Abstract
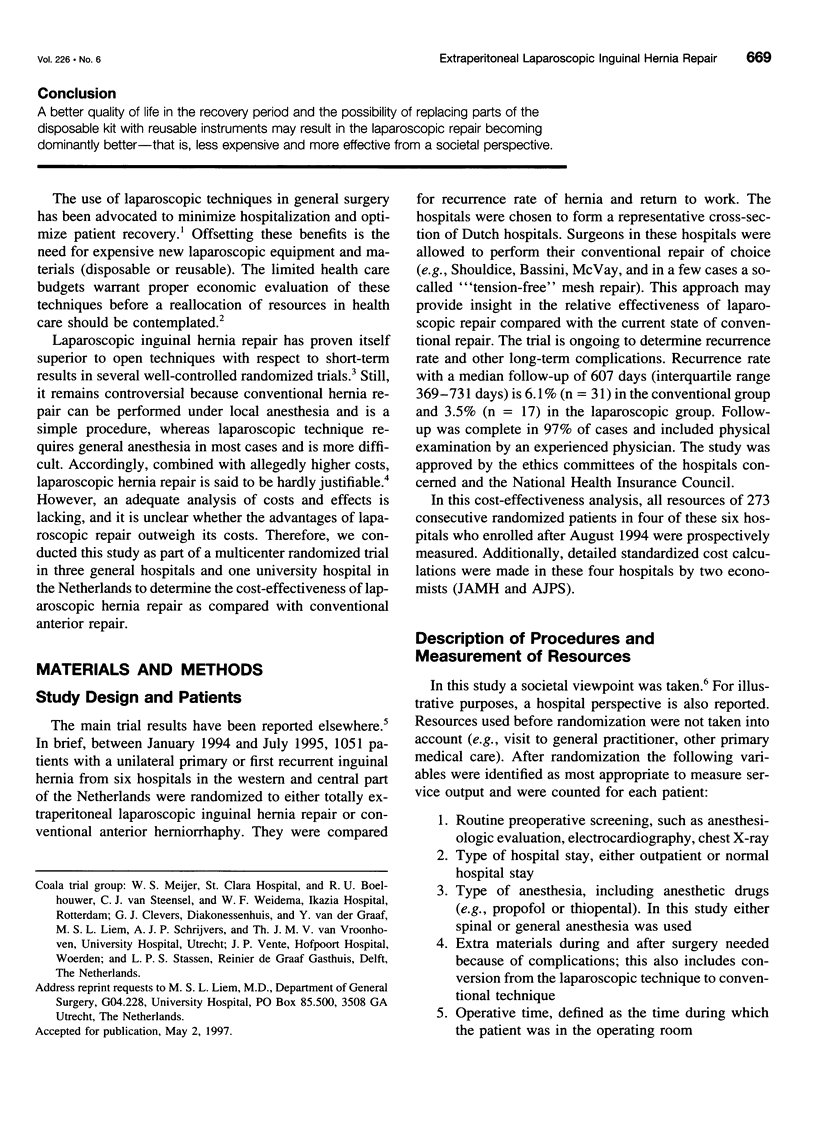
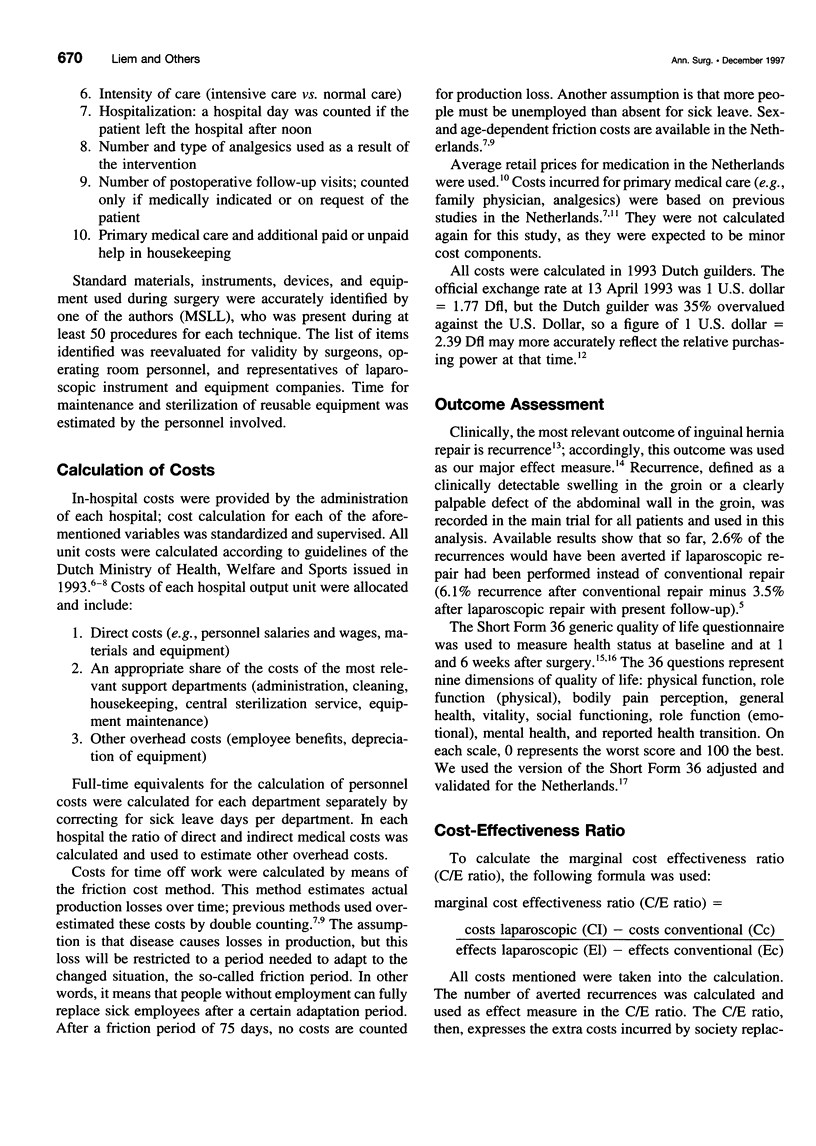
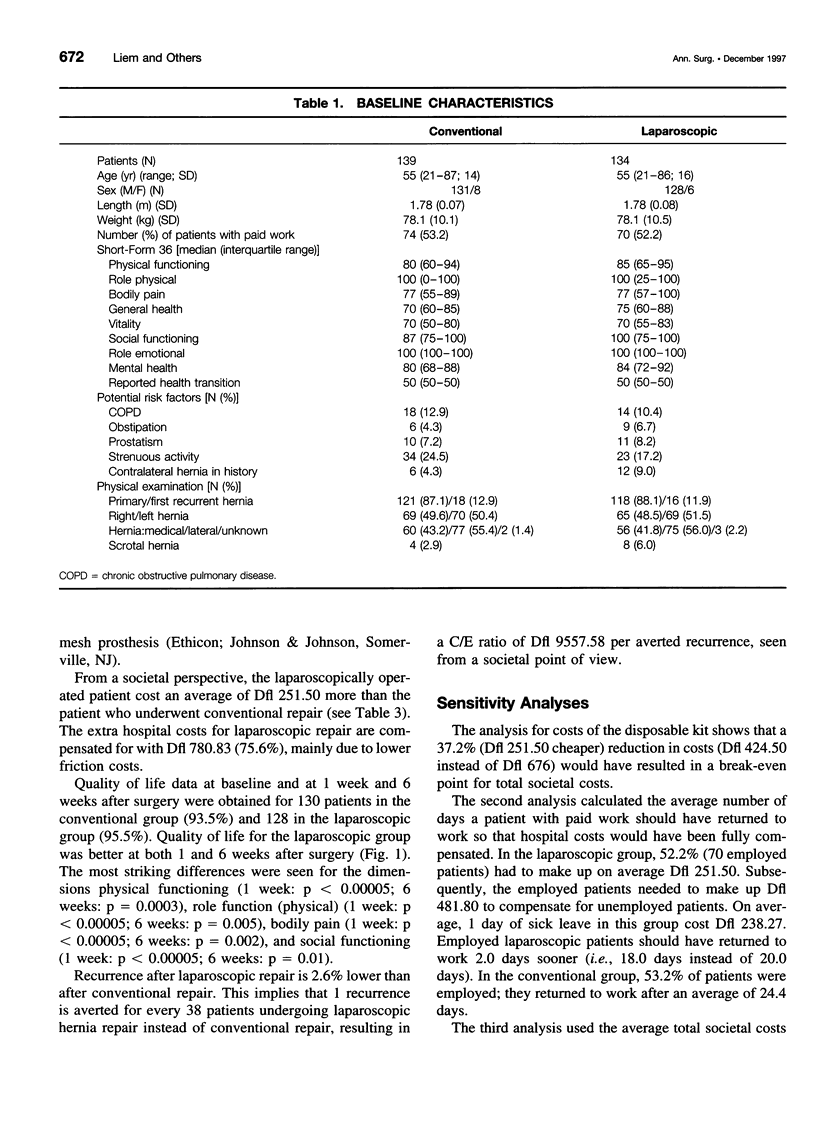
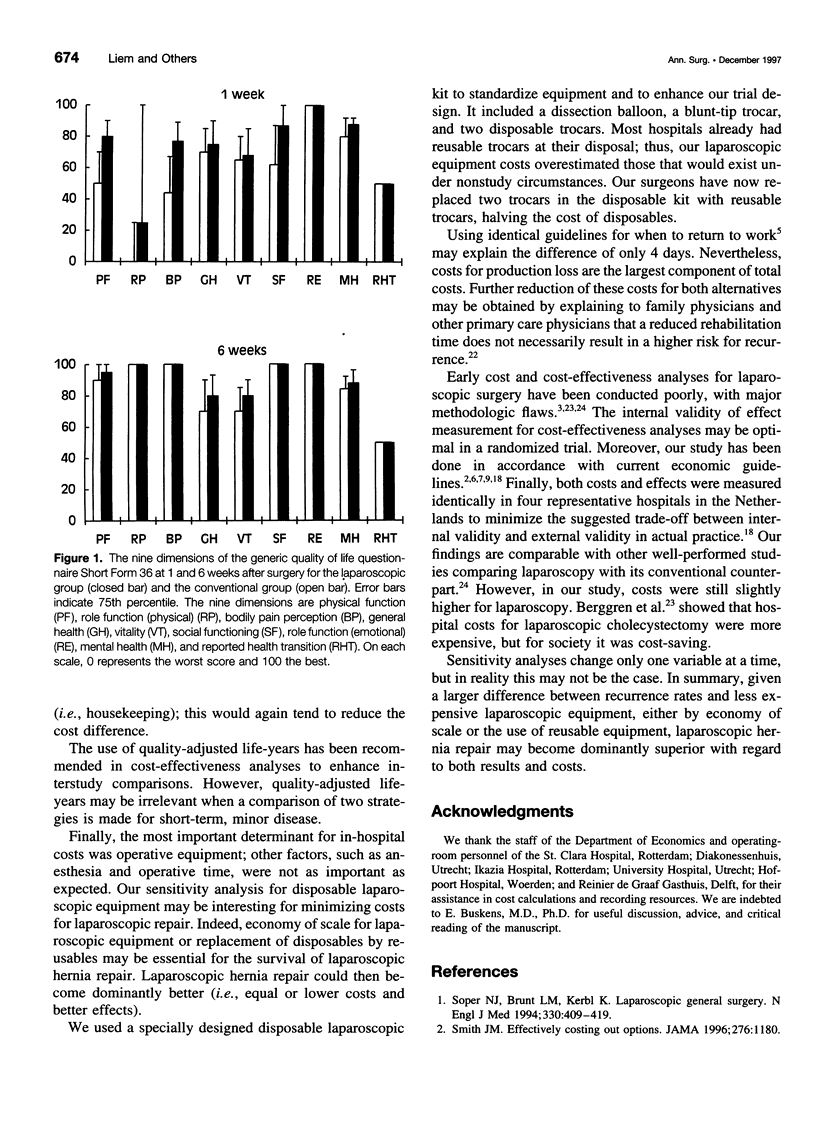
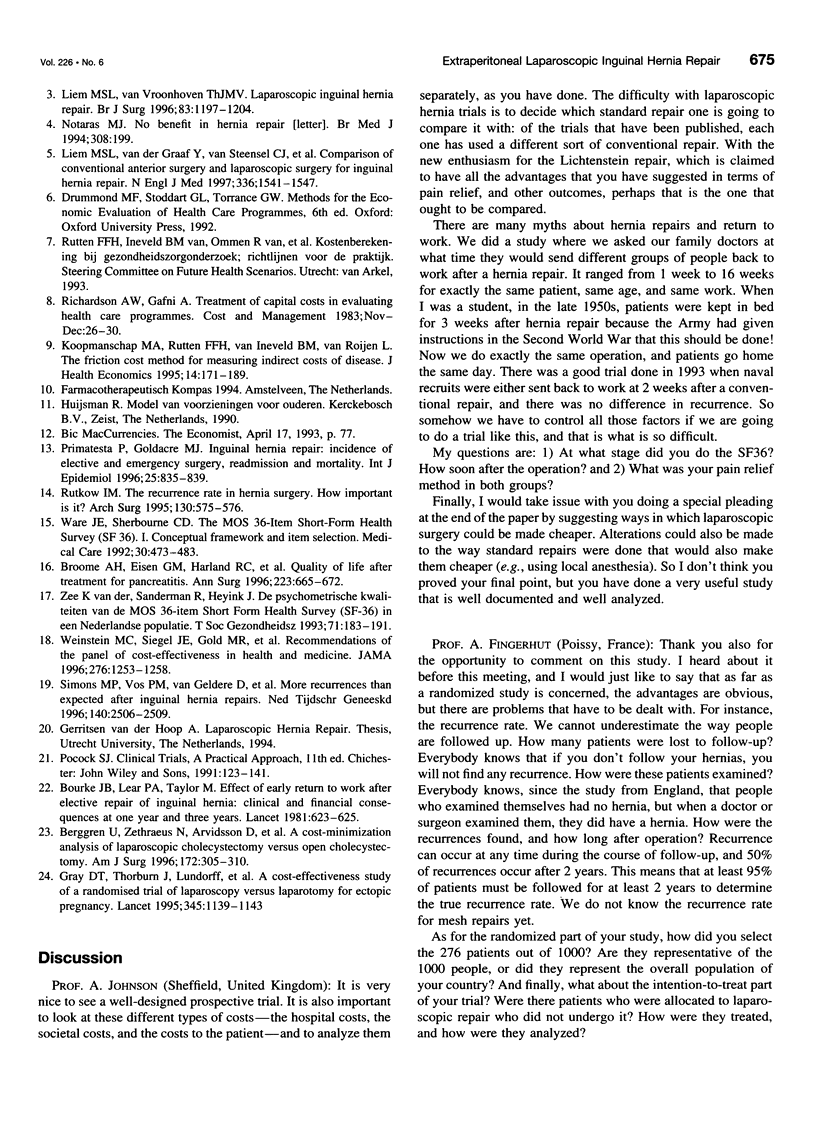
OBJECTIVE: To determine the cost-effectiveness of laparoscopic inguinal hernia repair. SUMMARY BACKGROUND DATA: Laparoscopic inguinal hernia repair seems superior to open techniques with respect to short-term results. An issue yet to be studied in depth remains the cost-effectiveness of the procedure. As part of a multicenter randomized study in which >1000 patients were included, a cost-effectiveness analysis from a societal point of view was performed. METHODS: After informed consent, all resource costs, both in and outside the hospital, for patients between August 1994 and July 1995 were recorded prospectively. Actual costs were calculated in a standardized fashion according to international guidelines. The main measures used for the evaluation of inguinal hernia repair were the number of averted recurrences and quality of life measured with the Short Form 36 questionnaire. RESULTS: Resource costs were recorded for 273 patients, 139 in the open and 134 in the laparoscopic group. Both groups were comparable at baseline. Average total hospital costs were Dfl 1384.91 (standard deviation: Dfl 440.15) for the open repair group and Dfl 2417.24 (standard deviation: Dfl 577.10) for laparoscopic repair, including a disposable kit of Dfl 676. Societal costs, including costs for days of sick leave, were lower for the laparoscopic repair and offset the hospital costs by Dfl 780.83 (75.6%), leaving the laparoscopic repair Dfl 251.50 more expensive (Dfl 4665 versus Dfl 4916.50). At present, the recurrence rate is 2.6% lower after laparoscopic repair. Thus, 38 laparoscopic repairs, costing an additional Dfl 9,557, prevent the occurrence of one recurrent hernia. Quality of life was better after laparoscopic repair. CONCLUSION: A better quality of life in the recovery period and the possibility of replacing parts of the disposable kit with reusable instruments may result in the laparoscopic repair becoming dominantly better--that is, less expensive and more effective from a societal perspective.
Full text
PDF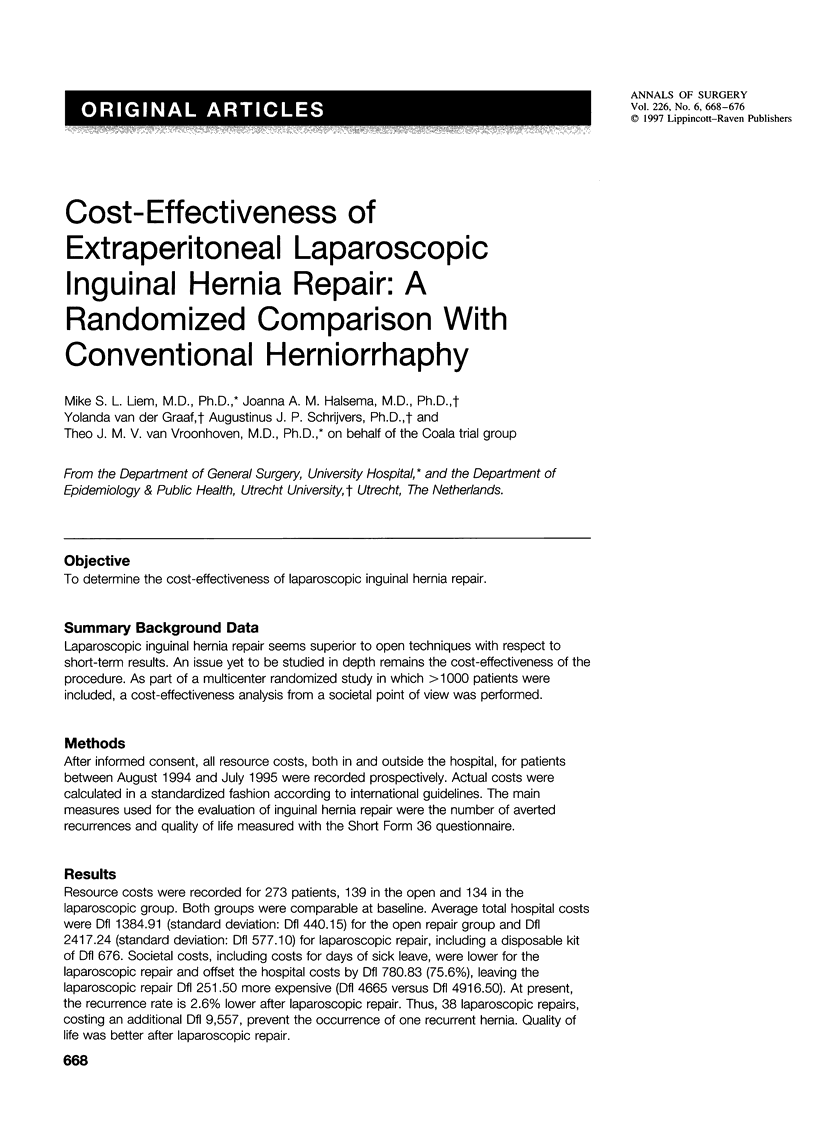

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berggren U., Zethraeus N., Arvidsson D., Haglund U., Jonsson B. A cost-minimization analysis of laparoscopic cholecystectomy versus open cholecystectomy. Am J Surg. 1996 Oct;172(4):305–310. doi: 10.1016/S0002-9610(96)00197-3. [DOI] [PubMed] [Google Scholar]
- Bourke J. B., Lear P. A., Taylor M. Effect of early return to work after elective repair of inguinal hernia: Clinical and financial consequences at one year and three years. Lancet. 1981 Sep 19;2(8247):623–625. doi: 10.1016/s0140-6736(81)92756-2. [DOI] [PubMed] [Google Scholar]
- Broome A. H., Eisen G. M., Harland R. C., Collins B. H., Meyers W. C., Pappas T. N. Quality of life after treatment for pancreatitis. Ann Surg. 1996 Jun;223(6):665–672. doi: 10.1097/00000658-199606000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray D. T., Thorburn J., Lundorff P., Strandell A., Lindblom B. A cost-effectiveness study of a randomised trial of laparoscopy versus laparotomy for ectopic pregnancy. Lancet. 1995 May 6;345(8958):1139–1143. doi: 10.1016/s0140-6736(95)90977-x. [DOI] [PubMed] [Google Scholar]
- Koopmanschap M. A., Rutten F. F., van Ineveld B. M., van Roijen L. The friction cost method for measuring indirect costs of disease. J Health Econ. 1995 Jun;14(2):171–189. doi: 10.1016/0167-6296(94)00044-5. [DOI] [PubMed] [Google Scholar]
- Liem M. S., van Vroonhoven T. J. Laparoscopic inguinal hernia repair. Br J Surg. 1996 Sep;83(9):1197–1204. [PubMed] [Google Scholar]
- Liem M. S., van der Graaf Y., van Steensel C. J., Boelhouwer R. U., Clevers G. J., Meijer W. S., Stassen L. P., Vente J. P., Weidema W. F., Schrijvers A. J. Comparison of conventional anterior surgery and laparoscopic surgery for inguinal-hernia repair. N Engl J Med. 1997 May 29;336(22):1541–1547. doi: 10.1056/NEJM199705293362201. [DOI] [PubMed] [Google Scholar]
- Notaras M. J. Minimally invasive surgery. No benefit in hernia repair... BMJ. 1994 Jan 15;308(6922):199–199. doi: 10.1136/bmj.308.6922.199b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primatesta P., Goldacre M. J. Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol. 1996 Aug;25(4):835–839. doi: 10.1093/ije/25.4.835. [DOI] [PubMed] [Google Scholar]
- Rutkow I. M. The recurrence rate in hernia surgery. How important is it? Arch Surg. 1995 Jun;130(6):575–577. doi: 10.1001/archsurg.1995.01430060013001. [DOI] [PubMed] [Google Scholar]
- Simons M. P., Vos P. M., van Geldere D., Hoitsma H. F., Obertop H. Meer recidieven na liesbreukchirurgie dan verwacht. Ned Tijdschr Geneeskd. 1996 Dec 14;140(50):2506–2509. [PubMed] [Google Scholar]
- Smith J. M. Effectively costing out options. JAMA. 1996 Oct 9;276(14):1180–1180. [PubMed] [Google Scholar]
- Soper N. J., Brunt L. M., Kerbl K. Laparoscopic general surgery. N Engl J Med. 1994 Feb 10;330(6):409–419. doi: 10.1056/NEJM199402103300608. [DOI] [PubMed] [Google Scholar]
- Ware J. E., Jr, Sherbourne C. D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992 Jun;30(6):473–483. [PubMed] [Google Scholar]
- Weinstein M. C., Siegel J. E., Gold M. R., Kamlet M. S., Russell L. B. Recommendations of the Panel on Cost-effectiveness in Health and Medicine. JAMA. 1996 Oct 16;276(15):1253–1258. [PubMed] [Google Scholar]


