Abstract
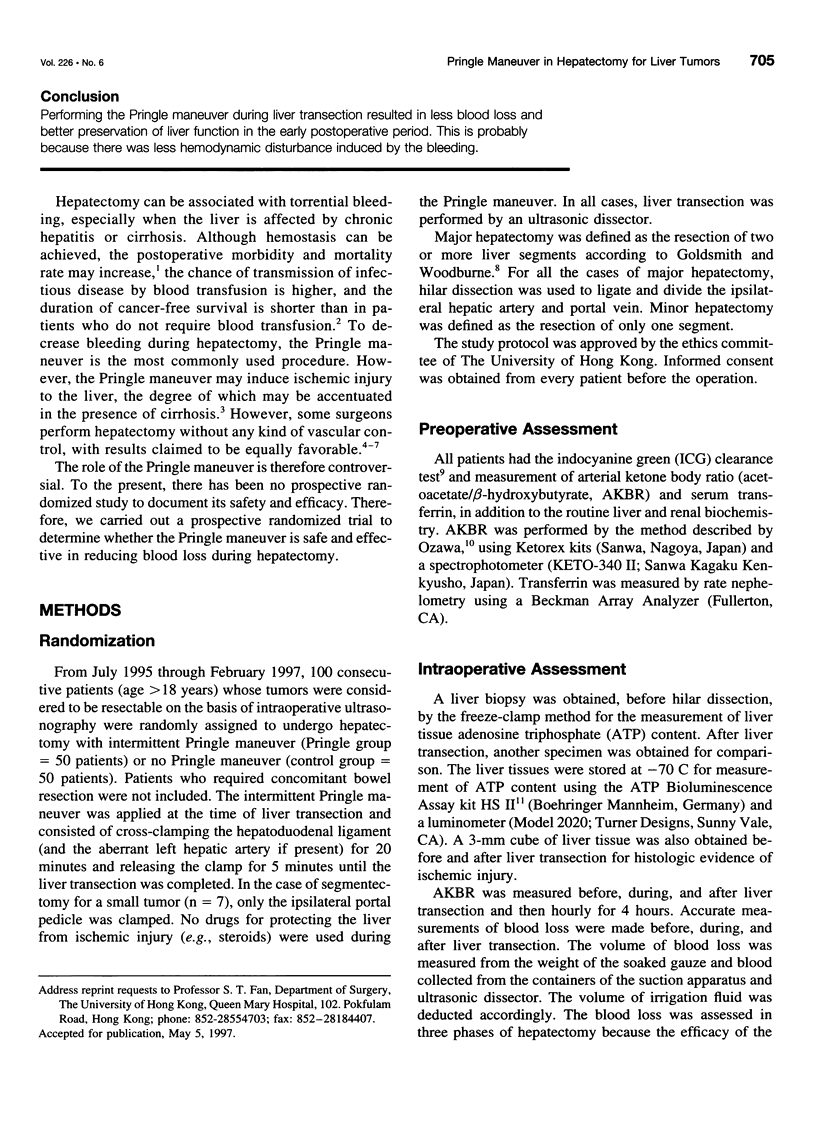
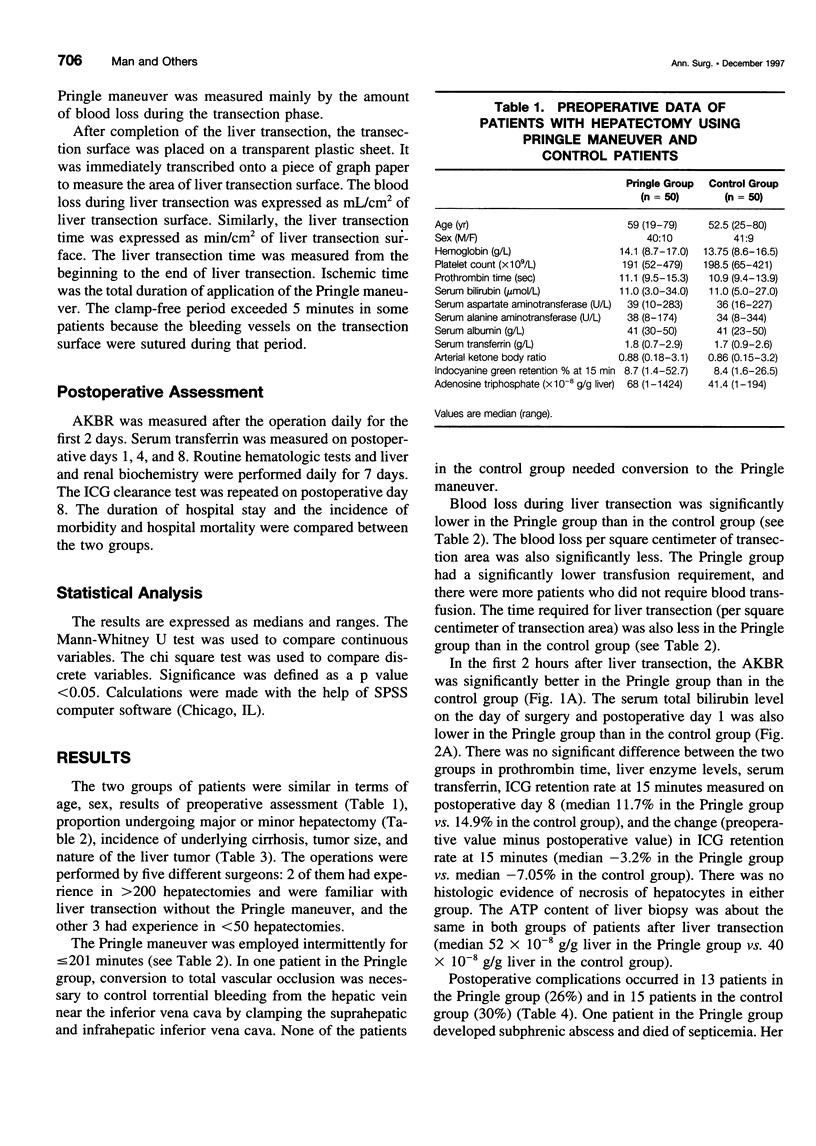
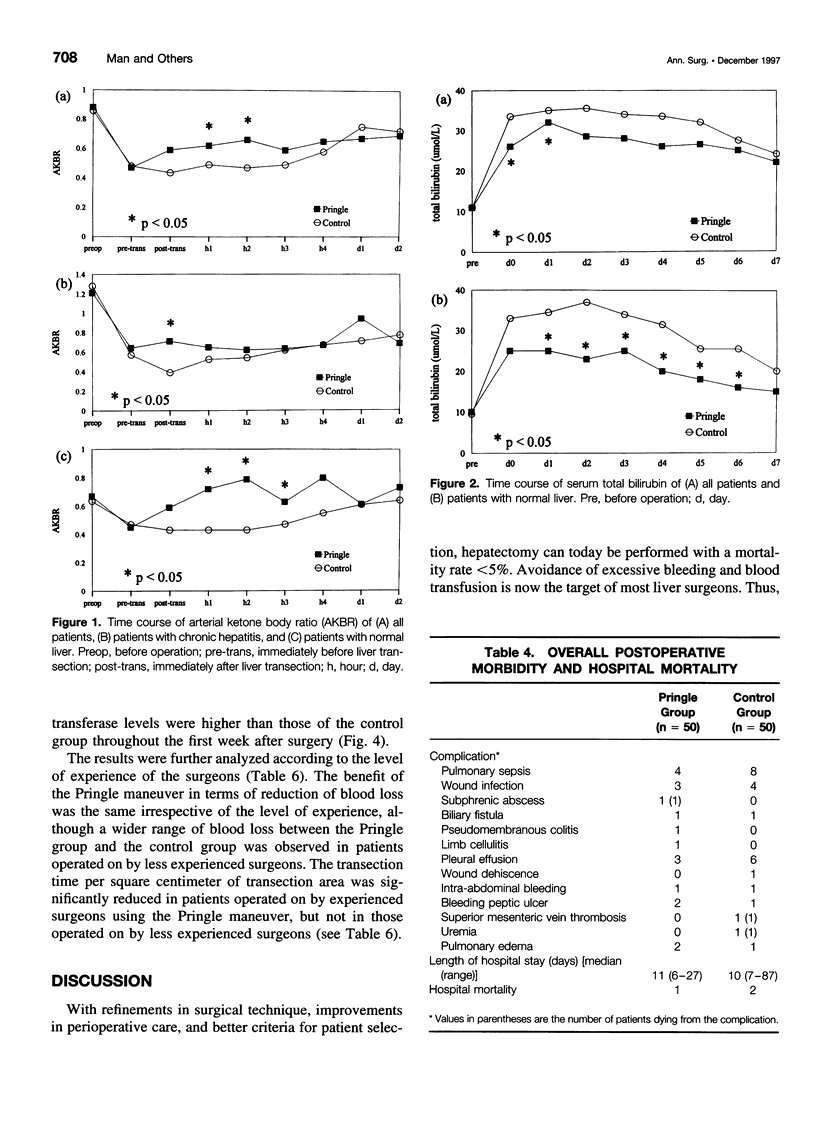
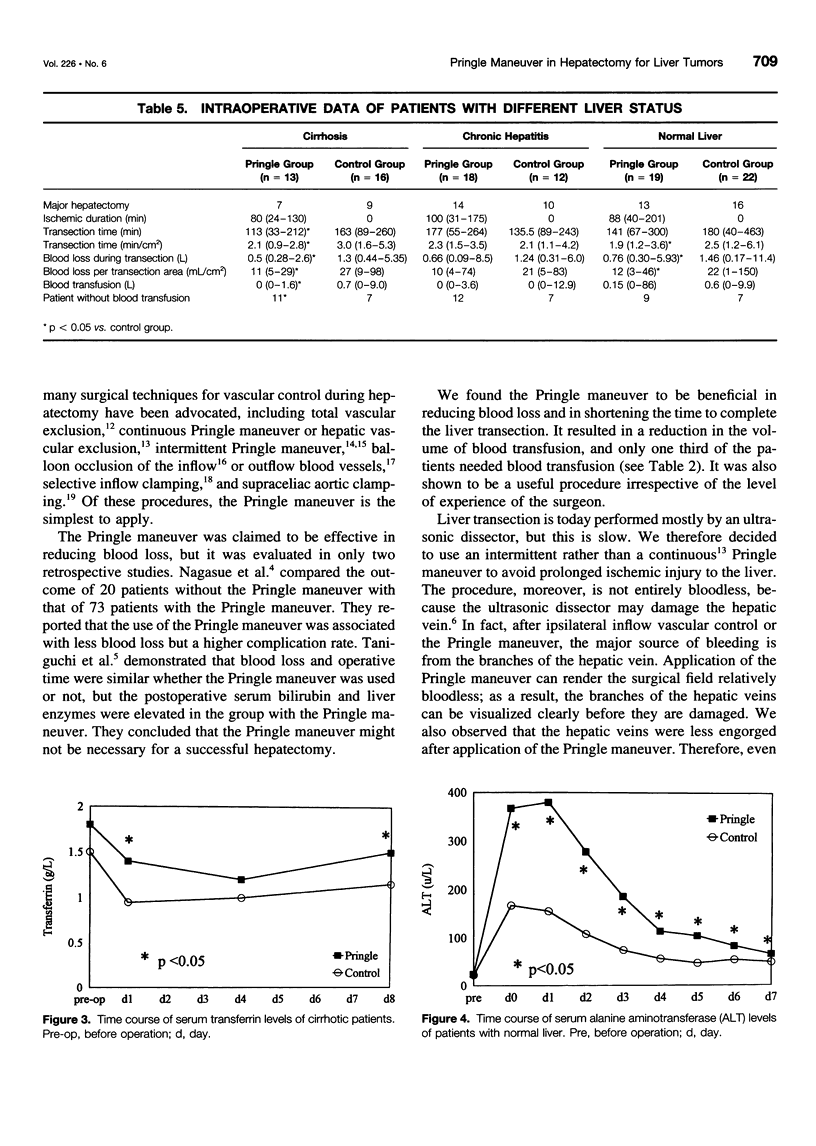
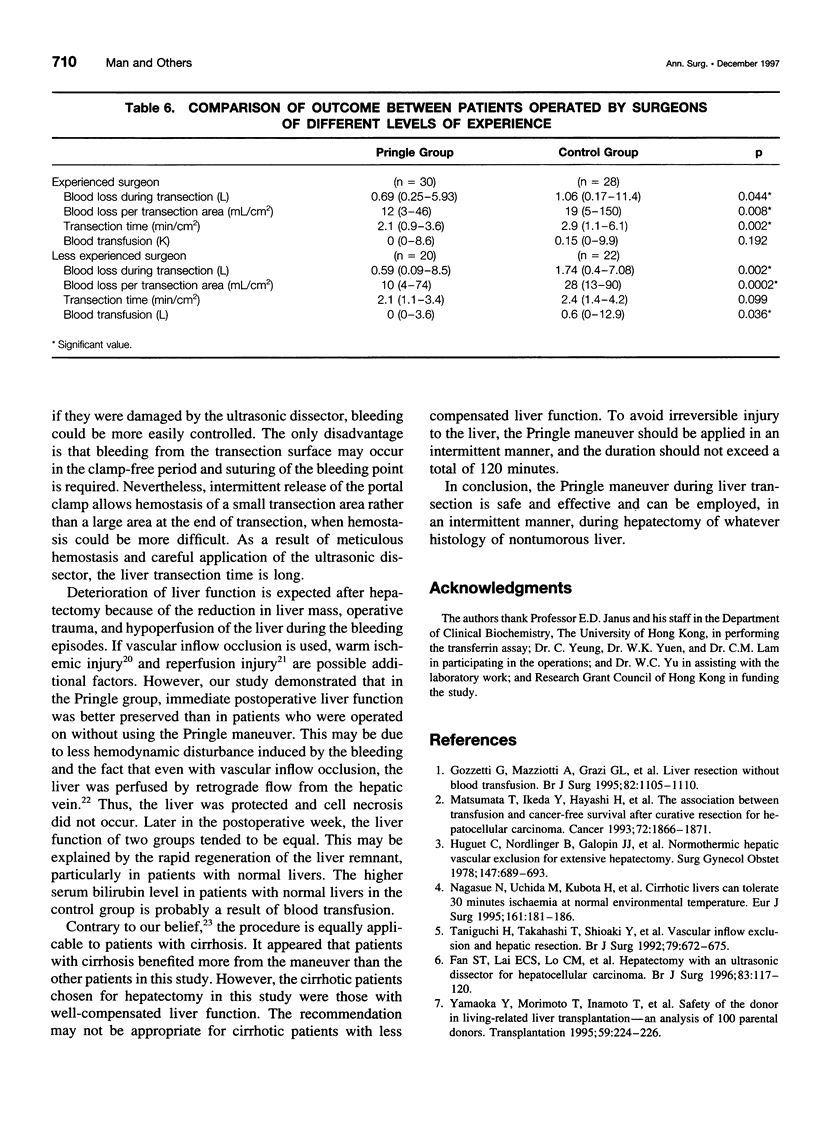
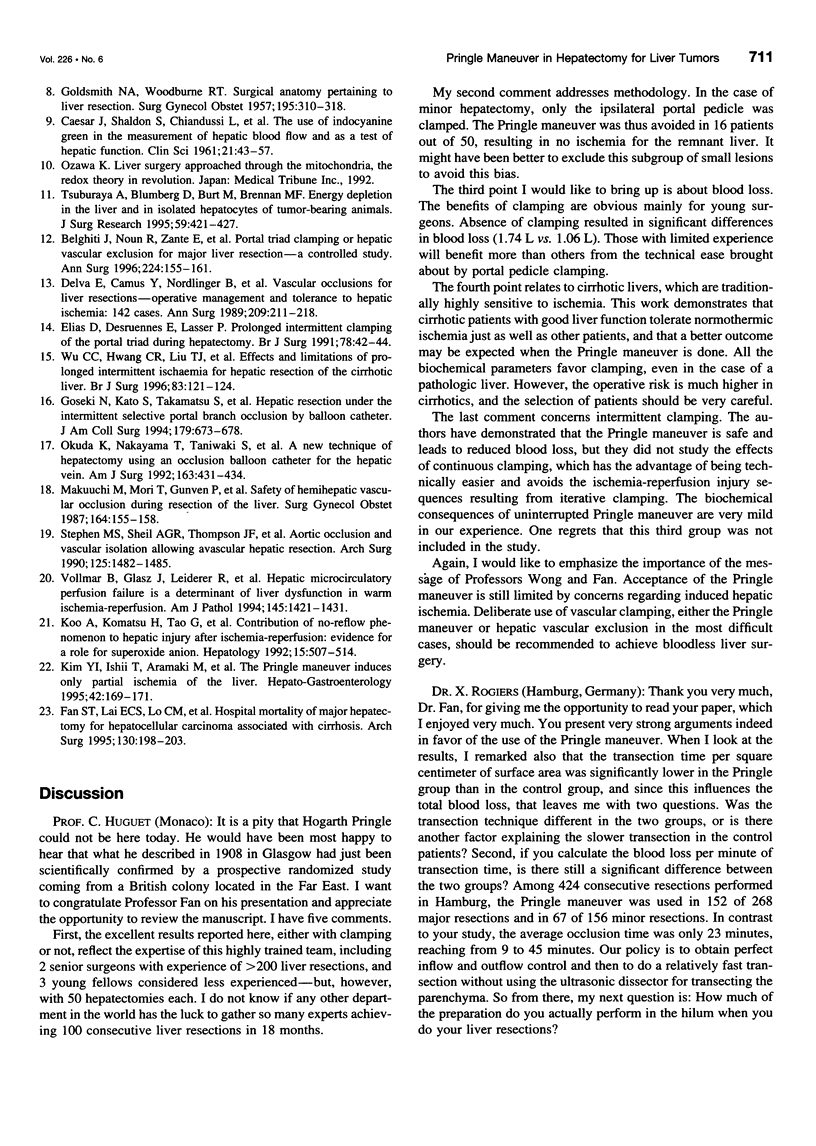
OBJECTIVE: To evaluate whether vascular inflow occlusion by the Pringle maneuver during hepatectomy can be safe and effective in reducing blood loss. SUMMARY BACKGROUND DATA: Hepatectomy can be performed with a low mortality rate, but massive hemorrhage during surgery remains a potentially lethal problem. The Pringle maneuver is traditionally used during hepatectomy to reduce blood loss, but there is a potential harmful effect on the metabolic function of hepatocytes. There has been no prospective randomized study to determine whether the Pringle maneuver can decrease blood loss during hepatectomy, improve outcome, or affect the metabolism of hepatocytes. METHODS: From July 1995 to February 1997, we studied 100 consecutive patients who underwent hepatectomy for liver tumors. The patients were randomly assigned to liver transection under intermittent Pringle maneuver of 20 minutes and a 5-minute clamp-free interval (n = 50), or liver transection without the Pringle maneuver (n = 50). The surface area of liver transection was measured and blood loss during transection per square centimeter of transection area was calculated. Routine liver biochemistry, arterial ketone body ratio (AKBR), and the indocyanine green (ICG) clearance test were done. RESULTS: The two groups were comparable in terms of preoperative liver function and in the proportion of patients having major hepatectomy. The Pringle maneuver resulted in less blood loss per square centimeter of transection area (12 mL/cm2 vs. 22 mL/cm2, p = 0.0001), a shorter transection time per square centimeter of transection area (2 min/cm2 vs. 2.8 min/cm2, p = 0.016), a significantly higher AKBR in the first 2 hours after hepatectomy, lower serum bilirubin levels in the early postoperative period, and, in cirrhotic patients, higher serum transferrin levels on postoperative days 1 and 8. The complication rate, the hospital mortality rate, and the ICG retention at 15 minutes on postoperative day 8 were equal for the two groups.CONCLUSION: Performing the Pringle maneuver during liver transection resulted in less blood loss and better preservation of liver function in the early postoperative period. This is probably because there was less hemodynamic disturbance induced by the bleeding.
Full text
PDF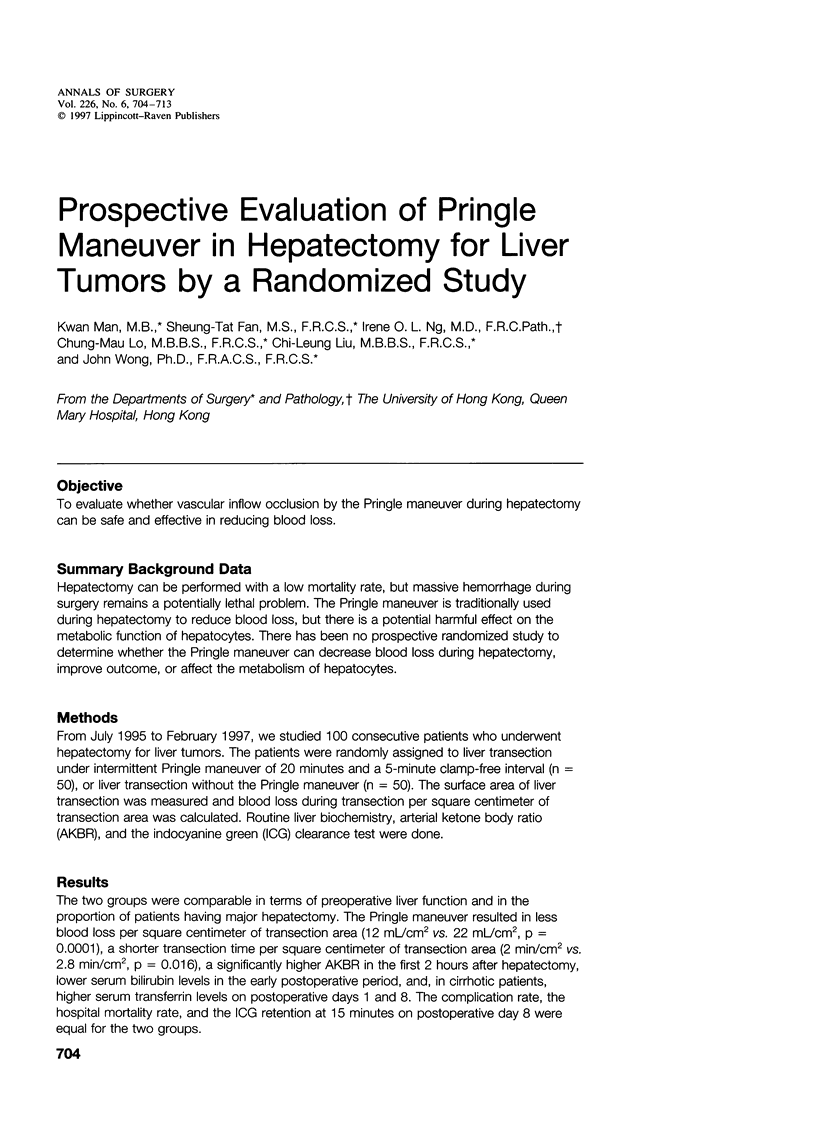

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Belghiti J., Noun R., Zante E., Ballet T., Sauvanet A. Portal triad clamping or hepatic vascular exclusion for major liver resection. A controlled study. Ann Surg. 1996 Aug;224(2):155–161. doi: 10.1097/00000658-199608000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CAESAR J., SHALDON S., CHIANDUSSI L., GUEVARA L., SHERLOCK S. The use of indocyanine green in the measurement of hepatic blood flow and as a test of hepatic function. Clin Sci. 1961 Aug;21:43–57. [PubMed] [Google Scholar]
- Delva E., Camus Y., Nordlinger B., Hannoun L., Parc R., Deriaz H., Lienhart A., Huguet C. Vascular occlusions for liver resections. Operative management and tolerance to hepatic ischemia: 142 cases. Ann Surg. 1989 Feb;209(2):211–218. doi: 10.1097/00000658-198902000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elias D., Desruennes E., Lasser P. Prolonged intermittent clamping of the portal triad during hepatectomy. Br J Surg. 1991 Jan;78(1):42–44. doi: 10.1002/bjs.1800780115. [DOI] [PubMed] [Google Scholar]
- Fan S. T., Lai E. C., Lo C. M., Chu K. M., Liu C. L., Wong J. Hepatectomy with an ultrasonic dissector for hepatocellular carcinoma. Br J Surg. 1996 Jan;83(1):117–120. doi: 10.1002/bjs.1800830138. [DOI] [PubMed] [Google Scholar]
- Fan S. T., Lai E. C., Lo C. M., Ng I. O., Wong J. Hospital mortality of major hepatectomy for hepatocellular carcinoma associated with cirrhosis. Arch Surg. 1995 Feb;130(2):198–203. doi: 10.1001/archsurg.1995.01430020088017. [DOI] [PubMed] [Google Scholar]
- GOLDSMITH N. A., WOODBURNE R. T. The surgical anatomy pertaining to liver resection. Surg Gynecol Obstet. 1957 Sep;105(3):310–318. [PubMed] [Google Scholar]
- Goseki N., Kato S., Takamatsu S., Dobashi Y., Hara Y., Teramoto K., Nakamura H., Endo M., Shimojyu K. Hepatic resection under the intermittent selective portal branch occlusion by balloon catheter. J Am Coll Surg. 1994 Dec;179(6):673–678. [PubMed] [Google Scholar]
- Gozzetti G., Mazziotti A., Grazi G. L., Jovine E., Gallucci A., Gruttadauria S., Frena A., Morganti M., Ercolani G., Masetti M. Liver resection without blood transfusion. Br J Surg. 1995 Aug;82(8):1105–1110. doi: 10.1002/bjs.1800820833. [DOI] [PubMed] [Google Scholar]
- Huguet C., Nordlinger B., Galopin J. J., Bloch P., Gallot D. Normothermic hepatic vascular exclusion for extensive hepatectomy. Surg Gynecol Obstet. 1978 Nov;147(5):689–693. [PubMed] [Google Scholar]
- Kim Y. I., Ishii T., Aramaki M., Nakashima K., Yoshida T., Kobayashi M. The Pringle maneuver induces only partial ischemia of the liver. Hepatogastroenterology. 1995 Apr;42(2):169–171. [PubMed] [Google Scholar]
- Koo A., Komatsu H., Tao G., Inoue M., Guth P. H., Kaplowitz N. Contribution of no-reflow phenomenon to hepatic injury after ischemia-reperfusion: evidence for a role for superoxide anion. Hepatology. 1992 Mar;15(3):507–514. doi: 10.1002/hep.1840150325. [DOI] [PubMed] [Google Scholar]
- Makuuchi M., Mori T., Gunvén P., Yamazaki S., Hasegawa H. Safety of hemihepatic vascular occlusion during resection of the liver. Surg Gynecol Obstet. 1987 Feb;164(2):155–158. [PubMed] [Google Scholar]
- Matsumata T., Ikeda Y., Hayashi H., Kamakura T., Taketomi A., Sugimachi K. The association between transfusion and cancer-free survival after curative resection for hepatocellular carcinoma. Cancer. 1993 Sep 15;72(6):1866–1871. doi: 10.1002/1097-0142(19930915)72:6<1866::aid-cncr2820720613>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Nagasue N., Uchida M., Kubota H., Hayashi T., Kohno H., Nakamura T. Cirrhotic livers can tolerate 30 minutes ischaemia at normal environmental temperature. Eur J Surg. 1995 Mar;161(3):181–186. [PubMed] [Google Scholar]
- Okuda K., Nakayama T., Taniwaki S., Ando K., Shigetomi K., Matsumoto A., Muta M., Mada Y., Saitsu H. A new technique of hepatectomy using an occlusion balloon catheter for the hepatic vein. Am J Surg. 1992 Apr;163(4):431–434. doi: 10.1016/0002-9610(92)90047-u. [DOI] [PubMed] [Google Scholar]
- Stephen M. S., Sheil A. G., Thompson J. F., Wilson T., Boland S. L. Aortic occlusion and vascular isolation allowing avascular hepatic resection. Arch Surg. 1990 Nov;125(11):1482–1485. doi: 10.1001/archsurg.1990.01410230076013. [DOI] [PubMed] [Google Scholar]
- Taniguchi H., Takahashi T., Shioaki Y., Itoh A., Oguro A. Vascular inflow exclusion and hepatic resection. Br J Surg. 1992 Jul;79(7):672–675. doi: 10.1002/bjs.1800790726. [DOI] [PubMed] [Google Scholar]
- Tsuburaya A., Blumberg D., Burt M., Brennan M. F. Energy depletion in the liver and in isolated hepatocytes of tumor-bearing animals. J Surg Res. 1995 Oct;59(4):421–427. doi: 10.1006/jsre.1995.1185. [DOI] [PubMed] [Google Scholar]
- Vollmar B., Glasz J., Leiderer R., Post S., Menger M. D. Hepatic microcirculatory perfusion failure is a determinant of liver dysfunction in warm ischemia-reperfusion. Am J Pathol. 1994 Dec;145(6):1421–1431. [PMC free article] [PubMed] [Google Scholar]
- Wu C. C., Hwang C. R., Liu T. J., P'eng F. K. Effects and limitations of prolonged intermittent ischaemia for hepatic resection of the cirrhotic liver. Br J Surg. 1996 Jan;83(1):121–124. doi: 10.1002/bjs.1800830139. [DOI] [PubMed] [Google Scholar]
- Yamaoka Y., Morimoto T., Inamoto T., Tanaka A., Honda K., Ikai I., Tanaka K., Ichimiya M., Ueda M., Shimahara Y. Safety of the donor in living-related liver transplantation--an analysis of 100 parental donors. Transplantation. 1995 Jan 27;59(2):224–226. [PubMed] [Google Scholar]


