Abstract
Peyronie’s disease is an acquired condition characterized by penile deformities caused by fibrosis of the penile tunica albuginea, leading to symptoms such as penile pain, erectile dysfunction, and other associated issues. Despite extensive research, the pathophysiology of this condition remains poorly understood, and standardized diagnostic and treatment protocols are lacking. While clinical guidelines from several professional societies exist, they do not consistently account for factors such as patient ethnicity, geography, and socioeconomic status. Thus, the Korean Society for Sexual Medicine and Andrology (KSSMA) aimed to develop recommendations tailored to clinical practice in Korea. These recommendations summarize the latest evidence, including clinical practice guidelines from various international professional societies, and represent the consensus opinion of an expert group within the KSSMA. They encompass all aspects of Peyronie’s disease, including the definition, diagnosis, non-surgical interventions, and surgical treatment options.
Keywords: Men’s health, Penile induration, Penis, Prostheses and implants, Transplants
INTRODUCTION
Peyronie’s disease is characterized by the development of fibrosis or nodule/plaque within the penile tunica albuginea, hindering penile tunica albuginea expansion during erection and resulting in a distinctive penile curvature [1]. In clinical settings, sexual difficulties often pose the primary concern, with severe cases resulting in mental distress. The reported prevalence rates vary, with some estimates reaching 20%, and they seem to be increasing [2,3,4]. While typically presenting in middle-aged men, Peyronie’s disease has been reported in individuals under the age of 40 years [5,6]. However, evidence-based treatments remain limited, primarily due to gaps in our understanding of disease pathophysiology and the lack of clinical trials on treatments. Additionally, social and cultural barriers hinder open discussion about sexual health, including genital concerns, limiting disease awareness and access to treatment.
Peyronie’s disease has a heterogenous presentation, and symptom severity varies. Concurrently, patients tend to have different expectations about treatment outcomes, creating a need for individuallly tailored interventions. While surgery has been the mainstay of treatment since the 1950s, non-surgical and minimally invasive interventions are now available and increasing, including an intralesional injection of collagenase of Clostridium histolyticum (CCH), approved by the U.S. Food and Drug Administration (FDA) in 2013.
This review aimed to provide clinical recommendations on Peyronie’s disease, endorsed by the Korean Society for Sexual Medicine and Andrology (KSSMA), including a summary of the latest evidence, which encompasses clinical guidelines compiled by international professional societies. These recommendations represent a consensus opinion of the KSSMA expert panel, capturing disease definition, and diagnosis and treatment protocols. This review should serve as a recommendation only, and the presented information should not supersede clinical judgment or be used without accounting for patient preferences and priorities.
METHODS
In August 2023, the KSSMA Clinical Practice Guideline Committee formed the project team to create a set of clinical recommendations on Peyronie’s disease. A comprehensive review of studies related to Peyronie’s disease was conducted using the PubMed and MEDLINE databases, with reference to clinical practice guidelines from the American Urological Association [1], the Canadian Urological Association [7], the European Association of Urology [8], and the International Society for Sexual Medicine [9]. Thereafter, the clinical consensus statement and recommendations were prepared based on the consensus opinion of the KSSMA expert group, aiming to reflect the clinical practice in Korea. Finally, these were reviewed by the KSSMA and the Association of Korean Urologist.
EPIDEMIOLOGY
1. Definition
Peyronie’s disease is a connective tissue disorder that is characterized by a variety of symptoms, including penile deformities such as bending and depression, pain, erectile dysfunction (ED), decreased penile length, and crystal formation, either alone or in combination, due to acquired fibrosis or nodule/plaque of the penile tunica albuginea [1]. The exact disease pathophysiology remains unknown. The most widely accepted hypothesis is that repeated microvascular injury or trauma to the penile tunica albuginea leads to abnormal wound healing and remodeling of the connective tissue into a fibrotic plaque [10,11]. Genetic predisposition to fibrosis has been suggested as a possible risk factor, but its contribution to disease onset remains controversial [12].
2. Natural progression
The duration and severity of Peyronie’s disease symptoms vary, as do the duration of treatment, severity of complications, and impact on sex life. In general, the disease onset tends to present with an acute active inflammatory phase, characterized by pain during erection and penile curvature progression, leading to chronic stable fibrotic phase at which the pain tends to disappear and penile curvature becomes stable [7].
Penile curvature resolves spontaneously, becomes permanent, and progresses in 3%–13%, 36%–67%, and 21%–48% of cases, respectively. Painful erections present in 20%–70% of cases and tend to disappear over 12 months in 90% of patients [2,3,4].
ED is often present in up to half of the cases (8%–52%), and Dupuytren’s contracture is reported in 4% to 26% of patients [13,14,15].
3. Prevalence
The prevalence of Peyronie’s disease has been estimated in the range of 0.4% to 20.3%, depending on the study method, target population, and diagnostic definition [2,3,4]. Although prevalence studies have not yet been reported in Korea, the Korean Health Insurance Review and Assessment Service has reported 3031 outpatient visits and 223 surgeries related to the disease in 2022. The disease most commonly presents in middle-aged men in their 50 to 60 years. However, disease prevalence in the range of 1.5% to 16.9% has also been reported in men under the age of 40 years [5,6]. Recent estimates tend to be higher than older estimates, which likely reflects the previous underreporting of the disease and a recent increase in disease awareness.
4. Risk factors
Commonly reported risk factors or comorbidities include hypertension, diabetes, dyslipidemia, ischemic heart disease, autoimmune disease, ED, smoking, alcohol consumption, low testosterone levels, and a history of pelvic surgery [16,17,18]. Neither cystourethroscopy nor transurethral procedures/surgeries have been known to be associated with Peyronie’s disease.
5. Summary and recommendations
Peyronie’s disease is an acquired condition that causes penile deformities due to the fibrosis of the penile tunica albuginea, resulting in erectile pain, difficulty in vaginal intromission, and other symptoms. The types and severity of symptoms vary from patient to patient. The disease is characterized by an initial acute active inflammatory phase, followed by a chronic stable fibrotic phase, and is mainly observed in men aged 50 to 60 years.
DIAGNOSIS
1. History taking
The diagnosis of Peyronie’s disease can be made based on patient history and physical examination findings alone. Accurate identification of the reported symptoms is key during history taking. The characteristics of the penis (length, girth, deformity, palpable nodule/plaque, and erectile pain), difficulty in vaginal intromission, presence of ED, timing of symptom onset, changes to symptoms over time, and duration of discomfort should be evaluated, and any aggravating factors should be identified. General medical history, including other diagnoses, treatments, and risk factors for ED and Peyronie’s disease, should be evaluated [19]. Although the Peyronie’s disease questionnaire (PDQ) may support effective history taking and diagnostics, it remains to be translated into Korean [20].
2. Physical examination
The shape of the penis at rest, size and location of any palpable nodule/plaques, and degree of deformity and curvature of the penis during erection should be noted. Stretched or erectile penile length measurements can be helpful in determining the subsequent treatment decisions and may be helpful in legal disputes [21]. An intracavernous injection using vasoactive agents can be used to accurately evaluate the erectile status of the penis, but photos taken by patients can also be used [1].
3. Imaging test
Imaging tests are not necessarily required for the diagnosis; however, the can help develop a treatment plan [22]. Ultrasound can be used to measure and locate the penile nodule/plaque, helping confirm the diagnosis. In addition, Doppler ultrasound can help assess erectile function. Abdominal computed tomography and magnetic resonance imaging scans are rarely used.
4. Summary and recommendations
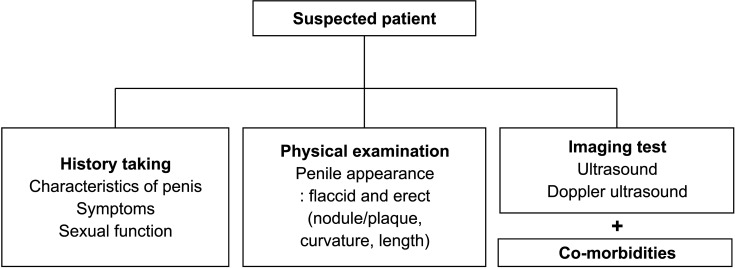
The diagnosis of Peyronie’s disease typically relies on history taking and physical examination, which capture the patient’s symptoms and penile condition (Fig. 1). An ultrasound can confirm the presence of penile nodule/plaque. Imaging tests can be helpful in developing a treatment plan.
Fig. 1. Diagnostic tools for Peyronie’s disease.
NON-SURGICAL TREATMENT
Non-surgical treatment of Peyronie’s disease involves conservative and adjuvant therapies, primarily aimed at relieving symptoms and controlling disease progression in patients with acute phase. These include oral medications, intralesional injections, extracorporeal shock wave treatment, and other topical therapies. However, treatment protocols are yet to be standardized. During the initial consultation, the physician should explain what is known and unknown about the cause and natural course of the disease, helping the patient understand the risks and benefits of any treatments, and setting up realistic expectations. The physician should evaluate any treatment risks and benefits, including long-term risks, supporting the patient in making the right decision. When judging the effectiveness of any particular treatment, the placebo effect should also be considered.
1. Oral treatment
Evidence on the efficacy of oral therapies for Peyronie’s disease is limited. The use of non-steroidal anti-inflammatory drugs (NSAIDs) is empirically recommended for pain relief. Phosphodiesterase type 5 inhibitors are helpful for patients with concomitant ED, and some preliminary findings suggest that they may help alleviate penile fibrosis [8,23].
Potassium para-aminobenzoate is a drug approved by the Korean Ministry of Food and Drug Safety, so it can be used, although the recommendation strength is not strong. Vitamin E, L-carnitine, tamoxifen, procarbazine, and omega-3, which are used empirically, have weak recommendations. Meanwhile, the use of pentoxifylline, colchicine, or co-enzyme Q10 has limited evidence, but could be tried [8].
2. Intralesional treatment
1) Collagenase of Clostridium histolyticum
CCH is a bacterial enzyme that hydrolyzes collagen, a key component of Peyronie’s disease, helping dissolve deposits. It is currently the only injectable drug approved by the U. S. FDA; however, it is yet to be authorized for use in Korea.
Previous studies have shown consistent improvement in penile curvature in 31.4% to 42.9% of patients, with an average improvement of 17°, but without significant significant improvement in pain levels, plaque size, or erectile function [24,25,26]. The use of CCH in hourglass or hinge deformity, penile ventral curvature, or calcified nodule/plaque at the penile base remains unsupported by evidence.
In almost all patients receiving this treatment, penile ecchymosis, penile swelling, and penile pain occurred, but resolved spontaneously within a few weeks in most of them. Although penile rupture is rare, sexual intercourse should be avoided for 4 weeks after the injection to prevent it.
2) Verapamil
Verapamil can inhibit plaque formation, by inhibiting extracellular matrix molecules such as fibronectin and collagen and increasing collagenase activities [27,28]. However, in the clinical trials, the efficacy was weak or unclear, but adverse events were rare and often mild. Therefore, verapamil can be considered as a treatment for Peyronie’s disease in selected patients [1].
3) Interferon
Interferon (IFN) could improve penile curvature, by decreasing fibroblast production of collagen while increasing collagenase production [29]. Clinical studies have shown that IFN relieved penile pain and improved penile blood flow, while triggering sinusitis, penile swelling, and flu-like symptoms in 40% to 100% of patients; however, these adverse events were often mild and rarely required further treatment [30,31]. IFN can be considered as a treatment for Peyronie’s disease, but its high cost and adverse events may limit its use.
4) Others
Corticosteroids, hyaluronic acid, or botulinum-toxin A are not currently recommended due to insufficient evidence for efficacy. Platelet-rich plasma may help relieve symptoms of Peyronie’s disease; however, it should be considered experimental [8].
3. Other treatments
1) Low-intensity extracorporeal shock wave treatment
In vitro studies have shown that low-intensity extracorporeal shock wave treatment (Li-ESWT) could disrupt plaque directly, and induce plaque lysis and resorption by vascularity increase [32,33]. Clinical studies have found that it relieved erectile pain but had no significant effect on reducing the plaque size or curvature [34,35]. It can be considered as a treatment for Peyronie’s disease, but the economic cost to clinical benefit ratio should be considered.
2) Penile traction and vacuum erection devices
The utility of this approaches remain undetermined, although several small studies have shown efficacy in alleviating penile curvature and increasing penile length [36,37]. However, these are safe with rare adverse events, so they can be used as single treatment or as part of combination treatments.
3) Others
Topical application of verapamil or irradiation to the lesion remains in the experimental stage and cannot be recommended until further supporting evidence becomes available.
4. Summary and recommendations
Nonsurgical treatments are mainly suitable for acute active inflammatory phase of Peyronie’s disease, or when surgical treatments are contraindicated. Despite a large library of studies, the evidence remains insufficient to make conclusive clinical recommendations [38,39].
Oral and intralesional treatments have relatively rare adverse events and have a potential to be effective, but further studies are needed. CCH, which is the only intralesional treatment option approved in the United States, is the best nonsurgical treatments option currently available. Li-ESWT and traction therapy are likely to be effective in improvement in penile pain and curvature, respectively.
SURGICAL TREATMENT
Surgical treatment for Peyronie’s disease aims to correct the penile curvature, and to allow penile penetration into the vagina during intercourse. Although surgical procedures and techniques vary and are not standardized, surgery shows the fastest, most stable and long-lasting results among the treatments for Peyronie’s disease.
Surgical procedures are broadly divided into three types: tunical shortening procedure, tunical lengthening procedure, and penile prosthesis insertion (PPI) [40,41,42,43,44,45,46]. Tunical shortening procedure can be considered first for simple and mild penile deformities, and is most commonly performed among the surgical procedures. Tunical lengthening procedure may be a favorable option for severe or complex deformities as well as severe penile length shortening. PPI is typically reserved in patient with concomitant ED that does not respond to any medical therapy. However, it should be kept in mind that any surgical procedure or technique does not have absolute indications. The detailed surgical method is selected based on preoperative assessments of penile length, degree of penile deformity including curvature, and erectile function, as well as physician/patient’s preference [1,9].
1. Preoperative preparation
When considering surgery, the general principle is that surgery should be performed on patients in a stable phase. Surgery may be considered 6 to 12 months after onset, given no changes in nodule/plaque or curvature for 3 to 6 months, or given a severe deformity that makes intercourse difficult [47]. Surgery may also be considered when conservative treatments fail, when the penile nodule/plaque is widespread to begin with, or when the patient wants fast results. It is also possible to skip nonsurgical treatment and proceed directly to surgery, but patients must be fully informed about the potential complications following surgery [40,48].
Ahead of surgery, patients should be guided toward having realistic expectations of treatment outcomes. Patients should be made aware that partial nodules/plaques or curvature may remain, and that shortening of the penile length may occur during erection. ED is often present before surgery and can occur after any surgery except PPI. Managing expectations is crucial for the therapeutic relationship between the physician and patient, helping prevent postsurgical conflicts.
The informed consent should include discussing the potential risks and benefits of possible surgical treatments including planned surgical method, with particular emphasis on patient-specific characteristics which may affect outcomes [47,49].
2. Tunical shortening procedure
The tunical shortening procedure is a surgical method of straightening the penis by shortening the longer, convex part to make it even with the opposite side. In patients with normal erectile function and adequate penile length, and without complicated deformities and significant curvature, a tunical shortening procedure may be suitable. The procedure can be broadly classified as excision, incision, and plication techniques. Although various techniques with modifications have been introduced, no one technique can be said to be superior to the other. Therefore, the selection of technique relies on the physician/patient’s preference and patient-specific characteristics.
The Nesbit technique involves the removal and suturing of a portion of the tunica albuginea on the convex side of the curvature [50]. The Yachia technique, instead of removing a portion of the tunica albuginea, involves making a longitudinal incision and suturing horizontally [51]. The penile plication technique is a method of shortening the length of convex side by passing sutures and creating knots through an appropriate range of the tunica albuginea without excision or incision [52].
Tunical shortening procedures are successful in correcting the curvature in most (>85%) patients. Recurrence of curvature and penile hypoesthesia are rare (up to 10%), and the risk of postoperative ED is low. Meanwhile, penile length shortening can occur, and procedures may not correct hinge or hourglass deformities but rather worsen them. Possible complications include persistent penile pain, persistent or recurrent penile curvature (>30°, 8%–11%), penile hematoma (0%–9%), urethral injury (0%–1.4%), palpable suture knots, and penile hypoesthesia. While tunical shortening procedures rarely cause postoperative sexual dysfunction, patients may perceive penile length shortening to be greater than it actually is. Therefore, regardless of the techniques used, measuring and recording penile length before and after surgery can be helpful for patient understanding [53,54,55,56,57,58,59].
3. Tunical lengthening procedure
The tunical lengthening procedure is a surgical method, in which a nodule/plaque or concave part of the penis is incised or excised (totally or partially), and a graft is used to cover the defect. In patients with normal erectile function, severe penile length shortening, and complex curvature/deformities or simple curvature greater than 60°, a tunical lengthening procedure may be suitable.
The ideal graft should be traction-resistant, easy to suture and manipulate, flexible, readily available, and cost-effective, and especially have a low risk of postsurgical infection; however, no graft meets all these requirements [60]. There are four main types of grafts: autograft, allograft, xenograft, and synthetic graft. However, there is no consistent evidence that any one graft type is superior to the others [61].
As for autografts, vein grafts, mainly using the saphenous vein, are commonly used. The use of buccal mucosal grafts has recently increased. Dermal grafts have been rarely used in recent years due to the risk of veno-occlusive ED [62,63]. The tunica albuginea graft is histologically most suitable. However, it should be used with caution, due to the limited size that can be obtained and potential for compromised penile support [64,65].
As for allografts, the cadaveric pericardium is commonly used. Cadaveric dura mater is no longer used due to concerns about infection risks [66].
As for xenografts, porcine small intestinal submucosa and bovine pericardium are commonly used [67]. Recently, the use of collagen fleece (TachoSil©) has become increasingly popular due to several key advantages, such as shorter surgical time, simplicity of technique, and hemostatic effect [68,69].
As for synthetic grafts, polyester (Dacron®) and polytetrafluoroethylene (Gore-Tex®) have been introduced but are not generally recommended due to the risk of infection, inflammation, and allergic reactions [70,71,72].
The tunical lengthening procedure does not actually lengthen the penis but rather extends the portion built up by the nodule/plaque to be the length of the original tunica albuginea when erect. Nevertheless, postoperative penile length shortening has been reported, with rates ranging from around 30% for saphenous veins, 23%–30% for allografts, and 13%–20% for xenografts, depending on the type of graft that covers the nodule/plaque after it is removed [8]. The cause of penile length shortening after a tunical lengthening procedure is not yet clear.
In tunical lengthening procedures, the risk of ED is reported to be 10% to 50%. The tunical lengthening procedure involves detaching and temporarily tractioning structures within the penis. Therefore, some degree of damage to the penile structures is inevitable, although direct damage to the cavernosal artery is rare. Tunical lengthening procedure may be more likely than the tunical shortening procedure to result in postoperative ED. The presence of preoperative ED, use of a graft larger than the defect, patient age >60 years, and ventral curvature are considered risk factors for postoperative ED [60].
Recurrent curvature is likely to be the result of failure to wait for the Peyronie’s disease to stabilize, reactivation of the disease, or the use of early absorbable sutures (such as Vicryl) which may lose their strength before fibrosis. Therefore, the use of non-absorbable sutures or delayed absorbable sutures (such as polydioxanone) is recommended after the disease is sufficiently stabilized. If non-absorbable sutures are used, the knots should be buried to avoid irritation of the penile skin. The use of delayed absorbable sutures may reduce the likelihood of this occurring [73].
Changes in penile sensation are associated with damage to the neurovascular bundle, the degree of dissection required to remove the nodule/plaque, and postoperative inflammation and fibrosis at the implantation site. Decreased penile sensation is reported in up to 25% of cases, although most studies report the rate of ≤5% [61].
4. Penile prosthesis insertion
PPI is a priority consideration in cases of concomitant ED not responding to any medical therapy. For mild to moderate curvature, satisfactory results can be expected with a PPI alone [9]. Inflatable prostheses are more commonly used than malleable prostheses, because the use of them may induce a more natural appearance of penis and be easier to correct for curvature.
If the degree of curvature is mild (<30°) after implantation, no further treatment is required, as the prosthesis itself can act as an internal expander over the next 6 to 9 months to correct remained curvature. For moderate to severe curvature (>30°), additional manual modeling of the penis can be required. Nevertheless, if the correction is still inadequate, a nodule/plaque incision or tunical lengthening procedure may be considered [74,75].
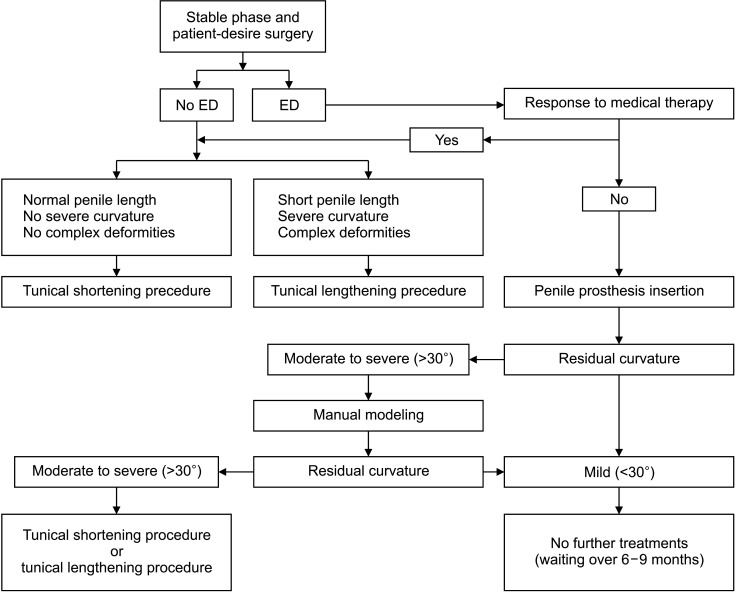
5. Summary and recommendations
Surgery for Peyronie’s disease aims to directly correct penile curvature, and allow penile penetration into the vagina during intercourse. It provides fast, reliable, and sustained results if the indication for surgery and surgery type are well chosen (Fig. 2). Surgical procedures broadly include tunical shortening procedure, tunical lengthening procedure, and PPI. The selection of the detailed surgical method is based on preoperative assessments of penile length, degree of penile deformity including curvature, and erectile function, as well as physician/patient’s preference. For simple and mild deformities, a tunical shortening procedure may be considered first. For complex/severe deformities or severe penile length shortening, a tunical lengthening procedure may be a viable option. For cases of concomitant ED not responding to any ED treatment, PPI should be considered.
Fig. 2. Algorithm of surgical treatments for Peyronie’s disease. ED: erectile dysfunction.
Acknowledgements
The members of the committee are as follows: Won Ki Lee (Department of Urology, Hallym University College of Medicine, Chuncheon, Korea), Hak Min Lee (Department of Urology, Seoul National University College of Medicine, Seoul, Korea), Dae Soon Son (Data Science School, Hallym University, Chuncheon, Korea), Hee Jo Yang (Department of Urology, Soonchunhyang University College of Medicine, Cheonan, Korea), Dong Sup Lee (Department of Urology, Catholic University College of Medicine, Seoul, Korea), Young Hoon Lee (Department of Urology, Yonsei Cham Urology Clinic, Goyang, Korea), Won Cheol Lee (Department of Urology, Hallym University College of Medicine, Chuncheon, Korea), Jun Ho Lee (Department of Urology, Eulji University College of Medicine, Daejeon, Korea), and Ui Hyun Im (Dasom Sexual Psychology Research Institute, Jeonju, Korea).
Footnotes
Conflict of Interest: The authors have nothing to disclose.
Funding: None.
- Conceptualization: SHS, WKL.
- Data curation: DSK, HJY, HCJ, WKL.
- Formal analysis: DSK, HJY, HCJ, WKL.
- Investigation: DSK, HJY, HCJ, WKL.
- Methodology: KHM, DSL, SHS, WKL.
- Project administration: WKL.
- Supervision: KHM, DSL, WKL.
- Writing – original draft: DSK, HJY, HCJ.
- Writing – review & editing: DSK, HJY, HCJ, WKL.
References
- 1.Nehra A, Alterowitz R, Culkin DJ, Faraday MM, Hakim LS, Heidelbaugh JJ, et al. American Urological Association Education and Research, Inc. Peyronie’s disease: AUA Guideline. J Urol. 2015;194:745–753. doi: 10.1016/j.juro.2015.05.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mulhall JP, Schiff J, Guhring P. An analysis of the natural history of Peyronie's disease. J Urol. 2006;175:2115–2118. doi: 10.1016/S0022-5347(06)00270-9. discussion 8. [DOI] [PubMed] [Google Scholar]
- 3.Grasso M, Lania C, Blanco S, Limonta G. The natural history of Peyronie's disease. Arch Esp Urol. 2007;60:326–331. doi: 10.4321/s0004-06142007000300021. [DOI] [PubMed] [Google Scholar]
- 4.Berookhim BM, Choi J, Alex B, Mulhall JP. Deformity stabilization and improvement in men with untreated Peyronie's disease. BJU Int. 2014;113:133–136. doi: 10.1111/bju.12346. [DOI] [PubMed] [Google Scholar]
- 5.Lindsay MB, Schain DM, Grambsch P, Benson RC, Beard CM, Kurland LT. The incidence of Peyronie's disease in Rochester, Minnesota, 1950 through 1984. J Urol. 1991;146:1007–1009. doi: 10.1016/s0022-5347(17)37988-0. [DOI] [PubMed] [Google Scholar]
- 6.Tefekli A, Kandirali E, Erol H, Alp T, Köksal T, Kadioğlu A. Peyronie's disease in men under age 40: characteristics and outcome. Int J Impot Res. 2001;13:18–23. doi: 10.1038/sj.ijir.3900635. [DOI] [PubMed] [Google Scholar]
- 7.Bella AJ, Lee JC, Grober ED, Carrier S, Benard F, Brock GB. 2018 Canadian Urological Association guideline for Peyronie's disease and congenital penile curvature. Can Urol Assoc J. 2018;12:E197–E209. doi: 10.5489/cuaj.5255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salonia A, Bettocchi C, Boeri L, Capogrosso P, Carvalho J, Cilesiz NC, et al. EAU Working Group on Male Sexual and Reproductive Health. European Association of Urology Guidelines on sexual and reproductive health-2021 update: male sexual dysfunction. Eur Urol. 2021;80:333–357. doi: 10.1016/j.eururo.2021.06.007. [DOI] [PubMed] [Google Scholar]
- 9.Chung E, Ralph D, Kagioglu A, Garaffa G, Shamsodini A, Bivalacqua T, et al. Evidence-based management guidelines on Peyronie's disease. J Sex Med. 2016;13:905–923. doi: 10.1016/j.jsxm.2016.04.062. [DOI] [PubMed] [Google Scholar]
- 10.Somers KD, Dawson DM. Fibrin deposition in Peyronie's disease plaque. J Urol. 1997;157:311–315. [PubMed] [Google Scholar]
- 11.Mulhall JP. Expanding the paradigm for plaque development in Peyronie's disease. Int J Impot Res. 2003;15(Suppl 5):S93–102. doi: 10.1038/sj.ijir.3901082. [DOI] [PubMed] [Google Scholar]
- 12.Mitsui Y, Yamabe F, Hori S, Uetani M, Kobayashi H, Nagao K, et al. Molecular mechanisms and risk factors related to the pathogenesis of Peyronie's disease. Int J Mol Sci. 2023;24:10133. doi: 10.3390/ijms241210133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.El-Sakka AI. Prevalence of Peyronie's disease among patients with erectile dysfunction. Eur Urol. 2006;49:564–569. doi: 10.1016/j.eururo.2005.10.026. [DOI] [PubMed] [Google Scholar]
- 14.Arafa M, Eid H, El-Badry A, Ezz-Eldine K, Shamloul R. The prevalence of Peyronie's disease in diabetic patients with erectile dysfunction. Int J Impot Res. 2007;19:213–217. doi: 10.1038/sj.ijir.3901518. [DOI] [PubMed] [Google Scholar]
- 15.Shindel AW, Sweet G, Thieu W, Durbin-Johnson B, Rothschild J, Szabo R. Prevalence of Peyronie's disease-like symptoms in men presenting with dupuytren contractures. Sex Med. 2017;5:e135–e141. doi: 10.1016/j.esxm.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sommer F, Schwarzer U, Wassmer G, Bloch W, Braun M, Klotz T, et al. Epidemiology of Peyronie's disease. Int J Impot Res. 2002;14:379–383. doi: 10.1038/sj.ijir.3900863. [DOI] [PubMed] [Google Scholar]
- 17.Rhoden EL, Riedner CE, Fuchs SC, Ribeiro EP, Halmenschlager G. A cross-sectional study for the analysis of clinical, sexual and laboratory conditions associated to Peyronie's disease. J Sex Med. 2010;7(4 Pt 1):1529–1537. doi: 10.1111/j.1743-6109.2009.01584.x. [DOI] [PubMed] [Google Scholar]
- 18.Mitsui Y, Kobayashi H, Yamabe F, Nakajima K, Nagao K. ABO blood type and risk of Peyronie's disease in Japanese males. World J Mens Health. 2022;40:509–516. doi: 10.5534/wjmh.210126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levine LA, Greenfield JM. Establishing a standardized evaluation of the man with Peyronie's disease. Int J Impot Res. 2003;15(Suppl 5):S103–S112. doi: 10.1038/sj.ijir.3901083. [DOI] [PubMed] [Google Scholar]
- 20.Hellstrom WJ, Feldman R, Rosen RC, Smith T, Kaufman G, Tursi J. Bother and distress associated with Peyronie's disease: validation of the Peyronie's disease questionnaire. J Urol. 2013;190:627–634. doi: 10.1016/j.juro.2013.01.090. [DOI] [PubMed] [Google Scholar]
- 21.Habous M, Muir G, Soliman T, Farag M, Williamson B, Binsaleh S, et al. Outcomes of variation in technique and variation in accuracy of measurement in penile length measurement. Int J Impot Res. 2018;30:21–26. doi: 10.1038/s41443-017-0013-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCauley JF, Dean RC. Diagnostic utility of penile ultrasound in Peyronie's disease. World J Urol. 2020;38:263–268. doi: 10.1007/s00345-019-02928-y. [DOI] [PubMed] [Google Scholar]
- 23.Spirito L, Manfredi C, La Rocca R, Napolitano L, Di Girolamo A, Capece M, et al. Daily low-dose tadalafil may reduce the penile curvature progression rate in patients with acute Peyronie's disease: a retrospective comparative analysis. Int J Impot Res. 2024;36:129–134. doi: 10.1038/s41443-022-00651-8. [DOI] [PubMed] [Google Scholar]
- 24.Gelbard M, Lipshultz LI, Tursi J, Smith T, Kaufman G, Levine LA. Phase 2b study of the clinical efficacy and safety of collagenase Clostridium histolyticum in patients with Peyronie disease. J Urol. 2012;187:2268–2274. doi: 10.1016/j.juro.2012.01.032. [DOI] [PubMed] [Google Scholar]
- 25.Gelbard M, Hellstrom WJ, McMahon CG, Levine LA, Smith T, Tursi J, et al. Baseline characteristics from an ongoing phase 3 study of collagenase Clostridium histolyticum in patients with Peyronie's disease. J Sex Med. 2013;10:2822–2831. doi: 10.1111/jsm.12312. [DOI] [PubMed] [Google Scholar]
- 26.Zhang F, Xiong Y, Wang W, Wu C, Qin F, Yuan J. The efficacy and safety of intralesional injection of collagenase Clostridium histolyticum for Peyronie's disease: a meta-analysis of published prospective studies. Front Pharmacol. 2022;13:973394. doi: 10.3389/fphar.2022.973394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roth M, Eickelberg O, Kohler E, Erne P, Block LH. Ca2+ channel blockers modulate metabolism of collagens within the extracellular matrix. Proc Natl Acad Sci U S A. 1996;93:5478–5482. doi: 10.1073/pnas.93.11.5478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mulhall JP, Anderson MS, Lubrano T, Shankey TV. Peyronie's disease cell culture models: phenotypic, genotypic and functional analyses. Int J Impot Res. 2002;14:397–405. doi: 10.1038/sj.ijir.3900874. [DOI] [PubMed] [Google Scholar]
- 29.Duncan MR, Berman B, Nseyo UO. Regulation of the proliferation and biosynthetic activities of cultured human Peyronie's disease fibroblasts by interferons-alpha, -beta and -gamma. Scand J Urol Nephrol. 1991;25:89–94. doi: 10.3109/00365599109024539. [DOI] [PubMed] [Google Scholar]
- 30.Kendirci M, Usta MF, Matern RV, Nowfar S, Sikka SC, Hellstrom WJ. The impact of intralesional interferon alpha-2b injection therapy on penile hemodynamics in men with Peyronie's disease. J Sex Med. 2005;2:709–715. doi: 10.1111/j.1743-6109.2005.00110.x. [DOI] [PubMed] [Google Scholar]
- 31.Hellstrom WJ, Kendirci M, Matern R, Cockerham Y, Myers L, Sikka SC, et al. Single-blind, multicenter, placebo controlled, parallel study to assess the safety and efficacy of intralesional interferon alpha-2B for minimally invasive treatment for Peyronie's disease. J Urol. 2006;176:394–398. doi: 10.1016/S0022-5347(06)00517-9. [DOI] [PubMed] [Google Scholar]
- 32.Husain J, Lynn NN, Jones DK, Collins GN, O'Reilly PH. Extracorporeal shock wave therapy in the management of Peyronie's disease: initial experience. BJU Int. 2000;86:466–468. doi: 10.1046/j.1464-410x.2000.00827.x. [DOI] [PubMed] [Google Scholar]
- 33.Kim KS, Choi YS, Bae WJ, Cho HJ, Ha US, Hong SH, et al. Efficacy of low-intensity extracorporeal shock wave therapy for the treatment of chronic pelvic pain syndrome IIIb: a prospective-randomized, double-blind, placebo-controlled study. World J Mens Health. 2022;40:473–480. doi: 10.5534/wjmh.210010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chitale S, Morsey M, Swift L, Sethia K. Limited shock wave therapy vs sham treatment in men with Peyronie's disease: results of a prospective randomized controlled double-blind trial. BJU Int. 2010;106:1352–1356. doi: 10.1111/j.1464-410X.2010.09331.x. [DOI] [PubMed] [Google Scholar]
- 35.Hatzichristodoulou G, Meisner C, Gschwend JE, Stenzl A, Lahme S. Extracorporeal shock wave therapy in Peyronie's disease: results of a placebo-controlled, prospective, randomized, single-blind study. J Sex Med. 2013;10:2815–2821. doi: 10.1111/jsm.12275. [DOI] [PubMed] [Google Scholar]
- 36.Moncada I, Krishnappa P, Romero J, Torremade J, Fraile A, Martinez-Salamanca JI, et al. Penile traction therapy with the new device 'Penimaster PRO' is effective and safe in the stable phase of Peyronie's disease: a controlled multicentre study. BJU Int. 2019;123:694–702. doi: 10.1111/bju.14602. [DOI] [PubMed] [Google Scholar]
- 37.Joseph J, Ziegelmann MJ, Alom M, Savage J, Köhler TS, Trost L. Outcomes of RestoreX Penile traction therapy in men with Peyronie's disease: results from open label and follow-up phases. J Sex Med. 2020;17:2462–2471. doi: 10.1016/j.jsxm.2020.10.003. [DOI] [PubMed] [Google Scholar]
- 38.Manka MG, White LA, Yafi FA, Mulhall JP, Levine LA, Ziegelmann MJ. Comparing and contrasting Peyronie's disease guidelines: points of consensus and deviation. J Sex Med. 2021;18:363–375. doi: 10.1016/j.jsxm.2020.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee HY, Pyun JH, Shim SR, Kim JH. Medical Treatment for Peyronie's disease: systematic review and network Bayesian meta-analysis. World J Mens Health. 2024;42:133–147. doi: 10.5534/wjmh.230016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kadioglu A, Küçükdurmaz F, Sanli O. Current status of the surgical management of Peyronie's disease. Nat Rev Urol. 2011;8:95–106. doi: 10.1038/nrurol.2010.233. [DOI] [PubMed] [Google Scholar]
- 41.Kendirci M, Hellstrom WJ. Critical analysis of surgery for Peyronie's disease. Curr Opin Urol. 2004;14:381–388. doi: 10.1097/00042307-200411000-00015. [DOI] [PubMed] [Google Scholar]
- 42.Levine LA, Burnett AL. Standard operating procedures for Peyronie's disease. J Sex Med. 2013;10:230–244. doi: 10.1111/j.1743-6109.2012.03003.x. [DOI] [PubMed] [Google Scholar]
- 43.Levine LA, Larsen SM. Surgery for Peyronie's disease. Asian J Androl. 2013;15:27–34. doi: 10.1038/aja.2012.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ralph D, Gonzalez-Cadavid N, Mirone V, Perovic S, Sohn M, Usta M, et al. The management of Peyronie's disease: evidence-based 2010 guidelines. J Sex Med. 2010;7:2359–2374. doi: 10.1111/j.1743-6109.2010.01850.x. [DOI] [PubMed] [Google Scholar]
- 45.Segal RL, Burnett AL. Surgical management for Peyronie's disease. World J Mens Health. 2013;31:1–11. doi: 10.5534/wjmh.2013.31.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zaid UB, Alwaal A, Zhang X, Lue TF. Surgical management of Peyronie's disease. Curr Urol Rep. 2014;15:446. doi: 10.1007/s11934-014-0446-x. [DOI] [PubMed] [Google Scholar]
- 47.Matsushita K, Stember DS, Nelson CJ, Mulhall JP. Concordance between patient and physician assessment of the magnitude of Peyronie's disease curvature. J Sex Med. 2014;11:205–210. doi: 10.1111/jsm.12337. [DOI] [PubMed] [Google Scholar]
- 48.Smith JF, Walsh TJ, Lue TF. Peyronie's disease: a critical appraisal of current diagnosis and treatment. Int J Impot Res. 2008;20:445–459. doi: 10.1038/ijir.2008.30. [DOI] [PubMed] [Google Scholar]
- 49.Taylor FL, Levine LA. Surgical correction of Peyronie's disease via tunica albuginea plication or partial plaque excision with pericardial graft: long-term follow up. J Sex Med. 2008;5:2221–2228. doi: 10.1111/j.1743-6109.2008.00941.x. discussion 9–30. [DOI] [PubMed] [Google Scholar]
- 50.Nesbit RM. Congenital curvature of the phallus: report of three cases with description of corrective operation. J Urol. 1965;93:230–232. doi: 10.1016/S0022-5347(17)63751-0. [DOI] [PubMed] [Google Scholar]
- 51.Yachia D. Modified corporoplasty for the treatment of penile curvature. J Urol. 1990;143:80–82. doi: 10.1016/s0022-5347(17)39871-3. [DOI] [PubMed] [Google Scholar]
- 52.Nooter RI, Bosch JL, Schröder FH. Peyronie's disease and congenital penile curvature: long-term results of operative treatment with the plication procedure. Br J Urol. 1994;74:497–500. doi: 10.1111/j.1464-410x.1994.tb00430.x. [DOI] [PubMed] [Google Scholar]
- 53.Sassine AM, Wespes E, Schulman CC. Modified corporoplasty for penile curvature: 10 years' experience. Urology. 1994;44:419–421. doi: 10.1016/s0090-4295(94)80106-1. [DOI] [PubMed] [Google Scholar]
- 54.Licht MR, Lewis RW. Modified Nesbit procedure for the treatment of Peyronie's disease: a comparative outcome analysis. J Urol. 1997;158:460–463. [PubMed] [Google Scholar]
- 55.Klevmark B, Andersen M, Schultz A, Talseth T. Congenital and acquired curvature of the penis treated surgically by plication of the tunica albuginea. Br J Urol. 1994;74:501–506. doi: 10.1111/j.1464-410x.1994.tb00431.x. [DOI] [PubMed] [Google Scholar]
- 56.Kümmerling S, Schubert J. Peyronie's disease. Investigation of staging, erectile failure and operative management. Int Urol Nephrol. 1995;27:629–637. doi: 10.1007/BF02564751. [DOI] [PubMed] [Google Scholar]
- 57.Thiounn N, Missirliu A, Zerbib M, Larrouy M, Dje K, Flam T, et al. Corporeal plication for surgical correction of penile curvature. Experience with 60 patients. Eur Urol. 1998;33:401–404. doi: 10.1159/000019624. [DOI] [PubMed] [Google Scholar]
- 58.Chahal R, Gogoi NK, Sundaram SK, Weston PM. Corporal plication for penile curvature caused by Peyronie's disease: the patients' perspective. BJU Int. 2001;87:352–356. doi: 10.1046/j.1464-410x.2001.00114.x. [DOI] [PubMed] [Google Scholar]
- 59.Geertsen UA, Brok KE, Andersen B, Nielsen HV. Peyronie curvature treated by plication of the penile fasciae. Br J Urol. 1996;77:733–735. doi: 10.1046/j.1464-410x.1996.97621.x. [DOI] [PubMed] [Google Scholar]
- 60.Mulhall J, Anderson M, Parker M. A surgical algorithm for men with combined Peyronie's disease and erectile dysfunction: functional and satisfaction outcomes. J Sex Med. 2005;2:132–138. doi: 10.1111/j.1743-6109.2005.20113.x. [DOI] [PubMed] [Google Scholar]
- 61.Langston JP, Carson CC., 3rd Peyronie disease: plication or grafting. Urol Clin North Am. 2011;38:207–216. doi: 10.1016/j.ucl.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 62.Devine CJ, Jr, Horton CE. Surgical treatment of Peyronie's disease with a dermal graff. J Urol. 1974;111:44–49. doi: 10.1016/s0022-5347(17)59886-9. [DOI] [PubMed] [Google Scholar]
- 63.Garcia-Gomez B, Ralph D, Levine L, Moncada-Iribarren I, Djinovic R, Albersen M, et al. Grafts for Peyronie's disease: a comprehensive review. Andrology. 2018;6:117–126. doi: 10.1111/andr.12421. [DOI] [PubMed] [Google Scholar]
- 64.Teloken C, Grazziotin T, Rhoden E, Da Ros C, Fornari A, Soares FC, et al. Penile straightening with crural graft of the corpus cavernosum. J Urol. 2000;164:107–108. [PubMed] [Google Scholar]
- 65.Da Ros CT, Graziottin TM, Ribeiro E, Averbeck MA. Long-term follow-up of penile curvature correction utilizing autologous albugineal crural graft. Int Braz J Urol. 2012;38:242–247. doi: 10.1590/s1677-55382012000200013. discussion 8–9. [DOI] [PubMed] [Google Scholar]
- 66.Collins JP. Experience with lyophilized human dura for treatment of Peyronie disease. Urology. 1988;31:379–381. doi: 10.1016/0090-4295(88)90728-5. [DOI] [PubMed] [Google Scholar]
- 67.Voytik-Harbin SL, Brightman AO, Kraine MR, Waisner B, Badylak SF. Identification of extractable growth factors from small intestinal submucosa. J Cell Biochem. 1997;67:478–491. [PubMed] [Google Scholar]
- 68.Hatzichristodoulou G, Gschwend JE, Lahme S. Surgical therapy of Peyronie's disease by partial plaque excision and grafting with collagen fleece: feasibility study of a new technique. Int J Impot Res. 2013;25:183–187. doi: 10.1038/ijir.2013.7. [DOI] [PubMed] [Google Scholar]
- 69.Lahme S, Götz T, Bichler KH. Collagen fleece for defect coverage following plaque excision in patients with Peyronie's disease. Eur Urol. 2002;41:401–405. doi: 10.1016/s0302-2838(02)00024-6. [DOI] [PubMed] [Google Scholar]
- 70.Schiffman ZJ, Gursel EO, Laor E. Use of Dacron patch graft in Peyronie disease. Urology. 1985;25:38–40. doi: 10.1016/0090-4295(85)90560-6. [DOI] [PubMed] [Google Scholar]
- 71.Faerber GJ, Konnak JW. Results of combined Nesbit penile plication with plaque incision and placement of Dacron patch in patients with severe Peyronie's disease. J Urol. 1993;149(5 Pt 2):1319–1320. doi: 10.1016/s0022-5347(17)36381-4. [DOI] [PubMed] [Google Scholar]
- 72.Ganabathi K, Dmochowski R, Zimmern PE, Leach GE. Peyronie's disease: surgical treatment based on penile rigidity. J Urol. 1995;153(3 Pt 1):662–666. [PubMed] [Google Scholar]
- 73.Ralph DJ, al-Akraa M, Pryor JP. The Nesbit operation for Peyronie's disease: 16-year experience. J Urol. 1995;154:1362–1363. [PubMed] [Google Scholar]
- 74.Wilson SK, Delk JR., 2nd A new treatment for Peyronie's disease: modeling the penis over an inflatable penile prosthesis. J Urol. 1994;152:1121–1123. doi: 10.1016/s0022-5347(17)32519-3. [DOI] [PubMed] [Google Scholar]
- 75.Wilson SK. Surgical techniques: modeling technique for penile curvature. J Sex Med. 2007;4:231–234. doi: 10.1111/j.1743-6109.2007.00407.x. [DOI] [PubMed] [Google Scholar]