Abstract
The chlamydiae are obligate intracellular bacteria that occupy a nonacidified vacuole (the inclusion) during their entire developmental cycle. These bacteria produce a set of proteins (Inc proteins) that localize to the surface of the inclusion within infected cells. Chlamydia trachomatis IncA is also commonly found in long fibers that extend away from the inclusion. We used standard and confocal immunofluorescence microscopy to demonstrate that these fibers extend to newly developed inclusions, termed secondary inclusions, within infected cells. Secondary inclusions observed at early time points postinfection were devoid of chlamydial reticulate bodies. Later in the developmental cycle, secondary inclusions containing variable numbers of reticulate bodies were common. Reticulate bodies were also observed within the IncA-laden fibers connecting primary and secondary inclusions. Quantitative differences in secondary inclusion formation were found among clinical isolates, and these differences were associated with serovar. Isolates of serovar G consistently produced secondary inclusions at the highest frequency (P < 0.0001). Similar quantitative studies demonstrated that secondary inclusion formation was associated with segregation of inclusions to daughter cells following cytokinesis. We conclude that the production of secondary inclusions via IncA-laden fibers allows chlamydiae to generate an expanded intracellular niche in which they can grow and may provide a means for continuous infection within progeny cells following cell division.
The chlamydiae are obligate intracellular bacteria that develop within a nonacidified vacuole, the inclusion, which provides them with a unique intracellular environment. The inclusion membrane is not passively permeable to low molecular weight compounds (13), yet intravacuolar ion concentrations are very similar to those found in the cytoplasm (11). The events leading to inclusion biogenesis are unclear, but the process is likely controlled by proteins produced by chlamydiae and delivered to the inclusion membrane and/or the host cell cytosol (29). All chlamydiae produce a set of proteins, termed Inc proteins, which are localized to the inclusion membrane (20) and are likely important in inclusion development. The IncA proteins of Chlamydia trachomatis, Chlamydophila caviae, and Chlamydophila pneumoniae have also been localized to discrete filamentous structures (IncA-laden fibers) that extend away from the inclusion membrane into the cytosol of host cells (3). Under conditions of stress, these fibers can accumulate antigens normally localized to the outer membrane of intracellular developmental forms (5). We undertook the studies reported here to elucidate the development and function of these unique IncA-laden fibers. Utilizing both standard and confocal immunofluorescence microscopy, we present evidence demonstrating that these fibers participate in the generation of secondary inclusions within cells. Additionally, we report that isolates of different C. trachomatis serovars produce widely varying amounts of both fibers and secondary inclusions within cells. We propose that these structures are important in the generation of new chlamydial inclusions within infected host cells, which may facilitate continuous infection of progeny cells following host cell mitosis and cytokinesis.
MATERIALS AND METHODS
Chlamydiae and chlamydial propagation.
Fifteen prototype strains (A/G-17/OT, B/TW-5/OT, C/TW-3/OT, D/UW-3/Cx, E/UW-5/Cx, F/UW-6/Cx, G/UW-57/Cx, H/UW-4/Cx, I/UW-12/Ur, Ia/UW-202/NP, J/UW-36/Cx, K/UW-31/Cx, L1/440/Bu, L2/434/Bu, and L3/404/Bu) and 75 archived cervical and urethral clinical isolates of C. trachomatis (27, 28) were examined in these studies. All prototype strains were microbiologically cloned by limiting dilution, and cloned chlamydiae were partially purified by centrifugation of lysates of infected cells through a 30% Renografin pad (6). Specimen collection, culture isolation techniques, and serotyping were conducted and purified as previously described (27). Infected HeLa or McCoy cells were incubated in minimal essential medium with 10% fetal bovine serum (Sigma-Aldrich) with or without cycloheximide (1 μg/ml) at 37°C in 5% CO2.
Antibodies and reagents for microscopy.
Monoclonal antibodies (MAbs) 3H7, directed at C. trachomatis IncA (21); 20F12, specific for the C. trachomatis Inc protein CT223p (2); LV-22, specific for C. trachomatis major outer membrane protein (MOMP) (28); and E6-H1, specific for chlamydial lipopolysaccharide (LPS) and rabbit anti-IncG sera (23) were utilized in immunofluorescent microscopy. All secondary antibodies were purchased from Southern Biotechnology Associates, Inc. The DNA-specific fluorescent label 4′,6-diamidino-2-phenylindole dihydrochloride (DAPI, 2 μg/ml in mounting medium; Vectashield, Vector Laboratories) was used to label host cell and bacterial DNA.
Immunofluorescence and green fluorescent protein (GFP) transfections.
The temporal analysis of fiber development and secondary inclusion formation were examined by growing chlamydiae at the indicated multiplicity of infection (MOI) within low-confluence monolayers of McCoy cells on 12-mm-diameter coverslips in glass shell vials as previously described (26). Cells were fixed with methanol at the indicated times postinfection and labeled with antibodies as indicated in Results and the figure legends.
In most experiments, conventional immunofluorescence microscopy was used for these studies. The one exception was the examination of reticulate bodies (RBs) within fibers linking primary and secondary inclusions, which was conducted using confocal immunofluorescence microscopy. Serial Z-sections of secondary inclusions were visualized and collected from monolayers of HeLa cells infected with G/UW-57 with a Leica TCS 4D confocal microscope.
For determination of GFP localization within C. trachomatis-infected cells, monolayers were transfected with a pcDNA4HisMaxC (Invitrogen) construct encoding GFP (pCDNA-GFP) and incubated for 24 h. The transfected monolayer was then infected with C. trachomatis G/UW-57 (MOI = 0.5). The transfected/infected monolayers were incubated 30 additional hours prior to being washed with phosphate-buffered saline and methanol fixation.
Inclusions were labeled using MAb 3H7 to detect IncA. A Texas red-conjugated anti-mouse immunoglobulin G (IgG) was used as secondary antibody. This labeling allowed the inclusions to be labeled red against a background of cytosolic GFP within transfected/infected cells. Monolayers were examined as described in the section above.
Quantification of inclusion structure as a function of time.
McCoy cells were infected with G/UW-57 at various MOIs (0.5, 0.05, and 0.005). These cells were incubated for different time intervals prior to fixation and labeled for fluorescent microscopy. C. trachomatis IncA was labeled with rabbit anti-IncA antiserum pooled with mouse monoclonal anti-IncA (IgG1). Chlamydial developmental forms were labeled with mouse anti-LPS (IgG2a). Secondary antibodies for these experiments were Texas red-conjugated anti-rabbit IgG, Texas red-conjugated anti-mouse IgG1, and fluorescein conjugated anti-mouse IgG2a. The presence of inclusions not associated with fibers or secondary inclusions, inclusions attached to one or more IncA-laden fibers, secondary inclusions devoid of chlamydia, and secondary inclusions carrying chlamydial developmental forms were each enumerated via fluorescent microscopic analysis. The data represent averages of three independent sets of coverslips at each time point, encompassing a total of >1,000 infected cells for each experiment.
Quantification of secondary inclusion formation as a function of serovar.
To examine strain variability in secondary inclusion formation, prototype strains and clinical isolates were grown in the same manner as above, using an MOI of 0.3. Cells on coverslips were cultured for 28 h postinfection (hpi) prior to fixation and labeled with anti-IncA and anti-LPS. The percentage of cells with secondary inclusions was determined by averaging triplicate counts of cells with secondary inclusions versus infected cells that lacked secondary inclusions.
The effect of cell division on secondary inclusion formation was examined by comparing C. trachomatis grown in the presence or absence of the eukaryotic protein synthesis inhibitor cycloheximide added to tissue culture medium at 1 μg/ml. This is a commonly used technique to inhibit cellular propagation in tissue culture cells (15). In control experiments, this treatment was effective in reducing cell numbers relative to untreated cells (data not shown). Selected strains were cultured in 20% confluent monolayers of HeLa cells on coverslips. Three clinical strains representing each of the serovars J (low secondary inclusion producer) and G (high secondary inclusion producer) were examined. Infected cells (MOI, ∼0.3) were incubated for an extended time period following infection (48 hpi) to allow for increased division of host cells. Monolayers were then fixed with methanol and labeled with MAb E6-H1. Three independent experiments were analyzed for each isolate.
Statistical analysis.
To test for differences between serovars in secondary inclusion formation, strains of each serovar were grown in McCoy cells treated with cycloheximide, and secondary inclusions were enumerated and compared by the Kruskal-Wallis test. Differences in the abundance of secondary inclusions between serovar G and all other (non-G) serovars were tested by the Wilcoxon rank-sum test. Results of cell division experiments were analyzed by plotting the means and their 95% confidence intervals for the number of infected cells by serovar and cycloheximide treatment (22). A two-way analysis of variance model with an interaction term was constructed to analyze the effects of serovar and cycloheximide treatment on the number of infected cells.
RESULTS
Identification of secondary inclusions within Chlamydia-infected cells.
During the microscopic analysis of clinical C. trachomatis isolates in cell culture, selected strains were identified that uniquely formed unusual, multiple inclusions at low MOIs. Analysis of these inclusions with antibodies to MOMP and IncA demonstrated a variety of inclusion structures. Figure 1 shows the types of inclusions present within McCoy cells infected with C. trachomatis G/UW-57 (MOI = 0.3) and fixed for microscopy at 28 hpi. Monovacuolar inclusions consistent with most published descriptions of C. trachomatis-infected mammalian cells were very common (Fig. 1A and B). However, many host cells contained inclusions connected to one or more IncA-laden fibers that extend from the inclusion into the cytosol of the infected cell (Fig. 1A). In many cases, these IncA-laden fibers connected the primary inclusion to IncA-laden vacuoles (secondary inclusions) that either lacked (Fig. 1B) or contained (Fig. 1C and D) chlamydial developmental forms. Secondary inclusions containing developmental forms ranged from those that had very few chlamydiae (Fig. 1C) to those that contained many chlamydiae and were virtually indistinguishable from the primary inclusion (Fig. 1D). While it is common to find vacuoles of nonchlamydial origin within host cells both infected and not infected with chlamydiae, only secondary inclusions had IncA in the vacuolar membrane and were connected to a primary inclusion by an IncA-laden fiber.
FIG. 1.
Fiber and secondary inclusion formation in cells infected by Chlamydia trachomatis. The four panels show the different forms of inclusions found within McCoy cells infected with C. trachomatis G/UW-57. Cells were infected at an MOI of 0.3 and fixed with methanol 28 hpi. All cells were labeled with anti-IncA (green) and anti-MOMP (red), and DNA is labeled with DAPI (blue). (A) Two infected cells, one containing an inclusion lacking a fiber and one containing an inclusion with a single IncA-laden fiber. (B) A cell with an IncA-laden vacuole at the end of a fiber. (C) A cell with a maturing primary inclusion, a secondary inclusion containing a limited number of developmental forms, and a connecting fiber. (D) An infected cell with two large inclusions, both filled with developmental forms and connected by an IncA-laden fiber. Scale bar, 10 μm.
Variation in secondary inclusion development as a function of chlamydial serovar.
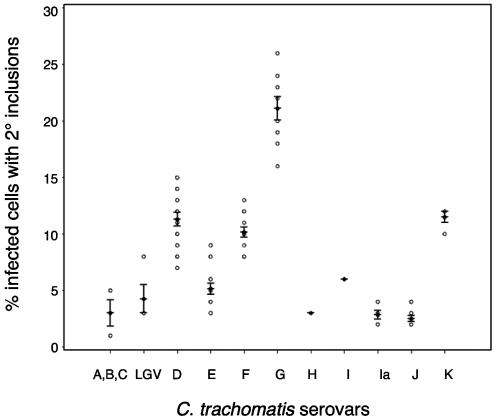
Seventy-five clinical isolates of differing serovars were examined to assess whether the rate of secondary inclusion formation varied with serovar. The MOI for these experiments was approximately 0.3, and infected cells were cultured in the presence of cycloheximide for 28 hpi. The overall statistical comparison of all serovars showed highly significant differences in distribution of secondary inclusions by serovar (P < 0.0001). In particular, isolates within serovar G produced secondary inclusions at a much higher frequency than the other serovars (P < 0.0001), followed by isolates within serovars D, K, F, I, H, E, B, Ia, and J in order of decreasing frequency (Fig. 2).
FIG. 2.
Quantitation of secondary inclusion formation by serovar. McCoy cells were infected with clinical isolates of each chlamydial serovar (MOI = ∼0.3) and fixed 28 hpi. The percentage of infected cells with secondary inclusions is plotted as a function of chlamydial serovar. The median for each serovar is represented by a black circle, while the individual strain data points are shown in open circles. The means and 95% confidence intervals are indicated for each serovar.
Quantification of secondary inclusions at different intervals postinfection and at different multiplicities of infection.
We next enumerated the formation of inclusions in McCoy cells by C. trachomatis G/UW-57 as a function of time and as a function of multiplicity of infection. The first time interval examined was 14 hpi, since IncA was not consistently detected at earlier time points. Initial experiments were conducted at MOI 0.5 (Fig. 3A), and subsequent experiments were conducted at decreasing MOIs of 0.05 and 0.005 (Fig. 3B). These analyses demonstrated that inclusions lacking fibers and inclusions with single fibers were predominant at 14 hpi, but some secondary inclusion formation was observed. All secondary inclusions observed at this time point were devoid of chlamydiae. At 20 hpi, the number of secondary inclusions increased dramatically. In the experiment conducted at an MOI of 0.5, 23% of infected cells had secondary inclusions that lacked developmental forms, and 8% of the infected cells now had secondary inclusions containing chlamydial developmental forms. There were no differences in the levels of different inclusion morphologies between 20 and 28 hpi. At these time points, the number of inclusions not connected to a fiber was lower than was observed at 14 hpi, while the number of secondary inclusions was greatly increased. These data support a model in which fibers are formed early in development, secondary inclusions associated with these fibers are subsequently formed, and C. trachomatis developmental forms then occupy the newly formed secondary inclusions.
FIG. 3.
Quantitation of secondary inclusions in cells fixed after different time intervals postinfection and at different multiplicities of infection. (A) Chlamydia trachomatis G/UW-57 EBs were inoculated onto McCoy cells at an MOI of 0.5 and allowed to grow for various time intervals prior to fixation and examination for inclusion structure. The horizontal axis represents the hours after infection that cells were fixed with methanol. The vertical axis shows the fraction of total infected cells carrying each inclusion type. The data compare the fraction of infected cells having no IncA-laden fiber (open bars), those that have one or more fibers but no secondary inclusion (dotted bars), those that have an secondary inclusion devoid of chlamydiae (gray bars), and those that have a secondary inclusion containing developmental forms (black bars). Each time point represents analysis from three independent experiments, and the error bars indicate standard deviation. A total of over 1,200 infected cells were evaluated for these data. (B) Examination of secondary inclusion formation at low MOI. Cells were infected with G/UW-57 at the indicated MOI, fixed with methanol 28 hpi, and examined by fluorescence microscopy. All labeling is consistent with that used in panel A. Note that the percentage of filled secondary inclusions does not vary with the reduction in MOI. A total of over 1,000 infected cells were examined for these calculations.
The observed phenotype could also be explained by independent infections by different elementary bodies (EBs), leading initially to the development of multiple inclusions within host cells. To examine this possibility, a second set of experiments were conducted that examined the level of secondary inclusion formation as a function of MOI. If the formation of filled secondary inclusions resulted from a second independent infection of a cell, then the number of filled secondary inclusions should be greatly reduced by a 10-fold reduction in MOI. As can be seen in Fig. 3B, the numbers of filled secondary inclusions was approximately equal in experiments conducted at MOIs of 0.05 and 0.005, suggesting that secondary inclusion formation was independent of MOI. The percentage of filled secondary inclusions was also similar in this experiment to the data presented in Fig. 3A, which represents an infection conducted at an MOI of 0.5. These data support the hypothesis that the formation of secondary inclusions was not a result of two independent infections of a single infected cell.
We also examined whether or not host cells infected with strains producing low numbers of fibers and secondary inclusions might simply produce these structures later during development. To test this possibility, we determined the number of secondary inclusions in McCoy cells infected with C. trachomatis J/UW-36 (a very low secondary inclusion former) that were fixed for microscopy at 24, 36, and 72 hpi. Consistent with the data in Fig. 2, the number of fibers and secondary inclusions was very low at each time point in cells infected with J/UW-36, suggesting that the length of incubation does not affect the phenotypes associated with the individual strains (not shown).
Distribution of additional Inc proteins in the formation of secondary inclusions.
As C. trachomatis produces several different Inc proteins (2), we next asked whether or not secondary inclusions and associated fibers contained Inc proteins other than IncA, specifically, Inc proteins CT223p and IncG. Figure 4 shows the differential abundance of three Inc proteins in developing secondary inclusions in G/UW-57-infected McCoy cells fixed with methanol at 28 hpi (MOI = 0.5). Figure 4A is a composite of Fig. 4B (IncA), C (CT223p), and D (IncG). Two of the infected cells in this image have well-defined IncA-laden fibers and secondary inclusions lacking chlamydiae. Note that neither CT223p nor IncG was found within these structures. The inclusion membrane of secondary inclusions subsequently accumulated IncG and CT223p after being occupied by chlamydial developmental forms (not shown). These data indicate that the distribution of Inc proteins within the IncA-laden fibers and secondary inclusions is selective and that these structures do not accumulate all Inc proteins until occupied by developmental forms.
FIG. 4.
Chlamydial fibers and secondary inclusions that lack developmental forms do not accumulate all Inc proteins. McCoy cells were infected with C. trachomatis G/UW-57 (serovar G) at an MOI of 0.5 and fixed for microscopy 28 hpi. Cells were then labeled with anti-IncA (green) (B), anti CT223p (red) (C), and anti-IncG (blue) (D). Panel A is a composite of the images in panels B, C, and D. Three cells in these images have well-defined IncA-laden fibers and secondary inclusions lacking developmental forms. These structures are indicated in panel A by an arrowhead and an arrow, respectively, for one cell. Note that neither CT223p nor IncG is found within the IncA-laden fibers or the empty secondary inclusions.
GFP and the vacuolar nature of early secondary inclusions.
The possibility existed that the apparent IncA-laden secondary vacuoles are not actual vacuoles but instead are loops of IncA-laden fibers in a lariat- or lasso-like structure. Heinzen and Hackstadt (13) showed that C. trachomatis inclusions exclude GFP that is present in the cytoplasm, and we used their approach to examine this question with infected McCoy cells. These experiments demonstrated that, similarly to that observed for filled inclusions, the IncA-laden structures that lack developmental forms also exclude GFP (Fig. 5).
FIG. 5.
IncA-laden secondary inclusions exclude the green fluorescence protein. Chlamydia trachomatis G/UW-57 was used to infect McCoy cells (MOI = 0.5) previously transfected with pCDNA-GFP. The cells were fixed for conventional immunofluorescence microscopy 30 hpi. (A) An infected cell that is producing GFP (green) and is labeled with anti-IncA (red) and DAPI (DNA; blue). A primary and two secondary inclusions can be seen in this cell. (B) GFP labeling of the same cell. Note that the primary inclusion, the filled secondary inclusion (thin arrows), and the secondary inclusion lacking chlamydiae (fat arrow) all exclude GFP. Scale bar in panel B, 10 μm.
Chlamydial developmental forms within fibers linking primary and secondary inclusions.
We hypothesized that the initial population of the secondary inclusion resulted from the transfer of developmental forms from primary inclusions to secondary inclusions. If this were the case, host cells which have chlamydiae moving between vacuoles would be identifiable in fixed monolayers. Confocal microscopy was used to determine whether chlamydial developmental forms (strain G/UW-57) were found within fibers connecting a primary and secondary inclusion. While these forms were not common, we did regularly find host cells with chlamydiae in IncA-laden fibers. The images in Fig. 6A and B show a cell that contains several developmental forms within a fiber connected to a secondary inclusion devoid of chlamydia. Figure 6C to E show three serial images of a confocal Z-section through an infected cell. A primary inclusion and secondary inclusion are connected via at least three IncA fibers. A MOMP-positive chlamydial development form is shown within one of the fibers. These data suggest that C. trachomatis can be transferred between inclusions via the IncA-laden fibers.
FIG. 6.
Chlamydial developmental forms within fibers linking primary and secondary inclusions. C. trachomatis G/UW-57-infected HeLa cells (MOI, 0.1) were fixed 28 hpi and labeled with anti-IncA (green) and anti-MOMP (red). Confocal microscopy was then used to identify and document the presence of chlamydial developmental forms within IncA-laden fibers. (A and B) Two infected cells are shown, one containing an inclusion lacking a fiber and one containing primary and secondary inclusions connected by a fiber. (A) The MOMP labeling identifies RBs that are found within the primary inclusion and within a fiber pointing to the right. (B) IncA and MOMP labeling within the same cells, demonstrating that the RBs outside the primary inclusion are present within an IncA-laden fiber. (C to E) A serial confocal Z-section showing an inclusion and associated fibers. (D) The secondary inclusion (arrow) is connected to the primary inclusion with at least two IncA-laden fibers (asterisk), and an RB (arrowhead) is found within one fiber. Scale bar, 10 μm. The assembled serial Z-sections represented in panels C to E can be found at http://oregonstate.edu/∼rockeyd/moviepage.htm.
The complete confocal Z-section assembly containing the images in Fig. 6C to E can be viewed by linking to http://oregonstate.edu/∼rockeyd/moviepage.htm.
Segregation of secondary inclusions in dividing host cells.
Fluorescence microscopy was used to examine the effect of cell division on inclusion distribution within host cells infected with a strain that readily forms secondary inclusions. For these studies, G/UW-57 (MOI = 0.5) was cultured in HeLa cells grown in the absence of cycloheximide and fixed for microscopy 28 hpi. The images in Fig. 7 represent infection patterns commonly observed in these analyses. In panel A, two secondary inclusions devoid of developmental forms, and several primary inclusions are shown. Each of the inclusions is adjacent to nuclei of distinct cells, and IncA-laden fibers connecting the primary and secondary inclusions are present within each cell. Figure 7B shows three inclusions within adjacent cells, each connected by an IncA-laden fiber to secondary inclusions within the same cell. The two secondary inclusions (labeled 1 and 2) have low numbers of RBs, while the primary inclusion (labeled 3) is heavily laden with EBs and RBs. The two secondary inclusions bracket a nucleus in the cell, with the IncA-laden fiber across the nucleus. Figure 7C is an enlarged section of Fig. 7B, showing more clearly the continuous IncA-laden fiber still joining two cells undergoing the final stages of cytokinesis. These images suggest that Chlamydia-infected cells, following cell division, can segregate secondary inclusions to daughter cells.
FIG. 7.
Formation of secondary inclusions by C. trachomatis G/UW-57 in dividing HeLa cells. (A) Two secondary inclusions devoid of developmental forms (arrows) separated from the primary inclusions but still exhibiting remnants of the connecting IncA fibers. Anti-IncA is shown as green, anti-MOMP is shown as red, and DNA is labeled with DAPI (blue). (B) Three inclusions are shown connected by an IncA-laden fiber (arrows). The two secondary inclusions (labeled 1 and 2) have low numbers of RBs, while the primary inclusion (labeled 3) is heavily laden with EBs and RBs. The two secondary inclusions are bracketing a nucleus in a daughter cell, with the IncA-laden fiber across the nucleus. (C) A magnified image of the fiber shown in panel B. All cells were infected at an MOI of 0.5 and fixed for microscopy 28 hpi. Scale bars in A and C, 10 μm.
If formation of secondary inclusions leads to infection of both daughter cells following division, then populations of host cells infected with strains that frequently form secondary inclusions and are allowed to undergo cell division should produce a corresponding increase in the number of infected cells in the monolayer. To test this, we examined the effect of cycloheximide treatment on the number of infected cells in a population. These studies were conducted with three strains of serovar G (frequent secondary inclusion formers) and three strains of J (very infrequent secondary inclusion formers) (Fig. 2). Qualitative examination of monolayers treated and not treated with cycloheximide suggested that infection by isolates of serovar G led to a higher number of infected cells in monolayers that were allowed to divide, but the number of serovar J-infected cells was not altered significantly in treated versus untreated cells (Fig. 8). We examined this quantitatively by counting the number of infected cells in monolayers treated or not treated with cycloheximide. The data were analyzed using a two-way analysis of variance model with an interaction term to determine the effects of serovar and cycloheximide on the percentage of infected cells. Treatment with cycloheximide led to a reduction of 23.4% (95% confidence interval, 18.7 to 28.0%) in the number of serovar G-infected cells, while this treatment led to a 3% reduction (95% confidence interval, −1.6 to 7.7%) in the number of serovar J-infected cells. The difference between means of serovar G-infected cells (cycloheximide treated versus not treated) was statistically significant (P < 0.001), while there was no statistical effect of cycloheximide on serovar J (P = 0.9473). Thus, blocking cell division had a significant effect on the number of cells infected with the serovar G isolates, but not on cells infected with the serovar J isolates. These data are consistent with a model where secondary inclusion formation leads to segregation of inclusions among daughter cells following host cell division.
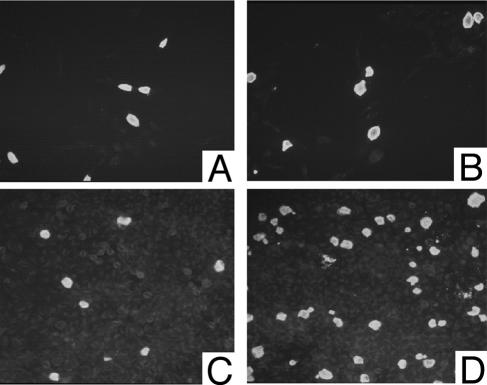
FIG. 8.
C. trachomatis serovars J and G infecting HeLa cells treated and untreated with cycloheximide. Low-magnification images of HeLa cells infected with C. trachomatis J/UW-36 (A and C) and serovar G/UW-57 (B and D). In each case, the cells were infected at a MOI of approximately 0.3 and fixed for microscopy 48 hpi. Cells shown in panels A and B were cultured in the presence of cycloheximide, while the cells shown in panel C and D were cultured in medium lacking cycloheximide. Each panel is labeled with antichlamydial LPS. Note that the absence of cycloheximide leads to a higher number of chlamydial inclusions in the cells infected with G/UW-57 but not in the cells infected with J/UW-36.
DISCUSSION
We have previously demonstrated that each chlamydial species tested produces IncA-laden fibers that extend away from the inclusion into the cytoplasm of the host cell (5, 18, 20). In some cases, these fibers were shown to contain outer membrane antigens from developmental forms. However, the function and molecular architecture of these fibers remained unclear. In the present report, we show data supporting a hypothesis that chlamydiae use these fibers to create a second intracellular environment and to transport chlamydiae to that environment. In this model, the IncA-laden fibers and secondary inclusions function to increase the inhabitable environment within individual infected cells.
The data support a model proposing the temporal development of fibers and secondary inclusions. Under this model, IncA-laden fibers extend from the developing inclusion membrane and grow into the cytosol of the host cell. The termini of the fibers then expand to form secondary inclusions lacking chlamydial developmental forms. Later in development, these secondary inclusions become laden with chlamydiae. These data are supported with quantitative analysis of fluorescent microscopic images of infected cells over the course of a single developmental cycle. We also propose that chlamydial developmental forms produced in the primary inclusion proceed down these fibers and occupy the secondary inclusion. RB division then proceeds in the secondary inclusion, eventually resulting in a fully occupied chlamydial inclusion. This view thus ascribes a much more dynamic role to the chlamydial inclusion membrane than has previously been held. Namely, it is not merely a barrier or interface between chlamydiae and the host cell cytoplasm, but also an active participant in developing an expanding environment for the developing RB.
A second possible function of the fibers and resulting secondary inclusions involves the infection of progeny cells following host cell division. We demonstrate that secondary inclusions, connected by IncA-laden fibers, are segregated to daughter cells during cell division. The biological significance of these results is somewhat unclear, because of the common premise that cells within the endocervical epithelium, the primary target of chlamydial infection, do not commonly divide. However, epithelial cells of the upper genital tract are replaced during menstrual cycling, and damage to mucosal surfaces through infection also leads to proliferation of epithelial cells, likely at all sites (14). In vitro studies have also demonstrated that mucosal cells in these environments are division competent and can be infected with chlamydiae (16). The ability to infect both daughter cells following cell division may help chlamydiae stay entrenched within the host mucosal cell environment in the face of routine sloughing of epithelia and during replacement of epithelial cells following pathogen-induced tissue damage. This, in combination with chlamydial antiapoptotic properties (7), and the possible inhibitory effect of cytokinesis by chlamydiae (10) may facilitate survival despite host processes that are designed for pathogen elimination.
IncA-laden fibers and secondary inclusions selectively accumulate specific Inc proteins prior to accumulation of developmental forms. In our experiments, CT223p and IncG were not abundant in the fibers or secondary inclusion until the secondary inclusion was occupied by chlamydiae. These differences are not a function of the temporal expression of the genes encoding each protein, as two laboratories have shown that transcripts for CT223p and IncG are produced prior to the transcription of incA (4, 17). Instead, it is likely that different Inc proteins have differing functions in the dynamic process of fiber and secondary inclusion formation. It is also possible that differences in protein half-life or Inc protein tethering and localization within the inclusion membrane (19) may affect the abundance of individual Inc proteins within the fibers and early secondary inclusions.
We (26) and others (12) have provided evidence showing that C. trachomatis IncA has a role in the fusion of inclusions during infection of cells by multiple EBs. Therefore, it is curious that IncA might also be uniquely associated with a process leading to an increase in the number of inclusions within the same cell. While our studies demonstrate clearly that IncA is associated with development of fibers and secondary inclusions, we do not provide data suggesting that IncA is necessary or sufficient for their generation. The chlamydiae encode at least 10 proteins localized to the inclusion membrane (3, 4, 8, 23, 24) and many proteins that may be localized to that environment (2). As yet, many of these have no known function. We hypothesize that one or more of these proteins, perhaps including IncA, have a significant role in secondary inclusion formation.
We also demonstrate that certain serovars, particularly serovar G, are associated with a much higher rate of IncA-fiber accumulation and secondary inclusion formation within infected cells. Interestingly, serovar G isolates have also been linked to specific tissue tropisms (a markedly increased prevalence in rectal infections, for example) and, perhaps, to cervical cancer (1, 9, 25). Whether these unique properties of serovar G infections are related to fiber or secondary inclusion formation is not known. However, further studies utilizing genomics, cell biology, and clinical epidemiology will be useful in exploring possible links between the propensity to form secondary inclusions and unique biological behavior such as tissue tropism and neoplasia.
Acknowledgments
We acknowledge members of the Chlamydia Laboratory (U.W.) and Melissa Andreas (O.S.U.) for excellent technical support. Antibodies against chlamydial LPS and C. trachomatis IncG were kindly provided by H. D. Caldwell and M. Scidmore, respectively. We thank Wendy Brown for her valuable expertise with the confocal microscope and Pacita Roberts for her statistical analysis of data.
This work was supported by U.S. Public Health Service awards AI42869, AI31448, and AI48769.
Editor: D. L. Burns
REFERENCES
- 1.Anttila, T., P. Saikku, P. Koskela, A. Bloigu, J. Dillner, I. Ikaheimo, E. Jellum, M. Lehtinen, P. Lenner, T. Hakulinen, A. Narvanen, E. Pukkala, S. Thoresen, L. Youngman, and J. Paavonen. 2001. Serotypes of Chlamydia trachomatis and risk for development of cervical squamous cell carcinoma. JAMA 285:47-51. [DOI] [PubMed] [Google Scholar]
- 2.Bannantine, J. P., R. S. Griffiths, W. Viratyosin, W. J. Brown, and D. D. Rockey. 2000. A secondary structure motif predictive of protein localization to the chlamydial inclusion membrane. Cell. Microbiol. 2:35-47. [DOI] [PubMed] [Google Scholar]
- 3.Bannantine, J. P., W. E. Stamm, R. J. Suchland, and D. D. Rockey. 1998. Chlamydia trachomatis IncA is localized to the inclusion membrane and is recognized by antisera from infected humans and primates. Infect. Immun. 66:6017-6021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Belland, R. J., G. Zhong, D. D. Crane, D. Hogan, D. Sturdevant, J. Sharma, W. L. Beatty, and H. D. Caldwell. 2003. Genomic transcriptional profiling of the developmental cycle of Chlamydia trachomatis. Proc. Natl. Acad. Sci. USA 100:8478-8483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown, W. J., Y. A. Skeiky, P. Probst, and D. D. Rockey. 2002. Chlamydial antigens colocalize within IncA-laden fibers extending from the inclusion membrane into the host cytosol. Infect. Immun. 70:5860-5864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caldwell, H. D., J. Kromhout, and J. Schachter. 1981. Purification and partial characterization of the major outer membrane protein of Chlamydia trachomatis. Infect. Immun. 31:1161-1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fan, T., H. Lu, H. Hu, L. Shi, G. A. McClarty, D. M. Nance, A. H. Greenberg, and G. Zhong. 1998. Inhibition of apoptosis in chlamydia-infected cells: blockade of mitochondrial cytochrome c release and caspase activation. J. Exp. Med. 187:487-496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fling, S. P., R. A. Sutherland, L. N. Steele, B. Hess, S. E. D'Orazio, J. Maisonneuve, M. F. Lampe, P. Probst, and M. N. Starnbach. 2001. CD8+ T cells recognize an inclusion membrane-associated protein from the vacuolar pathogen Chlamydia trachomatis. Proc. Natl. Acad. Sci. USA 98:1160-1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Geisler, W. M., W. L. Whittington, R. J. Suchland, and W. E. Stamm. 2002. Epidemiology of anorectal chlamydial and gonococcal infections among men having sex with men in Seattle: utilizing serovar and auxotype strain typing. Sex Transm. Dis. 29:189-195. [DOI] [PubMed] [Google Scholar]
- 10.Greene, W., and G. Zhong. 2003. Inhibition of host cell cytokinesis by Chlamydia trachomatis infection. J. Infect. 47:45-51. [DOI] [PubMed] [Google Scholar]
- 11.Grieshaber, S., J. A. Swanson, and T. Hackstadt. 2002. Determination of the physical environment within the Chlamydia trachomatis inclusion using ion-selective ratiometric probes. Cell. Microbiol. 4:273-283. [DOI] [PubMed] [Google Scholar]
- 12.Hackstadt, T., M. A. Scidmore-Carlson, E. I. Shaw, and E. R. Fischer. 1999. The Chlamydia trachomatis IncA protein is required for homotypic vesicle fusion. Cell. Microbiol. 1:119-130. [DOI] [PubMed] [Google Scholar]
- 13.Heinzen, R. A., and T. Hackstadt. 1997. The Chlamydia trachomatis parasitophorous vacuolar membrane is not passively permeable to low-molecular-weight compounds. Infect. Immun. 65:1088-1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kiviat, N. B., J. A. Paavonen, J. Brockway, C. W. Critchlow, R. C. Brunham, C. E. Stevens, W. E. Stamm, C. C. Kuo, T. DeRouen, and K. K. Holmes. 1985. Cytologic manifestations of cervical and vaginal infections. I. Epithelial and inflammatory cellular changes. JAMA 253:989-996. [PubMed] [Google Scholar]
- 15.Medrano, E. E., and A. B. Pardee. 1980. Prevalent deficiency in tumor cells of cycloheximide-induced cycle arrest. Proc. Natl. Acad. Sci. USA 77:4123-4126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moorman, D. R., J. W. Sixbey, and P. B. Wyrick. 1986. Interaction of Chlamydia trachomatis with human genital epithelium in culture. J. Gen. Microbiol. 132:1055-1067. [DOI] [PubMed] [Google Scholar]
- 17.Nicholson, T. L., L. Olinger, K. Chong, G. Schoolnik, and R. S. Stephens. 2003. Global stage-specific gene regulation during the developmental cycle of Chlamydia trachomatis. J. Bacteriol. 185:3179-3189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rockey, D. D., E. R. Fischer, and T. Hackstadt. 1996. Temporal analysis of the developing Chlamydia psittaci inclusion by use of fluorescence and electron microscopy. Infect. Immun. 64:4269-4278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rockey, D. D., D. Grosenbach, D. E. Hruby, M. G. Peacock, R. A. Heinzen, and T. Hackstadt. 1997. Chlamydia psittaci IncA is phosphorylated by the host cell and is exposed on the cytoplasmic face of the developing inclusion. Mol. Microbiol. 24:217-228. [DOI] [PubMed] [Google Scholar]
- 20.Rockey, D. D., R. A. Heinzen, and T. Hackstadt. 1995. Cloning and characterization of a Chlamydia psittaci gene coding for a protein localized in the inclusion membrane of infected cells. Mol. Microbiol. 15:617-626. [DOI] [PubMed] [Google Scholar]
- 21.Rockey, D. D., M. A. Scidmore, J. P. Bannantine, and W. J. Brown. 2002. Proteins in the chlamydial inclusion membrane. Microbes Infect. 4:333-340. [DOI] [PubMed] [Google Scholar]
- 22.Scheffé, H. 1959. The analysis of variance. John Wiley & Sons, Inc., New York, N.Y.
- 23.Scidmore, M. A., and T. Hackstadt. 2001. Mammalian 14-3-3β associates with the Chlamydia trachomatis inclusion membrane via its interaction with IncG. Mol. Microbiol. 39:1638-1650. [DOI] [PubMed] [Google Scholar]
- 24.Starnbach, M. N., W. P. Loomis, P. Ovendale, D. Regan, B. Hess, M. R. Alderson, and S. P. Fling. 2003. An inclusion membrane protein from Chlamydia trachomatis enters the MHC class I pathway and stimulates a CD8+ T cell response. J. Immunol. 171:4742-4749. [DOI] [PubMed] [Google Scholar]
- 25.Suchland, R. J., L. O. Eckert, S. E. Hawes, and W. E. Stamm. 2003. Longitudinal assessment of infecting serovars of Chlamydia trachomatis in Seattle public health clinics: 1988-1996. Sex Transm. Dis. 30:357-361. [DOI] [PubMed] [Google Scholar]
- 26.Suchland, R. J., D. D. Rockey, J. P. Bannantine, and W. E. Stamm. 2000. Isolates of Chlamydia trachomatis that occupy nonfusogenic inclusions lack IncA, a protein localized to the inclusion membrane. Infect. Immun. 68:360-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Suchland, R. J., and W. E. Stamm. 1991. Simplified microtiter cell culture method for rapid immunotyping of Chlamydia trachomatis. J. Clin. Microbiol. 29:1333-1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang, S. P., C. C. Kuo, R. C. Barnes, R. S. Stephens, and J. T. Grayston. 1985. Immunotyping of Chlamydia trachomatis with monoclonal antibodies. J. Infect. Dis. 152:791-800. [DOI] [PubMed] [Google Scholar]
- 29.Zhong, G., P. Fan, H. Ji, F. Dong, and Y. Huang. 2001. Identification of a chlamydial protease-like activity factor responsible for the degradation of host transcription factors. J. Exp. Med. 193:935-942. [DOI] [PMC free article] [PubMed] [Google Scholar]