Abstract
Digital interventions are increasingly utilized as a lever to promote population health, yet not everyone may equally benefit from them. This umbrella review pooled the insights from available systematic and scoping reviews regarding potential social inequalities in digital intervention uptake, engagement and effectiveness, focusing on the promotion of weight-related behaviors (diet, physical activity, sedentary behavior) and weight loss (maintenance) in adults. Six databases were searched from 1970 to October 2023. Forty-six reviews were included, of which most focused on physical activity and intervention effectiveness. Age and gender/ sex differences were most frequently studied. Most reviews found digital interventions to be effective irrespective of age, while men benefitted more from digital interventions than women. Other inequality indicators (e.g., income, education) were rarely studied, despite them being potential causes of a digital divide. A more systematic and thorough exploration of inequalities in digital health is required to promote health for all.
Subject terms: Human behaviour, Health services, Public health
Introduction
Overweight and obesity continue to rise globally1 and negatively affects individual health and puts considerable strain on healthcare systems and economies2. Inducing sustainable changes to weight-related behaviors such as diet and physical activity, including sedentary behavior, are seen as both the first-line treatment for overweight and obesity as well as an important measure of primary prevention3. In the past decades, programs targeting weight-related behaviors for both health promotion and treatment were increasingly digitized4, and they can now be delivered at relatively low cost5 and, given the high penetration of internet connectivity and digital device ownership globally6, with potentially far reach.
Indeed, digital interventions are effective in promoting physical activity and healthy diets in adults7. However, research indicates that not everyone might equally benefit from these interventions8,9, because of inequalities in digital determinants of health (e.g., digital literacy, accessibility, availability, affordability)10. For example, while broadband internet access (80% of Americans and 91% of Europeans) and smartphone ownership (90% of Americans and 86% of Europeans) are nearly universal in the United States and in Europe, there are notable differences by age, household income, rurality, and educational attainment11,12. This “digital divide” might not only re-enact existing health disparities, but also widen them due to the added layer of digital technology, for which additional barriers exist for certain population subgroups13. For instance, rural residents might lack access to healthcare facilities, but also to broadband internet; thus both in-person and online weight management programs might be difficult for them to engage with14. Potential social inequalities introduced through digital technology thus should be carefully evaluated to avoid causing more harm than good, across the first (access), second (skills to use) and third (benefits) levels of the digital divide13,15.
Many factors may influence whether there is a digital health divide, including the behaviors under study, the (digital) mode of delivery, or the social inequality indicator or population focus. Generally, systematic reviews related to the digital health divide have been one of two types. Some reviews exclusively focus on one “priority” population (previously referred to as “deprived,” “vulnerable,” “underrepresented” or other potentially stigmatizing terms16), such as older adults17, while other reviews explicitly compare groups of different levels (e.g., high vs low socio-economic status8). Compared to the latter, the former does not necessarily provide evidence for or against a digital divide since it is lacking a comparator. Results of the two types of reviews thus may diverge, e.g. if reviews focusing on older adults report that digital interventions are effective in this age group18, but reviews comparing younger and older adults report that younger adults benefit more19. Subsequently, conclusions that may influence policy and practice risk being erroneous. However, the latter type of review is often not conducted with the main aim to study the digital health divide but may report on it in heterogeneity assessments or sensitivity analyses, which makes the results more difficult to assess.
Thus, the objective of the present umbrella review was to pool insights from available systematic and scoping reviews with and without meta-analysis in order to understand potential social inequalities in the effectiveness of digital interventions for weight-related behaviors in adults. It also included reviews that focused on intervention uptake and engagement, since these are necessary prerequisites for intervention effectiveness20. Social inequality indicators under study were derived from the Cochrane PROGRESS-Plus framework21; by including a broad range of social inequality indicators the present umbrella review also provides insights regarding potential evidence gaps. Finally, it included both main types of reviews– that is, those that focus exclusively on priority populations and reviews contrasting different levels of these indicators to investigate whether conclusions align.
Results
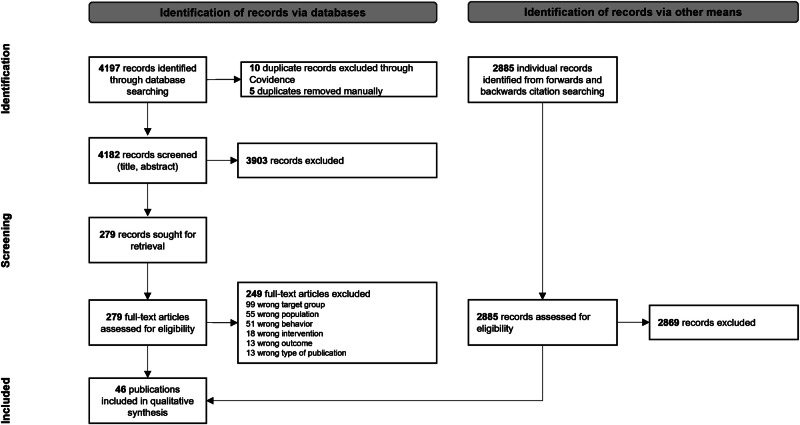
A total of 4197 studies were uploaded into Covidence, of which 15 were duplicates identified by the software. Out of the 4182 records initially screened, 3903 were deemed irrelevant after title and abstract screening. For the remaining 279 records, full-texts were retrieved; 247 were excluded (see Fig. 1 for a summary of reasons and the OSF repository for the reason per record). In addition to the 30 records identified through the database search, another 16 reviews were identified through handsearching. A total of 46 reviews were included; these reviews were published between 2012 and 2024.
Fig. 1. PRISMA flow diagram illustrating the screening process.
The diagram illustrates the selection process of reviews included in this umbrella review, from initial identification through final inclusion.
Characteristics of the included reviews
An overview of all included reviews is presented in Table 1. Most included reviews were systematic reviews with17–19,22–49 or without9,50–58 meta-analysis. The majority of included reviews (k = 26; with k representing the number of reviews) focused on health promotion without restrictions regarding the study population’s weight status9,17–19,23–26,33,34,36,37,39,40,42,43,46,49,50,54,55,57–61; 10 reviews each focused specifically on overweight of obese individuals27,38,41,56 and patients22,28,29,35,44,45,47,48,62,63, respectively. Twenty-two reviews focused exclusively on priority populations such as older adults (k = 13)17,18,25,34,40,43,49,50,63, women (k = 4)37,42,46,54, men (k = 1)33, racial and ethnic minorities (k = 3)51,53,54, and individuals with low income (k = 1)52 or low socio-economic status (k = 1)56. Another 22 reviews contrasted at least two levels for a range of social inequality indicators; 11 addressed disparities for genders/ sexes9,31,35,36,41,47,61,62, 20 for age groups9,19,23,35,36,38,39,41,44,45,47,48,55,61,62, 2 for races/ ethnicities9,62, 2 for levels of education9,61, 1 for income groups9, 1 for occupation/ employment9, and 4 for locations9,22,38,55. The remaining 2 reviews included both analyses of only a priority group (i.e., women24; sedentary older adults29) and a comparative analysis (i.e. younger vs older adults24; women vs men29).
Table 1.
Characteristics of included reviews
| First author and year | Type of review | Focus | Context | Number of studies | Number of participants | Outcome(s) | Target behavior(s) | Inequality indicator(s) | Digital intervention(s) |
|---|---|---|---|---|---|---|---|---|---|
| Arambepola 201622 | systematic review and meta-analysis | priority vs not priority | patients | 19 | 1155 | effectiveness | diet, physical activity, weight | location | text messages |
| Aslam 202057 | systematic review | only priority | health promotion | 10 | 383 | effectiveness | physical activity | age | smartphone apps; text messages; pedometers; smartwatches; wearables |
| Baer 202250 | systematic review | only priority | health promotion | 7 | 7655 | engagement | diet, physical activity | age | smartphone apps |
| Bennett 201451 | systematic review | only priority | overweight/ obesity | 6 | 4899 | effectiveness | weight | race/ ethnicity | computer, web, text, mobile phone, applications, email or related technologies. |
| Cavero-Redondo 202023 | systematic review and meta-analysis | priority vs not priority | health promotion | 20 | 2196 | effectiveness | weight | age | mHealth (web, PDA, smartphone) |
| Clark 202352 | systematic review | only priority | overweight/ obesity | 9 | 1606 | effectiveness | weight | income | computer, web, text message, telephone/mobile phone (including mobile applications), email, or related technologies |
| Cotie 201824 | systematic review and meta-analysis | both | health promotion | 60 | 8354 | effectiveness | physical activity, weight | age, gender/ sex | wearable healthand movement trackers; websites; smartphone applications; messaging services (i.e. text messaging, emails and voicemail); videogames or tele-health |
| D’Amore 202225 | systematic review and meta-analysis | only priority | health promotion | 18 | 3455 | effectiveness | physical activity | age | smart technology |
| Davies 201226 | systematic review and meta-analysis | priority vs not priority | health promotion | 34 | 11885 | effectiveness | physical activity | age, gender/ sex | web-based / emails |
| Dehghan Ghahfarokhi 202227 | systematic review and meta-analysis | priority vs not priority | overweight/ obesity | 26 | 2373 | effectiveness | physical activity | age, gender/ sex | wearables, smartphone apps |
| Duan 202128 | systematic review and meta-analysis | priority vs not priority | patients | 15 | not reported | effectiveness | diet, physical activity | age, gender/ sex | web sites or pages, telephone counseling, text messaging |
| Enyioha 202253 | systematic review | only priority | overweight/ obesity | 7 | 942 | effectiveness | weight | ethnicity | cellular phone calls, text messaging, web-based applications or downloadable mobile apps |
| Franssen 202029 | systematic review and meta-analysis | both | patients | 35 | 2858 | effectiveness | physical activity | age, gender/ sex | wearable activity trackers |
| Gravesande 202359 | scoping review | only priority | health promotion | 18 | 715 | engagement | physical activity | age | videoconferencing systems, DVDs, videolinks, videos streamed through websites |
| Hodkinson 202262 | individual patient data meta-analysis | priority vs not priority | patients | 9 | 1481 | effectiveness | physical activity | gender/ sex, age, ethnicity | wearable trackers |
| Jahangiry 201719 | systematic review and meta-analysis | priority vs not priority | health promotion | 22 | 30951 | effectiveness | physical activity | age | web-based interventions |
| Jahangiry 202130 | systematic review and meta-analysis | priority vs not priority | overweight/ obesity | 8 | 779 | effectiveness | weight | age | web-based interventions |
| Jonkman 201858 | systematic review | only priority | health promotion | 12 | 1208 | effectiveness | physical activity | age | used a computer, tablet, smartphone, or smartwatch |
| Joseph 201954 | systematic review | only priority | health promotion | 10 | not reported | effectiveness | physical activity | race/ ethnicity, gender/ sex | mobile phone or smartphone, social media platform, Internet-based website, e-mail, or text messaging |
| Kodama 201231 | systematic review and meta-analysis | priority vs not priority | overweight/ obesity | 23 | 8697 | effectiveness | weight | age, gender/ sex | web-based programs |
| Kwan 202018 | systematic review with meta-analysis | only priority | health promotion | 38 | 11194 | effectiveness | physical activity | age | using any forms of electronic devices, the internet, and related digital technology |
| Lau 202032 | systematic review and meta-analysis | priority vs not priority | overweight/ obesity | 15 | 5816 | effectiveness | weight | age | internet, apps, SMS, email or smartphone. |
| Lau 202441 | systematic review and meta-analysis | priority vs not priority | overweight/ obesity | 46 | 19670 | effectiveness | diet | age, gender/ sex | mobile applications (apps), websites, web-based programs, text messaging, technology-based systems, social media, wearable devices, video calls, phone calls, emails. |
| Leonard 202142 | systematic review and meta-analysis | only priority | health promotion | 21 | 6265 | effectiveness | diet, physical activity, weight | gender/ sex | websites, wearables, smartphone, digital scales |
| Liu 202017 | systematic review and meta-analysis | only priority | health promotion | 10 | 1035 | effectiveness | physical activity | age | wearable activity tracker |
| Livingstone 202355 | systematic review | priority vs not priority | health promotion | 30 | 13365 | effectiveness | diet | age, location | smartphone apps, text messages, websites, phone calls, emails |
| McMahon 202133 | systematic review and meta-analysis | only priority | health promotion | 9 | 1329 | effectiveness | weight | gender/ sex | mobile phones, computers, laptops, tablets |
| Myers-Ingram 202356 | systematic review | only priority | overweight/ obesity | 4 | 373 | effectiveness | physical activity, weight | income, education, occupation/ employment | web-based, mobile applications, text, social media or other related modalities |
| Nunez de Arenas-Arroyo 202134 | systematic review and meta-analysis | only priority | health promotion | 19 | 4937 | effectiveness | physical activity | age | websites, virtual agents, phone calls, text messages, smartphone apps, wearables |
| Oliveira 202043 | systematic review and meta-analysis | only priority | health promotion | 23 | 2766 | effectiveness | physical activity | age | wearable activity tracker |
| Patterson 202144 | systematic review and meta-analysis | priority vs not priority | patients | 19 | 1543 | effectiveness | physical activity | age | smartphone apps |
| Peng 202345 | systematic review and meta-analysis | priority vs not priority | patients | 25 | 2400 | effectiveness | physical activity | age | wearables with / without apps and web platforms |
| Qiu 201835 | systematic review and meta-analysis | priority vs not priority | patients | 15 | 1316 | effectiveness | physical activity | age, gender/ sex | step-counters |
| Rhodes 202046 | systematic review and meta-analysis | only priority | health promotion | 11 | 3280 | effectiveness | weight, physical activity | gender/ sex | digital interventions |
| Schepens Niemiec 202260 | ccoping review | only priority | health promotion | 13 | 1464 | effectiveness | physical activity | age | mobile phones, patient-monitoring devices, personal digital assistants, and other wireless devices for physical activity promotion |
| Seo 201536 | systematic review and meta-analysis | priority vs not priority | health promotion | 31 | 8442 | effectiveness | weight | age, gender/ sex | internet-based interventions |
| Sequí-Domínguez 202047 | systematic review and meta-analysis | priority vs not priority | patients | 9 | 709 | effectiveness | weight | age, gender/ sex | website, videoconferencing, smartphone apps |
| Sherifali 201737 | systematic review and meta-analysis | only priority | health promotion | 10 | 557 | effectiveness | diet, physical activity,aeight | gender/ sex | common eHealth technologicalelements such as text messaging or website support. |
| Szinay 20239 | systematic review | priority vs not priority | health promotion | 16 | 290039 | uptake, engagement, effectiveness | diet, physical activity,weight | age, education, ethnicity/ race, gender/ sex, income, location, occupation/ employment | smartphone, PDA, or wearable, without any intervention components being delivered face-to-face or using other digital tools such as computers or websites |
| Teo 202348 | systematic review and meta-analysis | priority vs not priority | patients | 17 | 293 | effectiveness | physical activity, weight | age | wearables |
| Trumpf 202363 | scoping review | only priority | patients | 17 | 827 | engagement | physical activity | age | pedometers, accelerometers, or smartphones |
| Wong 202238 | systematic review and meta-analysis | priority vs not priority | overweight/ obesity | 31 | 5361 | effectiveness | weight | Location, age | wearable devices, including accelerometers, pedometers, tailored wearable systems |
| Wu 202349 | systematic review and meta-analysis | only priority | health promotion | 45 | 7144 | effectiveness | physical activity | age | wearables |
| Yang 202261 | scoping review | priority vs not priority | health promotion | 54 | 34615 | engagement | physical activity, weight | gender/ sex, age, education | smartphones, smartwatches, PDAs, wristbands, and other wireless technologies |
| Yen 201939 | systematic review and meta-analysis | priority vs not priority | health promotion | 19 | 2292 | effectiveness | weight | age | wearable technologies |
| Yerrakalva 201940 | systematic review and meta-analysis | only priority | health promotion | 6 | 486 | effectiveness | physical activity | age | wearable trackers; smartphone apps |
The number of included studies per review ranged from 4 to 60. Total sample sizes ranged from 293 to 290039, with two reviews not reporting the sample size. Seven of the included reviews reported on outcomes related to diet9,22,28,37,41,42,55, 32 on physical activity9,17–19,22,24–29,34,35,37,40,42–46,48–50,54,56–63, and 21 on weight9,28,42,56, respectively. Most reviews studied intervention effectiveness (k = 43)9,60,62, while only one9 addressed intervention uptake and four9,59,61,63 addressed intervention engagement. Many different types of digital interventions were studied, ranging from websites, text messages and personal digital assistants (PDAs) to smartphone apps and wearable technology (see Table 1 for details).
Overlap between reviews
The 46 included systematic reviews included a total of 622 unique publications, out of which 146 were included in at least two and a maximum of nine reviews. Following Pieper et al.64, we calculated the corrected covered area (CCA) using the following formula: , with N indicating the total number of citations included in all reviews (864), r indicating the number of rows (i.e., number of included reviews, 46), and c indicating the number of columns (i.e., number of unique publications referenced). This resulted in CCA = 0.86%, which is considered a slight overlap64. The full citation matrix is provided on the project’s OSF page (https://osf.io/g4hzb/).
Quality appraisal
Based on the AMSTAR-2 assessment of the 46 reviews, 3 (6.5%) were rated as low quality, and the remaining 43 (93.5%) were rated as critically low. Quality domains that reviews scored well on included coverage of Population/Intervention/Comparison/Outcome components (k = 37), duplicate study selection (k = 40) and report of conflict of interest (k = 44), while only 6 reviews partially met the domain “a comprehensive literature search strategy”, and 3 studies met the domain “reporting of funding sources in included studies”. Individual study quality assessments for each AMSTAR-2 item are displayed in Supplementary Fig. 1.
Reviews focusing on priority populations
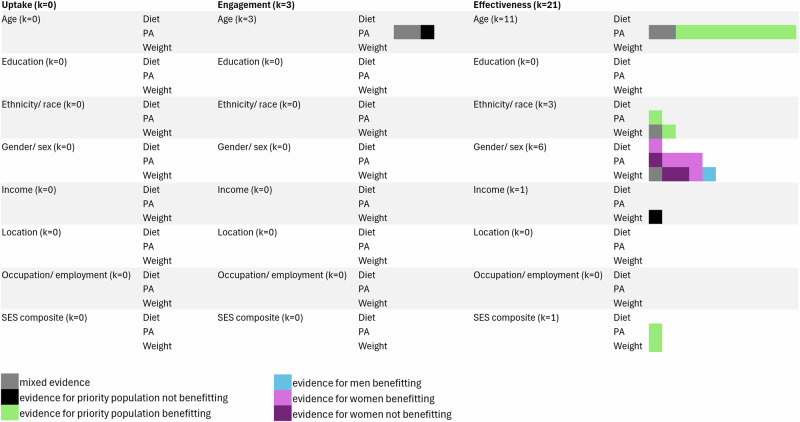
Results are visually summarized in Fig. 2.
Fig. 2. Visual summary of results for reviews focusing on priority populations.
Each box represents one finding from one review. Results are split by the respective focus on uptake, engagement, of effectiveness; outcome of interest (diet, physical activity, weight); and social inequality indicator studied. Legend: Gray box = mixed evidence; black box = evidence for priority population not benefitting; green box = evidence for priority population benefitting; blue box = evidence for men benefitting; light purple box = evidence for women benefitting; dark purle box = evidence for women not benefitting.
Uptake was not studied specifically in relation to priority populations in any of the included reviews. Engagement of priority populations with digital interventions for physical activity was reported in three of the included reviews50,59,63. Baer et al.50 reported low usage frequencies in middle-aged and older adults. Gravesande et al.59 reported adherence rates of, on average 75.5%, in adults aged 55 years and older, although adherence varied substantially from 16.7 to 100%. Finally, Trumpf et al.63 reported that participants aged 60 years and older wore the physical activity monitoring devices used in the included interventions, on average, on 87% of days; wear time ranged from 57% to 99% of days.
Eleven reviews focused specifically on effectiveness of digital interventions for physical activity promotion in older adults (typically from the ages of 55 or 60)17,18,25,29,34,40,43,49,57,58,60. Reviews consistently reported that most included interventions were effective in older adults when compared to various control groups such as waitlists or information provision; intervention effectiveness seemed to be largely independent of the type of digital intervention used57 or physical activity indicator studied17,34,40,49, but were mostly studied in health promotion contexts with the exception of Franssen, et al.29, who also found digital interventions to be effective in older adults with chronic conditions. D’Amore, et al.25 specifically compared digital to face-to-face interventions and found digital interventions were more effective in improving step counts and overall physical activity in older adults, but not moderate-to-vigorous physical activity. Somewhat in contrast to most reviews, Schepens Niemiec, et al.60 reported digital interventions were likely ineffective in reducing sedentary behavior in older adults.
Six reviews tested the effectiveness of digital interventions for specific genders/ sexes. Five reviews included only women24,54; three of them focused exclusively on pregnant and postpartum people37,42,46. One study tested interventions only in men33. Both Cotie, et al.24 and Joseph, et al.54 reported that digital interventions were, on average, effective in promoting physical activity in women. Cotie, et al.24 found that digital interventions were ineffective in promoting weight loss in women, while McMahon, et al.33 reported that online interventions were effective in promoting weight loss in men. In pregnant people, the effectiveness of digital interventions is unclear. According to Leonard, et al.42, digital interventions were effective in reducing gestational weight gain (GWG), promoting physical activity, and promoting healthy dietary behaviors (e.g., reduced caloric intake, increased fruit and vegetable consumption). Rhodes, et al.46, however, reported mostly insignificant changes in GWG and physical activity across included studies. Sherifali, et al.37 reported nonsignificant findings for GWG, but a statistically significant effect for postpartum weight loss.
Three reviews focused on specific racial/ ethnic minority groups. Regarding physical activity, Joseph, et al.54 indicated that digital interventions were effective in promoting physical activity in African American and Hispanic women. Similarly, Bennett, et al.51 reported significant effects on weight loss in digital interventions targeting ethnic minority groups. Results reported in Enyioha, et al.53 were somewhat more mixed, with 3 of 5 studies reporting significant effects on weight loss in African American and Hispanic adults.
SES was addressed in two reviews. Digital interventions were effective in promoting physical activity and weight loss in low SES adults with overweight and obesity (i.e., adults with low income, educational level, or occupational status)56. If the focus was specifically on low-income populations with overweight and obesity, however, digital interventions might be ineffective in inducing meaningful weight loss52.
Reviews contrasting different levels of inequality indicators
Results are visually summarized in Fig. 3.
Fig. 3. Visual summary of results for reviews contrasting different levels of inequality indicators.
Each box represents one finding from one review. Results are split by the respective focus on uptake, engagement, of effectiveness; outcome of interest (diet, physical activity, weight); and social inequality indicator studied. Legend: Gray box = mixed evidence; white box = evidence for no difference; green box = evidence for priority population benefitting more; orange box = evidence for priority population benefitting less; blue box = evidence for men benefitting more.
Only one review reported on the uptake of digital interventions for weight9, and this report was again based on only one included study. It was concluded that there were no differences in intervention uptake based on age, gender/ sex, ethnicity/ race, or education.
Engagement with digital interventions was compared between different levels of inequality indictors in two reviews, of which one focused only on physical activity interventions61, while the other included any mobile intervention for weight-related behaviors9. Results were inconsistent between the two reviews. Regarding age, Yang, et al.61 reported on two studies indicating greater adherence in older age and one not reporting differences, while four out of five studies included in Szinay et al.9 did not find age differences, but the fifth study also reported more engagement in older participants. Regarding gender/ sex, the two studies included in Yang et al.61 reported greater adherence in men. The findings reported in Szinay et al.9 were mixed for gender/sex, with women being more adherent in two studies and the remaining studies reporting null findings. Regarding education, Szinay et al.9 did not report differences in three out of four included studies, while one reported greater engagement in participants with a higher level of education. Similarly, the two included studies in Yang et al.61 reported greater adherence in middle and high education subgroups. Szinay et al.9 also investigated differences between ethnic/ racial subgroups, with two studies reporting that non-Hispanic White participants engaged more with the interventions, while two further studies did not find significant differences. Regarding further indicators of socio-economic status (income, occupation/employment), Szinay et al.9 reported no significant differences, but the number of included studies addressing these inequality indicators was small.
Twenty-one reviews either compared younger and older age groups or tested age as a moderator of intervention effectiveness. Regarding physical activity promotion, Szinay, et al.9 reported mixed findings, with younger age groups benefitting more in two studies and older age groups more in another. Also, Hodkinson et al.62 reported greater benefits in older compared to younger adults with cardiometabolic conditions; in Patterson, et al.44, results of the meta-analysis were even rendered nonsignificant if younger adults (i.e., adults younger than 60 years) with cardiovascular conditions were included. Other reviews did not report significant age differences in both health promotion and treatment contexts24,35,48. In addition, two reviews reported benefits for both younger and older age groups, but effects were stronger in younger adults19,45. For diet, no age differences reported in 3 reviews that included both healthy individuals with and without overweight or obesity and adults with noncommunicable diseases9,28,41, while one review conducted in the context of health promotion reported that a greater proportion of studies reported significant results in older compared to younger adults, indicating that digital dietary interventions might be more effective in older adults55. Also for weight, most reviews concluded there were no age differences across intervention contexts9,23,24,28,36,39,47,48. Three reviews concluded based on a meta-regression that adults with overweight or obesity who were older than 45 years benefited more from digital interventions for weight loss than younger adults30–32. Wong et al.38 contrast with this, since they reported increased weight loss for younger ages.
Eleven reviews reported on differences between genders/ sexes. Regarding physical activity, findings were heterogeneous. Szinay et al.9 reported mixed findings, with men and women benefitting more in one study each, and no differences in a third study. Dehghan Ghahfarokhi et al.27 reported significant improvements in all-men and mixed samples with overweight and obesity, but not in all-women samples; also Franssen, et al.29 reported increased effectiveness in predominantly male samples with chronic conditions. Hodkinson et al.62 reported that both men and women with cardiometabolic conditions benefited from wearables, but effects were strongest in White men. Three reviews reported no significant differences in physical activity outcomes based on gender or sex both in health promotion and treatment contexts26,28,35. For diet, Szinay et al.9 again reported mixed findings, while Duan et al.28 and Lau et al.41 did not find gender or sex differences in digital intervention effectiveness. Finally, regarding weight, no significant gender or sex differences were reported in Duan et al.28. Kodama et al.31 reported effectiveness only in studies with a relatively low (i.e. <80%) proportion of women with overweight or obesity in the sample; similar findings were reported in Seo and Niu36 in the context of health promotion. In contrast, Sequi-Dominguez et al.47, who focused on samples with metabolic syndrome, found that interventions were more effective in studies with a greater proportion of women. Szinay et al.9 again reported mixed findings with either (or neither) gender (or sex) benefiting more in different studies.
Effectiveness was compared in different ethnic groups in two reviews. Szinay, et al.9 found no differences for all three outcomes of interest to this umbrella review. Hodkinson et al.62 reported wearables to be most effective for physical activity promotion in White men with cardiometabolic conditions but indicated that other ethnic groups also significantly increased their physical activity.
Differences in effectiveness based on educational attainment was investigated only in Szinay et al.9; one study reported no differences for diet and weight management, while the other found that individuals with a university degree lost more weight. Regarding further SES indicators, Szinay et al.9 reported potential inequalities based on occupation for weight management (with less weight loss achieved in self-employed individuals or individuals working in agriculture), but not regarding employment or income for diet and weight management. Regarding location, Arambepola et al.22 reported increased effectiveness in studies conducted in low- and middle-income countries compared to high-income countries for physical activity and weight in populations with Type 2 diabetes. Szinay et al.9 reported on one study that found a digital intervention for weight loss to be more effective in urban compared to rural areas; similar results were reported by Livingstone et al.55 for dietary interventions.
Discussion
This umbrella review synthesized systematic and scoping reviews on social inequality in the uptake, engagement and effectiveness of digital interventions for weight-related behaviors in both health promotion and treatment contexts. Most reviews focused on effectiveness and studied age or gender/ sex. Uptake and engagement as well as other social inequality indicators included in the PROGRESS-Plus framework, such as SES, location, or race and ethnicity21, were rarely studied. Again others, such as religion, were not studied at all, indicating substantial gaps in the literature. Attention needs shifting from assessing basic demographic information to a more thorough assessment and analysis of potential sources of inequalities in digital health research to provide the basis for more equitable digital interventions65.
Age was most frequently studied with regards to effectiveness, potentially because of the prevailing stereotype that older adults struggle with using digital technology. However, this might rather be a cohort than an actual age effect, given that the internet was made public over 30 years ago and so also many older adults are familiar with this technology. Not only did reviews exclusively focused on older adults predominantly conclude that digital interventions such as wearables and smartphone apps are effective in promoting physical activity in older adults; reviews comparing different age groups regarding intervention effectiveness for diet, physical activity and weight also mostly reported no age differences or even older adults benefitting more. Digital interventions are thus a promising tool also for older populations. This is also especially important for healthcare professionals to recognize, who often act as gatekeepers and may discourage older adults from using digital health technologies due to likely outdated assumptions66.
Results were somewhat more mixed regarding gender and sex differences in intervention effectiveness. Most reviews focusing on only one gender or sex focused on women or pregnant people, mostly showing that digital interventions were effective in promoting healthier diets and physical activity; results for weight were overall mixed. Comparative reviews, however, either found no differences between genders/ sexes or found that men were more successful in increasing their physical activity levels or losing more weight. Men benefiting more from weight loss trials is a common finding67, and may be attributed to having more time for self-care68 or sex differences in body composition changes69.
Location was a heterogenous inequality indicator, depending on whether country-level parameters or urban-rural differences were examined. Two reviews concluded that urban populations - who already have better access to healthcare including weight management programs and generally are healthier70 - benefit more from digital interventions than rural populations. This might not only be due to limited access to broadband internet access in rural areas, but also reflect important barriers that individuals in rural areas face regarding opportunities for healthy eating or physical activity71 that cannot be overcome through technology alone. Future research needs to determine whether digital interventions can indeed be as effective in rural vs. urban areas if appropriately designed, or if structural barriers need to be removed first, e.g. through policy action. At the same time, one review looking at both physical activity and weight management interventions found they are indeed more effective in low- and middle- vs. high-income countries. This is a promising finding since it might signal an opportunity to reduce health disparities between the Global North and the Global South. However, the included studies were all RCTs, thus, participants were likely provided with the required devices and potentially even selected so they have access to relevant technology72. Global access to digital (health) technology thus might still be an issue; more work is needed to shed light on this.
Interestingly, (lacking) differences in effectiveness did not always align with differences in engagement. The three reviews identified here that specifically studied digital intervention engagement in older adults reported a wide range of estimates for adherence. Results were also mixed regarding age differences in engagement with digital physical activity interventions. Some reviews reported that older adults engage more than younger adults in digital physical activity interventions, while others reported effects in the opposite direction, and again others reported no differences. Factors previously associated with decreased intervention engagement specifically in older adults include illness or injury, competing priorities such as caring responsibilities (e.g., for grandchildren or spouse), and reduced self-efficacy73,74. At the same time, older adults might also have more time because they no longer hold full-time jobs and their children are grown up. Older adults also might have greater motivation for health promotion since they feel more vulnerable75. The diverging results could also be explained by different intervention components used, since in-person components have been shown to predict intervention engagement especially in older adults76. Also, more cognitively demanding intervention components (e.g., planning) may be challenging for older participants77. Digital interventions thus need to be specifically tailored to the needs and skills of older adults to ensure high levels of engagement.
Findings were also mixed regarding engagement differences between genders/ sexes and ethnicities/ races. Both findings point towards the importance of tailoring. For instance, one might speculate whether men are more willing to engage with digital technology for health behavior change since they are generally more interested in technology78. Observational studies on mHealth app uptake and engagement often do not support this finding and report rates to be similar across genders/ sexes, or higher in women79,80. However, genders differ not only in what they consider important regarding goals of a behavior change intervention (e.g., a greater focus on weight management among women vs building muscle mass in men81) but also regarding its design82,83. For example, men might be more interested in competitive elements and therefore might value gamification of health interventions more84. Similarly, cultural tailoring might be important especially for ethnic and racial minorities, not only in terms of culturally appropriate recommendations such as recipes, but also regarding language85.
Finally, uptake was only studied in one systematic review, reporting no evidence for a digital divide in uptake. Notably, findings were based on one study only and thus should be interpreted with caution. Since access to digital technology is unevenly distributed amongst population subgroups86, a digital health divide e.g. based on income or education could be assumed.
A range of possible underpinning mechanisms of the digital divide are discussed in the literature, including contextual factors that differ according to social inequality indicator87. Specific examples include differences in digital infrastructure, access and engagement frequency according to ethnicity, discrepancies in off-line behavioral opportunities (e.g., quality of environment for PA) according to income, and a dislike of social features like forums according to gender, with women showing greater engagement. It is important to note that akin to the present review, the conclusions drawn were derived from very few studies, and relied on often speculated rather than measured inferences about the mechanisms. Further empirical studies are required that test a range of social inequality indicators in relation to digital intervention uptake, engagement, and the mechanisms through which to narrow any identified inequalities, to close this gap.
Important limitations of this umbrella review need to be acknowledged. Most importantly, the quality of all included reviews was low, mostly due to a limited search strategy, a lack of detail on excluded studies, and inappropriate statistics used in meta-analyses. Furthermore, the vast majority of included reviews focused on age and gender/ sex; other social inequalities such as socio-economic status were rarely studied, despite accumulating evidence for its effects on digital intervention effectiveness8. Importantly, reviews are only able to reflect what is reported in primary studies; researchers evaluating the uptake of, engagement with, or effectiveness of digital interventions for weight-related behaviors thus should include a range of inequality indicators in their evaluations to provide sufficient primary data. For instance, social relationships (e.g., being married or living with children) were not studied at all in the included reviews, despite them being potentially helpful in overcoming barriers to digital technology use88. Moreover, most studies evaluate the potential influence of individual inequality indicators, yet certain inequality indicators such as gender and income intersect89. Future work needs to take these interdependencies into account (see also Hollands et al.90, for a call to action for health equity research more broadly) to identify key inequality indicators so disparities can be most effectively reduced. Finally, most included reviews focused predominantly or exclusively on randomized controlled trials, which in themselves also suffer from selection biases and often include fewer individuals from priority populations72. This could potentially mask differences e.g. regarding socio-economic status; data on uptake, engagement and effectiveness should thus also be collected outside the study context to provide ecologically valid insights (see also Szinay et al.9 for a discussion). Finally, the present review focused exclusively on adults. Different processes might influence intervention uptake, engagement, and effectiveness in children and adolescents; most notably, at least up to a certain age, primary caregivers have to be involved especially if technology is used.
Digital health inequity is multifaceted91, and may be affected by aspects such as ease of use, interactivity, digital literacy, digital accessibility, digital availability, digital affordability, and technology personalization10. However, digital health research focuses predominantly on age and gender/ sex differences, for which there is relatively little evidence for a divide especially regarding the effectiveness of digital interventions for weight-related behaviors. Other factors, that might also be more closely linked to inequalities in digital technology use such as income or education are comparatively rarely focused on; this constitutes an important gap in the literature. Studies are needed that compare these and other disadvantaged population subgroups to their privileged counterparts to identify the most important determinants of digital health inequity, which can then by systematically addressed in intervention development, e.g. via patient involvement, and testing to promote digital health for all.
Methods
The protocol was submitted to PROSPERO prior to data extraction and accepted on 24 October 2023, registration number: CRD42023472388. Raw data is provided on the Open Science Framework (OSF; https://osf.io/g4hzb/).
Search strategy
A medical librarian (AHD) searched the following six databases: PubMed (incl. MEDLINE), Web of Science, CINAHL, PsycInfo, Google Scholar, Embase. The search was limited to articles published in the English language between 1970 and October 2023, when the search was conducted. The search strategies were modified for each database using keywords and controlled vocabularies (e.g., Medical Subject Headings) as appropriate. All search strategies are provided in Supplementary Note 1. In addition, reference list searches of identified studies and forward citation tracking was performed in April 2024 by two authors (LMK and RAK) to identify further eligible publications. Instead of exclusively relying on Google Scholar as preregistered, we used the citationchaser Shiny app92 to compile a list of records for screening and supplemented the results for one publication that the tool was unable to identify35 via Google Scholar.
Screening
Duplicates were removed manually before all potentially eligible records identified through the database search were imported into Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia; available at www.covidence.org). Titles and abstracts were independently screened by two authors (LMK, RAK, or MJW), categorizing articles as provisionally eligible or excluded according to the pre-registered eligibility criteria (Table 2). Conflicts were resolved by discussion. Afterwards, all full texts were screened independently by the same authors and coded as eligible or excluded. Again, conflicts were resolved by discussion. The flow of records is documented in the PRISMA flow chart (Fig. 1). Regarding social inequality indicators, we focused on indicators of socioeconomic status (incl. income, education, occupation), but also further inequality indicators as defined in the PROGRESS framework21: gender, age, race/ethnicity, religion, location.
Table 2.
Inclusion and exclusion criteria
| Criterion | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Participants/ population | Adults aged 18 years and older; both healthy and clinical samples | Children, adolescents under the age of 18 years |
| Intervention(s), exposure(s) | Any intervention predominantly delivered through digital means (i.e., smartphone, app, mobile phone, personal digital assistant, text messaging, website, podcast, instant messaging, social media (e.g., Facebook, Twitter, Whatsapp, YouTube), wearable, chatbot, email, and interactive voice response) targeting weight-related behaviors (i.e., diet, physical activity, sedentary behavior). | Interventions using exclusively or primarily non-digital means (e.g., group sessions, pen-and-paper self-monitoring diaries) |
| Comparator(s)/ control | Systematic or scoping reviews either focusing exclusively on priority populations (e.g., African-American adults, adults of older age) or comparing priority and non-priority populations (e.g., comparing individuals with low and high socioeconomic status). | Reviews focusing exclusively on non-priority populations (e.g., Europeans) without explicitly including a quantitative or qualitative evaluation of social inequality (e.g., based on age, gender, or socioeconomic status) |
| Types of studies | Systematic reviews, scoping reviews, or meta analyses (as identified in title or abstract of the publication) that narratively or quantitatively summarize empirical studies | Empirical articles reporting on primary data; conference abstracts; theses; study or review protocols; narrative reviews; articles without peer review |
| Context | Studies in the context of health promotion/ prevention/ treatment. | Clinical contexts, e.g. rehabilitation |
| Outcomes |
Effectiveness in changing diet, physical activity, sedentary behavior, or weight Uptake of and engagement with the intervention |
Reviews focusing also or exclusively on other behaviors (e.g., gait speed, sleep, fall prevention) |
Data extraction and synthesis
Two reviewers (LMK and MJW) extracted data into a structured coding form. Discrepancies were resolved by discussion. Extracted information included review characteristics (e.g., target behavior(s), inequality indicator(s) studied), methodological characteristics (e.g., number and name of databases searched, eligibility criteria, date restrictions), information about the included studies (e.g., total sample size, study designs, countries), information about risk of bias, and conclusions drawn regarding social inequalities in intervention uptake, engagement, and effectiveness. Due to the heterogeneity of the target behaviors and the inequality indicators, results were narratively synthesized separately for reviews focusing exclusively on priority populations and for reviews contrasting different levels of these indicators as well as by intervention uptake, engagement, and effectiveness.
For most inequality indicators, there is consensus as to which population subgroup is considered “priority” in the contexts of health and digital technology (see Table 3). Empirical findings around gender and sex are somewhat mixed. For example, while men tend to be underrepresented in weight management studies93, women tend to be less successful than men in achieving weight loss67 for various possible reasons (e.g., lower adherence to self-monitoring94, more previous weight loss attempts95). Reporting was guided by the PRIOR checklist96 (see Supplementary Note 2).
Table 3.
Overview of populations considered a priority in the present review
| Inequality indicator | Priority population |
|---|---|
| Age | Older age |
| Education | Lower educational attainment |
| Ethnicity/ race | Non-White populations (e.g., African American, Latinx) |
| Gender/ sex | Any |
| Income | Low income |
| Location | Global South/ non-Western (e.g, countries in Africa, South America, certain regions in Asia) |
| Occupation/ employment | Unemployed/ employed in blue collar jobs |
| Religiona | Minority religion |
| SES | Low SES |
aSince no review was identified that included religion, it will not be further discussed.
Overlap of reviews
Overlap of reviews was evaluated quantitatively by calculating the Corrected Covered Area (CCA)64 based on the citation matrix.
Quality appraisal
Diverging from the review protocol, we used AMSTAR 297 to appraise the quality of systematic reviews of randomized-controlled trials, since this tool was deemed more comprehensive and appropriate. Two reviewers (RAK and MJW) independently assessed each included article across each AMSTAR-2 domain, with discrepancies resolved by discussion. Consistent with the guidelines, the AMSTAR-2 ratings were then categorized based on the number of critical and non-critical weaknesses. Specifically, if a study had weaknesses on items #2, #4, #7, #9, #11, #13, or #15 (see Supplementary Figure 1 for item list), the study was classified as having one or more critical weaknesses. If a study had weaknesses on the remaining items, the study was classified as having one or more non-critical weaknesses.
Supplementary information
Acknowledgements
This study was partially funded by National Institute of Diabetes and Digestive and Kidney Diseases (R01DK135227, MPI: Krukowski). The funder played no role in study design, data collection, analysis and interpretation of data, or the writing of this manuscript. Open access funding provided by University of Vienna.
Author contributions
L.M.K.: Conceptualization, data curation, methodology, project administration, visualization, writing—original draft. M.W.: Conceptualization, data curation, methodology, writing—review & editing. A.H.D.: Investigation, methodology, writing—review & editing. R.A.K.: Conceptualization, data curation, methodology, writing—review & editing
Data availability
The dataset generated during the current study is openly available in the Open Science Framework: https://osf.io/g4hzb/.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41746-024-01405-0.
References
- 1.Wang, Y. et al. Has the prevalence of overweight, obesity and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int. J. Epidemiol.49, 810–823 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Okunogbe, A. et al. Economic impacts of overweight and obesity: current and future estimates for 161 countries. BMJ Glob. health7, e009773 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jensen, M. D. et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation129, S102–S138 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu, C.-C. et al. mHealth research for weight loss, physical activity, and sedentary behavior: bibliometric analysis. J. Med. Internet Res.24, e35747 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krukowski, R. A., Tilford, J. M., Harvey-Berino, J. & West, D. S. Comparing behavioral weight loss modalities: incremental cost-effectiveness of an internet-based versus an in-person condition. Obesity19, 1629–1635 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Statista. Global internet penetration rate as of July 2024, by region <https://www.statista.com/statistics/269329/penetration-rate-of-the-internet-by-region/> (2024).
- 7.Singh, B. et al. A systematic umbrella review and meta-meta-analysis of eHealth and mHealth interventions for improving lifestyle behaviours. npj Digital Med.7, 179 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Western, M. J, et al. The effectiveness of digital interventions for increasing physical activity in individuals of low socioeconomic status: a systematic review and meta-analysis. Int J. Behav. Nutr. Phys.18, 1–21 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Szinay, D. et al. Is the uptake, engagement, and effectiveness of exclusively mobile interventions for the promotion of weight-related behaviors equal for all? A systematic review. Obes Rev, e13542 (2023). [DOI] [PubMed]
- 10.Chidambaram, S. et al. An introduction to digital determinants of health. PLOS Digital Health3, e0000346 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pew Research Center. Americans’ Use of Mobile Technology and Home Broadband. (2024).
- 12.Eurostat. Digital economy and society statistics - households and individuals [version: April 2014], <https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Digital_economy_and_society_statistics_-_households_and_individuals> (2024).
- 13.König, L. M. et al. Reducing intervention-and research-induced inequalities to tackle the digital divide in health promotion. Int. J. Equity Health22, 249 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ariel-Donges, A. H. et al. Rural/urban disparities in access to the National Diabetes Prevention Program. Transl Behav. Med10, 1554–1558 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scheerder, A., Van Deursen, A. & Van Dijk, J. Determinants of Internet skills, uses and outcomes. A systematic review of the second-and third-level digital divide. Telemat. Inform.34, 1607–1624 (2017). [Google Scholar]
- 16.Munari, S. C., Wilson, A. N., Blow, N. J., Homer, C. S. & Ward, J. E. Rethinking the use of ‘vulnerable’. Aust. N. Z. J. Public Health45, 197 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu, J. Y.-W., Kor, P. P.-K., Chan, C. P.-Y., Kwan, R. Y.-C. & Cheung, D. S.-K. The effectiveness of a wearable activity tracker (WAT)-based intervention to improve physical activity levels in sedentary older adults: a systematic review and meta-analysis. Arch. Gerontol. Geriatr.91, 104211 (2020). [DOI] [PubMed] [Google Scholar]
- 18.Kwan, R. Y. C. et al. The effect of e-health interventions promoting physical activity in older people: a systematic review and meta-analysis. Eur. Rev. Aging Phys. Act.17, 1–17 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jahangiry, L., Farhangi, M. A., Shab-Bidar, S., Rezaei, F. & Pashaei, T. Web-based physical activity interventions: a systematic review and meta-analysis of randomized controlled trials. Public Health152, 36–46 (2017). [DOI] [PubMed] [Google Scholar]
- 20.Yardley, L. et al. Understanding and promoting effective engagement with digital behavior change interventions. Am. J. Prev. Med51, 833–842 (2016). [DOI] [PubMed] [Google Scholar]
- 21.O’Neill, J. et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J. Clin. Epidemiol.67, 56–64 (2014). [DOI] [PubMed] [Google Scholar]
- 22.Arambepola, C. et al. The impact of automated brief messages promoting lifestyle changes delivered via mobile devices to people with type 2 diabetes: a systematic literature review and meta-analysis of controlled trials. J. Med. Internet Res. 18, e86 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cavero-Redondo, I. et al. Effect of behavioral weight management interventions using lifestyle mHealth self-monitoring on weight loss: a systematic review and meta-analysis. Nutrients12, 1977 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cotie, L. et al. The effectiveness of eHealth interventions on physical activity and measures of obesity among working-age women: a systematic review and meta-analysis. Obes. Rev.19, 1340–1358 (2018). [DOI] [PubMed] [Google Scholar]
- 25.D’Amore, C. et al. Interventions including smart technology compared with face-to-face physical activity interventions in older adults: systematic review and meta-analysis. J. Med. Internet Res. 24, e36134 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davies, C. A., Spence, J. C., Vandelanotte, C., Caperchione, C. M. & Mummery, W. K. Meta-analysis of internet-delivered interventions to increase physical activity levels. Int. J. Behav. Nutr. Phys.9, 1–13 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dehghan Ghahfarokhi, A., Vosadi, E., Barzegar, H. & Saatchian, V. The effect of wearable and smartphone applications on physical activity, quality of life, and cardiovascular health outcomes in overweight/obese adults: a systematic review and meta-analysis of randomized controlled trials. Biol. Res. Nurs.24, 503–518 (2022). [DOI] [PubMed] [Google Scholar]
- 28.Duan, Y. et al. Effects of eHealth-based multiple health behavior change interventions on physical activity, healthy diet, and weight in people with noncommunicable diseases: systematic review and meta-analysis. J. Med Internet Res23, e23786 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Franssen, W. M, Franssen, G. H, Spaas, J, Solmi, F & Eijnde, B. O Can consumer wearable activity tracker-based interventions improve physical activity and cardiometabolic health in patients with chronic diseases? A systematic review and meta-analysis of randomised controlled trials. Int J. Behav. Nutr. Phys17, 1–20 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jahangiry, L. & Farhangi, M. A. Obesity paradigm and web-based weight loss programs: an updated systematic review and meta-analysis of randomized controlled trials. J. Health, Popul. Nutr.40, 1–8 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kodama, S. et al. Effect of Web-based lifestyle modification on weight control: a meta-analysis. Int J. Obes.36, 675–685 (2012). [DOI] [PubMed] [Google Scholar]
- 32.Lau, Y., Chee, D. G. H., Chow, X. P., Cheng, L. J. & Wong, S. N. Personalised eHealth interventions in adults with overweight and obesity: a systematic review and meta-analysis of randomised controlled trials. Prev. Med.132, 106001 (2020). [DOI] [PubMed] [Google Scholar]
- 33.McMahon, J., Thompson, D. R., Pascoe, M. C., Brazil, K. & Ski, C. F. eHealth interventions for reducing cardiovascular disease risk in men: A systematic review and meta-analysis. Prev. Med145, 106402 (2021). [DOI] [PubMed] [Google Scholar]
- 34.Núñez de Arenas-Arroyo, S. et al. Effect of eHealth to increase physical activity in healthy adults over 55 years: A systematic review and meta-analysis. Scand. J. Med. Sci. Sports31, 776–789 (2021). [DOI] [PubMed] [Google Scholar]
- 35.Qiu, S. et al. Using step counters to promote physical activity and exercise capacity in patients with chronic obstructive pulmonary disease: A meta-analysis. Ther. Adv. Respir. Dis.12, 1753466618787386 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Seo, D.-C. & Niu, J. Evaluation of internet-based interventions on waist circumference reduction: a meta-analysis. J. Med. Internet Res.17, e3921 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sherifali, D. et al. The effectiveness of eHealth technologies on weight management in pregnant and postpartum women: systematic review and meta-analysis. J. Med. Internet Res.19, e337 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wong, S. H., Tan, Z. Y. A., Cheng, L. J. & Lau, S. T. Wearable technology-delivered lifestyle intervention amongst adults with overweight and obese: A systematic review and meta-regression. Int. J. Nurs. Stud.127, 104163 (2022). [DOI] [PubMed] [Google Scholar]
- 39.Yen, H. Y. & Chiu, H. L. The effectiveness of wearable technologies as physical activity interventions in weight control: A systematic review and meta-analysis of randomized controlled trials. Obes. Rev.20, 1485–1493 (2019). [DOI] [PubMed] [Google Scholar]
- 40.Yerrakalva, D., Yerrakalva, D., Hajna, S. & Griffin, S. Effects of mobile health app interventions on sedentary time, physical activity, and fitness in older adults: systematic review and meta-analysis. J. Med. Internet Res.21, e14343 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lau, Y. et al. Technology-delivered personalized nutrition intervention on dietary outcomes among adults with overweight and obesity: A systematic review, meta-analysis, and meta-regression. Obes. Rev.25, e13699 (2024). [DOI] [PubMed] [Google Scholar]
- 42.Leonard, K. S., Evans, M. B., Oravecz, Z., Smyth, J. M. & Symons Downs, D. Effect of technology-supported interventions on prenatal gestational weight gain, physical activity, and healthy eating behaviors: a systematic review and meta-analysis. J. Technol. Behav. Sci.6, 25–41 (2021). [Google Scholar]
- 43.Oliveira, J. S., Sherrington, C., Zheng, E. R., Franco, M. R. & Tiedemann, A. Effect of interventions using physical activity trackers on physical activity in people aged 60 years and over: a systematic review and meta-analysis. Br. J. Sports Med.54, 1188–1194 (2020). [DOI] [PubMed] [Google Scholar]
- 44.Patterson, K, Davey, R, Keegan, R & Freene, N Smartphone applications for physical activity and sedentary behaviour change in people with cardiovascular disease: A systematic review and meta-analysis. PloS One16, e0258460 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Peng, P., Zhang, N., Huang, J., Jiao, X. & Shen, Y. Effectiveness of wearable activity monitors on metabolic outcomes in patients with type 2 diabetes: a systematic review and meta-analysis. Endocr. Pract.29, 368–378 (2023). [DOI] [PubMed] [Google Scholar]
- 46.Rhodes, A., Smith, A. D., Chadwick, P., Croker, H. & Llewellyn, C. H. Exclusively digital health interventions targeting diet, physical activity, and weight gain in pregnant women: systematic review and meta-analysis. JMIR mhealth uHealth8, e18255 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sequi-Dominguez, I. et al. Effectiveness of mobile health interventions promoting physical activity and lifestyle interventions to reduce cardiovascular risk among individuals with metabolic syndrome: systematic review and meta-analysis. J. Med Internet Res22, e17790 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Teo, N. R., Siew, L. E. D., Ang, W. H. D. & Lau, Y. in Seminars in Oncology Nursing. 151403 (Elsevier). [DOI] [PubMed]
- 49.Wu, S. et al. The effectiveness of wearable activity trackers for increasing physical activity and reducing sedentary time in older adults: a systematic review and meta-analysis. Digital Health9, 20552076231176705 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Baer, N.-R, Vietzke, J & Schenk, L Middle-aged and older adults’ acceptance of mobile nutrition and fitness apps: A systematic mixed studies review. Plos One17, e0278879 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bennett, G. et al. Electronic health (e H ealth) interventions for weight management among racial/ethnic minority adults: A systematic review. Obes. Rev.15, 146–158 (2014). [DOI] [PubMed] [Google Scholar]
- 52.Clark, T. L. et al. eHealth weight loss interventions for adults with low income: A systematic review. Health Psychol.46, 353–367 (2023). [DOI] [PubMed] [Google Scholar]
- 53.Enyioha, C., Hall, M., Voisin, C. & Jonas, D. Effectiveness of mobile phone and web-based interventions for diabetes and obesity among African American and Hispanic adults in the United States: systematic review. JMIR Public Health Surveill.8, e25890 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Joseph, R. P., Royse, K. E. & Benitez, T. J. A systematic review of electronic and mobile health (e-and mHealth) physical activity interventions for African American and Hispanic women. J. Phys. Act. Health16, 230–239 (2019). [DOI] [PubMed] [Google Scholar]
- 55.Livingstone, K. M, et al. Digital behaviour change interventions to increase vegetable intake in adults: A systematic review. Int J. Behav. Nutr. Phys.20, 36 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Myers-Ingram, R., Sampford, J., Milton-Cole, R. & Jones, G. D. Effectiveness of eHealth weight management interventions in overweight and obese adults from low socioeconomic groups: a systematic review. Syst. Rev.12, 59 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Aslam, A. S., van Luenen, S., Aslam, S., van Bodegom, D. & Chavannes, N. H. A systematic review on the use of mHealth to increase physical activity in older people. Clin. EHealth3, 31–39 (2020). [Google Scholar]
- 58.Jonkman, N. H., van Schooten, K. S., Maier, A. B. & Pijnappels, M. eHealth interventions to promote objectively measured physical activity in community-dwelling older people. Maturitas113, 32–39 (2018). [DOI] [PubMed] [Google Scholar]
- 59.Gravesande, J. et al. Feasibility, usability, and acceptability of online mind–body exercise programs for plder adults: A scoping review. J. Integr. Complementary Med.29, 538–549 (2023). [DOI] [PubMed] [Google Scholar]
- 60.Schepens Niemiec, S. L., Cariño, B., Chatfield, A. J. & Quan, K. mHealth-supported interventions with potential to address sedentary behavior in older adults: a scoping review. J. Aging Phys. Act.30, 1085–1100 (2022). [DOI] [PubMed] [Google Scholar]
- 61.Yang, Y., Boulton, E. & Todd, C. Measurement of adherence to mHealth physical activity interventions and exploration of the factors that affect the adherence: scoping review and proposed framework. J. Med. Internet Res.24, e30817 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hodkinson, A. et al. Association between patient factors and the effectiveness of Wearable Trackers at increasing the number of steps per day among adults with Cardiometabolic conditions: meta-analysis of individual patient data from randomized controlled trials. J. Med. Internet Res.24, e36337 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Trumpf, R. et al. Physical activity monitoring-based interventions in geriatric patients: a scoping review on intervention components and clinical applicability. Eur. Rev. Aging Phys. Act.20, 10 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pieper, D., Antoine, S.-L., Mathes, T., Neugebauer, E. A. & Eikermann, M. Systematic review finds overlapping reviews were not mentioned in every other overview. J. Clin. Epidemiol.67, 368–375 (2014). [DOI] [PubMed] [Google Scholar]
- 65.Stadler, G. et al. Diversified innovations in the health sciences: Proposal for a Diversity Minimal Item Set (DiMIS). Sustain. Chem. Pharm.33, 101072 (2023). [Google Scholar]
- 66.Mace, R. A, Mattos, M. K & Vranceanu, A.-M Older adults can use technology: why healthcare professionals must overcome ageism in digital health. Transl Behav. Med12, 1102–1105 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Williams, R., Wood, L., Collins, C. & Callister, R. Effectiveness of weight loss interventions–is there a difference between men and women: a systematic review. Obes. Rev.16, 171–186 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sturm, R. & Cohen, D. A. Peer reviewed: free time and physical activity among Americans 15 years or older: cross-sectional analysis of the American time use survey. Preventing Chronic Dis.16, E133 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gasteyger, C. et al. Visceral fat loss induced by a low-calorie diet: a direct comparison between women and men. Diab. Obes. Metab.11, 596–602 (2009). [DOI] [PubMed] [Google Scholar]
- 70.Cohen, S. A, Greaney, M. L & Sabik, N. J Assessment of dietary patterns, physical activity and obesity from a national survey: Rural-urban health disparities in older adults. PloS One13, e0208268 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cleland, V. et al. A qualitative study of environmental factors important for physical activity in rural adults. PLoS One10, e0140659 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Krukowski, R. A. et al. Digital health interventions for all? Examining inclusivity across all stages of the digital health intervention research process. Trials25, 98 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cavill, N. A. & Foster, C. E. Enablers and barriers to older people’s participation in strength and balance activities: A review of reviews. J. Frailty Sarcopenia Falls3, 105 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gray, P. M., Murphy, M. H., Gallagher, A. M. & Simpson, E. E. Motives and barriers to physical activity among older adults of different socioeconomic status. J. Aging Phys. Act.24, 419–429 (2016). [DOI] [PubMed] [Google Scholar]
- 75.Putterman, E. & Linden, W. Appearance versus health: Does the reason for dieting affect dieting behavior? J. Behav. Med.27, 185–204 (2004). [DOI] [PubMed] [Google Scholar]
- 76.Gómez-Redondo, P., Valenzuela, P. L., Morales, J. S., Ara, I. & Mañas, A. Supervised Versus Unsupervised Exercise for the Improvement of Physical Function and Well-Being Outcomes in Older Adults: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Sports Med.54, 1877–1906 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.French, D. P., Banafa, R., Williams, S., Taylor, C. & Brown, L. J. How does the understanding, experience, and enactment of self-regulation behaviour change techniques vary with age? A thematic analysis. Appl. Psychol.: Health Well-Being13, 239–260 (2021). [DOI] [PubMed] [Google Scholar]
- 78.Franke, T., Attig, C. & Wessel, D. A personal resource for technology interaction: development and validation of the affinity for technology interaction (ATI) scale. Int. J. Hum.–Comput. Interact.35, 456–467 (2019). [Google Scholar]
- 79.König, L. M., Sproesser, G., Schupp, H. T. & Renner, B. Describing the Process of Adopting Nutrition and Fitness Apps: Behavior Stage Model Approach. JMIR mhealth uHealth6, e55 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Valinskas, S., Nakrys, M., Aleknavičius, K., Jonusas, J. & Lileikienė, A. User engagement and weight loss facilitated by a mobile app: retrospective review of medical records. JMIR Formative Res.7, e42266 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kelley, C. C. G., Neufeld, J. M. & Musher-Eizenman, D. R. Drive for thinness and drive for muscularity: Opposite ends of the continuum or separate constructs? Body Image7, 74–77 (2010). [DOI] [PubMed] [Google Scholar]
- 82.Crane, M. M., Lutes, L. D., Ward, D. S., Bowling, J. M. & Tate, D. F. A randomized trial testing the efficacy of a novel approach to weight loss among men with overweight and obesity. Obesity23, 2398–2405 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Morgan, P. J. et al. The SHED-IT community trial: a randomized controlled trial of internet-and paper-based weight loss programs tailored for overweight and obese men. Ann. Behav. Med.45, 139–152 (2013). [DOI] [PubMed] [Google Scholar]
- 84.König, L. M., Kanning, M., Hauptmann, H., Feuchtner, T. & Arigo, D. Who is willing to play skill-adapted exergames? Influences of sociodemographic factors and social comparison processes Manuscript submitted for publication (2024).
- 85.König, L. M., Attig, C., Franke, T. & Renner, B. Barriers to and facilitators for using nutrition apps: systematic review and conceptual framework. JMIR mHealth uHealth9, e20037 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Jahnel, T., Dassow, H.-H., Gerhardus, A. & Schüz, B. The digital rainbow: digital determinants of health inequities. Digital Health8, 20552076221129093 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mercer, L., Al Masri, M., Rocha, D., König, L. M. & Western, M. J. The mechanisms underpinning the digital health divide: A Scoping Review of interventions for weight-related behaviours. Manuscript submitted for publication (2024).
- 88.Wilson, S. et al. Recommendations to advance digital health equity: a systematic review of qualitative studies. NPJ Digital Med.7, 173 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Corrieri, S. et al. Income-, education-and gender-related inequalities in out-of-pocket health-care payments for 65+ patients-a systematic review. Int. J. equity health9, 1–11 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hollands, G. J. et al. Methods used to conceptualize dimensions of health equity impacts of public health interventions in systematic reviews. J. Clin. Epidemiol.169, 111312 (2024). [DOI] [PubMed] [Google Scholar]
- 91.Lyles, C. R., Nguyen, O. K., Khoong, E. C., Aguilera, A. & Sarkar, U. Multilevel determinants of digital health equity: a literature synthesis to advance the field. Annu. Rev. public health44, 383–405 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Haddaway, N., Grainger, M. & Gray, C. citationchaser: An R package and Shiny app for forward and backward citations chasing in academic searching. Zenodo, Feb16, 10.5281 (2021).
- 93.Pagoto, S. L. et al. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity20, 1234–1239 (2012). [DOI] [PubMed] [Google Scholar]
- 94.Krukowski, R. A., Harvey-Berino, J., Bursac, Z., Ashikaga, T. & West, D. S. Patterns of success: Online self-monitoring in a web-based behavioral weight control program. Health Psychol.32, 164 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Teixeira, P. J. et al. Who will lose weight? A reexamination of predictors of weight loss in women. Int. J. Behav. Nutr. Phys.1, 1–12 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gates, M. et al. Reporting guideline for overviews of reviews of healthcare interventions: development of the PRIOR statement. BMJ378, e070849 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Shea, B. J. et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised ornon-randomised studies of healthcare interventions, or both. BMJ358, j4008 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset generated during the current study is openly available in the Open Science Framework: https://osf.io/g4hzb/.