Abstract
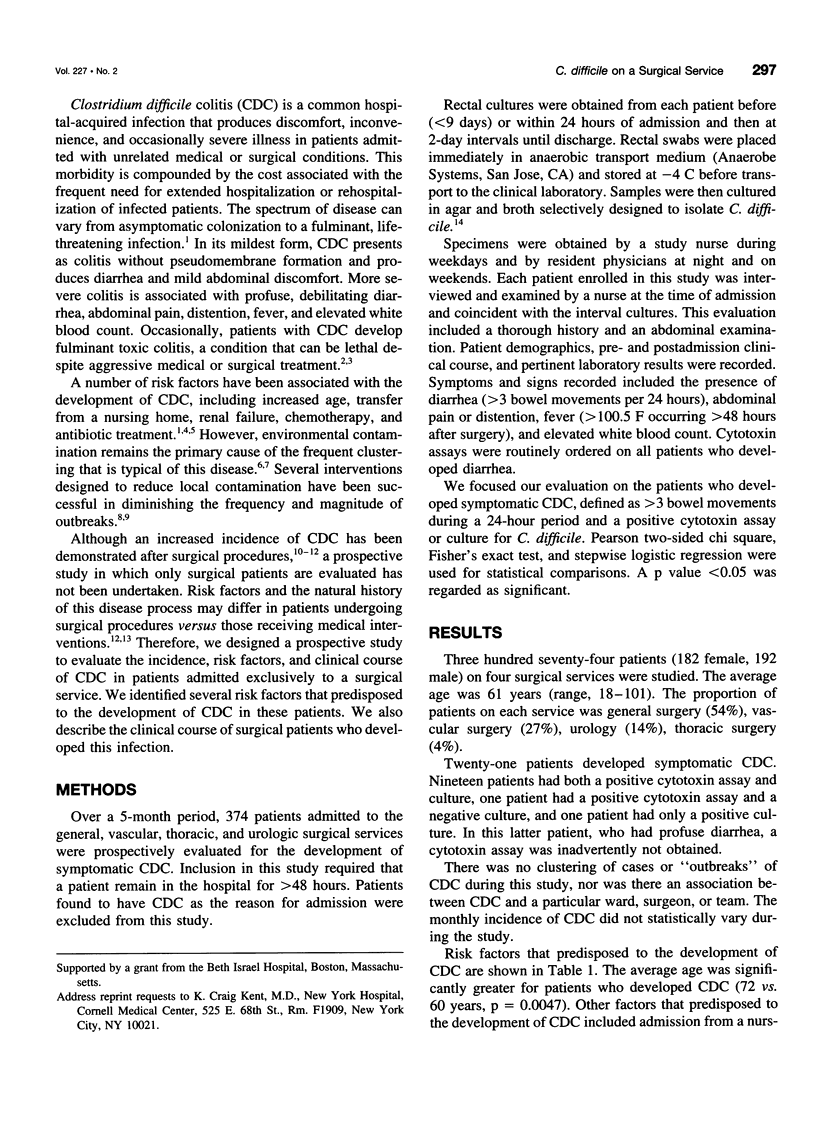
OBJECTIVE: To evaluate the epidemiology of Clostridium difficile colitis (CDC) in a subset of patients admitted specifically to a surgical service. SUMMARY BACKGROUND DATA: CDC is an increasingly prevalent nosocomial infection that can prolong hospitalization and adversely affect patient outcome. Although this disease has been investigated extensively in patients admitted to medical services, the incidence and risk factors for the development of this disease in patients admitted to a surgical service have not been studied. METHODS: Over a 5-month period, 374 patients admitted to the general, vascular, thoracic, and urologic surgery services were monitored for the development of symptomatic CDC (defined as >3 bowel movements per 24 hours and a positive cytotoxin assay or culture). RESULTS: Twenty-one patients developed CDC (incidence, 5.6%). Factors that independently predisposed to infection included admission from a skilled care facility, use of the antibiotic cefoxitin, and an operative procedure for bowel obstruction. Other factors associated with CDC included colectomy, treatment with any antibiotic, nasogastric tube suction, advanced age, and prior antibiotic treatment. Abdominal pain and fever were also more common in patients with CDC. Morbidity included prolonged hospitalization in all patients and urgent colectomy in one. CONCLUSIONS: CDC frequently affects surgical patients, producing morbidity ranging from mild diarrhea to life-threatening illness. A variety of factors, many of which are associated with intestinal stasis, predispose to the development of CDC.
Full text
PDF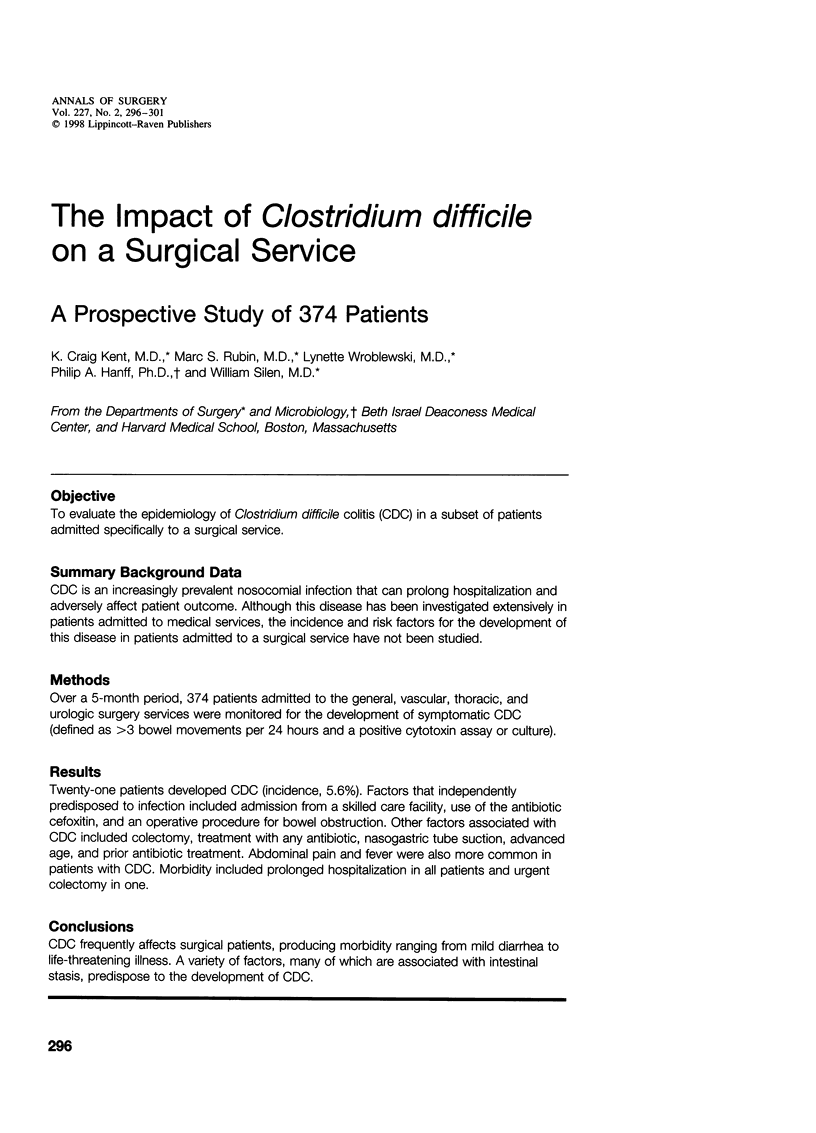


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brooks S. E., Veal R. O., Kramer M., Dore L., Schupf N., Adachi M. Reduction in the incidence of Clostridium difficile-associated diarrhea in an acute care hospital and a skilled nursing facility following replacement of electronic thermometers with single-use disposables. Infect Control Hosp Epidemiol. 1992 Feb;13(2):98–103. doi: 10.1086/646480. [DOI] [PubMed] [Google Scholar]
- Brown E., Talbot G. H., Axelrod P., Provencher M., Hoegg C. Risk factors for Clostridium difficile toxin-associated diarrhea. Infect Control Hosp Epidemiol. 1990 Jun;11(6):283–290. doi: 10.1086/646173. [DOI] [PubMed] [Google Scholar]
- Fekety R., Kim K. H., Brown D., Batts D. H., Cudmore M., Silva J., Jr Epidemiology of antibiotic-associated colitis; isolation of Clostridium difficile from the hospital environment. Am J Med. 1981 Apr;70(4):906–908. doi: 10.1016/0002-9343(81)90553-2. [DOI] [PubMed] [Google Scholar]
- Fekety R., Shah A. B. Diagnosis and treatment of Clostridium difficile colitis. JAMA. 1993 Jan 6;269(1):71–75. [PubMed] [Google Scholar]
- Gerding D. N., Olson M. M., Peterson L. R., Teasley D. G., Gebhard R. L., Schwartz M. L., Lee J. T., Jr Clostridium difficile-associated diarrhea and colitis in adults. A prospective case-controlled epidemiologic study. Arch Intern Med. 1986 Jan;146(1):95–100. [PubMed] [Google Scholar]
- Hanff P. A., Zaleznik D. F., Kent K. C., Rubin M. S., Kelly E., Cote J., Rosol-Donoghue J. Use of heat shock for culturing Clostridium difficile from rectal swabs. Clin Infect Dis. 1993 Jun;16 (Suppl 4):S245–S247. doi: 10.1093/clinids/16.supplement_4.s245. [DOI] [PubMed] [Google Scholar]
- Johnson S., Gerding D. N., Olson M. M., Weiler M. D., Hughes R. A., Clabots C. R., Peterson L. R. Prospective, controlled study of vinyl glove use to interrupt Clostridium difficile nosocomial transmission. Am J Med. 1990 Feb;88(2):137–140. doi: 10.1016/0002-9343(90)90462-m. [DOI] [PubMed] [Google Scholar]
- Kappas A., Shinagawa N., Arabi Y., Thompson H., Burdon D., Dimock F., George R. H., Alexander-Williams J., Keighley M. R. Diagnosis of pseudomembranous colitis. Br Med J. 1978 Mar 18;1(6114):675–678. doi: 10.1136/bmj.1.6114.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keighley M. R., Burdon D. W., Alexander-Williams J., Shinagawa N., Arabi Y., Thompson H., Youngs D., Bentley S., George R. H. Diarrhoea and pseudomembranous colitis after gastrointestinal operations. A prospective study. Lancet. 1978 Dec 2;2(8101):1165–1167. doi: 10.1016/s0140-6736(78)92151-7. [DOI] [PubMed] [Google Scholar]
- Kelly C. P., Pothoulakis C., LaMont J. T. Clostridium difficile colitis. N Engl J Med. 1994 Jan 27;330(4):257–262. doi: 10.1056/NEJM199401273300406. [DOI] [PubMed] [Google Scholar]
- McFarland L. V., Mulligan M. E., Kwok R. Y., Stamm W. E. Nosocomial acquisition of Clostridium difficile infection. N Engl J Med. 1989 Jan 26;320(4):204–210. doi: 10.1056/NEJM198901263200402. [DOI] [PubMed] [Google Scholar]
- McFarland L. V., Stamm W. E. Review of Clostridium difficile-associated diseases. Am J Infect Control. 1986 Jun;14(3):99–109. doi: 10.1016/0196-6553(86)90018-0. [DOI] [PubMed] [Google Scholar]
- Mulligan M. E., Citron D., Gabay E., Kirby B. D., George W. L., Finegold S. M. Alterations in human fecal flora, including ingrowth of Clostridium difficile, related to cefoxitin therapy. Antimicrob Agents Chemother. 1984 Sep;26(3):343–346. doi: 10.1128/aac.26.3.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolan N. P., Kelly C. P., Humphreys J. F., Cooney C., O'Connor R., Walsh T. N., Weir D. G., O'Briain D. S. An epidemic of pseudomembranous colitis: importance of person to person spread. Gut. 1987 Nov;28(11):1467–1473. doi: 10.1136/gut.28.11.1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce P. F., Jr, Wilson R., Silva J., Jr, Garagusi V. F., Rifkin G. D., Fekety R., Nunez-Montiel O., Dowell V. R., Jr, Hughes J. M. Antibiotic-associated pseudomembranous colitis: an epidemiologic investigation of a cluster of cases. J Infect Dis. 1982 Feb;145(2):269–274. doi: 10.1093/infdis/145.2.269. [DOI] [PubMed] [Google Scholar]
- Privitera G., Scarpellini P., Ortisi G., Nicastro G., Nicolin R., de Lalla F. Prospective study of Clostridium difficile intestinal colonization and disease following single-dose antibiotic prophylaxis in surgery. Antimicrob Agents Chemother. 1991 Jan;35(1):208–210. doi: 10.1128/aac.35.1.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin M. S., Bodenstein L. E., Kent K. C. Severe Clostridium difficile colitis. Dis Colon Rectum. 1995 Apr;38(4):350–354. doi: 10.1007/BF02054220. [DOI] [PubMed] [Google Scholar]
- Samore M. H., DeGirolami P. C., Tlucko A., Lichtenberg D. A., Melvin Z. A., Karchmer A. W. Clostridium difficile colonization and diarrhea at a tertiary care hospital. Clin Infect Dis. 1994 Feb;18(2):181–187. doi: 10.1093/clinids/18.2.181. [DOI] [PubMed] [Google Scholar]
- Silva J., Fekety R., Werk C., Ebright J., Cudmore M., Batts D., Syrjamaki C., Lukens J. Inciting and etiologic agents of colitis. Rev Infect Dis. 1984 Mar-Apr;6 (Suppl 1):S214–S221. doi: 10.1093/clinids/6.supplement_1.s214. [DOI] [PubMed] [Google Scholar]
- Triadafilopoulos G., Hallstone A. E. Acute abdomen as the first presentation of pseudomembranous colitis. Gastroenterology. 1991 Sep;101(3):685–691. doi: 10.1016/0016-5085(91)90526-q. [DOI] [PubMed] [Google Scholar]
- Trnka Y. M., Lamont J. T. Clostridium difficile colitis. Adv Intern Med. 1984;29:85–107. [PubMed] [Google Scholar]


