Abstract
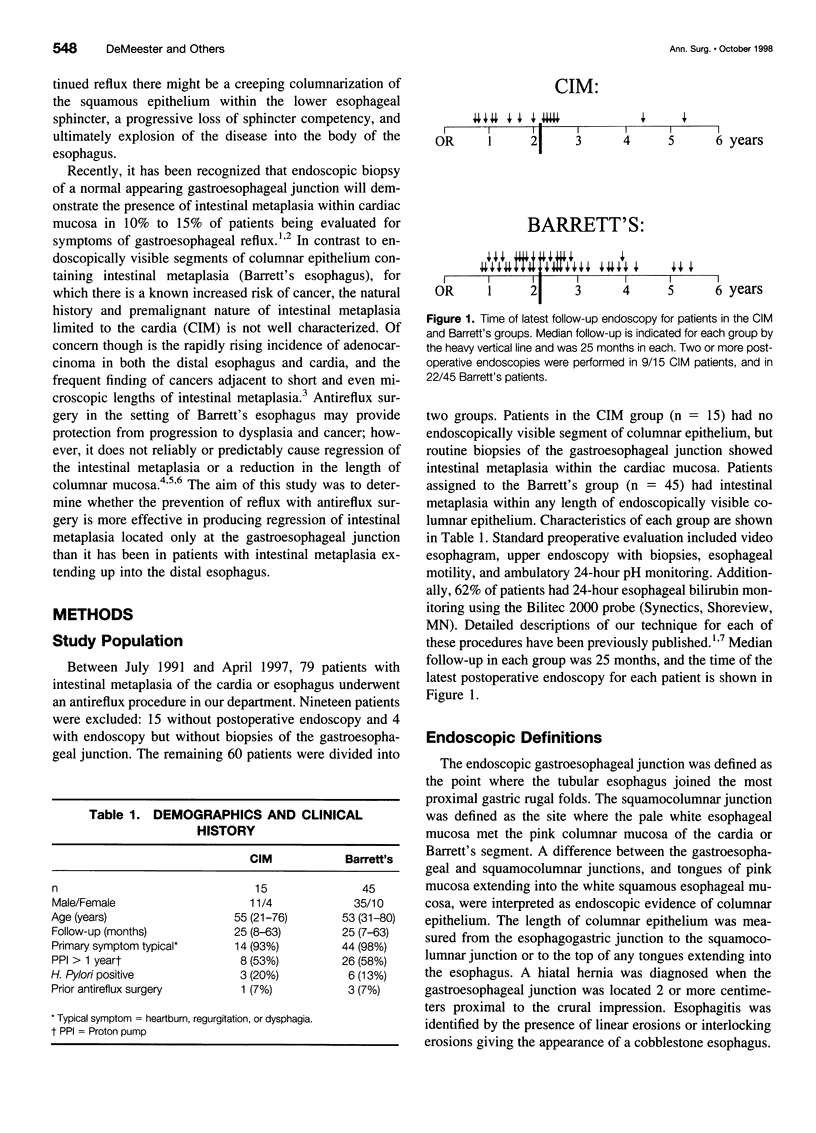
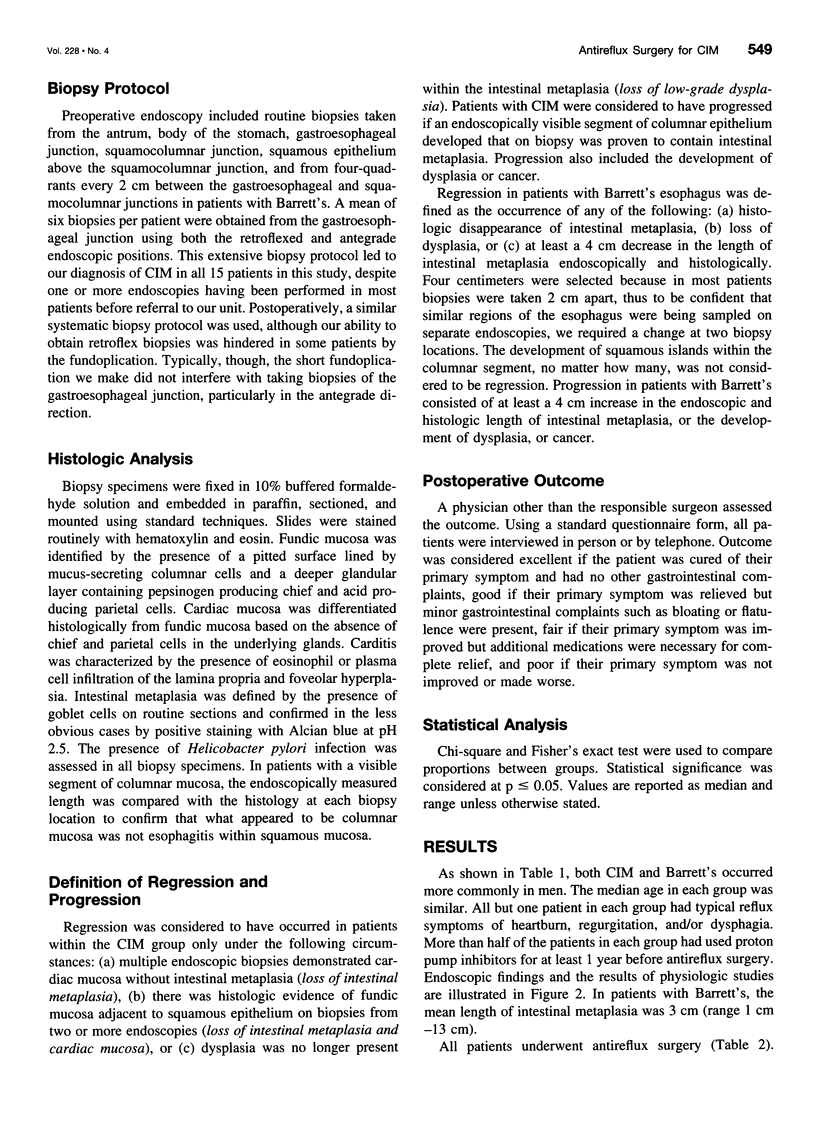
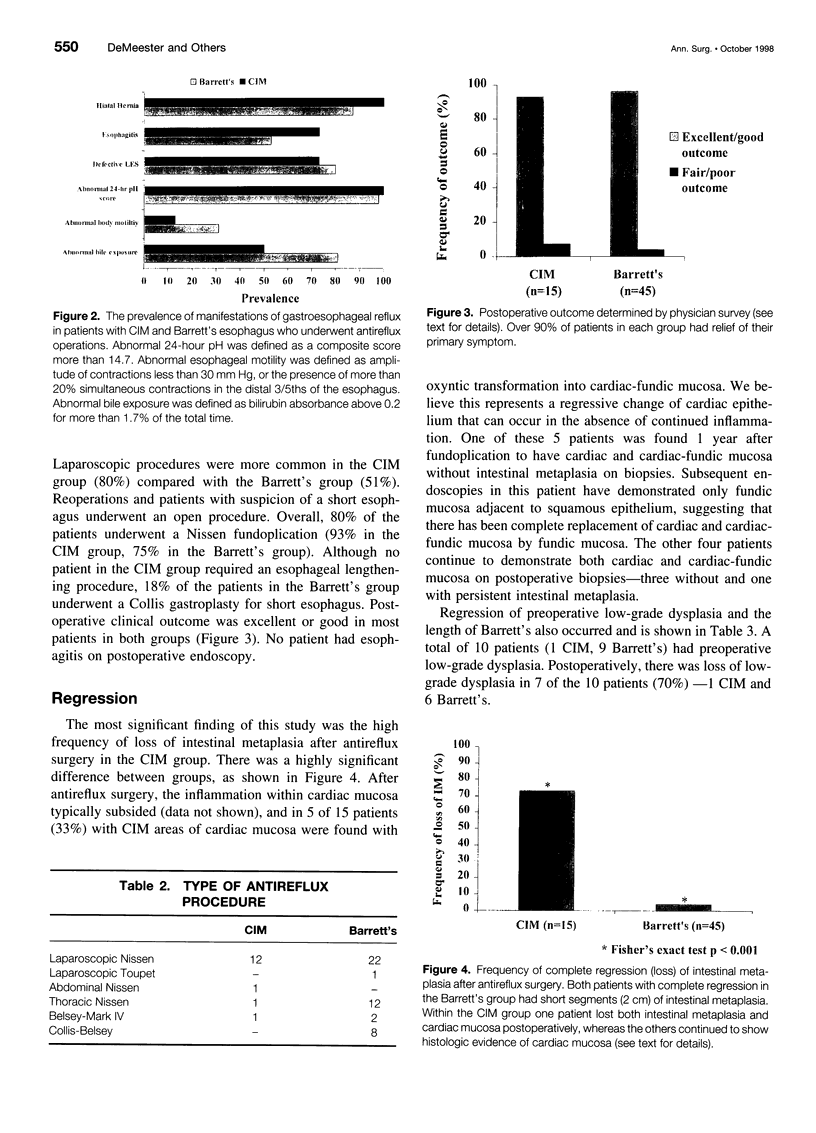
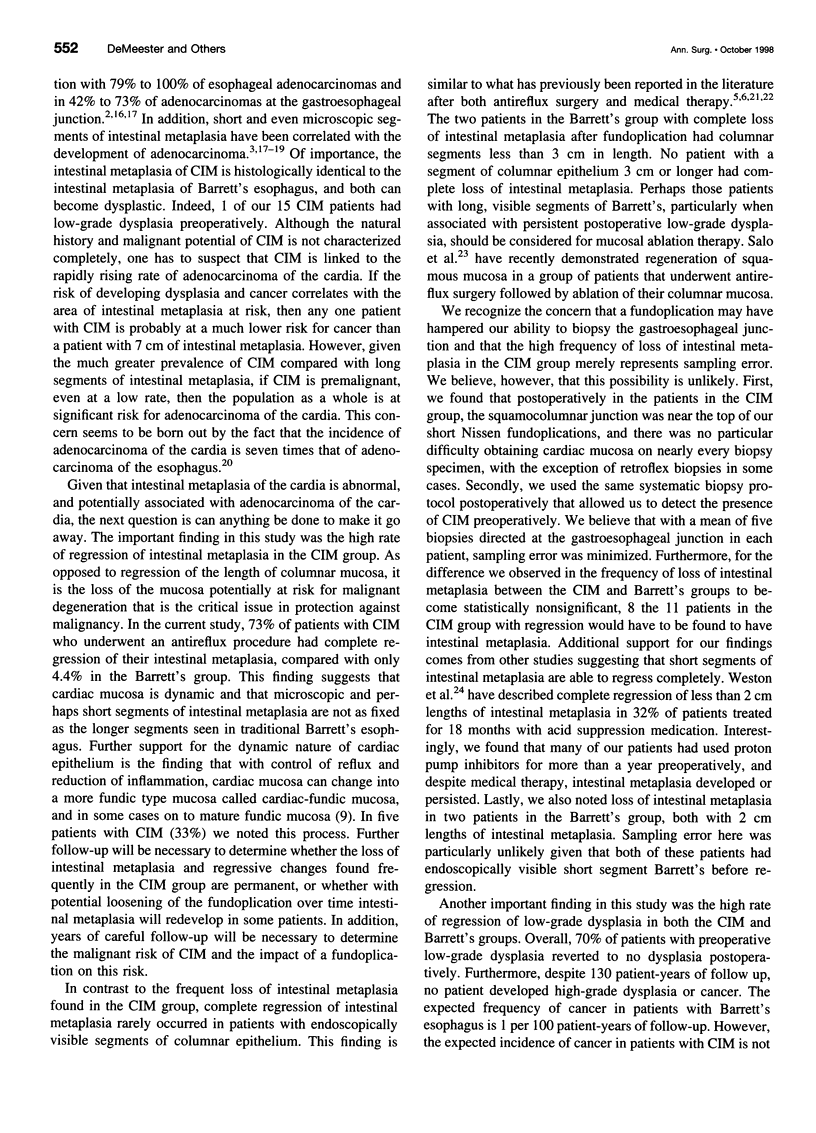
OBJECTIVE: The aim of this study was to determine whether antireflux surgery is more effective in producing loss of intestinal metaplasia located only at the gastroesophageal junction than it has been in patients with intestinal metaplasia extending up into the distal esophagus. SUMMARY BACKGROUND DATA: Biopsies of a normal appearing gastroesophageal junction will demonstrate cardiac mucosa containing goblet cells--the hallmark of intestinal metaplasia--in 10% to 15% of patients who are evaluated for symptoms of gastroesophageal reflux. The incidence of adenocarcinoma of the esophagus and cardia is rising faster than any other cancer in America, and most of these cancers are found adjacent to areas of intestinal metaplasia. Antireflux surgery in patients with Barrett's esophagus may provide protection from progression to dysplasia and cancer; however, it does not reliably cause regression of the intestinal metaplasia. Less is known about the potential for intestinal metaplasia limited to the cardia (CIM) to regress. METHODS: Sixty patients with intestinal metaplasia of the esophagus or cardia had antireflux surgery. Patients in the intestinal (CIM) group (n = 15) had no endoscopically visible segment of columnar epithelium. Patients in the Barrett's group (n = 45) had columnar epithelium visible within the esophagus. Median follow-up was 25 months in each group. RESULTS: Postoperative biopsies showed complete loss of intestinal metaplasia in 73% of the patients with CIM compared with 4.4% of the patients with Barrett's. Low-grade dysplasia, present in 10 patients preoperatively, regressed in 7 patients (70%). No patient progressed to high-grade dysplasia or cancer. CONCLUSIONS: Loss of intestinal metaplasia after antireflux surgery is rare in patients with Barrett's, but occurred in most patients with CIM. This suggests that cardiac epithelium is dynamic and that microscopic areas of intestinal metaplasia are able to regress much more frequently than longer, visible segments of intestinal metaplasia.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blot W. J., Devesa S. S., Kneller R. W., Fraumeni J. F., Jr Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA. 1991 Mar 13;265(10):1287–1289. [PubMed] [Google Scholar]
- Chandrasoma P. Pathophysiology of Barrett's esophagus. Semin Thorac Cardiovasc Surg. 1997 Jul;9(3):270–278. [PubMed] [Google Scholar]
- Clark G. W., Ireland A. P., Peters J. H., Chandrasoma P., DeMeester T. R., Bremner C. G. Short-segment Barrett's esophagus: A prevalent complication of gastroesophageal reflux disease with malignant potential. J Gastrointest Surg. 1997 Mar-Apr;1(2):113–122. doi: 10.1016/s1091-255x(97)80098-4. [DOI] [PubMed] [Google Scholar]
- Clark G. W., Smyrk T. C., Burdiles P., Hoeft S. F., Peters J. H., Kiyabu M., Hinder R. A., Bremner C. G., DeMeester T. R. Is Barrett's metaplasia the source of adenocarcinomas of the cardia? Arch Surg. 1994 Jun;129(6):609–614. doi: 10.1001/archsurg.1994.01420300051007. [DOI] [PubMed] [Google Scholar]
- Csendes A., Maluenda F., Braghetto I., Csendes P., Henriquez A., Quesada M. S. Location of the lower oesophageal sphincter and the squamous columnar mucosal junction in 109 healthy controls and 778 patients with different degrees of endoscopic oesophagitis. Gut. 1993 Jan;34(1):21–27. doi: 10.1136/gut.34.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMeester S. R. Management of Barrett's esophagus free of dysplasia. Semin Thorac Cardiovasc Surg. 1997 Jul;9(3):279–284. [PubMed] [Google Scholar]
- DeMeester T. R., Attwood S. E., Smyrk T. C., Therkildsen D. H., Hinder R. A. Surgical therapy in Barrett's esophagus. Ann Surg. 1990 Oct;212(4):528–542. doi: 10.1097/00000658-199010000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fein M., Ireland A. P., Ritter M. P., Peters J. H., Hagen J. A., Bremner C. G., DeMeester T. R. Duodenogastric reflux potentiates the injurious effects of gastroesophageal reflux. J Gastrointest Surg. 1997 Jan-Feb;1(1):27–33. doi: 10.1007/s11605-006-0006-x. [DOI] [PubMed] [Google Scholar]
- HAYWARD J. The lower end of the oesophagus. Thorax. 1961 Mar;16:36–41. doi: 10.1136/thx.16.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haggitt R. C., Tryzelaar J., Ellis F. H., Colcher H. Adenocarcinoma complicating columnar epithelium-lined (Barrett's) esophagus. Am J Clin Pathol. 1978 Jul;70(1):1–5. doi: 10.1093/ajcp/70.1.1. [DOI] [PubMed] [Google Scholar]
- Hamilton S. R., Smith R. R., Cameron J. L. Prevalence and characteristics of Barrett esophagus in patients with adenocarcinoma of the esophagus or esophagogastric junction. Hum Pathol. 1988 Aug;19(8):942–948. doi: 10.1016/s0046-8177(88)80010-8. [DOI] [PubMed] [Google Scholar]
- Hamilton S. R., Yardley J. H. Regnerative of cardiac type mucosa and acquisition of Barrett mucosa after esophagogastrostomy. Gastroenterology. 1977 Apr;72(4 Pt 1):669–675. [PubMed] [Google Scholar]
- Johnston M. H., Hammond A. S., Laskin W., Jones D. M. The prevalence and clinical characteristics of short segments of specialized intestinal metaplasia in the distal esophagus on routine endoscopy. Am J Gastroenterol. 1996 Aug;91(8):1507–1511. [PubMed] [Google Scholar]
- Lindahl H., Rintala R., Sariola H., Louhimo I. Cervical Barrett's esophagus: a common complication of gastric tube reconstruction. J Pediatr Surg. 1990 Apr;25(4):446–448. doi: 10.1016/0022-3468(90)90391-l. [DOI] [PubMed] [Google Scholar]
- McDonald M. L., Trastek V. F., Allen M. S., Deschamps C., Pairolero P. C., Pairolero P. C. Barretts's esophagus: does an antireflux procedure reduce the need for endoscopic surveillance? J Thorac Cardiovasc Surg. 1996 Jun;111(6):1135–1140. doi: 10.1016/s0022-5223(96)70214-3. [DOI] [PubMed] [Google Scholar]
- Morales T. G., Sampliner R. E., Bhattacharyya A. Intestinal metaplasia of the gastric cardia. Am J Gastroenterol. 1997 Mar;92(3):414–418. [PubMed] [Google Scholar]
- Oberg S., Peters J. H., DeMeester T. R., Chandrasoma P., Hagen J. A., Ireland A. P., Ritter M. P., Mason R. J., Crookes P., Bremner C. G. Inflammation and specialized intestinal metaplasia of cardiac mucosa is a manifestation of gastroesophageal reflux disease. Ann Surg. 1997 Oct;226(4):522–532. doi: 10.1097/00000658-199710000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz A., Martinez de Haro L. F., Parrilla P., Morales G., Molina J., Bermejo J., Liron R., Aguilar J. Conservative treatment versus antireflux surgery in Barrett's oesophagus: long-term results of a prospective study. Br J Surg. 1996 Feb;83(2):274–278. [PubMed] [Google Scholar]
- Salo J. A., Salminen J. T., Kiviluoto T. A., Nemlander A. T., Rämö O. J., Färkkilä M. A., Kivilaakso E. O., Mattila S. P. Treatment of Barrett's esophagus by endoscopic laser ablation and antireflux surgery. Ann Surg. 1998 Jan;227(1):40–44. doi: 10.1097/00000658-199801000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnell T. G., Sontag S. J., Chejfec G. Adenocarcinomas arising in tongues or short segments of Barrett's esophagus. Dig Dis Sci. 1992 Jan;37(1):137–143. doi: 10.1007/BF01308357. [DOI] [PubMed] [Google Scholar]
- Sharma P., Morales T. G., Bhattacharyya A., Garewal H. S., Sampliner R. E. Dysplasia in short-segment Barrett's esophagus: a prospective 3-year follow-up. Am J Gastroenterol. 1997 Nov;92(11):2012–2016. [PubMed] [Google Scholar]
- Weston A. P., Krmpotich P. T., Cherian R., Dixon A., Topalosvki M. Prospective long-term endoscopic and histological follow-up of short segment Barrett's esophagus: comparison with traditional long segment Barrett's esophagus. Am J Gastroenterol. 1997 Mar;92(3):407–413. [PubMed] [Google Scholar]