Abstract
Background:
Carpal tunnel syndrome (CTS) is a common nerve entrapment condition, and there is ongoing debate regarding the superiority of traditional open versus minimally invasive carpal tunnel surgery.
Methods:
This meta-analysis reviewed six studies involving 478 patients to compare recovery and functional outcomes between the traditional longitudinal technique and the minimally invasive mini-transverse technique. The primary outcomes included the functional status scale (FSS), symptoms severity scale (SSS), pain scores, time to return to work, duration of operation, and incidence of complications.
Results:
The mini-transverse technique was associated with lower FSS and SSS scores compared to the longitudinal technique, with mean differences (MD) of −0.32 (95% confidence level [CI]: −0.52, −0.12, P = 0.002) and −0.43 (95%CI: −0.6, −0.25, P < 0.00001), respectively. Pain scores were also lower with the mini-transverse technique (MD) of −0.5 (95%:CI: −0.71, −0.3, P < 0.00001). The mini-transverse group had a statistically significant shorter time to return to work (MD) of −8.34 (95%CI: −13.55, −3.13, P = 0.002). No significant differences were found in the duration of surgery (MD) of −6.96 (95%CI: −16.66, 2.74, P = 0.16) or incidence of complications (MD) of 0.46 (95%CI: 0.15, 1.4, P = 0.17).
Conclusion:
The mini-transverse approach for CTS resulted in better outcomes, including less pain, faster recovery, and improved hand function. There was no significant difference in surgery time or complications compared to the traditional technique, suggesting it may be the preferable option.
Keywords: Carpal tunnel syndrome, Median nerve entrapment, Mini-transverse

INTRODUCTION
Carpal tunnel syndrome (CTS) is the most prevalent upper limb entrapment neuropathy, constituting roughly 0.6–3.4% of the general population.[2,13,14] This prevalence jumps significantly for workers who regularly use their hands and wrists for daily tasks, affecting up to 5% of this specific group. Annually, there are 105 new cases of men and 197 new cases of women of CTS diagnosed for every 100,000 individuals.[14] Patients typically experience excruciating paresthesia or burning sensations in the radial half of their hand, especially at night.[19] When conservative measures fail, the standard surgical treatment involves dividing the transverse carpal ligament to release the trapped median nerve.[5]
Historically, three surgical approaches have been used: endoscopic, limited incision, and the classic open technique.[6] Open surgery has fallen out of favor due to concerns about longer, more painful scars, poor wound healing, pillar pain, and delayed return to work, all impacting quality of life.[11,20]
Minimally invasive techniques such as endoscopically assisted release, mini-open longitudinal, and mini-open transverse approaches were developed to address these issues.[7,23,30] Endoscopic carpal tunnel releases have shown advantages in terms of grip strength, pinch strength, and scar tenderness compared to open releases.[30] However, the evidence regarding symptom relief and return to work is mixed.[30] In addition, endoscopy has been linked to a higher risk of irreversible nerve damage and incomplete release of the flexor retinaculum.[4,6,10,30]
Due to this ongoing controversy and gap in knowledge regarding the superiority of the traditional open technique versus the minimally invasive technique, we conducted a systematic review and meta-analysis to compare the two techniques and their outcomes comprehensively.
MATERIALS AND METHODS
This study adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. This study was registered with PROSPERO (CRD42024548218).
Literature search
A comprehensive computerized search was performed to locate pertinent articles. The databases PubMed, Scopus and Web of Science were all searched. The following search terms were used from the beginning till April 2024: “Longitudinal,” “Transverse,” OR “Mini-transverse,” AND “ Carpal tunnel syndrome.” We did not apply any criteria, and we looked through the reference lists of the included articles to see if there were any more relevant publications that we missed in our search. Our search strategy resulted in a total of 532 articles; after duplicate removal, we screened 255 articles, as summarized in the PRISMA flowchart [Figure 1].
Figure 1:
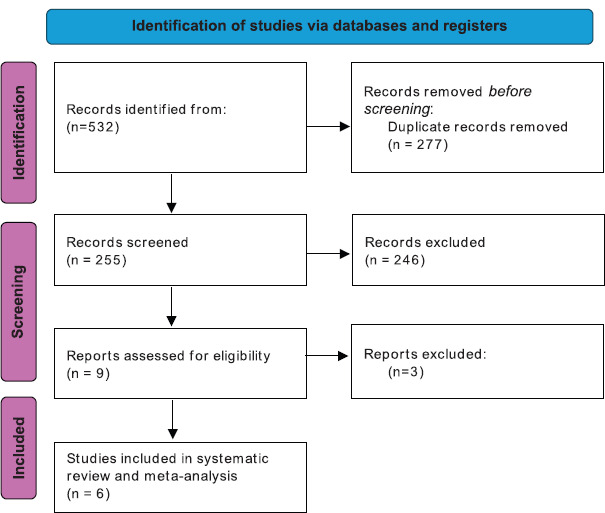
PRISMA flowchart of database searching and screening process.
Inclusion and exclusion criteria
The inclusion criteria for this review encompass studies that compare the use of mini-transverse techniques and longitudinal techniques in the surgical treatment of CTS patients, specifically focusing on primary research articles that present original data, regardless of the language of publication. Exclusion criteria include studies that do not directly compare these two surgical techniques, as well as review articles, opinion pieces, or case studies.
Study screening and selection
First, articles were screened by title and abstract by four independent authors in a blinded fashion. Articles that did not meet the inclusion criteria were excluded, and the first author settled any differences. Full texts of articles that met the inclusion criteria were retrieved and screened by two independent reviewers, and the first author settled conflicts.
Data extraction
Data extraction was carried out independently by two writers using Microsoft Excel sheets. A senior author arbitrated any disputes among the authors. The study design, gender, age, and sample size were retrieved as baseline features from the included studies. In addition, we extracted information on the operation’s duration, healing period, complications, and satisfactory, good, or exceptional results.
Quality assessment using the Newcastle–Ottawa Scale (NOS) tool
We assessed the quality of cohort studies using the NOS; studies with a score of 7–9 were of high quality, 4–6 were of moderate quality, and 1–3 was of low quality.[32] The risk of bias (ROB) in randomized controlled trials (RCTs) was assessed using the Cochrane ROB-2 tool.[27]
Outcomes measured
Primary outcomes of interest were comparative outcomes between two techniques considering variables: functional status scale (FSS), symptoms severity scale (SSS), pain scale, and time to return to work or activities. Secondary outcomes included the surgery time and the incidence of complications.
Statistical analysis and heterogeneity
We conducted the meta-analysis by pooling the results using Review Manager V. 5.4 software. A random effect model was utilized in pooling with P = 0.05 and a confidence level (CI) of 95%. The analysis for dichotomous variables was done using event and total to calculate the odds ratio (OR), while that of continuous variables was done using mean difference (MD). Heterogeneity between studies was assessed using the I2 statistical test. P < 0.05 was considered statistically significant.
RESULTS
Literature search
Our search strategy resulted in a total of532 articles; after duplicate removal, we screened 255 articles, as summarized in the PRISMA flowchart [Figure 1]. After title and abstract screening, nine articles entered the full-text screening resulting in a total of six articles[15,24,21,26,29,31] to be included in our meta-analysis [Table 1].
Table 1:
Baseline characteristics of the included studies.
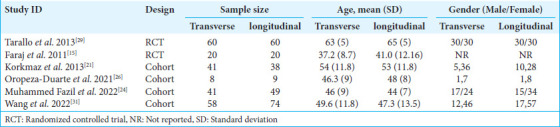
Characteristics of the included studies
A total of 478 patients were analyzed across the six studies included in this review. The studies consisted of four cohort studies and two RCTs, with 228 patients undergoing mini-transverse surgery and 250 patients undergoing longitudinal surgery. The baseline characteristics of the included studies are detailed in Table 1. The age and gender distributions were similar across the study groups, although specific gender data were not consistently reported across all studies.
Quality assessment of included studies
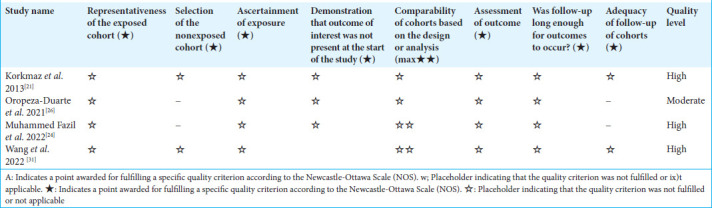
The two included RCTs were assessed using the Cochrane RoB-2 tool and demonstrated a low ROB [Figure 2]. The quality of the four cohort studies was evaluated using the NOS. Three studies were deemed to have high methodological quality, while one study was considered to have moderate quality [Table 2].
Figure 2:
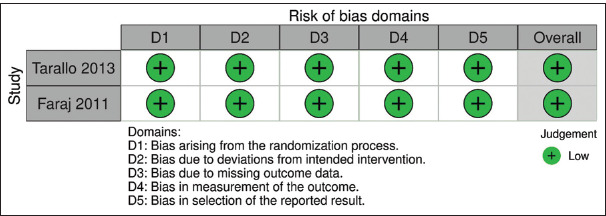
Risk of bias (RoB) assessment of the randomized controlled trials using the Rob-2 tool.
Table 2:
Quality assessment of the included cohort studies using the Newcastle–Ottawa Scale.
Data analysis
The meta-analysis demonstrated that the mini-transverse technique consistently provided better outcomes compared to the traditional longitudinal approach across a range of key measures. For functional outcomes, patients who underwent the mini-transverse technique had significantly lower scores on the Functional Status Scale (FSS), with a MD of −0.32 (95% CI, −0.52–−0.12; P = 0.002; I2 = 59%) [Figure 3]. This finding suggests that these patients experienced better functional recovery and an overall improvement in their ability to perform daily tasks compared to those who had the longitudinal technique. In addition, the mini-transverse group showed significantly lower scores on the Symptoms Severity Scale (SSS) (MD −0.43; 95% CI, −0.6–−0.25; P < 0.00001; I2 = 76%) [Figure 4], indicating a notable reduction in the severity of symptoms. This highlights the effectiveness of the mini-transverse approach in alleviating the discomfort associated with CTS. Another clear advantage of the mini-transverse approach was in pain management, with an MD of −0.5 (95% CI, −0.71–−0.3; P < 0.00001; I2 = 0%) on the Visual Analog Scale (VAS) for pain, individuals in the mini-transverse group reported significantly reduced pain [Figure 5]. The evidence suggests that the less invasive nature of the mini-transverse technique results in reduced postoperative discomfort, potentially leading to a faster and more comfortable recovery. In addition to reduced pain, patients who underwent the mini-transverse procedure recovered faster and returned to work and their regular activities. As shown in Figure 6, the MD in return-to-work time was −8.34 days (95% CI, −13.55–−3.13; P = 0.002; I2= 99%), indicating that patients in the mini-transverse group were able to resume their normal routines much sooner than those who had the longitudinal technique. This result underscores how the mini-transverse approach can lead to a quicker recovery and less disruption to personal and professional lives. Regarding surgery duration, no significant difference was observed between the two techniques. The meta-analysis found an MD of −6.96 (95% CI, −16.66–2.74; P = 0.16; I2 = 99%) [Figure 7], suggesting that both techniques required a similar amount of time to perform. This indicates that while the mini-transverse technique offers better recovery outcomes, it does not come at the expense of longer operating times. Finally, there were no notable differences between the two groups in terms of complications. The OR for the incidence of complications was 0.46 (95% CI, 0.15–1.4; P = 0.17; I2 = 0%) [Figure 8], indicating that the safety profiles of the mini-transverse and longitudinal procedures were comparable.
Figure 3:
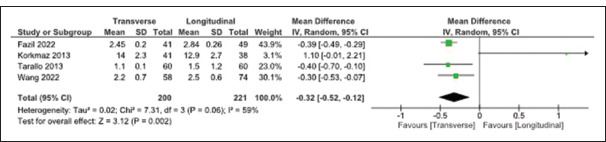
Comparison between mini-transverse and longitudinal techniques regarding functional status scale. SD: Standard deviation, CI: Confidence interval
Figure 4:
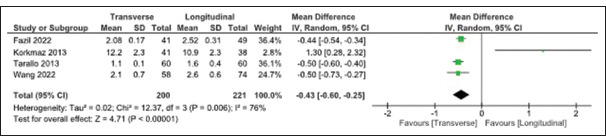
Comparison between mini-transverse and longitudinal techniques regarding symptoms severity scale. SD: Standard deviation, CI: Confidence interval
Figure 5:
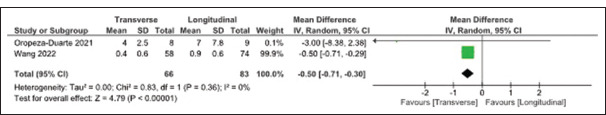
Comparison between mini-transverse and longitudinal techniques regarding pain. SD: Standard deviation, CI: Confidence interval.
Figure 6:
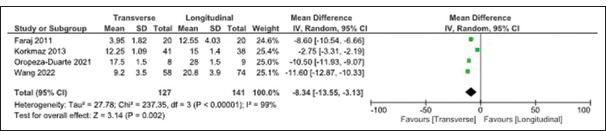
Comparison between mini-transverse and longitudinal techniques regarding time to return to work. SD: Standard deviation, CI: Confidence interval.
Figure 7:
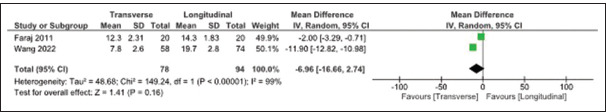
Comparison between mini-transverse and longitudinal techniques regarding operation time. SD: Standard deviation, CI: Confidence interval.
Figure 8:
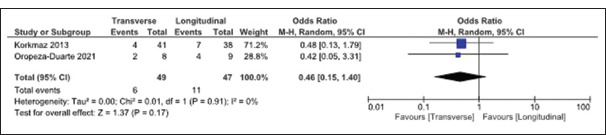
Comparison between mini-transverse and longitudinal techniques regardingcomplications. SD: Standard deviation, CI: Confidence interval.
DISCUSSION
The present study evaluated the effectiveness and safety of mini-transverse versus longitudinal surgical techniques for patients with CTS. Notably, the results leaned in favor of the mini-transverse method. Patients who underwent this procedure showed statistically significant improvements in functional status scale (FSS), symptoms severity scale (SSS), and pain levels. Furthermore, their recovery and return to daily activities were faster than those who underwent the longitudinal technique. Despite these advantages, there were no significant differences in operative time or complication rates between the two techniques. Several studies, as discussed, support the superiority of the mini-transverse approach.
Tarallo et al. (2014)[29] conducted a randomized clinical trial comparing the traditional open carpal tunnel release (TOCTR) technique with the minimal-access carpal tunnel release (MACTR) for treating CTS patients. The MACTR method offers several advantages, making it a strong alternative. It is a safe and reliable procedure with a short learning curve for surgeons, resulting in shorter operation times and potentially reduced costs. In addition, the MACTR technique can be executed with standard surgical instruments, eliminating the need for specialized or costly equipment. Their study further highlights the benefits of MACTR, showing significant improvements over the TOCTR technique. Moreover, patients tolerate the procedure well, aligning with the preference for minimally invasive approaches in modern surgery.[29]
Faraj et al. (2012)[15] compared two surgical methods for CTS: the mini-transverse incision and the traditional open incision. Their study assessed both subjective aspects (patient experience) and objective outcomes (surgical results). Subjectively, the majority of patients in both groups experienced symptom relief, though a slightly higher satisfaction rate was observed in the mini-transverse incision group. There were no significant differences in nerve function tests between the two techniques. Objectively, the mini-transverse approach led to a significantly smaller scar and a quicker return to daily activities. The researchers concluded that the mini-transverse incision is a safe and effective alternative to the traditional open method, providing the added advantages of a smaller scar and faster recovery.[15]
In a study by Oropeza-Duarte et al., (2021)[26], the mini-transverse incision was compared with the traditional longitudinal technique for CTS. The findings showed that patients who underwent the mini-transverse incision returned to work significantly faster, with a median of 17.5 days compared to 28 days for those who had the traditional technique. In addition, patients reported less pain during the 1st week, scoring 4 versus 7 on a VAS. There were no notable differences in complication rates between the two groups. These outcomes suggest that the mini-transverse incision may be a more effective option for carpal tunnel surgery, offering shorter recovery times and reduced disability.[26]
Muhammed Fazil et al.[24] explored the differences between two carpal tunnel release techniques: The limited longitudinal palmar incision and the mini-open transverse flexor crease incision. Their study focused on short-term outcomes, assessing patients preoperatively and at 2 weeks, 6 weeks, 3 months, 6 months, and 12 months after surgery. They used the Boston CTS Questionnaire scores, VAS, grip strength, and return-to-work days to track patient progress. Based on the follow-up results, Muhammed Fazil et al. concluded that the mini-open transverse flexor crease incision technique is a simpler, safer, and more cost-effective method for treating idiopathic CTS compared to the limited palmar incision. Although long-term outcomes are similar, the mini-open technique offers benefits in terms of pain relief, esthetics, and faster recovery.[24]
A recent study by Wang et al. (2022)[31] examined a minimally invasive technique for CTS, comparing a novel mini-transverse incision method with a traditional midpalmar small longitudinal incision. The mini-transverse group experienced significantly smaller scars shorter surgery durations, and showed a trend toward faster recovery, including an earlier return to work and daily activities. Both groups demonstrated substantial symptom improvement, and while hospital stays were similar, the mini-transverse incision group had fewer complications and better overall outcomes. The authors concluded that this innovative technique, which employs a mini-transverse incision and a specialized surgical tool (bush hook), presents a promising alternative for CTS surgery. Nevertheless, they stressed the importance of larger-scale studies to validate these results.[31] Numerous techniques have been described for carpal tunnel release, including the traditional open approach, the endoscopic method, and, more recently, the limited incision approach.[3,9,23] While each of these methods has been associated with certain challenges and adverse effects, all have proven effective in alleviating CTS symptoms.
Although open carpal tunnel release is widely regarded as the gold standard for treating CTS, its failure rate ranges from 7 to 20%.[9,18,26] In recent years, however, most cases have been treated using a small longitudinal incision that extends approximately 2–4 cm distal to the wrist crease.[28] Numerous studies have shown that smaller incisions lead to shorter recovery periods and improved functional outcomes.[3,7,16,25] The mini-transverse carpal tunnel release offers superior scar esthetics,[15] though symptom improvement may be slower compared to the mini-longitudinal approach.[15] Both of these methods are generally preferred over endoscopic surgery due to lower costs and a potentially reduced risk of complications.[15] Endoscopic carpal tunnel release, while advantageous in avoiding damage to palmar cutaneous nerve fibers and preventing scar-related discomfort,[12] has certain drawbacks. Research indicates incomplete ligament release and an increased risk of nerve injury during endoscopic procedures.[1] In addition, the steep learning curve, longer operative times, and need for specialized equipment contribute to higher costs, which may limit its widespread use among surgeons.[6]
Blind mini-open carpal tunnel release, a minimally invasive technique that offers faster recovery compared to open surgery,[3,7] involves the use of specialized instruments such as the Indiana Tome for ligament release.[22] While generally safe and effective, with a complication rate of just 0.83%, as reported by Lee et al., (2008)[22], there has been a documented case of nerve transection associated with the procedure.[8] Other devices, such as the Safeguard System and KnifeLight, utilize similar approaches for blind mini-open release.[16,17]
To the best of our knowledge, this is the first meta-analysis comparing minimally invasive versus longitudinal approaches in CTS patients. However, several limitations may affect the generalizability of the findings. First, the small number of included studies limits the statistical power of the analysis. In addition, the overall sample size may be insufficient to detect significant differences. Moreover, the inclusion of only two published RCTs on this topic weakens the overall strength of the evidence. Given these limitations, future well-designed RCTs with significantly larger sample sizes are needed to definitively assess the relative effectiveness of minimally invasive versus longitudinal approaches in CTS patients.
CONCLUSION
This study demonstrates that the mini-transverse surgical approach emerged as the superior method for CTS patients, yielding significant improvements in functional outcomes, symptom severity, pain scores, and time to return to work compared to the longitudinal technique. Notably, both approaches demonstrated comparable procedure length and complication rates.
Acknowledgments
The authors acknowledge the Deanship of Scientific Research at King Faisal University for obtaining financial support for research, authorship, and the publication of research under Research proposal Number (KFU241173).
Footnotes
How to cite this article: Aleid AM, Alanazi SN, Aljabr AA, Almalki SF, AlAidarous HAA, Alzahrani AA, et al. A comparative meta-analysis of mini-transverse versus longitudinal techniques in the treatment of carpal tunnel syndrome. Surg Neurol Int. 2024;15:468. doi: 10.25259/SNI_897_2024
Contributor Information
Abdulsalam Mohammed Aleid, Email: 225094489@student.kfu.edu.sa.
Sultan Nawaf Alanazi, Email: sultan12alanazi@gmail.com.
Abdulmajeed Abdulaziz Aljabr, Email: mjeedaziz2@gmail.com.
Sami Fadhel Almalki, Email: sa1ma1ki@kfu.edu.sa.
Hasan Ali Abdullah AlAidarous, Email: halaidarous@bu.edu.sa.
Abdulwahab Ahmed Alzahrani, Email: Abdulwahab@bu.edu.sa.
Zainab Mohammed Aleid, Email: Zeid@kfshrc.edu.sa.
Yousef Khalaf A. Alghamdi, Email: yal.ghamdi@bu.edu.sa.
Saud Nayef Aldanyowi, Email: saldanyowi@kfu.edu.sa.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
This work was supported by the Deanship of Scientific Research, Vice Presidency for Graduate Studies and Scientific Research, King Faisal University, Saudi Arabia [Grant No.KFL’241173].
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Agee JM, McCarroll HR, Jr, Tortosa RD, Berry DA, Szabo RM, Peimer CA. Endoscopic release of the carpal tunnel: A randomized prospective multicenter study. J Hand Surg Am. 1992;17:987–95. doi: 10.1016/s0363-5023(09)91044-9. [DOI] [PubMed] [Google Scholar]
- 2.Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, Rosén I. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999;282:153–8. doi: 10.1001/jama.282.2.153. [DOI] [PubMed] [Google Scholar]
- 3.Avci S, Sayli U. Carpal tunnel release using a short palmar incision and a new knife. J Hand Surg Br. 2000;25:357–60. doi: 10.1054/jhsb.2000.0445. [DOI] [PubMed] [Google Scholar]
- 4.Benson LS, Bare AA, Nagle DJ, Harder VS, Williams CS, Visotsky JL. Complications of endoscopic and open carpal tunnel release. Arthroscopy. 2006;22:919–24. doi: 10.1016/j.arthro.2006.05.008. 924.e1-2. [DOI] [PubMed] [Google Scholar]
- 5.Bromley GS. Minimal-incision open carpal tunnel decompression. J Hand Surg Am. 1994;19:119–20. doi: 10.1016/0363-5023(94)90234-8. [DOI] [PubMed] [Google Scholar]
- 6.Brown RA, Gelberman RH, Seiler J, 3rd, Abrahamsson SO, Weiland AJ, Urbaniak JR, et al. Carpal tunnel release. A prospective, randomized assessment of open and endoscopic methods. JBJS. 1993;75:1265–75. doi: 10.2106/00004623-199309000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Cellocco P, Rossi C, Bizzarri F, Patrizio L, Costanzo G. Mini-open blind procedure versus limited open technique for carpal tunnel release: A 30-month follow-up study. J Hand Surg Am. 2005;30:493–9. doi: 10.1016/j.jhsa.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 8.Chapman CB, Ristic S, Rosenwasser MP. Complete median nerve transection as a complication of carpal tunnel release with a carpal tunnel tome. Am J Orthop (Belle Mead NJ) 2001;30:652–3. [PubMed] [Google Scholar]
- 9.Chow JC. Endoscopic release of the carpal ligament: A new technique for carpal tunnel syndrome. Arthroscopy. 1989;5:19–24. doi: 10.1016/0749-8063(89)90085-6. [DOI] [PubMed] [Google Scholar]
- 10.Chung KC, Walters MR, Greenfield ML, Chernew ME. Endoscopic versus open carpal tunnel release: A cost-effectiveness analysis. Plast Reconstr Surg. 1998;102:1089–99. doi: 10.1097/00006534-199809040-00026. [DOI] [PubMed] [Google Scholar]
- 11.Cokluk C, Senel A, Iyigün O, Celik F, Rakunt C. Open median nerve release using double mini skin incision in patients with carpal tunnel syndrome: Technique and clinical results. Neurol Med Chir (Tokyo) 2003;43:465–7. doi: 10.2176/nmc.43.465. [DOI] [PubMed] [Google Scholar]
- 12.DaSilva MF, Moore DC, Weiss AP, Akelman E, Sikirica M. Anatomy of the palmar cutaneous branch of the median nerve: Clinical significance. J Hand Surg Am. 1996;21:639–43. doi: 10.1016/S0363-5023(96)80018-9. [DOI] [PubMed] [Google Scholar]
- 13.Dydyk AM, Negrete G, Sarwan G, Cascella M. StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Median nerve injury. [Google Scholar]
- 14.El-Helaly M, Balkhy HH, Vallenius L. Carpal tunnel syndrome among laboratory technicians in relation to personal and ergonomic factors at work. J Occup Health. 2017;59:513–20. doi: 10.1539/joh.16-0279-OA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Faraj AA, Ahmed MH, Saeed OA. A comparative study of the surgical management of carpal tunnel syndrome by mini-transverse wrist incisions versus traditional longitudinal technique. Eur J Orthop Surg Traumatol. 2012;22:221–5. [Google Scholar]
- 16.Hughes TB, Jr, Baratz M. Limited open carpal tunnel syndrome using the safeguard system. Tech Orthop. 2006;21:12–8. [Google Scholar]
- 17.Hwang PY, Ho CL. Minimally invasive carpal tunnel decompression using the KnifeLight. Neurosurgery. 2007;60:S162–8. doi: 10.1227/01.NEU.0000249249.33052.7E. [DOI] [PubMed] [Google Scholar]
- 18.Katz RT. Carpal tunnel syndrome: A practical review. Am Fam Physician. 1994;49:1371–9. 1385-6. [PubMed] [Google Scholar]
- 19.Keramettin A, Cengiz C, Nilgun C, Ayhan B. Microsurgical open mini uniskin incision technique in the surgical treatment of carpal tunnel syndrome. Neurol India. 2006;54:64–7. doi: 10.4103/0028-3886.24710. [DOI] [PubMed] [Google Scholar]
- 20.Kessler FB. Complications of the management of carpal tunnel syndrome. Hand Clin. 1986;2:401–6. [PubMed] [Google Scholar]
- 21.Korkmaz M, Ekici MA, Cepoglu MC, Oztürk H. Mini transverse versus longitudinal incision in carpal tunnel syndrome. J Coll Physicians Surg Pak. 2013;23:645–8. [PubMed] [Google Scholar]
- 22.Lee WP, Schipper BM, Goitz RJ. 13-year experience of carpal tunnel release using the Indiana Tome technique. J Hand Surg Am. 2008;33:1052–6. doi: 10.1016/j.jhsa.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 23.Lee WP, Strickland JW. Safe carpal tunnel release via a limited palmar incision. Plast Reconstr Surg. 1998;101:418–24. doi: 10.1097/00006534-199802000-00025. [DOI] [PubMed] [Google Scholar]
- 24.Muhammed Fazil VV, Surendran S, Karuppal R, Gopinathan P, Marthya A. Mini-open transverse flexor crease incision versus limited longitudinal palmar incision carpal tunnel release: A short term outcome study. J Orthop. 2022;29:15–21. doi: 10.1016/j.jor.2021.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nathan PA, Meadows KD, Keniston RC. Rehabilitation of carpal tunnel surgery patients using a short surgical incision and an early program of physical therapy. J Hand Surg Am. 1993;18:1044–50. doi: 10.1016/0363-5023(93)90401-N. [DOI] [PubMed] [Google Scholar]
- 26.Oropeza-Duarte C, Ramos-Maciel J, Naranjo-Hernández JD, Villarreal-Salgado JL, Torres-Salazar QL. Effectiveness of mini-transverse incision versus traditional reduced technique in the treatment of carpal tunnel syndrome. A prospective cohort study. Int J Surg Case Rep. 2021;88:106501. doi: 10.1016/j.ijscr.2021.106501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.RoB 2: A revised Cochrane risk-of-bias tool for randomized trials-Cochrane bias doi: 10.1016/j.jclinepi.2020.06.015. Available from: https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials [Last accessed on 2024 Oct 18] [DOI] [PubMed] [Google Scholar]
- 28.Rodner CM, Katarincic J. Open carpal tunnel release. Tech Orthop. 2008;23:199–207. [Google Scholar]
- 29.Tarallo M, Fino P, Sorvillo V, Parisi P, Scuderi N. Comparative analysis between minimal access versus traditional accesses in carpal tunnel syndrome: A prospective randomized study. J Plast Reconstr Aesthet Surg. 2014;67:237–43. doi: 10.1016/j.bjps.2013.10.033. [DOI] [PubMed] [Google Scholar]
- 30.Thoma A, Veltri K, Haines T, Duku E. A meta-analysis of randomized controlled trials comparing endoscopic and open carpal tunnel decompression. Plast Reconstr Surg. 2004;114:1137–46. doi: 10.1097/01.prs.0000135850.37523.d0. [DOI] [PubMed] [Google Scholar]
- 31.Wang D, Ma T, Hu Y, Zhao X, Song L. Effectiveness and safety of surgical treatment of carpal tunnel syndrome via a mini-transverse incision and a bush hook versus a mid-palmar small longitudinal incision. J Orthop Surg Res. 2022;17:75. doi: 10.1186/s13018-022-02967-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wells GA, Wells G, Shea B, Shea B, O’Connell D, Peterson J, et al. Research Programs. 2014. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. [Google Scholar]


