Abstract
Diabetic foot infections (DFIs) are a significant complication in diabetes mellitus, leading to increased morbidity, hospitalizations, and healthcare burdens. The growing prevalence of antibiotic-resistant pathogens has reduced the efficacy of conventional treatments, highlighting the need for alternative therapeutic strategies. Natural products, known for their antimicrobial, anti-inflammatory, and wound-healing properties, have garnered attention as potential treatments for DFIs. This review examines key natural compounds, including eugenol, thymol, carvacrol, curcumin, and Aloe vera, and their mechanisms of action in combating diabetic infections. We analyze the antimicrobial efficacy of these compounds, their ability to inhibit biofilm formation, and their role in wound healing. The review also explores challenges in integrating natural products into clinical practice and the potential for their use alongside or in place of traditional antibiotic therapies. Our findings suggest that natural products could play a crucial role in developing sustainable and effective treatment strategies for DFIs, especially in the face of rising antimicrobial resistance.
Keywords: Diabetic foot infection, Natural product, Treatment
Introduction
Diabetes mellitus (DM) is a chronic disease that has been rapidly increasing in prevalence worldwide, impacting millions of people [1]. As of 2021, approximately 485 million people were diagnosed with DM, and this number is projected to rise to 578 million by 2030 [2]. As the number of diabetes cases continues to grow, so does the occurrence of related complications and hospitalizations, creating significant challenges for healthcare systems globally [3]. One of the most severe complications is diabetic foot infections (DFIs), which contribute to a large proportion of diabetes-related hospital admissions [4]. People with diabetes have a 50-fold higher risk of hospitalization due to DFIs compared to non-diabetic individuals [5].
The conventional treatment of DFIs typically involves the use of antibiotics and advanced wound care management [6]. However, the rising threat of antibiotic resistance has made it increasingly difficult to treat these infections effectively [7]. As a result, there is a growing interest in exploring alternative therapies that can either complement or replace conventional antibiotics. Among these alternatives, natural products have shown significant promise due to their antimicrobial, anti-inflammatory, and wound-healing properties [8].
Natural products, derived from plants, microorganisms, and other natural sources, have long been extensively in traditional medicine and are now gaining recognition in modern healthcare for their therapeutic potential [9, 10]. These compounds offer unique mechanisms of action, making them particularly suitable for addressing complex infections such as DFIs [11, 12].
This review aims to explore the current understanding of natural products in the treatment of DFIs, focusing on their antimicrobial, wound healing, and anti-inflammatory properties. We will examine key compounds derived from medicinal plants, essential oils, and other natural sources, as well as their mechanisms of action, clinical efficacy, and potential for integration into modern DFIs management protocols. By highlighting these natural alternatives, this review seeks to provide insights into developing more sustainable and effective strategies for treating DFIs, particularly in the face of the global rise of antibiotic resistance.
Pathophysiology of diabetic foot infections
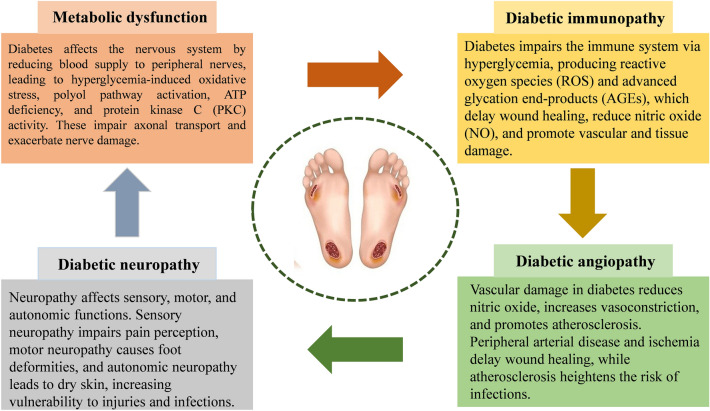
The development of DFIs is driven by a complex interplay of metabolic dysfunction, neuropathy, angiopathy, and immune system changes (Fig. 1) [13]. These factors contribute to the progression of DFIs and can lead to severe complications such as diabetic neuroarthropathy [14]. The pathophysiology of DFIs involves endothelial dysfunction, ischemia, impaired immune response, and neuroarthropathy, all of which are interlinked through various metabolic and vascular pathways [14]. In particular, metabolic imbalances, diabetic neuropathy, and angiopathy promote DFIs by disrupting the body’s normal defense mechanisms and tissue repair processes [15].
Fig. 1.
Pathophysiology of diabetic foot infections (DFIs)
Metabolic dysfunction
In diabetes, metabolic dysfunction affects the nervous system by reducing blood supply to nerves, particularly in the peripheral nervous system, where the long axons are vulnerable to damage [16]. Hyperglycemia, the hallmark of diabetes, leads to several pathological processes, including ATP deficiency, oxidative stress, activation of the polyol pathway, and protein kinase C (PKC) activity [17]. These processes collectively contribute to peripheral nerve damage by impairing axonal transport and inducing axonal degeneration [18]. Excessive oxidative stress and accumulation of harmful by-products like sorbitol and fructose further exacerbate nerve injury, while PKC activation leads to vascular dysfunction and worsens microvascular complications [19].
Diabetic immunopathy
Diabetes also impairs the immune system, reducing the body’s ability to fight infections [20]. Hyperglycemia leads to the overproduction of reactive oxygen species (ROS), which not only damages tissues but also triggers the formation of advanced glycation end-products (AGEs) [20]. These AGEs inhibit nitric oxide (NO) production, crucial for proper wound healing, and contribute to oxidative stress [21]. The excessive ROS in diabetic wounds delays healing and increases vulnerability to infections [21]. In addition, vascular damage from oxidative stress leads to microcirculation issues, further impairing wound repair and creating a favorable environment for infection [21].
Diabetic neuropathy
Neuropathy is one of the most prevalent complications in diabetic patients, significantly impacting sensory, motor, and autonomic functions [22]. More than 60% of diabetic foot ulcers (DFUs) are attributed to underlying neuropathy, with risk increasing proportionally to the duration of diabetes [23]. Damaged nerve endings impair pain perception, allowing unnoticed injuries to progress into ulcers [24]. Motor neuropathy contributes to foot deformities, while autonomic neuropathy results in dry, cracked skin that is more susceptible to injury and infection [25]. The combination of sensory, motor, and autonomic neuropathy leads to biomechanical imbalances in the foot, increasing the risk of ulceration and infection [26].
Diabetic angiopathy
Angiopathy, or vascular damage, is another critical factor in the pathogenesis of DFIs [14]. Hyperglycemia damages endothelial cells, leading to reduce NO production and increased vasoconstriction, platelet aggregation, and atherosclerosis [27]. Peripheral arterial disease, common in diabetic patients, impairs blood flow to the extremities, causing ischemia and delaying wound healing [28]. Atherosclerosis further complicates the condition by promoting vascular smooth muscle proliferation and platelet aggregation, leading to thrombosis and an increased risk of infections in ischemic tissues [29].
Traditional treatments for diabetic foot infections
Antibiotics and their limitations
Antibiotics remain the cornerstone of treatment for DFIs, with the choice of therapy guided by the infection's severity and the involved pathogens. For mild to moderate infections, oral antibiotics such as amoxicillin–clavulanate, clindamycin, or doxycycline are often sufficient to address common gram-positive bacteria like Staphylococcus aureus and Streptococcus species [30, 31]. In more severe cases, intravenous antibiotics, including vancomycin, piperacillin–tazobactam, and carbapenems, are necessary to cover a broader spectrum of pathogens, including gram-negative organisms and anaerobes [32]. Despite their importance, antibiotics face significant limitations. In diabetic patients with poor peripheral circulation, drug delivery to infected tissues is compromised, reducing efficacy [33]. In addition, bacterial biofilm formation, particularly by S. aureus, can shield pathogens from antibiotic action, leading to chronic, hard-to-treat infections [34]. Prolonged antibiotic use also introduces risks of adverse effects, such as gastrointestinal disturbances, nephrotoxicity, and hepatotoxicity, especially in older patients with multiple health issues [35].
The rise of multidrug-resistant bacteria
A major challenge in treating DFIs is the increasing prevalence of multidrug-resistant organisms (MDROs) [36]. Pathogens such as methicillin-resistant S. aureus (MRSA), extended-spectrum beta-lactamase producing gram-negative bacteria, and carbapenem-resistant Enterobacteriaceae are becoming more common [37, 38]. These resistant strains are difficult to treat with standard antibiotics, necessitating the use of more expensive or toxic alternatives like vancomycin, daptomycin, and polymyxins [39]. The rise in MDROs complicates treatment regimens, leading to prolonged hospitalizations, increased risk of severe complications like osteomyelitis and sepsis, and an overall greater healthcare burden [40, 41].
Surgical interventions and wound care
Surgical intervention is crucial in managing DFIs, particularly for infections involving deep tissue or bone, such as osteomyelitis [31]. Debridement, which involves the removal of necrotic tissue, is essential for reducing bacterial load and promoting wound healing [42]. In severe cases, amputation may be necessary to prevent the spread of infection and save the patient's life [43]. While amputation is a last resort, it has been shown to improve life expectancy in severe cases. Efforts to avoid amputation focus on limb-salvage procedures, such as revascularization, which can restore blood flow, enhance wound healing, and reduce complications [44]. Post-operative care is vital to improve mobility and quality of life following amputation [45].
Wound care complements antibiotics and surgical interventions in DFIs management. Specialized dressings, including hydrogels, hydrocolloids, and alginates, maintain a moist environment conducive to healing [46]. Antimicrobial dressings with silver or iodine help control bacterial growth and infection risk [47]. Negative pressure wound therapy applies controlled suction to the wound, promoting blood flow and reducing edema to accelerate tissue regeneration [48]. In addition, offloading devices, such as custom footwear or orthotics, are essential for redistributing pressure on ulcerated areas, particularly for patients with DFUs deformities. These devices prevent further damage and support faster recovery [49].
Despite the advances in surgical interventions and wound care, managing DFIs remains a significant challenge, particularly when deep tissues or bones are involved [50]. Surgical procedures, such as debridement and limb salvage techniques, are often complex and can carry risks, including delayed wound healing and recurrence of infection [51]. Moreover, the reliance on amputation in severe cases underscores the limitations of current treatments and the pressing need for more effective strategies to prevent infections from reaching such critical stages [52].
Natural products with antimicrobial properties
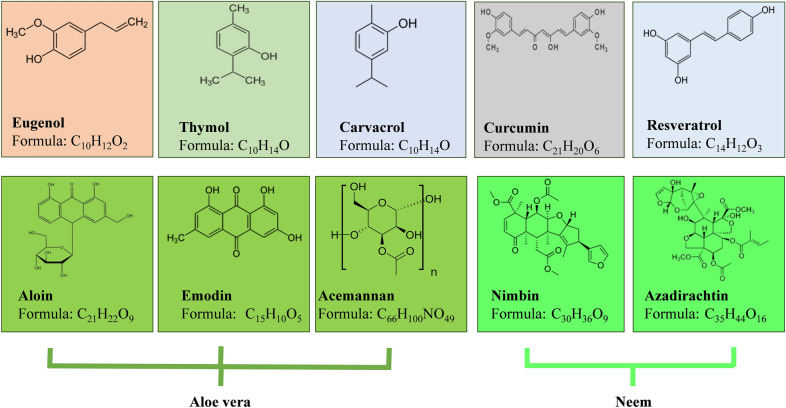
Natural products have long been recognized for their therapeutic potential, especially in combating infections. These products, derived from plants, herbs, and other natural sources, offer diverse chemical compounds that can serve as alternatives or complements to conventional pharmaceuticals (Fig. 2) [53]. Here, we highlight recent studies on the antimicrobial effects of natural products specifically applied to the management of DFIs (Tables 1 and 2).
Fig. 2.
Structure and chemical formula of active compounds in natural products
Table 1.
Overview of natural products research on bacterial diabetic foot infections
| Author(s) | Year | Substance | Function | Bacteria | References |
|---|---|---|---|---|---|
| Ali et al | 2022 | Eugenol | Antimicrobial, wound healing | Proteus mirabilis | [61] |
| Gupta et al | 2021 | Antifungal, wound healing | Candida spp. | [62] | |
| Obuotor et al | 2017 | Antimicrobial | Diabetic foot ulcer pathogens | [63] | |
| Salemi et al | 2024 | Thymol | Antimicrobial, reduces virulence gene expression | Staphylococcus aureus | [87] |
| Yuan et al | 2020 | Inhibits biofilm formation | MRSA | [88] | |
| Altememy et al | 2022 | Carvacrol | Wound healing, reduces inflammation | S. aureus | [100] |
| Taghavifar et al | 2022 | Curcumin | Wound healing, antimicrobial | MRSA | [114] |
| Muniz et al | 2021 | Antimicrobial, reduces inflammation | S. aureus | [115] | |
| Ali et al | 2018 | Aloe vera | Antimicrobial, wound healing | MRSA | [128] |
| Udgire et al | 2014 | Antibacterial, inhibits biofilm formation | Escherichia coli, S. aureus | [129] | |
| Arbab et al | 2021 | Antimicrobial, wound healing | Skin pathogens | [130] | |
| Chaturvedi et al | 2011 | Neem | Antimicrobial | S. aureus, Pseudomonas aeruginosa | [139] |
| Nishat Anzum et al | 2017 | Antimicrobial | S. aureus and Salmonella typhi | [140] | |
| Sarmiento et al | 2011 | Antimicrobial | MRSA | [141] | |
| Shevelev et al | 2020 | Resveratrol | Antimicrobial, wound healing | S. aureus, C. albicans | [157] |
Table 2.
Antimicrobial mechanisms of natural products
| Natural product | Antimicrobial mechanisms | References |
|---|---|---|
| Eugenol |
Disrupts bacterial membranes, causing leakage of intracellular components Inhibits cellular enzymes (e.g., protease, amylase, and ATPase) Induces production of reactive oxygen species (ROS), inhibiting cell growth and degrading DNA Enhances antimicrobial activity synergistically with conventional agents |
[54–59] |
| Thymol |
Disrupts bacterial cell membrane integrity, leading to leakage of intracellular contents and cell death Inhibits biofilm formation and induces bacterial autolysis Targets polysaccharide intracellular adhesin and extracellular DNA, enhancing antibiotic synergy |
[76–82] |
| Carvacrol |
Disrupts bacterial cell walls and membranes, increasing permeability and causing cytoplasmic leakage Inhibits cell wall enzymes, disrupting bacterial growth Causes rapid bactericidal effects and morphological changes in bacteria |
[95–97] |
| Curcumin |
Disrupts bacterial cell membranes, leading to leakage of cellular contents Inhibits quorum sensing, reducing bacterial virulence Synergizes with photodynamic therapy for antimicrobial effects |
[109, 110] |
| Aloe vera |
Anthraquinones (aloin and emodin) disrupt bacterial cell membranes and inhibit protein synthesis Physically damages bacterial cell walls, enhancing antimicrobial action Inhibits bacterial biofilm formation |
[124, 125] |
| Neem |
Disrupts bacterial cell membranes, causing leakage and cell death Inhibits bacterial protein synthesis and enzymatic activity. Prevents biofilm formation, enhancing antimicrobial efficacy |
[136–138] |
| Resveratrol |
Inhibits bacterial cell division by targeting FtsZ protein Compromises bacterial membrane integrity, causing leakage Disrupts DNA synthesis, quorum sensing, and metabolic pathways, reducing virulence and biofilm formation |
[148–151] |
Eugenol
Eugenol, a phenolic compound primarily found in clove oil, has garnered attention for its potent antimicrobial and anti-inflammatory properties, making it a promising candidate for the treatment of infections, particularly those complicated by antibiotic resistance [54, 55]. Structurally, eugenol features a free hydroxyl group and a hydrophobic aromatic ring, which contribute to its diverse biological activities [56].
The antimicrobial activity of eugenol is attributed to its ability to disrupt bacterial membranes, facilitated by its hydrophobic nature and the presence of a free hydroxyl group in its structure. This disruption compromises membrane integrity, causing leakage of intracellular components and ultimately leading to cell death [56, 57]. Eugenol also interacts with various cellular enzymes, inhibiting critical functions such as protease, amylase, and ATPase activity [58]. In addition, it induces the production of ROS, which can inhibit cell growth, damage membranes, and degrade DNA [59]. These multifaceted mechanisms enhance its effectiveness and also synergize with conventional antimicrobial agents [60].
Several studies have highlighted eugenol’s diverse applications. Ali et al. investigated the efficacy of clove flower extract (CFE), containing eugenol, against multidrug-resistant Proteus mirabilis isolated from DFUs. Their findings demonstrated that topical application of CFE hydrogel improved wound healing parameters, enhanced expression of growth factor signaling pathways, and reduced inflammatory cytokines, oxidative stress, and microbial load, suggesting CFE as a viable alternative to antibiotics for DFU therapy [61]. Gupta et al. developed eugenol-based nanofibers, with a focus on their dual wound-healing and antibiofilm properties. These nanofibers exhibited significant efficacy against Candida albicans, C. tropicalis, and other Candida species biofilms, and notably accelerated wound healing in vivo [62]. Similarly, Obuotor et al. examined the antimicrobial effects of essential oils from turmeric and clove on bacteria implicated in DFUs, including Salmonella paratyphi, S. arizona, Pseudomonas aeruginosa, P. fluorescens, Citrobacter species, Enterococcus faecalis, Enterobacter cloacae, P. mirabilis, P. vulgaris, Escherichia coli, S. aureus, Bacteroides fragilis, and Peptostreptococcus species. Their research revealed that clove oil, which is rich in eugenol, demonstrated the highest inhibitory activity, including against P. mirabilis, thereby highlighting its potential for developing natural antimicrobial agents [63].
Eugenol's anti-inflammatory activity is equally significant. It inhibits several pro-inflammatory mediators, including cytokines such as IL-1β, IL-6, and TNF-α, as well as pathways involving prostaglandins (PGE2), inducible nitric oxide synthase (iNOS), cyclooxygenase-2 (COX-2), and leukotrienes (5-LOX). These actions help reduce inflammation by modulating the immune response and limiting oxidative stress [64]. Eugenol also prevents chemotaxis of neutrophils and macrophages, thereby inhibiting inflammatory neurotransmitter synthesis (Fig. 3) [65].
Fig. 3.
Diverse anti-inflammatory mechanisms of seven natural products: eugenol, thymol, carvacrol, curcumin, Aloe vera, neem, and resveratrol
Bioinformatics studies suggest that eugenol's dual inhibition of COX-2 and 5-LOX could make it a promising natural alternative to nonsteroidal anti-inflammatory drugs for managing inflammatory diseases such as osteoarthritis or cancer [64]. Its anti-inflammatory properties further extend to blocking voltage-gated sodium channels in nerve cells, reducing pain perception, and offering potential analgesic benefits [66, 67].
Jiang et al. explored eugenol’s protective role in diabetes-induced muscle dysfunction, demonstrating that oral administration of eugenol at 10 mg/kg significantly reduced inflammation and insulin resistance while enhancing glucose uptake through GLUT4-AMPK signaling pathways [68]. Alharthy et al. evaluated the neuroprotective effects of isoeugenol and eugenol at 20 mg/kg in diabetic polyneuropathy, showing improvements in oxidative stress, inflammation, and behavioral deficits, with synergistic benefits observed in their combined use [69]. Trad et al. reported eugenol’s ability to improve insulin sensitivity, reduce hyperglycemia, and modulate GLUT4 and AMPK protein levels in diabetic rats treated with 10 mg/kg eugenol, supporting its role as a therapeutic agent for type 2 diabetes [70]. Finally, Qar et al. investigated eugenol's potential to mitigate diabetic cardiomyopathy, demonstrating that treatment with eugenol at 20 mg/kg effectively reduced myocardial oxidative stress, inflammation, fibrosis, and hyperglycemia, further establishing its therapeutic versatility [71].
Thymol
Thymol, a naturally occurring monoterpenoid phenol, is one of the primary bioactive components of thyme (Thymus vulgaris) and other aromatic plants [72]. Its chemical structure, characterized by a phenolic hydroxyl group attached to a hydrocarbon ring, underpins its biological activity [73]. Thymol has been extensively studied for its antimicrobial, anti-inflammatory, and antioxidant properties, which contribute to its therapeutic potential in managing infections, inflammatory conditions, and oxidative stress [74]. Beyond its traditional use in herbal medicine, thymol has gained recognition as a potent agent against various pathogens, including antibiotic-resistant strains, making it a valuable natural compound in the era of antimicrobial resistance [75].
The antimicrobial properties of thymol are broad-spectrum, encompassing bacteria, fungi, and even some viruses [76]. A critical mechanism of action is its ability to disrupt the integrity of bacterial cell membranes, attributed to its lipophilic nature [77]. This disruption compromises membrane permeability, causing leakage of intracellular components and leading to cell death. In addition, thymol inhibits biofilm formation, a protective strategy employed by many pathogens to evade antimicrobial agents, and can induce bacterial autolysis, further enhancing its effectiveness [78, 79]. Studies have shown that thymol-rich extracts are highly efficacious at low concentrations, emphasizing its potency [80, 81]. Furthermore, the antimicrobial activity of thyme oil, a primary source of thymol, varies with plant growth stages, correlating with fluctuations in thymol content, suggesting the significance of optimizing harvesting practices to maximize therapeutic efficacy [82].
Thymol has demonstrated anti-inflammatory effects by reducing the expression of pro-inflammatory cytokines, such as IL-1β, IL-6, TNF-α, and MCP-1, in cellular and animal models [83, 84]. It suppresses key inflammatory pathways, including the NF-κB pathway, by inhibiting phosphorylation of mediators like IKK, IκΒα, and NFκΒp65 [84]. These actions decrease downstream inflammatory markers such as PGE2, MCP-1, and IL-6. In clinical studies, thymol-containing varnishes have shown efficacy in reducing gingival inflammation and PGE2 levels [85]. Moreover, combinations of thymol and carvacrol reduce the production of IL-25, IL-33, and TSLP in bronchial epithelial cells, potentially through upregulation of negative regulators like SHIP-1 and SOCS-1 [86].
Salemi et al. synthesized chitosan and zinc oxide nanoparticles with thymol and tested their antimicrobial efficacy against S. aureus isolates from diabetic ulcers. The nanoparticles demonstrated strong antibacterial activity, significantly reducing bacterial growth and virulence gene expression [87]. Yuan et al. investigated the ability of thymol to inhibit biofilm formation and eradicate mature biofilms in MRSA. The study demonstrated that thymol could inhibit biofilm formation and eliminate established biofilms by reducing the production of polysaccharide intracellular adhesin and extracellular DNA (eDNA). The combined treatment of thymol and vancomycin showed greater efficacy in eradicating MRSA biofilms compared to vancomycin alone. Thymol also reduced inflammatory responses in a mouse infection model, lowering white blood cell counts and decreasing serum TNF-α and IL-6 levels [88].
Martirosyan et al. assessed the effects of thymol administration and low-level laser therapy on inflammatory and oxidative indicators in type 2 diabetes patients. In this study, the diabetic group was treated with thymol (25 mg/kg/day for 30 days). The results showed a significant reduction in inflammatory cytokines (TNF-α, IL-1β) and oxidative markers (malondialdehyde, hydrogen peroxide) in the thymol-treated group. In addition, thymol gel (0.5%) was studied for its potential to reduce dermatitis in the feet of diabetic patients, though this effect was not statistically significant. These findings suggest that thymol can aid in controlling diabetes-related complications through its antioxidant and anti-inflammatory properties [89]. Hamed Shosha et al. compared the therapeutic effects of T. vulgaris essential oil, which contains thymol, on peptic ulcers and ulcerative colitis (UC) induced by ethanol in rats. The study found that thymol-rich T. vulgaris essential oil significantly modulated oxidative stress markers, increasing glutathione (GSH) levels by 120.43% in the peptic ulcer model and reducing malondialdehyde levels by 20.05%. In addition, thymol treatment significantly decreased the inflammatory marker (PGE2) and restored stomach and colon function markers in both ulcer and UC models. These results highlight the potential of thymol as an effective treatment for ulcer-related diseases through its antioxidant and anti-inflammatory effects [90]. Oskouei et al. evaluated the positive and protective effects of thymol on streptozotocin-induced (STZ-induced) diabetic rats. In this study, thymol was administered at doses of 20 and 40 mg/kg. The results indicated significant anti-hypoglycemic and anti-hypolipidemic effects, as well as improvements in antioxidant enzyme levels in the liver and kidney. Thymol treatment also resulted in decreased levels of creatinine, low-density lipoprotein cholesterol, very low-density lipoprotein cholesterol, and liver function-related enzymes (AST and ALT), suggesting its potential as a protective agent against diabetic complications in animal models [91].
Carvacrol
Carvacrol, a monoterpenoid phenol derived from the essential oils of oregano (Origanum vulgare) and thyme (T. vulgaris), has garnered significant attention for its therapeutic potential [92]. Its unique structure, characterized by a hydroxyl group attached to a phenolic ring, grants it hydrophobic and reactive properties, enabling interactions with biological membranes and enzymes [93]. Carvacrol has demonstrated potent antimicrobial and anti-inflammatory activities, particularly in the context of chronic wound management, such as diabetic wounds [94]. Its multifaceted mechanisms of action make it a promising candidate for addressing both infections and inflammation associated with such conditions.
Carvacrol exhibits potent antimicrobial activity by interfering with the structural integrity of bacterial cell walls, leading to damage and cell death. It is believed to act by inhibiting the activity of cell wall enzymes, which disrupts the bacterial cell wall, thus inhibiting growth [95]. In addition, carvacrol induces rapid bactericidal effects by causing morphological changes and cytoplasmic leakage, resulting in cell damage [96]. This antimicrobial mechanism is further supported by carvacrol's ability to disrupt the cell membrane, increasing permeability and causing leakage of intracellular contents [96, 97].
In addition to its antimicrobial properties, carvacrol has shown significant anti-inflammatory effects. It protects cells against inflammation, oxidative stress, and apoptosis, particularly under conditions of high glucose levels. This protection is largely attributed to its ability to inhibit the transient receptor potential melastatin 2 (TRPM2) cation channel, which prevents excessive calcium influx and ROS generation [98]. Carvacrol also enhances the activity of antioxidant enzymes like glutathione and glutathione peroxidase, thereby reducing oxidative stress [98]. These anti-inflammatory properties are further evidenced by carvacrol’s ability to suppress the production of pro-inflammatory cytokines and markers such as IL-6, IL-8, ENA-78, GCP-2, PGE2, and COX-2 [99].
Several studies have explored carvacrol's effects in treating diabetic wounds and chronic infections. Altememy et al. evaluated the restorative effect of titanium dioxide nanoparticles (TiO2NPs) synthesized with O. vulgare, carvacrol, and other plant compounds on infected wounds in diabetic rats. The study found that treatment with TiO2NPs synthesized by carvacrol reduced wound microbial load and inflammation, accelerating wound healing compared to the control groups. The bacteria involved in the study was S. aureus (ATCC 12600), and the rats treated with carvacrol showed significant improvements in wound healing, including reduced size and microbial load, highlighting its potential as an effective remedy for chronic diabetic wounds [100]. Mir et al. further demonstrated the antimicrobial potential of carvacrol, especially when formulated into a nanoparticle delivery system for sustained release at infection sites. In their study, carvacrol-loaded poly (caprolactone) nanoparticles (PCL NPs) enhanced antimicrobial activity, with a 2–fourfold increase in efficacy compared to free carvacrol. The system also showed superior skin retention, with carvacrol-PCL NPs maintaining 83.8 ± 5.15% skin retention after 24 h [101].
In another study, Dezfuli et al. examined the use of carvacrol for managing diabetes-related complications. Diabetic rats were treated with 5, 10, or 15 mg/kg body weight/day of carvacrol, which significantly decreased levels of inflammatory markers like IL-1β, IL-6, and TNF-α, and improved antioxidant status by increasing the activities of enzymes such as catalase and superoxide dismutase. Notably, the 15 mg/kg dose showed the most pronounced effects, underscoring carvacrol's potential to mitigate inflammation and oxidative stress in diabetic conditions [102]. Marinelli et al. investigated the use of water-soluble carvacrol prodrugs (WSCPs) combined with hyaluronic acid (HA) to enhance wound healing. Their study demonstrated that WSCPs/HA formulations significantly increased the rate of wound closure compared to individual components. The formulations modulated inflammatory mediators, improving wound repair by regulating macrophage activity and promoting collagen synthesis [103].
Fauzian et al. focused on overcoming the challenges of carvacrol's hydrophobicity and potential skin irritation by formulating it into nanostructured lipid carriers (CAR–NLC). This formulation not only improved carvacrol’s stability and skin penetration but also enhanced its antimicrobial, antioxidant, and anti-inflammatory activities. The CAR–NLC showed superior wound healing in diabetic mice, with a 97.56% wound closure rate by day 15 [104].
Curcumin
Curcumin, a polyphenolic compound classified as a diarylheptanoid, is one of the primary curcuminoids derived from the rhizome of Curcuma longa, a plant commonly known as turmeric [105]. Turmeric has been extensively used in traditional medicine systems, particularly in Asia, due to its diverse therapeutic properties [106]. Curcumin is the most active bioactive component of turmeric, accounting for its characteristic yellow color and a wide range of pharmacological activities [107]. It has attracted significant scientific attention due to its potent antimicrobial, anti-inflammatory, and antioxidant properties, making it a promising candidate for managing various diseases, including chronic wounds such as DFUs [108].
One of its key antimicrobial actions is the disruption of bacterial cell membranes, leading to leakage of cellular contents and subsequent cell death. Curcumin also inhibits quorum sensing, a bacterial communication system that plays a critical role in virulence factor production, thus reducing bacterial pathogenicity [109]. Despite its promising effects, curcumin's therapeutic potential is limited by its poor bioavailability, resulting from rapid metabolism and low absorption [110].
In addition to its antimicrobial activity, curcumin exerts significant anti-inflammatory effects. It is a powerful inhibitor of NF-κB, a transcription factor involved in the regulation of inflammatory responses, by preventing its translocation to the nucleus and blocking the expression of pro-inflammatory mediators [111]. Curcumin also directly inhibits the activity of COX-2 and iNOS, enzymes responsible for the production of inflammatory compounds such as prostaglandins and NO [112]. Furthermore, curcumin demonstrates antioxidant properties by scavenging ROS, thereby protecting cells from oxidative damage and enhancing its antimicrobial effects [113]. It also modulates immune cell function, promoting a shift toward a less inflammatory phenotype, and interferes with key signaling pathways, including the MAPK cascade, involved in the inflammatory process [112].
Recent studies have provided further evidence of curcumin's efficacy in diabetic wound healing and its interaction with antimicrobial therapies. For example, Taghavifar et al. investigated the therapeutic potential of curcumin nanoparticles in diabetic wounds infected with MRSA. Their results indicated that curcumin nanoparticles, when combined with HAMLET (human α-lactalbumin made lethal to tumor cells), significantly improved wound healing in MRSA-infected diabetic wounds. The combination therapy, compared to other treatments, showed a remarkable reduction in bacterial load and improved histological parameters, including granulation tissue formation and collagen deposition [114]. Similarly, Muniz et al. explored the use of photodynamic therapy (PDT) with curcumin for treating MRSA infections in a diabetic mouse model. Their study found that PDT, when combined with curcumin, reduced bacterial load and inflammatory cytokine expression, offering an innovative strategy for managing chronic wound infections [115].
Moreover, Ranjbar-Mohammadi et al. demonstrated the potential of curcumin-loaded poly (ε-caprolactone) (PCL)/gum tragacanth nanofibers for wound healing in diabetic rats. These nanofibers exhibited antibacterial properties against both MRSA and extended-spectrum β-lactamase (ESBL) bacteria. The study highlighted the nanofibers' ability to accelerate wound closure, promote fibroblast proliferation, and enhance collagen deposition, which were not observed in untreated controls [116]. In addition, the study by Tong et al. introduced curcumin-loaded cellulose nanocrystal films as a drug delivery system for diabetic wound healing. These films exhibited sustained antimicrobial effects against various pathogens, including MRSA, and significantly reduced bacterial growth, thus promoting wound healing in diabetic rat models [117]. Finally, Sami et al. investigated the use of a combination of turmeric extract, oregano, and chitosan nanoparticles in wound care formulations for diabetic wound healing. Their findings demonstrated that this combination exhibited significant antibacterial activity against S. aureus and E. coli, with the potential for application in both diabetic and non-diabetic wounds. The ointment and hydrogel formulations, in particular, showed a marked improvement in wound healing compared to commercial dressings [118, 119].
Aloe vera
Aloe vera (L.) Burm. f., a succulent plant belonging to the Asphodelaceae family, has been valued for centuries for its medicinal properties [120]. The gel extracted from its leaves is rich in bioactive compounds, including polysaccharides, glycoproteins, enzymes, vitamins, and anthraquinones, which contribute to its diverse therapeutic effects [121]. In modern medicine, Aloe vera has garnered attention for its potent antimicrobial, anti-inflammatory, and wound-healing properties, making it a promising candidate for managing chronic wounds such as DFUs [122]. The plant's ability to modulate inflammation, combat microbial infections, and promote tissue repair underscores its relevance in addressing the complex pathophysiology of DFUs [123].
The antimicrobial activity of Aloe vera is largely attributed to anthraquinones, particularly aloin and emodin, which disrupt bacterial cell membranes and inhibit protein synthesis [124]. In addition, Aloe vera gel can physically damage bacterial cell walls, enhancing its antimicrobial effects [125]. On the anti-inflammatory front, acemannan, a key polysaccharide in Aloe vera, interacts with immune cells such as macrophages to suppress the production of pro-inflammatory cytokines like TNF-alpha, IL-1beta, and IL-6 [126]. Aloe vera also contains compounds that inhibit COX enzymes, reducing the synthesis of prostaglandins, which are key mediators of inflammation. Furthermore, studies indicate that Aloe vera modulates inflammatory signaling pathways by inhibiting the activation of transcription factors like NF-κB, thereby reducing overall inflammatory responses [127].
Ali et al. investigated the antibacterial activity of Aloe vera leaf aqueous extract against six MRSA strains. They demonstrated that concentrations of 15–20 mg/mL significantly reduced bacterial biomass dry weights after 24 and 48 h, with the strongest effects observed at 20 mg/mL. This concentration also showed inhibition of biofilm formation and produced the largest inhibition zones against S. aureus (LN871241), which was further confirmed using scanning electron microscopy [128]. Similarly, Udgire et al. demonstrated that Aloe vera extracts in various solvents showed antimicrobial activity against a range of gram-positive and gram-negative skin pathogens. Methanol extracts exhibited the highest activity, with zones of inhibition reaching 12 mm against S. aureus and S. epidermidis, followed by 10 mm against E. coli and P. vulgaris. These findings highlight Aloe vera’s potential as a natural antimicrobial agent [129].
Arbab et al. explored the antibacterial effects of Aloe vera gel and leaf extracts against pathogens causing skin infections, including E. coli, Shigella, Salmonella spp., and S. aureus. The study found that ethanol extracts from both the leaves and roots exhibited the highest antibacterial efficacy, showing potential as adjuncts to conventional antibiotics. Notably, the ethanol extracts were more effective than aqueous extracts, suggesting the solvent's role in enhancing bioactivity [130]. Bashir et al. supported these findings, showing that Aloe vera gel extracts displayed robust antibacterial activity against both gram-positive and gram-negative isolates obtained from wounds, burns, and acne patients. This antibacterial efficacy was comparable to or exceeded that of five broad-spectrum antibiotics tested alongside [131].
Valizadeh et al. developed an innovative Aloe vera-based nanoemulsion gel containing erythromycin (AVNE) to enhance topical bioavailability and accelerate wound healing. In diabetic and infected rat models, the AVNE significantly reduced inflammation, increased collagen synthesis, and promoted faster wound closure compared to controls. In addition, the formulation demonstrated potent antibacterial activity against E. coli and S. aureus, supporting its use in diabetic wound care [132].
Neem
Neem (Azadirachta indica), a medicinal plant native to the Indian subcontinent, has been celebrated for centuries in traditional medicine systems like Ayurveda for its wide-ranging therapeutic properties [133]. Modern pharmacological research has substantiated Neem’s efficacy, particularly its potent antimicrobial and anti-inflammatory effects, making it a promising candidate for managing various infections, including challenging conditions such as DFUs [134]. Neem’s diverse bioactive compounds, including nimbidin, nimbin, and azadirachtin, contribute to its multifaceted biological activities, offering both antimicrobial and anti-inflammatory benefits [135].
The antimicrobial efficacy of Neem arises from multiple complementary mechanisms. The bioactive compounds in Neem, including nimbidin, nimbin, and azadirachtin, have been shown to disrupt bacterial cell membranes, leading to cell leakage and eventual cell death [136]. These compounds also interfere with bacterial metabolic processes, inhibiting protein synthesis and enzymatic activity [137]. In addition, Neem has demonstrated the ability to inhibit biofilm formation, a key factor in bacterial virulence, making it effective against bacterial infections that are resistant to traditional antibiotics [138].
Recent studies have further expanded on Neem’s antimicrobial properties. Chaturvedi et al. investigated the antibacterial activities of crude Neem bark and leaf extracts against bacterial species isolated from clinical samples of diabetic individuals. Using the agar well diffusion method, they observed significant activity against both gram-positive and gram-negative bacteria, with coagulase-negative Staphylococcus (CONS) showing the highest inhibition zones. This suggests that Neem extracts, particularly in methanolic form, may hold promise in combating multidrug-resistant bacterial strains associated with diabetic infections [139]. Similarly, Nishat Anzum et al. evaluated the antimicrobial activities of commercially available Neem oil against pathogens such as S. aureus, Klebsiella pneumoniae, Bacillus cereus, and S. typhi. Their results showed that Neem oil exhibited over 99% growth inhibition for these pathogens, even at low concentrations, and was effective against P. aeruginosa using the dilution method. This highlights Neem’s potential as a natural antibiotic for managing infections caused by these bacteria [140].
Sarmiento et al. focused on Neem’s antibacterial efficacy against S. aureus, including MRSA. Neem leaf ethanol extracts exhibited a dose-dependent antibacterial activity, with significant inhibition zones at 100% concentration. While current antibiotics showed greater zones of inhibition, the study confirmed that Neem extracts hold promise as complementary or alternative antibacterial agents, particularly against antibiotic-resistant strains [141].
Neem’s anti-inflammatory mechanism involves inhibiting pro-inflammatory pathways by suppressing the production of inflammatory mediators such as TNF-alpha and IL-6. This is achieved through the modulation of key signaling molecules like NF-κB. In addition, Neem exhibits antioxidant properties by scavenging free radicals, thereby reducing oxidative stress that contributes to inflammation. Active compounds like nimbidin and azadirachtin play a significant role in these anti-inflammatory actions [142].
Thirukumaran et al. explored Neem’s anti-inflammatory and anti-diabetic properties. Their study demonstrated a dose-dependent positive correlation between the concentration of Neem extract and its efficacy in reducing inflammation and regulating blood glucose levels. This dual action makes Neem a potential candidate for managing inflammation and diabetic complications, especially in patients with comorbid conditions [143].
Resveratrol
Resveratrol, a naturally occurring polyphenol classified as a stilbene, is predominantly found in the skin of red grapes, berries, and products derived from these fruits, such as red wine and grape juice [144]. Known for its diverse pharmacological properties, resveratrol has garnered significant attention due to its potent antioxidant, anti-inflammatory, and antimicrobial activities [145]. Its capacity to modulate multiple molecular pathways makes it a promising therapeutic agent, particularly in the context of diabetes and its associated complications, including chronic wounds and infections [146]. The role of resveratrol in managing such complications is underpinned by its ability to target oxidative stress, inflammation, and microbial infection, all of which are critical factors in disease progression [147].
The antimicrobial activity of resveratrol is multifaceted and primarily involves the inhibition of FtsZ, a bacterial protein essential for cell division. By targeting FtsZ, resveratrol disrupts the assembly of the bacterial division machinery, leading to abnormal cell elongation, impaired cell wall synthesis, and eventual cell death. Beyond its effects on cell division, resveratrol compromises bacterial membrane integrity, causing structural damage and leakage of intracellular contents [148]. In addition, it interferes with quorum sensing, the bacterial communication system responsible for coordinating virulence factor production and biofilm formation, thereby diminishing bacterial pathogenicity [149]. Resveratrol’s antimicrobial mechanisms are further enhanced by its capacity to disrupt critical processes such as DNA synthesis and metabolic pathways, which may vary depending on the bacterial species [150, 151].
Resveratrol exerts its anti-inflammatory effects through several mechanisms. It inhibits the production of key inflammatory cytokines, including IL-1α, IL-6, TNF-α, and IL-17, by suppressing lymphocyte activation and macrophage function [152]. Resveratrol also downregulates inflammatory mediators such as COX-2, PGE2, and monocyte chemoattractant protein-1, particularly in response to lipopolysaccharide (LPS) stimulation [153, 154]. Furthermore, resveratrol attenuates the activation of inflammatory signaling pathways, including those involving Toll-like receptors (TLR-4) and NF-κB, thereby reducing the expression of pro-inflammatory proteins [155]. In addition, resveratrol suppresses the generation of ROS and NO, both of which contribute to inflammation, and enhances antioxidant activity, further alleviating inflammatory responses [156]. These actions highlight resveratrol’s potential as a therapeutic agent in controlling inflammation associated with various diseases.
Shevelev et al. investigated resveratrol’s antimicrobial activity against S. aureus and C. albicans in wound healing models. Resveratrol significantly reduced bacterial and fungal growth, promoting faster wound healing [157]. Chan et al. studied resveratrol’s dual antimicrobial and anti-inflammatory effects, demonstrating its efficacy in improving treatment outcomes for infections and inflammatory conditions [158].
Javid et al. examined resveratrol’s impact on diabetes management, noting improvements in glucose control and reduced oxidative stress [159]. Lee et al. explored resveratrol’s effects on inflammatory pathways in diabetic models, highlighting its potential to improve glucose metabolism and reduce diabetic complications [160].
Challenges and considerations in using natural products for treating diabetic foot infections
While natural products show significant promise in treating DFIs, several challenges and considerations must be addressed before they can be fully integrated into clinical practice. These challenges include variability in composition, lack of standardization, potential toxicity, and limited clinical evidence.
Variability in composition
The utilization of natural products in various industries, including pharmaceuticals, cosmetics, and food, presents a significant challenge due to the inherent variability in their chemical composition. This variability stems from a range of factors that can alter the concentration of bioactive compounds, thereby affecting the consistency, efficacy, and safety of natural product-based formulations. For instance, compounds such as thymol and carvacrol exhibit fluctuations in concentration depending on the species, geographical origin, and extraction methods employed [161–163]. Such variability complicates the standardization of natural product-derived therapeutics, potentially leading to inconsistent therapeutic outcomes and posing challenges for both regulatory compliance and consumer safety.
The primary source of variability in natural products is dependent on biological and environmental factors. Intra-species genetic variation plays a crucial role in the chemical profile of a plant, fungi, or microorganism, with different genotypes producing differing quantities or types of bioactive compounds [164]. This is exemplified by eugenol which may vary in concentration depending on the genetic lineage of the clove species and its growing conditions [165]. Environmental variables, such as soil composition, climate, and geographic location, further modulate the biosynthesis of secondary metabolites [166]. For example, factors such as temperature, humidity, and light exposure during plant growth can influence the yield and concentration of key compounds such as curcumin [167]. In addition, soil nutrients and mineral content can affect the biosynthesis of bioactive metabolites, leading to substantial differences in their concentrations [168].
Furthermore, the time of harvest and post-harvest processing play pivotal roles in the chemical composition of natural products [169]. The phenological stage at which a plant is harvested can alter the concentration of active compounds, as seen with curcumin, whose levels are influenced by the plant’s growth stage [170]. Post-harvest handling, including drying, storage, and transportation, can also result in the degradation, transformation, or volatilization of active compounds, further contributing to the variability of the final product. Natural products are typically complex mixtures of various bioactive molecules, with some compounds exhibiting higher variability in concentration than others [171]. This complexity presents a challenge for standardizing natural products, as it is difficult to achieve uniformity across different batches and sources of raw material.
To mitigate these challenges, several approaches have been developed. Standardization of natural product extracts, achieved by defining active ingredient levels, is commonly employed to reduce variability. In addition, advanced cultivation techniques, including controlled environmental conditions and optimized breeding programs, are utilized to minimize genetic and environmental influences on product composition. Post-harvest processing techniques, such as controlled drying and storage, can also help stabilize the chemical composition of natural products. In some cases, synthetic analogs or substitutes for natural compounds are developed to replicate the desired bioactivity, ensuring more consistent therapeutic outcomes. Despite these efforts, the inherent variability in natural products remains a significant challenge that requires ongoing research to address to optimize their application in various fields.
Lack of standardization and dosage guidelines
The lack of standardization and dosage guidelines is a significant challenge in the use of natural products, particularly in the treatment of conditions such as DFIs. Unlike conventional pharmaceuticals, which are subject to rigorous clinical trials and regulatory oversight, natural products often do not undergo the same level of scrutiny, leading to inconsistent quality and unclear therapeutic dosing. The absence of well-defined therapeutic doses for natural products complicates their integration into established treatment regimens, as healthcare providers may struggle to determine the appropriate quantity or frequency for safe and effective use. For example, while compounds like curcumin, eugenol, and thymol have demonstrated promising antimicrobial and anti-inflammatory properties, their efficacy is often contingent on factors such as extraction method, concentration, and bioavailability [172, 173]. Without standardized doses, patients may receive insufficient amounts of the active compound, leading to suboptimal therapeutic effects, or excessive amounts, resulting in toxicity or adverse reactions.
Furthermore, the experimental nature of many natural product-based therapies means that clinicians often lack comprehensive clinical guidelines to ensure optimal dosing and safety. Natural products are frequently used in combination with other medications, but the interactions between these compounds and conventional drugs are not always well understood. For example, curcumin may interact with drugs that affect liver enzymes, potentially altering their metabolism and efficacy [174]. The lack of clear guidelines for combining natural products with pharmaceuticals increases the risk of adverse effects, drug interactions, and compromised therapeutic outcomes. As natural products are integrated more into clinical practice, there is an urgent need for more rigorous research, standardized dosages, and comprehensive safety data to guide healthcare providers in their use.
To address these challenges, the development of standardized extracts with well-defined concentrations of active ingredients is essential. For example, standardized curcumin extracts with specified curcumin content have been introduced, enabling more reliable dosing in both clinical trials and therapeutic applications. In addition, dosage recommendations derived from robust clinical evidence would facilitate informed decision-making by healthcare providers regarding the use of natural products in treating DFIs and other conditions. Advances in drug delivery systems, such as nanoparticle-based formulations, may further enhance the bioavailability and precision of natural product administration. However, these innovations require rigorous evaluation to establish their safety and efficacy in clinical settings.
Conclusion
Natural products present a promising avenue for the treatment of DFIs, offering potent antimicrobial, anti-inflammatory, and wound-healing properties. Compounds derived from plants such as curcumin, Aloe vera, neem, and resveratrol have demonstrated significant efficacy in addressing the complex pathophysiology of DFIs, including infection control, inflammation modulation, and tissue regeneration. These properties make natural products a valuable addition to the therapeutic arsenal for managing chronic wounds, particularly in diabetic patients who are susceptible to persistent infections.
However, the integration of natural products into clinical practice is hindered by several challenges, including variability in composition, lack of standardization, and insufficient dosage guidelines. The chemical composition of natural products can vary significantly based on factors such as geographic origin, genetic variation, and extraction methods, which can impact their efficacy and safety. Furthermore, the absence of established therapeutic dosages and the potential for adverse drug interactions complicate their clinical application. Despite these challenges, continued research into standardization techniques, enhanced bioavailability, and clinical trial data will be essential for realizing the full therapeutic potential of natural products in treating DFIs.
Ultimately, while natural products hold considerable promise for advancing wound care in diabetic patients, further studies are needed to establish clear dosing regimens, safety profiles, and optimal formulations. Addressing these concerns will enable the broader adoption of these natural therapies in clinical settings, providing patients with safer, more effective alternatives for managing DFIs and improving overall quality of care.
Acknowledgements
The authors would like to acknowledge the Vice-Chancellor of Hamadan University of Medical Sciences for the support of the study.
Author contributions
MT, and MN conceived and designed the study. MN contributed to comprehensive research and wrote the paper. MT, and LS participated in editing the manuscript. All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
This study has been approved by the Ethics Committee of Hamadan University of Medical Sciences. Hamadan, Iran (IR.UMSHA.REC.1403.678).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Arokiasamy P, Salvi S, Selvamani Y. Global burden of diabetes mellitus. In: Kickbusch I, Ganten D, Moeti M, editors. Handbook of global health. Cham: Springer; 2021. p. 1–44. [Google Scholar]
- 2.Turzańska K, Adesanya O, Rajagopal A, Pryce MT, Fitzgerald Hughes D. Improving the management and treatment of diabetic foot infection: challenges and research opportunities. Int J Mol Sci. 2023;24(4):3913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, Song X, Ren Y, Shan P-F. Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025. Sci Rep. 2020;10(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu W, Song L, Sun W, Fang W, Wang C. Distribution of microbes and antimicrobial susceptibility in patients with diabetic foot infections in South China. Front Endocrinol. 2023;14:1113622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dörr S, Freier F, Schlecht M, Lobmann R. Bacterial diversity and inflammatory response at first-time visit in younger and older individuals with diabetic foot infection (DFI). Acta Diabetol. 2021;58:181–9. [DOI] [PubMed] [Google Scholar]
- 6.Peters E, Lipsky B, Aragón-Sánchez J, Boyko E, Diggle M, Embil J, Kono S, Lavery L, Senneville E, Urbančič-Rovan V. Interventions in the management of infection in the foot in diabetes: a systematic review. Diabetes Metab Res Rev. 2016;32:145–53. [DOI] [PubMed] [Google Scholar]
- 7.Singh T. Impact of antimicrobial resistance in diabetic foot infections. J Coast Life Med. 2023;11:487–502. [Google Scholar]
- 8.Liu E, Gao H, Zhao Y, Pang Y, Yao Y, Yang Z, Zhang X, Wang Y, Yang S, Ma X. The potential application of natural products in cutaneous wound healing: a review of preclinical evidence. Front Pharmacol. 2022;13:900439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qadir SU, Raja V. Herbal medicine: old practice and modern perspectives. In: Phytomedicine. Amsterdam: Elsevier; 2021. p. 149–80. [Google Scholar]
- 10.Chaachouay N, Zidane L. Plant-derived natural products: a source for drug discovery and development. Drugs and Drug Candidates. 2024;3(1):184–207. [Google Scholar]
- 11.Kim K, Mahajan A, Patel K, Syed S, Acevedo-Jake AM, Kumar VA. Materials and cytokines in the healing of diabetic foot ulcers. Adv Ther. 2021;4(9):2100075. [Google Scholar]
- 12.Prasathkumar M, Sadhasivam S. Chitosan/Hyaluronic acid/Alginate and an assorted polymers loaded with honey, plant, and marine compounds for progressive wound healing—Know-how. Int J Biol Macromol. 2021;186:656–85. [DOI] [PubMed] [Google Scholar]
- 13.Deng H, Li B, Shen Q, Zhang C, Kuang L, Chen R, Wang S, Ma Z, Li G. Mechanisms of diabetic foot ulceration: A review. J Diabetes. 2023;15(4):299–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim J. The pathophysiology of diabetic foot: a narrative review. J Yeungnam Med Sci. 2023;40(4):328–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Husain M, Agrawal YO. Antimicrobial remedies and emerging strategies for the treatment of diabetic foot ulcers. Curr Diabetes Rev. 2023;19(5):5–17. [DOI] [PubMed] [Google Scholar]
- 16.Zilliox LA. Diabetes and peripheral nerve disease. Clin Geriatr Med. 2021;37(2):253–67. [DOI] [PubMed] [Google Scholar]
- 17.González P, Lozano P, Ros G, Solano F. Hyperglycemia and oxidative stress: an integral, updated and critical overview of their metabolic interconnections. Int J Mol Sci. 2023;24(11):9352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang C, Zhao X, An X, Zhang Y, Sun W, Zhang Y, Duan Y, Kang X, Sun Y, Jiang L. Axonal transport deficits in the pathogenesis of diabetic peripheral neuropathy. Front Endocrinol. 2023;14:1136796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mishra S, Tiwari P, Yadav R, Patel PS. An extensive analysis of diseases associated with diabetes. J Pharma Insights Res. 2024;2(3):174–87. [Google Scholar]
- 20.Daryabor G, Atashzar MR, Kabelitz D, Meri S, Kalantar K. The effects of type 2 diabetes mellitus on organ metabolism and the immune system. Front Immunol. 2020;11:1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Deng L, Du C, Song P, Chen T, Rui S, Armstrong DG, Deng W. The role of oxidative stress and antioxidants in diabetic wound healing. Oxid Med Cell Longev. 2021;2021(1):8852759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sempere-Bigorra M, Julián-Rochina I, Cauli O. Differences and similarities in neuropathy in type 1 and 2 diabetes: a systematic review. J Pers Med. 2021;11(3):230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clayton W Jr, Elasy TA. A review of the pathophysiology, classification, and treatment of foot ulcers in diabetic patients. Clin Diabetes. 2009;27(2):52–8. [Google Scholar]
- 24.Singh S, Pai DR, Yuhhui C. Diabetic foot ulcer–diagnosis and management. Clin Res Foot Ankle. 2013;1(3):120. [Google Scholar]
- 25.Vinik AI. Management of neuropathy and foot problems in diabetic patients. Clin Cornerstone. 2003;5(2):38–55. [DOI] [PubMed] [Google Scholar]
- 26.Rebolledo FA, Soto JT, de la Peña JE. The pathogenesis of the diabetic foot ulcer: prevention and management. In: Dinh T, editor. Global perspective on diabetic foot ulcerations. London: Intechopen; 2011. p. 155–78. [Google Scholar]
- 27.Xu S, Ilyas I, Little PJ, Li H, Kamato D, Zheng X, Luo S, Li Z, Liu P, Han J. Endothelial dysfunction in atherosclerotic cardiovascular diseases and beyond: from mechanism to pharmacotherapies. Pharmacol Rev. 2021;73(3):924–67. [DOI] [PubMed] [Google Scholar]
- 28.Hinchliffe RJ, Forsythe RO, Apelqvist J, Boyko EJ, Fitridge R, Hong JP, Katsanos K, Mills JL, Nikol S, Reekers J. Guidelines on diagnosis, prognosis, and management of peripheral artery disease in patients with foot ulcers and diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36:e3276. [DOI] [PubMed] [Google Scholar]
- 29.Bravo GM, Annarapu G, Carmona E, Nawarskas J, Clark R, Novelli E, Alvidrez RIM. Platelets in thrombosis and atherosclerosis: a double-edged sword. Am J Pathol. 2024;194(9):1608–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.LaSalvia MT, Karchmer AW. Microbiology and treatment of diabetic foot infection. In: Veves A, Giurini JM, Schermerhorn ML, editors. The diabetic foot: medical and surgical management. Cham: Springer; 2024. p. 363–78. [Google Scholar]
- 31.Lipsky BA, Uçkay İ. Treating diabetic foot osteomyelitis: a practical state-of-the-art update. Medicina. 2021;57(4):339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baig MS, Banu A, Zehravi M, Rana R, Burle SS, Khan SL, Islam F, Siddiqui FA, Massoud EES, Rahman MH. An overview of diabetic foot ulcers and associated problems with special emphasis on treatments with antimicrobials. Life. 2022;12(7):1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bhardwaj H, Khute S, Sahu R, Jangde RK. Advanced drug delivery system for management of chronic diabetes wound healing. Curr Drug Targets. 2023;24(16):1239–59. [DOI] [PubMed] [Google Scholar]
- 34.Bonincontro G, Scuderi SA, Marino A, Simonetti G. Synergistic effect of plant compounds in combination with conventional antimicrobials against biofilm of staphylococcus aureus, pseudomonas aeruginosa, and Candida spp. Pharmaceuticals. 2023;16(11):1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Falcone M, Paul M, Tiseo G, Yahav D, Prendki V, Friberg LE, Guerri R, Gavazzi G, Mussini C, Tinelli M. Considerations for the optimal management of antibiotic therapy in elderly patients. J Glob Antimicrob Resist. 2020;22:325–33. [DOI] [PubMed] [Google Scholar]
- 36.Henig O, Pogue JM, Martin E, Hayat U, Jaara M, Kilgore PE, Cha R, Dhar S, Kaye KS. The impact of multidrug-resistant organisms on outcomes in patients with diabetic foot infections. Open Forum Infect Dis. 2020. 10.1093/ofid/ofaa161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Uivaraseanu B, Bungau S, Tit DM, Fratila O, Rus M, Maghiar TA, Maghiar O, Pantis C, Vesa CM, Zaha DC. Clinical, pathological and microbiological evaluation of diabetic foot syndrome. Medicina. 2020;56(8):380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nazari M, Azizi O, Solgi H, Fereshteh S, Shokouhi S, Badmasti F. Emergence of carbapenem resistant Acinetobacter baumannii clonal complexes CC2 and CC10 among fecal carriages in an educational hospital. Int J Environ Health Res. 2022;32(7):1478–88. [DOI] [PubMed] [Google Scholar]
- 39.Alaoui Mdarhri H, Benmessaoud R, Yacoubi H, Seffar L, Guennouni Assimi H, Hamam M, Boussettine R, Filali-Ansari N, Lahlou FA, Diawara I. Alternatives therapeutic approaches to conventional antibiotics: advantages, limitations and potential application in medicine. Antibiotics. 2022;11(12):1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Robben PM, Ayalew MD, Chung KK, Ressner RA. Multi-drug–resistant organisms in burn infections. Surg Infect. 2021;22(1):103–12. [DOI] [PubMed] [Google Scholar]
- 41.Hemmati J, Nazari M, Ahmadi A, Bayati M, Jalili M, Taheri M, Mohammadi Y, Asghari B. In vitro evaluation of biofilm phenotypic and genotypic characteristics among clinical isolates of Pseudomonas aeruginosa in Hamadan, West of Iran. J Appl Genet. 2024;65(1):213–22. [DOI] [PubMed] [Google Scholar]
- 42.Cazander G, den Ottelander BK, Kamga S, Doomen MC, Damen TH, van Well AME. Importance of debriding and wound cleansing agents in wound healing. In: Boateng J, editor. Therapeutic dressings and wound healing applications. Hoboken: Wiley; 2020. p. 59–89. [Google Scholar]
- 43.Frykberg RG, Attinger C, Smeets L, Koller A, Bal A, Kavarthapu V. Surgical strategies for prevention of amputation of the diabetic foot. J Clin Orthop Trauma. 2021;17:99–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Caetano AP, Conde Vasco I, Veloso Gomes F, Costa NV, Luz JH, Spaepen E, Formiga A, Coimbra E, Neves J, Bilhim T. Successful revascularization has a significant impact on limb salvage rate and wound healing for patients with diabetic foot ulcers: single-centre retrospective analysis with a multidisciplinary approach. Cardiovasc Intervent Radiol. 2020;43(10):1449–59. [DOI] [PubMed] [Google Scholar]
- 45.Ntloko S, Mayo A, Derbakova A, Kayssi A. A quality improvement initiative to decrease the incidence of post-operative wound complications following minor level amputations. Innov Innov More Innov. 2022. 10.56885/PLWR6547. [Google Scholar]
- 46.Freeman-Parry LE. Antimicrobial properties of wound dressings. Sheffield: Sheffield Hallam University; 2020. [Google Scholar]
- 47.Ma S, Frecklington M, Stewart S. The use of antimicrobial dressings for the management of diabetic foot ulcers: a survey of podiatrists in Aotearoa New Zealand. J Foot Ankle Res. 2024;17(2):e12032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Campitiello F, Mancone M, Corte AD, Guerniero R, Canonico S. Expanded negative pressure wound therapy in healing diabetic foot ulcers: a prospective randomised study. J Wound Care. 2021;30(2):121–9. [DOI] [PubMed] [Google Scholar]
- 49.Lazzarini PA, Jarl G. Knee-high devices are gold in closing the foot ulcer gap: a review of offloading treatments to heal diabetic foot ulcers. Medicina. 2021;57(9):941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Peters EJ, Lipsky BA, Senneville E, Abbas ZG, Aragón-Sánchez J, Diggle M, Embil JM, Kono S, Lavery LA, Malone M. Interventions in the management of infection in the foot in diabetes: a systematic review. Diabetes Metab Res Rev. 2020;36:e3282. [DOI] [PubMed] [Google Scholar]
- 51.Geierlehner A, Horch RE, Müller-Seubert W, Arkudas A, Ludolph I. Limb salvage procedure in immunocompromised patients with therapy-resistant leg ulcers—the value of ultra-radical debridement and instillation negative-pressure wound therapy. Int Wound J. 2020;17(5):1496–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Delgado IOS, Amaro GS, Barragán AdJL, Tapia AKG, Rivera EJG, Gonzalez IYP, Bravo VMM. Amputation VS revascularization in a patient with diabetic foot. Int J Med Sci Clin Res Stud. 2023;3(10):2269–72. [Google Scholar]
- 53.Dzobo K. The role of natural products as sources of therapeutic agents for innovative drug discovery. Comprehensive pharmacology. Amsterdam: Elsevier; 2022. p. 408. [Google Scholar]
- 54.Ulanowska M, Olas B. Biological properties and prospects for the application of eugenol—a review. Int J Mol Sci. 2021;22(7):3671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Didehdar M, Chegini Z, Shariati A. Eugenol: A novel therapeutic agent for the inhibition of Candida species infection. Front Pharmacol. 2022;13:872127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Marchese A, Barbieri R, Coppo E, Orhan IE, Daglia M, Nabavi SF, Izadi M, Abdollahi M, Nabavi SM, Ajami M. Antimicrobial activity of eugenol and essential oils containing eugenol: a mechanistic viewpoint. Crit Rev Microbiol. 2017;43(6):668–89. [DOI] [PubMed] [Google Scholar]
- 57.Devi KP, Nisha SA, Sakthivel R, Pandian SK. Eugenol (an essential oil of clove) acts as an antibacterial agent against Salmonella typhi by disrupting the cellular membrane. J Ethnopharmacol. 2010;130(1):107–15. [DOI] [PubMed] [Google Scholar]
- 58.Gill A, Holley R. Inhibition of membrane bound ATPases of Escherichia coli and Listeria monocytogenes by plant oil aromatics. Int J Food Microbiol. 2006;111(2):170–4. [DOI] [PubMed] [Google Scholar]
- 59.Hyldgaard M, Mygind T, Meyer RL. Essential oils in food preservation: mode of action, synergies, and interactions with food matrix components. Front Microbiol. 2012;3:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mak K-K, Kamal M, Ayuba S, Sakirolla R, Kang Y-B, Mohandas K, Balijepalli M, Ahmad S, Pichika M. A comprehensive review on eugenol’s antimicrobial properties and industry applications: a transformation from ethnomedicine to industry. Pharmacogn Rev. 2019;13(25):1–9. [Google Scholar]
- 61.Ali R, Khamis T, Enan G, El-Didamony G, Sitohy B, Abdel-Fattah G. The healing capability of clove flower extract (CFE) in streptozotocin-induced (STZ-induced) diabetic rat wounds infected with multidrug resistant bacteria. Molecules. 2022;27(7):2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gupta P, Mishra P, Mehra L, Rastogi K, Prasad R, Mittal G, Poluri KM. Eugenol-acacia gum-based bifunctional nanofibers as a potent antifungal transdermal substitute. Nanomedicine. 2021;16(25):2269–89. [DOI] [PubMed] [Google Scholar]
- 63.Obuotor T, Sarumi O, Anibaba O, Adeniyi P, Shittu O. Efficacy of the essential oils of curcuma longa and Syzygium Aromaticum against bacteria implicated in diabetic foot ulcers. IOSR J Pharm Biol Sci. 2017;12(1):21–8. [Google Scholar]
- 64.de Andrade FDCP, Mendes AN. Computational analysis of eugenol inhibitory activity in lipoxygenase and cyclooxygenase pathways. Sci Rep. 2020;10(1):16204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pytko-Polończyk J, Muszyńska B. Surowce naturalne w stomatologii. Med Int Rev. 2016;27(2):68–75. [Google Scholar]
- 66.Park C-K, Li H, Yeon K-Y, Jung S, Choi S-Y, Lee S, Lee S, Park K, Kim J, Oh S. Eugenol inhibits sodium currents in dental afferent neurons. J Dent Res. 2006;85(10):900–4. [DOI] [PubMed] [Google Scholar]
- 67.Hwang S-M, Lee K, Im S-T, Go EJ, Kim YH, Park C-K. Co-application of eugenol and QX-314 elicits the prolonged blockade of voltage-gated sodium channels in nociceptive trigeminal ganglion neurons. Biomolecules. 2020;10(11):1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jiang Y, Feng C, Shi Y, Kou X, Le G. Eugenol improves high-fat diet/streptomycin-induced type 2 diabetes mellitus (T2DM) mice muscle dysfunction by alleviating inflammation and increasing muscle glucose uptake. Front Nutr. 2022;9:1039753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Alharthy KM, Balaha MF, Devi S, Altharawi A, Yusufoglu HS, Aldossari RM, Alam A, Di Giacomo V. Ameliorative effects of isoeugenol and eugenol against impaired nerve function and inflammatory and oxidative mediators in diabetic neuropathic rats. Biomedicines. 2023;11(4):1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Al-Trad B, Alkhateeb H, Alsmadi W, Al-Zoubi M. Eugenol ameliorates insulin resistance, oxidative stress and inflammation in high fat-diet/streptozotocin-induced diabetic rat. Life Sci. 2019;216:183–8. [DOI] [PubMed] [Google Scholar]
- 71.Qar J, Al-Trad B, Muhaidat R, Omari S, Al-Omari G. The effect of eugenol treatment on diabetic cardiomyopathy in streptozotocin-induced diabetic rats. Biomed Pharmacol J. 2022;15(5):623–33. [Google Scholar]
- 72.Naghdi Badi H, Abdollahi M, Mehrafarin A, Ghorbanpour M, Tolyat S, Qaderi A, Ghiaci Yekta M. An overview on two valuable natural and bioactive compounds, thymol and carvacrol, in medicinal plants. J Med Plants. 2017;16(63):1–32. [Google Scholar]
- 73.Quideau S, Deffieux D, Douat-Casassus C, Pouységu L. Plant polyphenols: chemical properties, biological activities, and synthesis. Angew Chem Int Ed. 2011;50(3):586–621. [DOI] [PubMed] [Google Scholar]
- 74.Nagoor Meeran MF, Javed H, Al Taee H, Azimullah S, Ojha SK. Pharmacological properties and molecular mechanisms of thymol: prospects for its therapeutic potential and pharmaceutical development. Front Pharmacol. 2017;8:380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dhama K, Tiwari R, Chakraborty S, Saminathan M, Kumar A, Karthik K, Wani MY, Amarpal S, Rahal A. Evidence based antibacterial potentials of medicinal plants and herbs countering bacterial pathogens especially in the era of emerging drug resistance: an integrated update. Int J Pharmacol. 2014;10(1):1–43. [Google Scholar]
- 76.Šovljanski O, Kljakić AC, Tomić A. Antibacterial and antifungal potential of plant secondary metabolites. In: Mérillon J-M, Ramawat KG, editors. Plant specialized metabolites: phytochemistry, ecology and biotechnology. Cham: Springer; 2023. p. 1–43. [Google Scholar]
- 77.Murínová S, Dercová K. Response mechanisms of bacterial degraders to environmental contaminants on the level of cell walls and cytoplasmic membrane. Int J Microbiol. 2014;2014(1):873081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kowalczyk A, Przychodna M, Sopata S, Bodalska A, Fecka I. Thymol and thyme essential oil—new insights into selected therapeutic applications. Molecules. 2020;25(18):4125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Khan ST, Khan M, Ahmad J, Wahab R, Abd-Elkader OH, Musarrat J, Alkhathlan HZ, Al-Kedhairy AA. Thymol and carvacrol induce autolysis, stress, growth inhibition and reduce the biofilm formation by Streptococcus mutans. AMB Express. 2017;7:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Perez AP, Perez N, Lozano CMS, Altube MJ, de Farias MA, Portugal RV, Buzzola F, Morilla MJ, Romero EL. The anti MRSA biofilm activity of Thymus vulgaris essential oil in nanovesicles. Phytomedicine. 2019;57:339–51. [DOI] [PubMed] [Google Scholar]
- 81.Thosar N, Basak S, Bahadure RN, Rajurkar M. Antimicrobial efficacy of five essential oils against oral pathogens: an in vitro study. Eur J Dent. 2013;7:S071–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Pandur E, Micalizzi G, Mondello L, Horváth A, Sipos K, Horváth G. Antioxidant and anti-inflammatory effects of thyme (Thymus vulgaris L.) essential oils prepared at different plant phenophases on Pseudomonas aeruginosa LPS-activated THP-1 macrophages. Antioxidants. 2022;11(7):1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kwon HI, Jeong NH, Kim SY, Kim MH, Son JH, Jun SH, Kim S, Jeon H, Kang SC, Kim SH. Inhibitory effects of thymol on the cytotoxicity and inflammatory responses induced by Staphylococcus aureus extracellular vesicles in cultured keratinocytes. Microb Pathog. 2019;134:103603. [DOI] [PubMed] [Google Scholar]
- 84.Wang Q, Cheng F, Xu Y, Zhang J, Qi J, Liu X, Wang R. Thymol alleviates lipopolysaccharide-stimulated inflammatory response via downregulation of RhoA-mediated NF-κB signalling pathway in human peritoneal mesothelial cells. Eur J Pharmacol. 2018;833:210–20. [DOI] [PubMed] [Google Scholar]
- 85.Sköld K, Twetman S, Hallgren A, Yucel-Lindberg T, Modeer T. Effect of a chlorhexidine. Eur J Oral Sci. 1998;106:571–5. [DOI] [PubMed] [Google Scholar]
- 86.Khosravi AR, Erle DJ. Chitin-induced airway epithelial cell innate immune responses are inhibited by carvacrol/thymol. PLoS ONE. 2016;11(7):e0159459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Najafabadi SS, Doudi M, Tahmourespour A, Amiri G, Rezayatmand Z. Assessment of Antimicrobial Activity of Chitosan, ZnO, and Urtica dioica–ZnO NPs Against Staphylococcus aureus Isolated from Diabetic Ulcers. Curr Microbiol. 2024;81(9):295. [DOI] [PubMed] [Google Scholar]
- 88.Yuan Z, Dai Y, Ouyang P, Rehman T, Hussain S, Zhang T, Yin Z, Fu H, Lin J, He C. Thymol inhibits biofilm formation, eliminates pre-existing biofilms, and enhances clearance of methicillin-resistant Staphylococcus aureus (MRSA) in a mouse peritoneal implant infection model. Microorganisms. 2020;8(1):99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Martirosyan D, Jahanbakhshi F, Ashoori MR, Alkhamis S, Pezeshki S, Mikaeili AS, Mirmiranpour H. Effect of oral administration and topical gel application of thymol and low-level laser therapy on oxidative stress, inflammatory biomarkers and dermatitis in patients with type 2 diabetes mellitus. Bioactive Compd Health Dis. 2022;5(4):93–105. [Google Scholar]
- 90.Shosha NNH, Fahmy NM, Singab ANB, Mohamed RW. Anti-ulcer effects of cumin (Cuminum cyminum L.), thyme (Thymus vulgaris L.), and caraway (Carum carvi L.) essential oils on peptic ulcer and ulcerative colitis models in rats. J Herbmed Pharmacol. 2022;11(3):389–400. [Google Scholar]
- 91.Oskouei BG, Abbaspour-Ravasjani S, Musavinejad SJ, Salehzadeh SA, Abdolhosseinzadeh A, Ghahremanzadeh K, Shokouhi B. In vivo evaluation of anti-hyperglycemic, anti-hyperlipidemic and anti-oxidant status of liver and kidney of thymol in STZ-induced diabetic rats. Drug research. 2019;69(01):46–52. [DOI] [PubMed] [Google Scholar]
- 92.Lombrea A, Antal D, Ardelean F, Avram S, Pavel IZ, Vlaia L, Mut A-M, Diaconeasa Z, Dehelean CA, Soica C. A recent insight regarding the phytochemistry and bioactivity of Origanum vulgare L. essential oil. Int J Mol Sci. 2020;21(24):9653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Retnosari R, Ali AH, Zainalabidin S, Ugusman A, Oka N, Latip J. The recent discovery of a promising pharmacological scaffold derived from carvacrol: a review. Bioorg Med Chem Lett. 2024;109:129826. [DOI] [PubMed] [Google Scholar]
- 94.Cicalău GIP, Babes PA, Calniceanu H, Popa A, Ciavoi G, Iova GM, Ganea M, Scrobotă I. Anti-inflammatory and antioxidant properties of carvacrol and magnolol, in periodontal disease and diabetes mellitus. Molecules. 2021;26(22):6899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Soković M, Glamočlija J, Marin PD, Brkić D, Van Griensven LJ. Antibacterial effects of the essential oils of commonly consumed medicinal herbs using an in vitro model. Molecules. 2010;15(11):7532–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wijesundara NM, Lee SF, Cheng Z, Davidson R, Rupasinghe HV. Carvacrol exhibits rapid bactericidal activity against Streptococcus pyogenes through cell membrane damage. Sci Rep. 2021;11(1):1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Magi G, Marini E, Facinelli B. Antimicrobial activity of essential oils and carvacrol, and synergy of carvacrol and erythromycin, against clinical, erythromycin-resistant Group A Streptococci. Front Microbiol. 2015;6:165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Daldal H, Nazıroğlu M. Carvacrol protects the ARPE19 retinal pigment epithelial cells against high glucose-induced oxidative stress, apoptosis, and inflammation by suppressing the TRPM2 channel signaling pathways. Graefes Arch Clin Exp Ophthalmol. 2022;260(8):2567–83. [DOI] [PubMed] [Google Scholar]
- 99.Wijesundara NM, Lee SF, Davidson R, Cheng Z, Rupasinghe HV. Carvacrol suppresses inflammatory biomarkers production by lipoteichoic acid-and peptidoglycan-stimulated human tonsil epithelial cells. Nutrients. 2022;14(3):503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Altememy D, Darvishi M, Shokri S, Abbaszadeh S. The restorative effect of titanium dioxide nanoparticles synthesized with Origanum vulgare l., Carvacrol, Hypericum perforatum l., and hypericin loaded in calcium alginate scaffold on Staphylococcus aureus-infected ulcers in diabetic rats. Adv Anim Vet Sci. 2022;10(11):2285–93. [Google Scholar]
- 101.Mir M, Permana AD, Ahmed N, Khan GM, Rehman A, Donnelly RF. Enhancement in site-specific delivery of carvacrol for potential treatment of infected wounds using infection responsive nanoparticles loaded into dissolving microneedles: A proof of concept study. Eur J Pharm Biopharm. 2020;147:57–68. [DOI] [PubMed] [Google Scholar]
- 102.Tabibzadeh Dezfuli S, Ehsani M, Lakzaei Azar O. Modulation effects of carvacrol on inflammatory and antioxidant system’s gene expression of diabetic rats. GMJ Med. 2024;3(2):53–7. [Google Scholar]
- 103.Marinelli L, Cacciatore I, Costantini E, Dimmito MP, Serra F, Di Stefano A, Reale M. Wound-healing promotion and anti-inflammatory properties of carvacrol prodrugs/hyaluronic acid formulations. Pharmaceutics. 2022;14(7):1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Fauzian F, Garmana AN, Mauludin R. The efficacy of carvacrol loaded nanostructured lipid carrier in improving the diabetic wound healing activity: In vitro and in vivo studies. J Appl Pharm Sci. 2024;14(3):231–43. [Google Scholar]
- 105.Fuloria S, Mehta J, Chandel A, Sekar M, Rani NNIM, Begum MY, Subramaniyan V, Chidambaram K, Thangavelu L, Nordin R. A comprehensive review on the therapeutic potential of Curcuma longa Linn in relation to its major active constituent curcumin. Front Pharmacol. 2022;13:820806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Debjit Bhowmik C, Kumar K, Chandira M, Jayakar B. Turmeric: a herbal and traditional medicine. Arch Appl Sci Res. 2009;1(2):86–108. [Google Scholar]
- 107.Meng F-C, Zhou Y-Q, Ren D, Wang R, Wang C, Lin L-G, Zhang X-Q, Ye W-C, Zhang Q-W. Turmeric: A review of its chemical composition, quality control, bioactivity, and pharmaceutical application. In: Grumezescu AM, Holban AM, editors. Natural and artificial flavoring agents and food dyes. Amsterdam: Elsevier; 2018. p. 299–350. [Google Scholar]
- 108.Abd El-Hack ME, El-Saadony MT, Swelum AA, Arif M, Abo Ghanima MM, Shukry M, Noreldin A, Taha AE, El-Tarabily KA. Curcumin, the active substance of turmeric: its effects on health and ways to improve its bioavailability. J Sci Food Agric. 2021;101(14):5747–62. [DOI] [PubMed] [Google Scholar]
- 109.Hussain Y, Alam W, Ullah H, Dacrema M, Daglia M, Khan H, Arciola CR. Antimicrobial potential of curcumin: therapeutic potential and challenges to clinical applications. Antibiotics. 2022;11(3):322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Anand P, Kunnumakkara AB, Newman RA, Aggarwal BB. Bioavailability of curcumin: problems and promises. Mol Pharm. 2007;4(6):807–18. [DOI] [PubMed] [Google Scholar]
- 111.Zhang J, Zheng Y, Luo Y, Du Y, Zhang X, Fu J. Curcumin inhibits LPS-induced neuroinflammation by promoting microglial M2 polarization via TREM2/TLR4/NF-κB pathways in BV2 cells. Mol Immunol. 2019;116:29–37. [DOI] [PubMed] [Google Scholar]
- 112.Garufi A, Giorno E, Gilardini Montani MS, Pistritto G, Crispini A, Cirone M, D’Orazi G. p62/SQSTM1/Keap1/NRF2 axis reduces cancer cells death-sensitivity in response to Zn (II)–curcumin complex. Biomolecules. 2021;11(3):348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Wal P, Saraswat N, Pal RS, Wal A, Chaubey M. A detailed insight of the anti-inflammatory effects of curcumin with the assessment of parameters, sources of ROS and associated mechanisms. Open Med J. 2019;6(1):64. [Google Scholar]
- 114.Taghavifar S, Afroughi F, Saadati Keyvan M. Curcumin nanoparticles improved diabetic wounds infected with methicillin-resistant Staphylococcus aureus sensitized with HAMLET. Int J Low Extrem Wounds. 2022;21(2):141–53. [DOI] [PubMed] [Google Scholar]
- 115.Muniz IPR, Galantini MPL, Ribeiro IS, Gonçalves CV, Dos Santos DP, Moura TC, Silva ES, Silva NR, Cipriano BP, Correia TML. Antimicrobial photodynamic therapy (aPDT) with curcumin controls intradermal infection by Staphylococcus aureus in mice with type 1 diabetes mellitus: a pilot study. J Photochem Photobiol, B. 2021;224:112325. [DOI] [PubMed] [Google Scholar]
- 116.Ranjbar-Mohammadi M, Rabbani S, Bahrami SH, Joghataei M, Moayer F. Antibacterial performance and in vivo diabetic wound healing of curcumin loaded gum tragacanth/poly (ε-caprolactone) electrospun nanofibers. Mater Sci Eng, C. 2016;69:1183–91. [DOI] [PubMed] [Google Scholar]
- 117.Tong WY, Bin Abdullah AYK, Binti Rozman NAS, Bin Wahid MIA, Hossain MS, Ring LC, Lazim Y, Tan W-N. Antimicrobial wound dressing film utilizing cellulose nanocrystal as drug delivery system for curcumin. Cellulose. 2018;25:631–8. [Google Scholar]
- 118.Sami DG, Abdellatif A, Azzazy HM. Turmeric/oregano formulations for treatment of diabetic ulcer wounds. Drug Dev Ind Pharm. 2020;46(10):1613–21. [DOI] [PubMed] [Google Scholar]
- 119.Vidhya CS, Kalaimani PS, Sharma A, Magrey AH, Panik RK. Enhanced wound care solutions: Harnessing cellulose acetate-EUSOL/polyvinyl alcohol-curcumin electrospun dressings for diabetic foot ulcer treatment. Plant Sci Arch. 2022. 10.5147/PSA.2022.7.4.05. [Google Scholar]
- 120.Joseph B, Raj SJ. Pharmacognostic and phytochemical properties of Aloe vera linn an overview. Int J Pharm Sci Rev Res. 2010;4(2):106–10. [Google Scholar]
- 121.Babu SN, Noor A. Bioactive constituents of the genus Aloe and their potential therapeutic and pharmacological applications: a review. J Appl Pharm Sci. 2020;10(11):133–45. [Google Scholar]
- 122.Hetta HF, Elsaghir A, Sijercic VC, Akhtar MS, Gad SA, Moses A, Zeleke MS, Alanazi FE, Ahmed AK, Ramadan YN. Mesenchymal stem cell therapy in diabetic foot ulcer: an updated comprehensive review. Health Sci Rep. 2024;7(4):e2036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Pathak D, Mazumder A. A critical overview of challenging roles of medicinal plants in improvement of wound healing technology. Daru. 2024;32(1):379–419. [DOI] [PMC free article] [PubMed]
- 124.Forno-Bell N, Bucarey SA, García D, Iragüen D, Chacón O, Martin BS. Antimicrobial effects caused by aloe barbadensis miller on bacteria associated with mastitis in dairy cattle. Nat Prod Commun. 2019;14(12):1934578X19896670. [Google Scholar]
- 125.Chelu M, Musuc AM, Aricov L, Ozon EA, Iosageanu A, Stefan LM, Prelipcean A-M, Popa M, Moreno JC. Antibacterial Aloe vera based biocompatible hydrogel for use in dermatological applications. Int J Mol Sci. 2023;24(4):3893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mosayebi G, Ghazavi A, Aghili B, Mirshafiei A. Immunomodulating activity of Aloe Vera in animal model of multiple sclerosis. J Arak Univ Med Sci. 2009;12(3):109–15. [Google Scholar]
- 127.Boudreau MD, Beland FA. An evaluation of the biological and toxicological properties of Aloe barbadensis (miller), Aloe vera. J Environ Sci Health C. 2006;24(1):103–54. [DOI] [PubMed] [Google Scholar]
- 128.Saddiq AA, Al-Ghamdi H. Aloe vera extract: a novel antimicrobial and antibiofilm against methicillin resistant Staphylococcus aureus strains. Pak J Pharm Sci. 2018;31:2123. [PubMed] [Google Scholar]
- 129.Udgire M, Pathade G. Antibacerial activity of Aloe vera against skin pathogens. Am J Ethnomed. 2014;1(3):147–51. [Google Scholar]
- 130.Arbab S, Ullah H, Weiwei W, Wei X, Ahmad SU, Wu L, Zhang J. Comparative study of antimicrobial action of aloe vera and antibiotics against different bacterial isolates from skin infection. Vet Med Sci. 2021;7(5):2061–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Bashir A, Saeed B, Mujahid TY, Jehan N. Comparative study of antimicrobial activities of Aloe vera extracts and antibiotics against isolates from skin infections. Afr J Biotech. 2011;10(19):3835–40. [Google Scholar]
- 132.Valizadeh A, Darvishi MH, Amani A, Zarchi AAK. Design and development of novel formulation of Aloe Vera nanoemulsion gel contained erythromycin for topical antibacterial therapy: in vitro and in vivo assessment. J Drug Deliv Sci Technol. 2022;74:103519. [Google Scholar]
- 133.Tiwari R, Latheef SK, Ahmed I, Iqbal HM, Bule MH, Dhama K, Samad HA, Karthik K, Alagawany M, El-Hack ME. Herbal immunomodulators-a remedial panacea for designing and developing effective drugs and medicines: current scenario and future prospects. Curr Drug Metab. 2018;19(3):264–301. [DOI] [PubMed] [Google Scholar]
- 134.Aladejana EB, Adelabu OA, Aladejana AE, Ndlovu SI. Antimicrobial properties of alternative medicines used in the management of infections in diabetic patients: a comprehensive review. Pharmacol Res Mod Chin Med. 2024;11:100432. [Google Scholar]
- 135.Singh A, Jaiswal A, Yadav A, Mandal S, Sahoo JP. Nature’s Pharmacy: Exploring Potential Therapeutic Roles of Neem (Azadirachta indica L.). Vigyan Varta. 2024;5:149–54.
- 136.Brahmachari G. Neem—an omnipotent plant: a retrospection. ChemBioChem. 2004;5(4):408–21. [DOI] [PubMed] [Google Scholar]
- 137.Yarmohammadi F, Mehri S, Najafi N, Amoli SS, Hosseinzadeh H. The protective effect of Azadirachta indica (neem) against metabolic syndrome: A review. Iran J Basic Med Sci. 2021;24(3):280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.de Vor L, Rooijakkers SH, van Strijp JA. Staphylococci evade the innate immune response by disarming neutrophils and forming biofilms. FEBS Lett. 2020;594(16):2556–69. [DOI] [PubMed] [Google Scholar]
- 139.Chaturvedi P, Bag A, Rawat V, Jyala N, Satyavali V, Jha P. Antibacterial effects of Azadirachta indica leaf and bark extracts in clinical isolates of diabetic patients. NJIRM. 2011;2(1):5–9. [Google Scholar]
- 140.Shova NA. Comparative study on the antibacterial activities of neem oil, mustard oil and black seed oil against Staphylococcus aureus, Klebsiella pneumoniae, Bacillus cereus, Salmonella typhi and Pseudomonas aeruginosa. BRAC Univeristy; 2017.
- 141.Sarmiento WC, Maramba CC, Gonzales MLM. An in-vitro study on the antibacterial effect of neem (Azadirachta indica) leaf extract on methicillin-sensitive and Methicillin-resistant Staphylococcus aureus. PIDSP J. 2011;12(1):40–5. [Google Scholar]
- 142.Schumacher M, Cerella C, Reuter S, Dicato M, Diederich M. Anti-inflammatory, pro-apoptotic, and anti-proliferative effects of a methanolic neem (Azadirachta indica) leaf extract are mediated via modulation of the nuclear factor-κB pathway. Genes Nutr. 2011;6:149–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Priyadharshini R, Kumar SR, Sinduja P. Herbal formuLation of Azadirachta indica and Stevia rebaudiana and its anti-inflammatory and anti-diabetic activity. J Pharm Res Int. 2021;33(61B):200–7. [Google Scholar]
- 144.Hasan MM, Bae H. An overview of stress-induced resveratrol synthesis in grapes: perspectives for resveratrol-enriched grape products. Molecules. 2017;22(2):294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Vestergaard M, Ingmer H. Antibacterial and antifungal properties of resveratrol. Int J Antimicrob Agents. 2019;53(6):716–23. [DOI] [PubMed] [Google Scholar]
- 146.Jia Y, Shao J-H, Zhang K-W, Zou M-L, Teng Y-Y, Tian F, Chen M-N, Chen W-W, Yuan Z-D, Wu J-J. Emerging effects of resveratrol on wound healing: a comprehensive review. Molecules. 2022;27(19):6736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Yu X, Chen M, Wu J, Song R. Research progress of SIRTs activator resveratrol and its derivatives in autoimmune diseases. Front Immunol. 2024;15:1390907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Hwang D, Lim Y-H. Resveratrol antibacterial activity against Escherichia coli is mediated by Z-ring formation inhibition via suppression of FtsZ expression. Sci Rep. 2015;5(1):10029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Cui W, Wang Y, Zhang L, Liu F, Duan G, Chen S, Long J, Jin Y, Yang H. Recent advances in the use of resveratrol against Staphylococcus aureus infections. Med Int. 2024;4(6):67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Haranahalli K, Tong S, Ojima I. Recent advances in the discovery and development of antibacterial agents targeting the cell-division protein FtsZ. Bioorg Med Chem. 2016;24(24):6354–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Subramanian M, Soundar S, Mangoli S. DNA damage is a late event in resveratrol-mediated inhibition of Escherichia coli. Free Radical Res. 2016;50(7):708–19. [DOI] [PubMed] [Google Scholar]
- 152.Fuggetta MP, Bordignon V, Cottarelli A, Macchi B, Frezza C, Cordiali-Fei P, Ensoli F, Ciafrè S, Marino-Merlo F, Mastino A. Downregulation of proinflammatory cytokines in HTLV-1-infected T cells by resveratrol. J Exp Clin Cancer Res. 2016;35:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Zhong L-M, Zong Y, Sun L, Guo J-Z, Zhang W, He Y, Song R, Wang W-M, Xiao C-J, Lu D. Resveratrol inhibits inflammatory responses via the mammalian target of rapamycin signaling pathway in cultured LPS-stimulated microglial cells. PLoS ONE. 2012;7(2):e32195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Pinheiro DML, de Oliveira AHS, Coutinho LG, Fontes FL, de Medeiros Oliveira RK, Oliveira TT, Faustino ALF, da Silva VL, de Melo Campos JTA, Lajus TBP. Resveratrol decreases the expression of genes involved in inflammation through transcriptional regulation. Free Radical Biol Med. 2019;130:8–22. [DOI] [PubMed] [Google Scholar]
- 155.Panaro MA, Carofiglio V, Acquafredda A, Cavallo P, Cianciulli A. Anti-inflammatory effects of resveratrol occur via inhibition of lipopolysaccharide-induced NF-κB activation in Caco-2 and SW480 human colon cancer cells. Br J Nutr. 2012;108(9):1623–32. [DOI] [PubMed] [Google Scholar]
- 156.Reuter S, Gupta SC, Chaturvedi MM, Aggarwal BB. Oxidative stress, inflammation, and cancer: how are they linked? Free Radical Biol Med. 2010;49(11):1603–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Shevelev AB, La Porta N, Isakova EP, Martens S, Biryukova YK, Belous AS, Sivokhin DA, Trubnikova EV, Zylkova MV, Belyakova AV. In vivo antimicrobial and wound-healing activity of resveratrol, dihydroquercetin, and dihydromyricetin against Staphylococcus aureus, Pseudomonas aeruginosa, and Candida albicans. Pathogens. 2020;9(4):296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Chan MM-Y. Antimicrobial effect of resveratrol on dermatophytes and bacterial pathogens of the skin. Biochem Pharmacol. 2002;63(2):99–104. [DOI] [PubMed] [Google Scholar]
- 159.Javid AZ, Hormoznejad R, Allah Yousefimanesh H, Haghighi-Zadeh MH, Zakerkish M. Impact of resveratrol supplementation on inflammatory, antioxidant, and periodontal markers in type 2 diabetic patients with chronic periodontitis. Diabetes Metab Syndr Clin Res Rev. 2019;13(4):2769–74. [DOI] [PubMed] [Google Scholar]
- 160.Lee S-M, Yang H, Tartar D, Gao B, Luo X, Ye S, Zaghouani H, Fang D. Prevention and treatment of diabetes with resveratrol in a non-obese mouse model of type 1 diabetes. Diabetologia. 2011;54:1136–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Salehi B, Mishra AP, Shukla I, Sharifi-Rad M, Contreras MDM, Segura-Carretero A, Fathi H, Nasrabadi NN, Kobarfard F, Sharifi-Rad J. Thymol, thyme, and other plant sources: health and potential uses. Phytother Res. 2018;32(9):1688–706. [DOI] [PubMed] [Google Scholar]
- 162.Lorenzo JM, Mousavi Khaneghah A, Gavahian M, Marszałek K, Eş I, Munekata PE, Ferreira IC, Barba FJ. Understanding the potential benefits of thyme and its derived products for food industry and consumer health: from extraction of value-added compounds to the evaluation of bioaccessibility, bioavailability, anti-inflammatory, and antimicrobial activities. Crit Rev Food Sci Nutr. 2019;59(18):2879–95. [DOI] [PubMed] [Google Scholar]
- 163.Pirbalouti A, Rahimmalek M, Malekpoor F, Karimi A. Variation in antibacterial activity, Thymol and Carvacrol contents of wild populations of Thymus daenensis subsp. daenensis’ Celak. Plant Omics. 2011;4(4):209–14. [Google Scholar]
- 164.Meena RS, Vijayakumar V, Yadav GS, Mitran T. Response and interaction of Bradyrhizobium japonicum and arbuscular mycorrhizal fungi in the soybean rhizosphere. Plant Growth Regul. 2018;84:207–23. [Google Scholar]
- 165.Sharma N, Kumar A, Tiwari G, Gupta AK, Chanotiya C, Yadav A, Lal R. Unraveling genetic variability, heritability, genetic advance in agronomical traits, ameliorating essential oil yield, and its composition in clove basil (Ocimum gratissimum L.). Ind Crops Prod. 2024;221:119350. [Google Scholar]
- 166.Yang L, Wen K-S, Ruan X, Zhao Y-X, Wei F, Wang Q. Response of plant secondary metabolites to environmental factors. Molecules. 2018;23(4):762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Wu K, Zhang X, Sun S, Wang X. Factors affecting the accumulation of curcumin in microrhizomes of Curcuma aromatica Salisb. Biomed Res Int. 2015;2015(1):740794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Hassan A. Effects of mineral nutrients on physiological and biochemical processes related to secondary metabolites production in medicinal herbs. Med Arom Plant Sci Biotechnol. 2012;6(1):105–10. [Google Scholar]
- 169.Tiwari U, Cummins E. Factors influencing levels of phytochemicals in selected fruit and vegetables during pre-and post-harvest food processing operations. Food Res Int. 2013;50(2):497–506. [Google Scholar]
- 170.Sharangi A, Gowda MP, Das S. Responses of turmeric to light intensities and nutrients in a forest ecosystem: retrospective insight. Trees, For People. 2022;7:100208. [Google Scholar]
- 171.Kellogg JJ, Todd DA, Egan JM, Raja HA, Oberlies NH, Kvalheim OM, Cech NB. Biochemometrics for natural products research: comparison of data analysis approaches and application to identification of bioactive compounds. J Nat Prod. 2016;79(2):376–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Yixuan L, Qaria MA, Sivasamy S, Jianzhong S, Daochen Z. Curcumin production and bioavailability: a comprehensive review of curcumin extraction, synthesis, biotransformation and delivery systems. Ind Crops Prod. 2021;172:114050. [Google Scholar]
- 173.Rasheed HA, Rehman A, Karim A, Al-Asmari F, Cui H, Lin L. A comprehensive insight into plant-derived extracts/bioactives: Exploring their antimicrobial mechanisms and potential for high-performance food applications. Food Biosci. 2024;59:104035. [Google Scholar]
- 174.Khan H, Ullah H, Nabavi SM. Mechanistic insights of hepatoprotective effects of curcumin: therapeutic updates and future prospects. Food Chem Toxicol. 2019;124:182–91. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.