Abstract
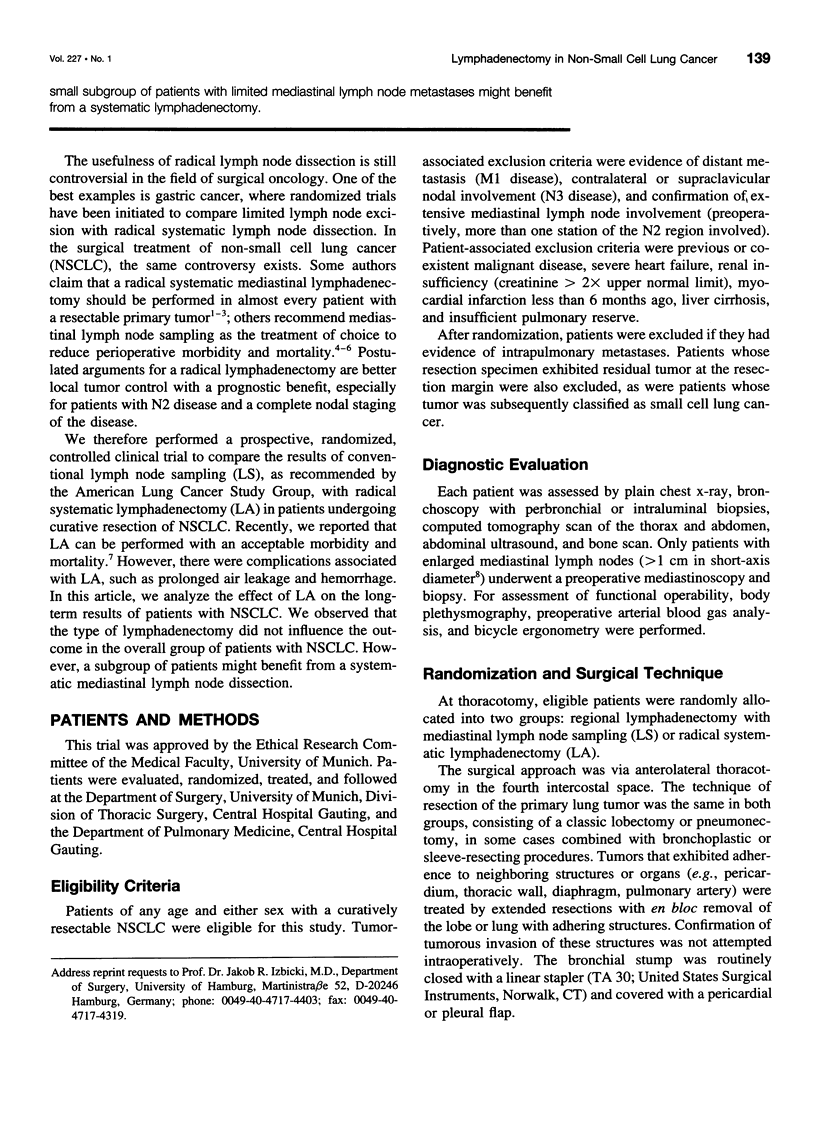
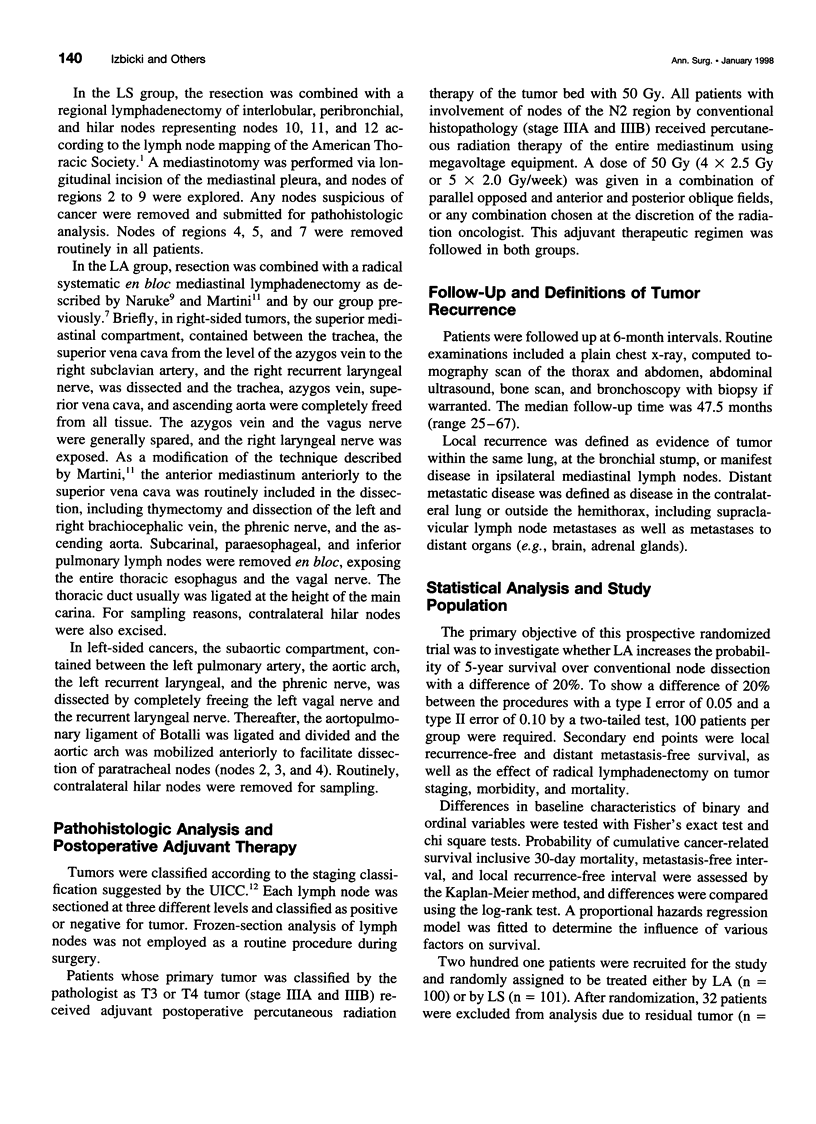
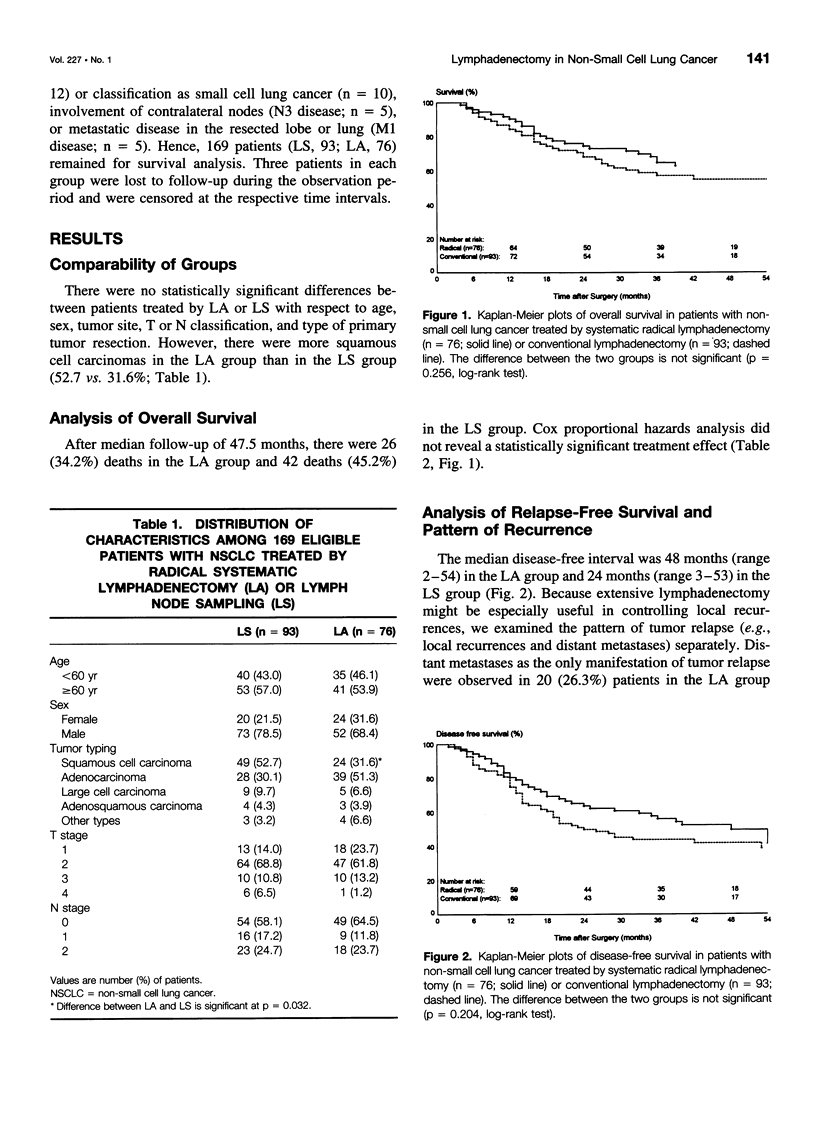
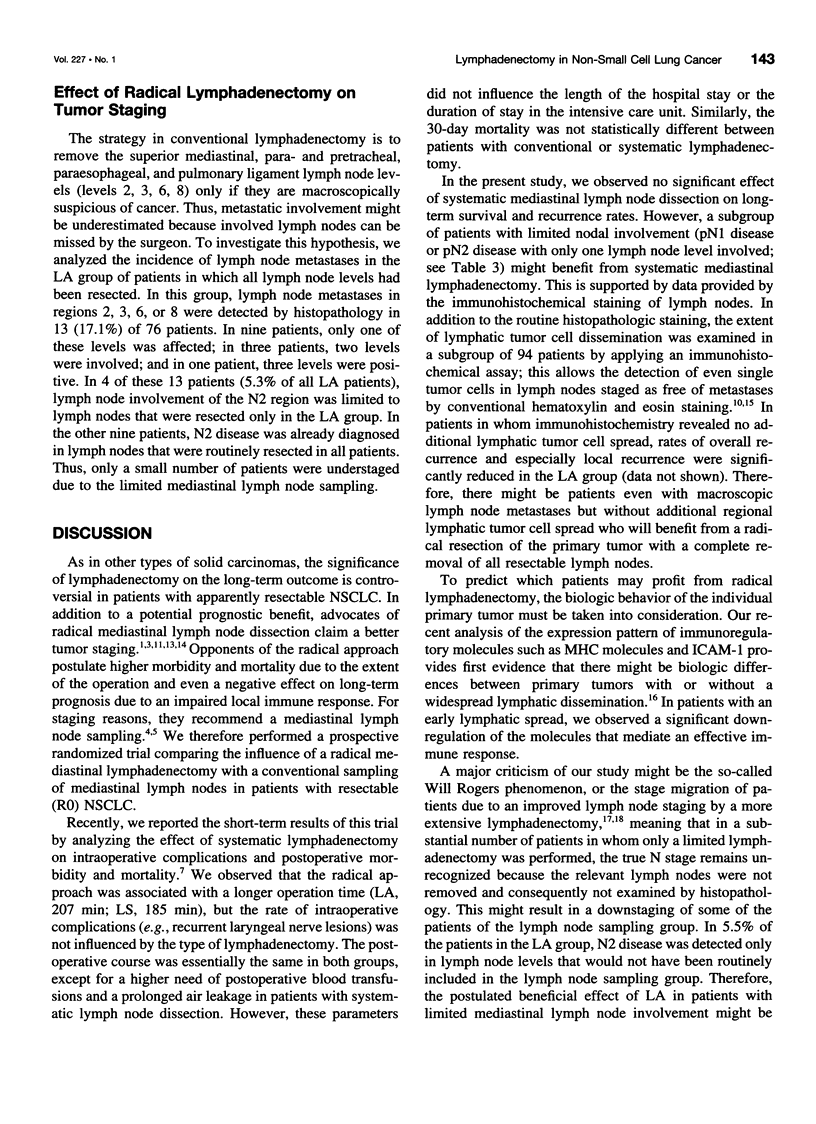
OBJECTIVE: To evaluate the effectiveness of lymphadenectomy in the treatment of non-small cell lung cancer (NSCLC). SUMMARY BACKGROUND DATA: The extent of lymphadenectomy in the treatment of NSCLC is still a matter of controversy. Although some centers perform mediastinal lymph node sampling (LS) with resection of only suspicious lymph nodes, others recommend a radical, systematic mediastinal lymphadenectomy (LA) to improve survival and to achieve a better staging. METHODS: In a controlled, prospective, randomized clinical trial, the effects of LA on recurrence rates and survival were analyzed, comparing LS and LA in 169 patients with operable NSCLC. RESULTS: After a median follow-up of 47 months, LA did not improve survival in the overall group of patients (hazard ratio: 0.78; 95% confidence interval: 0.47-1.24). Although recurrences rates tended to be reduced among patients who underwent LA, these decreases were not statistically significant (hazard ratio: 0.82; 95% confidence interval: 0.54-1.27). However, analysis of subgroups of patients according to histopathologic lymph node staging revealed that LA appears to prolong relapse-free survival (p = 0.037) with a borderline effect on overall survival (p = 0.058) in patients with limited lymph node involvement (pN1 disease or pN2 disease with involvement of only one lymph node level); in patients with pN0 disease, no survival benefit was observed. CONCLUSIONS: Radical systematic mediastinal lymphadenectomy does not influence disease-free or overall survival in patients with NSCLC and without overt lymph node involvement. However, a small subgroup of patients with limited mediastinal lymph node metastases might benefit from a systematic lymphadenectomy.
Full text
PDF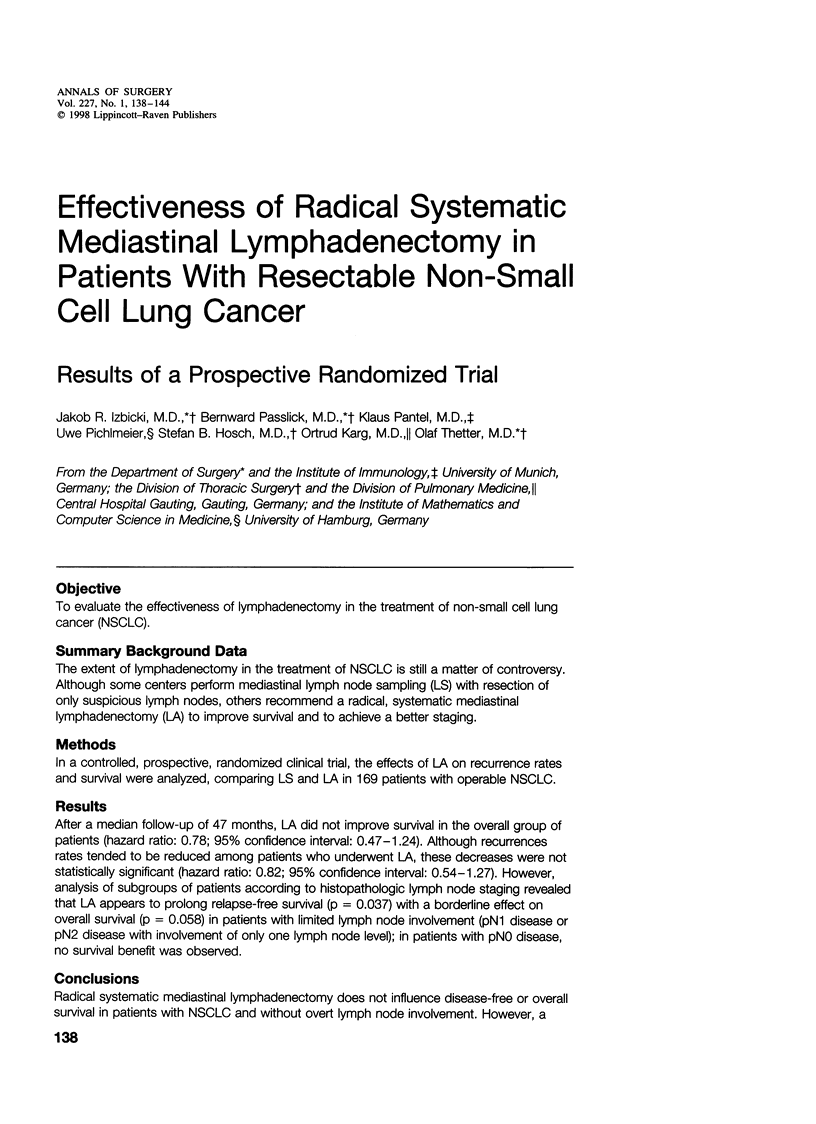

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bunt A. M., Hermans J., Smit V. T., van de Velde C. J., Fleuren G. J., Bruijn J. A. Surgical/pathologic-stage migration confounds comparisons of gastric cancer survival rates between Japan and Western countries. J Clin Oncol. 1995 Jan;13(1):19–25. doi: 10.1200/JCO.1995.13.1.19. [DOI] [PubMed] [Google Scholar]
- Feinstein A. R., Sosin D. M., Wells C. K. The Will Rogers phenomenon. Stage migration and new diagnostic techniques as a source of misleading statistics for survival in cancer. N Engl J Med. 1985 Jun 20;312(25):1604–1608. doi: 10.1056/NEJM198506203122504. [DOI] [PubMed] [Google Scholar]
- Izbicki J. R., Thetter O., Habekost M., Karg O., Passlick B., Kubuschok B., Busch C., Haeussinger K., Knoefel W. T., Pantel K. Radical systematic mediastinal lymphadenectomy in non-small cell lung cancer: a randomized controlled trial. Br J Surg. 1994 Feb;81(2):229–235. doi: 10.1002/bjs.1800810223. [DOI] [PubMed] [Google Scholar]
- Izbicki J. R., Thetter O., Karg O., Kreusser T., Passlick B., Trupka A., Häussinger K., Woeckel W., Kenn R. W., Wilker D. K. Accuracy of computed tomographic scan and surgical assessment for staging of bronchial carcinoma. A prospective study. J Thorac Cardiovasc Surg. 1992 Aug;104(2):413–420. [PubMed] [Google Scholar]
- Martini N., Flehinger B. J. The role of surgery in N2 lung cancer. Surg Clin North Am. 1987 Oct;67(5):1037–1049. doi: 10.1016/s0039-6109(16)44341-0. [DOI] [PubMed] [Google Scholar]
- Martini N., Flehinger B. J., Zaman M. B., Beattie E. J., Jr Results of resection in non-oat cell carcinoma of the lung with mediastinal lymph node metastases. Ann Surg. 1983 Sep;198(3):386–397. doi: 10.1097/00000658-198309000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martini N., Flehinger B. J., Zaman M. B., Bettie E. J., Jr Results of surgical treatment in N2 lung cancer. World J Surg. 1981 Sep;5(5):663–666. doi: 10.1007/BF01657924. [DOI] [PubMed] [Google Scholar]
- Naruke T., Goya T., Tsuchiya R., Suemasu K. Prognosis and survival in resected lung carcinoma based on the new international staging system. J Thorac Cardiovasc Surg. 1988 Sep;96(3):440–447. [PubMed] [Google Scholar]
- Naruke T., Goya T., Tsuchiya R., Suemasu K. The importance of surgery to non-small cell carcinoma of lung with mediastinal lymph node metastasis. Ann Thorac Surg. 1988 Dec;46(6):603–610. doi: 10.1016/s0003-4975(10)64717-0. [DOI] [PubMed] [Google Scholar]
- Naruke T., Suemasu K., Ishikawa S. Surgical treatment for lung cancer with metastasis to mediastinal lymph nodes. J Thorac Cardiovasc Surg. 1976 Feb;71(2):279–285. [PubMed] [Google Scholar]
- Passlick B., Izbicki J. R., Kubuschok B., Thetter O., Pantel K. Detection of disseminated lung cancer cells in lymph nodes: impact on staging and prognosis. Ann Thorac Surg. 1996 Jan;61(1):177–183. doi: 10.1016/0003-4975(95)01012-2. [DOI] [PubMed] [Google Scholar]
- Passlick B., Pantel K., Kubuschok B., Angstwurm M., Neher A., Thetter O., Schweiberer L., Izbicki J. R. Expression of MHC molecules and ICAM-1 on non-small cell lung carcinomas: association with early lymphatic spread of tumour cells. Eur J Cancer. 1996 Jan;32A(1):141–145. doi: 10.1016/0959-8049(95)00551-x. [DOI] [PubMed] [Google Scholar]
- Sørensen J. B., Badsberg J. H. Prognostic factors in resected stages I and II adenocarcinoma of the lung. A multivariate regression analysis of 137 consecutive patients. J Thorac Cardiovasc Surg. 1990 Feb;99(2):218–226. [PubMed] [Google Scholar]
- Thomas P., Rubinstein L. Cancer recurrence after resection: T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg. 1990 Feb;49(2):242–247. doi: 10.1016/0003-4975(90)90145-v. [DOI] [PubMed] [Google Scholar]


