Abstract
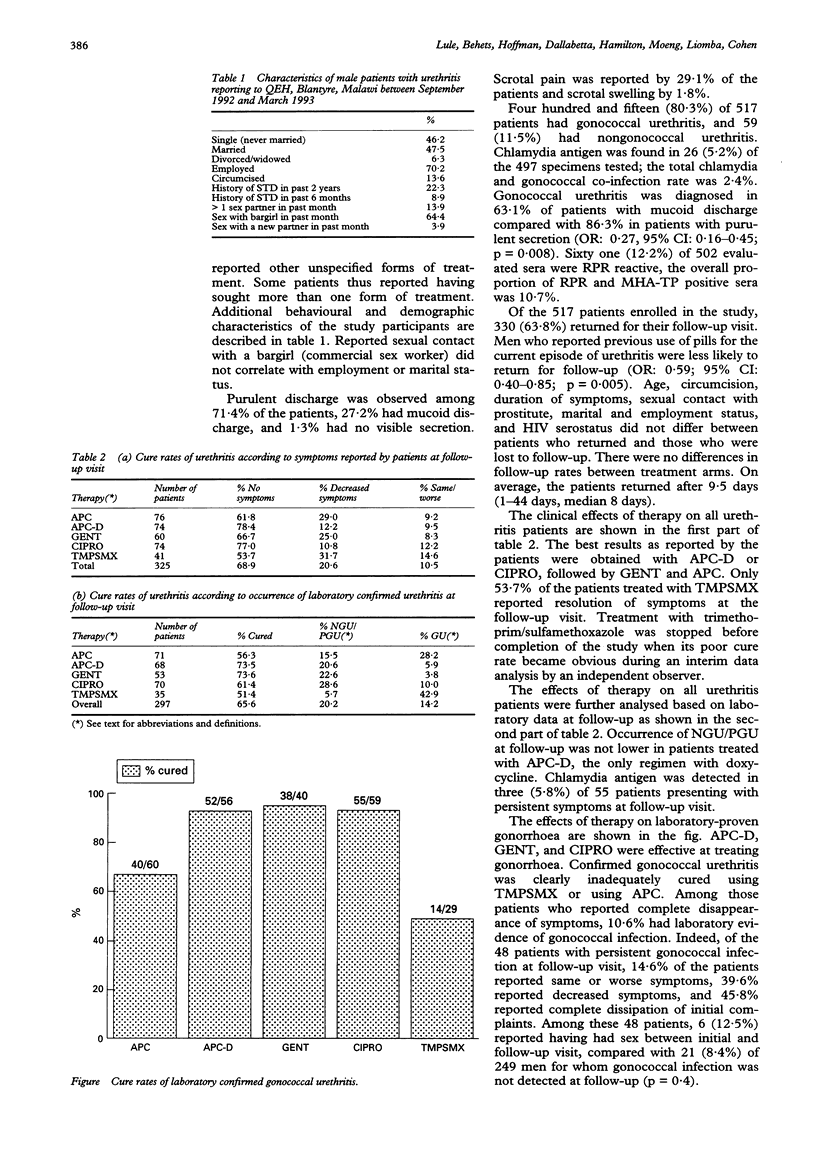
OBJECTIVES--To evaluate gonococcal (GU) and nongonococcal urethritis (NGU), chlamydia antigen, and serostatus for syphilis and human immunodeficiency virus (HIV) among males attending a Malawian STD clinic with complaints of urethral discharge and/or dysuria. To collect demographic and behavioural data and to determine the effectiveness of five treatments for urethritis. METHODS--Urethritis was diagnosed using microscopy and culture for Neisseria gonorrhoeae. Sera were screened with rapid plasma reagin (RPR) and if reactive, with microhaemagglutination for Treponema pallidum (MHA-TP). HIV antibodies and chlamydia antigen were detected using enzyme immunoassay. Patients were randomised for treatment, cure was assessed 8-10 days later. RESULTS--At enrolment, GU was diagnosed in 415 (80.3%) and NGU in 59 (11.2%) of 517 males. Chlamydia antigen was found in 26 (5.2%) of 497 specimens tested. Syphilis seropositivity rate (RPR and MHA-TP reactive) was 10.7%. Overall HIV seroprevalence was 44.2%; 71.7% of men with reactive syphilis serology were HIV(+) compared with 40.9% of syphilis seronegatives (OR: 3.6, p < 0.001). Trimethoprim 320 mg/sulphamethoxazole 1600 mg by mouth for 2 days (TMPSMX), or the combination of amoxicillin 3 gm, probenicid 1 gm, and clavulanate 125 mg by mouth once (APC), failed to cure gonorrhoea effectively. Amoxicillin 3 gm, probenicid 1 gm, and clavulanate 125 mg, by mouth once with doxycycline 100 mg BID for 7 days (APC-D), gentamicin 240 mg IM once (GENT), ciprofloxacin 250 mg by mouth once (CIPRO) cured 92.9% to 95% of gonorrhoea. APC-D treatment did not generate less NGU at follow-up. HIV serostatus did not affect cure of urethritis. CONCLUSION--All patients presenting with urethritis should be treated syndromically using a simple algorithm and screened for syphilis seroreactivity for appropriate treatment and counselling.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cohen M. S., Dallabetta G., Laga M., Holmes K. K. A new deal in HIV prevention: lessons from the global approach. Ann Intern Med. 1994 Feb 15;120(4):340–341. doi: 10.7326/0003-4819-120-4-199402150-00014. [DOI] [PubMed] [Google Scholar]
- Dallabetta G. A., Miotti P. G., Chiphangwi J. D., Saah A. J., Liomba G., Odaka N., Sungani F., Hoover D. R. High socioeconomic status is a risk factor for human immunodeficiency virus type 1 (HIV-1) infection but not for sexually transmitted diseases in women in Malawi: implications for HIV-1 control. J Infect Dis. 1993 Jan;167(1):36–42. doi: 10.1093/infdis/167.1.36. [DOI] [PubMed] [Google Scholar]
- Grosskurth H., Plummer F., Mhalu F., Mabey D. STD research in Africa. Lancet. 1993 Dec 4;342(8884):1415–1416. doi: 10.1016/0140-6736(93)92767-n. [DOI] [PubMed] [Google Scholar]
- Kristensen J. K. The prevalence of symptomatic sexually transmitted diseases and human immunodeficiency virus infection in outpatients in Lilongwe, Malawi. Genitourin Med. 1990 Aug;66(4):244–246. doi: 10.1136/sti.66.4.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merson M. H. Slowing the spread of HIV: agenda for the 1990s. Science. 1993 May 28;260(5112):1266–1268. doi: 10.1126/science.8493570. [DOI] [PubMed] [Google Scholar]
- Wasserheit J. N. Epidemiological synergy. Interrelationships between human immunodeficiency virus infection and other sexually transmitted diseases. Sex Transm Dis. 1992 Mar-Apr;19(2):61–77. [PubMed] [Google Scholar]


