Abstract
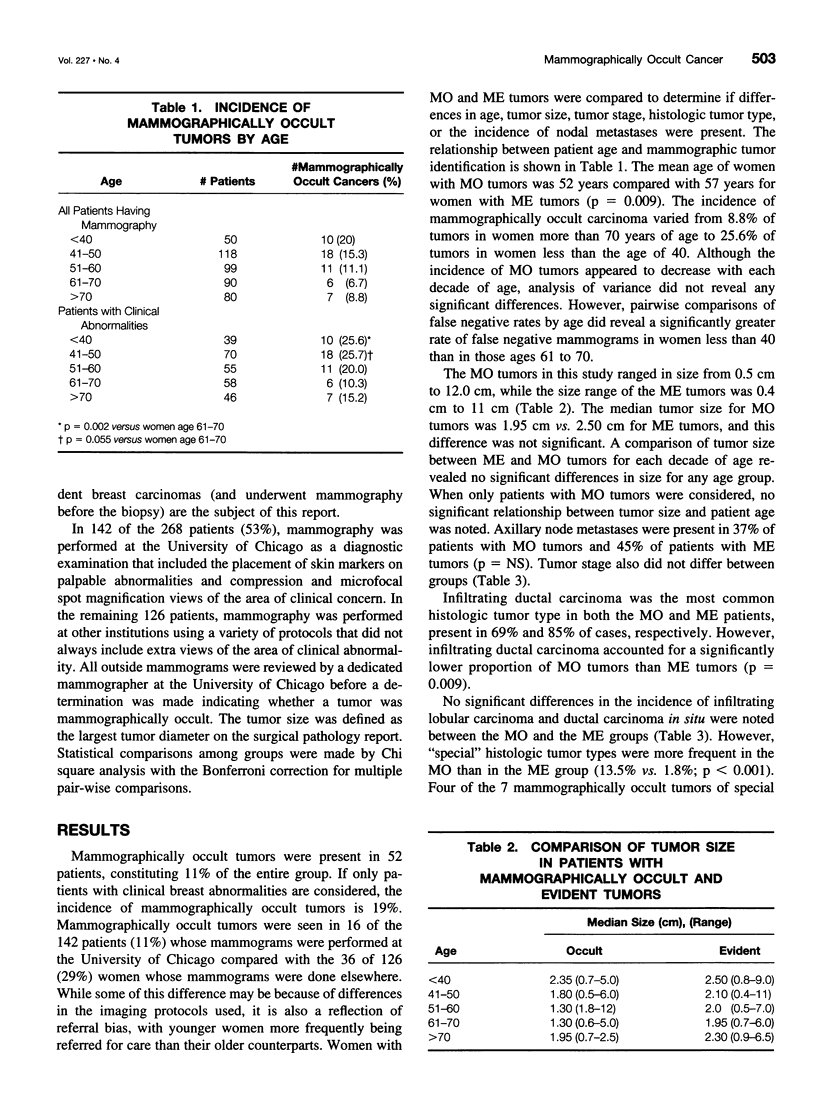
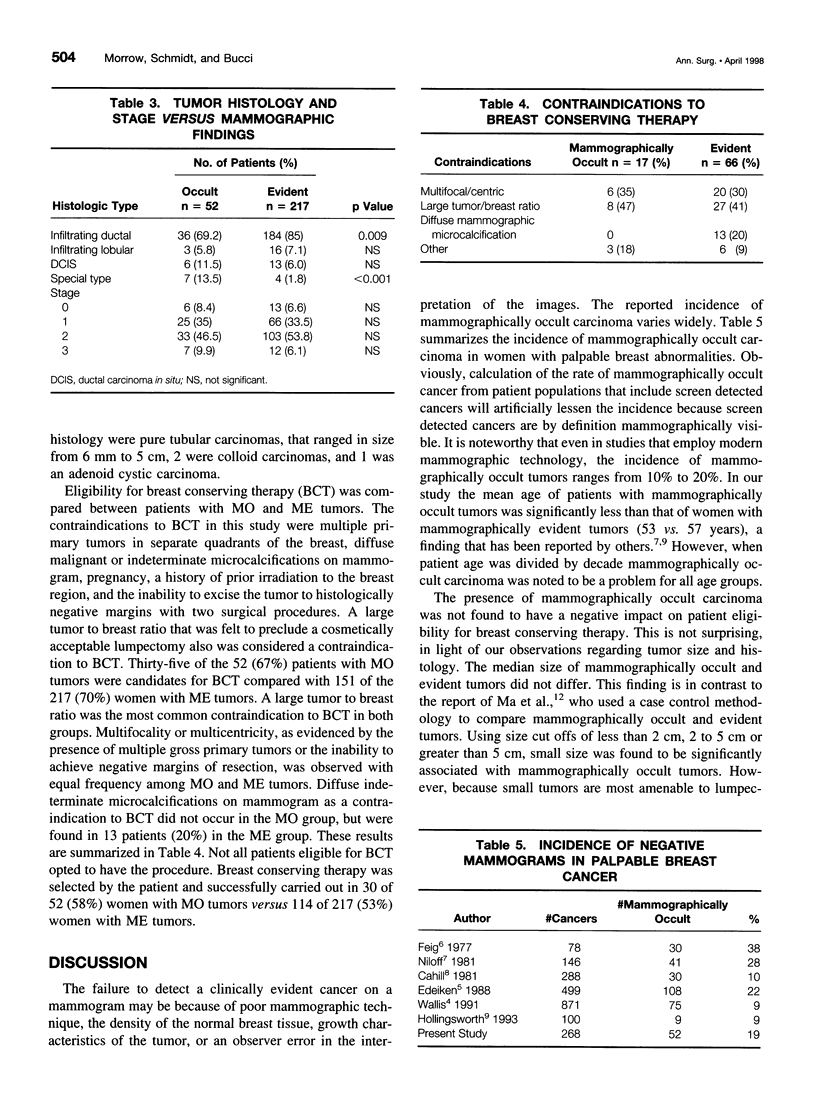
OBJECTIVE: Preoperative mammography is an essential part of the evaluation of patient eligibility for breast conserving therapy. SUMMARY BACKGROUND DATA: It is uncertain whether factors that contribute to the nonvisualization of carcinoma on mammograms are indications for mastectomy. The purpose of this study was to determine if the failure to identify clinically evident carcinoma on a mammogram is a contraindication to breast conserving therapy. METHODS: An analysis of 268 women with 269 clinically evident carcinomas who were treated from June 1988 to September 1993 was performed. Contraindications to breast preservation included multicentric tumors, diffuse indeterminate microcalcifications, pregnancy, prior irradiation to the breast region, the inability to achieve negative margins after two surgical procedures, and a large tumor to breast ratio. RESULTS: Mammographically occult tumors (MO) were present in 52 patients (19%). The mean age of patients with MO tumors was 52 versus 57 for mammographically evident (ME) tumors (p = 0.009), but the incidence by decade did not vary. Special histologic tumor types were more frequent among MO than ME tumors (13.5% vs. 1.8%, p < 0.001). Tumor size, the incidence of axillary node metastases, and stage did not vary. An equal proportion of patients with MO and ME tumors were candidates for breast preservation (67% vs. 70%), and a large tumor to breast ratio was the most common contraindication in both groups. CONCLUSIONS: Even with modem mammographic technology, MO tumors remain a significant problem. This study did not demonstrate an association between MO tumors and factors such as size, unfavorable histology, or multicentricity which would preclude the use of breast conserving therapy. These results support the treatment of MO tumors with breast conserving surgery after a detailed clinical evaluation.
Full text
PDF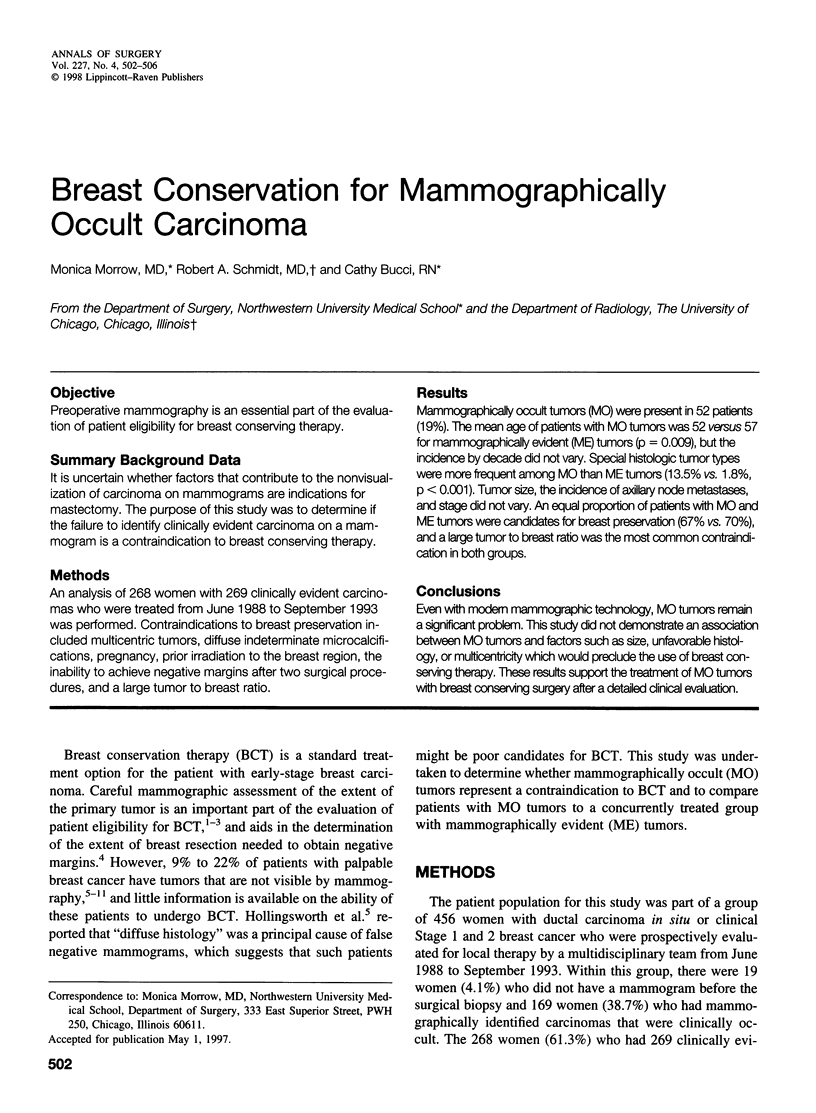


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cahill C. J., Boulter P. S., Gibbs N. M., Price J. L. Features of mammorgraphically negative breast tumours. Br J Surg. 1981 Dec;68(12):882–884. doi: 10.1002/bjs.1800681215. [DOI] [PubMed] [Google Scholar]
- Edeiken S. Mammography and palpable cancer of the breast. Cancer. 1988 Jan 15;61(2):263–265. doi: 10.1002/1097-0142(19880115)61:2<263::aid-cncr2820610211>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Feig S. A., Shaber G. S., Patchefsky A., Schwartz G. F., Edeiken J., Libshitz H. I., Nerlinger R., Curley R. F., Wallace J. D. Analysis of clinically occult and mammographically occult breast tumors. AJR Am J Roentgenol. 1977 Mar;128(3):403–408. doi: 10.2214/ajr.128.3.403. [DOI] [PubMed] [Google Scholar]
- Healey E. A., Osteen R. T., Schnitt S. J., Gelman R., Stomper P. C., Connolly J. L., Harris J. R. Can the clinical and mammographic findings at presentation predict the presence of an extensive intraductal component in early stage breast cancer? Int J Radiat Oncol Biol Phys. 1989 Dec;17(6):1217–1221. doi: 10.1016/0360-3016(89)90529-4. [DOI] [PubMed] [Google Scholar]
- Hilleren D. J., Andersson I. T., Lindholm K., Linnell F. S. Invasive lobular carcinoma: mammographic findings in a 10-year experience. Radiology. 1991 Jan;178(1):149–154. doi: 10.1148/radiology.178.1.1984294. [DOI] [PubMed] [Google Scholar]
- Holland R., Connolly J. L., Gelman R., Mravunac M., Hendriks J. H., Verbeek A. L., Schnitt S. J., Silver B., Boyages J., Harris J. R. The presence of an extensive intraductal component following a limited excision correlates with prominent residual disease in the remainder of the breast. J Clin Oncol. 1990 Jan;8(1):113–118. doi: 10.1200/JCO.1990.8.1.113. [DOI] [PubMed] [Google Scholar]
- Hollingsworth A. B., Taylor L. D., Rhodes D. C. Establishing a histologic basis for false-negative mammograms. Am J Surg. 1993 Dec;166(6):643–648. doi: 10.1016/s0002-9610(05)80671-3. [DOI] [PubMed] [Google Scholar]
- Kearney T. J., Morrow M. Effect of reexcision on the success of breast-conserving surgery. Ann Surg Oncol. 1995 Jul;2(4):303–307. doi: 10.1007/BF02307061. [DOI] [PubMed] [Google Scholar]
- Ma L., Fishell E., Wright B., Hanna W., Allan S., Boyd N. F. Case-control study of factors associated with failure to detect breast cancer by mammography. J Natl Cancer Inst. 1992 May 20;84(10):781–785. doi: 10.1093/jnci/84.10.781. [DOI] [PubMed] [Google Scholar]
- Morrow M., Schmidt R., Hassett C. Patient selection for breast conservation therapy with magnification mammography. Surgery. 1995 Oct;118(4):621–626. doi: 10.1016/s0039-6060(05)80027-3. [DOI] [PubMed] [Google Scholar]
- Niloff P. H., Sheiner N. M. False-negative mammograms in patients with breast cancer. Can J Surg. 1981 Jan;24(1):50–52. [PubMed] [Google Scholar]
- Samuels J. R., Haffty B. G., Lee C. H., Fischer D. B. Breast conservation therapy in patients with mammographically undetected breast cancer. Radiology. 1992 Nov;185(2):425–427. doi: 10.1148/radiology.185.2.1329142. [DOI] [PubMed] [Google Scholar]
- Sickles E. A. The subtle and atypical mammographic features of invasive lobular carcinoma. Radiology. 1991 Jan;178(1):25–26. doi: 10.1148/radiology.178.1.1984313. [DOI] [PubMed] [Google Scholar]
- Wallis M. G., Walsh M. T., Lee J. R. A review of false negative mammography in a symptomatic population. Clin Radiol. 1991 Jul;44(1):13–15. doi: 10.1016/s0009-9260(05)80218-1. [DOI] [PubMed] [Google Scholar]
- Winchester D. P., Cox J. D. Standards for breast-conservation treatment. CA Cancer J Clin. 1992 May-Jun;42(3):134–162. doi: 10.3322/canjclin.42.3.134. [DOI] [PubMed] [Google Scholar]
- Young J. O., Sadowsky N. L., Young J. W., Herman L. Mammography of women with suspicious breast lumps. Arch Surg. 1986 Jul;121(7):807–809. doi: 10.1001/archsurg.1986.01400070073015. [DOI] [PubMed] [Google Scholar]


