Abstract
This document determines the causes of mortality (2008–2022) and calculate per capita health expenditure (2013–2021) in octogenarians, nonagenarians and centenarians in the Colombian population, considering year, gender and age group. For this nationwide retrospective descriptive observational study, epidemiological regions, urban/rural areas and morbidities were also studied. A mean of 75,552 deaths was observed from 2008 to 2022. Deaths were higher due to ischemic heart disease, COVID-19, chronic obstructive pulmonary disease, cancer, and cerebrovascular diseases in the oldest old Colombian population with urban areas having higher mortality rates than rural areas (an average of 948 (min: 847, max: 1207) against 630 (min: 558, max: 789) per 10,000 people, respectively). Conditions of cerebrovascular diseases, cancer, influenza pneumonia and chronic obstructive pulmonary disease were the most expensive in health care, summing above 5000 purchasing power parity USD on average (min: 2234, max: 7539). These conditions, along with hypertension and diabetes mellitus, were the most frequently recorded. COVID-19 incurred higher health expenditure in rural areas compared to urban areas (1090 vs. 519 purchasing power parity USD respectively). High prevalence (14·3%) and medical attention (16·8 health care utilisations per capita) were shown for organic mental disorders. Our analysis found that centenarians survived COVID-19 more than octogenarians and nonagenarians, with several hypotheses attributing this to their immune profiles. We found high expenditure on HIV/AIDS among older males suggesting the need for further study on sexually transmitted diseases prevention in this population. Lastly, Alzheimer’s disease, particularly in rural areas, had substantial expenditure. Therefore, neurodegenerative diseases and the impact of stressful events on mental health must be priorities for the health system to ensure adequate resource management.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-84150-4.
Keywords: Centenarians, Colombia, Health care spending, Longevity, Mortality, Nonagenarians, Octogenarians
Subject terms: Statistics, Diseases, Health care
Introduction
The increase in life expectancy is one of the remarkable achievements of the last century. From 1950 to 2021, global life expectancy at birth increased by 22·7 years, rising from 49·0 years to 71·7 years1. With increased life expectancy, health care professionals and policymakers need to comprehend health care spending trends and mortality causes among older adults to allocate resources effectively and improve their quality of life. Therefore, this study is especially important from both socioeconomic and health perspectives, particularly in low- and middle-income countries, where a more rapid increase among those aged above 60 years has been observed2. Unfortunately, old age is perceived by many as a life stage with little societal participation due to disease burden and disability, a phenomenon known as ageism. The United Nations has designated 2021–2030 as the Decade of Healthy Aging, defined as “the process of developing and maintaining the functional ability that enables well-being in old age”2,3.
Several studies around the world, mainly in Asia, Europe, and North America, have investigated the causes of death among the elderly, including centenarians and supercentenarians. The results are heterogeneous, but it has been observed that poorly defined causes are increasing, as well as senility as a cause of death4,5. It is assumed that aging implies higher health spending, but, to date, there is insufficient evidence to demonstrate this association. Several authors suggest that age is not the main factor associated with higher spending; other factors such as health conditions, disability, and proximity to death, could be more significant6.
Some studies have even shown that health spending could decrease with aging, which implies the importance of studying the older adult population by subgroups due to their diversity7,8. The authors believe this is because older adults are healthier, and very old adults generally do not undergo extensive invasive treatments for a multitude of reasons9. However, in most studies, proximity to death is a more crucial factor than age per se in determining health spending.
In Colombia, there is limited literature on the subject; a higher prevalence of cardiovascular and metabolic diseases has been reported in the largest cohort of centenarians described so far, where a relatively healthy morbidity profile was observed in comparison with younger older adults10. The studies carried out have focused on clinical and sociodemographic characterisation; there is insufficiently robust data on quality of life, factors associated with aging, causes of death or health care spending10.
To our knowledge, this research is the first to study the elderly population in Colombia, stratifying by decades regarding health spending and mortality causes. In this context, we aimed to: (i) describe the mortality causes in individuals aged 80 years and older in Colombia, to better characterise the health conditions that impact healthy aging; (ii) study older adults stratified by age decades (octogenarians, nonagenarians and centenarians), given population heterogeneity and disease diversity; (iii) calculate health spending per capita by age groups, gender, health conditions and geographical location, that will serve as a key input in the formulation of policies for prioritisation, accountability and financial sustainability.
Methods
The National Administrative Department of Statistics (DANE – acronym in Spanish) provides sociodemographic, economic, cultural, and other relevant statistics for Colombia. From this data repository, we extracted the number of deaths from the Vital Statistics database based on death certificates completed by authorised health personnel for the 2008–2022 period (population from the entire country). Additionally, population projections from 2018 National Population and Housing Census were used to calculate mortality rates.
To estimate health spending, we utilised the Demand Management (GD – acronym in Spanish) database for the period 2013–2021. GD, which is hosted in the information systems of the Colombian Ministry of Health and Social Protection (MHSP), registers the expenditure for health services financed by the Capitation Payment Unit (CPU, i.e. a commercial premium) that health insurance companies of the contributory scheme receive for each member from the national government. MHSP holds the data and conducts validation procedures. The perspective was the health system view, and a direct cost analysis (based on CPU expenditures) was performed.
The database accounts for several variables from which we select gender, age, place of residence, and diagnosis code (according to International Classification of Diseases 10th Revision - ICD-10). For comparison across the years, monetary amounts were converted into purchasing power parity (PPP) United States dollars (USD) at 2017 prices using the index calculated by the World Bank11.
Cause of mortality analysis focused on twenty-one causes following the guidelines on health statistics by the Organization for Economic Cooperation and Development (OECD) (Table S1 appendix p. 1) and was related to death records by primary cause of death. Further analyses were conducted using two broad geographical aggregations: urban/rural areas and epidemiological regions. Urban and rural classification followed the guidelines of the National Planning Department of Colombia12, where rural area refers to municipalities (political-administrative geographical division of Colombia) with a population density of less than 100 inhabitants per square kilometre. Epidemiological regions were defined according to the country’s Public Health Plan13.
The analysis comprised descriptive analysis and statistical visualisations of mortality rates for octogenarians, nonagenarians, and centenarians (covering the entire country), along with their interaction with the health system under the contributory scheme in terms of frequency of use of health and expenditure. Data analysis was conducted using the R software version 4.3.2.
Results
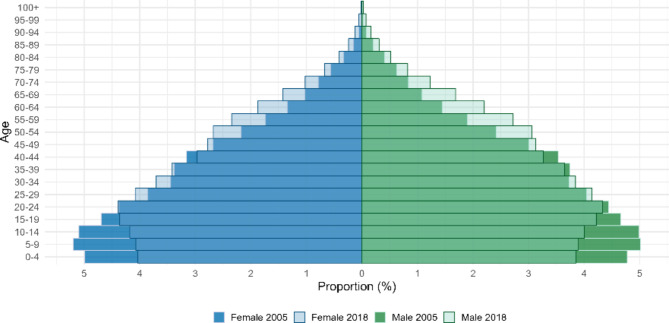
Colombia demographics are transitioning, as evidenced by the population pyramid in Fig. 1, which depicts lower birth rates and a rapid aging population from the 2005 to 2018 census. Table 1 illustrates the increasing proportion of the older adults over the years, with approximately 160 octogenarians, 38 nonagenarians, and 4 centenarians per 10,000 people in 2022. Prevalence rates for geographic political-administrative divisions are shown in Figure S1 (appendix p. 18).
Fig. 1.
Population pyramid of Colombia according to 2005 and 2018 Census.
Table 1.
Prevalence and number of octogenarians, nonagenarians, and centenarians in Colombia, 2012–2022.
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Prevalence (x10,000) | |||||||||||
| 80–89 | 137·0 | 139·5 | 141·5 | 143·1 | 144·8 | 146·4 | 148·3 | 150·8 | 155·7 | 157·9 | 160·3 |
| 90–99 | 28·5 | 30·6 | 32·9 | 35·2 | 37·3 | 39·2 | 41·5 | 41·4 | 41·0 | 39·7 | 38·4 |
| ≥ 100 | 2·3 | 2·5 | 2·7 | 2·9 | 3·2 | 3·6 | 4·5 | 4·6 | 4·7 | 4·4 | 4·0 |
| Number of people | |||||||||||
| 80–89 | 616,618 | 633,639 | 648,825 | 662,870 | 678,248 | 694,263 | 715,702 | 745,085 | 785,056 | 806,993 | 828,523 |
| 90–99 | 128,421 | 139,193 | 150,797 | 162,801 | 174,614 | 185,712 | 200,368 | 204,295 | 206,743 | 202,826 | 198,578 |
| ≥ 100 | 10,307 | 11,209 | 12,264 | 13,500 | 15,059 | 17,232 | 21,744 | 22,613 | 23,866 | 22,488 | 20,823 |
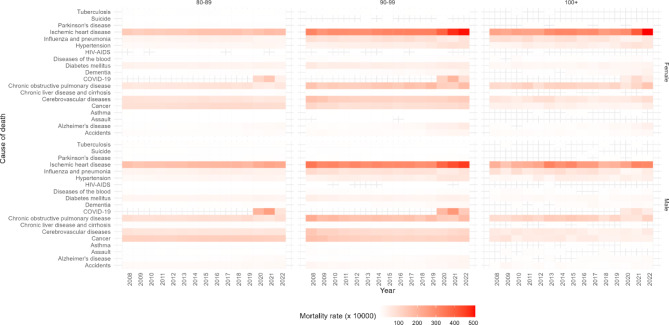
Heatmaps for mortality rates by gender and cause of death for 2008–2022 period are presented in Fig. 2. Ischemic heart disease on average represents the highest mortality rate for both genders, with nonagenarians at 335 deaths per 10,000 people, centenarians at 274 deaths per 10,000 people and octogenarians at 169 deaths per 10,000 people. The COVID-19 pandemic also explains high mortality rates with a mean of 146 deaths per 10,000 people for males and 99 deaths per 10,000 people for females. Chronic obstructive pulmonary disease, cancer, and cerebrovascular diseases have mean mortality rates exceeding 66 deaths per 10,000 people. The lowest rates are found for asthma, assault, suicide and HIV-AIDS.
Fig. 2.
Mortality rates by gender and health conditions in octogenarians, nonagenarians and centenarians in Colombia, 2008–2022.
Figure S2 (appendix p. 19) presents the disaggregation by urban and rural areas, where population projections are aggregated for those aged 80 and older, given the availability of information, and Figure S3 (appendix p. 20) by epidemiological regions. The previously identified causes of death remain more prevalent, but urban areas exhibit higher rates than rural areas, on average 38 deaths per 10,000 people in urban areas compared to 26 deaths per 10,000 people in rural areas. When observing regions in Figure S3 (appendix p. 20), Bogotá-Cundinamarca and Central regions have higher rates for both genders compared to other regions, particularly among nonagenarians, although in 2015 male centenarians in the Amazon-Orinoquía experienced the highest rate for ischemic heart disease (769 deaths per 10,000 people). We highlight that suicide and HIV-AIDS are causes more associated with men than women, especially among octogenarians.
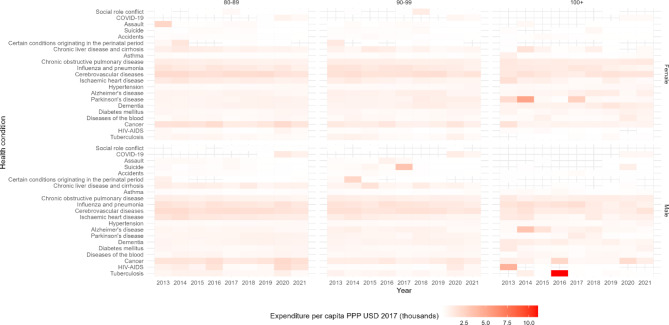
On the other hand, heatmaps demonstrating health spending per capita by gender and health conditions during the 2013–2021 period (over the years a mean of 401,958 octogenarians, 77,911 nonagenarians and 3407 centenarians) are presented in Fig. 3. The highest expenditure was for male centenarians in 2016 for tuberculosis with 11,042 PPP USD, although, on average the highest expenditure is incurred by octogenarians, both men and women, for cerebrovascular diseases with 1836 PPP USD. Cancer, influenza pneumonia and chronic obstructive pulmonary disease follow in expenditure for both genders, while ischemic heart disease (mean of 955 PPP USD) and HIV-AIDS (Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome) (mean of 667 PPP USD) have higher expenditure in men, and Parkinson’s disease (mean of 926 PPP USD) in women. The lowest expenditure is for accidents, assault, asthma and social role conflict.
Fig. 3.
Health spending per capita by gender and health conditions in octogenarians, nonagenarians and centenarians in Colombia, 2013–2021.
The disaggregation of health spending according to urban and rural areas is illustrated in Figure S4 (appendix p. 21). In general, urban areas had an average spending of 626 PPP USD per capita while rural areas had 669 PPP USD per capita. Alzheimer’s disease represents a considerable expense in rural areas, particularly among women. Also, COVID-19 incurred higher expenditure in rural areas compared to urban areas. Regarding epidemiological regions, Figure S5 (appendix p. 23) confirms substantial expenditure on COVID-19 in Amazon-Orinoquía region especially for male nonagenarians in 2020 and 2021 with an average of 24,363 PPP USD per capita. Parkinson’s disease for female centenarians in Bogotá-Cundinamarca and suicide for male centenarians in the Oriental region also accounted for more than 2700 PPP USD per capita.
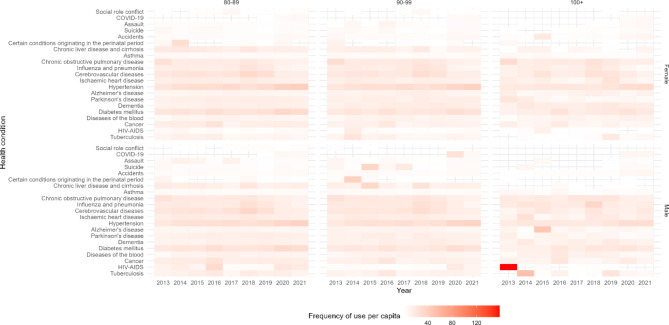
Figure 4 illustrates health care utilisation per capita with male centenarians in 2013 having the highest for HIV-AIDS with 158 health care utilisations per capita. On average during the 2013–2021 period, hypertension, diabetes mellitus, cerebrovascular diseases, chronic obstructive pulmonary disease and influenza pneumonia have over 17 health care utilisations per capita in both genders.
Fig. 4.
Frequency of use of health care services per capita by gender in octogenarians, nonagenarians and centenarians in Colombia, 2013–2021.
Examining health care utilisation per capita in urban and rural areas presents similar utilisation rates, noting a slightly higher rate in rural areas, albeit hypertension and diabetes mellitus are conditions more attended to in urban areas (Figure S6 appendix p. 24). In Figure S7 (appendix p. 26) the health care utilisation per capita for regions are illustrated, Oriental region has the highest utilisation per capita (mean of 15·1) for diagnoses of cerebrovascular diseases and influenza pneumonia. Centenarian men on average had 28·2 health care utilisations per capita in Amazon-Orinoquía also related to the previous diagnoses. On the other hand, the Caribbean region have the least health care utilisations per capita (mean of 11·5). Hypertension and diabetes mellitus are diseases with a heavier burden in the Central region (mean of 32·2 and 26 health care utilisations per capita, respectively).
It is also important to notice the disparities between health spending and causes of death. The two main health conditions with higher expenditure (cerebrovascular diseases and influenza pneumonia) are positioned by the average from 2008 to 2022 at fifth and sixth position in terms of mortality rates. Conversely, ischemic heart disease and COVID-19 despite being the primary causes of death in Colombia, do not account for substantial health expenditure. Although, some conditions such as chronic obstructive pulmonary disease and cancer rank at the top of expenditure and mortality rates, some conditions as assault, asthma and suicide are the lowest in both categories.
Additionally, from a morbidity perspective, we identified ICD-10 codes in the subgroup classification for the ten more frequent and prevalent conditions presented in Table S2 (appendix p. 2) and Table S3 (appendix p. 10), respectively. The number of health care utilisation per person ranges from 11·7 to 158 and prevalences range from 6·8% to 77·6%. Higher values are primary related to centenarians but in 2018 and 2021 the maximum frequency was observed in female octogenarians for hypertensive disease, the latter being the main prevalent condition over the years.
Similarities in morbidities were found between the previous mentioned mortality causes. Here, we can observe high prevalences of diabetes mellitus, hypertension, cerebrovascular and chronic obstructive pulmonary diseases. It is worth noting conditions not found among the mortality causes but are prevalent, such as arthropathies, dorsopathies, renal failure, diseases of oral cavity and organic mental disorders, which also incur a high number of health care utilisations. Other conditions that account for numerous utilisations include diseases of the peritoneum, liver, degenerative diseases of the nervous system, diseases of the external ear, disorders of the skin and subcutaneous tissue, and injuries in various body parts.
Discussion
The leading causes of mortality in our population were cardiovascular, COVID-19, and oncologic diseases. However, a relative increase in mortality from respiratory and infectious diseases was observed in the group of centenarians compared to nonagenarians and octogenarians. Although the results on the causes of mortality in the oldest old are heterogeneous, our findings are consistent with some researchers14,15. In our population, cerebrovascular, oncological, and respiratory diseases generated the highest health spending, in line with what is reported in OECD countries, where circulatory, digestive, musculoskeletal diseases, cancer, and mental illnesses account for almost 60% of health care spending16. In the United States, the main expenditure in the oldest old population is concentrated on cardiovascular diseases and dementia, with a marked increase in spending over the years on musculoskeletal diseases17.
When studying health spending per capita among octogenarians, nonagenarians, and centenarians, we found lower spending in the group of centenarians when compared to octogenarians and nonagenarians. These results coincide with some studies that highlight the influence of several factors on health expenditure, such as the decrease in invasive medical procedures with increasing age6,7,9. Although we did not directly examine these specific factors, our results support the idea that age alone is not a causal factor in health spending in the oldest old. Our findings emphasize the importance of investigating alternative factors related to health spending such as functional status and “what matters” to the patient, ability to understand their goals of care and wishes, for more efficient resource management in the future, rather than focusing solely on population aging.
Our study revealed disparities between health spending per capita and mortality rates according to different health conditions. This disparity is to be expected due to variations in the progression and nature of each disease. As with cancer and cardiovascular diseases, it is hoped that the high prevalence and mortality of chronic diseases will translate into high health spending18. On the other hand, there are chronic diseases, such as some neurological diseases, which, despite having a historically low mortality, can cause significant disability19.
In our population, falls had a low mortality rate and were among the diseases with the lowest health care costs. This fact is striking considering that worldwide, falls are one of the main reasons for emergency room visits, hospitalisation, and health care costs in older adults. More than one in four older people fall each year, but only one-third of those who suffer a fall seek medical care20. Falls have devastating effects on older adults, leading to negative and often permanent consequences such as compromised independence, increased morbidity, mortality, reduced overall functionality, early placement in long-term care, and heightened rates of emergency department visits and hospitalisations. These incidents are linked to a broad range of unintended physical outcomes, encompassing fractures, contusions, injuries, and other adverse effects20. Moreover, falls are the main cause of traumatic brain injuries, highlighting the risk of intracranial hematomas or haemorrhages, which showed a high mortality rate and health spending in our population. We want to highlight that, although falls were not directly shown to be associated with high expenditure or mortality, they are still clinically relevant in older adults. In addition, there may be underreporting of these events, as older adults may not specifically consult for this cause, or the baseline functional status is robust in this population resulting in better outcomes than rest of the world. Unfortunately, in this retrospective descriptive observational study we did not have information on the baseline functional status of the patients.
On the other hand, health spending for HIV/AIDS was high in our older adult population, especially among men. In contrast, the mortality rate for this disease was remarkably low. While global AIDS-related deaths have declined by more than 50% after Antiretroviral Therapy (ART) was implemented, the incidence rate of HIV/AIDS achieved only a slight decrease21. In Colombia, HIV/AIDS incidence has increased, in contrast to the global picture, while AIDS mortality has remained stable22. This is consistent with our results, with a low mortality rate but a high health spending correlating with an increasing incidence. In older adults, the incidence of HIV/AIDS is also increasing in Colombia, possibly due to late diagnosis and unprotected intercourse, caused by low knowledge of HIV/STD (sexually transmitted diseases) transmission and underestimation of risk in this population23.
The widespread belief that older people do not have sex contributes to the misconception that they are not vulnerable to STDs. However, studies indicate that sexually active older people tend to engage in high-risk sexual behaviours, rarely use condoms, and have limited knowledge of sexual health24. Our findings emphasize the need to conduct research on STDs in older adults along with the need to prioritize STD prevention programs in this group. These efforts are essential to advance UNAIDS’ goals and achieve Healthy Aging targets by 20302.
In the results by epidemiological region, the case of COVID-19 infection in the Amazonas-Orinoquia region stands out, where a significantly higher per capita expenditure was recorded compared to other regions. This could be explained by the insufficient supply of medical services and the lack of health professionals in the region25, which probably led to non-prioritized, late and inefficient care. These deficiencies in the health system would have contributed to avoidable complications of the disease and increased morbidity, thus increasing spending. Now, in relation to the mortality of this infectious disease for the country, compared to younger age groups like nonagenarians and octogenarians, our results showed that COVID-19 mortality was relatively low among centenarians. This finding has been previously reported in the literature. In Japan, the number of centenarians increased by 12·8% between 2020 and 2022, despite a decrease in life expectancy in 2021 due to the pandemic26. This has sparked some interest, leading to the hypothesis that centenarians appear to have survived the pandemic better, possibly due to genetic factors, isolation precautions, and early vaccination. However, the resistance of centenarians to COVID-19 remains controversial, with most studies failing to confirm this association.
What has been commonly observed in some studies in Italy and Belgium is that centenarians exposed to the 1918 H1N1 influenza virus had lower mortality from COVID-19 when compared to centenarians born after that pandemic27. It is suggested that this population could have developed immune memory cells capable of recognizing epitopes antigenically related to the H1N1 virus, even a century later. However, to our knowledge, there is no definitive evidence of a cross-reaction between these two viruses. Another proposed explanation suggests that the “older” centenarians are more select and have a more efficient immune profile; nevertheless, more studies are needed to elucidate the molecular mechanisms involved27.
In addition, our findings revealed a notably high health spending for Alzheimer’s disease (AD) among centenarians, particularly pronounced in rural regions. Given that dementia is associated with advanced age, its direct costs have become a growing health spending concern in some high-income countries. Our analysis suggests that this problem may also exist in low- and middle-income countries such as Colombia, and specifically more pronounced in rural areas. Among the main causes, the literature has expressed the association of a low educational and socioeconomic level with a higher risk of AD and other dementias, due to poor cognitive reserve and the health care access barriers faced by rural population28. Furthermore, older adults in rural Colombia are at a high risk of having faced stressful events due to the armed conflict and forced displacement throughout their lives, e.g. in the Oriental region.
A growing body of research suggests that cognitive decline in old age is associated with stress factors in war zones, supported by neurobiological changes such as glucocorticoid release, neuronal death, structural damage to brain regions (hippocampus, amygdala, and prefrontal cortex) and the accumulation of beta-amyloid peptide, the latter known as an AD precursor29. Although cognitive risk factors have been studied in military veterans, there is still little literature on similar effects of wartime stress in populations in low- and middle-income countries. This gap is concerning due to the significant war survivors in these countries and the increasing burden of AD, as shown by our results30.
In Colombia, research has been conducted to analyse how highly stressful events affect the mental health of the general population and older adults, such as violence, forced displacement, and internal armed conflict31. Our findings generate the hypothesis that these events could be related to dementia and AD. Following the findings of Giebel et al. and León et al., we emphasize the need for the health system to prioritize mental health services for older people living in rural areas. Likewise, we believe that it would be valuable to study soon the financial burden on the health care system of mental illness in people over 80 years of age.
The limitations of our work are threefold: (i) the possible error in filling out the cause of death of the population. However, Colombia is considered a country with medium-high quality civil registration and vital statistics;32 (ii) for the calculation of per capita expenditure, we used only information from the contributory health system (health scheme that covers approximately 45% of the national population)33. It was not possible to consider the members of the subsidised regime because their information systems are not available to the public due to their very poor quality;25,34 (iii) the databases we had access to did not allow us to know whether the mortality occurred at home or in hospital, nor whether the person lived in a family home or in a nursing home. Consideration of these data could complement the analysis of this retrospective descriptive observational study and should be considered as a line of future research in the geriatric field in our country.
Longevity in Colombia presents a future with several challenges that must be addressed to ensure health and security for the population. Effective resource management and preparation are essential to tackle upcoming health issues such as cerebrovascular diseases, cancer, influenza pneumonia, chronic obstructive pulmonary disease, infections, sexually transmitted diseases, and neurodegenerative diseases. Furthermore, it is crucial to overcome the inequalities across different geographic areas for this population.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
Conceptualisation: OE; data curation: OE, VB; formal analysis: OE, VB, IF, SP, investigation: OE, VB, IF, methodology: OE, project administration: OE, resources: OE, software: OE, VB, supervision: OE, MD, OF, validation: OE, MD, OF; visualisation: OE, VB, writing – original draft: OE, VB, IF, SP, MD, OF, and writing – review & editing: OE, VB, IF, SP, MD, OF. OE and VB directly accessed and verified the underlying data reported in this manuscript.
Data availability
The data and programming code can be found at https://github.com/oaespinosaa/Longevity_Colombia.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Schumacher, A. et al. Global age-sex-specific mortality, life expectancy, and population estimates in 204 countries and territories and 811 subnational locations, 1950–2021, and the impact of the COVID-19 pandemic: A comprehensive demographic analysis for the global burden of. Lancet403, 1989–2056 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.United Nations. United Nations Decade of Healthy Ageing: Plan of action. World Health Organ. (2020).
- 3.Keating, N. A research framework for the United Nations Decade of Healthy Ageing (2021–2030). Eur. J. Ageing. 19, 775–787 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koyama, T. et al. Trends in places and causes of death among centenarians in Japan from 2006 to 2016. Geriatr. Gerontol. Int.22, 675–680 (2022). [DOI] [PubMed] [Google Scholar]
- 5.Meslé, F. & Vallin, J. Causes of death at very old ages, including for supercentenarians. in Exceptional Lifespans. Demographic Research Monographs (eds Maier, H., Jeune, B. & Vaupel, J.) 69–84 (Springer) (2020).
- 6.Hazra, N., Rudisill, C. & Gulliford, M. Determinants of health care costs in the senior elderly: Age, comorbidity, impairment, or proximity to death? Eur. J. Heal Econ.19, 831–842 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nakanishi, Y. et al. Comparison of Japanese centenarians’ and noncentenarians’ medical expenditures in the last year of life. JAMA Netw. Open.4, e2131884 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kocot, E., Ferrero, A., Shrestha, S. & Dubas-Jakóbczyk, K. End-of-life expenditure on health care for the older population: A scoping review. Health Econ. Rev.14, 17 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mori, H., Ishizaki, T. & Takahashi, R. Association of long-term care needs, approaching death and age with medical and long-term care expenditures in the last year of life: An analysis of insurance claims data. Geriatr. Gerontol. Int.20, 277–284 (2020). [DOI] [PubMed] [Google Scholar]
- 10.Lozada-Martinez, I. et al. Demographics and clinical characteristics of a new population of centenarians in Colombia. The COOLCEN cohort. Arch. Gerontol. Geriatr. Plus. 1, 100006 (2024). [Google Scholar]
- 11.World Bank. World Development Indicators. (2024). https://databank.worldbank.org/source/world-development-indicators
- 12.Departamento Nacional de Planeación. Definición de categorías de ruralidad (Informe temático para la Misión para la Transformación del Campo). (2014).
- 13.Ministerio de Salud y Protección Social. Plan decenal de salud pública 2012–2021: La salud en Colombia la construyes tú. (2013).
- 14.Chen, Y. et al. Where and how centenarians die? The role of hospice care. Am. J. Hosp. Palliat. Med.36, 1068–1075 (2019). [DOI] [PubMed] [Google Scholar]
- 15.Evans, C. et al. Place and cause of death in centenarians: A population-based observational study in England, 2001 to 2010. PLOS Med.11, e1001653 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The Organisation for Economic Cooperation and Development (OECD). Expenditure by Disease, Age and Gender. (2016).
- 17.Dieleman, J. et al. US Health care spending by payer and health condition, 1996–2016. JAMA323, 863–884 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luengo, R. et al. Economic burden of cardiovascular diseases in the European Union: A population-based cost study. Eur. Heart J.44, 4752–4767 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Steinmetz, J. D. et al. Global, regional, and national burden of disorders affecting the nervous system, 1990–2021: A systematic analysis for the Global Burden of Disease study 2021. Lancet Neurol.23, 344–381 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mays, A. Falls in older adults. in Geriatric Medicine 1235–1249 (Springer) (2024).
- 21.Frank, T. et al. Global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2017, and forecasts to 2030, for 195 countries and territories: A systematic analysis for the Global Burden of Diseases, injuries, and risk factors study 2017. Lancet HIV. 6, e831–e859 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Montana, J. et al. The HIV epidemic in Colombia: Spatial and temporal trends analysis. BMC Public. Health. 21, 1–14 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Piñeirúa, A. et al. The HIV care continuum in Latin America: Challenges and opportunities. Lancet Infect. Dis.15, 833–839 (2015). [DOI] [PubMed] [Google Scholar]
- 24.Gómez, D., Onofre, D., Benavides, R. & Trujillo, P. A systematic review of individual, psychological and sociocultural factors associated with safe and risky sexual behavior in older adults. Am. J. Sex. Educ.16, 415–434 (2021). [Google Scholar]
- 25.Espinosa, O. et al. Study on the concentration, distribution, and persistence of health spending for the contributory scheme in Colombia. BMC Health Serv. Res.24, 1225 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aoki, Y. The number of centenarians continues to increase during the COVID-19 pandemic in Japan. Geriatr. Gerontol. Int.23, 395–396 (2023). [DOI] [PubMed] [Google Scholar]
- 27.Caruso, C. et al. Centenarians born before 1919 are resistant to COVID-19. Aging Clin. Exp. Res.35, 217–220 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McDowell, I., Xi, G., Lindsay, J. & Tierney, M. Mapping the connections between education and dementia. J. Clin. Exp. Neuropsychol.29, 127–141 (2007). [DOI] [PubMed] [Google Scholar]
- 29.Marin, M. et al. Chronic stress, cognitive functioning and mental health. Neurobiol. Learn. Mem.96, 583–595 (2011). [DOI] [PubMed] [Google Scholar]
- 30.Dorrington, S. et al. Trauma, post-traumatic stress disorder and psychiatric disorders in a middle-income setting: prevalence and comorbidity. Br. J. Psychiatry. 205, 383–389 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Giebel, C. et al. Coping in the face of violence: a qualitative study on the impacts of stressful life events on the mental health of older adults in Colombia. Clin. Gerontol. 1–11 (2023). [DOI] [PubMed]
- 32.Phillips, D. et al. A composite metric for assessing data on mortality and causes of death: The vital statistics performance index. Popul. Health Metr.12, 14 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Administradora de los Recursos del Sistema General de Seguridad Social en Salud. Base De Datos Única De Afiliados [Data file] (2022).
- 34.Ministerio de Salud y Protección Social. Estudio de suficiencia y de los mecanismos de ajuste del riesgo para el cálculo de la Unidad de Pago por Capitación, recursos para garantizar la financiación de tecnologías y servicios de salud en los regímenes Contributivo y Subsidiado. Año 2020. (2020).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data and programming code can be found at https://github.com/oaespinosaa/Longevity_Colombia.