Abstract
This study assessed the factors militating against the effective implementation of electronic health records (EHR) in Nigeria, the computerization of patients’ health records with a lot of benefits including improved patients’ satisfaction, improved care processes, reduction of patients’ waiting time, and medication errors. Despite these benefits, healthcare organizations are slow to adopt the EHR system. Therefore, the study assessed the factors militating against the effective implementation of the EHR system, the level of awareness of EHR, and the utilization of electronic health records; it also investigated the factors militating against the effective implementation of EHR. This is a descriptive cross-sectional study conducted among members of staff of the University of Medical Sciences Teaching Hospital (UNIMEDTH). Purposive sampling was adopted to select the study participants, and a structured questionnaire was used for data collection. Statistical Product and Service Solutions (SPSS) version 27 was used for data analysis, R and Microsoft Excel were used for data visualization. Findings revealed that the respondents had a high level of awareness of EHR with an average mean of 1.29. The study revealed a low utilization rate for EHR (mean 3.01, SD 0.115) and data storage (mean 3.00, SD 0.231), indicating major problems with EHR implementation. Financial limitations (mean 2.63, SD 0.486) and insufficient ICT resources (mean 2.62, SD 0.516) are the main challenges. The regression analysis revealed that EHR utilization is highly impacted by awareness (F = 4.26, p < 0.008), accounting for 15.1% of the variance. Governmental assistance and financial constraints showed a statistically significant negative correlation (r=−0.04, p < 0.05), while inadequate internet connectivity and epileptic power supply showed a statistically significant positive association (r = 0.1, p < 0.05). The results show that, more government support is needed to alleviate financial constraints, and a stable power supply may enhance internet accessibility. The study concluded that epileptic power supply, poor internet connectivity, financial constraints, and other factors mentioned in the study militate against the effective implementation of electronic health records. It was recommended that the management should implement electronic health records effectively for efficient and effective health care delivery.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-83009-y.
Keywords: Health records, Electronic, Computerization, Data integrity, Patients’ satisfaction
Subject terms: Health care, Medical research
Introduction
An important turning point in the quest for better patient care and more efficient healthcare delivery has been the use of information technology in the medical field1. The use of electronic health records (EHR) stands out as a revolutionary innovation among these developments2. The subject of EHR has recently gained prominence among scholars globally, and it has been described as the electronic collection and storage of a wide variety of information in healthcare. These include medical histories, diagnoses, prescriptions, plans of care, immunization records, allergies, and medical investigations3–5. While EHR integration improves patient outcomes and increases diagnosis accuracy, it facilitates easy and efficient information exchange among healthcare practitioners6,7. Notwithstanding these benefits, EHR is faced with numerous challenges that must be addressed if it can be successfully implemented, especially in developing nations like Nigeria8,9.
As an important aspect of patient care, health information comprises details about an individual’s health and disabilities10,11. Therefore, the management of this information encompasses how this data is created, handled, stored, maintained, analyzed, and utilized12. While the most popular method in Nigeria for keeping health records is manual or paper-based, various Nigerian healthcare facilities—public and private—are progressively putting into practice the electronic method of health information management13. However, the adoption of EHR still stands at a very low rate8. This corroborates the opinion of14 that the rate of adoption of EHR in Nigeria stands between 18 and 23%, while the use of automated physician order entry is as low as 15%.
Studies have revealed numerous challenges mitigating the implementation of EHR in Nigeria. These include high startup and maintenance costs, insufficient infrastructure, a lack of financial resources, and a scarcity of healthcare experts15,16. Furthermore, the inconsistent adoption of EHR across various healthcare institutions in low-income countries may result from the absence of a unified national framework for its implementation17. Studies suggest that for EHR systems to be implemented successfully, organizational factors are essential to be considered18. Workflow integration and leadership support are crucial factors that affect the adoption of EHR18–20.
Studies have shown that an encouraging organizational culture is also essential for overcoming resistance and ensuring successful EHR adoption18,21,22. Another significant obstacle is financial constraints, which may arise from a lack of finance for EHR implementation and maintenance, especially in environments with limited resources22. An important case study to examine these factors is the University of Medical Sciences Teaching Hospital (UNIMEDTH) in Nigeria. UNIMEDTH provides a distinctive setting for evaluating the various obstacles militating the implementation of EHR. This is due to its several unsuccessful attempts at the implementation of EHR16.
Encouraging patient outcomes, more accurate diagnoses, and more effective health information interchange are just a few of the possible advantages of electronic health records23,24. However, achieving these advantages necessitates addressing the different organizational, financial, human, technological, knowledge, and usage challenges influencing EHR implementation. While many studies have been done on the challenges of implementing EHR, little research looks critically at how organizational, financial, technological, and human factors interact in the Nigerian context. Whereas systemic problems like poor infrastructure, a lack of resources, and resistance to change are more prevalent in Nigeria’s healthcare system25.
This study therefore examined the interconnection of factors militating the successful implementation of Electronic Health Records (EHR) at the University of Medical Sciences Teaching Hospital (UNIMEDTH) in Nigeria.
Methods
This descriptive cross-sectional research was conducted at the University of Medical Sciences Teaching Hospital (UNIMEDTH), Ondo, a state-owned teaching hospital that was founded on August 7, 2018, by the Ondo State government, Nigeria, with three main responsibilities, including training aspiring medical and health professionals, conducting research, and providing clinical services. The descriptive research method was adopted because it is a non-experimental research type whereby variables are measured using numerical terms and the results can be analyzed quantitatively using frequencies, percentages, averages, or other statistical analyses to determine relationships26.
The population for this study was the members of staff of the UNIMEDTH, Ondo, including doctors, nurses, health information managers, pharmacists, and medical laboratory scientists, and a purposive sampling method was adopted to select seventy-six (76) participants from the total population. This sampling technique was adopted because it is a technique in which units are selected because they have characteristics that a researcher needs in his sample; in other words, units are selected on purpose27.
Data was obtained from the respondents with the aid of a structured questionnaire28, which was divided into four sections, where Sect. 1 assessed the socio-demographic characteristics of the respondents, Sect. 2 investigated the level of knowledge of electronic health records, Sect. 3 assessed the use of electronic health records in patient care, and Sect. 4 examined the factors militating the implementation of electronic health records. This method was considered convenient for data collection from a large number of people within a period while giving the respondents the freedom to express themselves without being intimidated by the presence of the researcher, such as in the interview method29. A Likert scale was used in assessing the respondents, and ethical approval was obtained from the ethical committee of the hospital30.
The University of Medical Sciences Teaching Hospital Research Committee granted ethical approval to conduct the study. (See supplementary material for ethical approval). The research was carried out according to the relevant guidelines and regulations, and informed consent was obtained from the study participants.
The collected data was entered, cleaned, and analyzed using Statistical Product and Service Solutions (SPSS)31 version 27, employing the analysis function to produce descriptive statistics, including percentage distribution, mean, standard deviation, and frequency counts, based on the questionnaire items aligned with the study’s objectives. Divergent stacked bar charts were used to visualize the descriptive statistics for enhanced comprehension of the results, these charts were generated using combo charts in Microsoft Excel.
Regression was used to establish a significant relationship between the awareness and utilization of electronic health records, and correlation was used to detect the interconnections that exist among the factors militating against the effective implementation of EHR.
The hypothesis (H01) “There is no significant relationship between the factors militating against the effective implementation of EHR” was tested using the nonparametric spearman correlation because the responses were graded using Likert scales.
The relationship between the variables of lack of governmental support and financial constraint as well as epileptic power supply and poor internet connectivity were investigated.
Correlation plot was used to visualize the results of the nonparametric spearman correlation analysis, this correlation plot was generated using R.
The findings indicated that the nonparametric spearman correlation between financial constraints and lack of governmental support was negative (r = -0.04, p = ˂ 0.05), but the link between epileptic power supply and poor internet connectivity was positive (r = 0.1, p = ˂ 0.05). Hence, the H01 was rejected because the correlation analysis is statistically significant stating that there is an existence of a relationship between factors militating against the effective implementation of Electronic Health Records. The results demonstrate that increased governmental support would lessen financial constraints, and a stable power supply would decrease poor internet connectivity.
Results
As contained in Table 1, a total of seventy-six consenting respondents were recruited for the study, and the majority of the respondents were females (59.2%). Most of the respondents were between the ages of 30 and 39 (44.7%), signifying that they were in their active working years, and a larger percentage of the respondents were married (71.1%). A larger percentage of the respondents were Yoruba (85.5%) by ethnicity. 59.2% of the respondents had less than 10 years of post-qualification work experience.
Table 1.
Socio-demographic characteristics of the respondents.
| Parameter | Classification | Frequency | Percentage |
|---|---|---|---|
| Gender | Female | 45 | 59.2 |
| Male | 31 | 40.8 | |
| Total | 76 | 100.0 | |
| Age range | 20–29years | 21 | 27.6 |
| 30–39years | 34 | 44.7 | |
| 40–49years | 11 | 14.5 | |
| 50–59years | 10 | 13.2 | |
| Total | 76 | 100.0 | |
| Marital status | Single | 22 | 28.9 |
| Married | 54 | 71.1 | |
| Total | 76 | 100.0 | |
| Ethnicity | Yoruba | 65 | 85.5 |
| Igbo | 11 | 14.5 | |
| Hausa | |||
| Total | 76 | 100.0 | |
| Religion | Christian | 54 | 71.1 |
| Muslim | 22 | 28.9 | |
| Total | 76 | 100.0 | |
| Educational qualification of the respondents | ND/Technician | 9 | 11.8 |
| HND | 16 | 21.1 | |
| BSc | 30 | 39.5 | |
| MSc | 21 | 27.6 | |
| Total | 76 | 100 | |
| Year of working experience | < 10years | 45 | 59.2 |
| 10–20years | 25 | 32.9 | |
| 20–30years | 6 | 7.9 | |
| Total | 76 | 100.0 | |
| Profession of the respondents | Health information management | 16 | 21.04 |
| Nursing | 15 | 19.74 | |
| Medicine | 15 | 19.74 | |
| Pharmacy | 15 | 19.74 | |
| Medical laboratory science | 15 | 19.74 | |
| Total | 76 | 100 |
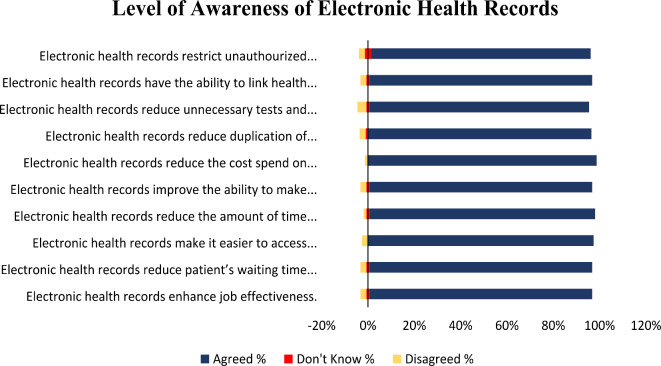
There is broad agreement among participants regarding the advantages of EHR, as shown by the results in Table 2. They concur that EHR improves work effectiveness with a mean of 1.13 (0.66), decreases patient wait times 1.13 (0.66), and facilitates access to medical records outside of hospitals 1.08 (0.48). Furthermore, acknowledged benefits of EHR include enhanced decision-making 1.14 (0.73) and reduced maintenance expenses 1.04 (0.34). While the standard deviations show substantial diversity, indicating some variances in individual judgements, notably about unauthorized access and decreasing unnecessary testing, the consistently low means point to a general consensus regarding the effectiveness of EHR.
Table 2.
Level of awareness of electronic health records.
| Variable N (76) | Agreed % | Don’t know % | Disagreed % | Mean | Standard deviation | Point value |
|---|---|---|---|---|---|---|
| Electronic health records enhance job effectiveness. | 73 (96.1) | 1(1.3) | 2 (2.6) | 1.13 | 0.66 | 2.94 |
| Electronic health records reduce patient’s waiting time in the hospital. | 73 (96.1) | 1(1.3) | 2 (2.6) | 1.13 | 0.66 | 2.94 |
| Electronic health records make it easier to access patients’ medical histories outside the hospital. | 74 (97.4) | 0 | 2 (2.6) | 1.08 | 0.483 | 2.95 |
| Electronic health records reduce the amount of time spent talking to patients. | 74 (97.4) | 1(1.3) | 1 (1.3) | 1.09 | 0.57 | 2.96 |
| Electronic health records improve the ability to make decisions about patients. | 73 (96.1) | 1(1.3) | 2 (2.6) | 1.14 | 0.725 | 2.94 |
| Electronic health records reduce the cost spent on maintaining patients’ health records. | 75 (98.7) | 0 | 1 (1.3) | 1.04 | 0.344 | 2.97 |
| Electronic health records reduce duplication of patients’ health records. | 73 (96.1) | 1(1.3) | 2 (2.6) | 1.13 | 0.66 | 2.94 |
| Electronic health records reduce unnecessary tests and treatments which may be costly and unsafe for the patients. | 72 (94.7) | 1(1.3) | 3 (3.9) | 1.17 | 0.737 | 2.91 |
| Electronic health records have the ability to link health records to sources of relevant and current research. | 73 (96.1) | 1(1.3) | 2 (2.6) | 1.13 | 0.66 | 2.94 |
| Electronic health records restrict unauthorized persons from accessing patients’ medical histories. | 72 (94.7) | 2(2.6) | 2 (2.6) | 1.18 | 0.795 | 2.92 |
Agreed = 3, Don’t know = 2, Disagreed = 1.
The table is elucidated more effectively by the diverging stacked bar charts presented below:
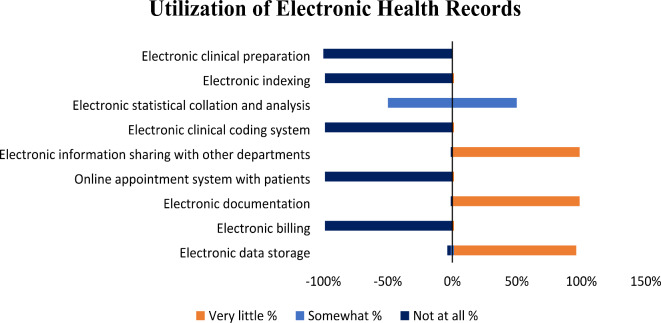
Table 3 shows that the University of Medical Sciences Teaching Hospital (UNIMEDTH) uses its Electronic Health Records (EHR) at a low rate. A mean score of 3.01 (0.115) indicates that 98.7% of respondents reported very limited utilization of electronic documentation and information sharing with other departments. Comparably, adoption of the online appointment system and electronic billing is minimal, likewise with a mean of 3.01 (0.115). The utilization of electronic data storage is marginally better, with 94.7% claiming very little use, yielding a mean of 3.00 (0.231). Both indexing and the electronic clinical coding system are essentially underutilized, with a mean of 3.99 (0.115). Notably, the mean score for electronic statistical collation and analysis is 2.00 (0.000), indicating comprehensive but moderate use, whereas the mean score for electronic clinical preparation is 4.00 (0.000), indicating no use at all. These findings indicate that EHR systems are significantly underutilized, with the majority of their features being used infrequently or never at all. This emphasizes the need for greater adoption and integration.
Table 3.
The level of utilisation of electronic health records.
| Variable N(76) | Very much % | Somewhat % | Very little % | Not at all % | Mean | SD | Point value |
|---|---|---|---|---|---|---|---|
| Electronic documentation | 0 | 0 | 75 (98.7) | 1 (1.3) | 3.01 | 0.115 | 2.00 |
| Electronic information sharing with other departments | 0 | 0 | 75 (98.7) | 1 (1.3) | 3.01 | 0.115 | 2.00 |
| Electronic billing | 0 | 0 | 1 (1.3) | 75 (98.7) | 3.99 | 0.115 | 1.02 |
| Online appointment system with patients | 0 | 0 | 1 (1.3) | 75 (98.7) | 3.99 | 0.115 | 1.02 |
| Electronic data storage | 0 | 2(2.6) | 72 (94.7) | 2 (2.6) | 3.00 | 0.231 | 2.01 |
| Electronic clinical coding system | 0 | 0 | 1 (1.3) | 75 (98.7) | 3.99 | 0.115 | 1.02 |
| Electronic indexing | 0 | 0 | 1 (1.3) | 75 (98.7) | 3.99 | 0.115 | 1.02 |
| Electronic statistical collation and analysis | 0 | 100 (100) | 0 | 0 | 2.00 | 0.000 | 3.01 |
| Electronic clinical preparation | 0 | 0 | 0 | 100 (100) | 4.00 | 0.000 | 1.01 |
Very much = 4, Somewhat = 3, Very little = 2, Not at all = 1.
Fig. 1.
Level of awareness of electronic health records.
The data in this table is represented using diverging stacked bar charts to enhance comprehension of the results.
Fig. 2.
Utilisation of electronic health records.
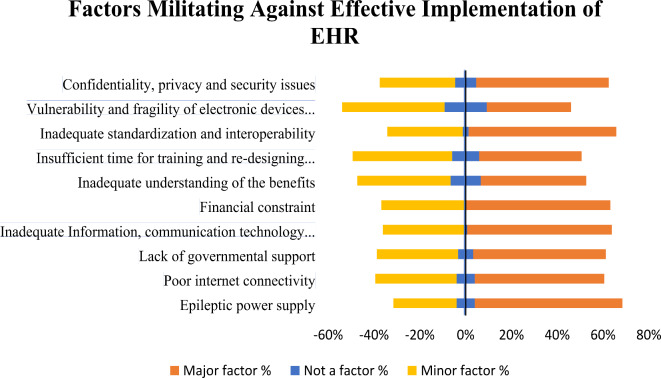
The deployment of Electronic Health Records (EHR) at UNIMEDTH, Ondo, is impeded by various noteworthy aspects, as indicated by Table 4. Financial restrictions (2.63, 0.486), inadequate standardization and interoperability (2.62, 0.541), and limited ICT resources (2.62, 0.516) are the most critical challenges. Major obstacles include an epileptic power supply (2.639) and inadequate internet access (2.4943). Concerns concerning security, privacy, and confidentiality 2.49 (0.663) and a lack of official backing 2.51 (0.622) make the deployment of EHR even more difficult. Notwithstanding their importance, problems like inadequate knowledge of the advantages of EHR 2.33 (0.700) and inadequate time for training and workflow redesign 2.33 (0.681) are viewed as somewhat less urgent. Electronic equipment has a 2.18 (0.725) vulnerability, which is acknowledged but not thought to have a significant impact. These results emphasize that to increase EHR uptake and utilization, resource, budgetary, and infrastructure-related issues must be addressed.
Table 4.
Factors Militating Against the Effective Implementation of Electronic Health Records in UNIMEDTH, Ondo, Ondo State.
| Variable N(76) | Not a factor % | Minor factor % | Major factor % | Mean | SD | Point value |
|---|---|---|---|---|---|---|
| Epileptic power supply | 6 (7.9) | 21 (27.6) | 49 (64.5) | 2.57 | 0.639 | 2.57 |
| Poor internet connectivity | 6 (7.9) | 27 (35.5) | 43 (56.6) | 2.49 | 0.643 | 2.49 |
| Lack of governmental support | 5 (6.6) | 27 (35.5) | 44 (57.9) | 2.51 | 0.622 | 2.51 |
| Inadequate Information, communication technology resources | 1 (1.3) | 27 (35.5) | 48 (63.2) | 2.62 | 0.516 | 2.62 |
| Financial constraint | 0 (0) | 28 (36.8) | 48 (63.2) | 2.63 | 0.486 | 2.63 |
| Inadequate understanding of the benefits | 10 (13.20 | 31 (40.8) | 35 (46.1) | 2.33 | 0.700 | 2.33 |
| Insufficient time for training and re-designing workflow | 9 (11.8) | 33 (43.4) | 34 (44.7) | 2.33 | 0.681 | 2.33 |
| Inadequate standardization and interoperability | 2 (2.6) | 25 (32.9) | 49 (64.5) | 2.62 | 0.541 | 2.62 |
| Vulnerability and fragility of electronic devices such as laptop, desktop, e.t.c | 14 (18.4) | 34 (44.7) | 28 (36.8) | 2.18 | 0.725 | 2.18 |
| Confidentiality, privacy and security issues | 7 (9.2) | 25 (32.9) | 44 (57.9) | 2.49 | 0.663 | 2.49 |
Major factor = 3, Minor factor = 2, Not a factor = 1.
The data in the preceding table is illustrated in the below figure for enhanced comprehension of the results.
Fig. 3.
Factors militating against effective implementation of EHR.
Table 5.
Relationship between the factors militating the effective implementation of electronic health records. ** Correlation is significant at a 0.05 level.
Table 6.
Effect of awareness on electronic health records utilization.
| Hypothesis | Regression weights | Beta co-efficient | R² | F | P-value |
|---|---|---|---|---|---|
| H02 | Awareness of EHR influences its utilisation | 0.049 | 0.15 | 4.26 | 0.008 |
H02: There is no significant effect between the awareness of EHR and its utilisation.
The hypothesis evaluated if awareness has a substantial effect on the utilization of EHR. Linear regression was performed to examine the significance of awareness of the utilization of EHR. The dependent variable (utilisation) was regressed on the independent variable (awareness) to test the hypothesis H0. It was however shown that awareness has a significant effect on the utilisation of EHR (F (3, 72) = 4.26, p < 0.008). This indicates that awareness can play a significant role in the utilisation of EHR (b = 0.049, p < 0.008). Moreover, the R² = 0.151 depicts that the model explains 15.1% of the variance in utilisation, for every unit increase in awareness, utilisation is expected to increase by 0.049 units. Hence, the H0 is not accepted. The table below shows the summary of the findings:
Discussions
The majority of UNIMEDTH employees are women (59.2%), and 44.7% of them are in their 30- to 39-year-old age range, showing that they are an active mid-career demographic. The majority of responders are married, which suggests that their families are supportive. With 85.5% of the workforce being Yoruba, they could influence cross-cultural communication. Less than ten years of post-qualification experience, held by 59.2% of the cohort, suggests possible challenges with implementing new technology.
The findings showed that participants agreed on the various benefits of EHR, which is consistent with previous research32. The agreement that EHR reduces patient wait times and increases work effectiveness is consistent with previous research highlighting its benefits for improving patient management and workflow efficiency33. EHR, for example, have been demonstrated in studies to improve patient flow and reduce administrative burdens by streamlining clinical operations34. Global research supports the idea that EHR improve labour efficiency and reduce patient wait times. Studies conducted in the United States and Europe, for example, show that EHR systems improve patient outcomes by speeding up clinical procedures and reducing waiting times35,36.
The consensus on better access to medical records outside of hospitals supports the findings of previous scholars, who emphasized the vital role that EHR play in guaranteeing continuity of care by providing convenient access to patient histories9. Additionally, participants reported better decision-making, which is consistent with studies showing that EHR facilitates clinical judgements by delivering accurate and swift patient data37. Error reduction and better patient outcomes depend on this functionality. Further supporting findings by scholars15, who talked about the potential for cost savings with EHR by reducing paper records and related storage costs, is the acknowledgement of lower maintenance expenses. Overall, these findings match with international research. Studies in the U.S. and the U.K. reveal that EHR considerably aid the continuity of treatment and promote better clinical judgements through accurate, real-time patient data4,38. Moreover, global studies reveal cost reductions by reducing paper records and storage expenditures39.
Notwithstanding, the notable standard deviations underscore the heterogeneity in subjective assessments, specifically about unapproved entry and the mitigation of excessive laboratory investigations. The literature frequently discusses the security and privacy of data in digital health records, with concerns about unauthorized access being no exception40. While this variance may be because healthcare professionals have varied exposure to and experience with EHR systems, the necessity of strong cybersecurity measures to protect patient information is highlighted in previous studies, both within and outside Nigeria4,41,42. Additionally, the results highlight the difficulty of cutting back on unnecessary laboratory investigations.
Although EHRs are intended to reduce unnecessary testing by providing thorough patient data43, real-world implementation challenges including interoperability and user training may prevent this from happening44. These results highlight how crucial it is for healthcare workers to get ongoing training and assistance to benefit from EHR fully45. The findings further emphasise the hospital’s low rate of EHR utilisation, highlighting major obstacles to successful adoption. The results indicate that 98.7% of the respondents used electronic documentation and information sharing with other departments very little35. This is consistent with previous research which found organisational, technological, and infrastructural barriers to be the main obstacles to EHR implementation in low-resource settings9.
A significant lack of integration of EHR into routine administrative and clinical workflows is indicated by the low adoption of online appointment systems and electronic billing, which is further indicated by a mean score of 3.01(0.115). This underutilisation could be explained by healthcare workers’ aversion to change and inadequate training, which has been noted as a major barrier in comparable situations46. While there has been a slight improvement in the use of electronic data storage (94.7%) of respondents report very little use—the utilisation is still insufficient, with a mean of 3.00(0.231). The efficacy of EHR systems is sometimes hampered in underdeveloped nations by inadequate ICT infrastructure and support, which could account for this restricted uptake47.
The electronic clinical coding system and indexing are almost entirely underutilised, as demonstrated by their means of 3.99(0.115), which further highlights the incomplete integration of EHR features. Scholar48, have highlighted the importance of these elements in boosting data management and clinical documentation efficiency. However, their lack indicates a lost chance to improve care delivery and operational efficiency. The mean score for electronic statistical collation and analysis is 2.00(0.000), which indicates moderate but thorough use, which is interesting49. This shows that while data analytics is being used, it is not being completely utilised, presumably because there is not enough qualified staff or equipment to take full advantage of these capabilities50. In contrast, the mean score of 4.00(0.000) for electronic clinical preparation, which denotes complete non-utilisation, highlights a crucial void in the use of EHR for clinical readiness and planning, that may have a substantial effect on patient outcomes51.
The findings also revealed noteworthy obstacles to the successful implementation of EHR in the hospital which are consistent with more general issues that have been reported in the literature. The main problems are prevalent in many low-resource settings and include budgetary limitations, inadequate standardisation and operability, and limited ICT resources9,52. Financial limitations make it difficult to acquire the required software and hardware, and a lack of standardisation and interoperability makes it difficult to share data across various systems and organisations, which reduces the usefulness of electronic health records12.
The results of the hypothesis testing provide valuable information on the relationship between crucial factors affecting the adoption of EHR, reaching a statistical significance. Increased government engagement may help alleviate financial constraints, according to the negative association (r = -0.04, p < 0.05) between the two. This result is consistent with studies carried out in resource-poor settings, such as Nigeria and other sub-Saharan African countries9,53–55, where regulatory frameworks and government financing were considered necessary to overcome financial barriers to the use of health technology.
Studies conducted in nations like Brazil and India highlight the importance of governmental funding and assistance in removing financial barriers and promoting the successful implementation of EHR systems42,56. Effective government funding and policy initiatives, like the Health Information Technology for Economic and Clinical Health (HITECH) Act, have been linked to higher rates of EHR adoption in well-to-do countries, such as the U.S. and the U.K57,58. This comparison shows that policy-driven financial support is essential at all income levels, but it is especially important in low- and middle-income countries59.
An important infrastructure problem is highlighted by the positive correlation (r = 0.1, p < 0.05) between a faulty power supply and insufficient internet connectivity. These challenges have been reported globally in low-resource settings, including some parts of Southeast Asia and Latin America, where electricity and internet availability are major barriers5,19,60,61. High-income countries, on the other hand, have mostly overcome these infrastructure barriers and have made interoperability and cybersecurity their top concerns. Power and connectivity issues are rarely a barrier in areas like Scandinavia, where digital health infrastructure is highly established62,63. This comparison reveals that in countries like Nigeria, resolving fundamental infrastructure, such as power supply and internet connectivity, is a vital prerequisite for efficient EHR deployment, which contrasts with more advanced EHR ecosystems globally where diverse issues prevail64.
Findings from regression analysis demonstrate that knowledge significantly influences the use of EHR, and the model is statistically significant (F-value = 4.26, p < 0.008). A 0.048-unit increase in EHR utilisation occurs for every unit increase in awareness, according to the coefficient (b = 0.049, p < 0.008). This is consistent with the large body of studies showing how important education and awareness are in encouraging the use of EHR system22,34. Previous research indicates that greater knowledge and understanding of the advantages associated with EHR have a good effect on their adoption. For instance, a study8 found that medical practitioners who are aware of the advantages of EHR are more likely to interact with and use them effectively. Similarly, another study65 found that addressing both the psychological and practical hurdles to adoption, awareness and training had a substantial impact on the successful implementation of EHR systems.
Conclusion and recommendations
This study highlighted important challenges to the adoption of the EHR system at the University of Medical Sciences Teaching Hospital (UNIMEDTH). Although the advantages of EHR are well acknowledged, such as increased work effectiveness and better decision-making, their actual utilization is still low because of some significant obstacles. The most urgent obstacles are limited funds, insufficient ICT resources, and infrastructure problems including unstable electricity supplies and bad internet access. The study also emphasized how important it is for governments to assist in alleviating financial hardships and how raising awareness is crucial to boosting the use of EHR.
However, to address these challenges, UNIMEDTH and relevant parties should concentrate on obtaining financial and political backing while reducing financial obstacles. For EHR systems to be used effectively, investments in a strong ICT infrastructure—including a dependable power source and internet connectivity—are essential. To improve healthcare practitioners’ comprehension of EHR and their advantages, focused awareness campaigns and training programs must be put into place. To ensure the smooth integration of EHR systems across departments, these initiatives should be supplemented with regulations focused on standardization and interoperability. By tackling these issues, UNIMEDTH can greatly increase EHR acceptance and usage, which will enhance healthcare outcomes and delivery.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors acknowledge Okunlola, Oluyemi Adewole for his immense contributions and support in the course of this research work.
Author contributions
A.E.B conceptualized the idea of this research work, A.E.B, I.P.A, D.O.A and K.O.A wrote the main manuscript text, while A.E.B and A.R.B prepared Tables 1, 2, 3, 4, 5 and 6 as well as Figures 1, 2 and 3. All authors reviewed the manuscript.
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Litwin, A. S. Technological change in health care delivery: Its drivers and consequences for work and workers. 1–99. (2020).
- 2.Iyanna, S., Kaur, P., Ractham, P., Talwar, S. & Najmul Islam, A. K. M. Digital transformation of healthcare sector. What is impeding adoption and continued usage of technology-driven innovations by end-users? J. Bus. Res.153, 150–161 (2022). [Google Scholar]
- 3.Wang, W., Ferrari, D., Haddon-Hill, G. & Curcin, V. Electronic Health Records as Source of Research Data. 331–354. (2023). [PubMed]
- 4.Negro-Calduch, E., Azzopardi-Muscat, N., Krishnamurthy, R. S. & Novillo-Ortiz, D. Technological progress in electronic health record system optimization: Systematic review of systematic literature reviews. Int. J. Med. Inform.152, 104507 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dornan, L. et al. Utilisation of electronic health records for public health in Asia: A review of success factors and potential challenges. In BioMed Research International. (Wiley, 2019). [DOI] [PMC free article] [PubMed]
- 6.Mahendher, S., Johar, S. & Patadundi, B. Electronic health record system - benefits and challenges: A literature review. Int. J. Res. Comput. Appl. Manag. (02) 2 . (2020).
- 7.de Mello, B. H. et al. Semantic interoperability in health records standards: a systematic literature review. In Health and Technology. Springer Science and Business Media Deutschland GmbH 255–72. https://link.springer.com/article/10.1007/s12553-022-00639-w (2022). [DOI] [PMC free article] [PubMed]
- 8.Akwaowo, C. D. et al. Adoption of electronic medical records in developing countries—A multi-state study of the Nigerian healthcare system. Front. Digit. Heal4, 1017231 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Attah, A. O. Implementing an electronic health record in a Nigerian secondary healthcare facility. Prospects and challenges. UiT-The Arct Univ Norw Tromso, Norway. 1–82. https://munin.uit.no/bitstream/handle/10037/12245/thesis.pdf?sequence=2&isAllowed=y%0Ahttps://munin.uit.no/handle/10037/12245 (2017).
- 10.Afolabi, O. A., Oladipo, E. K. & Popoola, Y. A. The adoption and challenges associated with the use of electronic health records management system in UNIMEDTH, Ondo, Ondo State. Adeleke Univ. J. Sci.1 (1), 2814–0427 (2022). [Google Scholar]
- 11.Devlin, A. M. et al. Delivering digital health and well-being at scale: Lessons learned during the implementation of the dallas program in the United Kingdom. J. Am. Med. Inf. Assoc.23 (1), 48–59 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alobo, I. G. et al. Implementing electronic health system in nigeria: Perspective assessment in a specialist hospital. Afr. Health Sci. 20 (2), 948–54. (2020). [DOI] [PMC free article] [PubMed]
- 13.Omokanye, S. A. & Adepoju, K. Influence of health information management practices on the quality of healthcare service delivery in OAUTHC Ile-Ife, Osun State Nigeri. World J. Adv. Res. Rev.21 (1), 1752–1765 (2024). [Google Scholar]
- 14.Salam, D. R., Kolawole, I. O., Ohaeri, B. & Babarimisa, O. Electronic health record: An underutilized tool in Nigeria’s healthcare system. Contiental J. Appl. Sci.18, 40–51 (2023). [Google Scholar]
- 15.Alobo, G. I. et al. Implementing electronic health system in Nigeria: perspective assessment in a specialist hospital. Afr. Health Sci.20 (2), 948–54. (2020). [DOI] [PMC free article] [PubMed]
- 16.Ope-Babadele, O. O., Ndurue, L. O. & Isaiah, R. Challenges of electronic health recording implementation by nurses in Babcock University teaching hospital, Ogun State. Commonw. J. Acad. Res.2, 1–12 (2021). [Google Scholar]
- 17.Woldemariam, M. T. & Jimma, W. Adoption of electronic health record systems to enhance the quality of healthcare in low-income countries: a systematic review. BMJ Heal Care Inf.30 (1), e100704 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fennelly, O. et al. Successfully implementing a national electronic health record: a rapid umbrella review. In International Journal of Medical Informatics. 104281 (Elsevier, 2020). [DOI] [PMC free article] [PubMed]
- 19.Tsai, C. H. et al. Effects of electronic health record implementation and barriers to adoption and use: A scoping review and qualitative analysis of the content. Life10 (12), 1–27. (2020). [DOI] [PMC free article] [PubMed]
- 20.Kilgore, D. J. Implementation of an electronic health record-keeping system.1–120. (2020).
- 21.Omosule, V. O. EHR Implementation Success Strategies by Hospital Leaders. Int. J. Adv. Res. 1–64. (2022).
- 22.Adepoju, E. O. & Opele, J. K. Barriers to implementing electronic health information management in patient care I. Background. Artic. IOSR J. Res. Method Educ. 1–24. (2021).
- 23.Hoover, R. Benefits of using an electronic health record. Nurs. Crit. Care12 (1), 9–10 (2017). [Google Scholar]
- 24.Adeniyi, A. O., Arowoogun, J. O., Chidi, R., Okolo, C. A. & Oloruntoba Babawarun. The impact of electronic health records on patient care and outcomes: A comprehensive review. World J. Adv. Res. Rev.21 (2), 1446–1455 (2024). [Google Scholar]
- 25.Mgbodi, G. O. Inadequate healthcare service administration and management in Nigeria and solutions. (2023).
- 26.Nassaji, H. Qualitative and descriptive research: Data type versus data analysis. Lang. Teach. Res.19 (2), 129–132 (2015). [Google Scholar]
- 27.Nikolopoulou, K. What Is purposive sampling ? | Definition & examples when to use purposive sampling purposive sampling methods and examples. 1–12. (2022).
- 28.GebreEyesus, F. A. et al. Levels and predictors of anxiety, depression, and stress during COVID-19 pandemic among frontline healthcare providers in Gurage zonal public hospitals, Southwest Ethiopia, 2020: A multicenter cross-sectional study. PLoS ONE16 (11), 1–24. 10.1371/journal.pone.0259906 (2021). [DOI] [PMC free article] [PubMed]
- 29.Yaddanapudi, S. & Yaddanapudi, L. How to design a questionnaire. Indian J. Anaesth.63 (5), 335–337 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wackenhut, A. F. Ethical considerations and dilemmas before, during and after fieldwork in less-democratic contexts: some reflections from post-uprising Egypt. Am. Sociol.49 (2), 242–257 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Daniel Arkkelin. Using SPSS to understand research and data analysis. Psychol. Curric. Mater. 1, 194. https://scholar.valpo.edu/psych_oer (2014).
- 32.Ariffin, N. A., Ismail, N., bt, A., Kadir, I. K. A. & Kamal, J. I. A. Implementation of electronic medical records in developing countries: Challenges & barriers. Int. J. Acad. Res. Progress Educ. Dev.7 (3), 187–99. (2018).
- 33.Wali, R. M., Alqahtani, R. M., Alharazi, S. K., Bukhari, S. A. & Quqandi, S. M. Patient satisfaction with the implementation of electronic medical records in the Western Region, Saudi Arabia. BMC Fam. Pract.21 (1), 1–6. https://bmcprimcare.biomedcentral.com/articles/ (2018). 10.1186/s12875-020-1099-0 (2020). [DOI] [PMC free article] [PubMed]
- 34.Vos, J. F. J., Boonstra, A., Kooistra, A., Seelen, M. & Van Offenbeek, M. The influence of electronic health record use on collaboration among medical specialties. BMC Health Serv. Res.20 (1), 1–11. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-020-05542-6 (2020). [DOI] [PMC free article] [PubMed]
- 35.Dhillon-Chattha, P., McCorkle, R. & Borycki, E. An evidence-based tool for safe configuration of electronic health records: The eSafety checklist. Appl. Clin. Inf.9 (4), 817–830 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zuo, Z. et al. Data anonymization for pervasive health care: Systematic literature mapping study, JMIR Medical Informatics. (JMIR Publications Inc., 2021). [DOI] [PMC free article] [PubMed]
- 37.Lenert, L., Dunlea, R., Del Fiol, G. & Hall, L. K. A model to support shared decision making in electronic health records systems. Med. Decis. Mak.34 (8), 987–995 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Akila, A., Parameswari, R. & Jayakumari, C. Big data in healthcare: Management, analysis, and future prospects. In: Handbook of Intelligent Healthcare Analytics: Knowledge Engineering with Big Data Analytics. 309–26. https://journalofbigdata.springeropen.com/articles/10.1186/s40537-019-0217-0 (SpringerOpen, 2022).
- 39.Zuniga, A. V. Patient access to electronic health records: Strengths, weaknesses and what’s needed to move forward. Sch. Inf. Student Res. J.5(1) (2015).
- 40.Abouelmehdi, K., Beni-Hessane, A. & Khaloufi, H. Big healthcare data: preserving security and privacy. J. Big Data5 (1), 1–18. https://journalofbigdata.springeropen.com/articles/10.1186/s40537-017-0110-7 (2018).
- 41.Murdoch, B. Privacy and artificial intelligence: challenges for protecting health information in a new era. BMC Med Ethics22 (1), 1–5. https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-021-00687-3 (2021). [DOI] [PMC free article] [PubMed]
- 42.Barbalho, I. M. P. et al. Electronic health records in Brazil: Prospects and technological challenges. In Frontiers in Public Health. (Frontiers Media S.A., 2022). [DOI] [PMC free article] [PubMed]
- 43.Cresswell, K. M., Worth, A. & Sheikh, A. Actor-network theory and its role in understanding the implementation of information technology developments in healthcare. BMC Med. Inf. Decis. Mak.10 (1), 67 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reisman, M. & EHRs The challenge of making electronic data usable and interoperable. P T. 42 (9), 572–5. (2017). [PMC free article] [PubMed]
- 45.Safdari, R., Ghazisaeidi, M. & Jebraeily, M. Electronic health records: Critical success factors in implementation. Acta Inf. Med.23 (2), 102–104 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Casey, J. A., Schwartz, B. S., Stewart, W. F. & Adler, N. E. Using electronic health records for population health research: A review of methods and applications. Annu. Rev. Public Health37 61–81. (2016). [DOI] [PMC free article] [PubMed]
- 47.Castaneda, C. et al. Clinical decision support systems for improving diagnostic accuracy and achieving precision medicine. J. Clin. Bioinform.5 (1). (2015). [DOI] [PMC free article] [PubMed]
- 48.Anian, S. & Ismail, N. Coding error and coder skill in implementing international classification of disease (ICD) case mix system in Malaysia. KPJ Healthc. Univ. Coll. (Icd), 1–19. (2016).
- 49.Kumar, M. et al. Healthcare internet of things (H-IoT): Current trends, future prospects, applications, challenges, and security issues. Electronics (Switzerland). 12 2050. (Multidisciplinary Digital Publishing Institute, 2023).
- 50.Dash, S., Shakyawar, S. K., Sharma, M. & Kaushik, S. Big data in healthcare: management, analysis and future prospects. J. Big Data6 (1), 1–25. https://journalofbigdata.springeropen.com/articles/10.1186/s40537-019-0217-0 (2019).
- 51.Evans, C. et al. Characterising the evidence base for advanced clinical practice in the UK: a scoping review protocol. BMJ Open10 (5), e036192. https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2019-036192 (2020). [DOI] [PMC free article] [PubMed]
- 52.Shah, J. R., Murtaza, M. B. & Opara, E. Electronic health records: Challenges and opportunities. J. Int. Technol. Inf. Manag.23 (3), 1–54 (2014). [Google Scholar]
- 53.Jawhari, B., Ludwick, D., Keenan, L., Zakus, D. & Hayward, R. Benefits and challenges of EMR implementations in low resource settings: A state-of-the-art review (BMC Medical Informatics and Decision Making, 2016). [DOI] [PMC free article] [PubMed]
- 54.Adetoyi, O. E. & Raji, O. A. Electronic health record design for inclusion in sub-Saharan Africa medical record informatics. Sci. Afr.7, e00304 (2020). [Google Scholar]
- 55.Odekunle, F. F., Odekunle, R. O. & Shankar, S. Why sub-Saharan Africa lags in electronic health record adoption and possible strategies to increase its adoption in this region. Int. J. Health Sci. (Qassim) 11 (4), 59–64. (2017). [PMC free article] [PubMed]
- 56.Rodrigo, R. Investigation on reasons and the obstacles that hinder the usability of electronic health records (EHR) systems in India. https://www.researchgate.net/publication/375422540_Investigation_on_reasons_and_the_obstacles_that_hinder_the_usability_of_Electronic_Health_Records_EHR_systems_in_India (2023).
- 57.Modi, S. & Feldman, S. S. The Value of Electronic Health Records since the Health Information Technology for Economic and Clinical Health Act: Systematic Review. (JMIR Publications Inc., 2022). [DOI] [PMC free article] [PubMed]
- 58.Moreno, L., Peikes, D. & Krilla, A. Necessary but not sufficient: The HITECH act and health information technology’s potential to build medical homes. Agency Healthc. Res. Qual. (10). (2010).
- 59.Wiysonge, C. S. et al. Financial arrangements for health systems in low-income countries: An overview of systematic reviews. In Cochrane Database of Systematic Reviews. (John Wiley and Sons, Inc. and the Cochrane Library, 2017). [DOI] [PMC free article] [PubMed]
- 60.Ferry, A. M. et al. Medical documentation in low- and middle-income countries: Lessons learned from implementing specialized charting software. Plast. Reconstr. Surg. Glob. Open 9 (6), E3651. (2021). [DOI] [PMC free article] [PubMed]
- 61.Gesulga, J. M., Berjame, A., Moquiala, K. S. & Galido, A. Barriers to electronic health record system implementation and information systems resources: A structured review. In Procedia Computer Science. 544–551. (Elsevier, 2017).
- 62.do Nascimento, B. I. J. et al. Barriers and facilitators to utilizing digital health technologies by healthcare professionals. In npj Digital Medicine. (Nature Publishing Group, 2023). [DOI] [PMC free article] [PubMed]
- 63.Stamatian, F., Baba, C. O. & Timofe, M. P. Barriers in the implementation of health information systems: A scoping review. Transylvanian Rev. Adm. Sci. (SPEC. ISSUE). 156–73. https://www.researchgate.net/publication/287270890_Barriers_in_the_Implementation_of_Health_Information_Systems_A_Scoping_Review (2013).
- 64.Ugwu Chika, E. et al. Digital healthcare tools in Nigeria: Strengthening public health and pandemic preparedness—Insights from the COVID-19 Crisis. Telehealth Med. Today9https://telehealthandmedicinetoday.com/index.php/journal/article/view/445/1046 (2024).
- 65.Ratwani, R. M. Electronic health records and improved patient care: Opportunities for applied psychology. Curr. Dir. Psychol. Sci.26 (4), 359–65. (2017). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.