Abstract
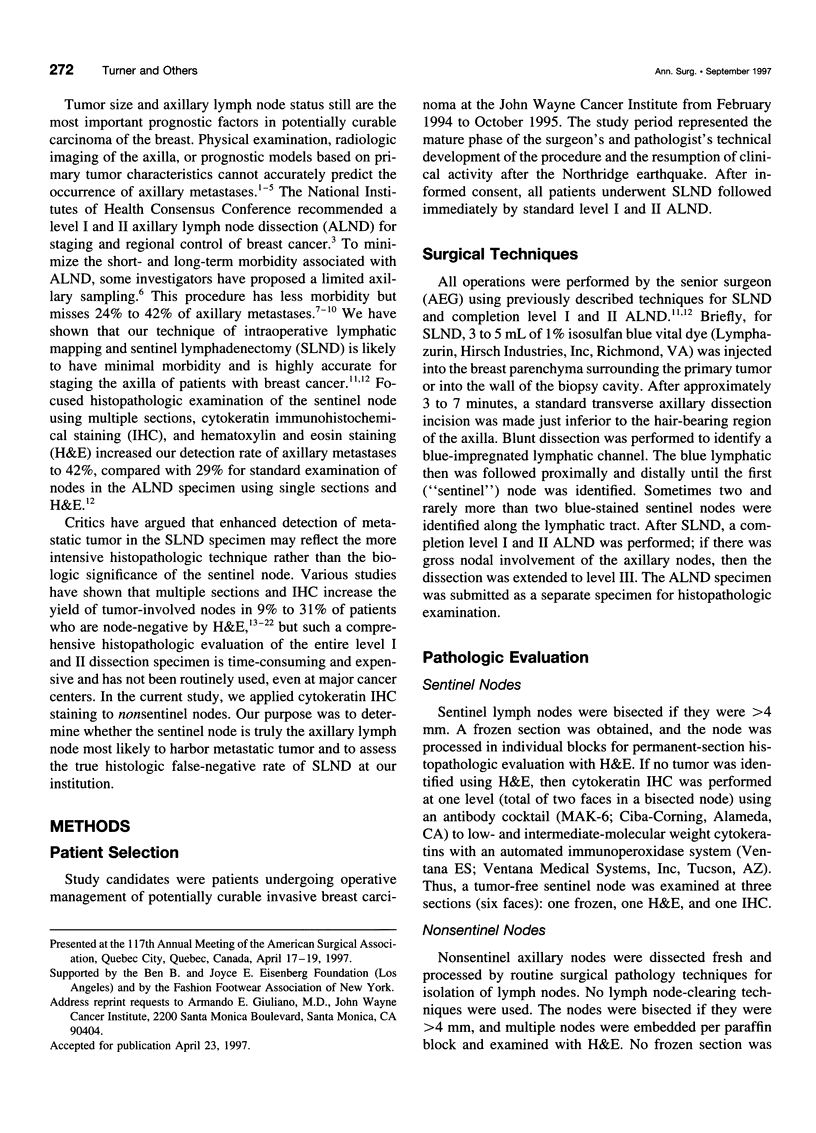
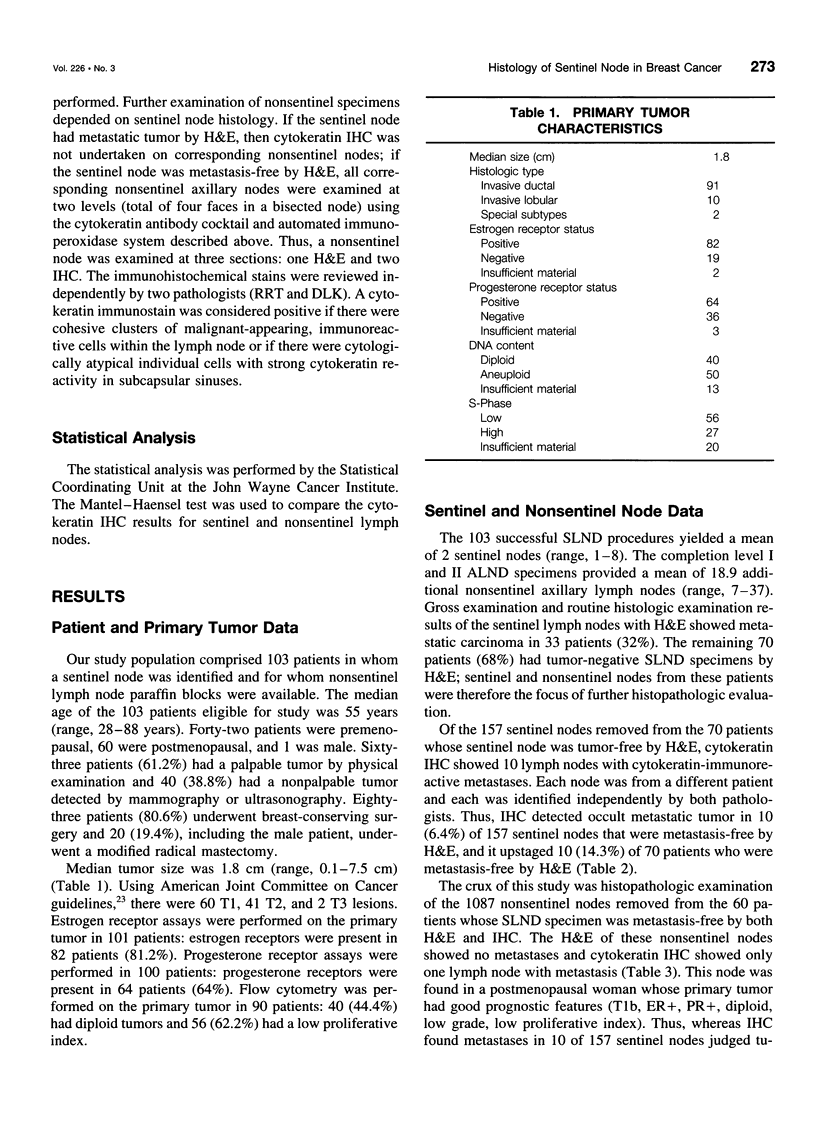
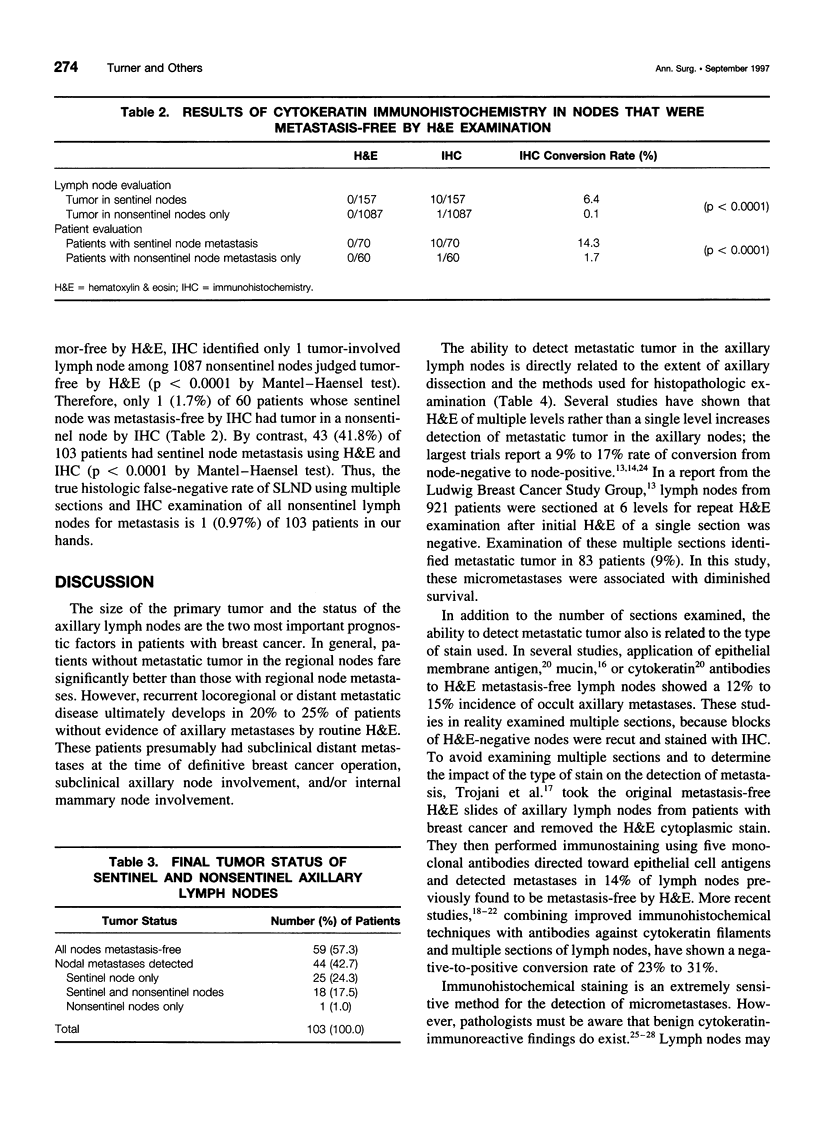
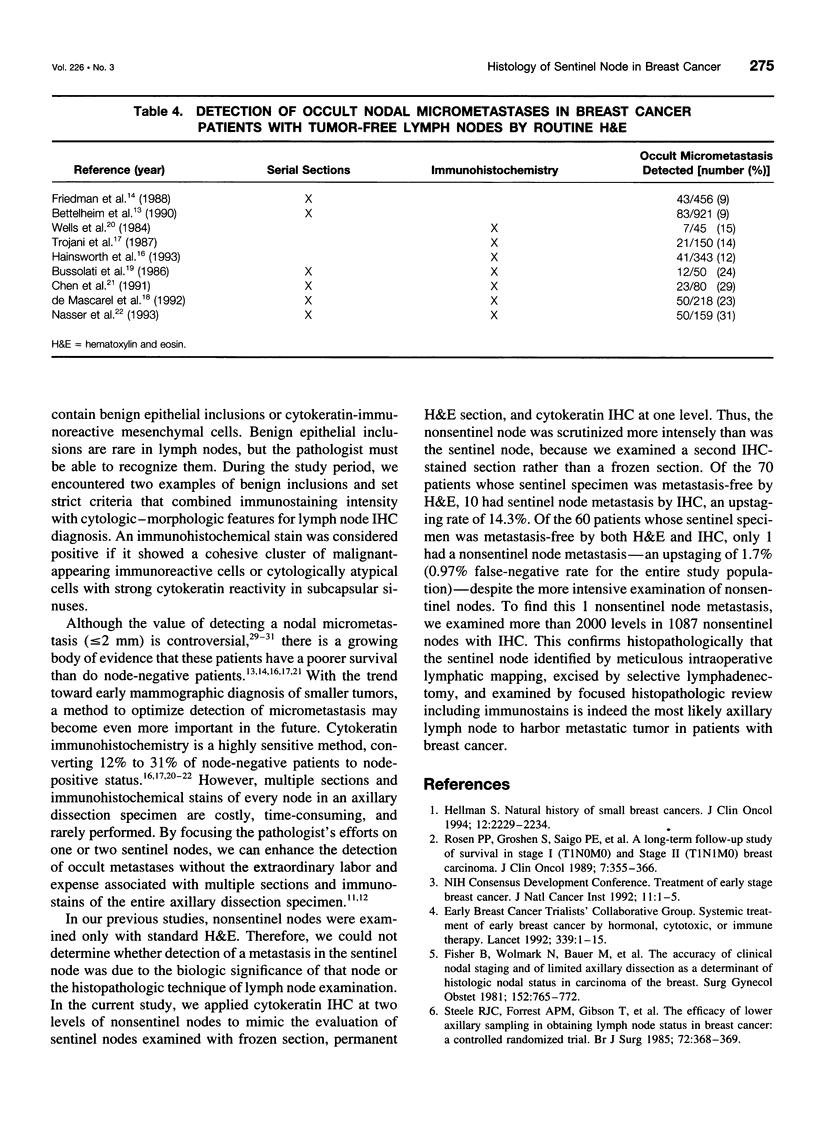
BACKGROUND AND OBJECTIVE: The sentinel node hypothesis assumes that a primary tumor drains to a specific lymph node in the regional lymphatic basin. To determine whether the sentinel node is indeed the node most likely to harbor an axillary metastasis from breast carcinoma, the authors used cytokeratin immunohistochemical staining (IHC) to examine both sentinel and nonsentinel lymph nodes. METHODS: From February 1994 through October 1995, patients with breast cancer were staged with sentinel lymphadenectomy followed by completion level I and II axillary dissection. If the sentinel node was free of metastasis by hematoxylin and eosin staining (H&E), then sentinel and nonsentinel nodes were examined with IHC. RESULTS: The 103 patients had a median age of 55 years and a median tumor size of 1.8 cm (58.3% T1, 39.8% T2, and 1.9% T3). A mean of 2 sentinel (range, 1-8) and 18.9 nonsentinel (range, 7-37) nodes were excised per patient. The H&E identified 33 patients (32%) with a sentinel lymph node metastasis and 70 patients (68%) with tumor-free sentinel nodes. Applying IHC to the 157 tumor-free sentinel nodes in these 70 patients showed an additional 10 tumor-involved nodes, each in a different patient. Thus, 10 (14.3%) of 70 patients who were tumor-free by H&E actually were sentinel node-positive, and the IHC lymph node conversion rate from sentinel node-negative to sentinel node-positive was 6.4% (10/157). Overall, sentinel node metastases were detected in 43 (41.8%) of 103 patients. In the 60 patients whose sentinel nodes were metastasis-free by H&E and IHC, 1087 nonsentinel nodes were examined at 2 levels by IHC and only 1 additional tumor-positive lymph node was identified. Therefore, one H&E sentinel node-negative patient (1.7%) was actually node-positive (p < 0.0001), and the nonsentinel IHC lymph node conversion rate was 0.09% (1/1087; p < 0.0001). CONCLUSIONS: If the sentinel node is tumor-free by both H&E and IHC, then the probability of nonsentinel node involvement is <0.1%. The true false-negative rate of this technique using multiple sections and IHC to examine all nonsentinel nodes for metastasis is 0.97% (1/103) in the authors' hands. The sentinel lymph node is indeed the most likely axillary node to harbor metastatic breast carcinoma.
Full text
PDF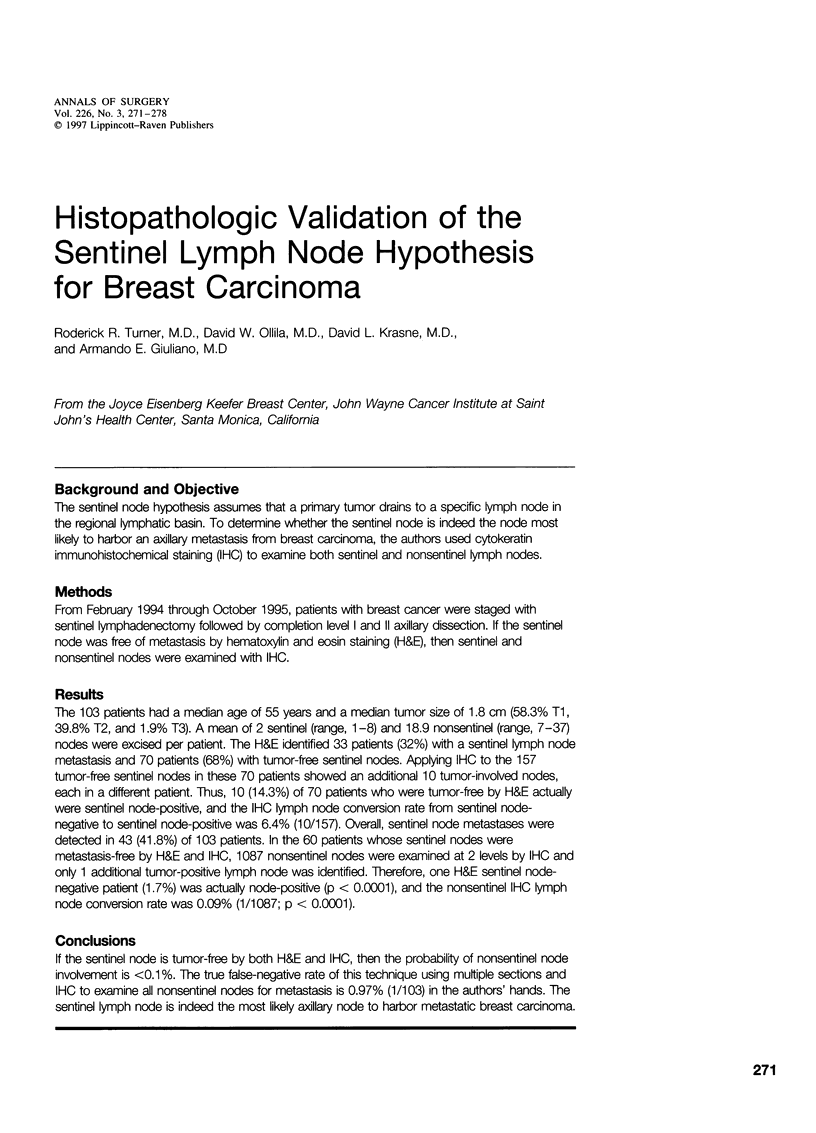
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bussolati G., Gugliotta P., Morra I., Pietribiasi F., Berardengo E. The immunohistochemical detection of lymph node metastases from infiltrating lobular carcinoma of the breast. Br J Cancer. 1986 Oct;54(4):631–636. doi: 10.1038/bjc.1986.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z. L., Wen D. R., Coulson W. F., Giuliano A. E., Cochran A. J. Occult metastases in the axillary lymph nodes of patients with breast cancer node negative by clinical and histologic examination and conventional histology. Dis Markers. 1991 Sep-Oct;9(5):239–248. [PubMed] [Google Scholar]
- Clayton F., Hopkins C. L. Pathologic correlates of prognosis in lymph node-positive breast carcinomas. Cancer. 1993 Mar 1;71(5):1780–1790. doi: 10.1002/1097-0142(19930301)71:5<1780::aid-cncr2820710512>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- Edlow D. W., Carter D. Heterotopic epithelium in axillary lymph nodes: report of a case and review of the literature. Am J Clin Pathol. 1973 May;59(5):666–673. doi: 10.1093/ajcp/59.5.666. [DOI] [PubMed] [Google Scholar]
- Fisher B., Wolmark N., Bauer M., Redmond C., Gebhardt M. The accuracy of clinical nodal staging and of limited axillary dissection as a determinant of histologic nodal status in carcinoma of the breast. Surg Gynecol Obstet. 1981 Jun;152(6):765–772. [PubMed] [Google Scholar]
- Fisher E. R., Palekar A., Rockette H., Redmond C., Fisher B. Pathologic findings from the National Surgical Adjuvant Breast Project (Protocol No. 4). V. Significance of axillary nodal micro- and macrometastases. Cancer. 1978 Oct;42(4):2032–2038. doi: 10.1002/1097-0142(197810)42:4<2032::aid-cncr2820420453>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Friedman S., Bertin F., Mouriesse H., Benchabat A., Genin J., Sarrazin D., Contesso G. Importance of tumor cells in axillary node sinus margins ('clandestine' metastases) discovered by serial sectioning in operable breast carcinoma. Acta Oncol. 1988;27(5):483–487. doi: 10.3109/02841868809093575. [DOI] [PubMed] [Google Scholar]
- Giuliano A. E., Dale P. S., Turner R. R., Morton D. L., Evans S. W., Krasne D. L. Improved axillary staging of breast cancer with sentinel lymphadenectomy. Ann Surg. 1995 Sep;222(3):394–401. doi: 10.1097/00000658-199509000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giuliano A. E., Kirgan D. M., Guenther J. M., Morton D. L. Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann Surg. 1994 Sep;220(3):391–401. doi: 10.1097/00000658-199409000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hainsworth P. J., Tjandra J. J., Stillwell R. G., Machet D., Henderson M. A., Rennie G. C., McKenzie I. F., Bennett R. C. Detection and significance of occult metastases in node-negative breast cancer. Br J Surg. 1993 Apr;80(4):459–463. doi: 10.1002/bjs.1800800417. [DOI] [PubMed] [Google Scholar]
- Hellman S. Karnofsky Memorial Lecture. Natural history of small breast cancers. J Clin Oncol. 1994 Oct;12(10):2229–2234. doi: 10.1200/JCO.1994.12.10.2229. [DOI] [PubMed] [Google Scholar]
- Holdsworth P. J., Hopkinson J. M., Leveson S. H. Benign axillary epithelial lymph node inclusions--a histological pitfall. Histopathology. 1988 Aug;13(2):226–228. doi: 10.1111/j.1365-2559.1988.tb02029.x. [DOI] [PubMed] [Google Scholar]
- Kissin M. W., Thompson E. M., Price A. B., Slavin G., Kark A. E. The inadequacy of axillary sampling in breast cancer. Lancet. 1982 May 29;1(8283):1210–1212. doi: 10.1016/s0140-6736(82)92337-6. [DOI] [PubMed] [Google Scholar]
- Kjaergaard J., Blichert-Toft M., Andersen J. A., Rank F., Pedersen B. V. Probability of false negative nodal staging in conjunction with partial axillary dissection in breast cancer. Br J Surg. 1985 May;72(5):365–367. doi: 10.1002/bjs.1800720511. [DOI] [PubMed] [Google Scholar]
- Mathiesen O., Carl J., Bonderup O., Panduro J. Axillary sampling and the risk of erroneous staging of breast cancer. An analysis of 960 consecutive patients. Acta Oncol. 1990;29(6):721–725. doi: 10.3109/02841869009092990. [DOI] [PubMed] [Google Scholar]
- Moffat F. L., Jr, Senofsky G. M., Davis K., Clark K. C., Robinson D. S., Ketcham A. S. Axillary node dissection for early breast cancer: some is good, but all is better. J Surg Oncol. 1992 Sep;51(1):8–13. doi: 10.1002/jso.2930510105. [DOI] [PubMed] [Google Scholar]
- Nasser I. A., Lee A. K., Bosari S., Saganich R., Heatley G., Silverman M. L. Occult axillary lymph node metastases in "node-negative" breast carcinoma. Hum Pathol. 1993 Sep;24(9):950–957. doi: 10.1016/0046-8177(93)90108-s. [DOI] [PubMed] [Google Scholar]
- Neville A. M., Price K. N., Gelber R. D., Goldhirsch A. Axillary node micrometastases and breast cancer. Lancet. 1991 May 4;337(8749):1110–1110. doi: 10.1016/0140-6736(91)91768-p. [DOI] [PubMed] [Google Scholar]
- Prognostic importance of occult axillary lymph node micrometastases from breast cancers. International (Ludwig) Breast Cancer Study Group. Lancet. 1990 Jun 30;335(8705):1565–1568. [PubMed] [Google Scholar]
- Rosen P. P., Saigo P. E., Braun D. W., Weathers E., Fracchia A. A., Kinne D. W. Axillary micro- and macrometastases in breast cancer: prognostic significance of tumor size. Ann Surg. 1981 Nov;194(5):585–591. doi: 10.1097/00000658-198111000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen P. R., Groshen S., Saigo P. E., Kinne D. W., Hellman S. A long-term follow-up study of survival in stage I (T1N0M0) and stage II (T1N1M0) breast carcinoma. J Clin Oncol. 1989 Mar;7(3):355–366. doi: 10.1200/JCO.1989.7.3.355. [DOI] [PubMed] [Google Scholar]
- Steele R. J., Forrest A. P., Gibson T., Stewart H. J., Chetty U. The efficacy of lower axillary sampling in obtaining lymph node status in breast cancer: a controlled randomized trial. Br J Surg. 1985 May;72(5):368–369. doi: 10.1002/bjs.1800720512. [DOI] [PubMed] [Google Scholar]
- Trojani M., de Mascarel I., Bonichon F., Coindre J. M., Delsol G. Micrometastases to axillary lymph nodes from carcinoma of breast: detection by immunohistochemistry and prognostic significance. Br J Cancer. 1987 Mar;55(3):303–306. doi: 10.1038/bjc.1987.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells C. A., Heryet A., Brochier J., Gatter K. C., Mason D. Y. The immunocytochemical detection of axillary micrometastases in breast cancer. Br J Cancer. 1984 Aug;50(2):193–197. doi: 10.1038/bjc.1984.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson E. J., Hause L. L., Hoffman R. G., Kuzma J. F., Rothwell D. J., Donegan W. L., Clowry L. J., Almagro U. A., Choi H., Rimm A. A. Occult axillary lymph node metastases in invasive breast carcinoma: characteristics of the primary tumor and significance of the metastases. Pathol Annu. 1982;17(Pt 2):67–91. [PubMed] [Google Scholar]
- de Mascarel I., Bonichon F., Coindre J. M., Trojani M. Prognostic significance of breast cancer axillary lymph node micrometastases assessed by two special techniques: reevaluation with longer follow-up. Br J Cancer. 1992 Sep;66(3):523–527. doi: 10.1038/bjc.1992.306. [DOI] [PMC free article] [PubMed] [Google Scholar]


