Summary
Background
Despite the immense impact of Long COVID on public health and those affected, its aetiology remains poorly understood. Findings suggest that psychological factors such as depression contribute to symptom persistence alongside pathophysiological mechanisms, but knowledge of their relative importance is limited. This study aimed to synthesise the current evidence on psychological factors potentially associated with Long COVID and condition-relevant outcomes like quality of life.
Methods
In this systematic review and meta-analysis, MEDLINE, PsycINFO, and the Cochrane Database of Systematic Reviews were searched for peer-reviewed studies published in English from 2019 to January 2, 2024. Studies providing cross-sectional or longitudinal data on the association between at least one psychological variable and the presence of Long COVID (primary outcome) or condition-relevant secondary outcomes (symptom severity, impairment, quality of life, and healthcare utilisation) were included. Psychological constructs with at least five comparisons were pooled as odds ratio (OR) for categorical data and standardised mean difference (SMD) for continuous data in random-effects meta-analyses of cross-sectional studies with control groups. This review is registered with PROSPERO, CRD42023408320.
Findings
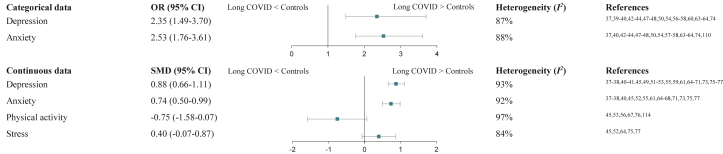
113 studies (n = 312,831 patients with Long COVID) provided data on at least one psychological variable, 63 in cross-sectional group comparisons, 53 in cross-sectional associations, and 18 longitudinal. Most reported findings related to depression and anxiety, and — less frequently — to physical activity, posttraumatic stress disorder, stress, and history of mental illness. Depression (OR 2.35; 95% CI, 1.49–3.70) and anxiety (OR 2.53; 95% CI, 1.76–3.61) were significantly associated with Long COVID and higher in affected patients than controls (depression: SMD 0.88; 95% CI, 0.66–1.11; anxiety: SMD 0.74; 95% CI, 0.50–0.99), while results for physical activity and stress were non-significant. In most prospective studies, the investigated psychological constructs significantly predicted Long COVID.
Interpretation
Evidence suggests depression and anxiety to be co-occurring phenomena and predictive factors of Long COVID. Future studies should prospectively investigate psychological constructs such as emotion regulation or dysfunctional symptom expectations, which are well-known risk factors and therapeutic targets of persistent somatic symptoms in other medical conditions, but are so far understudied in Long COVID.
Funding
None.
Keywords: Long COVID, Post COVID-19 condition, Persistent somatic symptoms, Biopsychosocial model, Psychological factors
Research in context.
Evidence before this study
Besides pathophysiological mechanisms, a growing number of studies indicate the potential role of psychological factors in the development and maintenance of Long COVID. Previous reviews of risk factors for Long COVID confirmed the importance of depression and anxiety; however, a broad spectrum of further psychological variables possibly involved in the persistence of somatic symptoms, such as emotion regulation or dysfunctional symptom expectations, has been relatively overlooked. To improve the understanding of Long COVID and inform research into much-needed treatments, aggregating the available evidence on psychological factors associated with Long COVID is of high relevance. We searched MEDLINE, PsycINFO, and the Cochrane Database of Systematic Reviews for peer-reviewed studies published in English from 2019 to January 2, 2024. Studies were required to report a) cross-sectional comparisons on psychological factors between patients with Long COVID and controls, b) cross–sectional associations with Long COVID or condition-relevant outcomes (symptom severity, impairment, quality of life, and healthcare utilisation), or c) prospective relations between psychological factors and Long COVID. 113 eligible studies of mostly fair quality included 312,831 patients with Long COVID and provided data for 58 psychological constructs in total.
Added value of this study
Of all psychological variables investigated, this systematic review could only confirm higher levels of depression and anxiety in individuals with Long COVID compared to controls in meta-analyses. Both factors were also predictive of Long COVID in longitudinal studies. The scarce evidence base for all other psychological variables hinders reliable conclusions.
Implications of all the available evidence
The results of this review, together with previous studies, support that depression and anxiety should be considered in multidisciplinary Long COVID treatments. Future studies should examine psychological constructs such as emotion regulation or expectations, which are well-known risk factors and therapeutic targets of persistent somatic symptoms in other medical conditions, but are so far understudied in Long COVID. Large methodological heterogeneity of the identified studies points to the need of guidelines for research on Long COVID.
Introduction
Five years after the outbreak of the COVID-19 pandemic, the aetiology of Long COVID1 is far from being clearly understood. Investigations into the pathophysiology of persistent somatic symptoms after SARS-CoV-2 infection have remained inconclusive so far, with no diagnostic markers known to fully explain them2 and several reports of objective clinical examinations discrepant with subjective symptom burden.3, 4, 5 While a growing body of research suggests that psychological factors like depression or anxiety contribute to the development and maintenance of Long COVID in addition to pathophysiological changes,6, 7, 8 the discussion about the involvement of psychological processes in its aetiology also raises critics who fear a “psychologisation” of the condition.6,9
Persistent somatic symptoms remain after many infectious diseases10 and are generally common in the general population.11 Research into persistent somatic symptoms and chronic medical diseases indicates accompanying psychological features such as health anxiety or negative expectations to be more crucial for impairment in quality of life or increase in healthcare utilisation of affected patients than the severity of the somatic symptoms per se.12 Accordingly, evidence-based etiological models clearly argue for the contribution of both biomedical and psychological mechanisms to the development and persistent course of somatic symptoms.13, 14, 15 Besides depression and anxiety,16,17 aggravating factors include cognitive-perceptual mechanisms such as selective attention, somatosensory amplification,18 and catastrophising.19,20 Additional assumed maintaining factors are unhelpful symptom-related behaviours like physical inactivity and dysfunctional healthcare use.21,22 Emotion regulation deficits, adverse childhood experiences, negative affectivity, or life stressors20,23, 24, 25 can predispose the development of persistent somatic symptoms. The same complex biopsychosocial interactions including a broad spectrum of psychological mechanisms can also be assumed for processes of symptom development and persistence in Long COVID.
While not accounting for non-affected control groups, van der Feltz-Cornelis et al.26 recently meta-analysed the all-time prevalence of any mental health condition in patients with Long COVID. They found a prevalence of 20.4%, with most studies on depression and anxiety, and the odds of mental health conditions significantly increasing over time after acute infection. Previous systematic reviews and meta-analyses of risk factors for Long COVID have largely neglected the role of psychological risk factors other than depression and anxiety.7,27
Regarding further potentially relevant psychological concepts, Hüsing et al.28 developed the PSY-PSS framework for systematic reviews to support the aggregation of empirical evidence on psychological (risk) factors in persistent somatic symptoms and related conditions. It provides the first comprehensive list of psychological variables to be considered in this field of research, which is constantly being expanded and has recently been applied in a systematic review of psychological risk factors for somatic symptom disorder.29 Considering Long COVID as dominated by persistent somatic symptoms, it is likely that the psychological constructs compiled in the PSY-PSS framework are also relevant with regard to this condition.
This study aimed to systematically review literature providing original data on psychological constructs associated with Long COVID and Long COVID-relevant outcomes by applying the PSY-PSS framework28 and, where possible, pool data using meta-analyses. For an individual psychological variable to be of relevance for Long COVID, it should either 1) be significantly higher in patients with Long COVID compared to controls, or 2) show a significant association with Long COVID or condition-relevant outcomes (symptom severity, impairment, quality of life, and healthcare utilisation), or 3) prove as a significant predictor of the development or maintenance of Long COVID. Consequently, three methodological approaches were followed and translated into the following three research questions (RQs):
-
1)
In which psychological factors do patients with Long COVID report significantly higher values compared to control groups (cross-sectional group comparisons; RQ1)?
-
2)
Which psychological factors are significantly associated with the presence of Long COVID or condition-relevant outcomes such as symptom severity, impairment, quality of life, and healthcare utilisation (cross-sectional associations; RQ2)?
-
3)
Which psychological factors significantly predict the development or maintenance of Long COVID (longitudinal data; RQ3)?
Methods
This systematic review and meta-analysis was preregistered on PROSPERO (CRD42023408320) and was conducted and reported in accordance with the PRISMA guidelines as well as the MOOSE reporting guidelines for meta-analyses of observational studies.30 It is the second review that emerged from a proposed framework of systematic reviews designed to facilitate research in the area of persistent somatic symptoms (PSY-PSS28) and follows the methodology outlined in the PROSPERO registration (CRD42022302014). Ethical approval was not sought or required, as the study involved no individual patient data.
Eligibility criteria
Articles were eligible if written in English and published in a peer-reviewed journal since 2019, i.e., since the COVID-19 outbreak. Studies were required to report original, quantitative data on at least one of the pre-defined psychological variables from the comprehensive list of the PSY-PSS framework by any tool of measure in patients of any age group who self-report to suffer from or have received a clinical diagnosis of Long COVID according to the NICE guideline (i.e., somatic symptoms that develop during or after SARS-CoV-2 infection, continue for at least 4 weeks, and are not explained by an alternative diagnosis).1 Studies that referred to other conditions or used an unclear definition of Long COVID were excluded.
Studies needed to provide a) cross-sectional comparisons between patients with Long COVID and controls, b) cross-sectional associations, or c) longitudinal data on the relation between psychological variables and the presence of Long COVID (primary outcome) or condition-relevant secondary outcomes (i.e., symptom severity, impairment defined as impaired functioning in activities of daily living,31 quality of life, or healthcare utilisation). Preprints, case reports, purely qualitative studies, reviews and meta-analyses with no new data, study protocols, editorials, comments, letters, conference abstracts, and grey literature such as dissertations were excluded. Studies using results from previous publications (secondary analyses) were not included to prevent bias.
Study selection
To ensure all relevant publications on Long COVID were found, an extensive list consisting of the 21 most commonly used terms for Long COVID in pertinent publications and guidelines1,32 in a variation of spellings was compiled. For psychological factors, the comprehensive list of the PSY-PSS framework28 was applied, which was generated to be used as search terms for literature reviews on persistent somatic symptoms. This list has a hierarchical structure, with seven overarching categories of psychological mechanisms (affective, cognitive, behavioural, psychophysiological, personality & interpersonal factors, prior experiences, and psychopathology) containing 120 psychological variables overall (e.g., emotion regulation, expectations, or illness behaviour; list and search terms can be found in the open science framework: https://osf.io/anbm6). All 120 terms from the list of potentially relevant psychological factors were crossed with all 21 Long COVID terms. The literature search was first run on 06/25/2023, and updated on 01/02/2024 using the bibliographic databases MEDLINE (via PubMed), PsycINFO (via OvidSP), and the Cochrane Database of Systematic Reviews (via Cochrane Library). The search syntax string including the precise search terms is available in eAppendix 1 in the Supplement. Due to the large number of hits, a manual search in the reference lists of obtained articles was not carried out.
Endnote33 was used to combine identified studies from all databases. Three authors (CS, MR, PE) removed duplicates and screened study titles and abstracts using the software Rayyan.34 Conflicts were resolved following discussion between the three authors. Studies identified for full-text review were independently reviewed twice against eligibility criteria by initially blinded authors (PE, MR, CS, SS, AT, MSM). Disagreements during full-text review were cleared through consultation of other authors (PE, MR, CS, SS, AT, MSM).
Data extraction
Full-text data extraction was independently completed and summarised in one descriptive and three results tables (one for each RQ) by four authors (PE, MR, CS, AT). Descriptive data comprising study design and objectives, sample characteristics, diagnostic criteria used for Long COVID, and a short summary of key results were extracted for all studies. If control groups were described as individuals without prior SARS-CoV-2 infection and not explicitly labelled as diagnosed with another medical condition, they were categorised as “healthy controls without a history of COVID-19”. For cross-sectional associations and longitudinal evidence (RQ2 and RQ3), condition-relevant outcomes and their assessment along with effect sizes (if reported) were compiled. Besides the operationalisation of the respective construct, the following data were retrieved regarding psychological variables: raw measures of central tendency, frequencies, significance statistics, and effect sizes for each group in cross-sectional comparisons (RQ1), correlations and proportions for cross-sectional associations (RQ2), and predictive testing for longitudinal studies (RQ3). When reported data were inconsistent or incomplete, corresponding authors were contacted for clarification during the data extraction process.
Statistics
The study quality assessment tools of the National Institutes of Health (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools) were employed to assess study quality and bias. Two authors (PE, AT) independently evaluated each study. Disparities were discussed between the two authors until reaching agreement.
To provide a concise overview of the available evidence for each psychological construct investigated so far in any of the included study designs, results were further summarised in a synthesis table. Meta-analyses were conducted if valid data was available for at least five studies per psychological variable, per type of data (psychological features in categorical vs. continuous format), and per outcome variable (for RQ2 and RQ3). The minimum number of studies for meta-analysis was increased from three to five compared to the predefined number stated in the PROSPERO registration (CRD42023408320) in favour of the robustness of findings given the heterogeneous assessment of psychological variables.
Meta-analyses were performed separately for psychological variables measured categorically (e.g., diagnosis of depression) and continuously (e.g., depression severity). If studies did not report the same central tendencies, corresponding authors were asked to provide mean values to integrate all continuous data. For studies that reported several follow-ups on persistent symptoms after SARS-CoV-2 infection, the first follow-up was used to be able to run analyses with the highest pooled sample size possible. Control groups of studies that examined both healthy controls without a history of SARS-CoV-2 infection and patients after SARS-CoV-2 infection without Long COVID were merged into one control group since no relevant differences between these two groups were assumed (i.e., healthy controls might have had a hidden infection).35 Studies with other control groups were excluded from meta-analyses due to an insufficient number of studies.
Due to the presumed heterogeneity between studies, random-effects models with raw data were employed. Effect sizes were estimated as odds ratio (OR) for categorical data and standardised mean difference (SMD) for continuous data. Heterogeneity between studies was quantified using I2. Risk for publication bias was assessed graphically through funnel plots and statistically with Egger's regression test. In case of significance, the trim-and-fill method was applied. Sensitivity analyses were conducted by first excluding studies with the greatest weight, then those with the smallest sample size (n < 20 per group), and again by excluding studies rated as poor in the quality assessment. All analyses were performed in RStudio version 4.2.3.36
Role of the funding source
There was no funding source for this study.
Results
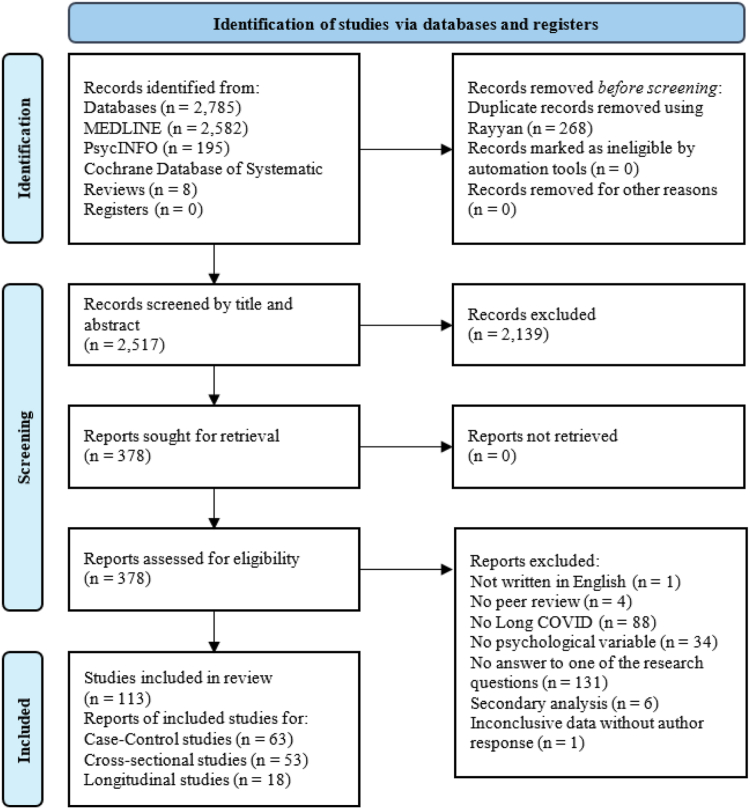
A PRISMA flow diagram of study selection is displayed in Fig. 1. Descriptive information of all included studies is shown in eTable 1 in the Supplement. Three results tables split by RQs 1–3 can be found in the Supplement (eTables 2–4).
Fig. 1.
PRISMA flow diagram. Note. Some studies give information for more than one research question.
Study characteristics and overall results
A final of 113 studies (see eReferences) were included in the review, assessing 312,831 patients with Long COVID. Sixty-eight studies were conducted in Europe (most frequent: Germany), followed by Northern America (32; most frequent: USA), Asia (24; most frequent: China), Latin America (16; most frequent: Brazil), and Australia (1), with several studies involving multiple countries. 63 studies provided data on at least one psychological construct in cross-sectional group comparisons, 53 in cross-sectional associations, and 18 longitudinal format (eTable 1 in the Supplement). According to the categories of the PSY-PSS framework,28 most studies (20) investigated signs of psychopathology, followed by cognitive factors and personality & interpersonal factors (11 each), affective and behavioural factors (5 each), and psychophysiological factors (4). For an overview of all 58 psychological features examined in total, their respective category, and their number of investigations, separated by research question, see eTable 5 in the Supplement. The available evidence for each psychological concept assessed in patients with Long COVID in each included study design is synthesised in Table 1.
Table 1.
Synthesis of evidence for all psychological variables by research question.
| Psychological variable | RQ1 (cross-sectional group comparisons) | RQ2 (cross-sectional associations) |
RQ3 (longitudinal data) |
||
|---|---|---|---|---|---|
| Sig. association | No sig. association | Sig. prediction | No sig. prediction | ||
| Depression | LC > CO (27)37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63/HC (17)37,44, 45, 46,55,56,61,64, 65, 66, 67, 68, 69, 70, 71, 72, 73 LC = CO (4)37,38,74,75/HC (4)37,64,76,77/FMS (1)78/CFS (1)78/PCS (1)79 LC < ME/CFS (1)80 |
QoL (9),41,81, 82, 83, 84, 85, 86, 87, 88 fatigue (6),41,51,68,80,82,89 impairment (5),80,88,90, 91, 92 LC (4),54,59,93,94 number of persistent symptoms (4),40,84,95,96 cognitive deficits (4),97, 98, 99, 100 pain (2),80,83 gastrointestinal symptoms (1)95 | LC (3),40,49,101 number of persistent symptoms (1),52 cognitive deficits (1)102 | LC (7),6,8,67,103, 104, 105, 106 impairment (2),6,106 fatigue (2)39,107 | LC (2),50,108 fatigue (1),109 pain (1),109 respiratory symptoms (1)109 |
| Anxiety | LC > CO (18)37,38,40,42, 43, 44, 45,47,48,52,54,55,57,58,61, 62, 63,110/HC (13)37,45,46,55,61,64, 65, 66, 67, 68,71, 72, 73 LC = CO (6)37,38,50,74,75,111/HC (4)37,44,64,77/ME/CFS (1)80/FMS (1)78/CFS (1)78/PCS (1)79 LC < ME/CFS (1)80 |
QoL (5),81,84,86, 87, 88 number of persistent symptoms (5),40,52,84,95,96 fatigue (4),68,80,82,89 cognitive deficits (4),97, 98, 99, 100 LC (3),40,54,93 impairment (2),91,92 pain (2),80,83 gastrointestinal symptoms (1)95 | QoL (4),82,83,85,112 impairment (1),80 fatigue (1),80 pain (1)80 | LC (3),6,8,110 impairment (1),6 cognitive deficits (1)107 | LC (3),50,67,108 fatigue (1),109 pain (1),109 respiratory symptoms (1)109 |
| Physical activity | LC = CO (2)53,113/HC (1)114 LC < CO (3)45,56,115/HC (4)45,56,67,76 |
LC (1),116 symptom severity (1),56 impairment (1),56 QoL (1),117 overall health (1)56 | LC (3),113,116,118 QoL (2)86,117 | LC (1)119 | – |
| Depression/Anxiety | LC > CO (6)44,63,120, 121, 122, 123/HC (2)44,124 LC = CO (1)125/HC (1)114 |
LC (2),126,127 fatigue (2),51,128 impairment (1),126 QoL (1)117 | – | LC (1),121 respiratory symptoms (1)129 | LC (1)125 |
| PTSD | LC > CO (4)44,47,63,122/HC (2)44,73 LC = CO (2)48,75 |
LC (1),93 number of persistent symptoms (1),95 gastrointestinal symptoms (1)95 | fatigue (1)130 | – | – |
| Stress | LC > CO (2)45,58/HC (2)45,64 LC = CO (3)52,75,113/HC (1)77/PCS (1)79 |
QoL (1)81 | QoL (1)81 | LC (2),6,106 impairment (2)6,106 | – |
| History of mental health disorders | LC > CO (3)39,131,132 LC = CO (2)39,74 LC < CO (1)115 |
LC (3)131, 132, 133 | LC (1)131 | fatigue (1)39 | |
| Alcohol abuse/dependence | LC = CO (2)60,134/PCS (1)79 | – | – | – | – |
| Suicidal ideation | LC > CO (1)47 LC = PCS (1)79 LC < ME/CFS (1)80 |
impairment (1),80 fatigue (1),80 pain (1)80 | – | – | – |
| Mood disorders | LC > CO (1)37/HC (2)37,76 | – | cognitive deficits (1)135 | dizziness (1),136 change in appetite (1)136 | fatigue (1),136 cognitive deficits (1),136 sleep disturbance (1)136 |
| Reaction to severe stress and adjustment disorders | LC > HC (1)72 LC = CO (1)110 |
– | – | LC (1)108 | LC (1)110 |
| Mania | LC = PCS (1)79 | – | – | – | – |
| Schizophrenia/Psychosis/Paranoia | LC < PCS (1)79 | – | – | LC (1)103 | – |
| ADHD | – | – | – | – | cognitive deficits (1)136 |
| Disorders of psychological development | LC = CO (1)110 | – | – | – | LC (1)110 |
| Nicotine abuse/dependence | – | – | – | LC (1)103 | LC (1)108 |
| Drug problems/substance abuse | LC = PCS (1)79 | – | – | LC (1)103 | – |
| Borderline features | LC = PCS (1)79 | – | – | – | – |
| Antisocial features | LC = PCS (1)79 | – | – | – | – |
| Thought disorder | LC > CO (1)37/HC (1)37 | – | – | – | – |
| Depression medications | LC = HC (1)76 | – | LC (1)137 | – | – |
| Anxiety medications | – | LC (1)137 | – | – | – |
| Loneliness | – | – | – | LC (2)6,119 | impairment (1)6 |
| Anger | LC = HC (1)76 | – | – | – | – |
| Positive trait affect | – | – | – | LC (1),106 impairment (1)106 | – |
| Fear of COVID-19 | LC > CO (1)62 LC = CO (1)138 LC < HC (1)138 |
LC (1)139 | LC (1)137 | LC (1),106 impairment (1)106 | – |
| Maternal health anxiety | LC > CO (1)138/HC (1)138 | – | – | – | – |
| Worry about COVID-19 | – | – | – | LC (1),6 impairment (1)6 | – |
| Catastrophising | LC > CO (1)45/HC (1)45 LC = FMS (1)78 LC < CFS (1)78 |
QoL (1)83 | pain (1)83 | – | – |
| Negative cognitions | LC = HC (1)114 | – | – | – | – |
| Personal control | – | fatigue (1)82 | QoL (1)82 | – | – |
| Treatment control | – | fatigue (1)82 | QoL (1)82 | – | – |
| Treatment rejection | LC = PCS (1)79 | – | – | – | – |
| Coherence | – | fatigue (1)82 | QoL (1)82 | – | – |
| Self-compassion | – | symptom severity (1),140 psychosocial impact (1)140 | – | – | – |
| Emotional representation | – | fatigue (1)82 | QoL (1)82 | – | – |
| Illness identity | – | QoL (1),82 fatigue (1)82 | – | – | – |
| Walking self-efficacy | LC = HC (1)76 | – | – | – | – |
| Fear avoidance/Kinesiophobia | LC > CO (1)45/HC (1)45 LC = CFS (1)78 LC < FMS (1)78 |
– | QoL (1),83 pain (1)83 | – | – |
| Avoidance | LC = HC (1)114 | – | – | – | – |
| Connection with friends | LC = HC (1)114 | – | LC (1),114 impairment (1)114 | – | – |
| Sedentary behaviour | – | LC (1),118 fatigue (1)118 | – | – | – |
| Neuroticism/emotional instability | LC > CO (1)141/HC (1)142 | – | fatigue (1)142 | – | – |
| Extraversion | LC < HC (1)142 | – | fatigue (1)142 | – | – |
| Openness | LC = HC (1)142 | – | fatigue (1)142 | – | – |
| Conscientiousness | LC = HC (1)142 | – | fatigue (1)142 | – | – |
| Agreeableness | LC < HC (1)142 | – | fatigue (1)142 | – | – |
| Resilience | LC = CO (1)75 LC < CO (1)141 |
– | LC (2)137,143 | – | – |
| Psychological flexibility | – | symptom severity (1),140 psychosocial impact (1)140 | – | – | – |
| Aggression | LC = PCS (1)79 | – | – | – | – |
| Dominance | LC = PCS (1)79 | – | – | – | – |
| Warmth | LC = PCS (1)79 | – | – | – | – |
| Stigma | LC > CO (1)144 | – | – | – | – |
| Life events | LC > CO (1)141 LC = CO (1)141 |
– | – | fatigue (1)119 | – |
| Nonsupport | LC = PCS (1)79 | – | – | – | – |
| Psychological distress | LC > CO (1)132 LC = HC (1)145 |
cognitive deficits (1)146 | – | – | – |
| Central sensitisation | LC > CO (1)45/HC (1)45 | QoL (2),83,85 pain (1)83 | – | – | – |
| Multisensory sensitivity/somatosensory amplification | LC = CFS (1)78 LC < FMS (1)78 |
– | – | – | – |
Note. Numbers in parentheses refer to the frequency of studies. For RQ1, directions of effect are shown. Some studies provide results for more than one comparison group or outcome. RQ, research question; LC, patients with Long COVID; CO, patients after COVID-19 without Long COVID; HC, healthy controls without a history of COVID-19; ME/CFS, patients with myalgic encephalomyelitis/chronic fatigue syndrome; FMS, patients with fibromyalgia syndrome; PCS, patients with post-concussion syndrome; QoL, quality of life; sig., significant; threshold for statistical significance p < 0.05.
For RQ1, meta-analyses could be calculated for depression (17 categorical and 24 continuous comparisons), anxiety (15 categorical and 16 continuous comparisons), physical activity (6 continuous comparisons), and stress (5 continuous comparisons). The variable “depression/anxiety”, which comprises measures of either “depression or anxiety” or “depression and anxiety” as reported in the included studies, was not meta-analysed due to the higher informative value of depression and anxiety alone. For RQ2 and RQ3, it was not possible to conduct meta-analyses for any psychological factor due to highly heterogeneous outcome variables and statistical coefficients for both categorical and continuous data. The diverse operationalisation of psychological variables can be viewed for those with at least five observations, along with the respective control groups (for RQ1) or outcomes of the studies (for RQ2 and RQ3), in eTables 6–17 in the Supplement.
Research question 1: In which psychological factors do patients with Long COVID report significantly higher values compared to control groups (cross-sectional group comparisons)?
Patients with Long COVID were compared to patients after SARS-CoV-2 infection but without Long COVID in 44 studies, to healthy controls without a history of COVID-19 in 24 studies, to patients with chronic fatigue syndrome in two studies, and to patients with fibromyalgia and post-concussion syndrome in one study respectively. The most studied psychological factors within any control group were depression and anxiety, followed by physical activity, a combination of depression and/or anxiety, posttraumatic stress disorder, stress, and history of mental health disorders. For all other searched psychological constructs, evidence was very limited, with a maximum of three studies per variable (eTable 2 in the Supplement). The majority of studies found almost all maladaptive psychological factors to be significantly higher and more frequent in patients with Long COVID than in both patients after SARS-CoV-2 infection who did not develop Long COVID and in healthy controls without a history of COVID-19, with no study reporting the opposite direction. Lower scores for depression, anxiety, history of mental health disorders, paranoia, catastrophising, kinesiophobia, somatosensory amplification, and suicidal ideation were reported in patients with Long COVID compared to controls in one study each, all but one of which referred to comparisons to a control group with other persistent somatic symptoms (chronic fatigue, fibromyalgia, post-concussion syndrome). Solely no significant differences between patients with Long COVID and controls were found for alcohol abuse, drug problems, disorders of psychological development, mania, borderline features, depression medications, walking self-efficacy (confidence in the ability to walk at a certain pace for a certain time without stopping), openness, conscientiousness, connection with friends, warmth, antisocial features, anger, aggression, dominance, negative cognitions, avoidance, nonsupport, and treatment rejection. However, it should be noted that, with the exception of alcohol abuse, all of these factors were only examined in one study each. Some studies reported both significant and non-significant differences between groups for the same psychological variable depending on measures (psychometric questionnaire data vs. clinical diagnosis of depression and anxiety37,64; adverse life events in the past year vs. earlier),141 follow-up time point on symptoms after SARS-CoV-2 infection,38,39 and different aspects of a construct (trait vs. state anxiety; Table 1: RQ1).80
Meta-analysis of cross-sectional studies with control groups
Meeting the required criteria (≥5 studies with valid data in the same format) allowed meta-analyses to be calculated for depression, anxiety (both categorical and continuous comparisons), physical activity, and stress (continuous comparisons). Pooled meta-analytic evidence for each construct is presented in Fig. 2. Sensitivity analyses led to almost identical results for all the meta-analyses executed, demonstrating model robustness (see eTable 18 in the Supplement). For all forest and funnel plots, see eFigures 1–12 in the Supplement.
Fig. 2.
Pooled data from random-effects meta-analyses of cross-sectional studies with control groups. Note. OR, odds ratio; SMD, standardised mean difference; CI, confidence interval.
Depression
Meta-analysis of continuous data revealed depression to be significantly higher in patients with Long COVID compared to controls (z = 7.73; p < 0.001; eFigure 1 in the Supplement). High between-study heterogeneity (I2 = 93%, p < 0.001) and a significant risk for publication bias were found (p < 0.01). After applying the trim-and-fill method, the model remained significant with a SMD of 0.37 (95% CI, 0.07–0.67). Meta-analysis of categorical data indicated a significant association between Long COVID and depression (z = 3.69; p < 0.001; eFigure 2 in the Supplement). Again, heterogeneity between studies was high (I2 = 87%, p < 0.001). Publication bias risk was not significant (p > 0.05).
Anxiety
Meta-analysis of continuous data showed significantly higher anxiety in patients with Long COVID compared to controls (z = 5.98; p < 0.001; eFigure 3 in the Supplement). Heterogeneity testing yielded high between-study variability (I2 = 92%, p < 0.001). Risk for publication bias was significant (p < 0.01) and the model remained significant after the trim-and-fill method (SMD = 0.32; 95% CI, 0.002–0.63). Meta-analysis of categorical data resulted in a significant association between Long COVID and anxiety (z = 5.07; p < 0.001; eFigure 4 in the Supplement). High heterogeneity between studies (I2 = 88%, p < 0.001) was found. Risk for publication bias was not significant (p > 0.05).
Physical activity
The model's overall effect was not significant (p = 0.07; eFigure 5 in the Supplement). Heterogeneity between studies was high (I2 = 97%, p < 0.001). No risk for publication bias was found (p > 0.05).
Stress
The model's overall effect was not significant (p = 0.10; eFigure 6 in the Supplement). Heterogeneity between studies was high (I2 = 84%, p < 0.001). No risk for publication bias was found (p > 0.05).
Research question 2: Which psychological factors are significantly associated with the presence of Long COVID or condition-relevant outcomes such as symptom severity, impairment, quality of life, and healthcare utilisation (cross-sectional associations)?
Cross-sectional associations with psychological variables were investigated in 16 studies for presence of Long COVID, in 11 for quality of life, in 8 for impairment, in 4 for number of persistent somatic symptoms, and 2 for symptom severity. In other studies, single Long COVID symptoms such as fatigue were used as outcomes. No study examined healthcare utilisation. Depression and anxiety were by far the most frequently investigated factors, followed by physical activity and a combination of depression and/or anxiety. All other constructs were examined in no more than three studies each (eTable 3 in the Supplement). In general, most studies demonstrated significant associations between maladaptive psychological factors and Long COVID or condition-relevant outcomes. Significant negative associations between psychological factors and condition-relevant outcomes were found in only three studies in total, with these relating to depression, anxiety, suicidal ideation, and illness identity. Solely no significant associations were reported in two studies for resilience and in one study each for the personality factors extraversion, openness, conscientiousness, agreeableness, and neuroticism as well as for connection with friends, kinesiophobia, depression medications, and mood disorders. Some studies reported both significant and non-significant results depending on measures (depression reported as mean vs. cut-off),40 outcomes (mental vs. physical quality of life),81,117 acute COVID-19 severity,131 and aspects of a construct (state vs. trait anxiety80; physical activity vs. inactivity; Table 1: RQ2).116
Research question 3: Which psychological factors significantly predict the development or maintenance of Long COVID (longitudinal data)?
Prospective relations with psychological factors were assessed in 16 studies for Long COVID and in two for impairment. Other outcomes were individual Long COVID symptoms. No study investigated symptom severity, quality of life, or healthcare utilisation. Again, depression and anxiety were assessed most frequently. A maximum of three longitudinal studies each were conducted on other variables (eTable 4 in the Supplement). The majority of studies showed maladaptive psychological factors to be significant predictors of Long COVID or impairment. The only exception was one study in which psychosis, tobacco smoking, and substance abuse significantly predicted a lower risk of Long COVID. For disorders of psychological development and Attention-Deficit Hyperactivity Disorder (ADHD), only non-significant results were reported (in one study each). Results for all psychological factors can be found in Table 1, RQ3.
Risk of bias of included studies
Twelve studies providing psychological data for cross-sectional group comparisons (e.g., in case–control studies) were of good quality, 44 were fair, and seven were poor. For data on cross–sectional associations, 11 studies were of good quality, 41 were fair, and one was poor. Regarding longitudinal data, 13 studies were of good quality, five were fair, and none was poor. For individual quality ratings by study design, see eAppendix 2 in the Supplement.
Discussion
This is the first systematic review and meta-analysis of a comprehensive range of pre-defined psychological factors with potential relevance for the development and/or maintenance of Long COVID and associated symptom severity, impairment, quality of life, and healthcare utilisation. Consequently, this study aimed to identify modifiable variables that could improve the understanding of Long COVID and have therapeutic relevance for affected patients. Overall, 113 studies of varying methodology provided original data for 58 psychological constructs in total (eTable 1 in the Supplement). Findings highlight above all the importance of depression and anxiety, which could be confirmed by meta-analyses of cross-sectional studies providing comparisons between patients with Long COVID and controls. Meta-analyses of physical activity and stress with only a small number of studies yielded no mean difference between patients with Long COVID and controls. The sound evidence found for depression and anxiety is in line with earlier systematic reviews and meta-analyses on Long COVID7,26,27 and also corroborates a biopsychosocial model of persistent somatic symptoms in general which proposes both to be important maintaining and aggravating factors.13, 14, 15 However, the evidence base for psychological features other than depression and anxiety is scarce, which hinders conclusions to be drawn regarding their relevance for Long COVID.
A narrative synthesis across all study designs indicates the investigated psychological constructs to be associated with and predictive of Long COVID, with only seven studies reporting contrary results.41,78, 79, 80,82,103,115 The latter mainly concern mental health differences between patients with Long COVID and those with other persistent somatic symptoms (chronic fatigue,78,80 fibromyalgia,78 and post-concussion syndrome).79 Considering the phenotypic resemblance between Long COVID and chronic fatigue syndrome in particular,147 studies with control groups should include individuals with fatigue but no history of COVID-19 to shed further light on the role of SARS-CoV-2 infection.119,148 Due to the high infection rates worldwide, such comparisons are becoming increasingly difficult though.
The vast majority of the evidence available to date relates to the role of depression and anxiety in Long COVID. However, the spectrum of psychological criteria known to be involved in chronic somatic symptoms is broader.149 Also with regard to other post-acute infection syndromes, findings point to the importance of various psychological constructs like neuroticism or attributional styles.150,151 In the course of this review, no studies were found on potentially relevant psychological variables such as alexithymia, emotion regulation, illness behaviour, symptom perception, and expectations.28,152 In contrast to biomedical and sociodemographic risk factors for Long COVID,7 psychological factors offer the advantage of being modifiable through interventions. Therefore, diversity of assessed constructs should be increased in Long COVID research, as is already the case with other forms of persistent somatic symptoms,153 to establish further evidence-based treatment targets and inform guidelines.1 A more solid foundation of robust research findings leading to thorough explanation models could help alleviate skepticism about the importance of psychological processes and disputes about their legitimacy in the context of Long COVID.6,9
In this review, high heterogeneity between publications and, in some cases, methodological shortcomings (e.g., insufficient reporting of statistical parameters such as sum scores or mean values) were observed. In addition to the monthly volume of new publications on the topic, widely varying methodologies (e.g., measures of psychological variables and outcomes such as impairment, methods of analysis, and reported statistical parameters) complicate the consolidation of evidence in this rapidly growing field of research and question the validity of results. Guidelines for research in the field of Long COVID, including harmonisation of data collection, could improve methodological quality and comparability of future studies and pooling of data. A core battery of instruments to standardise the assessment of psychological aspects in Long COVID, for instance, would not only facilitate conclusions on their contribution to symptom persistence in the interplay between biomedical, psychological, and social factors, but also on the effectiveness of therapies.154 Beyond that, more prospective analyses of representative cohorts are greatly needed to determine the predictive value of psychological features for trajectories of somatic symptoms after COVID-19, thereby improving our etiological understanding of Long COVID and the long-term impact of psychological burden on symptom severity. Fortunately, an increasing number of studies that strengthen our findings are currently being published.148,155
In contrast to previous reviews on Long COVID, we included a wide range of psychological factors in our literature search by applying the PSY-PSS framework,28 which provides the first comprehensive list of potentially relevant psychological features in persistent somatic symptoms and related conditions such as Long COVID. One limitation concerns the scarcity of studies on Long COVID investigating psychological constructs other than depression and anxiety. While there is no doubt about their relevance in mental health research,156 exclusively focusing on depression and anxiety prevents informed conclusions about the relative importance of other psychological risk factors for Long COVID. This disparity may also be due to the fact that valid self-report measures are widely available for depression and anxiety,157,158 whereas clear recommendations on which other psychological variables should be assessed are still lacking for Long COVID.31 Great methodological heterogeneity between studies further hindered the meta-analytical synthesis of existing data. In some studies, only significant effects were reported. Such publication bias was discovered in two of our meta-analyses. Individual studies employed innovative methods, for instance allowing for intra-individual trajectories over time, which unfortunately could not be meta-analysed.159 Based on the results of our meta-analyses, no inferences can be made as to causal relations between maladaptive psychological factors and Long COVID. This requires further prospective studies. In this review, it was also not possible to investigate any interactions between psychological constructs — such as depression and anxiety — and biological factors in the aetiology of Long COVID, e.g., via inflammatory processes,160,161 which could inform the further development of a biopsychosocial explanatory model for Long COVID. Severity of SARS-Cov-2 infection, virus variant, vaccination status, pre-existing or comorbid somatic and/or mental diseases, and duration of Long COVID are important factors to be considered in the interpretation of our results. However, many studies did not provide any information on these factors. Accounting for these parameters also exceeded the scope of our study where we defined Long COVID as per NICE guideline, i.e., purely symptom-based, which does not take any of the above listed factors into account.1 Females have a higher risk of developing Long COVID7; however, we did not consider sex and gender-specific differences regarding psychological variables in this review. Overall, the ratio of female and male patients was relatively balanced across all included studies (58% females). In addition, we did not account for race or ethnicity of patients in the interpretation of our results and therefore cannot draw any conclusions regarding the racial or ethnic representativeness of study populations. We extracted data reported in manuscripts or supplements. If values were inconsistent or incorrect and we did not receive an author response, the corresponding studies were excluded. It should also be noted that we only included English-language studies and only studies up to January 2024, but new studies on Long COVID are constantly being published. We extracted additional psychological constructs that were examined in the identified studies but are not included in the PSY-PSS framework list (e.g., anger, self-compassion). Our database search, however, was based on the original list of psychological variables28 and did not cover features such as psychodynamic factors added in a newer version.162 Regarding the definition of Long COVID, we used the NICE guideline,1 i.e., symptom duration of at least 4 weeks, instead of the stricter WHO criteria of post-COVID-19 condition,32 i.e., symptom duration of at least 2 months, to take more findings into account. In the majority of identified studies, the time criterion of the WHO criteria was met (eTable 1 in the Supplement). However, no distinction was made in our interpretation of the results.
This review summarises the current evidence for psychological factors of importance for the understanding and tailored treatment of Long COVID. There is sufficient evidence for depression and anxiety to consider these variables in interventions; however, many other relevant features either miss empirical investigation or have hardly been tested in prospective designs. Psychological factors, even depression and anxiety, have insufficiently been addressed in the current mechanistic understanding of Long COVID pathophysiolog.161 While this review does not allow causal inferences regarding the role of psychological factors for Long COVID, it provides a starting point for further research. More longitudinal studies and experimental research using harmonised methods are needed to advance etiologic models of Long COVID and help differentiate between patient subtypes.163 In light of the great burden on affected patients,164 driving forward multidisciplinary treatment for Long COVID based on a biopsychosocial perspective is of high clinical and societal relevance.
Contributors
MSM and AT conceptualised and supervised the study. PE run the database search. PE, MR, and CS screened titles and abstracts. Full texts were reviewed by PE, MR, CS, SS, AT, and MSM. PE, MR, CS, and AT extracted the data. PE and AT assessed study quality and bias. PE performed the meta-analysis and drafted the manuscript. AT, MSM, BL, SS, MR, CS, and PE revised and approved the final manuscript. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Data sharing statement
The authors confirm that the data supporting the findings of this study are available within the article and its Supplementary materials.
Declaration of interests
PE reports research funding (no personal honoraria) from the German Research Foundation. SS reports research funding (no personal honoraria) from the German Research Foundation and the German Heart Foundation/German Foundation of Heart Research. BL reports research funding (no personal honoraria) from the German Research Foundation, the German Federal Ministry of Education and Research, the German Innovation Committee at the Joint Federal Committee, the European Commission's Horizon 2020 Framework Programme, the European Joint Programme for Rare Diseases (EJP), the Ministry of Science, Research and Equality of the Free and Hanseatic City of Hamburg, Germany, and the Foundation Psychosomatics of Spinal Diseases, Stuttgart, Germany. He received remunerations for several scientific book articles from various book publishers, from the Norddeutscher Rundfunk (NDR) for interviews in medical knowledge programmes on public television, and as a committee member from Aarhus University, Denmark. He received travel expenses from the European Association of Psychosomatic Medicine (EAPM), and accommodation and meals from the Societatea de Medicina Biopsyhosociala, Romania, for a presentation at the EAPM Academy at the Conferința Națională de Psihosomatică, Cluj-Napoca, Romania, October 2023. He received remuneration and travel expenses for lecture at the Lindauer Psychotherapiewochen, April 2024. He is President of the German College of Psychosomatic Medicine (DKPM) (unpaid) since March 2024 and was a member of the Board of the European Association of Psychosomatic Medicine (EAPM) (unpaid) until 2022. He is member of the EIFFEL Study Oversight Committee (unpaid). AT reports research funding (no personal honoraria) from the German Research Foundation. She received remunerations for scientific book articles. MSM reports research funding (no personal honoraria) from the German Research Foundation and the German Academic Research Service. She received remunerations for scientific book articles, from the Norddeutscher Rundfunk (NDR) for interviews in medical knowledge programmes on public television, for post graduate training for psychotherapy, and for the review of a grant proposal at the University of Toledo, USA. She is member of the Scientific Advisory Board of PKD Cure e.V. (unpaid). She is Executive Board Member and Vice-Treasurer of the European Association of Psychosomatic Medicine (EAPM) (unpaid).
Acknowledgements
MR and CS both report a limited contract as research associates at the University Medical Centre Hamburg-Eppendorf, Hamburg, Germany.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2024.102756.
Appendix A. Supplementary data
References
- 1.Shah W., Hillman T., Playford E.D., Hishmeh L. Managing the long term effects of covid-19: summary of NICE, SIGN, and RCGP rapid guideline. BMJ. 2021;372:n136. doi: 10.1136/bmj.n136. [DOI] [PubMed] [Google Scholar]
- 2.Merad M., Blish C.A., Sallusto F., Iwasaki A. The immunology and immunopathology of COVID-19. Science. 2022;375(6585):1122–1127. doi: 10.1126/science.abm8108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fleischer M., Szepanowski F., Tovar M., et al. Post-COVID-19 syndrome is rarely associated with damage of the nervous system: findings from a prospective observational cohort study in 171 patients. Neurol Ther. 2022;11(4):1637–1657. doi: 10.1007/s40120-022-00395-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ladlow P., O'Sullivan O., Houston A., et al. Dysautonomia following COVID-19 is not associated with subjective limitations or symptoms but is associated with objective functional limitations. Heart Rhythm. 2022;19(4):613–620. doi: 10.1016/j.hrthm.2021.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baumeister A., Göritz A.S., Benoy C., Jelinek L., Moritz S. Long-COVID or long before? Neurocognitive deficits in people with COVID-19. Psychiatry Res. 2022;317 doi: 10.1016/j.psychres.2022.114822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang S., Quan L., Chavarro J.E., et al. Associations of depression, anxiety, worry, perceived stress, and loneliness prior to infection with risk of post-COVID-19 conditions. JAMA Psychiatry. 2022;79(11):1081–1091. doi: 10.1001/jamapsychiatry.2022.2640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsampasian V., Elghazaly H., Chattopadhyay R., et al. Risk factors associated with post-COVID-19 condition: a systematic review and meta-analysis. JAMA Intern Med. 2023;183(6):566–580. doi: 10.1001/jamainternmed.2023.0750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Subramanian A., Nirantharakumar K., Hughes S., et al. Symptoms and risk factors for long COVID in non-hospitalized adults. Nat Med. 2022;28(8):1706–1714. doi: 10.1038/s41591-022-01909-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Lancet Long COVID: 3 years in. Lancet. 2023;401(10379):795. doi: 10.1016/S0140-6736(23)00493-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Choutka J., Jansari V., Hornig M., Iwasaki A. Unexplained post-acute infection syndromes. Nat Med. 2022;28(5):911–923. doi: 10.1038/s41591-022-01810-6. [DOI] [PubMed] [Google Scholar]
- 11.Hiller W., Rief W., Brähler E. Somatization in the population: from mild bodily misperceptions to disabling symptoms. Soc Psychiatry Psychiatr Epidemiol. 2006;41(9):704–712. doi: 10.1007/s00127-006-0082-y. [DOI] [PubMed] [Google Scholar]
- 12.Löwe B., Levenson J., Depping M., et al. Somatic symptom disorder: a scoping review on the empirical evidence of a new diagnosis. Psychol Med. 2022;52(4):632–648. doi: 10.1017/s0033291721004177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Löwe B., Andresen V., Van den Bergh O., et al. Persistent SOMAtic symptoms ACROSS diseases - from risk factors to modification: scientific framework and overarching protocol of the interdisciplinary SOMACROSS research unit (RU 5211) BMJ Open. 2022;12(1) doi: 10.1136/bmjopen-2021-057596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burton C., Fink P., Henningsen P., Löwe B., Rief W. Functional somatic disorders: discussion paper for a new common classification for research and clinical use. BMC Med. 2020;18(1):34. doi: 10.1186/s12916-020-1505-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Henningsen P., Zipfel S., Sattel H., Creed F. Management of functional somatic syndromes and bodily distress. Psychother Psychosom. 2018;87(1):12–31. doi: 10.1159/000484413. [DOI] [PubMed] [Google Scholar]
- 16.Niles A.N., O'Donovan A. Comparing anxiety and depression to obesity and smoking as predictors of major medical illnesses and somatic symptoms. Health Psychol. 2019;38(2):172. doi: 10.1037/hea0000707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Monden R., Rosmalen J.G.M., Wardenaar K.J., Creed F. Predictors of new onsets of irritable bowel syndrome, chronic fatigue syndrome and fibromyalgia: the lifelines study. Psychol Med. 2022;52(1):112–120. doi: 10.1017/s0033291720001774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barends H., Claassen-van Dessel N., van der Wouden J.C., et al. Impact of symptom focusing and somatosensory amplification on persistent physical symptoms: a three-year follow-up study. J Psychosom Res. 2020;135 doi: 10.1016/j.jpsychores.2020.110131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Claassen-van Dessel N., van der Wouden J.C., Hoekstra T., Dekker J., van der Horst H.E. The 2-year course of medically unexplained physical symptoms (MUPS) in terms of symptom severity and functional status: results of the prospects cohort study. J Psychosom Res. 2018;104:76–87. doi: 10.1016/j.jpsychores.2017.11.012. [DOI] [PubMed] [Google Scholar]
- 20.Kleinstäuber M., Schröder A., Daehler S., et al. Aetiological understanding of fibromyalgia, irritable bowel syndrome, chronic fatigue syndrome and classificatory analogues: a systematic umbrella review. Clin Psychol Eur. 2023;5(3):1–25. doi: 10.32872/cpe.11179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vlaeyen J.W., Crombez G., Linton S.J. The fear-avoidance model of pain. Pain. 2016;157(8):1588–1589. doi: 10.1097/j.pain.0000000000000574. [DOI] [PubMed] [Google Scholar]
- 22.Kitselaar W.M., van der Vaart R., Perschl J., Numans M.E., Evers A.W.M. Predictors of persistent somatic symptoms in the general population: a systematic review of cohort studies. Psychosom Med. 2023;85(1):71–78. doi: 10.1097/psy.0000000000001145. [DOI] [PubMed] [Google Scholar]
- 23.Herzog J.I., Schmahl C. Adverse childhood experiences and the consequences on neurobiological, psychosocial, and somatic conditions across the lifespan. Front Psychiatry. 2018;9:420. doi: 10.3389/fpsyt.2018.00420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Loeb T.B., Joseph N.T., Wyatt G.E., et al. Predictors of somatic symptom severity: the role of cumulative history of trauma and adversity in a diverse community sample. Psychol Trauma. 2018;10(5):491–498. doi: 10.1037/tra0000334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weinreich Petersen M., Wisbech Carstensen T.B., Frostholm L., et al. Neuroticism and adverse life events are important determinants in functional somatic disorders: the DanFunD study. Sci Rep. 2022;12(1) doi: 10.1038/s41598-022-24213-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van der Feltz-Cornelis C., Turk F., Sweetman J., et al. Prevalence of mental health conditions and brain fog in people with long COVID: a systematic review and meta-analysis. Gen Hosp Psychiatry. 2024;88:10–22. doi: 10.1016/j.genhosppsych.2024.02.009. [DOI] [PubMed] [Google Scholar]
- 27.Joli J., Buck P., Zipfel S., Stengel A. Post-COVID-19 fatigue: a systematic review. Front Psychiatry. 2022;13 doi: 10.3389/fpsyt.2022.947973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hüsing P., Smakowski A., Löwe B., Kleinstäuber M., Toussaint A., Shedden-Mora M.C. The framework for systematic reviews on psychological risk factors for persistent somatic symptoms and related syndromes and disorders (PSY-PSS) Front Psychiatry. 2023;14 doi: 10.3389/fpsyt.2023.1142484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smakowski A., Hüsing P., Völcker S., et al. Psychological risk factors of somatic symptom disorder: a systematic review and meta-analysis of cross-sectional and longitudinal studies. J Psychosom Res. 2024;181 doi: 10.1016/j.jpsychores.2024.111608. [DOI] [PubMed] [Google Scholar]
- 30.Stroup D.F., Berlin J.A., Morton S.C., et al. Meta-analysis of observational studies in EpidemiologyA proposal for reporting. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 31.Rief W., Burton C., Frostholm L., et al. Core outcome domains for clinical trials on somatic symptom disorder, bodily distress disorder, and functional somatic syndromes: European network on somatic symptom disorders recommendations. Psychosom Med. 2017;79(9):1008–1015. doi: 10.1097/psy.0000000000000502. [DOI] [PubMed] [Google Scholar]
- 32.Soriano J.B., Murthy S., Marshall J.C., Relan P., Diaz J.V., WHO Clinical Case Definition Working Group on Post-COVID-19 Condition A clinical case definition of post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis. 2022;22(4):e102–e107. doi: 10.1016/S1473-3099(21)00703-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Version EndNote 20. Clarivate. 2013. [Google Scholar]
- 34.Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Contreras S., Dehning J., Loidolt M., et al. The challenges of containing SARS-CoV-2 via test-trace-and-isolate. Nat Commun. 2021;12(1):378. doi: 10.1038/s41467-020-20699-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Team RC . R Core Team; Vienna, Austria: 2023. R Development Core Team R: a language and environment for statistical computing 2023. [Google Scholar]
- 37.Frontera J.A., Lewis A., Melmed K., et al. Prevalence and predictors of prolonged cognitive and psychological symptoms following COVID-19 in the United States. Front Aging Neurosci. 2021;13 doi: 10.3389/fnagi.2021.690383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fernández-Alonso V., Rodríguez-Fernández S., Secadas-Rincón L., Pérez-Gómez M., Moro-Tejedor M.N., Salcedo M. Resilience after COVID-19: a descriptive, cross-sectional study. Clin Nurs Res. 2023;32(3):618–628. doi: 10.1177/10547738231154326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mazza M.G., Palladini M., Villa G., De Lorenzo R., Rovere Querini P., Benedetti F. Prevalence, trajectory over time, and risk factor of post-COVID-19 fatigue. J Psychiatr Res. 2022;155:112–119. doi: 10.1016/j.jpsychires.2022.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tebeka S., Carcaillon-Bentata L., Decio V., et al. Complex association between post-COVID-19 condition and anxiety and depression symptoms. Eur Psychiatry. 2023;67:1–36. doi: 10.1192/j.eurpsy.2023.2473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wright T.J., Pyles R.B., Sheffield-Moore M., et al. Low growth hormone secretion associated with post-acute sequelae SARS-CoV-2 infection (PASC) neurologic symptoms: a case-control pilot study. Mol Cell Endocrinol. 2024;579 doi: 10.1016/j.mce.2023.112071. [DOI] [PubMed] [Google Scholar]
- 42.Alghamdi S.A., Alfares M.A., Alsulami R.A., et al. Post-COVID-19 syndrome: incidence, risk factor, and the most common persisting symptoms. Cureus. 2022;14(11) doi: 10.7759/cureus.32058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bellan M., Apostolo D., Albè A., et al. Determinants of long COVID among adults hospitalized for SARS-CoV-2 infection: a prospective cohort study. Front Immunol. 2022;13 doi: 10.3389/fimmu.2022.1038227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cai J., Lin K., Zhang H., et al. A one-year follow-up study of systematic impact of long COVID symptoms among patients post SARS-CoV-2 omicron variants infection in Shanghai, China. Emerg Microbes Infect. 2023;12(2) doi: 10.1080/22221751.2023.2220578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Calvache-Mateo A., Navas-Otero A., Heredia-Ciuró A., et al. Post-COVID patients with new-onset chronic pain 2 years after infection: cross-sectional study. Pain Manag Nurs. 2023;24(5):528–534. doi: 10.1016/j.pmn.2023.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cuschieri S., Grech S., Grech V. A glimpse into Long COVID characteristics and the mental health impact within a highly vaccinated population: a Malta observational study. Ann Ist Super Sanita. 2023;59(2):101–107. doi: 10.4415/ann_23_02_02. [DOI] [PubMed] [Google Scholar]
- 47.Goodman M.L., Molldrem S., Elliott A., Robertson D., Keiser P. Long COVID and mental health correlates: a new chronic condition fits existing patterns. Health Psychol Behav Med. 2023;11(1) doi: 10.1080/21642850.2022.2164498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Huang L., Li X., Gu X., et al. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: a longitudinal cohort study. Lancet Respir Med. 2022;10(9):863–876. doi: 10.1016/S2213-2600(22)00126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lhuillier E., Yang Y., Morozova O., et al. The impact of world trade center related medical conditions on the severity of COVID-19 disease and its long-term sequelae. Int J Environ Res Public Health. 2022;19(12) doi: 10.3390/ijerph19126963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu T.C., Yoo S.M., Sim M.S., Motwani Y., Viswanathan N., Wenger N.S. Perceived cognitive deficits in patients with symptomatic SARS-CoV-2 and their association with post-COVID-19 condition. JAMA Netw Open. 2023;6(5) doi: 10.1001/jamanetworkopen.2023.11974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Magel T., Meagher E., Boulter T., et al. Fatigue presentation, severity, and related outcomes in a prospective cohort following post-COVID-19 hospitalization in British Columbia, Canada. Front Med. 2023;10 doi: 10.3389/fmed.2023.1179783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Magnavita N., Arnesano G., Di Prinzio R.R., et al. Post-COVID symptoms in occupational cohorts: effects on health and work ability. Int J Environ Res Public Health. 2023;20(9) doi: 10.3390/ijerph20095638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Margalit I., Yelin D., Sagi M., et al. Risk factors and multidimensional assessment of long coronavirus disease fatigue: a nested case-control study. Clin Infect Dis. 2022;75(10):1688–1697. doi: 10.1093/cid/ciac283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Meza-Torres B., Delanerolle G., Okusi C., et al. Differences in clinical presentation with long COVID after community and hospital infection and associations with all-cause mortality: English sentinel network database study. JMIR Public Health Surveill. 2022;8(8) doi: 10.2196/37668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mora A.M., Kogut K., Sandhu N.K., et al. SARS-CoV-2 infection and long COVID among California farmworkers. J Rural Health. 2023;40(2):292–302. doi: 10.1111/jrh.12796. [DOI] [PubMed] [Google Scholar]
- 56.Navas-Otero A., Calvache-Mateo A., Martín-Núñez J., et al. Characteristics of frailty in perimenopausal women with long COVID-19. Healthcare (Basel) 2023;11(10) doi: 10.3390/healthcare11101468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Peters C., Dulon M., Westermann C., Kozak A., Nienhaus A. Long-term effects of COVID-19 on workers in health and social services in Germany. Int J Environ Res Public Health. 2022;19(12) doi: 10.3390/ijerph19126983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Phu D.H., Maneerattanasak S., Shohaimi S., et al. Prevalence and factors associated with long COVID and mental health status among recovered COVID-19 patients in southern Thailand. PLoS One. 2023;18(7) doi: 10.1371/journal.pone.0289382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Salve H.R., Daniel R.A., Kumar A., Kumar R., Misra P. Prevalence and determinants of long COVID among patients attending the outpatient department of a subdistrict hospital in Haryana. Cureus. 2023;15(9) doi: 10.7759/cureus.46007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Song Z., Giuriato M. Demographic and clinical factors associated with long COVID. Health Aff (Millwood) 2023;42(3):433–442. doi: 10.1377/hlthaff.2022.00991. [DOI] [PubMed] [Google Scholar]
- 61.Staples L.G., Nielssen O., Dear B.F., et al. Prevalence and predictors of long COVID in patients accessing a national digital mental health service. Int J Environ Res Public Health. 2023;20(18) doi: 10.3390/ijerph20186756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Terai H., Ishii M., Takemura R., et al. Comprehensive analysis of long COVID in a Japanese nationwide prospective cohort study. Respir Investig. 2023;61(6):802–814. doi: 10.1016/j.resinv.2023.08.008. [DOI] [PubMed] [Google Scholar]
- 63.Zhang H., Huang C., Gu X., et al. 3-year outcomes of discharged survivors of COVID-19 following the SARS-CoV-2 omicron (B.1.1.529) wave in 2022 in China: a longitudinal cohort study. Lancet Respir Med. 2023;12(1):55–66. doi: 10.1016/s2213-2600(23)00387-9. [DOI] [PubMed] [Google Scholar]
- 64.Liang H., Ernst T., Oishi K., et al. Abnormal brain diffusivity in participants with persistent neuropsychiatric symptoms after COVID-19. NeuroImmune Pharm Ther. 2023;2(1):37–48. doi: 10.1515/nipt-2022-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Al-Hadrawi D.S., Al-Rubaye H.T., Almulla A.F., Al-Hakeim H.K., Maes M. Lowered oxygen saturation and increased body temperature in acute COVID-19 largely predict chronic fatigue syndrome and affective symptoms due to Long COVID: a precision nomothetic approach. Acta Neuropsychiatr. 2023;35(2):76–87. doi: 10.1017/neu.2022.21. [DOI] [PubMed] [Google Scholar]
- 66.Ariza M., Cano N., Segura B., et al. Neuropsychological impairment in post-COVID condition individuals with and without cognitive complaints. Front Aging Neurosci. 2022;14 doi: 10.3389/fnagi.2022.1029842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Durstenfeld M.S., Peluso M.J., Peyser N.D., et al. Factors associated with long COVID symptoms in an online cohort study. Open Forum Infect Dis. 2023;10(2) doi: 10.1093/ofid/ofad047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Heine J., Schwichtenberg K., Hartung T.J., et al. Structural brain changes in patients with post-COVID fatigue: a prospective observational study. eClinicalMedicine. 2023;58 doi: 10.1016/j.eclinm.2023.101874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kozik V., Reuken P., Utech I., et al. Characterization of neurocognitive deficits in patients with post-COVID-19 syndrome: persistence, patients' complaints, and clinical predictors. Front Psychol. 2023;14 doi: 10.3389/fpsyg.2023.1233144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Martin E.M., Rupprecht S., Schrenk S., et al. A hypoarousal model of neurological post-COVID syndrome: the relation between mental fatigue, the level of central nervous activation and cognitive processing speed. J Neurol. 2023;270(10):4647–4660. doi: 10.1007/s00415-023-11819-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mikuteit M., Baskal S., Klawitter S., et al. Amino acids, post-translational modifications, nitric oxide, and oxidative stress in serum and urine of long COVID and ex COVID human subjects. Amino Acids. 2023;55(9):1173–1188. doi: 10.1007/s00726-023-03305-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Roessler M., Tesch F., Batram M., et al. Post-COVID-19-associated morbidity in children, adolescents, and adults: a matched cohort study including more than 157,000 individuals with COVID-19 in Germany. PLoS Med. 2022;19(11) doi: 10.1371/journal.pmed.1004122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.O'Sullivan O., Holdsworth D.A., Ladlow P., et al. Cardiopulmonary, functional, cognitive and mental health outcomes post-COVID-19, across the range of severity of acute illness, in a physically active, working-age population. Sports Med Open. 2023;9(1):7. doi: 10.1186/s40798-023-00552-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Alkwai H.M., Khalifa A.M., Ahmed A.M., et al. Persistence of COVID-19 symptoms beyond 3 months and the delayed return to the usual state of health in Saudi Arabia: a cross-sectional study. SAGE Open Med. 2022;10 doi: 10.1177/20503121221129918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Becker C., Beck K., Zumbrunn S., et al. Long COVID 1 year after hospitalisation for COVID-19: a prospective bicentric cohort study. Swiss Med Wkly. 2021;151 doi: 10.4414/smw.2021.w30091. [DOI] [PubMed] [Google Scholar]
- 76.Carter S.J., Baranauskas M.N., Raglin J.S., Pescosolido B.A., Perry B.L. Functional status, mood state, and physical activity among women with post-acute COVID-19 syndrome. Int J Public Health. 2022;67 doi: 10.3389/ijph.2022.1604589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Marinkovic K., White D.R., Alderson Myers A., Parker K.S., Arienzo D., Mason G.F. Cortical GABA levels are reduced in post-acute COVID-19 syndrome. Brain Sci. 2023;13(12) doi: 10.3390/brainsci13121666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Haider S., Janowski A.J., Lesnak J.B., et al. A comparison of pain, fatigue, and function between post-COVID-19 condition, fibromyalgia, and chronic fatigue syndrome: a survey study. Pain. 2023;164(2):385–401. doi: 10.1097/j.pain.0000000000002711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fry L., Logemann A., Waldron E., et al. Emotional functioning in long COVID: comparison to post-concussion syndrome using the personality assessment inventory. Clin Neuropsychol. 2023;38:1–21. doi: 10.1080/13854046.2023.2264546. [DOI] [PubMed] [Google Scholar]
- 80.Azcue N., Gómez-Esteban J.C., Acera M., et al. Brain fog of post-COVID-19 condition and chronic fatigue syndrome, same medical disorder? J Transl Med. 2022;20(1):569. doi: 10.1186/s12967-022-03764-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Scholz U., Bierbauer W., Lüscher J. Social stigma, mental health, stress, and health-related quality of life in people with long COVID. Int J Environ Res Public Health. 2023;20(5) doi: 10.3390/ijerph20053927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bierbauer W., Luscher J., Scholz U. Illness perceptions in long-COVID: a cross-sectional analysis in adults. Cogent Psychology. 2022;9(1) doi: 10.1080/23311908.2022.2105007. [DOI] [Google Scholar]
- 83.Fernández-de-Las-Peñas C., Valera-Calero J.A., Herrero-Montes M., et al. The self-reported leeds assessment of neuropathic symptoms and signs (S-LANSS) and PainDETECT questionnaires in COVID-19 survivors with post-COVID pain. Viruses. 2022;14(7) doi: 10.3390/v14071486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Giurgi-Oncu C., Tudoran C., Pop G.N., et al. Cardiovascular abnormalities and mental health difficulties result in a reduced quality of life in the post-acute COVID-19 syndrome. Brain Sci. 2021;11(11) doi: 10.3390/brainsci11111456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pacho-Hernández J.C., Fernández-de-Las-Peñas C., Fuensalida-Novo S., Jiménez-Antona C., Ortega-Santiago R., Cigarán-Mendez M. Sleep quality mediates the effect of sensitization-associated symptoms, anxiety, and depression on quality of life in individuals with post-COVID-19 pain. Brain Sci. 2022;12(10) doi: 10.3390/brainsci12101363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Salci M.A., Carreira L., Baccon W.C., et al. Perceived quality of life and associated factors in long covid syndrome among older brazilians: a cross-sectional study. J Clin Nurs. 2024;33(1):178–191. doi: 10.1111/jocn.16618. [DOI] [PubMed] [Google Scholar]
- 87.Satar S., Şahin M.E., Ergün P. Health related quality of life and its determinants in COVID-19 patients. Tuberk Toraks. 2023;71(3):250–260. doi: 10.5578/tt.20239706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Walker S., Goodfellow H., Pookarnjanamorakot P., et al. Impact of fatigue as the primary determinant of functional limitations among patients with post-COVID-19 syndrome: a cross-sectional observational study. BMJ Open. 2023;13(6) doi: 10.1136/bmjopen-2022-069217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Beyer S., Haufe S., Meike D., et al. Post-COVID-19 syndrome: physical capacity, fatigue and quality of life. PLoS One. 2023;18(10) doi: 10.1371/journal.pone.0292928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hirahata K., Nawa N., Fujiwara T. Characteristics of long COVID: cases from the first to the fifth wave in greater Tokyo, Japan. J Clin Med. 2022;11(21) doi: 10.3390/jcm11216457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lier J., Stoll K., Obrig H., et al. Neuropsychiatric phenotype of post COVID-19 syndrome in non-hospitalized patients. Front Neurol. 2022;13 doi: 10.3389/fneur.2022.988359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Luedke J.C., Vargas G., Jashar D.T., Morrow A., Malone L.A., Ng R. Cognitive disengagement syndrome in pediatric patients with long covid: associations with mood, anxiety, and functional impairment. Child Neuropsychol. 2024;30(4):652–672. doi: 10.1080/09297049.2023.2252967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Busatto G.F., de Araujo A.L., Castaldelli-Maia J.M., et al. Post-acute sequelae of SARS-CoV-2 infection: relationship of central nervous system manifestations with physical disability and systemic inflammation. Psychol Med. 2022;52(12):2387–2398. doi: 10.1017/S0033291722001374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Loosen S.H., Jensen B.O., Tanislav C., Luedde T., Roderburg C., Kostev K. Obesity and lipid metabolism disorders determine the risk for development of long COVID syndrome: a cross-sectional study from 50,402 COVID-19 patients. Infection. 2022;50(5):1165–1170. doi: 10.1007/s15010-022-01784-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Elmunzer B.J., Palsson O.S., Forbes N., et al. Prolonged gastrointestinal manifestations after recovery from COVID-19. Clin Gastroenterol Hepatol. 2023;22(5):1098–1107.e3. doi: 10.1016/j.cgh.2023.11.009. [DOI] [PubMed] [Google Scholar]
- 96.Jung Y.H., Ha E.H., Choe K.W., Lee S., Jo D.H., Lee W.J. Persistent symptoms after acute COVID-19 infection in omicron era. J Korean Med Sci. 2022;37(27) doi: 10.3346/jkms.2022.37.e213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Delgado-Alonso C., Díez-Cirarda M., Pagán J., et al. Unraveling brain fog in post-COVID syndrome: relationship between subjective cognitive complaints and cognitive function, fatigue, and neuropsychiatric symptoms. Eur J Neurol. 2023 doi: 10.1111/ene.16084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Jung Y.H., Ha E.H., Park J., Choe K.W., Lee W.J., Jo D.H. Neurological and psychiatric manifestations of post-COVID-19 conditions. J Korean Med Sci. 2023;38(11) doi: 10.3346/jkms.2023.38.e83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Tavares-Júnior J.W.L., Oliveira D.N., da Silva J.B.S., et al. Long-covid cognitive impairment: cognitive assessment and apolipoprotein E (APOE) genotyping correlation in a Brazilian cohort. Front Psychiatry. 2022;13 doi: 10.3389/fpsyt.2022.947583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Whiteside D.M., Basso M.R., Naini S.M., et al. Outcomes in post-acute sequelae of COVID-19 (PASC) at 6 months post-infection part 1: cognitive functioning. Clin Neuropsychol. 2022;36(4):806–828. doi: 10.1080/13854046.2022.2030412. [DOI] [PubMed] [Google Scholar]
- 101.Yaksi N., Teker A.G., Imre A. Long COVID in hospitalized COVID-19 patients: a retrospective cohort study. Iran J Public Health. 2022;51(1):88–95. doi: 10.18502/ijph.v51i1.8297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Delgado-Alonso C., Valles-Salgado M., Delgado-Álvarez A., et al. Cognitive dysfunction associated with COVID-19: a comprehensive neuropsychological study. J Psychiatr Res. 2022;150:40–46. doi: 10.1016/j.jpsychires.2022.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hill E.L., Mehta H.B., Sharma S., et al. Risk factors associated with post-acute sequelae of SARS-CoV-2: an N3C and NIH RECOVER study. BMC Public Health. 2023;23(1):2103. doi: 10.1186/s12889-023-16916-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Antony B., Blau H., Casiraghi E., et al. Predictive models of long COVID. eBioMedicine. 2023;96 doi: 10.1016/j.ebiom.2023.104777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Binka M., Klaver B., Cua G., et al. An elastic net regression model for identifying long COVID patients using health administrative data: a population-based study. Open Forum Infect Dis. 2022;9(12) doi: 10.1093/ofid/ofac640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Milde C., Glombiewski J.A., Wilhelm M., Schemer L. Psychological factors predict higher odds and impairment of post-COVID symptoms: a prospective study. Psychosom Med. 2023;85(6):479–487. doi: 10.1097/PSY.0000000000001214. [DOI] [PubMed] [Google Scholar]
- 107.Zhang D., Chung V.C., Chan D.C., et al. Determinants of post-COVID-19 symptoms among adults aged 55 or above with chronic conditions in primary care: data from a prospective cohort in Hong Kong. Front Public Health. 2023;11 doi: 10.3389/fpubh.2023.1138147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kostev K., Smith L., Koyanagi A., Jacob L. Prevalence of and factors associated with post-coronavirus disease 2019 (COVID-19) condition in the 12 Months after the diagnosis of COVID-19 in adults followed in general practices in Germany. Open Forum Infect Dis. 2022;9(7) doi: 10.1093/ofid/ofac333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bottemanne H., Gouraud C., Hulot J.S., et al. Do anxiety and depression predict persistent physical symptoms after a severe COVID-19 episode? A prospective study. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.757685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kostev K., Smith L., Koyanagi A., Konrad M., Jacob L. Post-COVID-19 conditions in children and adolescents diagnosed with COVID-19. Pediatr Res. 2022;95:1–6. doi: 10.1038/s41390-022-02111-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Messin L., Puyraveau M., Benabdallah Y., et al. COVEVOL: natural evolution at 6 months of COVID-19. Viruses. 2021;13(11) doi: 10.3390/v13112151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Fujita K., Otsuka Y., Sunada N., et al. Manifestation of headache affecting quality of life in long COVID patients. J Clin Med. 2023;12(10) doi: 10.3390/jcm12103533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Pływaczewska-Jakubowska M., Chudzik M., Babicki M., Kapusta J., Jankowski P. Lifestyle, course of COVID-19, and risk of Long-COVID in non-hospitalized patients. Front Med (Lausanne) 2022;9 doi: 10.3389/fmed.2022.1036556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Shachar-Lavie I., Shorer M., Segal H., Fennig S., Ashkenazi-Hoffnung L. Mental health among children with long COVID during the COVID-19 pandemic. Eur J Pediatr. 2023;182(4):1793–1801. doi: 10.1007/s00431-023-04854-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Rastogi R., Cerda I.H., Ibrahim A., Chen J.A., Stevens C., Liu C.H. Long COVID and psychological distress in young adults: potential protective effect of a prior mental health diagnosis. J Affect Disord. 2023;340:639–648. doi: 10.1016/j.jad.2023.08.031. [DOI] [PubMed] [Google Scholar]
- 116.Rocha J.Q.S., Caputo E.L., Vieira Y.P., Afonso M.D.S., Duro S.M.S., de Oliveira Saes M. Physical activity status prevents symptoms of long covid: sulcovid-19 survey. BMC Sports Sci Med Rehabil. 2023;15(1):170. doi: 10.1186/s13102-023-00782-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Samper-Pardo M., León-Herrera S., Oliván-Blázquez B., Gascón-Santos S., Sánchez-Recio R. Clinical characterization and factors associated with quality of life in Long COVID patients: secondary data analysis from a randomized clinical trial. PLoS One. 2023;18(5) doi: 10.1371/journal.pone.0278728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Zheng C., Huang W.Y., Sun F.H., et al. Association of sedentary lifestyle with risk of acute and post-acute COVID-19 sequelae: a retrospective cohort study. Am J Med. 2023 doi: 10.1016/j.amjmed.2023.12.002. [DOI] [PubMed] [Google Scholar]
- 119.Selvakumar J., Havdal L.B., Drevvatne M., et al. Prevalence and characteristics associated with post-COVID-19 condition among nonhospitalized adolescents and young adults. JAMA Netw Open. 2023;6(3) doi: 10.1001/jamanetworkopen.2023.5763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Chen S.J., Morin C.M., Ivers H., et al. The association of insomnia with long COVID: an international collaborative study (ICOSS-II) Sleep Med. 2023;112:216–222. doi: 10.1016/j.sleep.2023.09.034. [DOI] [PubMed] [Google Scholar]
- 121.Jacobs E.T., Catalfamo C.J., Colombo P.M., et al. Pre-existing conditions associated with post-acute sequelae of COVID-19. J Autoimmun. 2023;135 doi: 10.1016/j.jaut.2022.102991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Kim Y., Kim S.W., Chang H.H., Kwon K.T., Hwang S., Bae S. One year follow-up of COVID-19 related symptoms and patient quality of life: a prospective cohort study. Yonsei Med J. 2022;63(6):499–510. doi: 10.3349/ymj.2022.63.6.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Román-Montes C.M., Flores-Soto Y., Guaracha-Basañez G.A., et al. Post-COVID-19 syndrome and quality of life impairment in severe COVID-19 mexican patients. Front Public Health. 2023;11 doi: 10.3389/fpubh.2023.1155951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.de Oliveira J.F., de Ávila R.E., de Oliveira N.R., et al. Persistent symptoms, quality of life, and risk factors in long COVID: a cross-sectional study of hospitalized patients in Brazil. Int J Infect Dis. 2022;122:1044–1051. doi: 10.1016/j.ijid.2022.07.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Gaspar P., Dias M., Parreira I., et al. Predictors of long-COVID-19 and its impact on quality of life: longitudinal analysis at 3, 6 and 9 months after discharge from a portuguese centre. Acta Med Port. 2023;36(10):647–660. doi: 10.20344/amp.19047. [DOI] [PubMed] [Google Scholar]
- 126.Bonner C., Ghouralal S.L. Long COVID and chronic conditions in the U.S. workforce: prevalence, productivity loss, and disability. J Occup Environ Med. 2024;66(3):e80–e86. doi: 10.1097/jom.0000000000003026. [DOI] [PubMed] [Google Scholar]
- 127.Hastie C.E., Lowe D.J., McAuley A., et al. Outcomes among confirmed cases and a matched comparison group in the long-COVID in scotland study. Nat Commun. 2022;13(1):5663. doi: 10.1038/s41467-022-33415-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Bungenberg J., Humkamp K., Hohenfeld C., et al. Long COVID-19: objectifying most self-reported neurological symptoms. Ann Clin Transl Neurol. 2022;9(2):141–154. doi: 10.1002/acn3.51496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zheng B., Vivaldi G., Daines L., et al. Determinants of recovery from post-COVID-19 dyspnoea: analysis of UK prospective cohorts of hospitalised COVID-19 patients and community-based controls. Lancet Reg Health Eur. 2023;29 doi: 10.1016/j.lanepe.2023.100635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Harenwall S., Heywood-Everett S., Henderson R., Smith J., McEnery R., Bland A.R. The interactive effects of post-traumatic stress symptoms and breathlessness on fatigue severity in post-COVID-19 syndrome. J Clin Med. 2022;11(20) doi: 10.3390/jcm11206214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Hedberg P., Granath F., Bruchfeld J., et al. Post COVID-19 condition diagnosis: a population-based cohort study of occurrence, associated factors, and healthcare use by severity of acute infection. J Intern Med. 2023;293(2):246–258. doi: 10.1111/joim.13584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Benoit-Piau J., Tremblay K., Piché A., et al. Long-term consequences of COVID-19 in predominantly immunonaive patients: a Canadian prospective population-based study. J Clin Med. 2023;12(18) doi: 10.3390/jcm12185939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Hirschtick J.L., Xie Y., Slocum E., et al. A statewide population-based approach to examining long COVID symptom prevalence and predictors in Michigan. Prev Med. 2023;177 doi: 10.1016/j.ypmed.2023.107752. [DOI] [PubMed] [Google Scholar]
- 134.Uniyal N., Sethi Y., Sharma P.C., et al. Post-COVID syndrome and severity of COVID-19: a cross-sectional epidemiological evaluation from north India. Cureus. 2022;14(7) doi: 10.7759/cureus.27345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Ruggeri M., Ricci M., Pagliaro M., Gerace C. Anosmia predicts memory impairment in post-covid-19 syndrome: results of a neuropsychological cohort study. Eur Arch Psychiatry Clin Neurosci. 2023 doi: 10.1007/s00406-023-01670-2. [DOI] [PubMed] [Google Scholar]
- 136.Chen E.Y., Morrow A.K., Malone L.A. Exploring the influence of pre-existing conditions and infection factors on pediatric long COVID symptoms and quality of life. Am J Phys Med Rehabil. 2023;103(7):567–574. doi: 10.1097/phm.0000000000002363. [DOI] [PubMed] [Google Scholar]
- 137.Pérez-López F.R., Blümel J.E., Vallejo M.S., et al. Anxiety but not menopausal status influences the risk of long-COVID-19 syndrome in women living in Latin America. Maturitas. 2023;180 doi: 10.1016/j.maturitas.2023.107873. [DOI] [PubMed] [Google Scholar]
- 138.Freda M.F., Scandurra C., Auriemma E., et al. Long-COVID in children: an exploratory case-control study from a bio-psycho-social perspective. J Psychosom Res. 2024;176 doi: 10.1016/j.jpsychores.2023.111564. [DOI] [PubMed] [Google Scholar]
- 139.Thronicke A., Hinse M., Weinert S., Jakubowski A., Grieb G., Matthes H. Factors associated with self-reported post/long-COVID-A real-world data study. Int J Environ Res Public Health. 2022;19(23) doi: 10.3390/ijerph192316124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Tudor L., Harenwall S., Henderson R., Bland A.R. Post-covid-19 syndrome: self-compassion and psychological flexibility moderate the relationship between physical symptom load and psychosocial impact. Acta Psychol (Amst) 2023;241 doi: 10.1016/j.actpsy.2023.104093. [DOI] [PubMed] [Google Scholar]
- 141.König B.H., van Jaarsveld C.H., Bischoff E.W., Schers H.J., Lucassen P.L., Olde Hartman T.C. Prognostic factors for persistent fatigue after COVID-19: a prospective matched cohort study in primary care. Br J Gen Pract. 2023;73(730):e340–e347. doi: 10.3399/bjgp.2022.0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Delgado-Alonso C., Valles-Salgado M., Delgado-Álvarez A., et al. Examining association of personality characteristics and neuropsychiatric symptoms in post-COVID syndrome. Brain Sci. 2022;12(2) doi: 10.3390/brainsci12020265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Nishimi K., Tan J., Scoglio A., et al. Psychological resilience to trauma and risk for COVID-19 infection and somatic symptoms over two years. Psychosom Med. 2023;85(6):488–497. doi: 10.1097/psy.0000000000001215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Buonsenso D., Camporesi A., Morello R., et al. Social stigma in children with long COVID. Children (Basel) 2023;10(9) doi: 10.3390/children10091518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Carazo S., Skowronski D.M., Laforce R., Jr., et al. Physical, psychological, and cognitive profile of post-COVID conditions in healthcare workers, Quebec, Canada. Open Forum Infect Dis. 2022;9(8) doi: 10.1093/ofid/ofac386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Gouraud C., Bottemanne H., Lahlou-Laforêt K., et al. Association between psychological distress, cognitive complaints, and neuropsychological status after a severe COVID-19 episode: a cross-sectional study. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.725861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Kedor C., Freitag H., Meyer-Arndt L., et al. A prospective observational study of post-COVID-19 chronic fatigue syndrome following the first pandemic wave in Germany and biomarkers associated with symptom severity. Nat Commun. 2022;13(1):5104. doi: 10.1038/s41467-022-32507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Greißel A., Schneider A., Donnachie E., Gerlach R., Tauscher M., Hapfelmeier A. Impact of pre-existing mental health diagnoses on development of post-COVID and related symptoms: a claims data-based cohort study. Sci Rep. 2024;14(1):2408. doi: 10.1038/s41598-024-52656-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Rief W., Martin A. How to use the new DSM-5 somatic symptom disorder diagnosis in research and practice: a critical evaluation and a proposal for modifications. Annu Rev Clin Psychol. 2014;10:339–367. doi: 10.1146/annurev-clinpsy-032813-153745. [DOI] [PubMed] [Google Scholar]
- 150.Hulme K., Hudson J.L., Rojczyk P., Little P., Moss-Morris R. Biopsychosocial risk factors of persistent fatigue after acute infection: a systematic review to inform interventions. J Psychosom Res. 2017;99:120–129. doi: 10.1016/j.jpsychores.2017.06.013. [DOI] [PubMed] [Google Scholar]
- 151.Klem F., Wadhwa A., Prokop L.J., et al. Prevalence, risk factors, and outcomes of irritable bowel syndrome after infectious enteritis: a systematic review and meta-analysis. Gastroenterology. 2017;152(5):1042–1054.e1. doi: 10.1053/j.gastro.2016.12.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Löwe B., Toussaint A., Rosmalen J.G.M., et al. Persistent physical symptoms: definition, genesis, and management. Lancet. 2024;403(10444):2649–2662. doi: 10.1016/S0140-6736(24)00623-8. [DOI] [PubMed] [Google Scholar]
- 153.Petersen M.W., Carstensen T.B.W., Wellnitz K.B., et al. Neuroticism, perceived stress, adverse life events and self-efficacy as predictors of the development of functional somatic disorders: longitudinal population-based study (DanFunD) BJPsych Open. 2024;10(1):e34. doi: 10.1192/bjo.2023.644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Munblit D., O'Hara M.E., Akrami A., Perego E., Olliaro P., Needham D.M. Long COVID: aiming for a consensus. Lancet Respir Med. 2022;10(7):632–634. doi: 10.1016/s2213-2600(22)00135-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Nishimi K., Neylan T.C., Bertenthal D., Seal K.H., O'Donovan A. Association of psychiatric disorders with clinical diagnosis of long COVID in US veterans. Psychol Med. 2024:1–9. doi: 10.1017/s0033291724000114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Kieling C., Buchweitz C., Caye A., et al. Worldwide prevalence and disability from mental disorders across childhood and adolescence: evidence from the global burden of disease study. JAMA Psychiatry. 2024;81(4):347–356. doi: 10.1001/jamapsychiatry.2023.5051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Kroenke K., Spitzer R.L. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32(9):509–515. [Google Scholar]
- 158.Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 159.Burton C., Dawes H., Goodwill S., Thelwell M., Dalton C. Within and between-day variation and associations of symptoms in long Covid: intensive longitudinal study. PLoS One. 2023;18(1) doi: 10.1371/journal.pone.0280343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Group P-CC Clinical characteristics with inflammation profiling of long COVID and association with 1-year recovery following hospitalisation in the UK: a prospective observational study. Lancet Respir Med. 2022;10(8):761–775. doi: 10.1016/S2213-2600(22)00127-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Castanares-Zapatero D., Chalon P., Kohn L., et al. Pathophysiology and mechanism of long COVID: a comprehensive review. Ann Med. 2022;54(1):1473–1487. doi: 10.1080/07853890.2022.2076901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Hüsing P., Smakowski A., Löwe B., Kleinstäuber M., Toussaint A., Shedden-Mora M.C. Response to commentary: the framework for systematic reviews on psychological risk factors for persistent somatic symptoms and related syndromes and disorders (PSY-PSS). General commentary. Front Psychiatr. 2024;15 doi: 10.3389/fpsyt.2024.1359434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Lemogne C., Gouraud C., Pitron V., Ranque B. Why the hypothesis of psychological mechanisms in long COVID is worth considering. J Psychosom Res. 2023;165 doi: 10.1016/j.jpsychores.2022.111135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Malik P., Patel K., Pinto C., et al. Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL)-A systematic review and meta-analysis. J Med Virol. 2022;94(1):253–262. doi: 10.1002/jmv.27309. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.