Abstract
Abstract
Objectives
In recent years, non-invasive stimulation technologies such as repetitive transcranial magnetic stimulation, transcranial direct current stimulation, bioresonance and auriculotherapy have been used for smoking cessation. Individuals may face various challenges throughout the quitting process. This study aimed to explore the challenges of smoking cessation for users of non-invasive stimulation technologies in Iran.
Design, setting and participants
This parallel-convergent mixed-methods study was conducted using both quantitative and qualitative components. In the quantitative component, a cross-sectional study involved 400 participants, randomly and proportionally sampled from clinics offering non-invasive stimulation technologies for smoking cessation. Data were collected through questionnaires on sociodemographic characteristics and the Challenges to Stopping Smoking scale, with descriptive statistics used for analysis. Participants ranked the challenges based on a predetermined list in the quantitative component. In the qualitative component, 25 users from Tehran, Tabriz and Karaj were selected via purposive and snowball sampling. Data were gathered through in-depth, semistructured individual interviews and analysed using qualitative content analysis with a conventional approach. A merging strategy and convergence model were employed to combine the quantitative and qualitative data.
Results
Quantitative results indicated that 71.5% of participants ranked fear of side effects as a major challenge, making it the most significant issue. Qualitative data also highlighted this, as the primary challenge in smoking cessation. 242 (60.5%) participants declared fear of failure as one of the main challenges. Qualitative data indicated that this often stems from previous unsuccessful quit attempts. The feeling of losing cigarettes was one of the major challenges for 129 (32.2%) participants, reflecting a deep emotional dependency on smoking. While the concern about the cost of using the technology was one of the major challenges for 76 (19.0%) of the participants, qualitative data provided a different perspective, with some participants assessing the high cost of quitting against potential future savings from not buying cigarettes. Fear of relapse was a notable challenge identified in the qualitative data, underscoring the importance of managing triggers and environments during the cessation process.
Conclusions
Fear of side effects and failure were the most significant challenges in smoking cessation using non-invasive stimulation technologies. Emotional dependency on cigarettes and concerns about the cost also played a role. Fear of relapse was highlighted in qualitative data. To overcome the challenges of smoking cessation with non-invasive stimulation technologies, supportive programmes that provide psychological counselling, financial aid and education are essential to improve success rates.
Keywords: Tobacco Use, PUBLIC HEALTH, Smoking Reduction
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The use of a parallel-convergent mixed-methods design, combining both quantitative and qualitative approaches, provided a more thorough understanding of the challenges users face with non-invasive stimulation technologies for smoking cessation.
The simultaneous use of quantitative and qualitative data allowed for the validation and reinforcement of the findings, increasing the reliability of the conclusions.
The inclusion of participants from three major cities in Iran (Tehran, Tabriz and Karaj) enhanced the geographic diversity and potential generalisability of the findings.
The study did not assess nicotine dependence using standardised tools like the Fagerström Test for Nicotine Dependence, which could have provided additional insights into the relationship between addiction levels and challenges of smoking cessation.
Only a limited number of non-invasive stimulation technologies available in Iran were investigated, potentially reducing the generalisability of the results to other technologies and contexts.
Introduction
Smoking is a major risk factor for chronic diseases, premature death and disability.1 Globally, the prevalence of smoking among adults in 2020 was reported to be 32.6% among men and 6.5% among women.2 Globally, smoking behaviours have significantly changed over the past decades, with the proportion of smokers decreasing in many countries, including the USA.3 However, in Iran, the prevalence of smoking has increased, particularly among younger populations and women.4 Most smokers report a desire to quit, but quitting is challenging and often requires multiple attempts to achieve long-term abstinence.5 Despite numerous efforts to quit smoking, few smokers use a wide range of available treatment options. Even the best available treatments achieve a 25%–30% success rate after several months.6
Various interventions help individuals quit smoking. In recent years, non-invasive stimulation technologies such as transcranial direct current stimulation (tDCS), repetitive transcranial magnetic stimulation (rTMS), bioresonance and auriculotherapy have been used for smoking cessation. tDCS is a non-invasive technique that stimulates the brain and can effectively influence human behaviour and perception by modulating cortical brain stimulation.7 On the other hand, rTMS uses magnetic fields to influence the brain’s electrical activity. Young’s study indicated that rTMS shows promise as a tool for smoking cessation.8 However, while initial results are encouraging, this research is preliminary, and further rigorous studies are necessary to confirm the effectiveness of rTMS for smoking cessation. Evidence has shown that tDCS and rTMS technologies can regulate brain activities related to nicotine addiction.9 10 In recent years, bioresonance therapy and auriculotherapy have been used as alternative treatments for various conditions, including smoking cessation.11 12 Bioresonance is a type of energy therapy that involves using electrodes and the Mora Nova device to analyse and process the body’s electromagnetic information.13 Bioresonance is a non-invasive method based on the hypothesis that every substance (including toxins and nicotine) has a specific frequency, and by using bioresonance devices, these frequencies can be identified and balanced, making them effective in reducing nicotine cravings and aiding in smoking cessation.11 Auriculotherapy is similar to acupuncture but uses an imperceptible electrical current instead of traditional needles to stimulate specific points on the ear to facilitate smoking cessation.14 Auriculotherapy can also be used as an effective method for quitting smoking and has shown positive results.15 While some studies show the potential benefits of these technologies on smoking cessation, more rigorous trials are needed to prove their effectiveness.
Individuals attempting to quit smoking may face various challenges. Numerous studies have examined the challenges and barriers to quitting smoking. Personal barriers, including withdrawal symptoms, addiction, higher perceived stress levels, doubt about the ability to quit, concerns about weight gain and environmental factors such as lack of support from healthcare professionals and peers, have been documented.6 16 17 Many individuals struggle with withdrawal symptoms such as irritability, anxiety and intense cravings for cigarettes. These symptoms can make the quitting process difficult.18 Smokers often experience higher stress levels and may use smoking as a coping mechanism. During quitting attempts, the absence of this coping mechanism can exacerbate stress and lead to relapse.19 A lack of confidence in the ability to quit, often stemming from previous unsuccessful attempts, can be a significant barrier. This doubt can diminish the motivation necessary for successful cessation.20 Fear of postcessation weight gain is a common concern, particularly among women, deterring many from attempting to quit.21 Inadequate support from healthcare professionals and lack of encouragement from peers can also make quit attempts more challenging. Successful cessation often requires a support system that many individuals find lacking.22
Identifying the challenges associated with quitting and the various personal and environmental factors influencing smoking behaviour may guide the selection of appropriate supportive strategies that are likely to be effective in future quit attempts.6 Smoking cessation is an interactive phenomenon influenced by various psychological, social, environmental and individual factors.23 Non-invasive stimulation methods can be pricey. It is often a significant barrier for individuals seeking treatment with these technologies.24 The determinants of the use of non-invasive technologies include not only financial capability but also accessibility of the technology.25
Given the limited resources and studies on the use of smoking cessation technologies, particularly the challenges faced by users of non-invasive stimulation technologies in Iran, a qualitative study could be an appropriate approach to this topic, as qualitative research aims to obtain a complete and rich understanding of individuals' experiences. Qualitative researchers typically focus on a phenomenon and gain deep insights into it. This approach may uncover aspects previously unidentified by quantitative studies and context-based findings.26 Considering the complex nature of human behaviour and social phenomena, combining quantitative and qualitative methods in data collection enriches researchers’ understanding of the studied population.27 Qualitative researchers consider triangulation a research strategy to enhance the reliability of the data and provide a more comprehensive understanding of the research topic by examining a phenomenon from multiple methods, data sources or perspectives.28 Completeness of findings refers to the breadth and depth of a researcher’s study, providing a more accurate depiction of a phenomenon. A parallel convergent mixed-methods study evaluates a phenomenon from different dimensions using diverse methods and tools. The more precise, timely, and controlled this integration is, the more accurate and valid the examination can be. The goal of parallel convergent mixed-methods study is to provide a comprehensive analysis of the research issue by converging or merging quantitative and qualitative data.27 29 This study aimed to explore the challenges of smoking cessation for users of non-invasive stimulation technologies through a parallel convergent mixed-methods study.
Methods
Study design
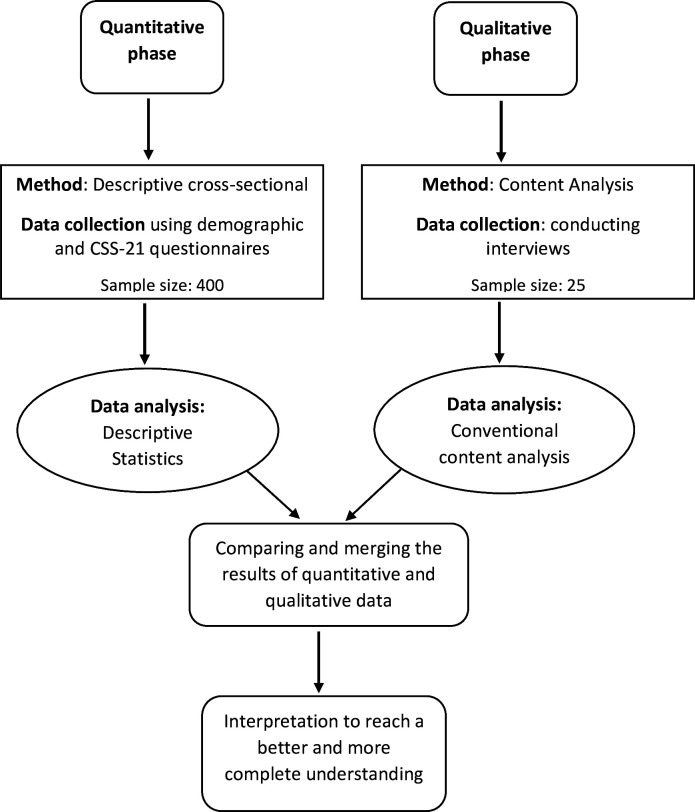
This mixed-method study employed a parallel-convergent design, incorporating both quantitative (descriptive-cross-sectional) and qualitative (content analysis) components. Quantitative and qualitative data were collected and analysed simultaneously and independently. Data analysis was conducted separately, and the results were integrated during the data interpretation (figure 1).
Figure 1. Study visual diagram. This diagram illustrates the parallel-convergent mixed-methods design used in the study. It depicts the simultaneous and independent collection and analysis of both quantitative (descriptive cross-sectional) and qualitative (content analysis) data. The figure also shows the point at which the results from both components were integrated during data interpretation. CSS-21, Challenges to Stopping Smoking-21.
Component one (quantitative study)
Study type, research setting and participants
In this component, a descriptive cross-sectional study was conducted to identify smoking cessation challenges. The study population comprised users of non-invasive smoking cessation technologies. The research settings included the Asayesh Clinic in Tabriz, which uses brain electrical and magnetic stimulation for smoking cessation; the Sana Clinic in Karaj and Mastaneh Clinic in Tehran, which specialises in bioresonance technology for smoking cessation; and the (I Quit Smoking) IQS Clinic in Tehran, which uses auriculotherapy.
The inclusion criteria included users of brain electrical and magnetic stimulation, bioresonance and auriculotherapy technologies for smoking cessation, with at least 6 months have passed since the last treatment session. Successful quitting was defined as abstinence from smoking for 6 months or longer within the past year.30 Exclusion criteria included known and treated psychiatric disorders and co-addiction to substances other than tobacco. Participants who were using other smoking cessation tools, such as e-cigarettes or nicotine replacement therapy, as well as those who were using two non-invasive technologies simultaneously, were excluded from the study.
Sample size and sampling method
The sample size was calculated based on the study by Nurulfarahin et al,16 considering the SD of the most challenging internal factor in smoking cessation (fear of failing to stop smoking) equal to 0.51, α=0.05 and d=0.05, resulting in a sample size of 400 participants. Random and proportional sampling was used based on the total number of eligible visitors to the smoking cessation clinics in Tabriz, Tehran and Karaj. A list of all users of each technology was extracted from the clinic records, and samples were randomly selected using www.random.org. The selected individuals were contacted by phone, the study objectives were briefly explained, and they were asked to visit the clinic at a specified time if they agreed to participate. Upon visiting the clinic, the study objectives were fully explained, and questionnaires were provided after informed consent was obtained. Of the 440 individuals initially approached, 400 participants were included in the study after meeting the inclusion criteria.
Data collection tools
The data were collected using a sociodemographic characteristics questionnaire, and the challenges to stopping smoking scale (CSS-21) were self-reported.
Demographic characteristics questionnaire
This questionnaire included information such as age, gender, education, occupation and family income adequacy. Its validity was evaluated and confirmed through content and face validity.
Challenges to stopping smoking scale
This questionnaire was developed by Thomas et al in 2016 to identify smoking cessation challenges and assess the individual and environmental factors influencing smoking cessation.6 It evaluates two dimensions: internal factors (personal factors such as withdrawal symptoms, feelings and emotions during cessation, comprising nine items) and external factors (environmental factors including support for cessation, cost of cessation, fear of side effects and fear of cessation, comprising 12 items). The respondents rated each of the 21 items on a four-point scale: 1 (no challenge), 2 (minor challenge), 3 (moderate challenge) or 4 (major challenge). Higher scores indicate major challenges. Thomas et al reported Cronbach’s alpha coefficients of 0.86 for internal factors and 0.82 for external factors.6
In this study, the questionnaire was translated into Persian using the forward-backward translation method. The content and face validity of the questionnaire were assessed and confirmed. The impact scores of all the items were above 1.5, confirming the face validity of the scale. CVI and CVR indices were used for content validity. A CVI of 0.8 or higher31 and a CVR above 0.4932 were considered acceptable. The CVRs ranged from 0.71 to 1.0, and the CVIs ranged from 0.84 to 1.0, confirming the content validity of the items. The overall CVI and CVR for the tool were 0.96 and 0.97, respectively. Construct validity was assessed by calculating the corrected item-total correlation, with values above 0.3 indicating suitable construct validity.33 The Cronbach’s alpha values for the internal and external factors and the overall scale were 0.85, 0.81 and 0.83, respectively. The intraclass correlation coefficients for the internal and external factors and the overall scale were 0.93, 0.91 and 0.92, respectively.
Data analysis
Descriptive statistics, including frequency (percentage) and mean (SD), were used to describe sociodemographic characteristics and smoking cessation challenges using SPSS V.24 software.
Component two (qualitative study)
Study type
This component involved a qualitative study using conventional content analysis to explore smoking cessation challenges in more detail. This approach obtains data directly from participants without imposing predefined categories or theories.34 This study adheres to the Standards for Reporting Qualitative Research (SRQR) guidelines. The completed SRQR checklist can be found in online supplemental file 1.
Participants and sampling method
Using purposive and snowball sampling methods, participants were selected from users of smoking cessation technologies (electrical and magnetic brain stimulation, bioresonance and auriculotherapy). Participants were chosen based on the study’s objectives, seeking those with sufficient information about the phenomenon. A range of ages and individuals who were successful and unsuccessful in quitting smoking with these technologies were included. Snowball sampling involved asking initial participants to refer others with similar characteristics. Sampling continued until data saturation (when new participants provided no new information) was achieved, resulting in 25 participants: eight using auriculotherapy, nine using bioresonance, five using rTMD and three using tDCS.
Data collection method
The data were collected through semistructured, in-depth interviews. The researcher visited the research setting, selected suitable participants, explained the study objectives and invited the participants to participate. The interviews were scheduled at the participant’s convenience and were conducted at the smoking cessation clinic or other preferred locations (workplace and park). The interviews started with general questions such as ‘What challenges did you face using this technology?’ and ‘Please explain your concerns during the smoking cessation period’. Follow-up probing questions were asked based on responses to gain deeper insights. Each interview lasted 30–60 min.
Data analysis
In the qualitative component, data analysis began with repeatedly reading the entire text to gain a comprehensive understanding. Subsequently, the texts were read word by word to extract codes. Initially, concrete words from the text that seemed to encompass the main concepts were identified. The researcher advanced the text analysis by note-taking from the initial analysis, continuing this process until preliminary codes began to emerge. Throughout this process, code labels representing more than one core idea were identified. This study used the conventional content analysis method proposed by Graneheim and Lundman.34 This method allows for accessing both the explicit content of the interview texts and the latent content and more abstract concepts. Based on this method, the following five steps were taken.
The entire interview was transcribed immediately after each interview was conducted.
The entire text was repeatedly read to gain a comprehensive understanding of its content.
The text was divided into meaning units, the summaries of these meaning units were extracted, and the units were coded.
The initial codes were classified into subcategories and categories based on comparisons of their similarities and differences.
The themes were extracted as expressions of the latent content and concepts within the data.
MAXQDA V.24 software was used for data management.
Rigour
This study adhered to the criteria for ensuring rigour as outlined by Guba and Lincoln, including credibility, transferability, dependability and confirmability.35 36 The researcher enhanced the credibility of the findings through prolonged engagement with the data, repeated readings of the interviews and reviewing the coding processes. After coding the interviews, the coded text was provided to the participants to verify the accuracy and relevance of the codes to their experiences. Additionally, the codes were reviewed by expert faculty members who critiqued and provided corrective feedback, which ultimately led to the validation of the coding and categories. The researcher contributed to the rigour of the study by maintaining documentation and detailed reporting at all stages, allocating sufficient time for data collection and maintaining objectivity and neutrality. To enhance transferability, the researcher described the research process and characteristics of the study population clearly and precisely, enabling others to trace the research path and understand the study population’s characteristics. Furthermore, the results were presented to some participants and other individuals to assess the similarity of the findings with their experiences. To ensure dependability, the research stages, decisions and activities regarding data collection and analysis were documented. Initial codes were derived from interpreting the participants’ experiences, including examples of theme extraction and excerpts from the interviews. To increase authenticity, the researcher endeavoured to honestly narrate the participants’ words, feelings and experiences.
Strategy for combining quantitative and qualitative data
To combine quantitative and qualitative data, a merging strategy was used, interpreting the results by comparing and integrating the quantitative and qualitative data for a more comprehensive understanding. The convergence model27 was employed for this purpose. In the convergence model, the researcher compared the different results during the interpretation phase after analysing the quantitative and qualitative data.
Results
Quantitative component
The average age of the participants in this study was 39.66±9.50 years, with an age range of 18–65 years. Most participants were male (75.5%), married (80.5%) and had a bachelor’s degree (68.7%). In terms of family income, more than 60% had expenses exceeding their income (table 1). The participants’ average daily cigarette consumption over 1 year was 28.52 cigarettes, with an SD of 23.61 (range: 0–100), and the years of daily smoking averaged 22.14 years, with an SD of 9.49 (range: 4–54) years. Of the 400 participants, 329 (82.3%) successfully quit smoking following the use of non-invasive stimulation technologies.
Table 1. Sociodemographic characteristics of the participants (n=400).
| Variables | Status | Frequency | Per cent |
| Gender | Male | 302 | 75.5 |
| Female | 98 | 24.5 | |
| Marital status | Single | 78 | 19.5 |
| Married | 322 | 80.5 | |
| Education | Diploma and below | 61 | 15.3 |
| Associate Degree | 38 | 9.5 | |
| Bachelor’s degree | 275 | 68.7 | |
| Masters’ degree and higher | 26 | 6.5 | |
| Socioprofessional situation | Unemployed | 22 | 5.5 |
| Worker | 34 | 8.5 | |
| Employee | 110 | 27.5 | |
| Free | 155 | 38.7 | |
| Retired | 42 | 10.5 | |
| Housekeeper | 37 | 9.3 | |
| Household income | Income less than expenses | 247 | 61.7 |
| Income equals expenses | 130 | 32.5 | |
| More income than expenses | 23 | 5.8 |
The distribution and mean scores of the items related to smoking cessation challenges are presented in table 2. As shown in this table, the most significant challenges included fear of side effects, fear of failure to quit smoking, the feeling of losing something without smoking, the belief that they could quit smoking in the future if needed and severe dependence on cigarettes.
Table 2. Distribution of the frequency and mean scores of the items related to the challenges of quitting smoking using non-invasive stimulation technologies (n=400).
| Statements | Not a challengen (%) | Minor challengen (%) | Moderate challengen (%) | Major challengen (%) | Mean±SD | Priority |
|
100 (25.0) | 144 (36.0) | 111 (27.8) | 45 (11.2) | 0.95±2.25 | 7 |
|
26 (6.5) | 93 (23.3) | 152 (38.0) | 129 (32.2) | 0.90±2.96 | 3 |
|
51 (12.7) | 183 (45.8) | 124 (31.0) | 42 (10.5) | 0.83±2.39 | 6 |
|
220 (55.0) | 138 (34.5) | 22 (5.5) | 20 (5.5) | 0.80±1.60 | 14 |
|
160 (40.0) | 122 (30.5) | 94 (23.5) | 24 (6.0) | 0.93±1.95 | 8 |
|
176 (44.0) | 145 (36.2) | 63 (15.8) | 16 (4.0) | 0.84±1.79 | 9 |
|
177 (44.2) | 151 (37.8) | 55 (13.8) | 17 (4.2) | 0.83±1.78 | 10 |
|
205 (51.2) | 107 (26.8) | 65 (16.2) | 23 (5.8) | 0.92±1.76 | 11 |
|
197 (49.2) | 138 (34.5) | 41 (10.3) | 24 (6.0) | 0.87±1.73 | 12 |
|
299 (74.7) | 61 (15.3) | 20 (5.0) | 20 (5.0) | 0.80±1.40 | 17 |
|
329 (82.2) | 27 (6.8) | 23 (5.7) | 21 (5.3) | 0.80±1.34 | 20 |
|
40 (10.0) | 103 (25.8) | 181 (45.2) | 76 (19.0) | 0.88±2.73 | 4 |
|
15 (3.8) | 19 (4.7) | 80 (20.0) | 286 (71.5) | 0.75±3.59 | 1 |
|
322 (80.5) | 35 (8.8) | 24 (6.0) | 19 (4.7) | 0.79±1.35 | 19 |
|
299 (74.7) | 41 (10.3) | 38 (9.5) | 22 (5.5) | 0.87±1.45 | 15 |
|
324 (81.0) | 33 (8.3) | 19 (4.7) | 24 (6.0) | 0.82±1.35 | 18 |
|
27 (6.8) | 21 (5.2) | 110 (27.5) | 242 (60.5) | 0.86±3.41 | 2 |
|
227 (56.7) | 118 (29.5) | 31 (7.8) | 24 (6.0) | 0.86±1.63 | 13 |
|
299 (74.7) | 58 (14.5) | 24 (6.0) | 20 (5.0) | 0.81±1.41 | 16 |
|
102 (25.5) | 82 (20.5) | 95 (23.8) | 121 (30.2) | 1.16±2.58 | 5 |
|
335 (83.7) | 27 (6.7) | 17 (4.3) | 21 (5.3) | 0.78±1.31 | 21 |
Qualitative component
Based on content analysis, six themes related to the challenges of quitting smoking were identified.
Fear of side effects
Fear and concern about side effects were significant challenges for participants in the interviews. Participants reported experiencing short-term and mild headaches and discomfort at the stimulation site during the initial sessions of using rTMS and tDCS technologies and feared that these side effects might continue or worsen throughout the quitting process.
At first, I was afraid that this device might harm me, and that is why I was scared to use it. (Participant 1)
Before using the device and during the first session, I was more worried about its side effects, thinking it might have serious consequences for me. (Participant 9)
Short-term experience of withdrawal symptoms
One of the significant challenges mentioned by participants was experiencing smoking withdrawal symptoms. The participants in the interviews reported symptoms such as irritability, anger, sleep problems, dry mouth, depression, anxiety, lack of concentration in daily tasks and restlessness during the quitting days.
For the first two or three days, I also had a dry mouth, but with the doctor’s recommendation to drink plenty of fluids and use gum, I followed those instructions, and it was resolved. (Participant 10)
Another challenge I faced was feeling discomfort and depression during the treatment process. The doctor told me that sometimes this unpleasant feeling could be due to quitting smoking and chemical changes in the brain. This challenge was very difficult for me. (Participant 21)
During quitting, I had headaches in the first few days, felt restless, and was anxious. This situation only lasted for the first few days, but after that, I had no problems. (Participant 12)
Concern about failure
Participants in this study were worried about failing to quit smoking. For some, this concern stemmed from previous unsuccessful attempts to quit smoking. These individuals felt that quitting smoking was a difficult challenge and doubted their ability to succeed, leading to feelings of hopelessness.
I was worried that I would not be able to quit smoking with this method either. Although I had researched bioresonance and concluded that it would be effective, I was still concerned that I might not be able to quit. (Participant 3)
When I was going to the clinic, I was scared that I might relapse and smoke again because of my first failed attempt. (Participant 13)
Feeling of losing cigarette
Participants in the study felt like they were losing something dear to them by quitting smoking. Cigarettes might have been an important tool in their lives, and losing this tool could significantly impact them.
At first, it was like losing a loved one; I was mourning at home and did not want to go out. I kept thinking to myself, “Oh God, what am I going to do without cigarettes?” (Participant 1)
The journey from home to the clinic was truly strange for me. It felt like something that had been with me for 17 years was being taken away, like losing a loved one who was always by my side. That first moment of giving up cigarettes felt like losing someone dear. My hands were shaking, and it was as if I wanted to beg them not to take it away. After the first session, I went home. I used to smoke a cigarette as soon as I got home to relax. I reached home and thought, “What do I do now?” It was a strange feeling of helplessness like my tools for life were taken away, and I had to live without them. It was a very weird experience, and I kept thinking about how I was going to live without this tool.(Participant 7)
Fear of relapse
Fear of returning to smoking in specific environments and situations and anxiety about relapsing were significant challenges during the quitting process. Participants in this study were worried about relapsing when exposed to certain environments and situations.
I was afraid that if I went out, I might suddenly crave it and buy a cigarette, or if I smelled it, I would want it. It took me about two or three weeks before I went out because I was scared of relapsing. (Participant 1)
Until the last session, I had this anxiety that I might want to smoke again and that I would not be able to quit. (Participant 2)
Cost of using technology
The cost of quitting with technology was a significant challenge in the quitting process. Participants had concerns about the expenses associated with using technology to quit smoking. The high cost of using such technology could be a major barrier and make it difficult for some individuals to decide to use these modern methods. However, when individuals realise that spending on quitting could ensure their health and prevent future costs associated with buying cigarettes, they might be more encouraged to use these technologies.
The biggest challenge for me was the cost of this method. rTMS is a relatively new and advanced treatment method and is quite expensive. However, I went to this clinic with the hope that by spending money, I could ensure my health. Compared to the cost of buying cigarettes, which I would have spent much more on over the years if I did not quit, the cost of quitting with this method was incomparable. (Participant 24)
Discussion
This study examines the main challenges and concerns individuals face in the process of quitting smoking using non-invasive stimulation technologies. By integrating quantitative and qualitative findings, we can draw a comprehensive picture of the challenges faced by those trying to quit smoking with the help of non-invasive stimulation technologies.
One of the primary challenges for users of non-invasive stimulation technologies in quitting smoking was the fear and concern about the side effects of these technologies. Both quantitative and qualitative data emphasised the fear of side effects. Quantitatively, it was ranked as the main concern, which was corroborated by qualitative data detailing specific side effects such as headaches and discomfort. Participants in this study reported experiencing headaches and mild discomfort at the stimulation site during the initial sessions of rTMS and tDCS. Although these side effects were temporary and mild, they caused concern among participants about the persistence and intensification of these effects throughout the quitting process. In the study by Tobaiqy et al in Saudi Arabia, fear of side effects was reported as one of the most significant challenges in quitting smoking.37 Similarly, Morphett et al identified fear of side effects as a major reason for not using prescribed smoking cessation medications.38 Concerns about treatment side effects can pose serious barriers to the quitting process39 and may lead to a failure to quit smoking. Fear and concern about side effects indicate a need for more information and education for users of these technologies.
The findings of this study revealed that one of the most significant concerns of participants was the fear of failure in the process of quitting smoking. The fear of failure to quit smoking was the second most common quantitative concern and was supported by qualitative data showing that this fear often stemmed from previous unsuccessful attempts. This concern was particularly pronounced among individuals who had previously experienced unsuccessful attempts to quit smoking. The results suggest that past unsuccessful experiences can act as a significant psychological barrier to quitting smoking. Those who have faced repeated failures feel that they might never succeed in quitting smoking. This concern and doubt can be examined from several perspectives. Previous unsuccessful experiences can lead to the formation of negative emotions and mental patterns.40 In such situations, individuals doubt their ability to quit smoking, and their self-confidence decreases. Research shows that negative emotions and mental patterns, along with a lack of self-confidence, can significantly reduce the success rate of quitting smoking.41,43 Repeated failures in quitting smoking may cause stress and despair, leading to low self-confidence in attempting or succeeding in future efforts.44 Therefore, individuals in the process of quitting smoking need more psychological support. Counselling and psychological support can help increase self-confidence and change negative mental patterns, thereby increasing the likelihood of success in quitting smoking.
The results indicated that individuals felt as though they were losing a ‘loved one’ and an important tool in their lives when quitting smoking. The quantitative data identified this as the third major challenge. The qualitative findings revealed a deep emotional connection to smoking, confirming that individuals experienced a sense of losing a significant part of their lives when they quit smoking. These findings indicate that for some people, smoking is more than just a habit or physical dependency; it has become an important part of their life and identity. This phenomenon can be attributed to various factors, including the psychological and social roles of smoking and the emotional attachment people develop. Smoking can be used as a tool for stress management or even for creating social bonds.45 Therefore, quitting smoking may be an important tool. Some individuals might feel that quitting smoking is akin to losing a friend or companion due to emotional attachment.46 This emotional dependency can increase the difficulty of quitting smoking. Those who see smoking as an important tool in their lives may need to find alternative mechanisms to cope with stress or create social bonds, which can help them better manage the quitting process.
The findings of this study also indicated that the cost of using smoking cessation technologies was a significant challenge in the quitting process. While the quantitative component ranked financial concerns as the fourth challenge, the qualitative data presented a different perspective in which some participants evaluated this issue against the potential future savings from not buying cigarettes. The high cost of smoking cessation treatments can be a serious barrier to individuals deciding to use these methods.47 This is especially prominent for individuals with limited income or low financial capability. However, it should be noted that investing in smoking cessation technologies can have significant long-term benefits. Those who successfully quit smoking not only improve their health but also avoid the future costs of buying cigarettes. Raising awareness about the long-term economic and health benefits of using smoking cessation technologies can play a crucial role in encouraging people to use these technologies.
Experiencing withdrawal symptoms was highlighted as one of the major challenges faced during the quitting process. Although this challenge ranked seventh in the quantitative data, it was also highlighted as a challenge in the qualitative findings, bringing attention to specific issues such as irritability and sleep problems. An important point regarding the experience of withdrawal symptoms was that most participants mentioned that these symptoms were short-term and present in the early days of quitting. Quitting smoking causes physiological changes in the body, which manifest as withdrawal symptoms. Nicotine is an addictive substance, and its cessation can lead to symptoms such as anger, irritability, depression, anxiety and restlessness.48 These symptoms can be due to physical and psychological dependency on cigarettes and changes in neurotransmitter levels, such as dopamine, that occur when nicotine use is stopped.49 Experiencing withdrawal symptoms can significantly impact the quality of life and daily functioning of individuals.50 Craving for cigarettes is one of the major challenges in the quitting process and can lead to relapse.51 This craving can be triggered by various factors, such as stress, the environment and even daily habits.52 53 These problems can reduce the motivation and ability of individuals to continue smoking. Therefore, providing appropriate support and developing effective strategies to manage these symptoms can help individuals successfully quit smoking. The use of these technologies can help individuals experience these symptoms with lower intensity and duration.
One of the challenges participants in this study mentioned was the fear of relapse. Although this challenge did not rank highly in the quantitative data, it was significantly highlighted in the qualitative component by the participants, indicating an important concern about managing triggers and specific environments during the quitting process. Many smokers face specific triggers that prompt smoking. These triggers can include social situations and daily stresses.54 These triggers can easily lead to relapse, especially if the individual is not fully aware of them and does not have effective strategies to manage them. Fear of relapse can have negative psychological effects, including depression.55 These concerns can lead to reduced self-confidence and a sense of control over the quitting process. To reduce the risk of relapse, planning and using preventive strategies, which can include identifying personal triggers, developing coping strategies and making changes in the individual’s living and working environment, are essential.
The quantitative component of the study showed that one of the challenges in quitting smoking was that many participants believed they could quit smoking in the future if needed. This belief can be a serious barrier to smoking cessation efforts, causing delays in taking action and reducing motivation to start the quitting process. This challenge was also identified as a significant barrier to smoking cessation in a study by Marzo et al56 This issue may stem from individuals’ lack of full understanding of the complexity and length of the quitting process. Therefore, smoking cessation programmes should clearly explain to individuals that quitting smoking is a complex and time-consuming process that requires continuous effort and ongoing decision-making. Additionally, educational programmes that emphasise the importance of immediate action for health improvement and strengthen motivation to quit smoking can help reduce the negative impacts of misconceptions such as ‘I can quit whenever I want’.
In this study, the simultaneous use of quantitative and qualitative methods allowed for a more comprehensive and in-depth examination of the challenges and concerns of users of non-invasive stimulation technologies. The reinforcement and validation of the quantitative results with qualitative data increased the accuracy and reliability of the findings. Moreover, selecting participants from three populous cities in Iran contributed to the diversity of the data and the generalisability of the results. There were a few limitations in this study. One limitation of this study is that we did not assess nicotine dependence levels using standardised tools, such as the Fagerström Test for Nicotine Dependence. Evaluating nicotine addiction levels could provide additional insights into participants' smoking behaviours and their challenges during the cessation process. Future studies should consider including such assessments to obtain a more detailed understanding of the relationship between addiction levels and smoking cessation success. The results of the quantitative component are based on cross-sectional data and may not reflect long-term challenges and concerns regarding the technologies. Therefore, future longitudinal studies in this area are recommended. This study examined only a few types of non-invasive stimulation technologies available in Iran and did not consider other technologies. Consequently, future studies should also include users of other non-invasive stimulation technologies in different countries. This study did not examine the impact of contextual psychological and social factors on the challenges of quitting smoking with these technologies, so future research should investigate the influence of psychological and social factors such as family support, stress and working conditions on smoking cessation challenges. Although sample selection was randomised, this study includes a high proportion of participants who successfully quit smoking, which may suggest selection bias. Future research should aim to include a more diverse sample, including those with unsuccessful outcomes, to provide a comprehensive view of the challenges of these technologies.
Conclusion
Both quantitative and qualitative data emphasised the fear of side effects as a major challenge. Fear of failure ranked second in the quantitative data, and qualitative data indicated that this was often due to previous unsuccessful attempts to quit. The sense of loss associated with quitting smoking was identified as the third major challenge in the quantitative data, reflecting a deep emotional attachment to smoking. While concern over the cost of using the technology ranked fourth in the quantitative findings, qualitative data offered a different perspective, where some participants evaluated the high cost of quitting against potential future savings from not buying cigarettes. The experience of withdrawal symptoms ranked seventh in the quantitative data, but qualitative findings highlighted this issue as a significant challenge. Fear of relapse did not rank highly in the quantitative data but did significantly increase in the qualitative data, indicating a key concern about managing triggers and specific environments during the quitting process.
Overall, this study emphasises the importance of developing comprehensive and multidimensional strategies to support individuals aiming to quit smoking using non-invasive stimulation technologies. Success in quitting smoking with these technologies requires supportive programmes that address various psychological, economic and social aspects. Providing psychological counselling, financial and educational support and developing techniques for stress and trigger management can help reduce challenges and increase the likelihood of successful smoking cessation with these technologies.
supplementary material
Acknowledgements
The researchers are deeply grateful to the Vice-Chancellery for Research and Technology of Tabriz University of Medical Sciences and the staff and colleagues at Asayesh Tabriz Clinic, Sana Karaj Clinic, Mastaneh Clinic and IQS Tehran Clinic for their assistance in facilitating participant interviews. We also thank the participants who dedicated their time to the interviews.
Footnotes
Funding: This study was funded by Tabriz University of Medical Sciences (Grant Number: 71437).
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2024-091253).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: This study involves human participants. The study received approval from the Ethics Committee of the Deputy of Research and Technology of Tabriz University of Medical Sciences (Ethics Code: IR.TBZMED.REC.1402.151). Participants gave informed consent to participate in the study before taking part.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Contributor Information
Mohammad Hasan Sahebihagh, Email: sahebihagh@yahoo.com.
Mina Hosseinzadeh, Email: m.hosseinzadeh63@gmail.com.
Mojgan Mirghafourvand, Email: mirghafourvand@gmail.com.
Parvin Sarbakhsh, Email: p.sarbakhsh@gmail.com.
Hossein Nemati, Email: nematihossein72@gmail.com.
Data availability statement
Data are available upon reasonable request.
References
- 1.Farcher R, Syleouni ME, Vinci L, et al. Burden of smoking on disease-specific mortality, DALYs, costs: the case of a high-income European country. BMC Public Health. 2023;23:698. doi: 10.1186/s12889-023-15535-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dai X, Gakidou E, Lopez AD. Evolution of the global smoking epidemic over the past half century: strengthening the evidence base for policy action. Tob Control. 2022;31:129–37. doi: 10.1136/tobaccocontrol-2021-056535. [DOI] [PubMed] [Google Scholar]
- 3.Cornelius ME, Loretan CG, Jamal A, et al. Tobacco Product Use Among Adults - United States, 2021. MMWR Morb Mortal Wkly Rep. 2023;72:475–83. doi: 10.15585/mmwr.mm7218a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ravaghi H, Tourani S, Khodayari-Zarnaq R, et al. Agenda-setting of tobacco control policy in Iran: a retrospective policy analysis study. BMC Public Health. 2021;21:2288. doi: 10.1186/s12889-021-12339-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Borland R, Partos TR, Yong HH, et al. How much unsuccessful quitting activity is going on among adult smokers? Data from the International Tobacco Control Four Country cohort survey. Addiction. 2012;107:673–82. doi: 10.1111/j.1360-0443.2011.03685.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thomas D, Mackinnon AJ, Bonevski B, et al. Development and validation of a 21-item challenges to stopping smoking (CSS-21) scale. BMJ Open. 2016;6:e011265. doi: 10.1136/bmjopen-2016-011265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zvolska K, Pankova A, Nohavova I, et al. A narrative review of facilitators and barriers to smoking cessation and tobacco-dependence treatment in patients with tuberculosis in low- and middle-income countries. Tob Induc Dis. 2020;18:67. doi: 10.18332/tid/125195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Young J. rTMS for smoking cessation in primary care. Brain Stimulation: Basic, Translational, and Clinical Research in Neuromodulation. 2023;16:139. doi: 10.1016/j.brs.2023.01.079. [DOI] [Google Scholar]
- 9.Mondino M, Luck D, Grot S, et al. Effects of repeated transcranial direct current stimulation on smoking, craving and brain reactivity to smoking cues. Sci Rep. 2018;8:8724. doi: 10.1038/s41598-018-27057-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tang VM, Goud R, Zawertailo L, et al. Repetitive transcranial magnetic stimulation for smoking cessation: Next steps for translation and implementation into clinical practice. Psychiatry Res. 2023;326:115340. doi: 10.1016/j.psychres.2023.115340. [DOI] [PubMed] [Google Scholar]
- 11.Pihtili A, Galle M, Cuhadaroglu C, et al. Evidence for the efficacy of a bioresonance method in smoking cessation: a pilot study. Forsch Komplementmed. 2014;21:239–45. doi: 10.1159/000365742. [DOI] [PubMed] [Google Scholar]
- 12.Vieira A, Reis AM, Matos LC, et al. Does auriculotherapy have therapeutic effectiveness? An overview of systematic reviews. Complement Ther Clin Pract. 2018;33:61–70. doi: 10.1016/j.ctcp.2018.08.005. [DOI] [PubMed] [Google Scholar]
- 13.Muresan D, Voidăzan S, Salcudean A, et al. Bioresonance, an alternative therapy for mild and moderate depression. Exp Ther Med. 2022;23:264. doi: 10.3892/etm.2022.11190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fritz DJ, Carney RM, Steinmeyer B, et al. The efficacy of auriculotherapy for smoking cessation: a randomized, placebo-controlled trial. J Am Board Fam Med. 2013;26:61–70. doi: 10.3122/jabfm.2013.01.120157. [DOI] [PubMed] [Google Scholar]
- 15.Di YM, May BH, Zhang AL, et al. A meta-analysis of ear-acupuncture, ear-acupressure and auriculotherapy for cigarette smoking cessation. Drug Alcohol Depend. 2014;142:14–23. doi: 10.1016/j.drugalcdep.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 16.Nurulfarahin KA, Nina SA, Lailati S, et al. Challenges to Quit Smoking among Smokers in Bandar Baru Salak Tinggi, Sepang, Selangor, Malaysia. IJPHS. 2018;7:65. doi: 10.11591/ijphs.v7i1.10759. [DOI] [Google Scholar]
- 17.Can Gür G. Psychometric properties of the Turkish version: the challenges to stopping smoking (CSS-21) scale. J Subst Use. 2021;26:107–13. doi: 10.1080/14659891.2020.1846090. [DOI] [Google Scholar]
- 18.Cui ZY, Li YH, Liu Z, et al. The experience of tobacco withdrawal symptoms among current smokers and ex-smokers in the general population: Findings from nationwide China Health Literacy Survey during 2018-19. Front Psychiatry. 2022;13:1023756. doi: 10.3389/fpsyt.2022.1023756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patterson JG, Macisco JM, Glasser AM, et al. Psychosocial factors influencing smoking relapse among youth experiencing homelessness: A qualitative study. PLoS One. 2022;17:e0270665. doi: 10.1371/journal.pone.0270665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rajani NB, Mastellos N, Filippidis FT. Self-Efficacy and Motivation to Quit of Smokers Seeking to Quit: Quantitative Assessment of Smoking Cessation Mobile Apps. JMIR Mhealth Uhealth. 2021;9:e25030. doi: 10.2196/25030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Germeroth LJ, Levine MD. Postcessation weight gain concern as a barrier to smoking cessation: Assessment considerations and future directions. Addict Behav. 2018;76:250–7. doi: 10.1016/j.addbeh.2017.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Veeraiah S, Elangovan V, Tripathy JP, et al. Quit attempts among tobacco users identified in the Tamil Nadu Tobacco Survey of 2015/2016: a 3 year follow-up mixed methods study. BMJ Open. 2020;10:e034607. doi: 10.1136/bmjopen-2019-034607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Crossnohere NL, Davey-Rothwell M, Latkin C, et al. The Interaction of Smoking Cessation Norms and Nicotine Dependence on Quit Attempts: Gender-Stratified Results for Low-Income Smokers in Baltimore, MD. Subst Use Misuse. 2020;55:424–8. doi: 10.1080/10826084.2019.1683200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yam P. Brain stimulation poised to move from last resort to frontline treatment. Proc Natl Acad Sci USA. 2024;121:e2401731121. doi: 10.1073/pnas.2401731121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yu Y, Jain B, Anand G, et al. Technologies for non-invasive physiological sensing: Status, challenges, and future horizons. Biosens Bioelectron X. 2024;16:100420. doi: 10.1016/j.biosx.2023.100420. [DOI] [Google Scholar]
- 26.Tenny S, Brannan JM, Brannan GQ. StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. Qualitative study.https://www.ncbi.nlm.nih.gov/books/NBK470395/ Available. [PubMed] [Google Scholar]
- 27.Creswell JW, Clark VLP. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: Sage Publications; 2017. [Google Scholar]
- 28.Arias Valencia MM. Principles, Scope, and Limitations of the Methodological Triangulation. Invest Educ Enferm. 2022;40:e03. doi: 10.17533/udea.iee.v40n2e03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tashakkori A, Johnson RB, Teddlie C. Foundations of mixed methods research: Integrating quantitative and qualitative approaches in the social and behavioral sciences. Sage publications; 2020. [Google Scholar]
- 30.Walton K, Wang TW, Prutzman Y, et al. Characteristics and Correlates of Recent Successful Cessation Among Adult Cigarette Smokers, United States, 2018. Prev Chronic Dis. 2018;17:E154. doi: 10.5888/pcd17.200173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Polit DF, Beck CT. The content validity index: are you sure you know what’s being reported? Critique and recommendations. Res Nurs Health. 2006;29:489–97. doi: 10.1002/nur.20147. [DOI] [PubMed] [Google Scholar]
- 32.Lawshe CH. A quantitative approach to content validity. Pers Psychol. 1975;28:563–75. doi: 10.1111/j.1744-6570.1975.tb01393.x. [DOI] [Google Scholar]
- 33.Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med. 2016;15:155–63. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–12. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 35.Lincoln YS, Guba EG. Naturalistic Inquiry. SAGE; 1985. [Google Scholar]
- 36.Guba EG, Lincoln YS. Competing paradigms in qualitative research. Handbook of qualitative research. 1994;2 [Google Scholar]
- 37.Tobaiqy M, Thomas D, MacLure A, et al. Staff and student experiences and attitudes towards smoking and smoking cessation, University of Jeddah, Saudi Arabia. Tob Prev Cessat. 2021;7:73.:73. doi: 10.18332/tpc/144178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Morphett K, Partridge B, Gartner C, et al. Why Don’t Smokers Want Help to Quit? A Qualitative Study of Smokers’ Attitudes towards Assisted vs. Unassisted Quitting. Int J Environ Res Public Health. 2015;12:6591–607. doi: 10.3390/ijerph120606591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sin MK, Ro K. Factors Influencing Smoking Decisions Among Older Korean American Men: A Qualitative Study. J Addict Nurs. 2023;34:E39–44. doi: 10.1097/JAN.0000000000000429. [DOI] [PubMed] [Google Scholar]
- 40.Ferreira-Brito F, Alves S, Guerreiro T, et al. Digital health and patient adherence: A qualitative study in older adults. D Health. 2024;10:20552076231223805. doi: 10.1177/20552076231223805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ünübol H, Hızlı Sayar G. Psychological factors associated with smoking and quitting: addiction map of Turkey study. Neuropsychiatr Dis Treat. 2019;15:1971–82. doi: 10.2147/NDT.S204167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Luo Z, Xu W, Jiang S, et al. The mediating role of negative emotions in the relationship between smoking and health-related quality of life among Chinese individuals: A cross-sectional study. Tob Induc Dis. 2023;21:135. doi: 10.18332/tid/171355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chinwong S, Chinwong D. A National Survey of Community Pharmacists on Smoking Cessation Services in Thailand. Pharmacy (Basel) 2018;6:101. doi: 10.3390/pharmacy6030101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mohd Noordin Z, Neoh CF, Ibrahim Ghazali NH, et al. “A person who do not smoke will not understand a person who smokes and trying to quit…” Insights From Quit Smoking Clinics’ Defaulters: A Qualitative Study. J Patient Exp. 2023;10:23743735231184690. doi: 10.1177/23743735231184690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Taylor GM, Lindson N, Farley A, et al. Smoking cessation for improving mental health. Cochrane Database Syst Rev. 2021;3:CD013522. doi: 10.1002/14651858.CD013522.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paharia MI. Comprehensive handbook of clinical health psychology. 2008. Tobacco cessation; p. 105. [Google Scholar]
- 47.Rosenthal L, Carroll-Scott A, Earnshaw VA, et al. Targeting cessation: understanding barriers and motivations to quitting among urban adult daily tobacco smokers. Addict Behav. 2013;38:1639–42. doi: 10.1016/j.addbeh.2012.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Keizer I, Gex-Fabry M, Croquette P, et al. Tobacco craving and withdrawal symptoms in psychiatric patients during a motivational enhancement intervention based on a 26-hour smoking abstinence period. Tob Prev Cessat. 2019;5:22. doi: 10.18332/tpc/109785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Devi S, Goyal S, Rathor B, et al. Updated review on successful control with nicotine replacement therapy for nicotine withdrawal symptoms. Int J Sci Res Arch. 2023;9:142–55. doi: 10.30574/ijsra.2023.9.1.0352. [DOI] [Google Scholar]
- 50.Despoina H, Maria M, Anna K, et al. Smoking cessation process and quality of life. JNEP. 2017;7:1. doi: 10.5430/jnep.v7n9p1. [DOI] [Google Scholar]
- 51.Domingo JSF, Reyes KDT, Villegas CKM, et al. Quitting is such a sweet sorrow: a grounded theory study of unassisted smoking cessation among Filipino adult smokers. J Public Health Emerg. 2022;6 doi: 10.21037/jphe-21-110. [DOI] [Google Scholar]
- 52.Schultz ME, Fronk GE, Jaume N, et al. Stressor-elicited smoking and craving during a smoking cessation attempt. J Psychopathol Clin Sci. 2022;131:73–85. doi: 10.1037/abn0000702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Buczkowski K, Dachtera-Frąckiewicz M, Luszkiewicz D, et al. Reasons for and Scenarios Associated with Failure to Cease Smoking: Results from a Qualitative Study Among Polish Smokers Who Had Unsuccessfully Attempted to Quit. Pat Prefer Adherence. 2021;15:2071–84. doi: 10.2147/PPA.S320798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Buczkowski K, Marcinowicz L, Czachowski S, et al. Motivations toward smoking cessation, reasons for relapse, and modes of quitting: results from a qualitative study among former and current smokers. Patient Prefer Adherence. 2014;8:1353–63. doi: 10.2147/PPA.S67767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tsoh JY, Humfleet GL, Muñoz RF, et al. Development of Major Depression After Treatment for Smoking Cessation. AJP. 2000;157:368–74. doi: 10.1176/appi.ajp.157.3.368. [DOI] [PubMed] [Google Scholar]
- 56.Marzo RR, El-Fass KA, Osman NA, et al. Identifying the barriers of smoking cessation and predictors of nicotine dependence among adult Malaysian smokers: A cross-sectional study. Tob Induc Dis. 2022;20:109. doi: 10.18332/tid/154964. [DOI] [PMC free article] [PubMed] [Google Scholar]