Abstract
Background
Temporomandibular joint disorders (TMDs) cause pain and functional restrictions in the temporomandibular joint that interfere with daily activities. This study aimed to evaluate and compare the effectiveness and safety of various traditional East Asian medicine treatments, including acupuncture, electroacupuncture, moxibustion, and herbal medicine, in the management of TMD.
Methods
We included searches of MEDLINE, CENTRAL, EMBASE, AMED, CINAHL, OASIS, KISS, RISS, KMbase, KCI, CNKI, and CiNii from inception to November 12, 2023, for randomized controlled trials of traditional East Asian medicine treatments in patients with TMD. A network meta-analysis was performed using frequentist methods, and the Confidence In Network Meta-Analysis methodology were employed to assess evidence quality.
Results
Forty-five studies with 2,211 participants were finally included. Acupotomy (Mean difference (MD) -5.07, 95 % Confidence interval (CI) -7.37 to -2.78) and acupuncture (MD -1.18, 95 % CI -2.28 to -0.09) showed statistically significant superiority in reducing pain intensity compared to sham treatment. According to the SUCRA rankings, acupotomy was considered the most effective treatment, followed by electroacupuncture, acupuncture, manipulation, laser therapy and occlusal splint. A total of 12 studies reported incidence of adverse events, and none were serious adverse events.
Conclusion
Acupotomy and acupuncture could be more beneficial than sham treatment in pain relief and might be a better option than occlusal splint. However, future rigorous, well-designed trials are needed to draw clear conclusions.
Protocol registration
PROSPERO (CRD42023467340).
Keywords: Temporomandibular joint disorders, Traditional East Asian medicine, Acupuncture, Systematic review, Network meta-analysis
1. Introduction
Temporomandibular joint disorder (TMD) is marked by acute or chronic pain and dysfunction of the temporomandibular joint (TMJ), often accompanied by symptoms like headaches, earaches, and limited mandibular range of motion.1 According to data from South Korea's Healthcare Big Data Hub of the Health Insurance Review and Assessment Service, TMD cases, classified under the KCD (Korean Standard Classification of Diseases) code ‘K076’ for ‘temporomandibular joint disorders’, have steadily increased over the past decade. In 2010, there were 244,708 reported cases, rising to 484,241 by 2022.2
In the past, TMD was thought to result primarily from dental occlusion issues, but recent studies have revealed it is a much more complex disorder involving multiple contributing factors.3 These include trauma to the TMJ, cervical posture imbalances, and psychological factors. For instance, trauma from cervical sprains or jaw injuries can cause oxidative stress within the TMJ, leading to inflammation and degenerative changes.4 Moreover, poor head and neck posture can worsen TMD symptoms due to the close relationship between the mandible, head, and neck muscles.5 Psychological factors such as stress and anxiety are also known to influence the onset and progression of TMD by contributing to muscle tension and altered pain perception mechanisms.6
The diagnosis of TMD encompasses a range of TMD categories, including pain-related TMD, which primarily focuses on pain; intra-articular TMD, characterized by joint crepitus or locking symptoms; and degenerative TMD, which results from joint degeneration.7 Common treatments for TMD include occlusal splints, non-steroidal anti-inflammatory drugs (NSAIDs), physical therapy, injections, and surgery, with an emphasis on less invasive, reversible treatments.8 However, despite the variety of conventional options, many patients experience only partial relief, leading to an increased interest in integrative approaches.9
In recent years, traditional East Asian medicine has gained attention as a complementary approach to managing TMD. Traditional East Asian medicine treatments such as acupuncture, moxibustion, cupping, and herbal medicine target both the localized symptoms and systemic imbalances that contribute to TMD, offering a holistic perspective on pain and functional restoration.10
In South Korea, a research on clinical practice trends in TMD treatment reveals that non-pharmacological approaches, particularly occlusal splint and acupuncture, have gained popularity over the years.11 Based on this, the occlusal splint was selected among the common treatments and the effectiveness of the common treatment and traditional East Asian medicine was compared.
Although several systematic reviews have been conducted on individual treatments such as laser therapy,12 acupuncture,13 warm acupuncture,14 and manual therapy,15 these reviews focus on specific interventions and do not comprehensively cover the broader spectrum of traditional East Asian medicine treatments. Furthermore, no systematic review or network meta-analysis (NMA) has been conducted to evaluate the full range of traditional East Asian medicine treatments for TMD, including acupuncture, moxibustion, cupping, chuna, and herbal medicine. Therefore, this study aims to fill this gap by analyzing the effectiveness of these clinically used treatments. By employing conventional pair-wise meta-analysis (PMA) and NMA methodologies, this study seeks to identify which treatments are most beneficial and comparatively effective, providing valuable insights for the management of TMD.
2. Methods
2.1. Protocol and registration
The study protocol was registered with PROSPERO (CRD42023467340), and the study was reported in accordance with the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) 2020 guidelines and the PRISMA Extension version (PRISMA-NMA) (Supplement 1).16,17
2.2. Search strategies
Articles published up to November 12, 2023 were searched in five English databases (MEDLINE, Cochrane Central Register of Controlled Trials (CENTRAL), EMBASE, Allied and Complementary Medicine Database (AMED), Cumulative Index to Nursing and Allied Health Literature (CINAHL)), six Korean databases (Oriental Medicine Advanced Searching Integrated System (OASIS), Korean studies Information Service System (KISS), Research Information Service System (RISS), Korean Medical Database (KMbase), Korea Citation Index (KCI)), one Chinese database (China National Knowledge Infrastructure (CNKI)), and one Japanese database (CiNii) without restrictions on publication date or language. The search strategy is available in the Supplement 2.
2.3. Eligibility criteria
2.3.1. Study types
Only parallel-designed RCTs were included. Quasi RCTs, cross-over studies, cluster RCTs, controlled (non-randomized) clinical trials (CCTs), cluster trials, case series, and case reports were excluded to minimize potential bias.
2.3.2. Participant types
Studies of myogenous, arthrogenous, or mixed TMD were included, based on either the Research Diagnostic Criteria for TMD (RDC/TMD) or the revised dual-axis Diagnostic Criteria for TMD (DC/TMD) protocol,7,18 or through a clear clinical diagnosis including signs and symptoms of TMD. Studies in people with any inflammatory or rheumatic joint disorders, congenital abnormalities, neoplastic conditions in the TMJ region, and TMD induced by prior surgical procedures were excluded.
2.3.3. Intervention types
The intervention included occlusal splints and a range of traditional East Asian medicine interventions that are commonly administered in Korean Medicine clinics. These treatments encompassed acupuncture, warm acupuncture, fire acupuncture, electroacupuncture, pharmacopuncture, laser therapy, moxibustion, cupping, herbal medicine, chuna, and exercise. Since exercise is often prescribed as part of a comprehensive traditional East Asian medicine treatment plan, it was included as an intervention in this study. To objectively compare the effectiveness of the intervention, only studies that applied it as a single treatment were included, and studies that used it as a combination treatment were excluded. In multi-arm trials, study groups assessing interventions other than those mentioned above were not eligible.
2.3.4. Outcomes measures
The primary outcome was pain intensity evaluated using the Visual Analogue Scale (VAS), Numerical Rating Scale (NRS), and validated other self-reported pain assessment tools. The pain intensity measured by the VAS is quantified on a scale from 0 to 100, while the NRS is quantified on a scale from 0 to 10. Based on prior research, the VAS scores are rescaled to a 0 to 10 scale to facilitate comparability in meta-analyses and mean difference (MD) is employed for the pooled estimates in these analyses.19
Secondary outcome measures were maximum mouth opening (MMO) and incidence of adverse events during the treatment period. For studies with multiple time points of assessment, the evaluation at 4 weeks was designated as the representative point. In the absence of 4 weeks outcomes, results from the nearest time point were selected for consideration. Outcomes of all data forms were extracted as reported in the included studies.
2.4. Study selection and data extraction
Two review authors (S Ha and S Kang) independently screened the titles and abstracts and then the full texts, and extracted data on basic information, baseline characteristics, treatment specifics, and outcomes using EndNote Software 20 (Clarivate Analytics, CA) and a standardized Excel spreadsheet format. Any disagreements were resolved through discussion with a third independent author (S Lee).
2.5. Risk of bias assessment
The methodological quality of the included studies was assessed independently by two authors (S Ha and S Kang) using the Cochrane Risk of Bias 2 assessment tool.20 In the event of any disagreements, a third reviewer (S Lee) were consulted to facilitate resolution.
2.6. Certainty of evidence
The quality of evidence for all outcomes was evaluated using the Confidence In Network Meta-Analysis (CINeMA) methodology (https://cinema.ispm.unibe.ch/). This assessment encompasses domains such as within-study bias, reporting bias, indirectness, imprecision, heterogeneity, and incoherence. The quality of evidence was categorized as high, moderate, low, or very low based on this evaluation.21,22 To assess imprecision, the minimum clinically important difference was established at 1.90 on a scale of 0–10 for pain intensity and 2.5 mm for MMO.23
2.7. Statistical methods
In the conventional PMA, the “meta” package available in the R program (R version 4.2.2, Foundation for Statistical Computing, Vienna, Austria) was utilized for data analysis.24 Continuous data was presented as a MD with 95 % confidence interval (CI). To assess heterogeneity among the studies, the I² statistic were used, considering heterogeneity significant if it exceeded 75 %. Furthermore, χ² test was employed, considering a p-value lesser than 0.1 as an indication that the studies were heterogeneous.25 The random-effects model was employed for analysis because TMD encompasses a wide variety of clinical conditions.
To conduct frequentist NMA, the “netmeta” package available in the R program was utilized.26 The raw data, which included information about the study, sample size, mean, standard deviation, and treatment, was transformed into effect size data using the pairwise function. The reference variable was set up as sham treatment group, and the effect size was expressed as the MD. A network plot was generated to visually represent the direct comparison relationships between treatment groups. In this plot, the thickness of the edges connecting each node indicates the number of comparisons between interventions. To assess clinical and methodological similarities and ensure logical transitivity between studies, study characteristics, including potential effect modifiers such as sample size, age, gender, treatment dosage, and treatment duration were qualitatively compared for each study. To test for consistency, both global and local approaches are employed. The global approach is conducted using a design-by-treatment interaction model by inserting a network model into the “decomp.design” function and testing the linearity of the regression coefficients for the entire model using the Wald test. If the p-value is greater than 0.05, it supports the null hypothesis of consistency, and the network model is adopted.27 For individual treatment comparisons, the local approach is conducted using node-splitting method by inserting a network model into the “netsplit” function. In individual comparisons, if the p-value is <0.1, it is considered inconsistent, and caution is advised when interpreting the treatment results.28,29 Additionally, a league table using P-scores and a ranking metric using surface under the cumulative ranking curve (SUCRA) were presented to illustrate the comparative advantages between treatments.30 Due to the limited number of studies included for multiple comparisons, subgroup or sensitivity analyses could not be conducted. Funnel plots were employed for the assessment of publication bias within NMA.
3. Results
3.1. Study characteristics
A total of 4,885 records identified. After duplicate papers were removed, 3,410 papers were screened for title and abstract. Forty-five papers with 2,211 participants were finally included after screening full text. The study selection process is presented in a PRISMA flow chart (Supplement 3).
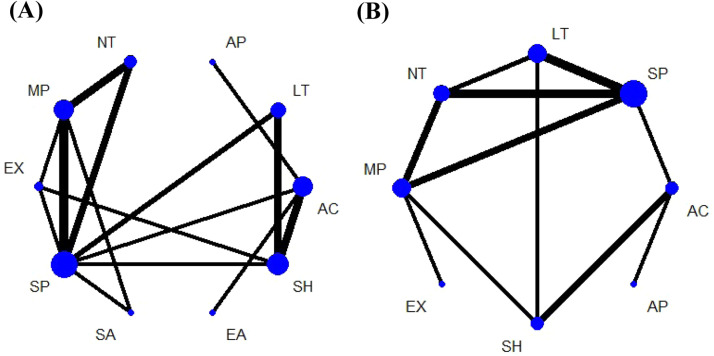
The included studies consisted of 31 two-arm comparative studies,31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61 12 three-arm comparative studies,62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73 and 2 four-arm comparative studies.74,75 The included studies conducted in a total of 15 different countries: 14 studies from Brazil,36,37,39,40,42,45, 46, 47, 48, 55,59,61,64,67 7 from Turkey,32,34,44,52,63,72,74 5 from Egypt,31,33,62,65,69 3 each from China,41,43,70 and Japan,51,54,56 2 each from Croatia,38,68 Spain,50,58 and USA,57,75 1 each from Australia,49 India,66 Iran,71 Italy,35 Jordan,73 Switzerland,53 and the United Kingdoms.60 The following 13 types of interventions were used: acupotomy, acupuncture, ear acupuncture, electroacupuncture, exercise, laser therapy, manipulation, moxibustion, no treatment, sham treatment, scalp acupuncture, occlusal splint, and warm acupuncture. A total of 37 studies, reporting the primary outcome of pain intensity measured through either VAS or NRS, were included. Nine studies were excluded due to missing mean or standard deviation values.33,37,38,50,60,61,69,72,75 The secondary outcome, MMO, was reported from 28 studies. Three studies that did not provide mean or standard deviation values was excluded.38,50,60 Regarding adverse events, a total of 12 studies discussed this aspect. Characteristics of included studies are described in Table 1. Fig. 1 shows network plots for the available direct comparisons between treatments for pain intensity and range of motion. Each node represents a treatment, and the lines between nodes indicate direct comparisons between these treatments in the included studies. The thickness of the lines corresponds to the number of studies, with thicker lines indicating more comparisons.
Table 1.
Characteristics of the included studies.
| First author (Year) | Country | Age (year) | Sample size (M/F) | Treatment intervention | Outcome of interest reported | Overall risk of bias |
|---|---|---|---|---|---|---|
| Benli (2023)32 |
Turkey | (A) 39.1 (B) 39.1 |
(A) 30(6/24) (B) 30(6/24) |
(A) Massage (B) No treatment |
VAS MMO |
Some concerns |
| El‐Shaheed (2023)31 |
Egypt | (A) 26.2 (B) 26.3 |
(A) 14(2/12) (B) 14(3/11) |
(A) Low-level laser therapy (B) Stabilization splint |
VAS MMO |
Low |
| Emam (2023)62 |
Egypt | 21–44 | (A) 25 (B) 24 (C) 23 |
(A) Low-level laser therapy (B) Anterior repositioning splint (C) Stabilization splint |
MMO AE |
Some concerns |
| Aroca (2022)64 |
Brazil | (A) 22.8 (B) 27.6 (C) 29.8 |
(A) 13(0/13) (B) 14(1/13) (C) 14(2/12) |
(A) Ear acupuncture (B) Occlusal splint (C) Sham acupuncture |
VAS MMO |
Some concerns |
| Damar Örenler (2022)34 |
Turkey | (A) 29.0 (B) 27.8 |
(A) 15(0/15) (B) 14(0/14) |
(A) Manipulation (B) Stabilization splint |
VAS MMO |
Some concerns |
| Ekici (2022)63 |
Turkey | (A) 28.6 (B) 31.5 (C) 29.5 |
(A) 34(10/24) (B) 32(10/22) (C) 34(3/31) |
(A) Stabilization splint (B) High-level laser therapy (C) No treatment |
VAS MMO AE |
Some concerns |
| Rady (2022)33 |
Egypt | (A) 23.2 (B) 24.2 |
(A) 9(0/9) (B) 9(1/8) |
(A) Low-level laser therapy (B) Anterior repositioning splint |
VAS AE |
High |
| de Resende (2021)36 |
Brazil | 28.0 | (A) 21 (B) 22 |
(A) Manipulation (B) Occlusal splint |
VAS | High |
| El Zawahry (2021)69 |
Egypt | 25.0 | (A) 10 (B) 10 (C) 10 |
(A) Anterior repositioning splint (B) Low-level laser therapy (C) Sham laser |
VAS | High |
| Eraslan (2021)74 |
Turkey | (A) 24.2 (B) 30.3 (C) 28.3 (D) 23.1 |
(A) 20(4/16) (B) 20(4/16) (C) 20(4/16) (D) 10(2/8) |
(A) Low-level laser therapy (B) Stabilization splint (C) Anterior repositioning splint (D) No treatment |
MMO | Some concerns |
| Gikić (2021)68 |
Croatia | (A) 35.5 (B) 35.7 (C) 38.2 |
(A) 10(0/10) (B) 10(0/10) (C) 10(0/10) |
(A) Exercise (B) Stabilization splint (C) Sham splint |
VAS MMO AE |
Some concerns |
| Peixoto (2021)67 |
Brazil | 18–65 | (A) 15 (B) 15 (C) 15 |
(A) Scalp acupuncture (B) Manipulation (C) Occlusal splint |
VAS | High |
| Ram (2021)66 |
India | (A) 37.6 (B) 42.3 (C) 37.5 |
(A) 37 (B) 37 (C) 36 |
(A) Manipulation (B) Stabilization splint (C) No treatment |
VAS MMO |
Some concerns |
| Serritella (2021)35 |
Italy | (A) 48.3 (B) 38.5 |
(A) 20(3/17) (B) 20(4/16) |
(A) Acupuncture (B) Electroacupuncture |
VAS AE |
Some concerns |
| Shousha (2021)65 |
Egypt | (A) 26.2 (B) 25.7 (C) 27.3 |
(A) 37(0/37) (B) 37(0/37) (C) 38(0/38) |
(A) Low-level laser therapy (B) Stabilization splint (C) No treatment |
VAS | Some concerns |
| de Salles-Neto (2020)37 |
Brazil | (A) 37.5 (B) 41.4 |
(A) 16(0/16) (B) 16(0/16) |
(A) Acupuncture (B) Sham acupuncture |
VAS AE |
Some concerns |
| Madani (2020)71 |
Iran | (A) 32.0 (B) 43.0 (C) 35.0 |
(A) 15(5/10) (B) 15(6/9) (C) 15(2/13) |
(A) Low-level laser therapy (B) Laser acupuncture (C) Sham laser |
VAS MMO |
High |
| Pan (2020)70 |
China | (A) 34.2 (B) 34.5 (C) 34.5 |
(A) 25(11/14) (B) 25(10/15) (C) 25(10/15) |
(A) Manipulation (B) Stabilization splint (C) No treatment |
VAS MMO |
Some concerns |
| Calixtre (2019)40 |
Brazil | (A) 26.1 (B) 26.3 |
(A) 30(0/30) (B) 31(0/31) |
(A) Manipulation (B) No treatment |
VAS AE |
Low |
| Rodrigues (2019)39 |
Brazil | (A) 47.5 (B) 43.6 |
(A) 11(0/11) (B) 10(0/10) |
(A) Laser acupuncture (B) Occlusal splint |
VAS MMO |
High |
| Vrbanović (2019)38 |
Croatia | (A) 38.9 (B) 32.7 |
(A) 17(0/17) (B) 13(0/13) |
(A) Stabilization splint (B) Placebo splint |
VAS MMO |
High |
| Xie (2018)41 |
China | (A) 38.4 (B) 40.6 |
(A) 60(34/26) (B) 66(26/40) |
(A) Acupotomy (B) Acupuncture |
VAS MMO |
Some concerns |
| Hosgor (2017)44 |
Turkey | 30.4 | (A) 10 (B) 10 |
(A) Stabilization splint (B) Low-level laser therapy |
VAS MMO |
Some concerns |
| Huang (2017)43 |
China | (A) 37.0 (B) 36.0 |
(A) 40(17/23) (B) 40(18/22) |
(A) Moxibustion (B) Warm acupuncture |
VAS MMO |
Some concerns |
| Zotelli (2017)42 |
Brazil | (A) 38.0 (B) 35.1 |
(A) 20(2/18) (B) 20(6/14) |
(A) Acupuncture (B) Sham acupuncture |
NRS MMO |
Some concerns |
| Packer (2015)45 |
Brazil | (A) 23.5 (B) 26.1 |
(A) 16(0/16) (B) 16(0/16) |
(A) Manipulation (B) Sham manipulation |
MMO | Low |
| Grillo (2015)46 |
Brazil | 30.0 | (A) 20(0/20) (B) 20(0/20) |
(A) Acupuncture (B) Occlusal splint |
VAS MMO |
Some concerns |
| de Moraes Maia (2014)48 |
Brazil | 27.8 | (A) 12 (B) 9 |
(A) Low-level laser therapy (B) Sham laser |
VAS | High |
| De Paula Gomes (2014)47 |
Brazil | (A) 30.1 (B) 29.7 |
(A) 14(4/10) (B) 14(4/10) |
(A) Massage (B) Stabilization splint |
MMO | Low |
| Demirkol (2014)72 |
Turkey | NA | (A) 10 (B) 10 (C) 10 |
(A) Low-level laser therapy (B) Stabilization splint (C) Sham laser |
VAS AE |
Some concerns |
| DeVocht (2013)75 |
USA | (A) 31.7 (B) 36.9 (C) 33.1 (D) 38.0 |
(A) 20(4/16) (B) 20(3/17) (C) 19(4/15) (D) 21(5/16) |
(A) Manipulation (B) Stabilization Splint (C) Sham manipulation (D) No treatment |
NRS | Some concerns |
| Kalamir (2013)49 |
Australia | (A) 28.2 (B) 26.8 |
(A) 23(9/14) (B) 23(8/15) |
(A) Manipulation (B) Exercise |
NRS MMO AE |
Low |
| Itoh (2012)51 |
Japan | (A) 21.7 (B) 21.4 |
(A) 7 (B) 8 |
(A) Acupuncture (B) Sham acupuncture |
VAS MMO AE |
Some concerns |
| Vicente-Barrero (2012)50 |
Spain | 39.0 | (A) 10(2/8) (B) 10(1/9) |
(A) Acupuncture (B) Stabilization Splint |
VAS MMO |
High |
| Asai (2010)56 |
Japan | (A) 21.6 (B) 21.4 |
(A) 17(4/13) (B) 17(3/14) |
(A) Acupuncture (B) Sham acupuncture |
VAS MMO |
Some concerns |
| de Felício (2010)55 |
Brazil | (A)29.0 (B)34.0 |
(A) 10(0/10) (B) 10(0/10) |
(A) Stabilization splint (B) No treatment |
MMO | Some concerns |
| Gotou (2010)54 |
Japan | (A) 33.6 (B) 38.1 |
(A) 17(4/13) (B) 17(3/14) |
(A) Manipulation (B) Exercise |
NRS MMO |
Some concerns |
| Katsoulis (2010)53 |
Switzerland | (A) 34.0 (B) 28.0 |
(A) 3 (B) 4 |
(A) Laser acupuncture (B) Sham laser |
VAS | High |
| Öz (2010)52 |
Turkey | (A) 31.3 (B) 34.5 |
(A) 20(3/17) (B) 20(3/17) |
(A) Low-level laser therapy (B) Stabilization splint |
VAS MMO AE |
High |
| Shen (2009)57 |
USA | (A) 36.9 (B) 44.8 |
(A) 16(0/16) (B) 12(0/12) |
(A) Acupuncture (B) Sham acupuncture |
NRS | Some concerns |
| Mansilla Ferragud (2008)58 |
Spain | (A) 37.0 (B) 36.0 |
(A) 26(7/19) (B) 26(5/21) |
(A) Manipulation (B) No treatment |
MMO | Some concerns |
| Frare (2008)59 |
Brazil | 27.0 | (A) 10(0/10) (B) 8(0/8) |
(A) Low-level laser therapy (B) Sham laser |
VAS AE |
High |
| Smith (2007)60 |
United Kingdom | (A) 38.3 (B) 43.2 |
(A) 15(13/2) (B) 12(11/1) |
(A) Acupuncture (B) Sham acupuncture |
VAS MMO |
High |
| Mazzetto (2007)61 |
Brazil | NA | (A) 12 (B) 12 |
(A) Low-level laser therapy (B) Sham laser |
VAS | Some concerns |
| Al Quran (2006)73 |
Jordan | (A) 32.7 (B) 31.8 (C) 36.0 |
(A) 38 (B) 38 (C) 38 |
(A) Anterior repositioning splint (B) Stabilization splint (C) No treatment |
VAS | Some concerns |
AE, adverse events; F, female; M, male; MMO, maximum mouth opening; NA, not applicable; NRS, numeric rating scale; SD, standard deviation; VAS, visual analogue scale.
Fig. 1.
Network plot of available direct comparisons on each outcome. (A) pain intensity (B) range of motion. Abbreviations: AC, acupuncture; AP, acupotomy; EA, electroacupuncture; EX, exercise; LT, laser therapy; MP, manipulation; NT, no treatment; SA, scalp acupuncture; SH, sham treatment; SP, occlusal splint.
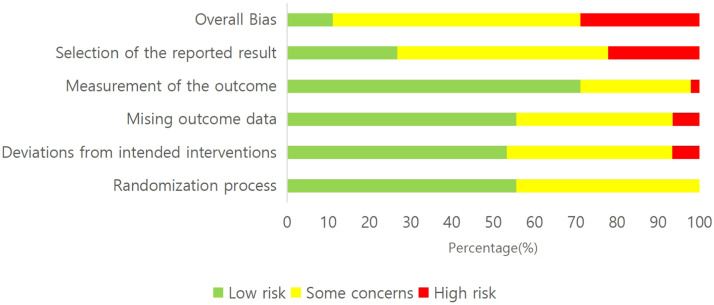
3.2. Risk of bias assessment
Regarding the risk of bias of the studies, >50 % of the studies were judged to be low risk in the areas of randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and <10 % were judged to be high risk. On the other hand, there was prevalent of high risk in the selection bias of the reported results, with 10 studies suspected of having performed multiple measurements or multiple analyses of the outcome data. The overall bias was assessed as being of some concerns in 27 studies, and at high risk in 13 studies. Most of the studies judged to be high risk were due to high risk in the selection bias of the reported result (Fig. 2 and Supplement 4).
Fig. 2.
Summary of risk of bias as percentage based on the Cochrane Risk of Bias 2.0 tool.
3.3. Meta-analysis
3.3.1. Pain intensity
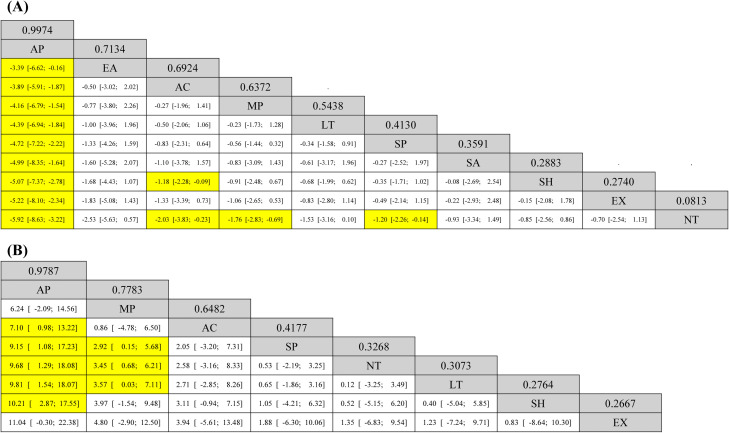
In total, twenty-one RCTs were included in the analysis of the pain intensity. The PMA showed that there were significant differences in pain intensity between acupuncture and acupotomy (1 study, MD 3.89, 95 % CI 3.39 to 4.39), exercise and manipulation (1 study, MD 0.87, 95 % CI 0.50 to 1.24), manipulation and no treatment (3 studies, MD −1.42, 95 % CI −2.21 to −0.62, I2=69 %), and no treatment and occlusal splint (3 studies, MD 1.49, 95 % CI 0.94 to 2.04, I2=53 %) (Supplement 5). Fig. 3A presents a league table showing the pairwise comparisons of pain intensity between different treatments. Treatments are ranked by their P-scores, which indicate the probability of being the best treatment. Each cell displays the MD in pain intensity between the column and row treatments, along with 95 % CI. Significant pairwise comparisons are highlighted in yellow. The NMA showed that acupotomy significantly reduced the pain intensity compared to electroacupuncture, acupuncture, manipulation, laser therapy, occlusal splint, scalp acupuncture, sham treatment, exercise, and no treatment. Additionally, acupuncture, manipulation, and occlusal splint significantly reduced the pain intensity compared with no treatment, and acupuncture reduced it compared with sham treatment. As a result of cumulative ranking probabilities using SUCRA for pain intensity, acupotomy was the optimal treatment, followed by electroacupuncture, acupuncture, manipulation, laser therapy, scalp acupuncture, occlusal splint, sham treatment, exercise, and no treatment (Supplement 6).
Fig. 3.
(A) League table of pain intensity. (B) League table of maximum mouth opening. The league table shows the pair-wise comparisons in network meta-analysis (the column's treatment vs. the row's treatment). Treatments are ordered in the rank of their chance of being the best treatment. Numbers in grey boxes are P-scores, which are used to rank the treatments. Significant pairwise comparisons are coloured in yellow boxes. Abbreviations: AC, acupuncture; AP, acupotomy; EA, electroacupuncture; EX, exercise; LT, laser therapy; MP, manipulation; NT, no treatment; SA, scalp acupuncture; SH, sham treatment; SP, occlusal splint.
3.3.2. MMO
Twenty-two RCTs were included in the analysis of the MMO. The PMA showed that there were significant differences in MMO between acupuncture and acupotomy (1 study, MD −7.10, 95 % CI −8.53 to −5.67), manipulation and no treatment (4 studies, MD 2.62, 95 % CI 0.21 to 5.03, I2=91 %), and manipulation and occlusal splint (4 studies, MD 4.09, 95 % CI 0.12 to 8.07, I2=92 %) (Supplement 7). Fig. 3B shows a league table for MMO comparisons between treatments. Similar to Fig. 3A, treatments are ranked by their P-scores, with higher scores indicating better effectiveness. Each cell presents the MD in MMO between the column and row treatments, alongside 95 % CI. Significant differences are highlighted in yellow. The NMA showed that acupotomy significantly increased the MMO compared to acupuncture, occlusal splint, no treatment, laser therapy, and sham treatment. Additionally, manipulation significantly increased the MMO compared to occlusal splint, no treatment, and laser therapy. As a result of cumulative ranking probabilities using SUCRA for MMO, acupotomy was the optimal treatment, followed by manipulation, acupuncture, occlusal splint, no treatment, laser therapy, exercise, and sham treatment (Supplement 8).
3.3.3. Adverse events
A total of 12 studies evaluated adverse events. None of the included studies reported any serious adverse events. Two studies reported minor adverse events such as pain, hematomas, and slight swelling after acupuncture.35,37 In one study using trigger point acupuncture, one patient withdrew due to worsening symptoms.51 Nine studies reported adverse events were not observed during the study.33,40,49,52,59,62,63,68,72
3.4. Publication bias
The network funnel plots for each outcome show relatively symmetrical shapes suggesting a lower likelihood of publication bias, as it implies that studies with both positive and negative results are distributed evenly across the range of precision (Supplement 9).
3.5. Certainty of the evidence
The certainty of evidence from the network meta-analyses was evaluated using the CINeMA methodology, considering six key domains: within-study bias, reporting bias, indirectness, imprecision, heterogeneity, and incoherence. Given that most individual studies were assessed with “some concerns” regarding overall bias, within-study bias was also evaluated as “some concerns”. In several studies, imprecision was deemed to have “major concerns” as it failed to meet the criteria for a minimum clinically important difference. Additionally, heterogeneity among individual studies raised “some concerns”. With downgrades primarily observed in these three areas, the level of evidence across most studies was rated as low to very low (Supplement 10).
4. Discussion
4.1. Summary of evidence
A comprehensive search across English, Korean, Chinese and Japanese databases yielded a total of 4,885 studies. Forty-five studies were ultimately selected for analysis, with 36 studies included in meta-analysis. A total of 13 interventions were included, and the most frequently used interventions were occlusal splint, manipulation, and acupuncture. In terms of the primary outcome, pain intensity, acupotomy significantly reduces pain intensity. Regarding the rank of treatments using SUCRA, acupotomy, electroacupuncture, acupuncture, manipulation, laser therapy, scalp acupuncture, and occlusal splint are superior in pain reduction in that order. However, upon examining the network plot, acupotomy and electroacupuncture have only one connected edge, both linked to acupuncture. Additionally, the forest plot of PMA shows that there is a statistically significant difference between acupuncture and acupotomy, and the difference is the largest among all comparisons. Consequently, the effects of acupotomy and electroacupuncture may be exaggerated, making it challenging to interpret acupotomy as the optimal treatment and electroacupuncture as the next best. On the other hand, the treatment of the subsequent ranking, acupuncture can be considered more effective based on the cumulative probability plots for relieving pain than other treatments. This is because not only are there many studies comparing it to sham treatment, which is the reference treatment, but also there is a significant difference in network estimates. In terms of the secondary outcome, MMO, acupotomy significantly increases the range of motion. Regarding the rank of treatments using SUCRA, acupotomy, manipulation, acupuncture, and occlusal splint are excellent in increasing the range of motion in that order. However, for the same reason, it is difficult to interpret acupotomy as the best treatment because its effects may be exaggerated. On the other hand, the treatment of the subsequent ranking, manipulation and acupuncture are stably connected in the network plot due to the large number of compared studies. Particularly, in the case of manipulation, compared to occlusal splint, both direct estimate and network estimate were found to have significant differences, so it can be considered effective in increasing the range of mouth opening. In terms of safety, 12 of 45 studies evaluated adverse events, and none of the included studies reported any serious adverse events. Two studies reported minor side effects, and one study reported that trigger point acupuncture led to worsening symptoms in one patient, leading to discontinuation. The remaining nine studies reported that no adverse events were observed during the study period.
4.2. Comparison with previous study - Clinical perspectives
Previous systematic reviews have focused on some individual treatments such as occlusal splint, acupuncture and manipulation. The effectiveness of occlusal splint, a commonly used intervention in clinical practice for TMD, has been a topic of ongoing debate.76,77 The controversy surrounding the usefulness of occlusal splint in treating TMD has prompted the need of alternative treatments. Some studies have shown that acupuncture may be a contender, with results that are similar to those of using occlusal splint in reducing pain intensity and improving range of motion.78, 79, 80 Manipulation also showed promising effects in the management of TMD.15,81 Consistent with the results of previous reviews, this review shows that acupuncture and manipulation may relieve pain intensity and improve range of motion, surpassing the effects of occlusal splint or sham treatment. However, it is important to note that the confidence in these results is tempered by the overall quality and nature of the available evidence, graded as low to very low. Most of the existing evidence relates to acupuncture and manipulation, with limited evidence for acupotomy and electroacupuncture. This lack of evidence should not be interpreted as an absence of efficacy but rather highlights the need for more robust further researches.
4.3. Comparison with previous study - Methodological perspective
This study is the first to conduct a systematic review and NMA on the effectiveness of traditional East Asian medicine treatment for TMD patients. Although clinical practice guidelines for TMD in Korean Medicine have been published, only qualitative evaluation of each intervention was conducted and quantitative analysis was not performed, making it difficult to objectively evaluate the treatment effect.82 Existing systematic reviews on various treatments for TMD have searched studies using dry needling, but only needling in the concept of stimulating trigger points were included.83,84 Therefore, none have undertaken a comprehensive analysis of the comparative effectiveness of various traditional East Asian medicine treatments including acupuncture-related modalities through systematic review and NMA. The findings suggest that, in comparison to the frequently employed occlusal splint, traditional East Asian medicine treatments such as acupuncture and manipulation could be effective treatment options for TMD.
4.4. Limitations of review
There are several limitations in this review. First, this study included only monotherapy to objectively evaluate the treatment effect. If sufficient RCTs are conducted in the future, it will be necessary to analyze the effectiveness of combination therapies used in actual clinical practice. Second, given the inclusion of sham treatment as reference treatment, we decided to conduct separate analyses for pharmacological and non-pharmacological interventions. To explore the status of research on traditional East Asian medicine treatments, the search encompassed herbal medicine and pharmacopuncture, but there were no eligible studies. If research on pharmacological intervention in traditional East Asian medicine is conducted in the future, it will be necessary to evaluate comparisons between pharmacological interventions such as NSAIDs and injections. Finally, regarding safety considerations, the insufficient reporting of adverse events across the included studies hinders conclusive assessments. While the limited reporting might suggest a general safety profile for non-pharmacological treatments, it also raises concerns about potential underreporting of dropout rates and adverse events in these studies. In the future studies, it needs to adopt more rigorous reporting standards for dropout rates and occurrences of adverse events.
4.4. Clinical and research implications
Acupotomy has been ranked highest in terms of comparative effectiveness for alleviating TMD pain and improving the range of mouth opening. However, the reliability of these findings is hindered by the scarcity of related research. Consequently, there is an immediate need for robust evidence supporting various traditional East Asian medicine treatments, including electroacupuncture, acupuncture, and manipulation, as well as acupotomy, through well-designed RCTs on TMD.
4.5. Conclusion
This systematic review represents the first comprehensive attempt to assess the effectiveness of various traditional East Asian medicine treatment for TMD. In the absence of a definitive gold standard for TMD management, this study showed the potential efficacy of traditional East Asian medicine treatments, specifically highlighting acupuncture and manipulation as promising options. However, the robustness of these findings is limited by the lack of related research, emphasizing the need for further high-quality research to inform evidence-based practices and enhance our understanding of optimal therapeutic approaches.
Author contributions
Conceptualization: SJH. Methodology: SJH, SWK. Software: SJH, SWK. Validation: SJH, SWK, SHL. Formal analysis: SJH, SWK. Investigation: SJH, SWK, SHL. Resources: SJH. Data curation: SJH, SWK. Writing – Original Draft: SJH. Writing – Review & Editing: SWK, SHL. Visualization: SJH. Supervision: SHL. Project administration: SHL.
Declaration of competing interest
The authors declare that they have no conflicts of interest.
Funding
None.
Ethical statement
Not applicable.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.imr.2024.101114.
Supplement 1. PRISMA NMA Checklist
Supplement 2. Search strategy
Supplement 3. Flow diagram of the study selection process
Supplement 4. Summary of risk of bias for each study based on Cochrane Risk of Bias 2.0 tool
Supplement 5. Pairwise meta-analysis for pain intensity
Supplement 6. Cumulative ranking probability plots (SUCRA) for pain intensity
Supplement 7. Pairwise meta-analysis for maximum mouth opening
Supplement 8. Cumulative ranking probability plots (SUCRA) for maximum mouth opening
Supplement 9. Comparison-adjusted funnel plots
Supplement 10. Level of evidence by CINeMA methodology
Supplement 11. Excluded studies and reason after full-text review
Appendix. Supplementary materials
Supplement 1. PRISMA NMA Checklist
Supplement 2. Search strategy
Supplement 3. Flow diagram of the study selection process
Supplement 4. Summary of risk of bias for each study based on Cochrane Risk of Bias 2.0 tool
Supplement 5. Pairwise meta-analysis for pain intensity
Supplement 6. Cumulative ranking probability plots (SUCRA) for pain intensity
Supplement 7. Pairwise meta-analysis for maximum mouth opening
Supplement 8. Cumulative ranking probability plots (SUCRA) for maximum mouth opening
Supplement 9. Comparison-adjusted funnel plots
Supplement 10. Level of evidence by CINeMA methodology
Supplement 11. Excluded studies and reason after full-text review
References
- 1.Cooper B.C., Kleinberg I. Examination of a large patient population for the presence of symptoms and signs of temporomandibular disorders. Cranio. 2007;25(2):114–126. doi: 10.1179/crn.2007.018. [DOI] [PubMed] [Google Scholar]
- 2.Service H.I.R.A. South Korea's healthcare big data hub of the health insurance review and assessment service, https://opendata.hira.or.kr/home.do. Accessed September 27, 2023.
- 3.Slade G.D., Ohrbach R., Greenspan J.D., Fillingim R.B., Bair E., Sanders A.E., et al. Painful Temporomandibular Disorder: Decade of Discovery from OPPERA Studies. J Dent Res. 2016;95(10):1084–1092. doi: 10.1177/0022034516653743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Milam S.B., Zardeneta G., Schmitz J.P. Oxidative stress and degenerative temporomandibular joint disease: a proposed hypothesis. J Oral Maxillofac Surg. 1998;56(2):214–223. doi: 10.1016/s0278-2391(98)90872-2. [DOI] [PubMed] [Google Scholar]
- 5.Forssell H., Kauko T., Kotiranta U., Suvinen T. Predictors for future clinically significant pain in patients with temporomandibular disorder: A prospective cohort study. Eur J Pain. 2017;21(1):188–197. doi: 10.1002/ejp.916. [DOI] [PubMed] [Google Scholar]
- 6.Ferrando M., Andreu Y., Galdón M.J., Durá E., Poveda R., Bagán J.V. Psychological variables and temporomandibular disorders: distress, coping, and personality. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98(2):153–160. doi: 10.1016/j.tripleo.2003.12.030. [DOI] [PubMed] [Google Scholar]
- 7.Schiffman E., Ohrbach R., Truelove E., Look J., Anderson G., Goulet J.P., et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache. 2014;28(1):6–27. doi: 10.11607/jop.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu F., Steinkeler A. Epidemiology, Diagnosis, and Treatment of Temporomandibular Disorders. Dent Clin North Am. 2013;57(3):465–479. doi: 10.1016/j.cden.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 9.Wieckiewicz M., Boening K., Wiland P., Shiau Y.Y., Paradowska-Stolarz A. Reported concepts for the treatment modalities and pain management of temporomandibular disorders. J Headache Pain. 2015;16:106. doi: 10.1186/s10194-015-0586-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Serritella E., Colombo V., Özcan M., Galluccio G., Di Paolo C. Acupuncture and Traditional Chinese Medicine in the Management of Orofacial Pain and Temporomandibular Disorders: a Narrative Review. Curr Oral Health Rep. 2024;11(1):59–67. [Google Scholar]
- 11.Jung S.Y., Kim E.S., Kim K.W., Cho J.H., Lee Y.J., Ha I.H. Treatment for temporomandibular disorders in South Korea: A 9-year trend using cluster analysis. J Oral Rehabil. 2022;49(7):691–700. doi: 10.1111/joor.13333. [DOI] [PubMed] [Google Scholar]
- 12.Ahmad S.A., Hasan S., Saeed S., Khan A., Khan M. Low-level laser therapy in temporomandibular joint disorders: a systematic review. J Med Life. 2021;14(2):148–164. doi: 10.25122/jml-2020-0169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jung A., Shin B.C., Lee M.S., Sim H., Ernst E. Acupuncture for treating temporomandibular joint disorders: a systematic review and meta-analysis of randomized, sham-controlled trials. J Dent. 2011;39(5):341–350. doi: 10.1016/j.jdent.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 14.Liu G.F., Gao Z., Liu Z.N., Yang M., Zhang S., Tan T.P. Effects of Warm Needle Acupuncture on Temporomandibular Joint Disorders: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Evid Based Complement Alternat Med. 2021;2021 doi: 10.1155/2021/6868625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Armijo-Olivo S., Pitance L., Singh V., Neto F., Thie N., Michelotti A. Effectiveness of Manual Therapy and Therapeutic Exercise for Temporomandibular Disorders: Systematic Review and Meta-Analysis. Phys Ther. 2016;96(1):9–25. doi: 10.2522/ptj.20140548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hutton B., Salanti G., Caldwell D.M., Chaimani A., Schmid C.H., Cameron C., et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–784. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- 18.Dworkin S.F., LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6(4):301–355. [PubMed] [Google Scholar]
- 19.Wewege M.A., Jones M.D., Williams S.A., Kamper S.J., McAuley J.H. Rescaling pain intensity measures for meta-analyses of analgesic medicines for low back pain appears justified: an empirical examination from randomised trials. BMC Med Res Methodol. 2022;22(1):285. doi: 10.1186/s12874-022-01763-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sterne J.A.C., Savović J., Page M.J., Elbers R.G., Blencowe N.S., Boutron I., et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 21.Nikolakopoulou A., Higgins J.P.T., Papakonstantinou T., Chaimani A., Del Giovane C., Egger M., et al. CINeMA: An approach for assessing confidence in the results of a network meta-analysis. PLoS Med. 2020;17(4) doi: 10.1371/journal.pmed.1003082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Papakonstantinou T., Nikolakopoulou A., Higgins J.P.T., Egger M., CINeMA Salanti G. Software for semiautomated assessment of the confidence in the results of network meta-analysis. Campbell Syst Rev. 2020;16(1):e1080. doi: 10.1002/cl2.1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Calixtre L.B., Oliveira A.B., Alburquerque-Sendín F., Armijo-Olivo S. What is the minimal important difference of pain intensity, mandibular function, and headache impact in patients with temporomandibular disorders? Clinical significance analysis of a randomized controlled trial. Musculoskeletal Science and Practice. 2020;46 doi: 10.1016/j.msksp.2020.102108. [DOI] [PubMed] [Google Scholar]
- 24.Shim S.R., Kim S.J. Intervention meta-analysis: application and practice using R software. Epidemiol Health. 2019;41 doi: 10.4178/epih.e2019008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Higgins J.P., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 26.Shim S.R., Kim S.J., Lee J., Rücker G. Network meta-analysis: application and practice using R software. Epidemiol Health. 2019;41 doi: 10.4178/epih.e2019013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jackson D., Barrett J.K., Rice S., White I.R., Higgins J.P. A design-by-treatment interaction model for network meta-analysis with random inconsistency effects. Stat Med. 2014;33(21):3639–3654. doi: 10.1002/sim.6188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dias S., Welton N.J., Caldwell D.M., Ades A.E. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. 2010;29(7-8):932–944. doi: 10.1002/sim.3767. [DOI] [PubMed] [Google Scholar]
- 29.Higgins J.P., Jackson D., Barrett J.K., Lu G., Ades A.E., White I.R. Consistency and inconsistency in network meta-analysis: concepts and models for multi-arm studies. Res Synth Methods. 2012;3(2):98–110. doi: 10.1002/jrsm.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rücker G., Schwarzer G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol. 2015;15(1):58. doi: 10.1186/s12874-015-0060-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.El-Shaheed N.H., Mostafa A.Z.H., Aboelez M.A. Efficacy of stabilisation splint and low-level laser therapy for patients with chronic closed lock from non-reducible displaced temporo-mandibular joint discs: a parallel randomised clinical trial. J Oral Rehabil. 2023;50(3):177–193. doi: 10.1111/joor.13405. [DOI] [PubMed] [Google Scholar]
- 32.Benli M., Olson J., Huck O., Özcan M. A novel treatment modality for myogenous temporomandibular disorders using aromatherapy massage with lavender oil: A randomized controlled clinical trial. CRANIO: The Journal of Craniomandibular & Sleep Practice. 2023;41(1):48–58. doi: 10.1080/08869634.2020.1819067. [DOI] [PubMed] [Google Scholar]
- 33.Rady N.A., Bahgat M.M., Abdel-Hamid A.M. Promising minimally invasive treatment modalities for symptomatic temporomandibular joint disc displacement with reduction: a randomized controlled clinical trial. BMC Oral Health. 2022;22(1):547. doi: 10.1186/s12903-022-02579-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Damar Örenler S., Tuncer A., Najafov E. A comparison of manual therapy and splint therapy in patients diagnosed with myofascial temporomandibular dysfunction with sleep bruxism. Turkish Journal of Physiotherapy and Rehabilitation. 2022;33(2):89–97. [Google Scholar]
- 35.Serritella E., Galluccio G., Impellizzeri A., Di Giacomo P., Di Paolo C. Comparison of the Effectiveness of Three Different Acupuncture Methods for TMD-Related Pain: A Randomized Clinical Study. Evidence-based Complementary & Alternative Medicine (eCAM) 2021:1–10. doi: 10.1155/2021/1286570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.de Resende C.M.B.M., de Oliveira Medeiros F.G.L., de Figueiredo, Rêgo CR, Bispo ASL, Barbosa GAS, de Almeida EO. Short-term effectiveness of conservative therapies in pain, quality of life, and sleep in patients with temporomandibular disorders: A randomized clinical trial. Cranio: the journal of craniomandibular practice. 2021;39(4):335–343. doi: 10.1080/08869634.2019.1627068. [DOI] [PubMed] [Google Scholar]
- 37.de Salles-Neto F.T., de Paula J.S., Romero J.G.A.J., Almeida-Leite C.M. Acupuncture for pain, mandibular function and oral health-related quality of life in patients with masticatory myofascial pain: A randomised controlled trial. J Oral Rehabil. 2020;47(10):1193–1201. doi: 10.1111/joor.13055. [DOI] [PubMed] [Google Scholar]
- 38.Vrbanović E., Alajbeg I.Z. Long-term Effectiveness of Occlusal Splint Therapy Compared to Placebo in Patients with Chronic Temporomandibular Disorders. Acta Stomatol Croat. 2019;53(3):195–206. doi: 10.15644/asc53/3/1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.MdF Rodrigues, Rodrigues M.L., Bueno K.S., Aroca J.P., Camilotti V., Busato M.C.A., et al. Effects of low-power laser auriculotherapy on the physical and emotional aspects in patients with temporomandibular disorders: A blind, randomized, controlled clinical trial. Complement Ther Med. 2019;42:340–346. doi: 10.1016/j.ctim.2018.12.010. [DOI] [PubMed] [Google Scholar]
- 40.Calixtre L.B., Oliveira A.B., de Sena, Rosa L.R., Armijo-Olivo S., Visscher C.M. Alburquerque-Sendín F. Effectiveness of mobilisation of the upper cervical region and craniocervical flexor training on orofacial pain, mandibular function and headache in women with TMD. A randomised, controlled trial. J Oral Rehabil. 2019;46(2):109–119. doi: 10.1111/joor.12733. [DOI] [PubMed] [Google Scholar]
- 41.Xie M., Diao J., Yang W. Clinical study of acupotomy spinal adjustment and traditional acupuncture treatment for patients with temporomandibular joint disorder syndrome. China Medicine and Pharmacy. 2018;8(13):76–79. [Google Scholar]
- 42.Zotelli V.L., Grillo C.M., Gil M.L., Wada RS, Sato JE, da Luz Rosário de, Sousa M. Acupuncture Effect on Pain, Mouth Opening Limitation and on the Energy Meridians in Patients with Temporomandibular Dysfunction: A Randomized Controlled Trial. JAMS Journal of Acupuncture and Meridian Studies. 2017;10(5):351–359. doi: 10.1016/j.jams.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 43.Z-h Huang, K-s Xu, J-q Zheng, Y-q He, Wu F. Bamboo-circled Salt-partitioned Moxibustion for Arthritis of Temporomandibular Joint: A Randomized Controlled Clinical Trial. Shanghai Journal of Acupuncture and Moxibustion. 2017;36(02):180–183. [Google Scholar]
- 44.Hosgor H., Bas B., Celenk C. A comparison of the outcomes of four minimally invasive treatment methods for anterior disc displacement of the temporomandibular joint. Int J Oral Maxillofac Surg. 2017;46(11):1403–1410. doi: 10.1016/j.ijom.2017.05.010. [DOI] [PubMed] [Google Scholar]
- 45.Packer A.C., Fernandes Pires P., Dibai Filho A.V., Rodrigues Bigaton D. Effect of upper thoracic manipulation on mouth opening and electromyographic activity of masticatory muscles in women with temporomandibular disorder: A randomized clinical trial. J Manipulative Physiol Ther. 2015;38(4):253–261. doi: 10.1016/j.jmpt.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 46.Grillo C.M., Canales G.T., Wada R.S., Alves M.C., Barbosa C.M.R., Berzin F., et al. Could Acupuncture Be Useful in the Treatment of Temporomandibular Dysfunction? JAMS Journal of Acupuncture and Meridian Studies. 2015;8(4):192–199. doi: 10.1016/j.jams.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 47.De Paula, Gomes C.A.F., Politti F., Andrade DV, De Sousa DFM, Herpich CM, Dibai-Filho AV, et al. Effects of massage therapy and occlusal splint therapy on mandibular range of motion in individuals with temporomandibular disorder: A randomized clinical trial. J Manipulative Physiol Ther. 2014;37(3):164–169. doi: 10.1016/j.jmpt.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 48.de Moraes Maia M.L., Ribeiro M.A.G., Maia L.G.M., Stuginski-Barbosa J., Costa Y.M., Porporatti A.L., et al. Evaluation of low-level laser therapy effectiveness on the pain and masticatory performance of patients with myofascial pain. Lasers Med Sci. 2014;29(1):29–35. doi: 10.1007/s10103-012-1228-7. [DOI] [PubMed] [Google Scholar]
- 49.Kalamir A., Graham P.L., Vitiello A.L., Bonello R., Pollard H. Intra-oral myofascial therapy versus education and self-care in the treatment of chronic, myogenous temporomandibular disorder: a randomised, clinical trial. Chiropr Man Therap. 2013;21(1):17–26. doi: 10.1186/2045-709X-21-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vicente-Barrero M., SL Yu-Lu, Zhang B., Bocanegra-Pérez S., Durán-Moreno D., López-Márquez A., et al. The efficacy of acupuncture and decompression splints in the treatment of temporomandibular joint pain-dysfunction syndrome. Patologia Oral y Cirugia Bucal. 2012;17(6):e1028. doi: 10.4317/medoral.17567. Medicina Oral. -e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Itoh K., Assi S., Ohyabu H., Imai K., Kitakoji H. Effects of trigger point acupuncture treatment on temporomandibular disorders: A preliminary randomized clinical trial. J Acupunct Meridan Stud. 2012;5(2):57–62. doi: 10.1016/j.jams.2012.01.013. [DOI] [PubMed] [Google Scholar]
- 52.Öz S., Gökçen-Röhlig B., Saruhanoglu A., Tuncer E.B. Management of myofascial pain: Low-level laser therapy versus occlusal splints. Journal of Craniofacial Surgery. 2010;21(6):1722–1728. doi: 10.1097/SCS.0b013e3181f3c76c. [DOI] [PubMed] [Google Scholar]
- 53.Katsoulis J., Ausfeld-Hafter B., Windecker-Gétaz I., Katsoulis K., Blagojevic N., Mericske-Stern R. Laser acupuncture for myofascial pain of the masticatory muscles. A controlled pilot study. Schweiz Monatsschr Zahnmed. 2010;120(3):213–225. [PubMed] [Google Scholar]
- 54.Gotou M., Nagata K., Sugawara Y. Short-term effectiveness of the Jog-manipulation technique for temporomandibular disorder (TMD) patients with limited mouth-opening -A randomized controlled trial. Journal of the Japanese Society for the Temporomandibular Joint. 2010;22(2):84–91. [Google Scholar]
- 55.de Felício C.M., Melchior M.O., de Silva M.A.M.R. Effects of orofacial myofunctional therapy on temporomandibular disorders. Cranio - Journal of Craniomandibular Practice. 2010;28(4):249–259. doi: 10.1179/crn.2010.033. [DOI] [PubMed] [Google Scholar]
- 56.Asai S., Itho K., Asai F., Imai K., Kitakoji H. Effect of acupuncture treatment on temporomandibular disorders-Questionnaire and acupuncture treatment for university students. Zen Nihon Shinkyu Gakkai zasshi (Journal of the Japan Society of Acupuncture and Moxibustion) 2010;60(4):728–36.
- 57.Shen Y.F., Younger J., Goddard G., Mackey S. Randomized clinical trial of acupuncture for myofascial pain of the jaw muscles. J Orofac Pain. 2009;23(4):353–359. [PMC free article] [PubMed] [Google Scholar]
- 58.Mansilla Ferragud P., Boscá Gandia J.J. Effect of upper cervical spine manipulation on mouth opening. Osteopatia Cientifica. 2008;3(2):45–51. [Google Scholar]
- 59.Frare J.C., Nicolau R.A. Clinical analysis of the effect of laser photobiomodulation (GaAs-904nm) on temporomandibular joint dysfunction. Braz J Phys Ther. 2008;12(1):37–42. [Google Scholar]
- 60.Smith P., Mosscrop D., Davies S., Sloan P., Al-Ani Z. The efficacy of acupuncture in the treatment of temporomandibular joint myofascial pain: A randomised controlled trial. J Dent. 2007;35(3):259–267. doi: 10.1016/j.jdent.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 61.Mazzetto M.O., Carrasco T.G., Bidinelo E.F., de Andrade Pizzo R.C., Mazzetto R.G. Low intensity laser application in temporomandibular disorders: a phase I double-blind study. CRANIO: The Journal of Craniomandibular & Sleep Practice. 2007;25(3):186–192. doi: 10.1179/crn.2007.029. [DOI] [PubMed] [Google Scholar]
- 62.Emam A.M., Abdel-Gawwad E.A., Baiomy A.A.A., Farhat M.Y., Atito E., Helal M.A. Efficacy of Occlusal Splints and Low-Level Laser Therapy on the Mandibular Range of Motion in Subjects with Temporomandibular Joint Disc Displacement with Reduction. J Int Soc Prev Community Dent. 2023;13(3):229–236. doi: 10.4103/jispcd.JISPCD_159_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ekici Ö., Dündar Ü., Gökay G.D., Büyükbosna M. Evaluation of the efficiency of different treatment modalities in individuals with painful temporomandibular joint disc displacement with reduction: a randomised controlled clinical trial. British Journal of Oral and Maxillofacial Surgery. 2022;60(3):350–356. doi: 10.1016/j.bjoms.2021.08.001. [DOI] [PubMed] [Google Scholar]
- 64.Aroca J.P., Cardoso P.M.F., Favarão J., Zanini M.M., Camilotti V., Busato M.C.A., et al. Auricular acupuncture in TMD - A sham-controlled, randomized, clinical trial. Complement Ther Clin Pract. 2022;48 doi: 10.1016/j.ctcp.2022.101569. [DOI] [PubMed] [Google Scholar]
- 65.Shousha T., Alayat M., Moustafa I. Effects of low-level laser therapy versus soft occlusive splints on mouth opening and surface electromyography in females with temporomandibular dysfunction: A randomized-controlled study. PLoS One. 2021;16 doi: 10.1371/journal.pone.0258063. (10 October) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ram H.K., Shah D.N. Comparative evaluation of occlusal splint therapy and muscle energy technique in the management of temporomandibular disorders: A randomized controlled clinical trial. J Indian Prosthodont Soc. 2021;21(4):356–365. doi: 10.4103/jips.jips_332_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Peixoto K.O., Da Silva Bezerra A., Melo R.A., De Resende C.M.B.M., De Almeida E.O., Barbosa G.A.S. Short-Term Effect of Scalp Acupuncture on Pain, Sleep Disorders, and Quality of Life in Patients with Temporomandibular Disorders: A A Randomized Clinical Trial. Pain Medicine (United States) 2021;22(4):905–914. doi: 10.1093/pm/pnab048. [DOI] [PubMed] [Google Scholar]
- 68.Gikić M., Vrbanović E., Zlendić M., Alajbeg I.Z. Treatment responses in chronic temporomandibular patients depending on the treatment modalities and frequency of parafunctional behaviour. J Oral Rehabil. 2021;48(7):785–797. doi: 10.1111/joor.13173. [DOI] [PubMed] [Google Scholar]
- 69.El Zawahry N.O., Salah Fayed M.M., Abouelezz A.M., Aboulfotouh M.H. Comparison of disability score and chronic pain grading with different treatment modalities in a sample of temporomandibular joint disc displacement with reduction patients. Indian Journal of Public Health Research and Development. 2021;12(3):603–610. [Google Scholar]
- 70.Pan L., Hu J., Ye P. Effect of Stable Occlusal Pad Combined with Manual Therapy on MFIQ Score,Maximum Mouth Opening and VAS Score in Patients with Temporomandibular Joint Disorder. Zhejiang Journal of Integrated Traditional Chinese and Western Medicine. 2020;30(11):914–917. [Google Scholar]
- 71.Madani A., Ahrari F., Fallahrastegar A., Daghestani N. A randomized clinical trial comparing the efficacy of low-level laser therapy (LLLT) and laser acupuncture therapy (LAT) in patients with temporomandibular disorders. Lasers Med Sci. 2020;35(1):181–192. doi: 10.1007/s10103-019-02837-x. [DOI] [PubMed] [Google Scholar]
- 72.Demirkol N., Sari F., Bulbul M., Demirkol M., Simsek I., Usumez A. Effectiveness of occlusal splints and low-level laser therapy on myofascial pain. Lasers Med Sci. 2014:1–6. doi: 10.1007/s10103-014-1522-7. [DOI] [PubMed] [Google Scholar]
- 73.Al Quran F.A., Kamal M.S. Anterior midline point stop device (AMPS) in the treatment of myogenous TMDs: comparison with the stabilization splint and control group. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;101(6):741–7. [DOI] [PubMed]
- 74.Eraslan R., Kilic K., Zararsiz G. Effects of Different Therapeutic Modalities on the Clicking Sound and Quantitative Assessment of the Vertical and Lateral Mandibular Movements of Patients with Internal Derangements of the Temporomandibular Joint. Int J Prosthodont. 2021;34(2):173–182. doi: 10.11607/ijp.6836. [DOI] [PubMed] [Google Scholar]
- 75.DeVocht J.W., Goertz C.M., Hondras M.A., Long C.R., Schaeffer W., Thomann L., et al. A pilot study of a chiropractic intervention for management of chronic myofascial temporomandibular disorder. Journal of the American Dental Association (JADA) 2013;144(10):1154–1163. doi: 10.14219/jada.archive.2013.0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Al-Moraissi E.A., Farea R., Qasem K.A., Al-Wadeai M.S., Al-Sabahi M.E., Al-Iryani G.M. Effectiveness of occlusal splint therapy in the management of temporomandibular disorders: network meta-analysis of randomized controlled trials. Int J Oral Maxillofac Surg. 2020;49(8):1042–1056. doi: 10.1016/j.ijom.2020.01.004. [DOI] [PubMed] [Google Scholar]
- 77.Fouda A.A.H. No evidence on the effectiveness of oral splints for the management of temporomandibular joint dysfunction pain in both short and long-term follow-up systematic reviews and meta-analysis studies. J Korean Assoc Oral Maxillofac Surg. 2020;46(2):87–98. doi: 10.5125/jkaoms.2020.46.2.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Peixoto K.O., Abrantes P.S., De Carvalho I.H.G., De Almeida E.O., Barbosa G.A.S. Temporomandibular disorders and the use of traditional and laser acupuncture: a systematic review. CRANIO®. 2023;41(6):501–507. doi: 10.1080/08869634.2021.1873605. [DOI] [PubMed] [Google Scholar]
- 79.Wu J.Y., Zhang C., Xu Y.P., Yu Y.Y., Peng L., Leng W.D., et al. Acupuncture therapy in the management of the clinical outcomes for temporomandibular disorders: A PRISMA-compliant meta-analysis. Medicine (Baltimore) 2017;96(9):e6064. doi: 10.1097/MD.0000000000006064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jung A., Shin B.C., Lee M.S., Sim H., Ernst E. Acupuncture for treating temporomandibular joint disorders: A systematic review and meta-analysis of randomized, sham-controlled trials. J Dent. 2011;39(5):341–350. doi: 10.1016/j.jdent.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 81.Asquini G., Pitance L., Michelotti A., Falla D. Effectiveness of manual therapy applied to craniomandibular structures in temporomandibular disorders: A systematic review. J Oral Rehabil. 2022;49(4):442–455. doi: 10.1111/joor.13299. [DOI] [PubMed] [Google Scholar]
- 82.Rehabilitation TSoKM. Clinical Practice Guideline of Korean Medicine for Temporomandibular Disorders. National Institute of the Korean Medicine Development, Seoul, Korea: Standard Clinical Practice Guideline Development for Korean Medicine Project Agency; 2021.
- 83.EA Al-Moraissi, Conti P.C.R., Alyahya A., Alkebsi K., Elsharkawy A., Christidis N. The hierarchy of different treatments for myogenous temporomandibular disorders: a systematic review and network meta-analysis of randomized clinical trials. Oral Maxillofac Surg. 2022;26(4):519–533. doi: 10.1007/s10006-021-01009-y. [DOI] [PubMed] [Google Scholar]
- 84.Menéndez-Torre Á., Pintado-Zugasti A.M., Zaldivar J.N.C., García-Bermejo P., Gómez-Costa D., Molina-Álvarez M., et al. Effectiveness of deep dry needling versus manual therapy in the treatment of myofascial temporomandibular disorders: a systematic review and network meta-analysis. Chiropr Man Therap. 2023;31(1):46. doi: 10.1186/s12998-023-00489-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplement 1. PRISMA NMA Checklist
Supplement 2. Search strategy
Supplement 3. Flow diagram of the study selection process
Supplement 4. Summary of risk of bias for each study based on Cochrane Risk of Bias 2.0 tool
Supplement 5. Pairwise meta-analysis for pain intensity
Supplement 6. Cumulative ranking probability plots (SUCRA) for pain intensity
Supplement 7. Pairwise meta-analysis for maximum mouth opening
Supplement 8. Cumulative ranking probability plots (SUCRA) for maximum mouth opening
Supplement 9. Comparison-adjusted funnel plots
Supplement 10. Level of evidence by CINeMA methodology
Supplement 11. Excluded studies and reason after full-text review
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.