Abstract
Objective
The dispensing of non-prescription antibiotics is a worldwide concern, and antibiotics should only be dispensed with a legitimate prescription.
Methodology
A cross-sectional study was conducted using the simulated client methodology, with data collected, recorded, and analyzed using SPSS.
Results
The simulated client visited 210 pharmacies, of which 70 dispensed antibiotics without a prescription. Outcomes The most often suggested antibiotics for upper respiratory tract infections (URTIs) were Amoxicillin (n = 17, 8.1%), Clarithromycin (n = 20, 9.5%), and Moxifloxacin (n = 13, 6.2%), with 33.3% of medications dispensed without a prescription for URTIs. Cefixime (n = 20, 9.5%) and ceftriaxone (n = 17, 8.1%) were the most often administered medications for urinary tract infections (UTIs). The non-prescribed dispensing of upper respiratory tract infections (URTIs) and urinary tract infections (UTIs) was markedly elevated (p < 0.05). Antibiotics were dispensed without a prescription for diarrheal diseases in over 50% of pharmacies, with Metronidazole (n = 23, 11%), Azithromycin (n = 16, 7.6%), and Rifaximin (n = 15, 7.1%) being the most often prescribed. In all bivariate and multivariate models, male gender was associated with reduced likelihood (COR: 0.30, 95% CI: 0.12–0.72; p = 0.0079 and AOR: 0.03, 95% CI: 0.005–0.15; p = 0.0001). Individuals aged 30 years and older exhibited increased odds of dispensing in both bivariate (COR: 3.67, 95% CI: 1.69–8.87; p = 0.0018) and multivariate analyses (AOR: 9.44, 95% CI: 2.55–61.70; p = 0.001). The presence of a pharmacist on duty markedly diminished the likelihood of administering antibiotics without a prescription (COR: 0.13, 95% CI: 0.06–0.25; p = < 0.001; AOR: 0.06, 95% CI: 0.03–0.16; p = < 0.001).
Conclusion
These findings highlight the imperative of enforcing existing laws and implementing rigorous rules, alongside pharmacy-centered antimicrobial stewardship programs that focus on accurate dispensing practices to mitigate antimicrobial resistance.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13104-024-07030-0.
Keywords: Antibiotics, Without prescription antibiotics dispensing, AWaRe classification, Urinary tract infection, Upper respiratory tract infection, Diarrheal infections, Pharmacy
Introduction
The irrational practice of dispensing antibiotics without a prescription is a major global public health concern and can cause antimicrobial resistance (AMR), treatment failures, drug toxicity, increase in treatment costs [2, 11]. World Health Organization (WHO) identified AMR as one of the ten most significant threats to global health [21]. AMR presents a considerable risk to global public health, especially among patients in South Asian countries [6]. Since the bacteria that antibiotics were meant to kill are evolving new resistance patterns to the drug, an increasing percentage of infections are becoming more difficult to cure. Worldwide, an estimated 700,000 people pass away from AMR every year. If immediate action is not taken to encourage the rationale use of antibiotics, this number is expected to rise dramatically, reaching up to 10 million fatalities yearly by 2050 [1].
Antibiotics are widely available in low- and middle-income countries (LMICs) without a prescription, mostly because there are fewer laws or insufficient enforcement of those that do exist [15, 16]. In 2017, the WHO categorized antibiotics into three distinct groups to promote rational prescribing and dispensing: Access, Watch, and Reserve (AWaRe) antibiotics [ 20]. The Access group includes first- and second-line antibiotics for the empirical treatment of common infections. The Watch group consists of antibiotics with a higher potential for resistance, and their use is restricted to a smaller number of patient groups. The Reserve group should be reserved for use as a “last resort” treatment option [19].
Pakistan ranks third among LMICs in terms of antibiotic use [10]. Urban pharmacies sell over one-third of antibiotics without a valid prescription [9]. The antibiotic’s defined daily doses (DDDs) increased by 65% worldwide Between 2000 and 2015, with a daily consumption level of roughly 20 DDDs per 1000 persons in 2015. Analysis of cephalosporin and fluoroquinolone consumption during a five-year period from 2014 to 2018 revealed a notable 65% increase in cephalosporin consumption that was included in the WHO’s “Watch” category of antibiotics, while the number receiving “Reserve” cephalosporin treatment doubled. Of the fluoroquinolones, ciprofloxacin consumption increased significantly [13]. According to a study, 88.1% of patients in Pakistan were given many antibiotics without first undergoing a culture or sensitivity test. The most commonly recommended antibiotic for COVID-19 patients was azithromycin [14]. In the community there was 90% antibiotic dispensing in Lahore Pakistan before COVID-19 as reposted by Saleem et al. [18]. The post Covid a study from Hazara division Pakistan reported 95% antibiotic dispensing. The primary factors associated with inappropriate prescribing in Pakistan are socioeconomic aspects of customers, limited knowledge of dispensers, a wrong perception of being qualified, customers’ demands, public opinions, high consulting costs of physicians, costly diagnostic tests, and a desire to maximize profits [4, 18]. The COVID-19 pandemic significantly impacted antibiotic dispensing and resistance in Pakistan, driven by over-prescription of antibiotics like azithromycin for viral infections, fear of secondary infections, and widespread self-medication due to misinformation [17]. Weak regulatory controls allowed over-the-counter antibiotic access, while disrupted antimicrobial stewardship programs and limited diagnostic facilities exacerbated inappropriate use [18]. Hospitalized COVID-19 patients and improper waste management increased the spread of multidrug-resistant organisms. Public reliance on antibiotics and economic hardships further amplified misuse [17]. To combat the surge in antimicrobial resistance, Pakistan must strengthen stewardship programs, enforce prescription regulations, enhance AMR surveillance, and raise public awareness about the dangers of irrational antibiotic use. There are limited studies that compare or reported the post Covid-19 antibiotic dispensing in the most populated cities of Punjab, Pakistan. This study aims to evaluate the proportion and dispensing pattern of antibiotics used in URTIs, UTIs, and diarrheal infections without prescription at pharmacies in three cities in Punjab, Pakistan.
Methodology
Study setting
This was a multicenter cross-sectional study, carried out from February 2023 to May 2023 employing the simulated client method (SCM) in 3 main cities Lahore, Sialkot, and Gujranwala of Punjab province, Pakistan. All three districts had a total of 1500 drug retail outlets, including pharmacies; the study sample was selected from this population.
The study conducted in geographic location as per the socio-economic status, number of community pharmacies and drug outlets, and frequency of self-medication by including three different cities in the Punjab province.
Study population
In Pakistan, pharmacists or pharmacy technicians operate the medical scores whereas registered pharmacists run mostly community pharmacies. We visited 210 pharmacies that were providing medication accessibility to the community during the study period. Based on their availability and qualifications at pharmacies, simulated clientele (SCs) selected pharmacy staff members (dispensers) as their study target. The simulated clients observed the dispenser and license of qualified person at the pharmacy, also enquired about the pharmacist availability upon asking from the dispenser in the absence of qualified person or available pharmacist the simulated client decided the dispenser as a non-pharmacist.
Sample size
For our research, we included 210 community pharmacies from three main cities of Pakistan i.e. Lahore, Sialkot, and Gujranwala by utilizing convenience sampling.
Data collection team
We developed a data collection team to collect the data as per SCM criteria. A total of 11 group members conducted the study among which 3 were male and 8 were female members. The data collection process was supervised by 2 members. The simulated clients (pseudo patients) were pharmacy students in their final year aged between 22 and 25 years enrolled in M. Islam College of Pharmacy Gujranwala. Several training sessions were held, and SC received instruction and practice using SCM procedures in their role as SCs.
Data collection procedure and approach
Pharmacies in Pakistan are run by registered pharmacists. The main metropolis of Sialkot Lahore and Gujranwala together have 1500 pharmacies, all of which are staffed by pharmacists, pharmacy technicians, and dispensers. The numbers provided were verified using the licensing office of health authorities’ database in each district of the division. A convenience sample strategy, which is non-probability, was used to include 210 drug stores in the study. A 5% margin of error (95% CI) was used in the calculation of the sample size.
Every SC was given the task of presenting a pre-established clinical scenario for urinary tract infections (UTIs) and upper respiratory tract infections (URTIs). Visits were made to the community pharmacies and drug stores as one SC tasked with observing the license display, availability of a qualified individual at community pharmacy (CP), and dispenser behavior. The second SC job was to record information on drug counselling and the name, dosage, duration, and dosage type of the medicine dispensed.
A scenario was developed (Supplementary file 1) and presented involving cases of URTI, UTI, and diarrhea as pseudo patients. These infectious conditions were chosen as they are the most communal illnesses associated with antibiotic overuse in both self-medication at home and primary healthcare [8]. Based on prior simulated type studies with positive outcomes, these are the most frequently utilized reported scenarios [5]. The process of visits includes symptoms, and predefined responses to questions anticipated to be enquired by pharmacy workers have already been developed. The visit method and presentation transcript were tested and changed using a pilot survey, and the pilot results were excluded from the final analysis. The investigators treated the employees as if they were typical consumers, minimizing suspicion. The investigator employed three degrees of DPR (direct product request) until the dispensing of antibiotics was made or refused. Our SC’s first responsibility was to keep attention on the pharmacy/medicine counter atmosphere and make mental notes of critical indicators such as name of dispensed antibiotic, dose and counseling notes. Then the SC asked, “I want medications (antibiotics) to relieve my symptoms” without presenting a prescription (demand level 1), “Could you please give me antibiotics?” (Demand level 2), and “I would like amoxicillin or macrolides” (Demand level 3). This approach allowed us to identify incorrect antibiotic dispensing on the supply side (Level 1) vs. the demand side (Levels 2 and 3). SCs requested Macrolides (azithromycin and erythromycin) and amoxicillin since they are widely used in the general population and in clinical settings, thus they are unlikely to raise any concerns among pharmacy staff. The SCs were encouraged to memorize each demand level information to complete form of data collection. The SCs documented all of the information, including whether or not an antibiotic dispensed and type, as well as any additional facts, on a previously developed data collection form. These forms were done within 15 min of leaving the pharmacies to improve the data-gathering accuracy. The SCs described everything on each new data collection form, including whether antibiotics were administered or refused by pharmacy professionals, as well as any advice given to them.
Data collection quality control
Data collection forms were filled out promptly by SCs to enhance the data-collection accuracy after visiting the pharmacies. All data was kept in proper files and files were named accordingly to avoid any misplacing of data form and to lessen maximally the chances of errors associated with poor data quality control.
Data analysis
Data was analyzed using SPSS (Statistical Package for Social Science) version 21. A descriptive analysis using mean, frequency, standard deviation, and percentage for each of the variables, was conducted. To evaluate the relationship of the dispensing of non-prescription antibiotics with independent variables (type of pharmacy and pharmacist availability). A chi-square test was performed. The p < 0.05 value considered statistically significant. The relationship between the dispensing of antibiotics without a prescription and various factors (pharmacy location, age, gender, and pharmacist availability) was analyzed using bivariate and multivariate logistic regression. Variables identified as significant in the bivariate analysis were included in the multivariate model.
Results
Characteristics of pharmacies and pharmacy workforce personnel
A total of 210 pharmacies, were visited by the SCs. The number of chain pharmacies and independent community pharmacies visited by the SC was 35.2% (n = 74) and 64.8% (n = 136) respectively as shown in Table 1. A significant majority of the pharmacies were run by male healthcare professionals 180 (85.71%). The study population consists of 38.09% (n = 80) pharmacists and 61.90% (n = 130) other healthcare professionals like pharmacy technicians or health assistants. Most of the healthcare professionals were aged between 30 and 35 (72.9%).
Table 1.
Characteristics of pharmacies and pharmacy workforce personnel
| Study Variables | N (%) |
|---|---|
| Gender of personnels | |
| Male | 180 (85.71) |
| Female | 30 (14.28) |
| Type of Pharmacy | |
| Independent pharmacy | 136 (64.8) |
| Chain Pharmacy | 74 (35.2) |
| Title of workforce at pharmacies | |
| Pharmacist | 80 (38.09) |
| Non-Pharmacist | 130 (61.90) |
| Age of workforce at pharmacies | |
| < 30 | 53 (25.2) |
| 30–35 | 153 (72.9) |
| > 50 | 4 (1.9) |
Regional location of different types of pharmacies/drug outlets visited by simulated clients (SCs)
Simulated clients (SCs) visited various types of pharmacies, with the majority (70%) located in community and high-income areas within major urban centers, such as Lahore, Gujranwala, and Sialkot. This was followed by pharmacies in urban areas with comparatively lower economic status than the main regions of these cities. Pharmacies in medical centers and lower-income urban areas accounted for a smaller proportion of visits. The lowest proportion (30%) of visits occurred in rural areas, likely due to the limited development and scarcity of community pharmacies in these regions.
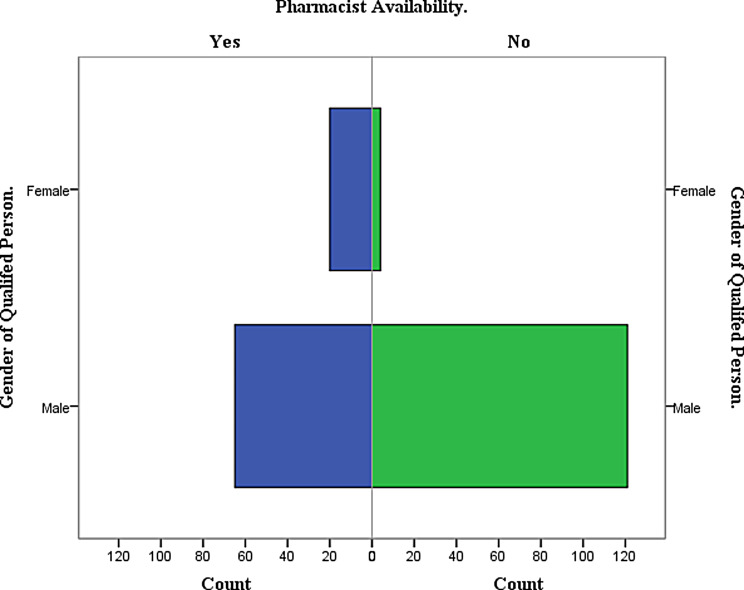
Gender-wise comparison of pharmacists and other healthcare professionals at pharmacies
A comparison between the numbers and gender distribution of pharmacists and other healthcare professionals has been illustrated in Fig. 1.
Fig. 1.
Comparison between the numbers and gender distribution of pharmacists and other healthcare professionals
It can be observed from Fig. 1 that the female pharmacists were fewer in numbers 9.5% (n = 20) than male pharmacists 28.5% (n = 60) at pharmacies. Similarly, among other non-pharmacist professionals, there were also fewer females 0.047% (n = 10) compared to males 57% (n = 120).
Sales of antibiotics without a prescription under different levels of demands
pharmacy staff dispensed 210 antibiotics each for URTI, UTI, and DI to SCs without any prescription (Table 2).
Table 2.
Sale of antibiotics without a prescription under different levels of demand
| Level of demands | Case presented | Antibiotics dispensing n (%) |
|---|---|---|
| DL-1 (RTIs) | For Respiratory tract infections | 70 (33.3) |
| DL-2 (UTIs) | Demand for urinary tract infections | 40 (19.1) |
| DL-3 (Dis) | Demand for Diarrheal infections | 100 (47.6) |
Non-prescription antibiotics dispensed for acute upper respiratory tract infection
210 pharmacies were visited by SCs and the clinical scenario of acute URTI was presented to the pharmacy staff. 70 of 210 community pharmacies dispensed non-prescription antibiotics. Clarithromycin 9.5% (n = 20), Amoxicillin 8.1% (n = 17), and Moxifloxacin 6.2% (n = 13) were the antibiotics dispensed by most pharmacies in the case of URTIs. 140 pharmacies did not dispense any antibiotic without a prescription for URTIs at any level of demand.
Non-prescription antibiotics dispensing for urinary tract infections
SCs visited 210 pharmacies again but this time they presented the clinical scenario of UTIs. They asked for some medicines for UTI without having a prescription. The extent of antibiotics dispensing without prescription in case of urinary tract infection was found to be 33.3%. Cefixime 9.5% (n = 20) and Ceftriaxone 8.1% (n = 17) were the antibiotics that were dispensed by most pharmacies in case of UTIs.
Non-prescription antibiotics dispensing for diarrheal infections
Non-prescription dispensing of antibiotics For DIs occurred in 70 of 210 community pharmacies/drug outlets. Metronidazole 11% (n = 23), Azithromycin 7.6% (n = 16), and Rifaximin 7.1% (n = 15) were most frequently dispensed.
Reasons to decline antibiotics dispensing without a prescription
In the case of non-prescription antibiotics, antibiotics without a prescription were refused at 66.7% (N = 140) of pharmacies. out of these 66.7% cases, 33% were the cases, where the patients were referred for additional clinical investigations and were refused antibiotics dispensing by the staff. The 2nd significant reason for denying antibiotics (23.9%) dispensing was administrative restriction (as by rules and regulations set by local legislation) that antibiotics are not over-the-counter products and unavailability of antibiotics at the time of visit was also the reason (12.8%). Antibiotic alternatives provided by the pharmacy staff are presented in Table 3.
Table 3.
Pharmacy staff-provided alternatives in specified scenarios of antibiotics
| For URTI’s | For UTI’s | For diarrhea |
|---|---|---|
| Paracetamol + Orphenadrine | Tramadol + Paracetamol | Oral Rehydrating Solution |
| Montelukast | Nimesulide | Attapulgite |
| Fexofenadine | Diclofenac | Loperamide |
| Cetirizine | Cranberry | Diphenhydramine + Atropine |
| Ebastine | Diloxanide |
Medication counselling and medication history taking from simulated clients by pharmacy staff
As for the proportion of major inquiries and counseling, at 56.7% (n = 119) of pharmacies, previous treatment and history of allergies were asked by pharmacy staff and they provided counseling. However, 43.3% (n = 91) did not provide any counseling and neither inquired about past medication or allergy history while dispensing medications.
Pharmacy type and demand level in which the antibiotics were dispensed without prescription
In chain pharmacies, 25, 31, and 18 antibiotics were dispensed under demand levels 1, 2 and 3 respectively. In independent Pharmacies under demand levels 1, 2, and 3 there were 45, 39, and 52 antibiotics that were dispensed without prescription, respectively (Table 4).
Table 4.
Pharmacist availability and dispensing antibiotics under demand levels
| Variables | Demand Levels | p-value | ||
|---|---|---|---|---|
| Pharmacy Type |
Below which demand level was the anti-biotic dispensed without a prescription. |
0.07 | ||
| DL-1 (URTIs) | DL-2 (UTIs) | DL-3 (DIs) | ||
| Chain Pharmacy | 25 | 31 | 18 | |
| Independent Pharmacy | 45 | 39 | 52 | |
| Pharmacist availability |
Dispense antibiotics under the first demand level - I (URTI) |
0.001 | ||
| Yes | No | |||
| 18 | 67 | |||
| 52 | 73 | |||
| Pharmacist availability |
Dispense antibiotics under the second demand level - II (UTI) |
0.004 | ||
| Yes | No | |||
| 42 | 43 | |||
| 28 | 97 | |||
| Pharmacist availability |
Dispensed Antibiotics under the third demand level - III (DIs) |
0.19 | ||
| Yes | No | |||
| 25 | 60 | |||
| 45 | 80 | |||
The type of Pharmacy and demand level in which the antibiotics were dispensed without prescription were not associated significantly.
Association between pharmacists’ availability and antibiotics dispensing at different levels of demand
Pharmacists’ availability was significantly associated with the dispensing of URTIs and UTIs. Non-prescribed dispensing of URTIs and UTIs was significantly higher (p = 0.001) and (p = 0.004) respectively, at the pharmacies where pharmacists were not available. However, there was no significant relationship between the availability of pharmacists and non-prescribed dispensing of antibiotics for DIs (Table 4). The presence of a pharmacist ensured a decrease in the number of antibiotics dispensed without a prescription. Under demand level one, antibiotics dispensed at the pharmacies with pharmacists was less than 20 while more than 50 antibiotics were dispensed in the pharmacies that had no pharmacist there.
The bivariate and multivariate logistic regression analyses revealed key factors influencing the dispensing of antibiotics without a prescription. Chain pharmacies and urban locations showed no significant associations in both bivariate (COR: 1.03, 95% CI: 0.56–1.87; p = 0.9186 and COR: 1.76, 95% CI: 0.92–3.47; p = 0.0919, respectively) and multivariate analyses (AOR: 1.51, 95% CI: 0.36–6.22; p = 0.5649 and AOR: 1.65, 95% CI: 0.82–3.44; p = 0.1686, respectively). The absence of a pharmacist was significant in the bivariate analysis (COR: 0.37, 95% CI: 0.19–0.69; p = 0.0024) but was excluded from the multivariate model. Male gender was significantly associated with reduced odds in both bivariate (COR: 0.30, 95% CI: 0.12–0.72; p = 0.0079) and multivariate analyses (AOR: 0.03, 95% CI: 0.005–0.15; p = 0.0001). Individuals aged ≥ 30 years showed higher odds of dispensing in the bivariate (COR: 3.67, 95% CI: 1.69–8.87; p = 0.0018) and multivariate analyses (AOR: 9.44, 95% CI: 2.55–61.70; p = 0.0037). The presence of a pharmacist on duty significantly reduced the likelihood of dispensing antibiotics without a prescription, with strong associations observed in the bivariate (COR: 0.13, 95% CI: 0.06–0.25; p < 0.001) and multivariate analyses (AOR: 0.06, 95% CI: 0.03–0.16; p < 0.001). These findings underscore the importance of pharmacist availability, gender, and age in influencing dispensing practices, while pharmacy type and location were not significant factors (Table 5).
Table 5.
Multivariate and Bivariate logistic regression
| Bivariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|
| Variables | COR (95% Cl) | P-value | AOR (95% Cl) | P-Value | |
| Type of Pharmacy | Independent Pharmacy | Reference | Reference | ||
| Chain Pharmacy | 1.03 (0.56–1.87) | 0.9186 | 1.51 (0.36–6.22) | 0.5649 | |
| Pharmacy Location | Rural | Reference | Reference | ||
| Urban | 1.76 (0.92–3.47) | 0.0919 | 1.65 (0.82–3.44) | 0.1686 | |
| Pharmacist Availability | No | Reference | Reference | ||
| Yes | 0.37 (0.19–0.69) | 0.0024 | removed from model* | ||
| Gender | Female | Reference | Reference | ||
| Male | 0.30 (0.12–0.72) | 0.0079 | 0.03 (0.005–0.15) | 0.0001 | |
| age | < 30 | Reference | Reference | ||
| ≥ 30 | 3.67 (1.69–8.87) | 0.0018 | 9.44 (2.55–61.70) | 0.0037 | |
| Pharmacist on duty | No | Reference | Reference | ||
| Yes | 0.13 (0.06–0.25) | < 0.001 | 0.06 (0.03–0.16) | < 0.001 |
*: Later on, due to multi-co-linearity between “availability of pharmacist” and “pharmacist on duty” predictors, availability of pharmacist was removed from model
Discussion
The results of our study reveal significant patterns in the dispensing of antibiotics without a prescription across various types of pharmacies and healthcare settings. The findings raise important considerations regarding regulatory compliance, public health, and the role of healthcare professionals in antibiotic stewardship.
The study highlights a notable gender disparity within the pharmacy workforce, with a predominance of male healthcare professionals (85.71%) and a smaller proportion of pharmacists (38.09%) compared to other healthcare professionals (61.90%). Similar patterns have been observed in other studies conducted in Pakistan and South Asia, where the pharmacy workforce tends to be male-dominated [7, 12] and includes a significant number of non-pharmacist personnel [3]. This composition can influence dispensing practices, as non-pharmacist staff usually have different levels of training and adherence to antibiotic stewardship principles compared to licensed pharmacists in Pakistan.
The primary reasons for refusing to dispense antibiotics without a prescription were referral for additional clinical investigations, administrative restrictions, and unavailability of antibiotics. These reasons reflect a mix of regulatory compliance and practical constraints. The significant portion of pharmacies (66.7%) that adhered to these restrictions highlights a substantial adherence to proper protocols. However, the reasons also suggest areas where further education and reinforcement of regulations might improve compliance, particularly in areas where administrative enforcement is weaker.
The findings on medication counseling and history taking are concerning, with only 56.7% of pharmacies engaging in these critical practices. Effective patient education and thorough history-taking are essential components of responsible antibiotic dispensing, ensuring that medications are used appropriately and safely. The absence of these practices in 43.3% of pharmacies highlights a significant gap in patient care and identifies an area for potential intervention and training. Our findings contrast with those of Majid et al., who reported that 87.1% of dispensers provide patient counseling when dispensing antibiotics in community pharmacies across Punjab, Pakistan.
The significant association between the availability of pharmacists and reduced non-prescription dispensing of antibiotics for URTIs and UTIs suggests that the presence of trained pharmacists is a critical factor in enforcing prescription regulations. Pharmacies without pharmacists were more likely to dispense antibiotics without a prescription, indicating that the expertise and authority of pharmacists play a crucial role in adhering to regulatory standards. This finding is consistent with research from Sri Lanka and Pakistan, which shows that pharmacies staffed by licensed pharmacists are less likely to dispense antibiotics without a prescription [2, 22]. This finding underscores the importance of ensuring that qualified pharmacists are present in all pharmacies to safeguard.
The study’s findings have several important implications. Firstly, regulatory bodies need to enhance the enforcement of prescription-only sales of antibiotics to limit inappropriate use and mitigate the risk of antimicrobial resistance. Moreover, targeted educational campaigns as well as training programs for pharmacy staff, particularly non-pharmacist healthcare workers, could improve adherence to antibiotic stewardship principles. Addressing the gender disparity and ensuring the equitable distribution of pharmacists across all regions, including rural and low-economic areas, could also enhance the overall quality of pharmacy services and public health outcomes.
Study strength and limitations
A key strength of our study was its simulation-based design, which provided a realistic approach and accurately reflected the scenarios encountered by individuals in community pharmacies.
Our study primarily focused on pharmacies located in a select few cities in Pakistan characterized by relatively favorable demographic and socioeconomic conditions. As a result, the findings may not be fully generalizable to the entire country. Nevertheless, we believe that the results are robust and offer valuable insights to guide future research and policy development.
Conclusion
Despite the regulations, it is concluded that dispensing of non-prescription antibiotics is still a predominant practice in big cities of the province of Punjab, Pakistan. In addition, the pharmacy staff did not frequently enquire about the allergy history of patients, or previous medication history, or did not provide pharmaceutical recommendations. Non-prescribed antibiotics dispensing is a complex problem in the community. Therefore, an effective and comprehensive strategy is required to address this issue and combat the daily rise in antimicrobial resistance, Moreover, authorities must improve policies and rules to ensure the responsible use of pharmaceuticals.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We acknowledge the simulated clients, pharmacist, and district administration.The Consent form was not applicable for this study becaseue of study design. This study design was simulated client study.
Author contributions
“FUK and FUK set the methodology and study concept, TA.; software, THM; validation, SA, SS; formal analysis and data collection AS.; writing—original draft preparation, FUK.; writing—review and editing, KH.; resources, visiting and traning to data collector TA.; visualization, FUK; supervision, FUK.; project administration. All authors have read and agreed to the published version of the manuscript.”
Funding
This research received no funding.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Study approval was granted by the Biomedical Ethics Committee for Medical Research of M. Islam College of Pharmacy Gujranwala, Pakistan. Moreover, a list of pharmacies to be included in the study was issued by the department. Since it was an SC study, therefore, did not require the informed consent of the respondents, however, it was approved by the ethics committees.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Faiz Ullah Khan, Email: fkhan@bs.qau.edu.pk.
Tawseef Ahmad, Email: tausifsafi95@gmail.com.
References
- 1.Abubakar S, Sartelli M. Ten golden rules for optimal antibiotic use in hospital settings: the WARNING call to action. World J Emerg Surgery: WJES. 2023;18(50). 10.1186/s13017-023-00518-3. [DOI] [PMC free article] [PubMed]
- 2.Ahmad T, Khan FU, Ali S, et al. Assessment of without prescription antibiotic dispensing at community pharmacies in Hazara Division, Pakistan: a simulated client’s study. PLoS ONE. 2022;17(2):e0263756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahmad T, Khan SA, Mallhi TH et al. (2023) Assessing antibiotic dispensing without prescription through simulated client methodology in developing countries: a comprehensive literature review from 2009 to 2021. J Public Health: 1–23.
- 4.Asghar S, Atif M, Mushtaq I, et al. Factors associated with inappropriate dispensing of antibiotics among non-pharmacist pharmacy workers. Res Social Administrative Pharm. 2020;16(6):805–11. [DOI] [PubMed] [Google Scholar]
- 5.Auta A, Hadi MA, Oga E, et al. Global access to antibiotics without prescription in community pharmacies: a systematic review and meta-analysis. J Infect. 2019;78(1):8–18. [DOI] [PubMed] [Google Scholar]
- 6.Gandra S, Alvarez-Uria G, Turner P, et al. Antimicrobial resistance surveillance in low-and middle-income countries: progress and challenges in eight south Asian and southeast Asian countries. Clin Microbiol Rev. 2020;33(3). 10.1128/cmr. 00048 – 00019. [DOI] [PMC free article] [PubMed]
- 7.Gillani AH, Zhao M, Hussain AK, et al. Community pharmacists’ perception and exposure to drug promotion in Pakistan: a cross-sectional study. BMJ open. 2022;12(1):e048249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haque M, Sartelli M, McKimm J et al. (2018) Health care-associated infections–an overview. Infection and drug resistance: 2321–2333. [DOI] [PMC free article] [PubMed]
- 9.Imtiaz F, Hafeez A, Ashraf F, et al. Antibiotic dispensing & prescription pattern in pharmacies of Islamabad & Rawalpindi: Pakistan. Int J Collaborative Res Intern Med Public Health. 2017;9(5):683–92. [Google Scholar]
- 10.Klein EY, Van Boeckel TP, Martinez EM, et al. Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proc Natl Acad Sci. 2018;115(15):E3463–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Llor C, Bjerrum L. Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Therapeutic Adv drug Saf. 2014;5(6):229–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Majid Aziz M, Haider F, Rasool MF et al. (2021) Dispensing of non-prescribed antibiotics from community pharmacies of Pakistan: a cross-sectional survey of pharmacy staff’s opinion. Antibiotics 10(5): 482. https://www.mdpi.com/2079-6382/10/5/482 [DOI] [PMC free article] [PubMed]
- 13.Malik F, Figueras A. Continuous rise in cephalosporin and fluoroquinolone consumption in Pakistan: a 5 year analysis (2014–18). JAC-Antimicrobial Resist. 2019;1(3):dlz063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mustafa ZU, Salman M, Aldeyab M et al. SS Hasan antimicrobial consumption among hospitalized patients with COVID-19 in Pakistan. 2021;3. 10.1007/s42399-021-00966-5. PMID: https://www.ncbi.nlm.nih.gov/pubmed/34095752: 1691–1695. [DOI] [PMC free article] [PubMed]
- 15.Oleribe OO, Momoh J, Uzochukwu BS et al. (2019) Identifying key challenges facing healthcare systems in Africa and potential solutions. Int J Gen Med 395–403. [DOI] [PMC free article] [PubMed]
- 16.Porter G, Kotwani A, Bhullar L, et al. Over-the-counter sales of antibiotics for human use in India: the challenges and opportunities for regulation. Med Law Int. 2021;21(2):147–73. [Google Scholar]
- 17.Raheem M, Anwaar S, Aziz Z et al. (2020) Adherence to the core elements of outpatient antibiotic stewardship: a cross-sectional survey in the tertiary care hospitals of Punjab, Pakistan. Infection and drug resistance: 3833–3841. [DOI] [PMC free article] [PubMed]
- 18.Saleem Z, Hassali MA, Hashmi FK et al. (2019) Antimicrobial dispensing practices and determinants of antimicrobial resistance: a qualitative study among community pharmacists in Pakistan. Family Med Community Health 7(3). [DOI] [PMC free article] [PubMed]
- 19.Sharland M, Pulcini C, Harbarth S, et al. Classifying antibiotics in the WHO essential Medicines list for optimal use—be AWaRe. Lancet Infect Dis. 2018;18(1):18–20. [DOI] [PubMed] [Google Scholar]
- 20.WHO. (2017) The selection and use of essential medicines: report of the WHO expert committee, 2017 (including the 20th WHO model list of essential medicines and the 6th model list of essential medicines for children).
- 21.WHO. (2020) 10 global health issues to track in 2021.
- 22.Zawahir S, Lekamwasam S, Aslani P. Factors related to antibiotic supply without a prescription for common infections: a cross-sectional national survey in Sri Lanka. Antibiotics. 2021;10(6):647. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.