Abstract
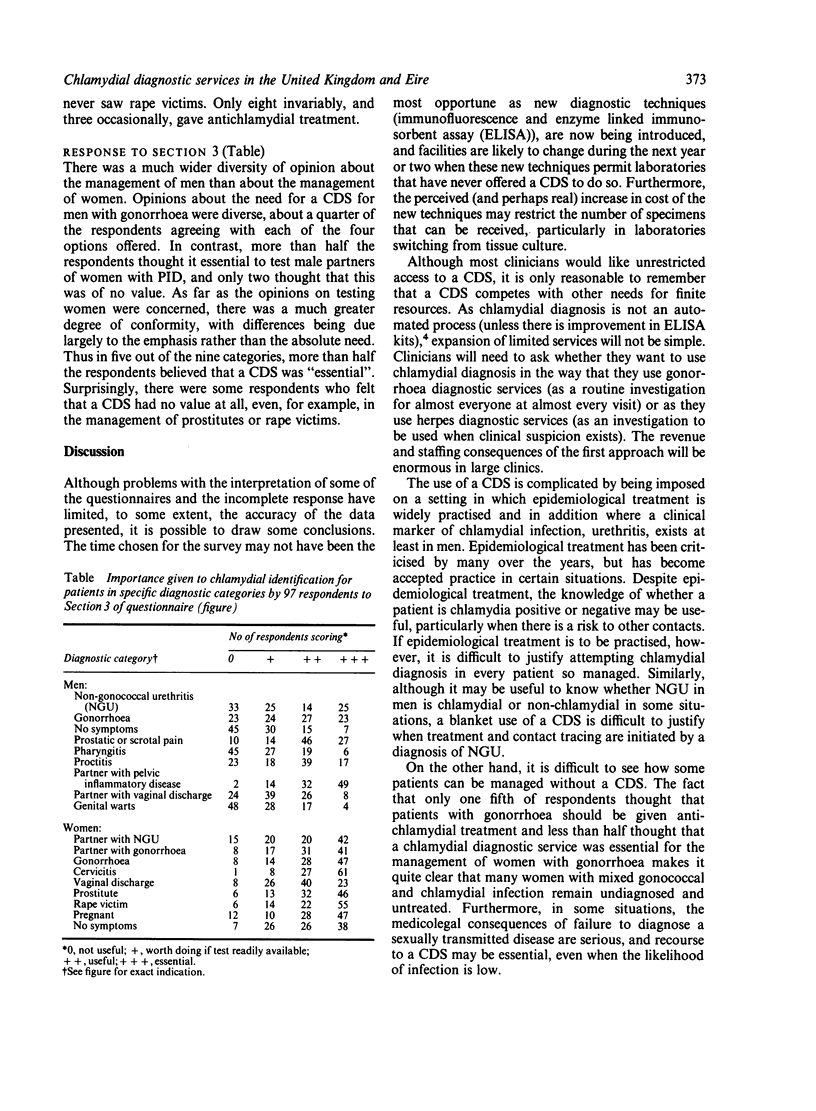
Consultant genitourinary physicians were asked about facilities for chlamydial diagnosis and their perception of the need for this service. A wide range of facilities was available, but eight respondents had no access to a chlamydial diagnostic service (CDS). Epidemiological treatment was widely practised as a substitute for chlamydial diagnosis; some clinicians used a CDS as an adjunct to epidemiological treatment, but few clinicians based their treatment of female contacts of men with non-gonococcal urethritis on the results of a test for chlamydial infection. All respondents felt that a CDS was essential in some situations, although there was a difference of opinion about the extent of the CDS. Most clinicians believed that all or most women should be tested, but the need for testing men routinely was more controversial. Although a CDS is costly, many clinicians believed that early diagnosis was a cost effective procedure if it prevented the long term sequelae of pelvic inflammatory disease--ectopic pregnancy, chronic pelvic pain, and probably infertility.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arya O. P., Mallinson H., Goddard A. D. Epidemiological and clinical correlates of chlamydial infection of the cervix. Br J Vener Dis. 1981 Apr;57(2):118–124. doi: 10.1136/sti.57.2.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger R. E., Alexander E. R., Monda G. D., Ansell J., McCormick G., Holmes K. K. Chlamydia trachomatis as a cause of acute "idiopathic" epididymitis. N Engl J Med. 1978 Feb 9;298(6):301–304. doi: 10.1056/NEJM197802092980603. [DOI] [PubMed] [Google Scholar]
- Møller B. R., Allen J., Toft B., Hansen K. B., Taylor-Robinson D. Pelvic inflammatory disease after hysterosalpingography associated with Chlamydia trachomatis and Mycoplasma hominis. Br J Obstet Gynaecol. 1984 Dec;91(12):1181–1187. doi: 10.1111/j.1471-0528.1984.tb04734.x. [DOI] [PubMed] [Google Scholar]
- Osser S., Persson K. Postabortal pelvic infection associated with Chlamydia trachomatis and the influence of humoral immunity. Am J Obstet Gynecol. 1984 Nov 15;150(6):699–703. doi: 10.1016/0002-9378(84)90670-7. [DOI] [PubMed] [Google Scholar]
- Southgate L. J., Treharne J. D., Forsey T. Chlamydia trachomatis and Neisseria gonorrhoeae infections in women attending inner city general practices. Br Med J (Clin Res Ed) 1983 Sep 24;287(6396):879–881. doi: 10.1136/bmj.287.6396.879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weström L., Mårdh P. A. Chlamydial salpingitis. Br Med Bull. 1983 Apr;39(2):145–150. doi: 10.1093/oxfordjournals.bmb.a071806. [DOI] [PubMed] [Google Scholar]


