Abstract
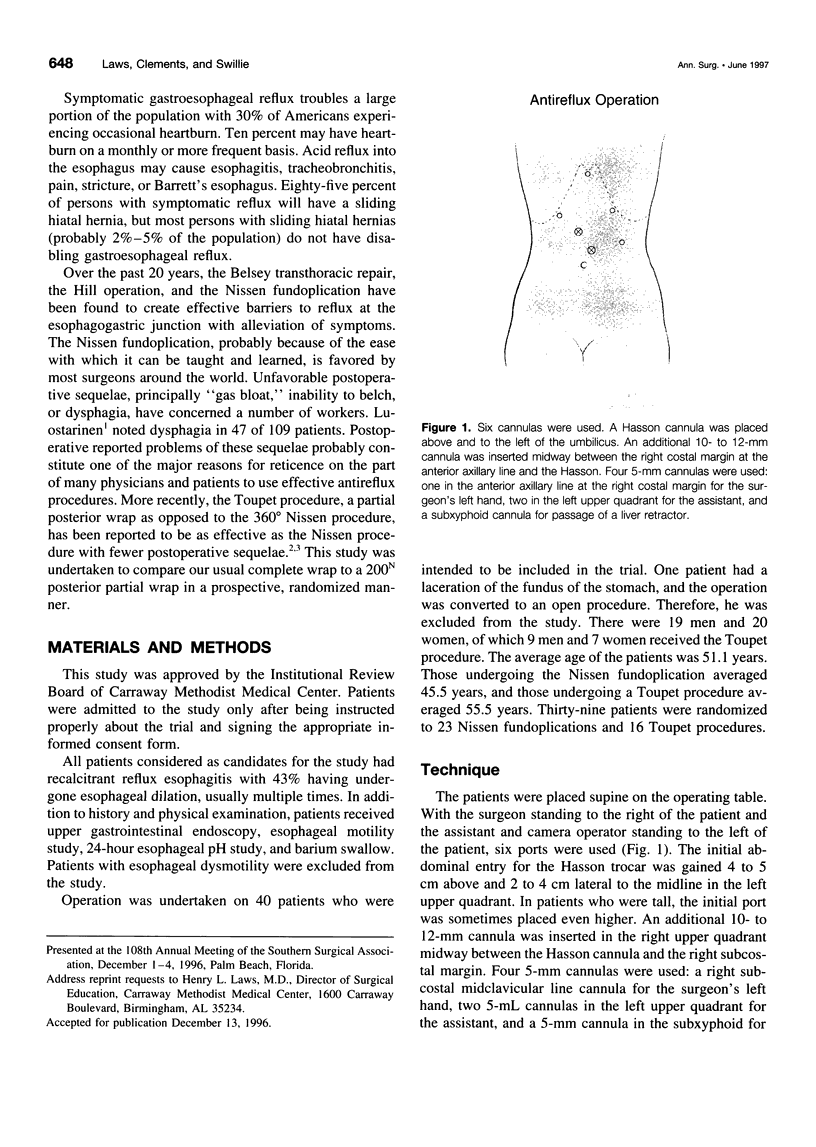
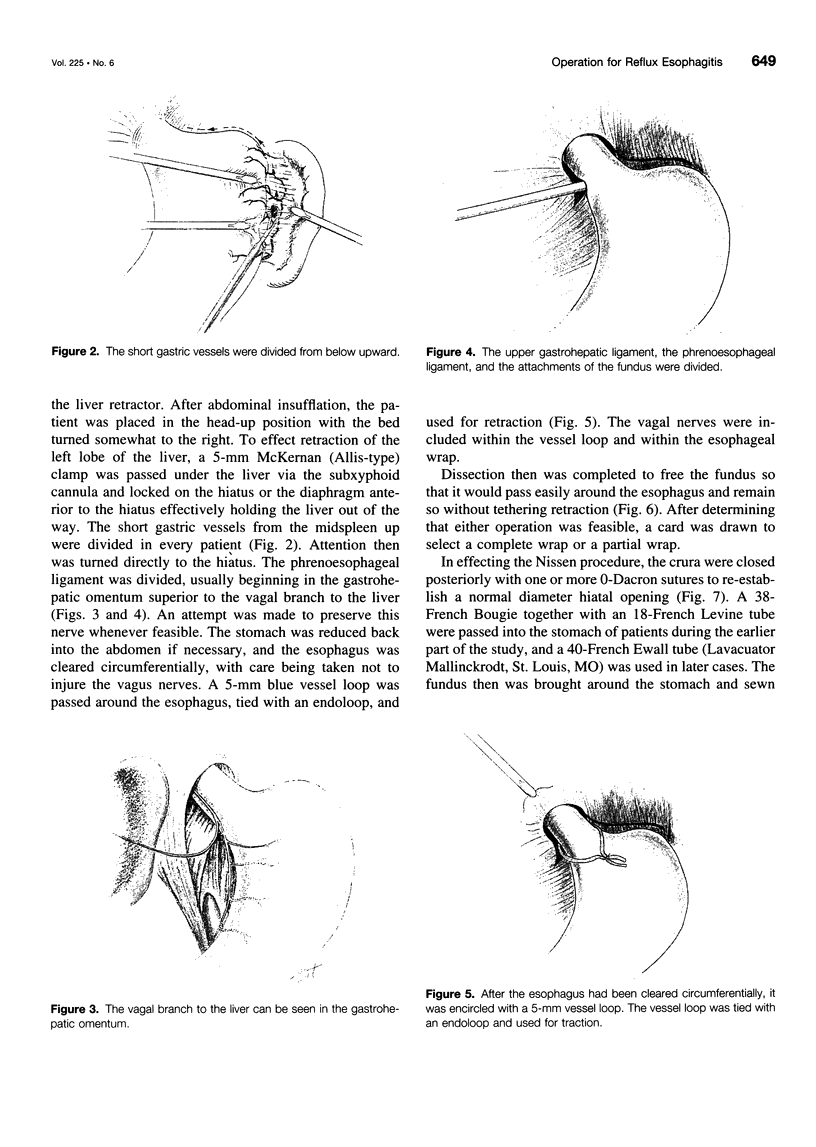
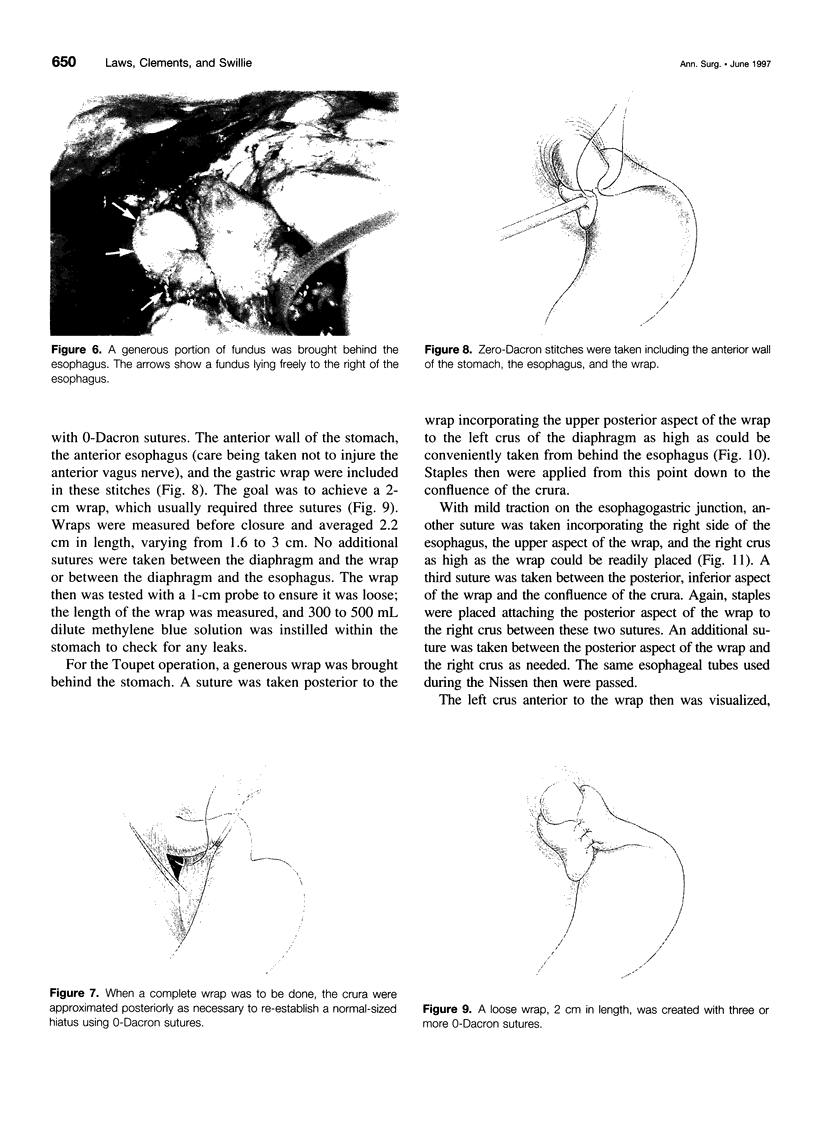
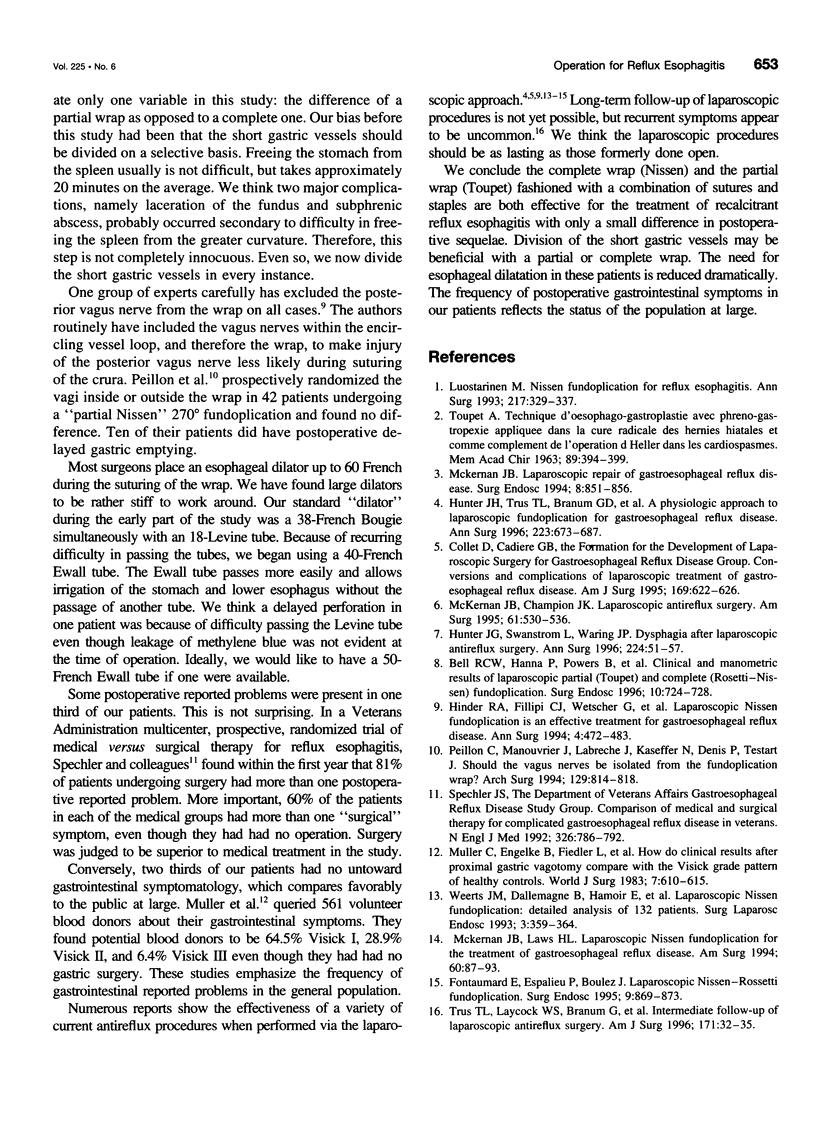
OBJECTIVE: A prospective, randomized trial was performed to determine which of two antireflux procedures, a complete wrap (Nissen) or a 200N wrap (Toupet), was more effective with fewer sequelae. SUMMARY BACKGROUND DATA: Laparoscopic procedures for gastroesophageal reflux disease appear to be as effective as those done by open laparotomy. The Nissen fundoplication is used most frequently, but postoperative bloating, inability to belch, and dysphagia occur. The partial wrap has been said to be as effective with less unfavorable postoperative symptoms. METHODS: Patients with reflux esophagitis were approached laparoscopically using a six-port technique. After division of the short gastric vessels and dissection of the terminal esophagus and fundus of the stomach to allow performance of either procedure, patients randomly were assigned one of the procedures by a card drawn in the operating room. RESULTS: Forty patients underwent operation, but 1 was excluded when an open procedure became necessary. Twenty-three patients received a complete wrap and 16 received a partial wrap. The average operating time was 155 minutes for the Nissen procedures and 162 minutes for the Toupet procedures. The postoperative stay averaged 2.7 days for the Nissen procedures and 2.5 days for the Toupet procedures. There were no deaths. Including the patient converted to an open procedure, three patients had operative complications. At follow-up, Visick scores after the complete wraps were I-13, II-8, III-2 and after the partial wrap were I-12 and II-3. Two patients indicated they would not have the operation again. CONCLUSIONS: A partial or a complete wrap after division of the short gastric vessel offers effective therapy for reflux esophagitis with > 90% patient satisfaction. The authors' study shows no clear advantage of one wrap (partial or complete) over the other.
Full text
PDF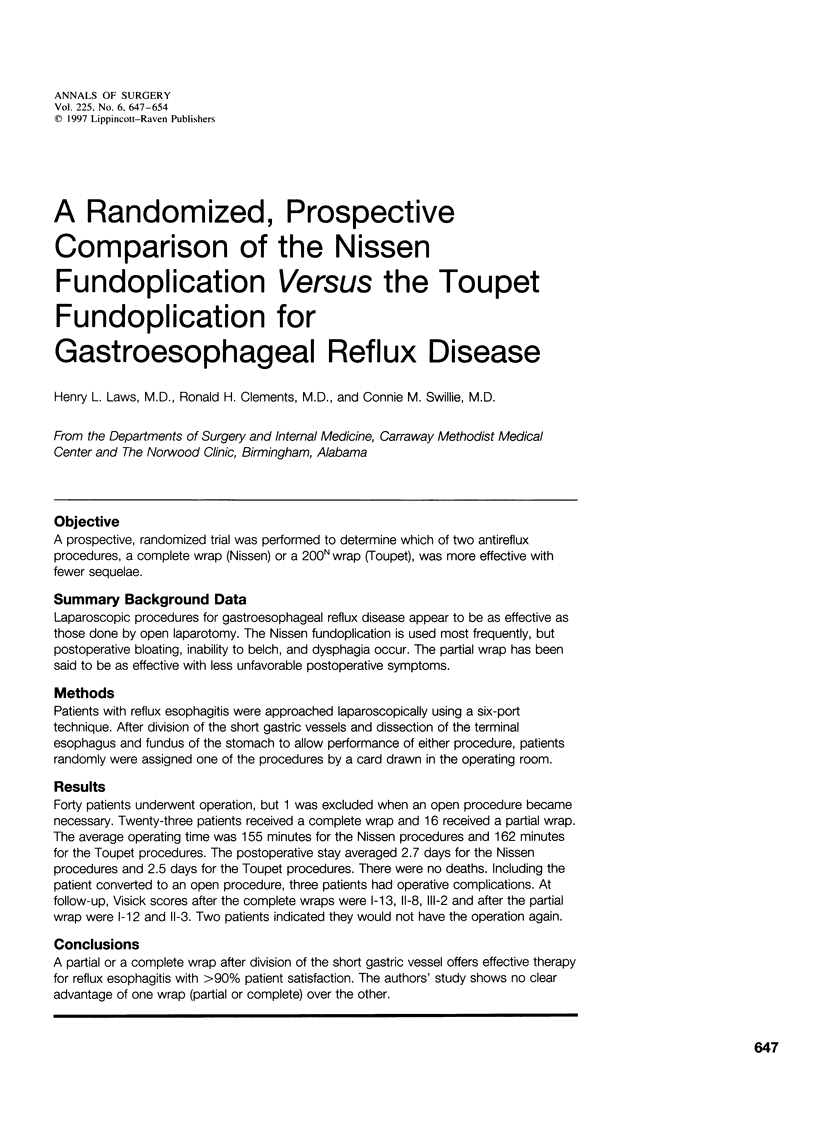
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bell R. C., Hanna P., Powers B., Sabel J., Hruza D. Clinical and manometric results of laparoscopic partial (Toupet) and complete (Rosetti-Nissen) fundoplication. Surg Endosc. 1996 Jul;10(7):724–728. doi: 10.1007/BF00193044. [DOI] [PubMed] [Google Scholar]
- Collet D., Cadière G. B. Conversions and complications of laparoscopic treatment of gastroesophageal reflux disease. Formation for the Development of Laparoscopic Surgery for Gastroesophageal Reflux Disease Group. Am J Surg. 1995 Jun;169(6):622–626. doi: 10.1016/s0002-9610(99)80234-7. [DOI] [PubMed] [Google Scholar]
- Fontaumard E., Espalieu P., Boulez J. Laparoscopic Nissen-Rossetti fundoplication. First results. Surg Endosc. 1995 Aug;9(8):869–873. doi: 10.1007/BF00768880. [DOI] [PubMed] [Google Scholar]
- Hinder R. A., Filipi C. J., Wetscher G., Neary P., DeMeester T. R., Perdikis G. Laparoscopic Nissen fundoplication is an effective treatment for gastroesophageal reflux disease. Ann Surg. 1994 Oct;220(4):472–483. doi: 10.1097/00000658-199410000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter J. G., Swanstrom L., Waring J. P. Dysphagia after laparoscopic antireflux surgery. The impact of operative technique. Ann Surg. 1996 Jul;224(1):51–57. doi: 10.1097/00000658-199607000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter J. G., Trus T. L., Branum G. D., Waring J. P., Wood W. C. A physiologic approach to laparoscopic fundoplication for gastroesophageal reflux disease. Ann Surg. 1996 Jun;223(6):673–687. doi: 10.1097/00000658-199606000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luostarinen M. Nissen fundoplication for reflux esophagitis. Long-term clinical and endoscopic results in 109 of 127 consecutive patients. Ann Surg. 1993 Apr;217(4):329–337. doi: 10.1097/00000658-199304000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKernan J. B., Champion J. K. Laparoscopic antireflux surgery. Am Surg. 1995 Jun;61(6):530–536. [PubMed] [Google Scholar]
- McKernan J. B. Laparoscopic repair of gastroesophageal reflux disease. Toupet partial fundoplication versus Nissen fundoplication. Surg Endosc. 1994 Aug;8(8):851–856. doi: 10.1007/BF00843453. [DOI] [PubMed] [Google Scholar]
- McKernan J. B., Laws H. L. Laparoscopic Nissen fundoplication for the treatment of gastroesophageal reflux disease. Am Surg. 1994 Feb;60(2):87–93. [PubMed] [Google Scholar]
- Muller C., Engelke B., Fiedler L., Marrie A., Mühe E., Schmitz-Harbauer W., Zumtobel V. How do clinical results after proximal gastric vagotomy compare with the Visick grade pattern of healthy controls? World J Surg. 1983 Sep;7(5):610–615. doi: 10.1007/BF01655337. [DOI] [PubMed] [Google Scholar]
- Peillon C., Manouvrier J. L., Labreche J., Kaeffer N., Denis P., Testart J. Should the vagus nerves be isolated from the fundoplication wrap? A prospective study. Arch Surg. 1994 Aug;129(8):814–818. doi: 10.1001/archsurg.1994.01420320036006. [DOI] [PubMed] [Google Scholar]
- Spechler S. J. Comparison of medical and surgical therapy for complicated gastroesophageal reflux disease in veterans. The Department of Veterans Affairs Gastroesophageal Reflux Disease Study Group. N Engl J Med. 1992 Mar 19;326(12):786–792. doi: 10.1056/NEJM199203193261202. [DOI] [PubMed] [Google Scholar]
- Trus T. L., Laycock W. S., Branum G., Waring J. P., Mauren S., Hunter J. G. Intermediate follow-up of laparoscopic antireflux surgery. Am J Surg. 1996 Jan;171(1):32–35. doi: 10.1016/S0002-9610(99)80069-5. [DOI] [PubMed] [Google Scholar]
- Weerts J. M., Dallemagne B., Hamoir E., Demarche M., Markiewicz S., Jehaes C., Lombard R., Demoulin J. C., Etienne M., Ferron P. E. Laparoscopic Nissen fundoplication: detailed analysis of 132 patients. Surg Laparosc Endosc. 1993 Oct;3(5):359–364. [PubMed] [Google Scholar]