Abstract
Objective
To compare the efficacy of handrubbing with an alcohol based solution versus conventional handwashing with antiseptic soap in reducing hand contamination during routine patient care.
Design
Randomised controlled trial during daily nursing sessions of 2 to 3 hours.
Setting
Three intensive care units in a French university hospital.
Participants
23 healthcare workers.
Interventions
Handrubbing with alcohol based solution (n=12) or handwashing with antiseptic soap (n=11) when hand hygiene was indicated before and after patient care. Imprints taken of fingertips and palm of dominant hand before and after hand hygiene procedure. Bacterial counts quantified blindly.
Main outcome measures
Bacterial reduction of hand contamination.
Results
With handrubbing the median percentage reduction in bacterial contamination was significantly higher than with handwashing (83% v 58%, P=0.012), with a median difference in the percentage reduction of 26% (95% confidence interval 8% to 44%). The median duration of hand hygiene was 30 seconds in each group.
Conclusions
During routine patient care handrubbing with an alcohol based solution is significantly more efficient in reducing hand contamination than handwashing with antiseptic soap.
What is already known on this topic
To improve compliance with hand hygiene during patient care, handrubbing with an alcohol based solution has been proposed as a substitute for handwashing because of its rapid action and accessibility
Experimental studies show that handrubbing is at least as effective as medicated soap in reducing artificial contamination of hands
Many healthcare workers still have reservations regarding its efficacy and are reluctant to use this technique
What this study adds
When used in routine practice, handrubbing with an alcohol based solution after contact with patients achieved a greater reduction in bacterial contamination of hands than conventional handwashing with medicated soap
Introduction
Handwashing is emphasised as the single most important measure to prevent cross transmission of micro-organisms and thus to prevent nosocomial infections.1 However, under routine hospital practice compliance with this measure is still unacceptably low, less than 50% in most studies published in the past 20 years.2,3 This constant finding is worrying because recent studies have shown that this level of compliance will not reduce the risk of transmission of multiresistant bacteria in hospital.4 Attempts to improve compliance have included increasing the number of accessible sinks5 and educating healthcare workers,6,7 but none of these interventions led to a marked and sustained improvement in compliance.
Handrubbing with an alcohol based, waterless hand antiseptic seems to be the best method of increasing compliance with hand hygiene. Recent studies have shown a significant improvement in compliance after the introduction of handrubbing as a substitute for handwashing with plain soap and water.7,8 However, introduction of this new method as a substitute to standard handwashing after decades of enforcement of the latter can be a real challenge for infection control teams. Despite showing healthcare workers that only half of the opportunities of handwashing are completed, mainly because of lack of time, and that compliance can be improved by handrubbing, staff may be reluctant to use it. We carried out a survey in a representative sample of 271 healthcare workers in our hospital. The main reason raised for not adhering to the recommendation to use handrubbing was the lack of confidence about its efficacy.9 It seems there is still reluctance to accept handrubbing as a substitute for handwashing, even among some infection control practitioners.
There is growing evidence from experimental studies on artificial contamination of volunteer's hands that handrubbing is at least as effective as handwashing with either unmedicated soap or antiseptic agent.3 To our knowledge only two clinical studies, one observational study and one randomised controlled trial, have evaluated handwashing with plain soap versus handrubbing in everyday practice, and both studies showed positive results in favour of handrubbing.10,11 One randomised clinical study compared handwashing with an antiseptic soap versus handrubbing with an alcohol based solution with the assessment of skin tolerance as the primary objective.12 Handrubbing was better tolerated than handwashing and achieved comparable reduction in bacterial contamination. We performed a randomised clinical trial to assess the efficacy of an alcohol based solution compared with standard handwashing with a medicated soap in reducing hand contamination during routine patient care.
Methods
Enrolment of participants
The study was a prospective randomised clinical trial with blinded evaluation of microbiological results. It was performed from June to July 2000 in three intensive care units (two surgical and one medical) of a 940 bed tertiary care and referral university hospital. Eligible healthcare workers were all permanent and temporary nurses and nursing assistants of each unit. All workers were asked to volunteer for the study. When a worker refused to participate, an alternative person was enrolled.
Treatment groups
At the beginning of each session when each participant arrived at the unit (7 am) we used opaque sealed envelopes to assign randomly him or her to standard handwashing with a medicated soap (chlorhexidine gluconate 4%; Hibiscrub, Zeneca Pharma)13 or handrubbing with a waterless alcohol based solution (45% 2-propanol, 30% 1-propanol, 0.2% mecetronium ethyl sulphate, average 3-5 ml; Sterillium, Bode Chemie, Hamburg, Germany). All participants had been previously instructed in the use of the alcohol based solution when the hospital-wide handrubbing policy was launched a year ago by the infection control committee. A written protocol was available in each unit, and no additional information was provided to participants before the study started. The sole exclusion criteria applied to those participants who were assigned to handrubbing but whose hands became visibly soiled (such as with body fluids). They then had to wash their hands with a standard antiseptic soap, and the session was ceased. In this paper hand hygiene refers to either handrubbing or handwashing.
Monitoring and data collection
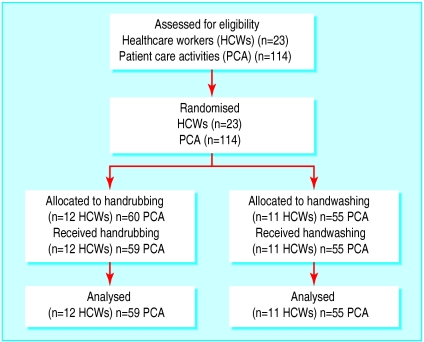
Patient care activities were monitored during daily sessions of two to three hours until a predetermined number of eligible activities had been performed (see fig 1). One session comprised five patient care activities that required hand hygiene before and after, which corresponded to 10 hand samplings (five samples obtained before and five after hand cleaning). Eligible activities were direct contact with the skin of a patient before invasive care, after interruption of care, and after contact with any part of a patient that was colonised with multiresistant bacteria. We also recorded the type of care performed, duration of care, whether the participant wore gloves, number of opportunities for hand hygiene according to the recent guidelines,12 number of actual hand hygiene procedures performed, and duration of hand hygiene procedure (that is, duration of the use of antiseptic agent).
Figure 1.
Schematic schedule of monitoring sampling sessions (one participant allocated to handrubbing did not use it on one occasion because of visible soiling with body fluids—the sole contraindication for using alcohol based solutions)
Microbiological samples and processing
When an opportunity for hand hygiene occurred we took an imprint of fingertips and palm from the participant's dominant hand before and one minute after the procedure. If the participant wore gloves during the procedure the gloves were removed before we carried out sampling. Each fingertip and the palm were pressed on to commercial contact agar plates (one plate per finger and one per palm) that contained neutralisers (lecithin, polysorbate 80, sodium thiosulfate; Count-Tact, BioMérieux SA, Marcy l'Etoile, France). We incubated plates at 37°C under aerobic conditions. We recorded the total bacterial contamination of hands as the number of colony forming units (cfu) recovered from both the fingertips and palm after 48 hours of incubation. We evaluated the precise count up to a maximum of 300 cfu, as beyond this point colonies formed a confluent growth.10 We identified Staphylococcus aureus or other pathogenic bacteria not usually found in skin flora by using standard microbiological procedures and determined their susceptibility to antibiotics. We specifically looked for methicillin resistant S aureus (MRSA), the most prevalent multiresistant organism at our institution. No anaerobic cultures were done. We performed preliminary tests to assess the effective neutralisation of each tested product using a suspension of 104 MRSA per ml. Two observers (SL and FO) were responsible for the whole protocol (monitoring and sampling) in all units. They stayed in the unit without interfering with hand hygiene (that is, quality of hand hygiene) whatever the method used. The microbiologist who examined the culture plates and reported the microbiological results was unaware of the hand hygiene method used.
Statistical analysis
Our primary objective was the reduction of total bacterial hand contamination. To detect a difference of 30% in the median reduction of hand contamination with the two techniques at a significance level of 5% and a power of 95% we calculated we would need 80 patient care activities. We extended the sample size to 100 to take into account possible technical difficulties at the beginning of the study.
Our analyses were based on the intention to treat principle; one participant dropped out of the study after four samplings instead of five because his hands were visibly soiled with body fluids. The participants were the unit of analysis. Bacterial counts were expressed as number of cfu per hand. Firstly, we calculated the percentage reduction in hand contamination for each cleaning procedure. Secondly, we obtained the average percentage reduction for each participant by calculating the mean over the five procedures per participant and used Mann-Whitney tests to compare the percentage reduction between the two groups. We have expressed summary statistics on bacterial counts as means (SD) with 95% confidence intervals, medians, and interquartile ranges. We used Epi-Info 6.0 (Centers for Disease Control, Atlanta) to perform the analysis and considered P<0.05 as significant.
Results
A total of 23 healthcare workers were included in the study and analysed; 12 were randomised to handrubbing and 11 to handwashing (fig 1). Randomised participants performed 114 patient care activities (59 in the handrubbing group and 55 in the handwashing group). The distribution of activities was comparable between the two groups. Table 1 shows the baseline characteristics of the two randomised groups and the activities performed. Gloves were worn during most activities with a similar frequency between groups.
Table 1.
Characteristics of two groups of healthcare workers randomised to handrubbing with alcohol based solution or handwashing
| Handrubbing (n=12)
|
Handwashing (n=11)
|
|
|---|---|---|
| Nurses | 5 | 6 |
| Nurse assistants | 6 | 3 |
| Nursing students | 1 | 2 |
| No of patient care activities included | 59 | 55 |
| Median (IQR) duration of patient care activities (min) | 11 (5-20) | 15 (7-25) |
| No (%) activities when gloves were worn | 51 (86) | 46 (83) |
| Cumulative No (IQR) of hand hygiene procedures performed during monitoring sessions | 11 (7-15) | 8 (7-13) |
| Median (IQR) duration of monitoring sessions (min) | 91 (58-177) | 75 (35-132) |
| No of opportunities observed | 184 | 158 |
| Proportion (95% CI) compliance with hand hygiene | 71 (45-96) | 64 (36-93) |
IQR=interquartile range.
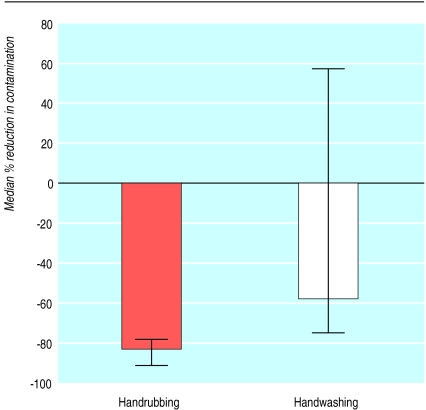
In both groups bacterial counts were lower after hand hygiene (table 2). Figure 2 shows that for each participant the median reduction of bacterial contamination achieved by handrubbing was significantly higher than the reduction achieved by handwashing (83% (interquartile range 78-92%) v 58% (−58-74%), respectively, P=0.012). The difference in the percentage reduction between the two groups was 26% (95% confidence interval 8% to 44%).
Table 2.
Bacterial counts (colony forming units) before and after two methods of hand cleaning
| Before
|
After
|
Median % reduction (IQR)
|
||||
|---|---|---|---|---|---|---|
| Mean (SD); 95% CI
|
Median (IQR)
|
Mean (SD); 95% CI
|
Median (IQR)
|
|||
| Handrubbing | 271 (372); 174 to 368 | 101 (29-380) | 35 (59); 20 to 50 | 7 (2-31) | 86 (70-96) | |
| Handwashing | 232 (331); 143 to 321 | 117 (15-239) | 69 (106); 41 to 97 | 9 (1-135) | 73 (25-93) | |
IQR=interquartile range.
Figure 2.
Comparison of percentage reduction in bacterial contamination of participants' hands obtained after handrubbing with alcohol based solution or after handwashing with antiseptic soap. Results expressed as median and interquartile range; difference between two groups significant (P=0.012)
During monitoring sessions, the median cumulative number of observed handrubbings was 1 (0-3) before the first sample and 10 (6-14) before the fifth sample. The percentage reduction in contamination at the first evaluated handrubbing was 88% (74-97%) and at the fifth was 95% (76-99%). Thus, handrubbing remained effective after several applications of alcohol based solution.
The median time spent on hand hygiene was relatively low in the handwashing group, where the antiseptic soap was applied for only 30 seconds (23-37 sec); 36 handwashing procedures (65%) lasted less than 30 seconds. The median duration of handrubbing was also 30 seconds (29 to 33 sec), which is the required time for bactericidal activity.
Discussion
We have shown that handrubbing with an alcohol based solution is more effective than handwashing with an antiseptic soap in reducing bacterial contamination of healthcare workers' hands during routine patient care. This was due in part to the inadequate time spent washing hands conventionally.
Several experimental studies in which hands were artificially contaminated with various micro-organisms have shown that handrubbing with alcohol based products is more effective that handwashing with unmedicated or antiseptic soap.14–18 Most of these studies incorporated supervised hand hygiene techniques to ensure conformity to usual recommendations or at least insisted on the quality of the technique. Despite these specifications, standard techniques of handwashing were always found to be less efficient than handrubbing in removing transient contamination on hands. Our study was designed not to interfere with the actual practice of participants in terms of compliance with and quality of hand hygiene, our main objective being to evaluate the efficacy in routine care.
Our results show that in routine conditions, handrubbing was at least as effective as handwashing with an antiseptic detergent. The reduction of total bacterial contamination of participants' hands was actually significantly higher after handrubbing than after antiseptic handwashing. In a recent study, Larson et al found that handrubbing was equivalent to antiseptic handwashing in reducing hand contamination.11 However, the product tested contained less alcohol than the one we used (61% versus 75%) and contained another antiseptic compound. In addition, it was not clear whether hands were sampled during patient care activities. The sampling method used was the glove juice technique, which is difficult to perform during routine care activities.
Duration of cleaning and effect
The difference in efficacy may have been partly due to the duration of handwashing. The recommended optimal duration of handwashing is at least 30 seconds and up to 1 minute, a time that was adhered to in less than 35% of opportunities. Handrubbing and handwashing were actually performed by participants for a similar length of time. This duration (30 seconds) seems sufficient for handrubbing with alcohol based solutions but may not be long enough for handwashing with a medicated soap. Most observational studies have shown that handwashing is seldom performed for more than 30 seconds, and our study confirms these findings.19–21 Therefore, the rapid efficacy of alcohol based solutions compared with handwashing, even with an antiseptic agent, is a major argument supporting their use in clinical practice.22 Handrubbing also achieved a higher reduction in bacterial contamination, suggesting higher efficacy.
We also found that handrubbing remained effective after a series of applications. This finding contradicts the results of Paulson et al, who reported that the efficacy of handrubbing after artificial inoculation of hands decreased with the number of procedures performed.23
Limitations
One potential limitation of our study includes the fact that we assessed bacterial contamination by taking agar fingerprints of the dominant hand and did not use the glove juice technique, which may be more effective in recovering the whole bacterial burden on hands.12 Our technique may have underestimated the degree of hand contamination, though we are not aware of a direct comparison of the two techniques in terms of assessment of bacterial burden on hands. However, bacterial counts before hand hygiene were consistent with baseline hand contamination found in two other clinical studies that used fingerprinting.10,11 The design of our study, which was planned not to interfere with regular activities, did not allow using the glove juice technique. However, we believe the comparison of the two procedures tested, using the same technique for culture, remains valid.
The rapid efficacy of alcohol based solutions and their availability at the bedside make these solutions an ideal substitute for conventional handwashing and should help in achieving increased compliance with hand hygiene during patient care. Improving hand hygiene compliance can lead to reduced rates of nosocomial infection and acquisition of multiresistant bacteria.24 Other investigations are still needed to assess the best methods for promoting handrubbing and education on indications for hand hygiene at the bedside.
Footnotes
Funding: Bode SA, Hamburg, Germany.
Competing interests: EG has received funds for research and has been reimbursed by Bode for expenses associated with attending conferences where this work has been presented.
References
- 1.Conly JM, Hill S, Ross J, Lertzman J, Louie TJ. Handwashing practices in an intensive care unit: the effects of an educational program and its relationship to infection rates. Am J Infect Control. 1989;17:330–339. doi: 10.1016/0196-6553(89)90002-3. [DOI] [PubMed] [Google Scholar]
- 2.Pittet D, Mourouga P, Perneger TV the Members of the Infection Control Program. Compliance with handwashing in a teaching hospital. Ann Intern Med. 1999;130:126–130. doi: 10.7326/0003-4819-130-2-199901190-00006. [DOI] [PubMed] [Google Scholar]
- 3.Rotter ML. Hand washing, hand disinfection and skin disinfection. In: Mayhall G, editor. Hospital epidemiology and infection control. 2nd ed. Baltimore: Williams and Wilkins; 1999. pp. 691–709. [Google Scholar]
- 4.Austin DJ, Bonten MJM, Weinstein RA, Slaughter S, Anderson RM. Vancomycin-resistant enterococci in intensive-care hospital settings: transmission dynamics, persistence, and the impact of infection control programs. Proc Natl Acad Sci U S A. 1999;96:6908–6913. doi: 10.1073/pnas.96.12.6908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Preston GA, Larson EL, Stamm WE. The effect of private isolation rooms on patient care practices, colonization and infection in an intensive care unit. Am J Med. 1981;70:641–645. doi: 10.1016/0002-9343(81)90588-x. [DOI] [PubMed] [Google Scholar]
- 6.Simmons B, Bryant J, Neiman K, Spencer L, Arheart K. The role of handwashing in prevention of endemic intensive care unit infections. Infect Control Hosp Epidemiol. 1990;11:589–594. doi: 10.1086/646100. [DOI] [PubMed] [Google Scholar]
- 7.Bischoff WE, Reynolds TM, Sessler CN, Edmond MB, Wenzel RP. Handwashing compliance by health care workers: the impact of introducing an accessible, alcohol-based hand antiseptic. Arch Intern Med. 2000;160:1017–1021. doi: 10.1001/archinte.160.7.1017. [DOI] [PubMed] [Google Scholar]
- 8.Maury E, Alzieu M, Baudel JL, Haram N, Barbut F, Guidet B, et al. Availability of an alcohol solution can improve hand disinfection compliance in an intensive care unit. Am J Respir Crit Care Med. 2000;162:324–327. doi: 10.1164/ajrccm.162.1.9908118. [DOI] [PubMed] [Google Scholar]
- 9.Girou E, Oppein F. Handwashing compliance in a French university hospital: new perspective with the introduction of hand-rubbing with a waterless alcohol-based solution. J Hosp Infect. 2001;48(suppl A):S55–S57. doi: 10.1016/s0195-6701(01)90015-5. [DOI] [PubMed] [Google Scholar]
- 10.Pittet D, Dharan S, Touveneau S, Sauvan V, Perneger TV. Bacterial contamination of the hands of hospital staff during routine patient care. Arch Intern Med. 1999;159:821–826. doi: 10.1001/archinte.159.8.821. [DOI] [PubMed] [Google Scholar]
- 11.Zaragoza M, Sallés M, Gomez J, Bayas JM, Trilla A. Handwashing with soap or alcoholic solutions? A randomized clinical trial of its effectiveness. Am J Infect Control. 1999;27:258–261. doi: 10.1053/ic.1999.v27.a97622. [DOI] [PubMed] [Google Scholar]
- 12.Larson EL, Aiello AE, Bastyr J, Lyle C, Stahl J, Cronquist A, et al. Assessment of two hand hygiene regimens for intensive care unit personnel. Crit Care Med. 2001;29:944–951. doi: 10.1097/00003246-200105000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Larson E the Association for Professionals in Infection Control and Epidemiology. APIC guideline for handwashing and hand antisepsis in health care settings. Am J Infect Control. 1995;23:251–269. doi: 10.1016/0196-6553(95)90070-5. [DOI] [PubMed] [Google Scholar]
- 14.Cardoso CL, Pereira HH, Zequim JC, Guilhermetti M. Effectiveness of hand-cleansing agents for removing Acinetobacter baumannii strain from contaminated hands. Am J Infect Control. 1999;27:327–331. doi: 10.1016/s0196-6553(99)70052-0. [DOI] [PubMed] [Google Scholar]
- 15.Guilhermetti M, Hernandes SE, Fukushigue Y, Garcia LB, Cardoso CL. Effectiveness of hand-cleansing agents for removing methicillin-resistant Staphylococcus aureus from contaminated hands. Infect Control Hosp Epidemiol. 2001;22:105–108. doi: 10.1086/501872. [DOI] [PubMed] [Google Scholar]
- 16.Wade JJ, Desai N, Casewell MW. Hygienic hand disinfection for the removal of epidemic vancomycin-resistant Enterococcus faecium and gentamicin-resistant Enterobacter cloacae. J Hosp Infect. 1991;18:211–218. doi: 10.1016/0195-6701(91)90145-x. [DOI] [PubMed] [Google Scholar]
- 17.Bartzokas CA, Gibson MF, Graham R, Pinder DC. A comparison of triclosan and chlorhexidine preparations with 60 per cent isopropyl alcohol for hygienic hand disinfection. J Hosp Infect. 1983;4:245–255. doi: 10.1016/0195-6701(83)90025-7. [DOI] [PubMed] [Google Scholar]
- 18.Ayliffe GAJ, Babb JR, Davies JG, Lilly HA. Hand disinfection: a comparison of various agents in laboratory and ward studies. J Hosp Infect. 1988;11:226–243. doi: 10.1016/0195-6701(88)90101-6. [DOI] [PubMed] [Google Scholar]
- 19.Coignard B, Grandbastien B, Berrouane Y, Krembel C, Queverue M, Salomez JL, et al. Handwashing quality: Impact of a special program. Infect Control Hosp Epidemiol. 1998;19:510–513. doi: 10.1086/647860. [DOI] [PubMed] [Google Scholar]
- 20.Gould D. Nurses' hand decontamination practice: results of a local study. J Hosp Infect. 1994;28:15–30. doi: 10.1016/0195-6701(94)90149-x. [DOI] [PubMed] [Google Scholar]
- 21.Lund S, Jackson J, Leggett J, Hales L, Dworkin R, Gilbert D. Reality of glove use and handwashing in a community hospital. Am J Infect Control. 1994;22:352–357. doi: 10.1016/0196-6553(94)90034-5. [DOI] [PubMed] [Google Scholar]
- 22.Voss A, Widmer AF. No time for handwashing!? Handwashing versus alcoholic rub: can we afford 100% compliance? Infect Control Hosp Epidemiol. 1997;18:205–208. doi: 10.1086/647590. [DOI] [PubMed] [Google Scholar]
- 23.Paulson DS, Fendler EJ, Dolan MJ, Williams RA. A close look at alcohol gel as antimicrobial sanitizing agent. Am J Infect Control. 1999;27:332–338. doi: 10.1016/s0196-6553(99)70053-2. [DOI] [PubMed] [Google Scholar]
- 24.Pittet D, Hugonnet S, Harbath S, Mourouga P, Sauvan V, Touveneau S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Lancet. 2000;356:1307–1312. doi: 10.1016/s0140-6736(00)02814-2. [DOI] [PubMed] [Google Scholar]