Abstract
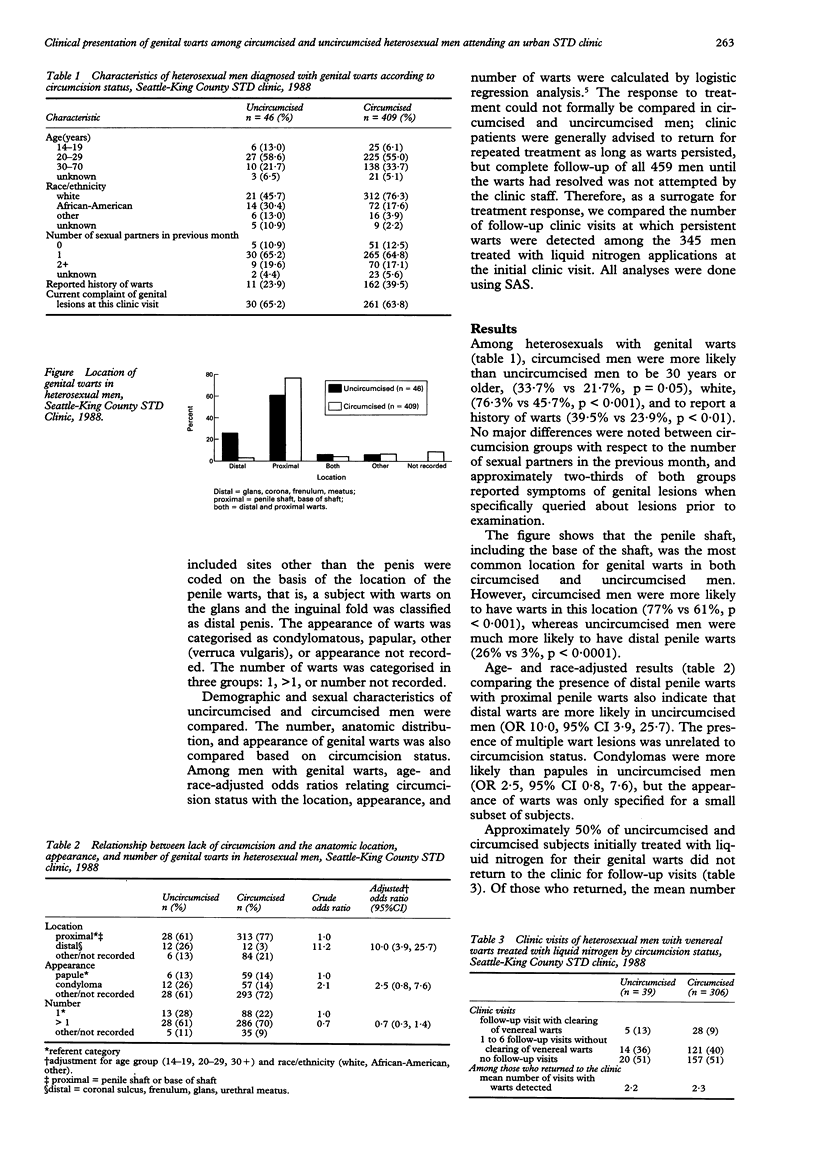
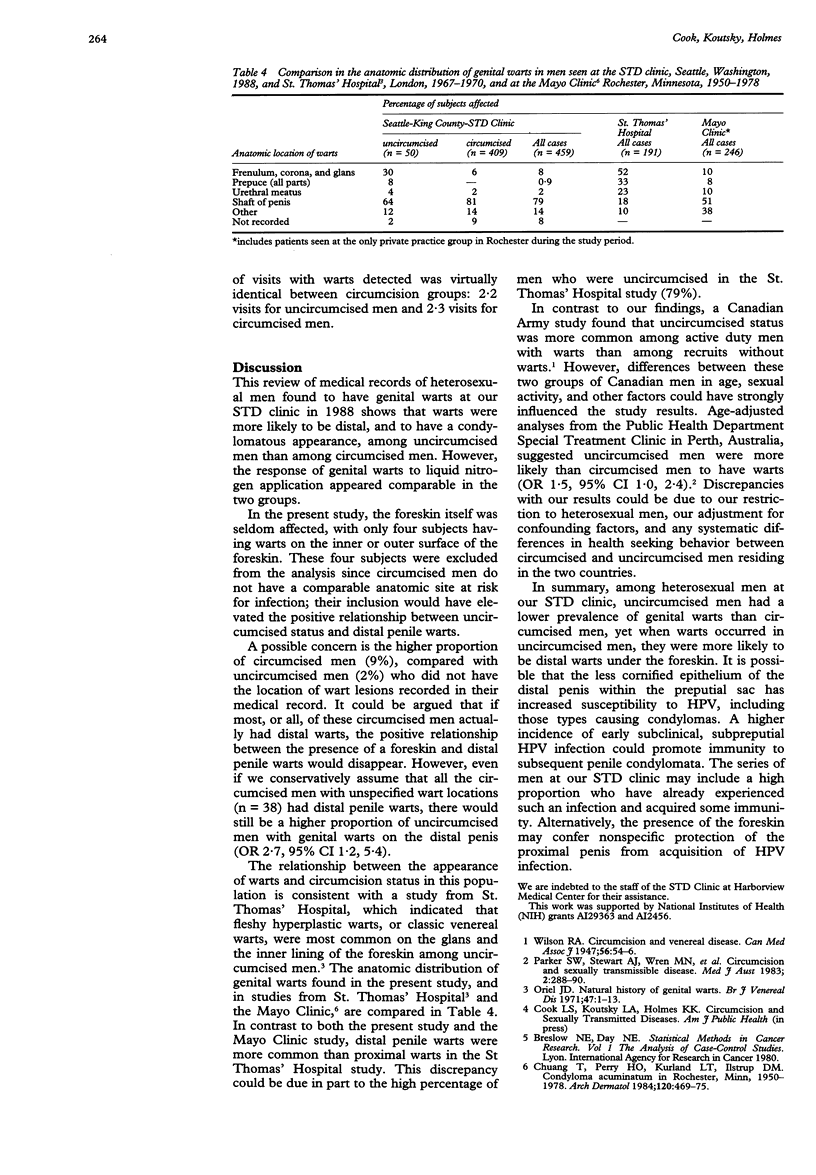
INTRODUCTION--A recent study comparing heterosexual men with and without confirmed sexually transmitted diseases (STDs) in an urban STD clinic showed that uncircumcised men were less likely than circumcised men to have genital warts detectable by clinical examination (adjusted odds ratio 0.7, 95% confidence interval 0.4, 0.9). Based on these initial findings we hypothesised that the appearance and anatomic distribution of genital warts, and possibly treatment response, may be different for circumcised and uncircumcised men. METHODS--The anatomic location, appearance, number of warts, and response to treatment was investigated through review of medical records of 459 heterosexual men with genital warts detected in 1988. RESULTS--Age- and race-adjusted estimates indicated that among men with genital warts, warts were detected much more commonly on the distal penis--that is, the corona, frenulum, glans or urethral meatus-, among uncircumcised men (26%) than among circumcised men (3%) (OR 10.0, 95% CI 3.9, 25.7). Where the appearance was specified, warts were more often described as condylomatous in uncircumcised men and slightly more often as papular in circumcised men. No significant difference between circumcised and uncircumcised men was seen in the number of return visits to the clinic for persistent warts after treatment with liquid nitrogen: 2.2 visits for 19 uncircumcised men and 2.3 visits for 149 circumcised men. CONCLUSION--Circumcised men were more likely than uncircumcised men to have genital warts, but when present, warts were more often located on the distal portion of the penis among uncircumcised men. This paradox is not understood, but could reflect either nonspecific resistance to proximal penile warts conferred by the foreskin, or heightened susceptibility to various HPV types in uncircumcised men, some of which may confer subsequent immunity to genital warts.
Full text
PDF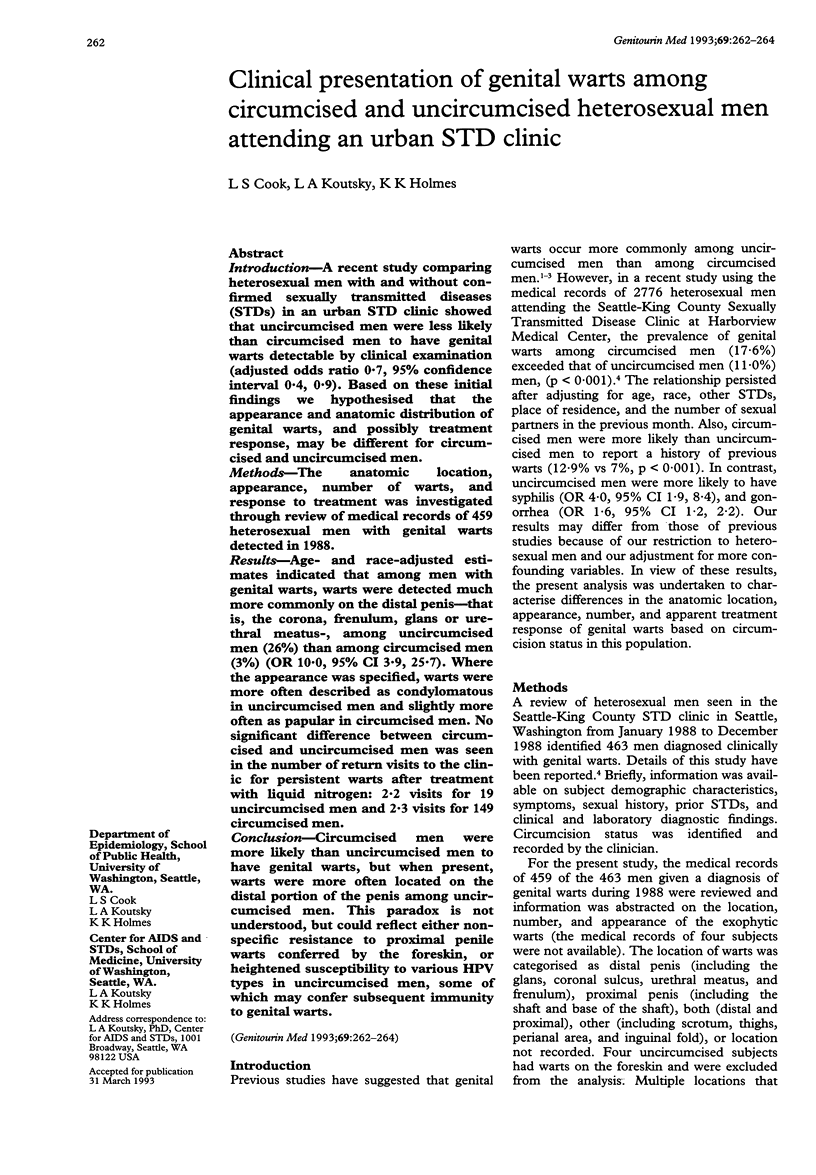
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chuang T. Y., Perry H. O., Kurland L. T., Ilstrup D. M. Condyloma acuminatum in Rochester, Minn., 1950-1978. I. Epidemiology and clinical features. Arch Dermatol. 1984 Apr;120(4):469–475. [PubMed] [Google Scholar]
- Oriel J. D. Natural history of genital warts. Br J Vener Dis. 1971 Feb;47(1):1–13. doi: 10.1136/sti.47.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker S. W., Stewart A. J., Wren M. N., Gollow M. M., Straton J. A. Circumcision and sexually transmissible disease. Med J Aust. 1983 Sep 17;2(6):288–290. doi: 10.5694/j.1326-5377.1983.tb122467.x. [DOI] [PubMed] [Google Scholar]
- WILSON R. A. Circumcision and venereal disease. Can Med Assoc J. 1947 Jan;56(1):54–56. [PMC free article] [PubMed] [Google Scholar]


