Abstract
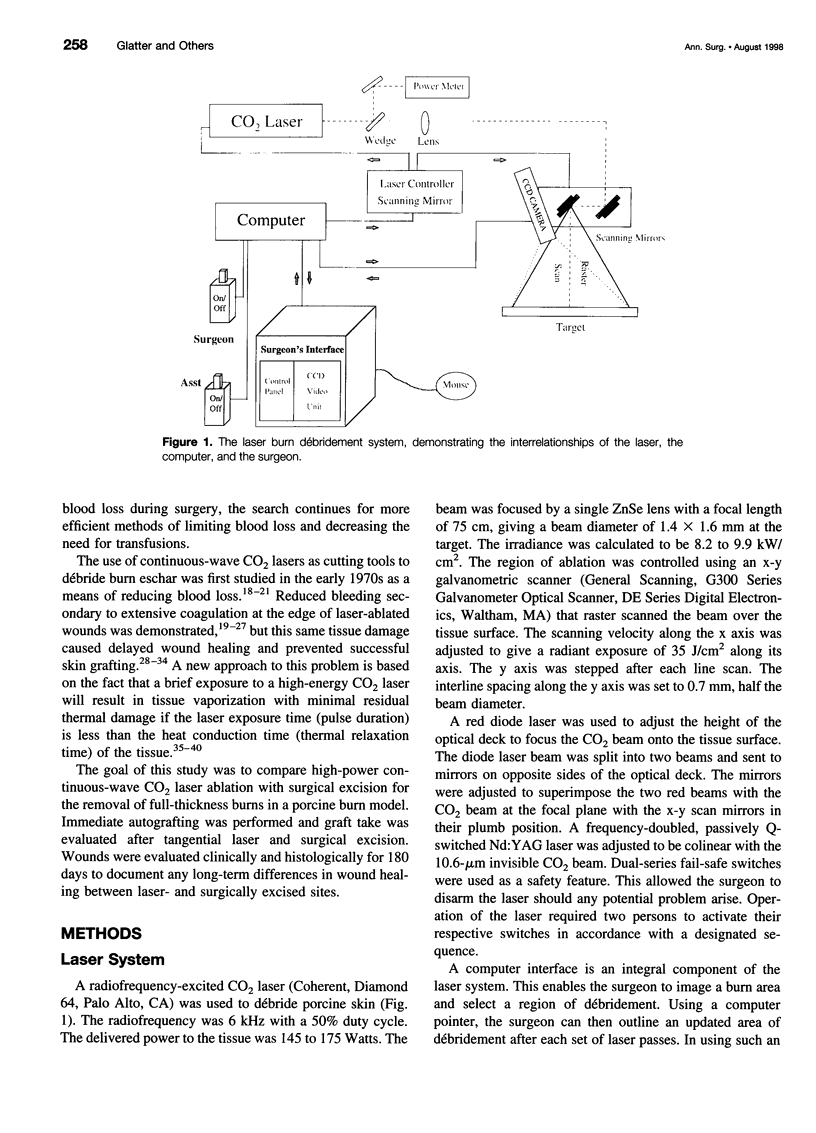
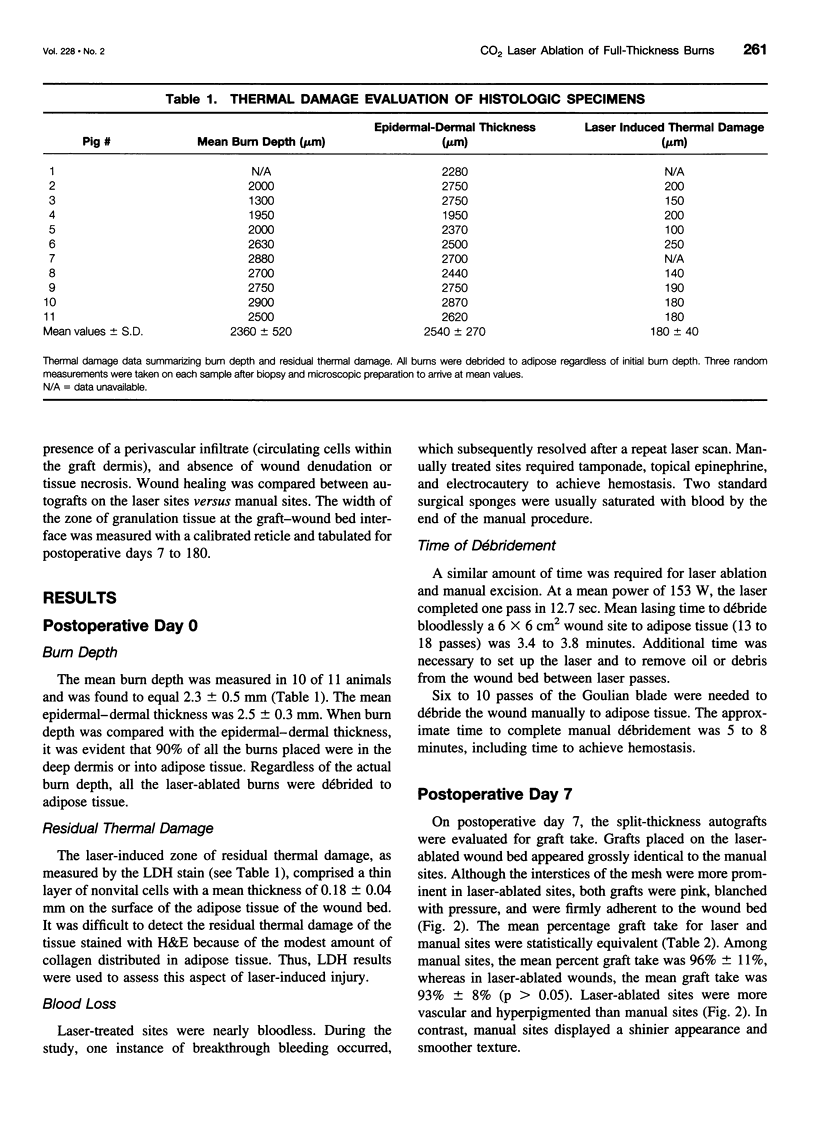
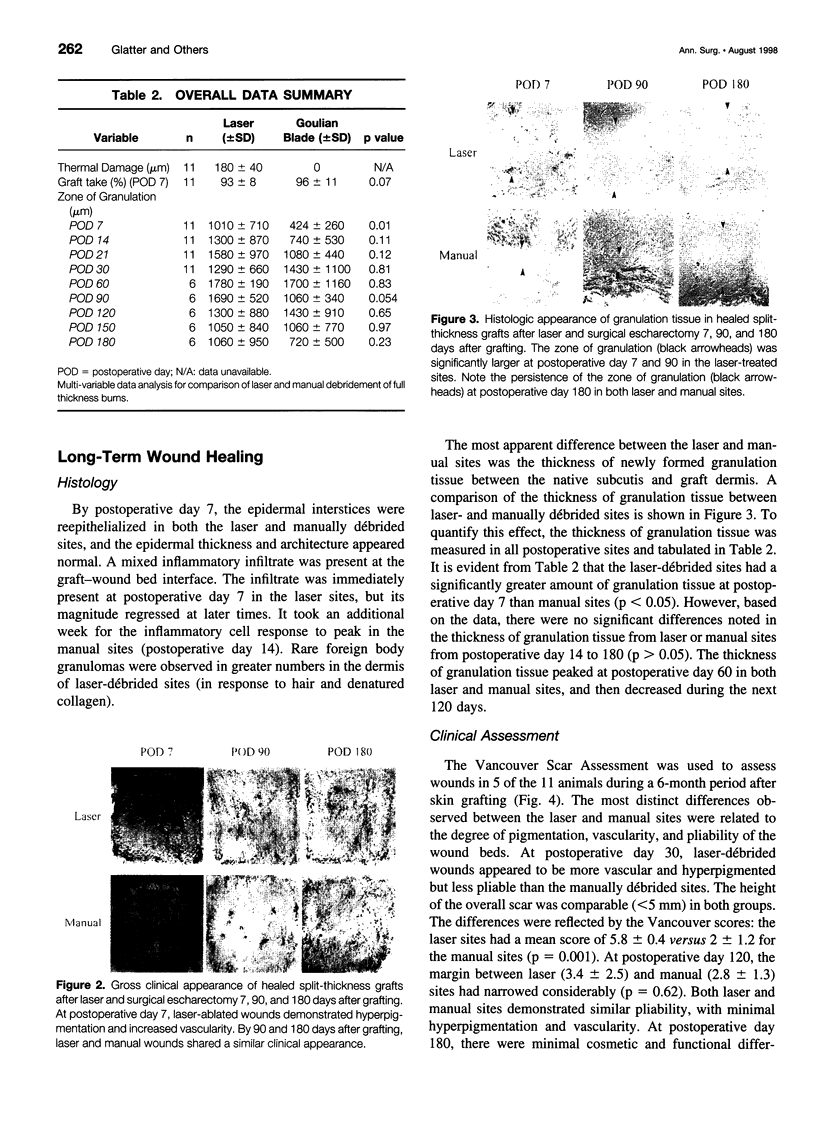
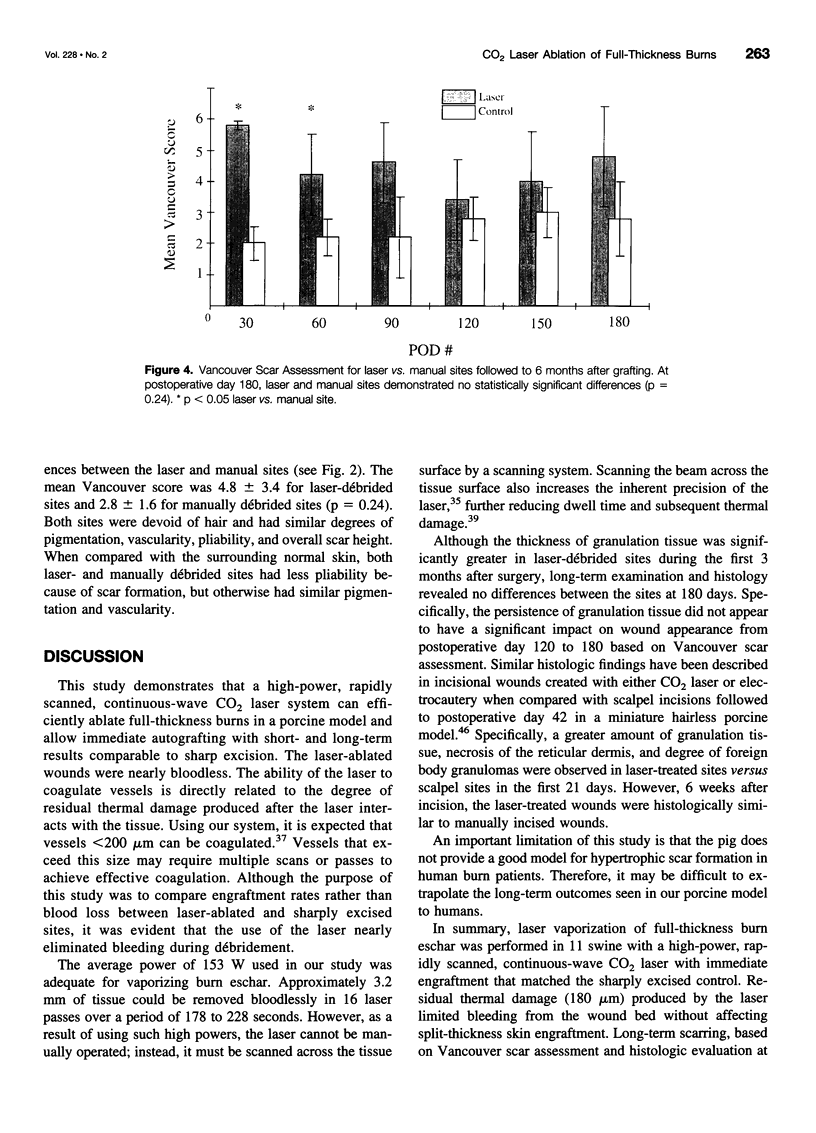
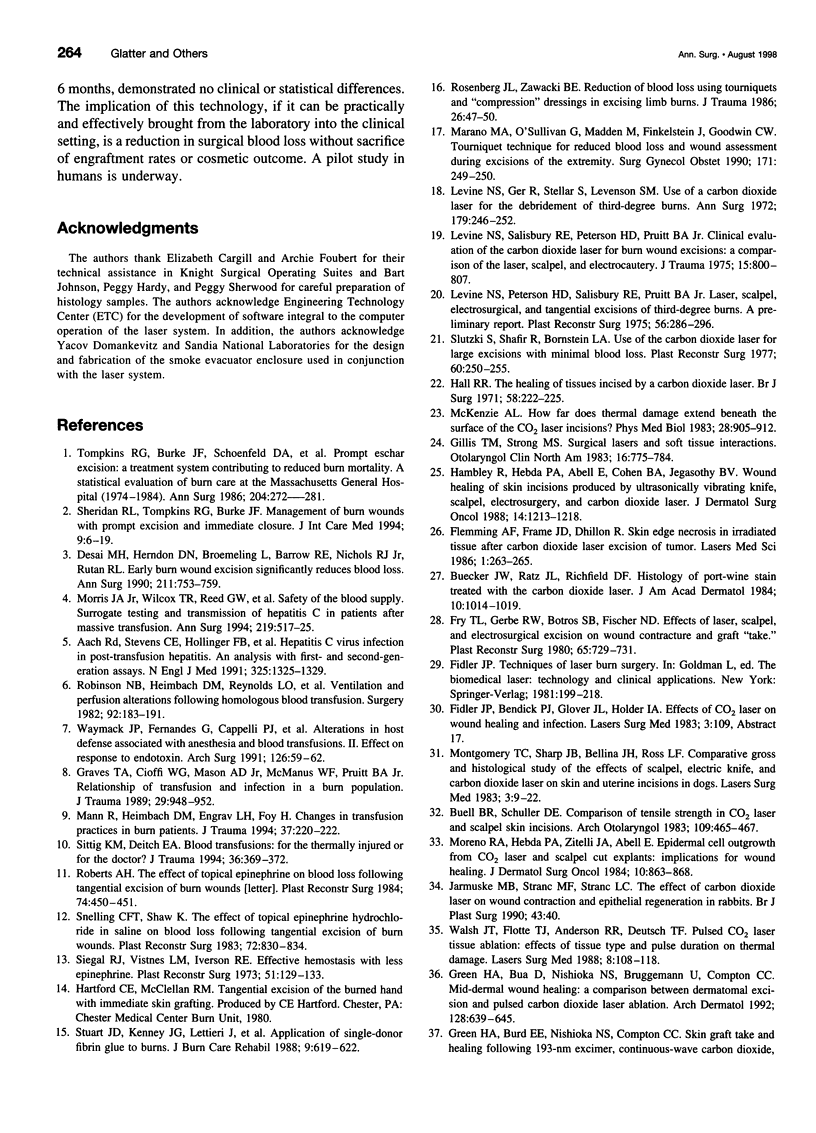
OBJECTIVE: To compare the long-term clinical and histologic outcome of immediate autografting of full-thickness burn wounds ablated with a high-power continuous-wave CO2 laser to sharply débrided wounds in a porcine model. SUMMARY BACKGROUND DATA: Continuous-wave CO2 lasers have performed poorly as tools for burn excision because the large amount of thermal damage to viable subeschar tissues precluded successful autografting. However, a new technique, in which a high-power laser is rapidly scanned over the eschar, results in eschar vaporization without significant damage to underlying viable tissues, allowing successful immediate autografting. METHODS: Full-thickness paravertebral burn wounds measuring 36 cm2 were created on 11 farm swine. Wounds were ablated to adipose tissue 48 hours later using either a surgical blade or a 150-Watt continuous-wave CO2 laser deflected by an x-y galvanometric scanner that translated the beam over the tissue surface, removing 200 microm of tissue per scan. Both sites were immediately autografted and serially evaluated clinically and histologically for 180 days. RESULTS: The laser-treated sites were nearly bloodless. The mean residual thermal damage was 0.18+/-0.05 mm. The mean graft take was 96+/-11% in manual sites and 93+/-8% in laser sites. On postoperative day 7, the thickness of granulation tissue at the graft-wound bed interface was greater in laser-debrided sites. By postoperative day 180, the manual and laser sites were histologically identical. Vancouver scar assessment revealed no differences in scarring at postoperative day 180. CONCLUSIONS: Long-term scarring, based on Vancouver scar assessments and histologic evaluation, was equivalent at 6 months in laser-ablated and sharply excised sites. Should this technology become practical, the potential clinical implications include a reduction in surgical blood loss without sacrifice of immediate engraftment rates or long-term outcome.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aach R. D., Stevens C. E., Hollinger F. B., Mosley J. W., Peterson D. A., Taylor P. E., Johnson R. G., Barbosa L. H., Nemo G. J. Hepatitis C virus infection in post-transfusion hepatitis. An analysis with first- and second-generation assays. N Engl J Med. 1991 Nov 7;325(19):1325–1329. doi: 10.1056/NEJM199111073251901. [DOI] [PubMed] [Google Scholar]
- Buecker J. W., Ratz J. L., Richfield D. F. Histology of port-wine stain treated with carbon dioxide laser. A preliminary report. J Am Acad Dermatol. 1984 Jun;10(6):1014–1019. doi: 10.1016/s0190-9622(84)80326-6. [DOI] [PubMed] [Google Scholar]
- Buell B. R., Schuller D. E. Comparison of tensile strength in CO2 laser and scalpel skin incisions. Arch Otolaryngol. 1983 Jul;109(7):465–467. doi: 10.1001/archotol.1983.00800210041009. [DOI] [PubMed] [Google Scholar]
- Desai M. H., Herndon D. N., Broemeling L., Barrow R. E., Nichols R. J., Jr, Rutan R. L. Early burn wound excision significantly reduces blood loss. Ann Surg. 1990 Jun;211(6):753–762. doi: 10.1097/00000658-199006000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domankevitz Y., Nishioka N. S. Effects of a rapidly scanned carbon dioxide laser on porcine dermis. J Burn Care Rehabil. 1997 May-Jun;18(3):206–209. doi: 10.1097/00004630-199705000-00005. [DOI] [PubMed] [Google Scholar]
- Fry T. L., Gerbe R. W., Botros S. B., Fischer N. D. Effects of laser, scalpel, and electrosurgical excision on wound contracture and graft "take". Plast Reconstr Surg. 1980 Jun;65(6):729–731. doi: 10.1097/00006534-198006000-00002. [DOI] [PubMed] [Google Scholar]
- Gillis T. M., Strong M. S. Surgical lasers and soft tissue interactions. Otolaryngol Clin North Am. 1983 Nov;16(4):775–784. [PubMed] [Google Scholar]
- Graves T. A., Cioffi W. G., Mason A. D., Jr, McManus W. F., Pruitt B. A., Jr Relationship of transfusion and infection in a burn population. J Trauma. 1989 Jul;29(7):948–954. doi: 10.1097/00005373-198907000-00007. [DOI] [PubMed] [Google Scholar]
- Green H. A., Burd E. E., Nishioka N. S., Compton C. C. Skin graft take and healing following 193-nm excimer, continuous-wave carbon dioxide (CO2), pulsed CO2, or pulsed holmium: YAG laser ablation of the graft bed. Arch Dermatol. 1993 Aug;129(8):979–988. [PubMed] [Google Scholar]
- Green H. A., Burd E., Nishioka N. S., Brüggemann U., Compton C. C. Middermal wound healing. A comparison between dermatomal excision and pulsed carbon dioxide laser ablation. Arch Dermatol. 1992 May;128(5):639–645. doi: 10.1001/archderm.128.5.639. [DOI] [PubMed] [Google Scholar]
- Hall R. R. The healing of tissues incised by a carbon-dioxide laser. Br J Surg. 1971 Mar;58(3):222–225. doi: 10.1002/bjs.1800580316. [DOI] [PubMed] [Google Scholar]
- Hambley R., Hebda P. A., Abell E., Cohen B. A., Jegasothy B. V. Wound healing of skin incisions produced by ultrasonically vibrating knife, scalpel, electrosurgery, and carbon dioxide laser. J Dermatol Surg Oncol. 1988 Nov;14(11):1213–1217. doi: 10.1111/j.1524-4725.1988.tb03478.x. [DOI] [PubMed] [Google Scholar]
- Hebda P. A., Klingbeil C. K., Abraham J. A., Fiddes J. C. Basic fibroblast growth factor stimulation of epidermal wound healing in pigs. J Invest Dermatol. 1990 Dec;95(6):626–631. doi: 10.1111/1523-1747.ep12513528. [DOI] [PubMed] [Google Scholar]
- Jarmuske M. B., Stranc M. F., Stranc L. C. The effect of carbon dioxide laser on wound contraction and epithelial regeneration in rabbits. Br J Plast Surg. 1990 Jan;43(1):40–46. doi: 10.1016/0007-1226(90)90043-y. [DOI] [PubMed] [Google Scholar]
- Levine N. S., Peterson H. D., Salisbury R. E., Pruitt B. A., Jr Laser, scalpel, electrosurgical, and tangential excisions of third degree burns. A preliminary report. Plast Reconstr Surg. 1975 Sep;56(3):286–296. doi: 10.1097/00006534-197509000-00006. [DOI] [PubMed] [Google Scholar]
- Levine N. S., Salisbury R. E., Peterson H. D., Pruitt B. A., Jr Clinical evaluation of the carbon dioxide laser for burn wound excisions: a comparison of the laser, scalpel, and electrocautery. J Trauma. 1975 Sep;15(9):800–807. doi: 10.1097/00005373-197509000-00008. [DOI] [PubMed] [Google Scholar]
- Levine N., Ger R., Stellar S., Levenson S. M. Use of a carbon dioxide laser for the debridement of third degree burns. Ann Surg. 1974 Feb;179(2):246–252. doi: 10.1097/00000658-197402000-00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MONTAGNA W., YUN J. S. THE SKIN OF THE DOMESTIC PIG. J Invest Dermatol. 1964 Jul;42:11–21. [PubMed] [Google Scholar]
- Mann R., Heimbach D. M., Engrav L. H., Foy H. Changes in transfusion practices in burn patients. J Trauma. 1994 Aug;37(2):220–222. doi: 10.1097/00005373-199408000-00012. [DOI] [PubMed] [Google Scholar]
- Marano M. A., O'Sullivan G., Madden M., Finkelstein J., Goodwin C. W. Tourniquet technique for reduced blood loss and wound assessment during excisions of burn wounds of the extremity. Surg Gynecol Obstet. 1990 Sep;171(3):249–250. [PubMed] [Google Scholar]
- McKenzie A. L. How far does thermal damage extend beneath the surface of CO2 laser incisions? Phys Med Biol. 1983 Aug;28(8):905–912. doi: 10.1088/0031-9155/28/8/003. [DOI] [PubMed] [Google Scholar]
- Molgat Y. M., Pollack S. V., Hurwitz J. J., Bunas S. J., Manning T., McCormack K. M., Pinnell S. R. Comparative study of wound healing in porcine skin with CO2 laser and other surgical modalities: preliminary findings. Int J Dermatol. 1995 Jan;34(1):42–47. doi: 10.1111/j.1365-4362.1995.tb04379.x. [DOI] [PubMed] [Google Scholar]
- Montgomery T. C., Sharp J. B., Bellina J. H., Ross L. F. Comparative gross and histological study of the effects of scalpel, electric knife, and carbon dioxide laser on skin and uterine incisions in dogs. Lasers Surg Med. 1983;3(1):9–22. doi: 10.1002/lsm.1900030103. [DOI] [PubMed] [Google Scholar]
- Moreno R. A., Hebda P. A., Zitelli J. A., Abell E. Epidermal cell outgrowth from CO2 laser- and scalpel-cut explants: implications for wound healing. J Dermatol Surg Oncol. 1984 Nov;10(11):863–868. doi: 10.1111/j.1524-4725.1984.tb01338.x. [DOI] [PubMed] [Google Scholar]
- Morris J. A., Jr, Wilcox T. R., Reed G. W., Hunter E. B., Wallas C. H., Steane E. A., Shotts S. D., Vitsky J. L. Safety of the blood supply. Surrogate testing and transmission of hepatitis C in patients after massive transfusion. Ann Surg. 1994 May;219(5):517–526. doi: 10.1097/00000658-199405000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts A. H. The effect of topical epinephrine on blood loss following tangential excision of burn wounds. Plast Reconstr Surg. 1984 Sep;74(3):450–451. doi: 10.1097/00006534-198409000-00031. [DOI] [PubMed] [Google Scholar]
- Robinson N. B., Heimbach D. M., Reynolds L. O., Pavlin E., Durtschi M. B., Riem M., Craig K. Ventilation and perfusion alterations following homologous blood transfusion. Surgery. 1982 Aug;92(2):183–191. [PubMed] [Google Scholar]
- Rosenberg J. L., Zawacki B. E. Reduction of blood loss using tourniquets and 'compression' dressings in excising limb burns. J Trauma. 1986 Jan;26(1):47–50. doi: 10.1097/00005373-198601000-00008. [DOI] [PubMed] [Google Scholar]
- Schomacker K. T., Walsh J. T., Jr, Flotte T. J., Deutsch T. F. Thermal damage produced by high-irradiance continuous wave CO2 laser cutting of tissue. Lasers Surg Med. 1990;10(1):74–84. doi: 10.1002/lsm.1900100115. [DOI] [PubMed] [Google Scholar]
- Sheridan R. L., Tompkins R. G., Burke J. F. Management of burn wounds with prompt excision and immediate closure. J Intensive Care Med. 1994 Jan;9(1):6–17. doi: 10.1177/088506669400900103. [DOI] [PubMed] [Google Scholar]
- Siegel R. J., Vistnes L. M., Iverson R. E. Effective hemostasis with less epinephrine. An experimental and clinical study. Plast Reconstr Surg. 1973 Feb;51(2):129–133. doi: 10.1097/00006534-197302000-00003. [DOI] [PubMed] [Google Scholar]
- Sittig K. M., Deitch E. A. Blood transfusions: for the thermally injured or for the doctor? J Trauma. 1994 Mar;36(3):369–372. [PubMed] [Google Scholar]
- Slutzki S., Shafir R., Bornstein L. A. Use of the carbon dioxide laser for large excisions with minimal blood loss. Plast Reconstr Surg. 1977 Aug;60(2):250–255. doi: 10.1097/00006534-197708000-00012. [DOI] [PubMed] [Google Scholar]
- Snelling C. F., Shaw K. The effect of topical epinephrine hydrochloride in saline on blood loss following tangential excision of burn wounds. Plast Reconstr Surg. 1983 Dec;72(6):830–836. doi: 10.1097/00006534-198312000-00016. [DOI] [PubMed] [Google Scholar]
- Stuart J. D., Kenney J. G., Lettieri J., Spotnitz W., Baker J. Application of single-donor fibrin glue to burns. J Burn Care Rehabil. 1988 Nov-Dec;9(6):619–622. doi: 10.1097/00004630-198811000-00010. [DOI] [PubMed] [Google Scholar]
- Sullivan T., Smith J., Kermode J., McIver E., Courtemanche D. J. Rating the burn scar. J Burn Care Rehabil. 1990 May-Jun;11(3):256–260. doi: 10.1097/00004630-199005000-00014. [DOI] [PubMed] [Google Scholar]
- Tompkins R. G., Burke J. F., Schoenfeld D. A., Bondoc C. C., Quinby W. C., Jr, Behringer G. C., Ackroyd F. W. Prompt eschar excision: a treatment system contributing to reduced burn mortality. A statistical evaluation of burn care at the Massachusetts General Hospital (1974-1984). Ann Surg. 1986 Sep;204(3):272–281. doi: 10.1097/00000658-198609000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh J. T., Jr, Flotte T. J., Anderson R. R., Deutsch T. F. Pulsed CO2 laser tissue ablation: effect of tissue type and pulse duration on thermal damage. Lasers Surg Med. 1988;8(2):108–118. doi: 10.1002/lsm.1900080204. [DOI] [PubMed] [Google Scholar]
- Waymack J. P., Fernandes G., Cappelli P. J., Burleson D. G., Guzman R. F., Mason A. D., Jr, Pruitt B. A., Jr Alterations in host defense associated with anesthesia and blood transfusions. II. Effect on response to endotoxin. Arch Surg. 1991 Jan;126(1):59–62. doi: 10.1001/archsurg.1991.01410250065010. [DOI] [PubMed] [Google Scholar]