- NTS
Nucleus Tractus Solitarii
- OCD
Obsessive-Compulsive Disorder
- PD
Parkinson’s Disease
- PET
Positron Emission Tomography
- PFC
Prefrontal Cortex
- PI3K
Phosphoinositide 3-Kinase
- PTSD
Post-Traumatic Stress Disorder
- TrkB
Tropomyosin Receptor Kinase B
- UPDRS III
Unified Parkinson’s Disease Rating Scale, Part III
- VNS
Vagus Nerve Stimulation
- iVNS
Implantable Vagus Nerve Stimulation
- nVNS
Non-invasive Vagus Nerve Stimulation
- tVNS
Transcutaneous Vagus Nerve Stimulation
- taVNS
Transcutaneous Auricular Vagus Nerve Stimulation
- tcVNS
Transcutaneous Cervical Vagus Nerve Stimulation
- VS/UWS
Vegetative State/Unresponsive Wakefulness Syndrome
- WMFT
Wolf Motor Function Test
- Y-BOCS
Yale-Brown Obsessive-Compulsive Scale
Funding Statement
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Author contributions
CW: Data curation, Writing – original draft. BW: Conceptualization, Supervision, Validation, Writing – review & editing. RL: Conceptualization, Validation, Writing – original draft. YPC: Conceptualization, Methodology, Writing – review & editing. JH: Data curation, Software, Validation, Writing – review & editing. YYC: Conceptualization, Software, Writing – review & editing. JB: Data curation, Validation, Writing – original draft.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Lanska DJ. J.L. corning and vagal nerve stimulation for seizures in the 1880s. Neurology. (2002) 58:452–9. doi: 10.1212/wnl.58.3.452, PMID: [DOI] [PubMed] [Google Scholar]
- 2.Penry JK, Dean JC. Prevention of intractable partial seizures by intermittent vagal stimulation in humans: preliminary results. Epilepsia. (1990) 31:S40–3. doi: 10.1111/j.1528-1157.1990.tb05848.x, PMID: [DOI] [PubMed] [Google Scholar]
- 3.Ben-Menachem E. Vagus-nerve stimulation for the treatment of epilepsy. Lancet Neurol. (2002) 1:477–82. doi: 10.1016/s1474-4422(02)00220-x [DOI] [PubMed] [Google Scholar]
- 4.Silberstein SD, Calhoun AH, Lipton RB, Grosberg BM, Cady RK, Dorlas S, et al. Chronic migraine headache prevention with noninvasive vagus nerve stimulation: the EVENT study. Neurology. (2016) 87:529–38. doi: 10.1212/wnl.0000000000002918, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aaronson ST, Sears P, Ruvuna F, Bunker M, Conway CR, Dougherty DD, et al. A 5-year observational study of patients with treatment-resistant depression treated with vagus nerve stimulation or treatment as usual: comparison of response, remission, and suicidality. Am J Psychiatry. (2017) 174:640–8. doi: 10.1176/appi.ajp.2017.16010034, PMID: [DOI] [PubMed] [Google Scholar]
- 6.Giordano F, Zicca A, Barba C, Guerrini R, Genitori L. Vagus nerve stimulation: surgical technique of implantation and revision and related morbidity. Epilepsia. (2017) 58:85–90. doi: 10.1111/epi.13678 [DOI] [PubMed] [Google Scholar]
- 7.Wong S, Mani R, Danish S. Comparison and selection of current implantable anti-epileptic devices. Neurotherapeutics. (2019) 16:369–80. doi: 10.1007/s13311-019-00727-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nicolai EN, Larco JA, Madhani SI, Asirvatham SJ, Chang SY, Ludwig KA, et al. Vagus nerve stimulation using an endovascular electrode array. J Neural Eng. (2023) 20:046008. doi: 10.1088/1741-2552/acdb9b, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tatum WO, Moore DB, Stecker MM, Baltuch GH, French JA, Ferreira JA, et al. Ventricular asystole during vagus nerve stimulation for epilepsy in humans. Neurology. (1999) 52:1267–9. doi: 10.1212/wnl.52.6.1267 [DOI] [PubMed] [Google Scholar]
- 10.Fahy BG. Intraoperative and perioperative complications with a vagus nerve stimulation device. J Clin Anesth. (2010) 22:213–22. doi: 10.1016/j.jclinane.2009.10.002, PMID: [DOI] [PubMed] [Google Scholar]
- 11.Clark AJ, Kuperman RA, Auguste KI, Sun PP. Intractable episodic bradycardia resulting from progressive lead traction in an epileptic child with a vagus nerve stimulator: a delayed complication. J Neurosurg Pediatr. (2012) 9:389–93. doi: 10.3171/2011.12.Peds11124, PMID: [DOI] [PubMed] [Google Scholar]
- 12.Murphy JV. Left vagal nerve stimulation in children with medically refractory epilepsy. J Pediatr. (1999) 134:563–6. doi: 10.1016/s0022-3476(99)70241-6 [DOI] [PubMed] [Google Scholar]
- 13.Tran Y, Shah AK, Mittal S. Lead breakage and vocal cord paralysis following blunt neck trauma in a patient with vagal nerve stimulator. J Neurol Sci. (2011) 304:132–5. doi: 10.1016/j.jns.2011.02.022, PMID: [DOI] [PubMed] [Google Scholar]
- 14.Yap JYY, Keatch C, Lambert E, Woods W, Stoddart PR, Kameneva T. Critical review of transcutaneous vagus nerve stimulation: challenges for translation to clinical practice. Front Neurosci. (2020) 14:284. doi: 10.3389/fnins.2020.00284, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Agnew WF, McCreery DB. Considerations for safety with chronically implanted nerve electrodes. Epilepsia. (1990) 31:S27–32. doi: 10.1111/j.1528-1157.1990.tb05845.x, PMID: [DOI] [PubMed] [Google Scholar]
- 16.Schneider UC, Bohlmann K, Vajkoczy P, Straub HB. Implantation of a new vagus nerve stimulation (VNS) therapy® generator, AspireSR®: considerations and recommendations during implantation and replacement surgery--comparison to a traditional system. Acta Neurochir. (2015) 157:721–8. doi: 10.1007/s00701-015-2362-3, PMID: [DOI] [PubMed] [Google Scholar]
- 17.Mertens A, Raedt R, Gadeyne S, Carrette E, Boon P, Vonck K. Recent advances in devices for vagus nerve stimulation. Expert Rev Med Devices. (2018) 15:527–39. doi: 10.1080/17434440.2018.1507732 [DOI] [PubMed] [Google Scholar]
- 18.Butt MF, Albusoda A, Farmer AD, Aziz Q. The anatomical basis for transcutaneous auricular vagus nerve stimulation. J Anat. (2020) 236:588–611. doi: 10.1111/joa.13122, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peuker ET, Filler TJ. The nerve supply of the human auricle. Clin Anat. (2002) 15:35–7. doi: 10.1002/ca.1089 [DOI] [PubMed] [Google Scholar]
- 20.Yakunina N, Kim SS, Nam EC. Optimization of transcutaneous vagus nerve stimulation using functional MRI. Neuromodulation. (2017) 20:290–300. doi: 10.1111/ner.12541, PMID: [DOI] [PubMed] [Google Scholar]
- 21.Ben-Menachem E, Revesz D, Simon BJ, Silberstein S. Surgically implanted and non-invasive vagus nerve stimulation: a review of efficacy, safety and tolerability. Eur J Neurol. (2015) 22:1260–8. doi: 10.1111/ene.12629, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen M, Yu L, Ouyang F, Liu Q, Wang Z, Wang S, et al. The right side or left side of noninvasive transcutaneous vagus nerve stimulation: based on conventional wisdom or scientific evidence? Int J Cardiol. (2015) 187:44–5. doi: 10.1016/j.ijcard.2015.03.351 [DOI] [PubMed] [Google Scholar]
- 23.Hein E, Nowak M, Kiess O, Biermann T, Bayerlein K, Kornhuber J, et al. Auricular transcutaneous electrical nerve stimulation in depressed patients: a randomized controlled pilot study. J Neural Transm. (2013) 120:821–7. doi: 10.1007/s00702-012-0908-6, PMID: [DOI] [PubMed] [Google Scholar]
- 24.He W, Jing X, Wang X, Rong P, Li L, Shi H, et al. Transcutaneous auricular vagus nerve stimulation as a complementary therapy for pediatric epilepsy: a pilot trial. Epilepsy Behav. (2013) 28:343–6. doi: 10.1016/j.yebeh.2013.02.001, PMID: [DOI] [PubMed] [Google Scholar]
- 25.Uthman BM, Wilder BJ, Penry JK, Dean C, Ramsay RE, Reid SA, et al. Treatment of epilepsy by stimulation of the vagus nerve. Neurology. (1993) 43:1338–45. doi: 10.1212/wnl.43.7.1338 [DOI] [PubMed] [Google Scholar]
- 26.Ben-Menachem E, Mañon-Espaillat R, Ristanovic R, Wilder BJ, Stefan H, Mirza W, et al. Vagus nerve stimulation for treatment of partial seizures: 1. A controlled study of effect on seizures. First international vagus nerve stimulation study group. Epilepsia. (1994) 35:616–26. doi: 10.1111/j.1528-1157.1994.tb02482.x, PMID: [DOI] [PubMed] [Google Scholar]
- 27.Fisher RS, Krauss GL, Ramsay E, Laxer K, Gates J. Assessment of vagus nerve stimulation for epilepsy: report of the therapeutics and technology assessment Subcommittee of the American Academy of Neurology. Neurology. (1997) 49:293–7. doi: 10.1212/wnl.49.1.293, PMID: [DOI] [PubMed] [Google Scholar]
- 28.Fisher RS, Handforth A. Reassessment: vagus nerve stimulation for epilepsy: a report of the therapeutics and technology assessment subcommittee of the American Academy of Neurology. Neurology. (1999) 53:666–9. doi: 10.1212/wnl.53.4.666, PMID: [DOI] [PubMed] [Google Scholar]
- 29.Morris GL, 3rd, Gloss D, Buchhalter J, Mack KJ, Nickels K, Harden C. Evidence-based guideline update: vagus nerve stimulation for the treatment of epilepsy: report of the guideline development Subcommittee of the American Academy of Neurology. Neurology. (2013) 81:1453–9. doi: 10.1212/WNL.0b013e3182a393d1, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kuba R, Brázdil M, Kalina M, Procházka T, Hovorka J, Nežádal T, et al. Vagus nerve stimulation: longitudinal follow-up of patients treated for 5 years. Seizure. (2009) 18:269–74. doi: 10.1016/j.seizure.2008.10.012, PMID: [DOI] [PubMed] [Google Scholar]
- 31.Boluk C, Ozkara C, Isler C, Uzan M. Vagus nerve stimulation in intractable epilepsy. Turk Neurosurg. (2021) 32:97–102. doi: 10.5137/1019-5149.Jtn.33775-21.2 [DOI] [PubMed] [Google Scholar]
- 32.Ramsay RE, Uthman BM, Augustinsson LE, Upton ARM, Naritoku D, Willis J, et al. Vagus nerve stimulation for treatment of partial seizures: 2. Safety, side effects, and tolerability. First international vagus nerve stimulation study group. Epilepsia. (1994) 35:627–36. doi: 10.1111/j.1528-1157.1994.tb02483.x, PMID: [DOI] [PubMed] [Google Scholar]
- 33.Toffa DH, Touma L, El Meskine T, Bouthillier A, Nguyen DK. Learnings from 30 years of reported efficacy and safety of vagus nerve stimulation (VNS) for epilepsy treatment: a critical review. Seizure. (2020) 83:104–23. doi: 10.1016/j.seizure.2020.09.027, PMID: [DOI] [PubMed] [Google Scholar]
- 34.Boon P, Vonck K, D'Have M, O'Connor S, Vandekerckhove T, de Reuck J. Cost-benefit of vagus nerve stimulation for refractory epilepsy. Acta Neurol Belg. (1999) 99:275–80. PMID: [PubMed] [Google Scholar]
- 35.Purser MF, Mladsi DM, Beckman A, Barion F, Forsey J. Expected budget impact and health outcomes of expanded use of vagus nerve stimulation therapy for drug-resistant epilepsy. Adv Ther. (2018) 35:1686–96. doi: 10.1007/s12325-018-0775-0, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Burke T, Hughes D, Forsey J, Bunker M, Bhattacharya D, Smithson WH. A study of the impact of VNS on health care utilisation in England. Seizure. (2016) 34:12–7. doi: 10.1016/j.seizure.2015.11.002, PMID: [DOI] [PubMed] [Google Scholar]
- 37.Evans K, Stamas N, Li Q, Vincent T, Halchenko Y, Zhang L, et al. Impact of vagus nerve stimulation for the treatment of drug-resistant epilepsy on patterns of use and cost of health care services and pharmacotherapy: comparisons of the 24-month periods before and after implantation. Clin Ther. (2023) 45:136–50. doi: 10.1016/j.clinthera.2023.01.007, PMID: [DOI] [PubMed] [Google Scholar]
- 38.Suller Marti A, Mirsattari SM, MacDougall K, Steven DA, Parrent A, de Ribaupierre S, et al. Vagus nerve stimulation in patients with therapy-resistant generalized epilepsy. Epilepsy Behav. (2020) 111:107253. doi: 10.1016/j.yebeh.2020.107253 [DOI] [PubMed] [Google Scholar]
- 39.Shahwan A, Bailey C, Maxiner W, Harvey AS. Vagus nerve stimulation for refractory epilepsy in children: more to VNS than seizure frequency reduction. Epilepsia. (2009) 50:1220–8. doi: 10.1111/j.1528-1167.2008.01940.x [DOI] [PubMed] [Google Scholar]
- 40.Orosz I, McCormick D, Zamponi N, Varadkar S, Feucht M, Parain D, et al. Vagus nerve stimulation for drug-resistant epilepsy: a European long-term study up to 24 months in 347 children. Epilepsia. (2014) 55:1576–84. doi: 10.1111/epi.12762, PMID: [DOI] [PubMed] [Google Scholar]
- 41.Soleman J, Stein M, Knorr C, Datta AN, Constantini S, Fried I, et al. Improved quality of life and cognition after early vagal nerve stimulator implantation in children. Epilepsy Behav. (2018) 88:139–45. doi: 10.1016/j.yebeh.2018.09.014, PMID: [DOI] [PubMed] [Google Scholar]
- 42.Parker AP, Polkey CE, Robinson RO. Vagal nerve stimulation in the epileptic encephalopathies: 3-year follow-up. Pediatrics. (2001) 108:221. doi: 10.1542/peds.108.1.221, PMID: [DOI] [PubMed] [Google Scholar]
- 43.Murphy JV, Wheless JW, Schmoll CM. Left vagal nerve stimulation in six patients with hypothalamic hamartomas. Pediatr Neurol. (2000) 23:167–8. doi: 10.1016/s0887-8994(00)00170-3, PMID: [DOI] [PubMed] [Google Scholar]
- 44.Parain D, Penniello MJ, Berquen P, Delangre T, Billard C, Murphy JV. Vagal nerve stimulation in tuberous sclerosis complex patients. Pediatr Neurol. (2001) 25:213–6. doi: 10.1016/s0887-8994(01)00312-5 [DOI] [PubMed] [Google Scholar]
- 45.Parker AP, Polkey CE, Binnie CD, Madigan C, Ferrie CD, Robinson RO. Vagal nerve stimulation in epileptic encephalopathies. Pediatrics. (1999) 103:778–82. doi: 10.1542/peds.103.4.778 [DOI] [PubMed] [Google Scholar]
- 46.Frost M, Gates J, Helmers SL, Wheless JW, Levisohn P, Tardo C, et al. Vagus nerve stimulation in children with refractory seizures associated with Lennox-Gastaut syndrome. Epilepsia. (2001) 42:1148–52. doi: 10.1046/j.1528-1157.2001.23900.x, PMID: [DOI] [PubMed] [Google Scholar]
- 47.Wilfong AA, Schultz RJ. Vagus nerve stimulation for treatment of epilepsy in Rett syndrome. Dev Med Child Neurol. (2006) 48:683–6. doi: 10.1017/s0012162206001435, PMID: [DOI] [PubMed] [Google Scholar]
- 48.Major P, Thiele EA. Vagus nerve stimulation for intractable epilepsy in tuberous sclerosis complex. Epilepsy Behav. (2008) 13:357–60. doi: 10.1016/j.yebeh.2008.04.001 [DOI] [PubMed] [Google Scholar]
- 49.Dibué-Adjei M, Fischer I, Steiger HJ, Kamp MA. Efficacy of adjunctive vagus nerve stimulation in patients with Dravet syndrome: a meta-analysis of 68 patients. Seizure. (2017) 50:147–52. doi: 10.1016/j.seizure.2017.06.007, PMID: [DOI] [PubMed] [Google Scholar]
- 50.Elliott RE, Rodgers SD, Bassani L, Morsi A, Geller EB, Carlson C, et al. Vagus nerve stimulation for children with treatment-resistant epilepsy: a consecutive series of 141 cases. J Neurosurg Pediatr. (2011) 7:491–500. doi: 10.3171/2011.2.Peds10505 [DOI] [PubMed] [Google Scholar]
- 51.Houser MV, Hennessy MD, Howard BC. Vagal nerve stimulator use during pregnancy for treatment of refractory seizure disorder. Obstet Gynecol. (2010) 115:417–9. doi: 10.1097/AOG.0b013e3181bd1a8b, PMID: [DOI] [PubMed] [Google Scholar]
- 52.Suller Marti A, Mirsattari SM, Steven DA, Parrent AG, MacDougall KW, McLachlan RS, et al. Experience on the use of vagus nerve stimulation during pregnancy. Epilepsy Res. (2019) 156:106186. doi: 10.1016/j.eplepsyres.2019.106186, PMID: [DOI] [PubMed] [Google Scholar]
- 53.Sabers A, Battino D, Bonizzoni E, Craig J, Lindhout D, Perucca E, et al. Maternal and fetal outcomes associated with vagus nerve stimulation during pregnancy. Epilepsy Res. (2017) 137:159–62. doi: 10.1016/j.eplepsyres.2017.05.013 [DOI] [PubMed] [Google Scholar]
- 54.Ding J, Wang L, Wang C, Gao C, Wang F, Sun T. Is vagal-nerve stimulation safe during pregnancy? A mini review. J Epilepsy. (2021) 174:106671. doi: 10.1016/j.eplepsyres.2021.106671, PMID: [DOI] [PubMed] [Google Scholar]
- 55.Fahoum F, Boffini M, Kann L, Faini S, Gordon C, Tzadok M, et al. VNS parameters for clinical response in epilepsy. Brain Stimul. (2022) 15:814–21. doi: 10.1016/j.brs.2022.05.016, PMID: [DOI] [PubMed] [Google Scholar]
- 56.Tzadok M, Verner R, Kann L, Tungala D, Gordon C, el Tahry R, et al. Rapid titration of VNS therapy reduces time-to-response in epilepsy. Epilepsy Behav. (2022) 134:108861. doi: 10.1016/j.yebeh.2022.108861, PMID: [DOI] [PubMed] [Google Scholar]
- 57.Bagić AI, Verner R, Afra P, Benbadis S. ASCEND: a randomized controlled trial of titration strategies for vagus nerve stimulation in drug-resistant epilepsy. Epilepsy Behav. (2023) 145:109333. doi: 10.1016/j.yebeh.2023.109333, PMID: [DOI] [PubMed] [Google Scholar]
- 58.Barbella G, Cocco I, Freri E, Marotta G, Visani E, Franceschetti S, et al. Transcutaneous vagal nerve stimulatio (t-VNS): an adjunctive treatment option for refractory epilepsy. Seizure. (2018) 60:115–9. doi: 10.1016/j.seizure.2018.06.016, PMID: [DOI] [PubMed] [Google Scholar]
- 59.Rong P, Liu A, Zhang J, Wang Y, Yang A, Li L, et al. An alternative therapy for drug-resistant epilepsy: transcutaneous auricular vagus nerve stimulation. Chin Med J. (2014) 127:300–3. doi: 10.3760/cma.j.issn.0366-6999.20131511, PMID: [DOI] [PubMed] [Google Scholar]
- 60.Rong P., Liu A., Zhang J., Wang Y., He W., Yang A., et al. Transcutaneous vagus nerve stimulation for refractory epilepsy: a randomized controlled trial. Clin Sci. (2014). doi: 10.1042/cs20130518 [DOI] [PubMed] [Google Scholar]
- 61.Aihua L, Lu S, Liping L, Xiuru W, Hua L, Yuping W. A controlled trial of transcutaneous vagus nerve stimulation for the treatment of pharmacoresistant epilepsy. Epilepsy Behav. (2014) 39:105–10. doi: 10.1016/j.yebeh.2014.08.005, PMID: [DOI] [PubMed] [Google Scholar]
- 62.Stefan H, Kreiselmeyer G, Kerling F, Kurzbuch K, Rauch C, Heers M, et al. Transcutaneous vagus nerve stimulation (t-VNS) in pharmacoresistant epilepsies: a proof of concept trial. Epilepsia. (2012) 53:e115–8. doi: 10.1111/j.1528-1167.2012.03492.x, PMID: [DOI] [PubMed] [Google Scholar]
- 63.Yang H, Shi W, Fan J, Wang X, Song Y, Lian Y, et al. Transcutaneous auricular vagus nerve stimulation (ta-VNS) for treatment of drug-resistant epilepsy: a randomized, double-blind clinical trial. Neurotherapeutics. (2023) 20:870–80. doi: 10.1007/s13311-023-01353-9, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bauer S, Baier H, Baumgartner C, Bohlmann K, Fauser S, Graf W, et al. Transcutaneous vagus nerve stimulation (tVNS) for treatment of drug-resistant epilepsy: a randomized, double-blind clinical trial (cMPsE02). Brain Stimul. (2016) 9:356–63. doi: 10.1016/j.brs.2015.11.003 [DOI] [PubMed] [Google Scholar]
- 65.Song GF, Wang HY, Wu CJ, Li X, Yang FY. A retrospective study of transcutaneous vagus nerve stimulation for poststroke epilepsy. Medicine (Baltimore). (2018) 97:e11625. doi: 10.1097/md.0000000000011625, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.von Wrede R, Surges R. Transcutaneous vagus nerve stimulation in the treatment of drug-resistant epilepsy. Autonomic Neurosci Basic Clin. (2021) 235:102840. doi: 10.1016/j.autneu.2021.102840, PMID: [DOI] [PubMed] [Google Scholar]
- 67.Keatch C, Lambert E, Woods W, Kameneva T. Measuring brain response to transcutaneous vagus nerve stimulation (tVNS) using simultaneous magnetoencephalography (MEG). J Neural Eng. (2022) 19:026038. doi: 10.1088/1741-2552/ac620c, PMID: [DOI] [PubMed] [Google Scholar]
- 68.Elger G, Hoppe C, Falkai P, Rush AJ, Elger CE. Vagus nerve stimulation is associated with mood improvements in epilepsy patients. Epilepsy Res. (2000) 42:203–10. doi: 10.1016/s0920-1211(00)00181-9, PMID: [DOI] [PubMed] [Google Scholar]
- 69.Harden CL, Pulver MC, Ravdin LD, Nikolov B, Halper JP, Labar DR. A pilot study of mood in epilepsy patients treated with vagus nerve stimulation. Epilepsy Behav. (2000) 1:93–9. doi: 10.1006/ebeh.2000.0046, PMID: [DOI] [PubMed] [Google Scholar]
- 70.Sackeim H. A., Rush A. J., George M. S., Marangell L. B., Husain M. M., Nahas Z., et al. Vagus nerve stimulation (VNS™) for treatment-resistant depression efficacy, side effects, and predictors of outcome. Neuropsychopharmacology. (2001) 25:713–28. doi: 10.1016/s0893-133x(01)00271-8 [DOI] [PubMed] [Google Scholar]
- 71.Rush AJ, George MS, Sackeim HA, Marangell LB, Husain MM, Giller C, et al. Vagus nerve stimulation (VNS) for treatment-resistant depressions: a multicenter study. Biol Psychiatry. (2000) 47:276–86. doi: 10.1016/s0006-3223(99)00304-2, PMID: [DOI] [PubMed] [Google Scholar]
- 72.Marangell LB, Rush AJ, George MS, Sackeim HA, Johnson CR, Husain MM, et al. Vagus nerve stimulation (VNS) for major depressive episodes: one year outcomes. Biol Psychiatry. (2002) 51:280–7. doi: 10.1016/s0006-3223(01)01343-9 [DOI] [PubMed] [Google Scholar]
- 73.Nahas Z, Marangell LB, Husain MM, Rush AJ, Sackeim HA, Lisanby SH, et al. Two-year outcome of vagus nerve stimulation (VNS) for treatment of major depressive episodes. J Clin Psychiatry. (2005) 66:1097–104. doi: 10.4088/jcp.v66n0902, PMID: [DOI] [PubMed] [Google Scholar]
- 74.Rush AJ, Sackeim HA, Marangell LB, George MS, Brannan SK, Davis SM, et al. Effects of 12 months of vagus nerve stimulation in treatment-resistant depression: a naturalistic study. Biol Psychiatry. (2005) 58:355–63. doi: 10.1016/j.biopsych.2005.05.024 [DOI] [PubMed] [Google Scholar]
- 75.Conway CR, Kumar A, Xiong W, Bunker M, Aaronson ST, Rush AJ. Chronic vagus nerve stimulation significantly improves quality of life in treatment-resistant major depression. J Clin Psychiatry. (2018) 79:22269. doi: 10.4088/JCP.18m12178, PMID: [DOI] [PubMed] [Google Scholar]
- 76.Trottier-Duclos F, Desbeaumes Jodoin V, Fournier-Gosselin MP, Richer F, Desjardins N, Tieu S, et al. A 6-year follow-up study of vagus nerve stimulation effect on quality of life in treatment-resistant depression: a pilot study. J ECT. (2018) 34:e58–60. doi: 10.1097/yct.0000000000000485, PMID: [DOI] [PubMed] [Google Scholar]
- 77.Rush AJ, Marangell LB, Sackeim HA, George MS, Brannan SK, Davis SM, et al. Vagus nerve stimulation for treatment-resistant depression: a randomized, controlled acute phase trial. Biol Psychiatry. (2005) 58:347–54. doi: 10.1016/j.biopsych.2005.05.025 [DOI] [PubMed] [Google Scholar]
- 78.Schlaepfer TE, Frick C, Zobel A, Maier W, Heuser I, Bajbouj M, et al. Vagus nerve stimulation for depression: efficacy and safety in a European study. Psychol Med. (2008) 38:651–61. doi: 10.1017/s0033291707001924 [DOI] [PubMed] [Google Scholar]
- 79.Mesches GA, Wisner KL, Betcher HK. A common clinical conundrum: antidepressant treatment of depression in pregnant women. Semin Perinatol. (2020) 44:151229. doi: 10.1016/j.semperi.2020.151229, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Husain MM, Stegman D, Trevino K. Pregnancy and delivery while receiving vagus nerve stimulation for the treatment of major depression: a case report. Ann General Psychiatry. (2005) 4:16. doi: 10.1186/1744-859x-4-16, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hallböök T, Lundgren J, Stjernqvist K, Blennow G, Strömblad LG, Rosén I. Vagus nerve stimulation in 15 children with therapy resistant epilepsy; its impact on cognition, quality of life, behaviour and mood. Seizure. (2005) 14:504–13. doi: 10.1016/j.seizure.2005.08.007 [DOI] [PubMed] [Google Scholar]
- 82.Evensen K, Jørgensen MB, Sabers A, Martiny K. Transcutaneous vagal nerve stimulation in treatment-resistant depression: a feasibility study. Neuromodulation. (2022) 25:443–9. doi: 10.1111/ner.13366, PMID: [DOI] [PubMed] [Google Scholar]
- 83.Rong P, Liu J, Wang L, Liu R, Fang J, Zhao J, et al. Effect of transcutaneous auricular vagus nerve stimulation on major depressive disorder: a nonrandomized controlled pilot study. J Affect Disord. (2016) 195:172–9. doi: 10.1016/j.jad.2016.02.031, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fang J, Egorova N, Rong P, Liu J, Hong Y, Fan Y, et al. Early cortical biomarkers of longitudinal transcutaneous vagus nerve stimulation treatment success in depression. NeuroImage Clin. (2017) 14:105–11. doi: 10.1016/j.nicl.2016.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tu Y, Fang J, Cao J, Wang Z, Park J, Jorgenson K, et al. A distinct biomarker of continuous transcutaneous vagus nerve stimulation treatment in major depressive disorder. Brain Stimul. (2018) 11:501–8. doi: 10.1016/j.brs.2018.01.006, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Li S, Rong P, Wang Y, Jin G, Hou X, Li S, et al. Comparative effectiveness of transcutaneous auricular vagus nerve stimulation vs citalopram for major depressive disorder: a randomized trial. Neuromodulation. (2022) 25:450–60. doi: 10.1016/j.neurom.2021.10.021, PMID: [DOI] [PubMed] [Google Scholar]
- 87.Tan C, Qiao M, Ma Y, Luo Y, Fang J, Yang Y. The efficacy and safety of transcutaneous auricular vagus nerve stimulation in the treatment of depressive disorder: a systematic review and meta-analysis of randomized controlled trials. J Affect Disord. (2023) 337:37–49. doi: 10.1016/j.jad.2023.05.048, PMID: [DOI] [PubMed] [Google Scholar]
- 88.Lee KB, Lim SH, Kim KH, Kim KJ, Kim YR, Chang WN, et al. Six-month functional recovery of stroke patients: a multi-time-point study. Int J Rehabil Res. (2015) 38:173–80. doi: 10.1097/mrr.0000000000000108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dawson J, Liu CY, Francisco GE, Cramer SC, Wolf SL, Dixit A, et al. Vagus nerve stimulation paired with rehabilitation for upper limb motor function after ischaemic stroke (VNS-REHAB): a randomised, blinded, pivotal, device trial. Lancet (London, England). (2021) 397:1545–53. doi: 10.1016/s0140-6736(21)00475-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Dawson J, Engineer ND, Prudente CN, Pierce D, Francisco G, Yozbatiran N, et al. Vagus nerve stimulation paired with upper-limb rehabilitation after stroke: one-year follow-up. Neurorehabil Neural Repair. (2020) 34:609–15. doi: 10.1177/1545968320924361 [DOI] [PubMed] [Google Scholar]
- 91.Francisco GE, Engineer ND, Dawson J, Kimberley TJ, Cramer SC, Prudente CN, et al. Vagus nerve stimulation paired with upper-limb rehabilitation after stroke: 2- and 3-year follow-up from the pilot study. Arch Phys Med Rehabil. (2023) 104:1180–7. doi: 10.1016/j.apmr.2023.02.012, PMID: [DOI] [PubMed] [Google Scholar]
- 92.Redgrave JN, Moore L, Oyekunle T, Ebrahim M, Falidas K, Snowdon N, et al. Transcutaneous auricular vagus nerve stimulation with concurrent upper limb repetitive task practice for poststroke motor recovery: a pilot study. J Stroke Cerebrovasc Dis. (2018) 27:1998–2005. doi: 10.1016/j.jstrokecerebrovasdis.2018.02.056, PMID: [DOI] [PubMed] [Google Scholar]
- 93.Capone F, Miccinilli S, Pellegrino G, Zollo L, Simonetti D, Bressi F, et al. Transcutaneous vagus nerve stimulation combined with robotic rehabilitation improves upper limb function after stroke. Neural Plast. (2017) 2017:7876507–6. doi: 10.1155/2017/7876507, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cook DN, Thompson S, Stomberg-Firestein S, Bikson M, George MS, Jenkins DD, et al. Design and validation of a closed-loop, motor-activated auricular vagus nerve stimulation (MAAVNS) system for neurorehabilitation. Brain Stimul. (2020) 13:800–3. doi: 10.1016/j.brs.2020.02.028, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Badran BW, Peng X, Baker-Vogel B, Hutchison S, Finetto P, Rishe K, et al. Motor activated auricular vagus nerve stimulation as a potential neuromodulation approach for post-stroke motor rehabilitation: a pilot study. Neurorehabil Neural Repair. (2023) 37:374–83. doi: 10.1177/15459683231173357, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bolognini N, Russo C, Edwards DJ. The sensory side of post-stroke motor rehabilitation. Restor Neurol Neurosci. (2016) 34:571–86. doi: 10.3233/rnn-150606, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kilgard MP, Rennaker RL, Alexander J, Dawson J. Vagus nerve stimulation paired with tactile training improved sensory function in a chronic stroke patient. NeuroRehabilitation. (2018) 42:159–65. doi: 10.3233/nre-172273, PMID: [DOI] [PubMed] [Google Scholar]
- 98.Yuan Y, Wang J, Wu D, Zhang D, Song W. Effect of transcutaneous vagus nerve stimulation in dysphagia after lateral medullary infarction: a case report. Am J Speech Lang Pathol. (2019) 28:1381–7. doi: 10.1044/2019_ajslp-18-0262, PMID: [DOI] [PubMed] [Google Scholar]
- 99.Wang Y, He Y, Jiang L, Chen X, Zou F, Yin Y, et al. Effect of transcutaneous auricular vagus nerve stimulation on post-stroke dysphagia. J Neurol. (2023) 270:995–1003. doi: 10.1007/s00415-022-11465-5, PMID: [DOI] [PubMed] [Google Scholar]
- 100.Cortese MD, Vatrano M, Arcuri F, Raso MG, Tonin P, Calabrò RS, et al. Behavioral scales variability in patients with prolonged disorders of consciousness. Neurol Sci. (2023) 44:3107–22. doi: 10.1007/s10072-023-06812-x, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Noé E, Ferri J, Colomer C, Moliner B, O'Valle M, Ugart P, et al. Feasibility, safety and efficacy of transauricular vagus nerve stimulation in a cohort of patients with disorders of consciousness. Brain Stimul. (2020) 13:427–9. doi: 10.1016/j.brs.2019.12.005 [DOI] [PubMed] [Google Scholar]
- 102.Zhai W, Jiao H, Zhuang Y, Yang Y, Zhang J, Wang Y, et al. Optimizing the modulation paradigm of transcutaneous auricular vagus nerve stimulation in patients with disorders of consciousness: a prospective exploratory pilot study protocol. Front Neurosci. (2023) 17:1145699. doi: 10.3389/fnins.2023.1145699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yu YT, Yang Y, Wang LB, Fang JL, Chen YY, He JH, et al. Transcutaneous auricular vagus nerve stimulation in disorders of consciousness monitored by fMRI: the first case report. Brain Stimul. (2017) 10:328–30. doi: 10.1016/j.brs.2016.12.004, PMID: [DOI] [PubMed] [Google Scholar]
- 104.Yu Y, Yang Y, Gan S, Guo S, Fang J, Wang S, et al. Cerebral hemodynamic correlates of transcutaneous auricular vagal nerve stimulation in consciousness restoration: an open-label pilot study. Front Neurol. (2021) 12:684791. doi: 10.3389/fneur.2021.684791, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Corazzol M, Lio G, Lefevre A, Deiana G, Tell L, André-Obadia N, et al. Restoring consciousness with vagus nerve stimulation. Curr Biol. (2017) 27:R994–r996. doi: 10.1016/j.cub.2017.07.060, PMID: [DOI] [PubMed] [Google Scholar]
- 106.Hakon J, Moghiseh M, Poulsen I, Øland CML, Hansen CP, Sabers A. Transcutaneous vagus nerve stimulation in patients with severe traumatic brain injury: a feasibility trial. Neuromodulation. (2020) 23:859–64. doi: 10.1111/ner.13148, PMID: [DOI] [PubMed] [Google Scholar]
- 107.Zhou YF, Kang JW, Xiong Q, Feng Z, Dong XY. Transauricular vagus nerve stimulation for patients with disorders of consciousness: a randomized controlled clinical trial. Front Neurol. (2023) 14:1133893. doi: 10.3389/fneur.2023.1133893, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Yifei W, Yi Y, Yu W, Jinling Z, Weihang Z, Shaoyuan LI, et al. Transcutaneous auricular vague nerve stimulation improved brain connection activity on patients of disorders of consciousness: a pilot study. J Trad Chinese Med. (2022) 42:463–71. doi: 10.19852/j.cnki.jtcm.2022.03.012, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Osińska A, Rynkiewicz A, Binder M, Komendziński T, Borowicz A, Leszczyński A. Non-invasive vagus nerve stimulation in treatment of disorders of consciousness - longitudinal case study. Front Neurosci. (2022) 16:834507. doi: 10.3389/fnins.2022.834507, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Dong X, Tang Y, Zhou Y, Feng Z. Stimulation of vagus nerve for patients with disorders of consciousness: a systematic review. Front Neurosci. (2023) 17:1257378. doi: 10.3389/fnins.2023.1257378, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Lane CA, Hardy J, Schott JM. Alzheimer's disease. Eur J Neurol. (2018) 25:59–70. doi: 10.1111/ene.13439 [DOI] [PubMed] [Google Scholar]
- 112.Sjogren MJC, Hellstrom PTO, Jonsson MAG, Runnerstam M, C-son Silander H, Ben-Menachem E, et al. Cognition-enhancing effect of vagus nerve stimulation in patients with Alzheimer's disease: a pilot study. J Clin Psychiatry. (2002) 63:972–80. doi: 10.4088/jcp.v63n1103, PMID: [DOI] [PubMed] [Google Scholar]
- 113.Merrill CA, Jonsson MAG, Minthon L, Ejnell H, Silander HCS, Blennow K, et al. Vagus nerve stimulation in patients with Alzheimer's disease. J Clin Psychiatry. (2006) 67:1171–8. doi: 10.4088/jcp.v67n0801 [DOI] [PubMed] [Google Scholar]
- 114.Sun L, Peräkylä J, Holm K, Haapasalo J, Lehtimäki K, Ogawa KH, et al. Vagus nerve stimulation improves working memory performance. J Clin Exp Neuropsychol. (2017) 39:954–64. doi: 10.1080/13803395.2017.1285869, PMID: [DOI] [PubMed] [Google Scholar]
- 115.Clark KB, Naritoku DK, Smith DC, Browning RA, Jensen RA. Enhanced recognition memory following vagus nerve stimulation in human subjects. Nat Neurosci. (1999) 2:94–8. doi: 10.1038/4600, PMID: [DOI] [PubMed] [Google Scholar]
- 116.Jacobs HI, Riphagen JM, Razat CM, Wiese S, Sack AT. Transcutaneous vagus nerve stimulation boosts associative memory in older individuals. Neurobiol Aging. (2015) 36:1860–7. doi: 10.1016/j.neurobiolaging.2015.02.023, PMID: [DOI] [PubMed] [Google Scholar]
- 117.Giraudier M, Ventura-Bort C, Weymar M. Transcutaneous vagus nerve stimulation (tVNS) improves high-confidence recognition memory but not emotional word processing. Front Psychol. (2020) 11:1276. doi: 10.3389/fpsyg.2020.01276, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Sun JB, Cheng C, Tian QQ, Yuan H, Yang XJ, Deng H, et al. Transcutaneous auricular vagus nerve stimulation improves spatial working memory in healthy Young adults. Front Neurosci. (2021) 15:790793. doi: 10.3389/fnins.2021.790793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Mertens A, Naert L, Miatton M, Poppa T, Carrette E, Gadeyne S, et al. Transcutaneous vagus nerve stimulation does not affect verbal memory performance in healthy volunteers. Front Psychol. (2020) 11:551. doi: 10.3389/fpsyg.2020.00551, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Vargas-Caballero M, Warming H, Walker R, Holmes C, Cruickshank G, Patel B. Vagus nerve stimulation as a potential therapy in early Alzheimer's disease: a review. Front Hum Neurosci. (2022) 16:866434. doi: 10.3389/fnhum.2022.866434, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Choudhary T, Elliott M, Euliano NR, Gurel NZ, Rivas AG, Wittbrodt MT, et al. Effect of transcutaneous cervical vagus nerve stimulation on declarative and working memory in patients with posttraumatic stress disorder (PTSD): a pilot study. J Affect Disord. (2023) 339:418–25. doi: 10.1016/j.jad.2023.07.025, PMID: [DOI] [PubMed] [Google Scholar]
- 122.Sellaro R, de Gelder B, Finisguerra A, Colzato LS. Transcutaneous vagus nerve stimulation (tVNS) enhances recognition of emotions in faces but not bodies. Cortex. (2018) 99:213–23. doi: 10.1016/j.cortex.2017.11.007 [DOI] [PubMed] [Google Scholar]
- 123.Jongkees BJ, Immink MA, Finisguerra A, Colzato LS. Transcutaneous vagus nerve stimulation (tVNS) enhances response selection during sequential action. Front Psychol. (2018) 9:1159. doi: 10.3389/fpsyg.2018.01159, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Steenbergen L, Sellaro R, Stock AK, Verkuil B, Beste C, Colzato LS. RETRACTED: transcutaneous vagus nerve stimulation (tVNS) enhances response selection during action cascading processes. Eur Neuropsychopharmacol. (2015) 25:773–8. doi: 10.1016/j.euroneuro.2015.03.015, PMID: [DOI] [PubMed] [Google Scholar]
- 125.Fischer R, Ventura-Bort C, Hamm A, Weymar M. Transcutaneous vagus nerve stimulation (tVNS) enhances conflict-triggered adjustment of cognitive control. Cogn Affect Behav Neurosci. (2018) 18:680–93. doi: 10.3758/s13415-018-0596-2 [DOI] [PubMed] [Google Scholar]
- 126.Tona KD, Revers H, Verkuil B, Nieuwenhuis S. Noradrenergic regulation of cognitive flexibility: no effects of stress, transcutaneous vagus nerve stimulation, and atomoxetine on task-switching in humans. J Cogn Neurosci. (2020) 32:1881–95. doi: 10.1162/jocn_a_01603 [DOI] [PubMed] [Google Scholar]
- 127.Borges U, Knops L, Laborde S, Klatt S, Raab M. Transcutaneous vagus nerve stimulation may enhance only specific aspects of the core executive functions. A randomized crossover trial. Front Neurosci. (2020) 14:523. doi: 10.3389/fnins.2020.00523, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zhou Q, Yu L, Yin C, Zhang Q, Wang X, Kang K, et al. Effect of transcutaneous auricular vagus nerve stimulation on delayed neurocognitive recovery in elderly patients. Aging Clin Exp Res. (2022) 34:2421–9. doi: 10.1007/s40520-022-02177-x, PMID: [DOI] [PubMed] [Google Scholar]
- 129.Wang L, Zhang J, Guo C, He J, Zhang S, Wang Y, et al. The efficacy and safety of transcutaneous auricular vagus nerve stimulation in patients with mild cognitive impairment: a double blinded randomized clinical trial. Brain Stimul. (2022) 15:1405–14. doi: 10.1016/j.brs.2022.09.003, PMID: [DOI] [PubMed] [Google Scholar]
- 130.Chavel SM, Westerveld M, Spencer S. Long-term outcome of vagus nerve stimulation for refractory partial epilepsy. Epilepsy Behav. (2003) 4:302–9. doi: 10.1016/s1525-5050(03)00109-4, PMID: [DOI] [PubMed] [Google Scholar]
- 131.George MS, Ward HE, Jr, Ninan PT, Pollack M, Nahas Z, Anderson B, et al. A pilot study of vagus nerve stimulation (VNS) for treatment-resistant anxiety disorders. Brain Stimul. (2008) 1:112–21. doi: 10.1016/j.brs.2008.02.001, PMID: [DOI] [PubMed] [Google Scholar]
- 132.Souza RR, Robertson NM, Pruitt DT, Gonzales PA, Hays SA, Rennaker RL, et al. Vagus nerve stimulation reverses the extinction impairments in a model of PTSD with prolonged and repeated trauma. Stress. (2019) 22:509–20. doi: 10.1080/10253890.2019.1602604, PMID: [DOI] [PubMed] [Google Scholar]
- 133.Noble LJ, Meruva VB, Hays SA, Rennaker RL, Kilgard MP, McIntyre CK. Vagus nerve stimulation promotes generalization of conditioned fear extinction and reduces anxiety in rats. Brain Stimul. (2019) 12:9–18. doi: 10.1016/j.brs.2018.09.013, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Mathew E, Tabet MN, Robertson NM, Hays SA, Rennaker RL, Kilgard MP, et al. Vagus nerve stimulation produces immediate dose-dependent anxiolytic effect in rats. J Affect Disord. (2020) 265:552–7. doi: 10.1016/j.jad.2019.11.090, PMID: [DOI] [PubMed] [Google Scholar]
- 135.Burger AM, Verkuil B, van Diest I, van der Does W, Thayer JF, Brosschot JF. The effects of transcutaneous vagus nerve stimulation on conditioned fear extinction in humans. Neurobiol Learn Mem. (2016) 132:49–56. doi: 10.1016/j.nlm.2016.05.007, PMID: [DOI] [PubMed] [Google Scholar]
- 136.Genheimer H, Andreatta M, Asan E, Pauli P. Reinstatement of contextual conditioned anxiety in virtual reality and the effects of transcutaneous vagus nerve stimulation in humans. Sci Rep. (2017) 7:17886. doi: 10.1038/s41598-017-18183-3, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Park YD. The effects of vagus nerve stimulation therapy on patients with intractable seizures and either Landau-Kleffner syndrome or autism. Epilepsy Behav. (2003) 4:286–90. doi: 10.1016/s1525-5050(03)00080-5 [DOI] [PubMed] [Google Scholar]
- 138.Levy ML, Levy KM, Hoff D, Amar AP, Park MS, Conklin JM, et al. Vagus nerve stimulation therapy in patients with autism spectrum disorder and intractable epilepsy: results from the vagus nerve stimulation therapy patient outcome registry. J Neurosurg Pediatr. (2010) 5:595–602. doi: 10.3171/2010.3.Peds09153, PMID: [DOI] [PubMed] [Google Scholar]
- 139.Danielsson S, Viggedal G, Gillberg C, Olsson I. Lack of effects of vagus nerve stimulation on drug-resistant epilepsy in eight pediatric patients with autism spectrum disorders: a prospective 2-year follow-up study. Epilepsy Behav. (2008) 12:298–304. doi: 10.1016/j.yebeh.2007.10.007, PMID: [DOI] [PubMed] [Google Scholar]
- 140.Hull MM, Madhavan D, Zaroff CM. Autistic spectrum disorder, epilepsy, and vagus nerve stimulation. Childs Nerv Syst. (2015) 31:1377–85. doi: 10.1007/s00381-015-2720-8, PMID: [DOI] [PubMed] [Google Scholar]
- 141.Mondal B, Choudhury S, Simon B, Baker MR, Kumar H. Noninvasive vagus nerve stimulation improves gait and reduces freezing of gait in Parkinson's disease. Mov Disord. (2019) 34:917–8. doi: 10.1002/mds.27662, PMID: [DOI] [PubMed] [Google Scholar]
- 142.Farrand AQ, Verner RS, McGuire RM, Helke KL, Hinson VK, Boger HA. Differential effects of vagus nerve stimulation paradigms guide clinical development for Parkinson's disease. Brain Stimul. (2020) 13:1323–32. doi: 10.1016/j.brs.2020.06.078, PMID: [DOI] [PubMed] [Google Scholar]
- 143.Sadler RM, Purdy RA, Rahey S. Vagal nerve stimulation aborts migraine in patient with intractable epilepsy. Cephalalgia. (2002) 22:482–4. doi: 10.1046/j.1468-2982.2002.00387.x, PMID: [DOI] [PubMed] [Google Scholar]
- 144.Hord ED, Evans MS, Mueed S, Adamolekun B, Naritoku DK. The effect of vagus nerve stimulation on migraines. J Pain. (2003) 4:530–4. doi: 10.1016/j.jpain.2003.08.001 [DOI] [PubMed] [Google Scholar]
- 145.Cecchini A. P., Mea E., Tullo V., Curone M., Franzini A., Broggi G., et al. Vagus nerve stimulation in drug-resistant daily chronic migraine with depression: preliminary data. Neurol Sci. (2009) 30:101–4. doi: 10.1007/s10072-009-0073-3 [DOI] [PubMed] [Google Scholar]
- 146.Mauskop A. Vagus nerve stimulation relieves chronic refractory migraine and cluster headaches. Cephalalgia. (2005) 25:82–6. doi: 10.1111/j.1468-2982.2005.00611.x, PMID: [DOI] [PubMed] [Google Scholar]
- 147.Goadsby PJ, Grosberg BM, Mauskop A, Cady R, Simmons KA. Effect of noninvasive vagus nerve stimulation on acute migraine: an open-label pilot study. Cephalalgia. (2014) 34:986–93. doi: 10.1177/0333102414524494, PMID: [DOI] [PubMed] [Google Scholar]
- 148.Zhang Y, Huang Y, Li H, Yan Z, Zhang Y, Liu X, et al. Transcutaneous auricular vagus nerve stimulation (taVNS) for migraine: an fMRI study. Reg Anesth Pain Med. (2021) 46:145–50. doi: 10.1136/rapm-2020-102088, PMID: [DOI] [PubMed] [Google Scholar]
- 149.Nesbitt AD, Marin JC, Tompkins E, Ruttledge MH, Goadsby PJ. Initial use of a novel noninvasive vagus nerve stimulator for cluster headache treatment. Neurology. (2015) 84:1249–53. doi: 10.1212/wnl.0000000000001394, PMID: [DOI] [PubMed] [Google Scholar]
- 150.Silberstein SD, Mechtler LL, Kudrow DB, Calhoun AH, McClure C, Saper JR, et al. Non-invasive vagus nerve stimulation for the ACute treatment of cluster headache: findings from the randomized, double-blind, sham-controlled ACT1 study. Headache. (2016) 56:1317–32. doi: 10.1111/head.12896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Berthoud HR, Neuhuber WL. Functional and chemical anatomy of the afferent vagal system. Autonomic Neurosci Basic Clin. (2000) 85:1–17. doi: 10.1016/s1566-0702(00)00215-0 [DOI] [PubMed] [Google Scholar]
- 152.Shiozawa P, Silva ME, Carvalho TC, Cordeiro Q, Brunoni AR, Fregni F. Transcutaneous vagus and trigeminal nerve stimulation for neuropsychiatric disorders: a systematic review. Arq Neuropsiquiatr. (2014) 72:542–7. doi: 10.1590/0004-282x20140061, PMID: [DOI] [PubMed] [Google Scholar]
- 153.Ullah F, Liang A, Rangel A, Gyengesi E, Niedermayer G, Münch G. High bioavailability curcumin: an anti-inflammatory and neurosupportive bioactive nutrient for neurodegenerative diseases characterized by chronic neuroinflammation. Arch Toxicol. (2017) 91:1623–34. doi: 10.1007/s00204-017-1939-4 [DOI] [PubMed] [Google Scholar]
- 154.Manta S, Dong J, Debonnel G, Blier P. Enhancement of the function of rat serotonin and norepinephrine neurons by sustained vagus nerve stimulation. J Psychiatry Neurosci. (2009) 34:272–80. PMID: [PMC free article] [PubMed] [Google Scholar]
- 155.Mazarati AM, Lewis ML, Pittman QJ. Neurobehavioral comorbidities of epilepsy: role of inflammation. Epilepsia. (2017) 58:48–56. doi: 10.1111/epi.13786 [DOI] [PubMed] [Google Scholar]
- 156.Johnson RL, Wilson CG. A review of vagus nerve stimulation as a therapeutic intervention. J Inflamm Res. (2018) 11:203–13. doi: 10.2147/jir.S163248, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Tracey KJ. Physiology and immunology of the cholinergic antiinflammatory pathway. J Clin Invest. (2007) 117:289–96. doi: 10.1172/jci30555, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Fang YT, Lin YT, Tseng WL, Tseng P, Hua GL, Chao YJ, et al. Neuroimmunomodulation of vagus nerve stimulation and the therapeutic implications. Front Aging Neurosci. (2023) 15:1173987. doi: 10.3389/fnagi.2023.1173987, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Perry VH, Holmes C. Microglial priming in neurodegenerative disease. Nat Rev Neurol. (2014) 10:217–24. doi: 10.1038/nrneurol.2014.38 [DOI] [PubMed] [Google Scholar]
- 160.Plastira I, Bernhart E, Goeritzer M, Reicher H, Kumble VB, Kogelnik N, et al. 1-Oleyl-lysophosphatidic acid (LPA) promotes polarization of BV-2 and primary murine microglia towards an M1-like phenotype. J Neuroinflammation. (2016) 13:205. doi: 10.1186/s12974-016-0701-9, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Chen H, Feng Z, Min L, Deng W, Tan M, Hong J, et al. Vagus nerve stimulation reduces neuroinflammation through microglia polarization regulation to improve functional recovery after spinal cord injury. Front Neurosci. (2022) 16:813472. doi: 10.3389/fnins.2022.813472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Kaczmarczyk R, Tejera D, Simon BJ, Heneka MT. Microglia modulation through external vagus nerve stimulation in a murine model of Alzheimer's disease. J Neurochem. (2018) 146:76–85. doi: 10.1111/jnc.14284 [DOI] [PubMed] [Google Scholar]
- 163.Zhang Q, Lu Y, Bian H, Guo L, Zhu H. Activation of the α7 nicotinic receptor promotes lipopolysaccharide-induced conversion of M1 microglia to M2. Am J Transl Res. (2017) 9:971–85. PMID: [PMC free article] [PubMed] [Google Scholar]
- 164.Parada E, Egea J, Buendia I, Negredo P, Cunha AC, Cardoso S, et al. The microglial α7-acetylcholine nicotinic receptor is a key element in promoting neuroprotection by inducing heme oxygenase-1 via nuclear factor erythroid-2-related factor 2. Antioxid Redox Signal. (2013) 19:1135–48. doi: 10.1089/ars.2012.4671, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Jiang Y, Li L, Liu B, Zhang Y, Chen Q, Li C. Vagus nerve stimulation attenuates cerebral ischemia and reperfusion injury via endogenous cholinergic pathway in rat. PLoS One. (2014) 9:e102342. doi: 10.1371/journal.pone.0102342, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Meneses G, Bautista M, Florentino A, Díaz G, Acero G, Besedovsky H, et al. Electric stimulation of the vagus nerve reduced mouse neuroinflammation induced by lipopolysaccharide. J Inflamm. (2016) 13:33. doi: 10.1186/s12950-016-0140-5, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Lu XX, Hong ZQ, Tan Z, Sui MH, Zhuang ZQ, Liu HH, et al. Nicotinic acetylcholine receptor Alpha7 subunit mediates vagus nerve stimulation-induced neuroprotection in acute permanent cerebral ischemia by a7nAchR/JAK2 pathway. Med Sci Monit. (2017) 23:6072–81. doi: 10.12659/msm.907628, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.de Jonge WJ, Ulloa L. The alpha7 nicotinic acetylcholine receptor as a pharmacological target for inflammation. Br J Pharmacol. (2007) 151:915–29. doi: 10.1038/sj.bjp.0707264, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Guo M, Li C, Lei Y, Xu S, Zhao D, Lu XY. Role of the adipose PPARγ-adiponectin axis in susceptibility to stress and depression/anxiety-related behaviors. Mol Psychiatry. (2017) 22:1056–68. doi: 10.1038/mp.2016.225, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Jiang Y, Li L, Liu B, Zhang Y, Chen Q, Li C. PPARγ upregulation induced by vagus nerve stimulation exerts anti-inflammatory effect in cerebral ischemia/reperfusion rats. Med Sci Monit. (2015) 21:268–75. doi: 10.12659/msm.891407, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Wang JY, Zhang Y, Chen Y, Wang Y, Li SY, Wang YF, et al. Mechanisms underlying antidepressant effect of transcutaneous auricular vagus nerve stimulation on CUMS model rats based on hippocampal α7nAchR/NF-κB signal pathway. J Neuroinflammation. (2021) 18:291. doi: 10.1186/s12974-021-02341-6, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Smith EE, Schneider JA, Wardlaw JM, Greenberg SM. Cerebral microinfarcts: the invisible lesions. Lancet Neurol. (2012) 11:272–82. doi: 10.1016/s1474-4422(11)70307-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Varatharaj A, Galea I. The blood-brain barrier in systemic inflammation. Brain Behav Immun. (2017) 60:1–12. doi: 10.1016/j.bbi.2016.03.010 [DOI] [PubMed] [Google Scholar]
- 174.Chen X, He X, Luo S, Feng Y, Liang F, Shi T, et al. Vagus nerve stimulation attenuates cerebral microinfarct and colitis-induced cerebral microinfarct aggravation in mice. Front Neurol. (2018) 9:798. doi: 10.3389/fneur.2018.00798, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Lopez NE, Krzyzaniak MJ, Costantini TW, Putnam J, Hageny AM, Eliceiri B, et al. Vagal nerve stimulation decreases blood-brain barrier disruption after traumatic brain injury. J Trauma Acute Care Surg. (2012) 72:1562–6. doi: 10.1097/TA.0b013e3182569875, PMID: [DOI] [PubMed] [Google Scholar]
- 176.Wang Y, Zhan G, Cai Z, Jiao B, Zhao Y, Li S, et al. Vagus nerve stimulation in brain diseases: therapeutic applications and biological mechanisms. Neurosci Biobehav Rev. (2021) 127:37–53. doi: 10.1016/j.neubiorev.2021.04.018, PMID: [DOI] [PubMed] [Google Scholar]
- 177.Yang Y, Yang LY, Orban L, Cuylear D, Thompson J, Simon B, et al. Non-invasive vagus nerve stimulation reduces blood-brain barrier disruption in a rat model of ischemic stroke. Brain Stimul. (2018) 11:689–98. doi: 10.1016/j.brs.2018.01.034, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Jin Z, Dong J, Wang Y, Liu Y. Exploring the potential of vagus nerve stimulation in treating brain diseases: a review of immunologic benefits and neuroprotective efficacy. Eur J Med Res. (2023) 28:444. doi: 10.1186/s40001-023-01439-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Lin TW, Harward SC, Huang YZ, McNamara JO. Targeting BDNF/TrkB pathways for preventing or suppressing epilepsy. Neuropharmacology. (2020) 167:107734. doi: 10.1016/j.neuropharm.2019.107734, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Shimizu E, Hashimoto K, Okamura N, Koike K, Komatsu N, Kumakiri C, et al. Alterations of serum levels of brain-derived neurotrophic factor (BDNF) in depressed patients with or without antidepressants. Biol Psychiatry. (2003) 54:70–5. doi: 10.1016/s0006-3223(03)00181-1 [DOI] [PubMed] [Google Scholar]
- 181.O’Leary OF, Ogbonnaya ES, Felice D, Levone BR, Conroy CL, Fitzgerald P, et al. The vagus nerve modulates BDNF expression and neurogenesis in the hippocampus. Eur Neuropsychopharmacol. (2018) 28:307–16. doi: 10.1016/j.euroneuro.2017.12.004, PMID: [DOI] [PubMed] [Google Scholar]
- 182.Follesa P, Biggio F, Gorini G, Caria S, Talani G, Dazzi L, et al. Vagus nerve stimulation increases norepinephrine concentration and the gene expression of BDNF and bFGF in the rat brain. Brain Res. (2007) 1179:28–34. doi: 10.1016/j.brainres.2007.08.045 [DOI] [PubMed] [Google Scholar]
- 183.Biggio F, Gorini G, Utzeri C, Olla P, Marrosu F, Mocchetti I, et al. Chronic vagus nerve stimulation induces neuronal plasticity in the rat hippocampus. Int J Neuropsychopharmacol. (2009) 12:1209–21. doi: 10.1017/s1461145709000200, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Li J, Zhang Q, Li S, Niu L, Ma J, Wen L, et al. α7nAchR mediates transcutaneous auricular vagus nerve stimulation-induced neuroprotection in a rat model of ischemic stroke by enhancing axonal plasticity. Neurosci Lett. (2020) 730:135031. doi: 10.1016/j.neulet.2020.135031, PMID: [DOI] [PubMed] [Google Scholar]
- 185.Furmaga H, Carreno FR, Frazer A. Vagal nerve stimulation rapidly activates brain-derived neurotrophic factor receptor TrkB in rat brain. PLoS One. (2012) 7:e34844. doi: 10.1371/journal.pone.0034844, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Huang EJ, Reichardt LF. Trk receptors: roles in neuronal signal transduction. Annu Rev Biochem. (2003) 72:609–42. doi: 10.1146/annurev.biochem.72.121801.161629 [DOI] [PubMed] [Google Scholar]
- 187.Reichardt LF. Neurotrophin-regulated signalling pathways. Philos Trans R Soc Lond Ser B Biol Sci. (2006) 361:1545–64. doi: 10.1098/rstb.2006.1894, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Carreno FR, Frazer A. Activation of signaling pathways downstream of the brain-derived neurotrophic factor receptor, TrkB, in the rat brain by vagal nerve stimulation and antidepressant drugs. Int J Neuropsychopharmacol. (2014) 17:247–58. doi: 10.1017/s1461145713000977, PMID: [DOI] [PubMed] [Google Scholar]
- 189.Shah AP, Carreno FR, Wu H, Chung YA, Frazer A. Role of TrkB in the anxiolytic-like and antidepressant-like effects of vagal nerve stimulation: comparison with desipramine. Neuroscience. (2016) 322:273–86. doi: 10.1016/j.neuroscience.2016.02.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Chen CC, Williams CL. Interactions between epinephrine, ascending vagal fibers, and central noradrenergic systems in modulating memory for emotionally arousing events. Front Behav Neurosci. (2012) 6:35. doi: 10.3389/fnbeh.2012.00035, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Dorr AE, Debonnel G. Effect of vagus nerve stimulation on serotonergic and noradrenergic transmission. J Pharmacol Exp Ther. (2006) 318:890–8. doi: 10.1124/jpet.106.104166, PMID: [DOI] [PubMed] [Google Scholar]
- 192.Piñeyro G, Blier P. Autoregulation of serotonin neurons: role in antidepressant drug action. Pharmacol Rev. (1999) 51:533–91. PMID: [PubMed] [Google Scholar]
- 193.Furmaga H, Shah A, Frazer A. Serotonergic and noradrenergic pathways are required for the anxiolytic-like and antidepressant-like behavioral effects of repeated vagal nerve stimulation in rats. Biol Psychiatry. (2011) 70:937–45. doi: 10.1016/j.biopsych.2011.07.020, PMID: [DOI] [PubMed] [Google Scholar]
- 194.Liu AF, Zhao FB, Wang J, Lu YF, Tian J, Zhao Y, et al. Effects of vagus nerve stimulation on cognitive functioning in rats with cerebral ischemia reperfusion. J Transl Med. (2016) 14:101. doi: 10.1186/s12967-016-0858-0, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Manta S, El Mansari M, Debonnel G, Blier P. Electrophysiological and neurochemical effects of long-term vagus nerve stimulation on the rat monoaminergic systems. Int J Neuropsychopharmacol. (2013) 16:459–70. doi: 10.1017/s1461145712000387, PMID: [DOI] [PubMed] [Google Scholar]
- 196.Landau AM, Dyve S, Jakobsen S, Alstrup AKO, Gjedde A, Doudet DJ. Acute vagal nerve stimulation lowers α2 adrenoceptor availability: possible mechanism of therapeutic action. Brain Stimul. (2015) 8:702–7. doi: 10.1016/j.brs.2015.02.003, PMID: [DOI] [PubMed] [Google Scholar]
- 197.Raedt R, Clinckers R, Mollet L, Vonck K, el Tahry R, Wyckhuys T, et al. Increased hippocampal noradrenaline is a biomarker for efficacy of vagus nerve stimulation in a limbic seizure model. J Neurochem. (2011) 117:461–9. doi: 10.1111/j.1471-4159.2011.07214.x, PMID: [DOI] [PubMed] [Google Scholar]
- 198.Collins L, Boddington L, Steffan PJ, McCormick D. Vagus nerve stimulation induces widespread cortical and behavioral activation. Curr Biol. (2021) 31:2088–2098.e3. doi: 10.1016/j.cub.2021.02.049, PMID: [DOI] [PubMed] [Google Scholar]
- 199.Kumagai S, Shiramatsu TI, Matsumura A, Ishishita Y, Ibayashi K, Onuki Y, et al. Frequency-specific modulation of oscillatory activity in the rat auditory cortex by vagus nerve stimulation. Brain Stimul. (2023) 16:1476–85. doi: 10.1016/j.brs.2023.09.019 [DOI] [PubMed] [Google Scholar]
- 200.Duman RS, Sanacora G, Krystal JH. Altered connectivity in depression: GABA and glutamate neurotransmitter deficits and reversal by novel treatments. Neuron. (2019) 102:75–90. doi: 10.1016/j.neuron.2019.03.013, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Tzilivaki A, Tukker JJ, Maier N, Poirazi P, Sammons RP, Schmitz D. Hippocampal GABAergic interneurons and memory. Neuron. (2023) 111:3154–75. doi: 10.1016/j.neuron.2023.06.016, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Frangos E, Ellrich J, Komisaruk BR. Non-invasive access to the vagus nerve central projections via electrical stimulation of the external ear: fMRI evidence in humans. Brain Stimul. (2015) 8:624–36. doi: 10.1016/j.brs.2014.11.018, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Ben-Menachem E, Hamberger A, Hedner T, Hammond EJ, Uthman BM, Slater J, et al. Effects of vagus nerve stimulation on amino acids and other metabolites in the CSF of patients with partial seizures. Epilepsy Res. (1995) 20:221–7. doi: 10.1016/0920-1211(94)00083-9 [DOI] [PubMed] [Google Scholar]
- 204.Walker BR, Easton A, Gale K. Regulation of limbic motor seizures by GABA and glutamate transmission in nucleus tractus solitarius. Epilepsia. (1999) 40:1051–7. doi: 10.1111/j.1528-1157.1999.tb00818.x [DOI] [PubMed] [Google Scholar]
- 205.Marrosu F, Serra A, Maleci A, Puligheddu M, Biggio G, Piga M. Correlation between GABA(A) receptor density and vagus nerve stimulation in individuals with drug-resistant partial epilepsy. Epilepsy Res. (2003) 55:59–70. doi: 10.1016/s0920-1211(03)00107-4, PMID: [DOI] [PubMed] [Google Scholar]
- 206.Beste C, Steenbergen L, Sellaro R, Grigoriadou S, Zhang R, Chmielewski W, et al. Effects of concomitant stimulation of the GABAergic and norepinephrine system on inhibitory control - a study using transcutaneous vagus nerve stimulation. Brain Stimul. (2016) 9:811–8. doi: 10.1016/j.brs.2016.07.004, PMID: [DOI] [PubMed] [Google Scholar]
- 207.Hoeller AA, Duzzioni M, Duarte FS, Leme LR, Costa APR, Santos ECS, et al. GABA-A receptor modulators alter emotionality and hippocampal theta rhythm in an animal model of long-lasting anxiety. Brain Res. (2013) 1532:21–31. doi: 10.1016/j.brainres.2013.07.045, PMID: [DOI] [PubMed] [Google Scholar]
- 208.Broncel A, Bocian R, Kłos-Wojtczak P, Konopacki J. GABAergic mediation of hippocampal theta rhythm induced by stimulation of the vagal nerve. Brain Res Bull. (2019) 147:110–23. doi: 10.1016/j.brainresbull.2019.02.010, PMID: [DOI] [PubMed] [Google Scholar]
- 209.Ghosal S, Hare B, Duman RS. Prefrontal cortex GABAergic deficits and circuit dysfunction in the pathophysiology and treatment of chronic stress and depression. Curr Opin Behav Sci. (2017) 14:1–8. doi: 10.1016/j.cobeha.2016.09.012, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Chong ZZ, Li F, Maiese K. Activating Akt and the brain's resources to drive cellular survival and prevent inflammatory injury. Histol Histopathol. (2005) 20:299–315. doi: 10.14670/hh-20.299, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Krafft PR, Altay O, Rolland WB, Duris K, Lekic T, Tang J, et al. α7 nicotinic acetylcholine receptor agonism confers neuroprotection through GSK-3β inhibition in a mouse model of intracerebral hemorrhage. Stroke. (2012) 43:844–50. doi: 10.1161/strokeaha.111.639989, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Zhang L, Qu Y, Tang J, Chen D, Fu X, Mao M, et al. PI3K/Akt signaling pathway is required for neuroprotection of thalidomide on hypoxic-ischemic cortical neurons in vitro. Brain Res. (2010) 1357:157–65. doi: 10.1016/j.brainres.2010.08.007 [DOI] [PubMed] [Google Scholar]
- 213.Kakinuma Y, Ando M, Kuwabara M, Katare RG, Okudela K, Kobayashi M, et al. Acetylcholine from vagal stimulation protects cardiomyocytes against ischemia and hypoxia involving additive non-hypoxic induction of HIF-1alpha. FEBS Lett. (2005) 579:2111–8. doi: 10.1016/j.febslet.2005.02.065, PMID: [DOI] [PubMed] [Google Scholar]
- 214.Mridha Z, de Gee JW, Shi Y, Alkashgari R, Williams J, Suminski A, et al. Graded recruitment of pupil-linked neuromodulation by parametric stimulation of the vagus nerve. Nat Commun. (2021) 12:1539. doi: 10.1038/s41467-021-21730-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Bowles S, Hickman J, Peng X, Williamson WR, Huang R, Washington K, et al. Vagus nerve stimulation drives selective circuit modulation through cholinergic reinforcement. Neuron. (2022) 110:2867–2885.e7. doi: 10.1016/j.neuron.2022.06.017, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Hulsey DR, Riley JR, Loerwald KW, Rennaker RL, II, Kilgard MP, Hays SA. Parametric characterization of neural activity in the locus coeruleus in response to vagus nerve stimulation. Exp Neurol. (2017) 289:21–30. doi: 10.1016/j.expneurol.2016.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Rho HJ, Kim JH, Lee SH. Function of selective neuromodulatory projections in the mammalian cerebral cortex: comparison between cholinergic and noradrenergic systems. Front Neural Circ. (2018) 12:47. doi: 10.3389/fncir.2018.00047, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Hulsey DR, Hays SA, Khodaparast N, Ruiz A, das P, Rennaker RL, II, et al. Reorganization of motor cortex by vagus nerve stimulation requires cholinergic innervation. Brain Stimul. (2016) 9:174–81. doi: 10.1016/j.brs.2015.12.007, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Nichols JA, Nichols AR, Smirnakis SM, Engineer ND, Kilgard MP, Atzori M. Vagus nerve stimulation modulates cortical synchrony and excitability through the activation of muscarinic receptors. Neuroscience. (2011) 189:207–14. doi: 10.1016/j.neuroscience.2011.05.024, PMID: [DOI] [PubMed] [Google Scholar]
- 220.Zhu F, Elnozahy S, Lawlor J, Kuchibhotla KV. The cholinergic basal forebrain provides a parallel channel for state-dependent sensory signaling to auditory cortex. Nat Neurosci. (2023) 26:810–9. doi: 10.1038/s41593-023-01289-5, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Sara SJ, Bouret S. Orienting and reorienting: the locus coeruleus mediates cognition through arousal. Neuron. (2012) 76:130–41. doi: 10.1016/j.neuron.2012.09.011, PMID: [DOI] [PubMed] [Google Scholar]
- 222.Reimer J, McGinley MJ, Liu Y, Rodenkirch C, Wang Q, McCormick DA, et al. Pupil fluctuations track rapid changes in adrenergic and cholinergic activity in cortex. Nat Commun. (2016) 7:13289. doi: 10.1038/ncomms13289, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.McGinley MJ, David SV, McCormick DA. Cortical membrane potential signature of optimal states for sensory signal detection. Neuron. (2015) 87:179–92. doi: 10.1016/j.neuron.2015.05.038, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]