Abstract
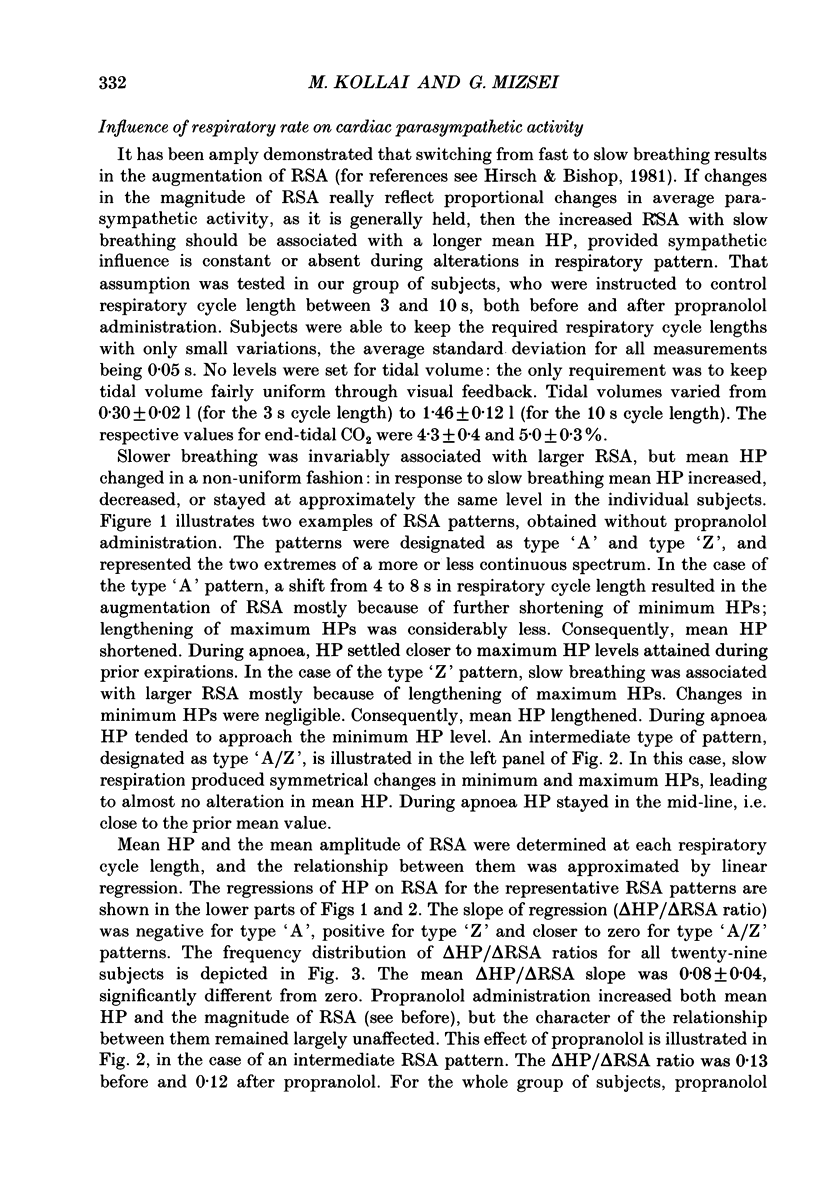
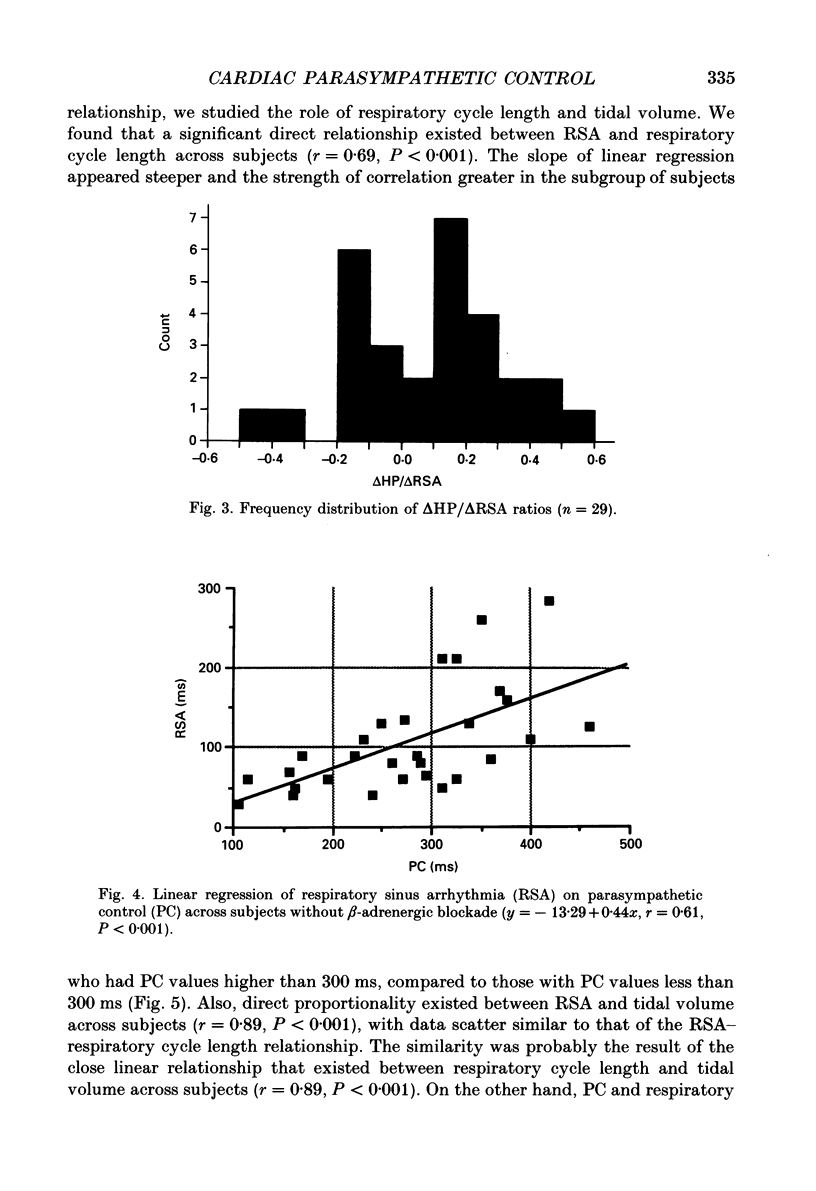
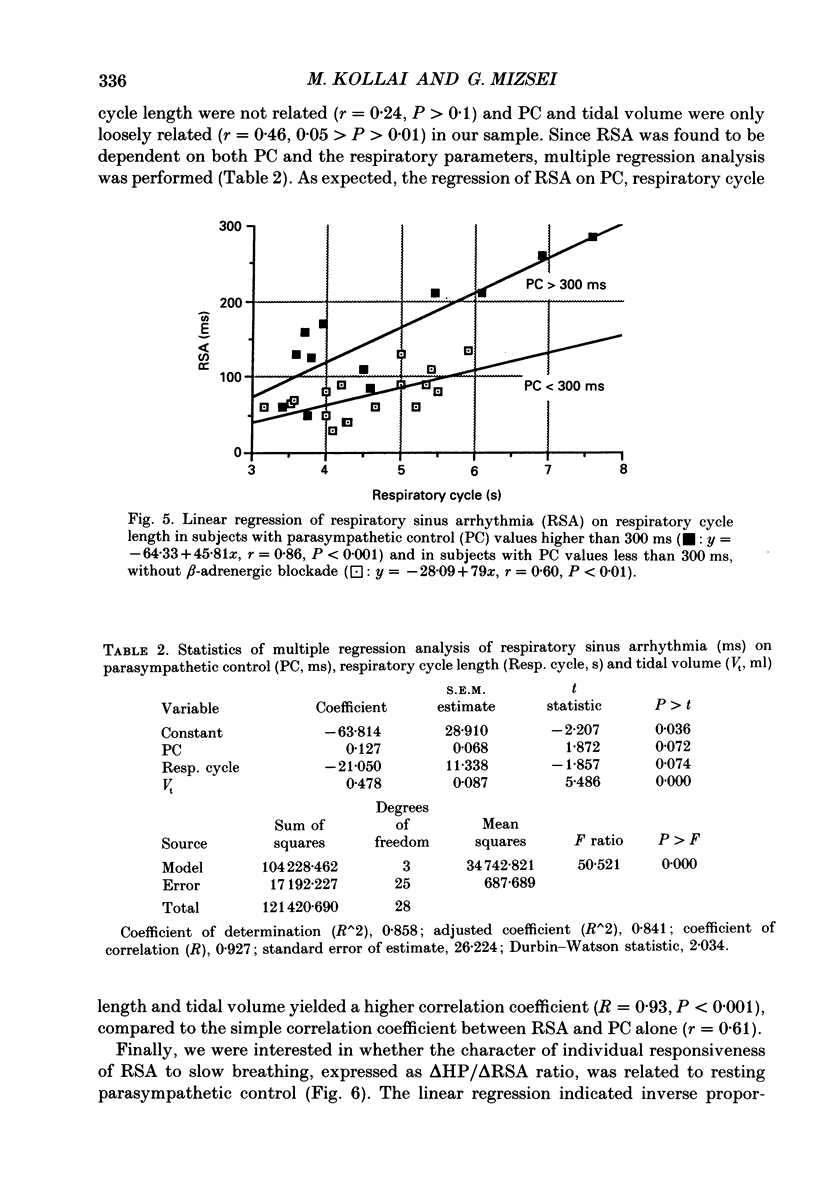
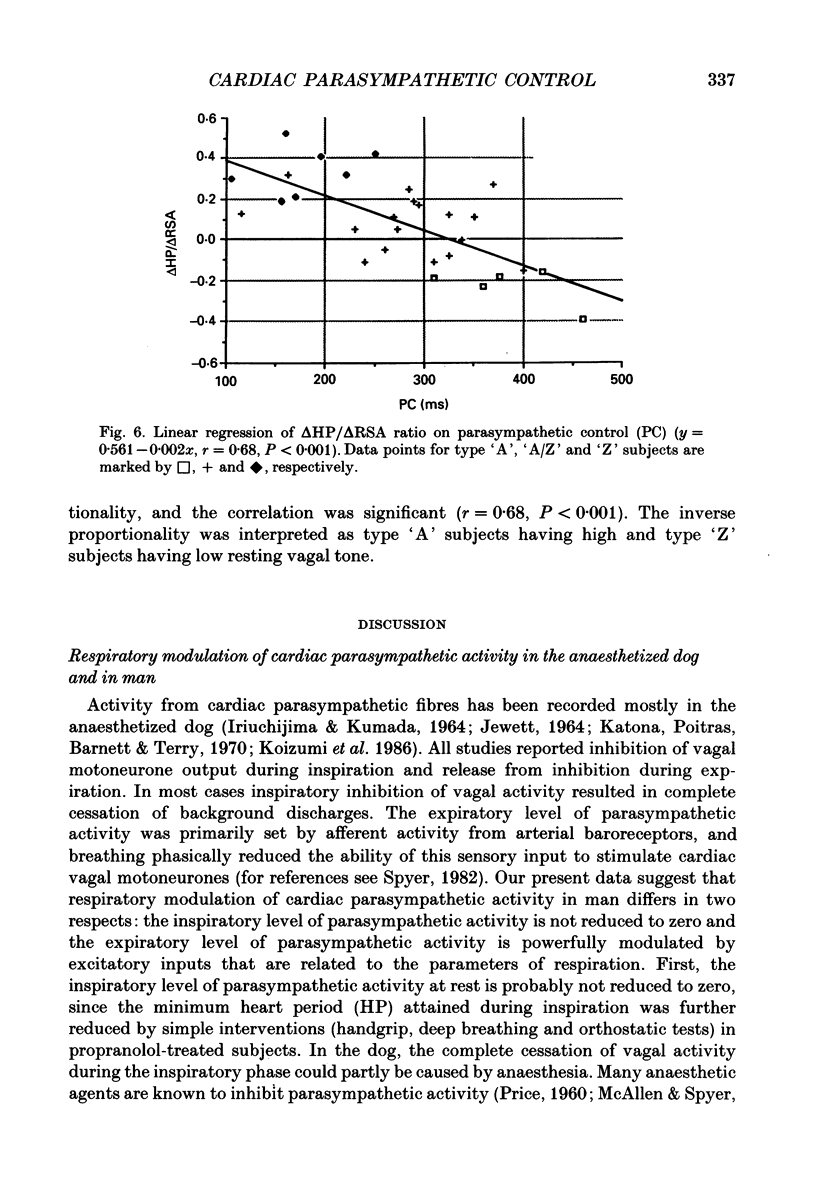
1. Respiratory modulation of cardiac parasympathetic activity and the relationship between respiratory sinus arrhythmia and parasympathetic control has been studied in twenty-nine conscious, healthy young adult subjects. 2. Changes in heart period in propranolol-treated subjects were taken as the measure of changes in cardiac parasympathetic activity; respiratory sinus arrhythmia was quantified as the difference between maximum and minimum heart periods in a given respiratory cycle; cardiac parasympathetic control was defined as the change in heart period after administration of a full dose of atropine. 3. During normal quiet breathing the inspiratory level of cardiac parasympathetic activity was not reduced to zero. The expiratory level was influenced by excitatory inputs whose activation was related to respiratory cycle length. 4. Slow breathing was associated with augmented sinus arrhythmia, but in different individuals the influence on minimum and maximum heart periods varied so that mean heart period was increased in some subjects but decreased in others. This occurred both in control conditions and after administration of a full dose of propranolol. 5. During normal breathing the correlation across subjects between respiratory sinus arrhythmia and parasympathetic control, although significant, was not close (r = 0.61). The relationship was not affected by beta-adrenergic blockade (r = 0.63). The strength of the correlation improved when multiple regression of respiratory sinus arrhythmia was performed on three variables: parasympathetic control, respiratory cycle length and tidal volume (R = 0.93). 6. It is concluded that in conscious human subjects the respiratory modulation of cardiac parasympathetic activity is different from that observed in the anaesthetized dog, and that variations in the amplitude of respiratory sinus arrhythmia do not necessarily reflect proportional changes in cardiac parasympathetic control.
Full text
PDF
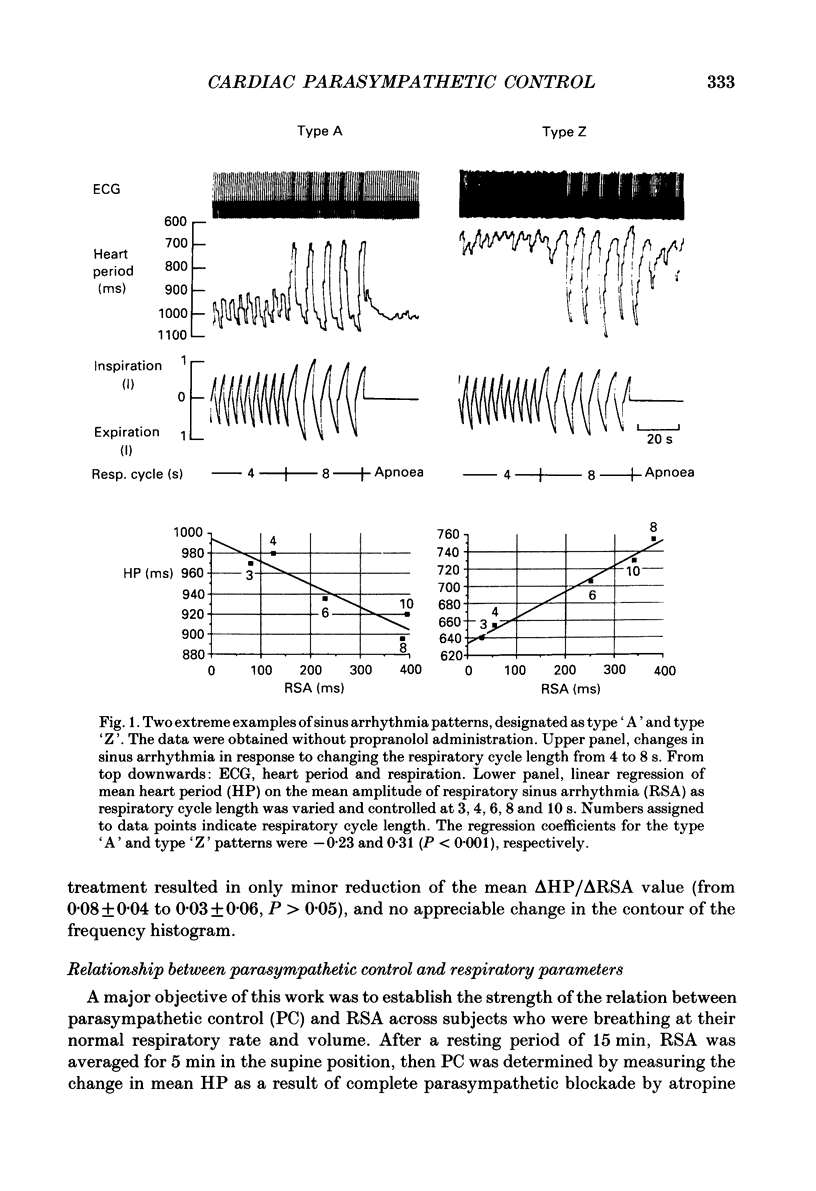
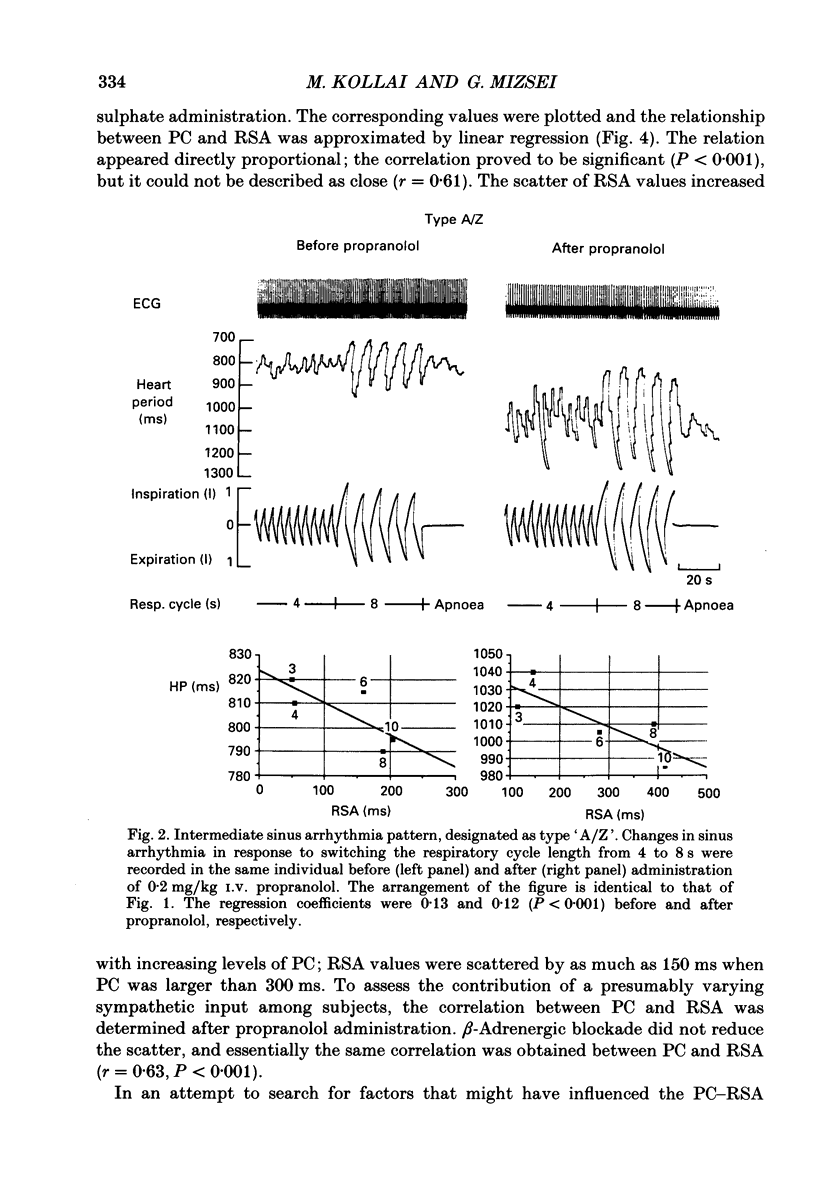
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Coker R., Koziell A., Oliver C., Smith S. E. Does the sympathetic nervous system influence sinus arrhythmia in man? Evidence from combined autonomic blockade. J Physiol. 1984 Nov;356:459–464. doi: 10.1113/jphysiol.1984.sp015476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies C. T., Neilson J. M. Sinus arrhythmia in man at rest. J Appl Physiol. 1967 May;22(5):947–955. doi: 10.1152/jappl.1967.22.5.947. [DOI] [PubMed] [Google Scholar]
- Donchin Y., Feld J. M., Porges S. W. Respiratory sinus arrhythmia during recovery from isoflurane-nitrous oxide anesthesia. Anesth Analg. 1985 Aug;64(8):811–815. [PubMed] [Google Scholar]
- Eckberg D. L. Human sinus arrhythmia as an index of vagal cardiac outflow. J Appl Physiol Respir Environ Exerc Physiol. 1983 Apr;54(4):961–966. doi: 10.1152/jappl.1983.54.4.961. [DOI] [PubMed] [Google Scholar]
- Eckberg D. L., Kifle Y. T., Roberts V. L. Phase relationship between normal human respiration and baroreflex responsiveness. J Physiol. 1980 Jul;304:489–502. doi: 10.1113/jphysiol.1980.sp013338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckberg D. L., Nerhed C., Wallin B. G. Respiratory modulation of muscle sympathetic and vagal cardiac outflow in man. J Physiol. 1985 Aug;365:181–196. doi: 10.1113/jphysiol.1985.sp015766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckoldt K., Bodmann K. H., Cammann H., Pfeifer B., Schubert E. Sinus arrhythmia and heart rate in hypertonic disease. Adv Cardiol. 1976;16:366–369. doi: 10.1159/000398425. [DOI] [PubMed] [Google Scholar]
- Ewing D. J., Borsey D. Q., Bellavere F., Clarke B. F. Cardiac autonomic neuropathy in diabetes: comparison of measures of R-R interval variation. Diabetologia. 1981 Jul;21(1):18–24. doi: 10.1007/BF03216217. [DOI] [PubMed] [Google Scholar]
- Fouad F. M., Tarazi R. C., Ferrario C. M., Fighaly S., Alicandri C. Assessment of parasympathetic control of heart rate by a noninvasive method. Am J Physiol. 1984 Jun;246(6 Pt 2):H838–H842. doi: 10.1152/ajpheart.1984.246.6.H838. [DOI] [PubMed] [Google Scholar]
- Hilsted J., Jensen S. B. A simple test for autonomic neuropathy in juvenile diabetics. Acta Med Scand. 1979;205(5):385–387. doi: 10.1111/j.0954-6820.1979.tb06069.x. [DOI] [PubMed] [Google Scholar]
- Hirsch J. A., Bishop B. Respiratory sinus arrhythmia in humans: how breathing pattern modulates heart rate. Am J Physiol. 1981 Oct;241(4):H620–H629. doi: 10.1152/ajpheart.1981.241.4.H620. [DOI] [PubMed] [Google Scholar]
- IRIUCHIJIMA J., KUMADA M. ACTIVITY OF SINGLE VAGAL FIBERS EFFERENT TO THE HEART. Jpn J Physiol. 1964 Oct 15;14:479–487. doi: 10.2170/jjphysiol.14.479. [DOI] [PubMed] [Google Scholar]
- JEWETT D. L. ACTIVITY OF SINGLE EFFERENT FIBRES IN THE CERVICAL VAGUS NERVE OF THE DOG, WITH SPECIAL REFERENCE TO POSSIBLE CARDIO-INHIBITORY FIBRES. J Physiol. 1964 Dec;175:321–357. doi: 10.1113/jphysiol.1964.sp007520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston L. C. The abnormal heart rate response to a deep breath in borderline labile hypertension: a sign of autonomic nervous system dysfunction. Am Heart J. 1980 Apr;99(4):487–493. doi: 10.1016/0002-8703(80)90384-1. [DOI] [PubMed] [Google Scholar]
- Julius S., Pascual A. V., London R. Role of parasympathetic inhibition in the hyperkinetic type of borderline hypertension. Circulation. 1971 Sep;44(3):413–418. doi: 10.1161/01.cir.44.3.413. [DOI] [PubMed] [Google Scholar]
- Kallenbach J. M., Webster T., Dowdeswell R., Reinach S. G., Millar R. N., Zwi S. Reflex heart rate control in asthma. Evidence of parasympathetic overactivity. Chest. 1985 May;87(5):644–648. doi: 10.1378/chest.87.5.644. [DOI] [PubMed] [Google Scholar]
- Katona P. G., Jih F. Respiratory sinus arrhythmia: noninvasive measure of parasympathetic cardiac control. J Appl Physiol. 1975 Nov;39(5):801–805. doi: 10.1152/jappl.1975.39.5.801. [DOI] [PubMed] [Google Scholar]
- Katona P. G., Poitras J. W., Barnett G. O., Terry B. S. Cardiac vagal efferent activity and heart period in the carotid sinus reflex. Am J Physiol. 1970 Apr;218(4):1030–1037. doi: 10.1152/ajplegacy.1970.218.4.1030. [DOI] [PubMed] [Google Scholar]
- McAllen R. M., Spyer K. M. Two types of vagal preganglionic motoneurones projecting to the heart and lungs. J Physiol. 1978 Sep;282:353–364. doi: 10.1113/jphysiol.1978.sp012468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe P. M., Yongue B. G., Ackles P. K., Porges S. W. Changes in heart period, heart-period variability, and a spectral analysis estimate of respiratory sinus arrhythmia in response to pharmacological manipulations of the baroreceptor reflex in cats. Psychophysiology. 1985 Mar;22(2):195–203. doi: 10.1111/j.1469-8986.1985.tb01585.x. [DOI] [PubMed] [Google Scholar]
- PRICE H. L. General anesthesia and circulatory homeostasis. Physiol Rev. 1960 Apr;40:187–218. doi: 10.1152/physrev.1960.40.2.187. [DOI] [PubMed] [Google Scholar]
- Rigel D. F., Lipson D., Katona P. G. Excess tachycardia: heart rate after antimuscarinic agents in conscious dogs. Am J Physiol. 1984 Feb;246(2 Pt 2):H168–H173. doi: 10.1152/ajpheart.1984.246.2.H168. [DOI] [PubMed] [Google Scholar]
- Smith S. A. Reduced sinus arrhythmia in diabetic autonomic neuropathy: diagnostic value of an age-related normal range. Br Med J (Clin Res Ed) 1982 Dec 4;285(6355):1599–1601. doi: 10.1136/bmj.285.6355.1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spyer K. M. Central nervous integration of cardiovascular control. J Exp Biol. 1982 Oct;100:109–128. doi: 10.1242/jeb.100.1.109. [DOI] [PubMed] [Google Scholar]
- Sundkvist G., Almér L. 0., Lilja B. Respiratory influence on heart rate in diabetes mellitus. Br Med J. 1979 Apr 7;1(6168):924–925. doi: 10.1136/bmj.1.6168.924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner H. R., Russell R. O., Jr Effect of combined sympathetic and vagal stimulation on heart rate in the dog. Circ Res. 1969 Apr;24(4):567–573. doi: 10.1161/01.res.24.4.567. [DOI] [PubMed] [Google Scholar]
- Wheeler T., Watkins P. J. Cardiac denervation in diabetes. Br Med J. 1973 Dec 8;4(5892):584–586. doi: 10.1136/bmj.4.5892.584. [DOI] [PMC free article] [PubMed] [Google Scholar]


