Abstract
Antibiotic-resistant bacterial infections are a significant clinical challenge, especially when involving multiple species. Antimicrobial peptides and their synthetic analogues, peptoids, which target bacterial cell membranes as well as intracellular components, offer potential solutions. We evaluated the biological activities of novel peptoids TM11-TM20, which include an additional charged NLys residue, against multidrug-resistant Pseudomonas aeruginosa and Staphylococcus aureus, both in vitro and in vivo. Building on insights from previously reported compounds TM1-TM10, the lipo-peptoid TM18, which forms self-assembled ellipsoidal micelles, demonstrated potent antimicrobial, anti-biofilm, and anti-abscess activity. Transcriptome sequencing (RNA-seq) revealed that TM18 disrupted gene expression pathways linked to antibiotic resistance and tolerance, and biofilm formation in both pathogens. Under dual-species conditions, TM18 induced overlapping but attenuated transcriptional changes, suggesting a priming effect that enhances bacterial tolerance. In a murine skin infection model, TM18 significantly reduced dermonecrosis and bacterial burden in mono-species infections. When combined with the antibiotic meropenem, they synergistically nearly cleared co-infections. Our findings highlight that TM18 has potential as a novel therapeutic for combating antibiotic-resistant pathogens and associated biofilm-driven tolerance.
Keywords: Polymicrobial, Host-mimicking conditions, Abscess model, Biofilms, Peptides, Peptoids
Highlights
-
•
Lipo-peptoid TM18 disrupts biofilms formed by antibiotic-resistant pathogens.
-
•
TM18 self-assembles into core-shell ellipsoidal micelles with potent antimicrobial activity.
-
•
TM18 modulates bacterial gene expression, impacting biofilm tolerance mechanisms.
-
•
TM18 shows strong anti-abscess effects in a murine skin infection model.
-
•
TM18 synergizes with meropenem, significantly reducing polymicrobial infections in vivo.
Significance statement
Antibiotic-resistant infections are increasingly complex, especially when multiple bacterial species are involved. This study introduces a novel lipo-peptoid, TM18, as a potent antimicrobial agent that effectively disrupts the defenses of multidrug-resistant Pseudomonas aeruginosa and Staphylococcus aureus, both individually and in dual-species settings. By targeting both biofilm formation and gene expression pathways related to bacterial tolerance, TM18 not only reduces bacterial load but also alleviates dermonecrosis in a murine infection model. Notably, the combined use of TM18 and meropenem approaches near eradication of co-infections. This work highlights TM18's potential to fill critical gaps in the treatment of dual-species infections and improve clinical outcomes against challenging antibiotic-resistant pathogens.
1. Introduction
Chronic infections are a significant burden worldwide, with approximately 80% attributed to biofilms [1]. Biofilms are aggregates of bacteria encased in a self-produced extracellular matrix (ECM) that protects them from the environment and allows them to adhere to various surfaces [2,3]. Bacteria within biofilms are challenging to treat due to structural and phenotypic heterogeneity, which includes limited antimicrobial penetration of the ECM, but also physiological adaptations of biofilm-associated cells, including metabolic dormancy of some bacterial subpopulations, protection from the host immune system, negatively charged extracellular DNA decreasing antibiotic efficacy, increased horizontal gene transfer of resistance genes, and complex cell-to-cell interactions that enable synergistic cooperation [[3], [4], [5]]. Biofilms are frequently polymicrobial, involving two or more species, and are often associated with worse patient outcomes [6]. Pseudomonas aeruginosa and Staphylococcus aureus are commonly co-isolated from chronic infections such as otitis media, chronic wound infections, and lung infections in cystic fibrosis patients [7]. The complex nature of biofilms often renders antibiotic therapy ineffective, allowing infections to persist.
The importance of polymicrobial infections and biofilm-associated infections has been increasingly recognized [8,9], highlighting the need for effective treatment strategies. Different bacterial species can co-evolve and interact during these infections, leading to increased tolerance and antibiotic resistance [10,11]. Current methods of studying multispecies polymicrobial infections and biofilms are limited as in vitro co-culture techniques often favor one species over others. Additionally, resistance quantification typically uses standard antimicrobial susceptibility tests and antibiofilm activity assays in laboratory media, which do not capture aspects of the complex host environment and bacterial interactions [12,13]. Indeed, it is well-established that the host environment has a major impact on the efficacy of antimicrobial compounds against pathogens, influencing and interfering with compound activity [14].
Antimicrobial peptides (AMPs) have emerged as a promising avenue to combat biofilm-associated infections due to their broad-spectrum activity against both Gram-negative and Gram-positive bacteria, parasites, and viruses [15,16] and activity in both standard laboratory media and host-mimicking conditions [17]. However, many peptides exhibit drawbacks such as poor stability, susceptibility to proteolytic degradation, and poor absorption [18]. To overcome these limitations, peptidomimetics, which are more stable than peptides, resistant to enzymatic degradation, and have higher selectivity, have been developed and studied [19]. Peptidomimetics include peptoids, synthetic molecules that mimic peptide structures but are less susceptible to enzymatic degradation and show excellent in vivo stability due to the amino acid functional side chain being appended to the nitrogen atom rather than to the α-carbon in the oligoamide backbone [20]. Antimicrobial peptoids self-assemble into complex multimeric structures, including helical bundles, core-shell ellipsoidal micelles, or worm-like micelles, with the most efficacious compounds forming monodisperse ellipsoidal micelles in particular [17,21,22]. Critically, peptoids have demonstrated strong activity against biofilm-associated bacteria [17,23,24].
Previously, we showed that peptoids TM1-TM10 exhibit antimicrobial and antibiofilm activity against mono- and dual-species biofilms in vitro, as well as anti-abscess activity against mono-species infections of P. aeruginosa and S. aureus [17]. The bioactivity of these peptoids was associated with their supramolecular assembly. Here we introduce new peptoids TM11-TM20, variants of TM1-TM10 with an added NLys group to increase the net positive charge. We demonstrate that lipo-peptoid TM18 exhibited potent activity against co-infections of P. aeruginosa and S. aureus in vitro and in vivo and synergized with the carbapenem antibiotic meropenem in vivo.
2. Results
2.1. Peptoids maintained their antimicrobial activity against P. aeruginosa and S. aureus under conditions that mimic the host environment
The host environment is composed of various components that can affect drug effectiveness [25,26]. In our previous study, we demonstrated the broad-spectrum activity of peptoids TM1-TM10 against all ESKAPE pathogens. We also found that the antimicrobial activity of some peptoids was altered when tested against P. aeruginosa and S. aureus under host-mimicking conditions [17]. Here, we screened a new library of ten peptoids (TM11-TM20), which are variants of our previously published peptoids with an added C-terminal NLys residue, introducing an additional positive charge. Specifically, TM11 is TM1 with an additional NLys, TM12 is TM2 + NLys, etc. This single NLys monomer has been shown to increase selectivity for bacteria over mammalian cells without affecting potency [27].
We selected the multidrug-resistant Liverpool Epidemic strain P. aeruginosa B58 (LESB58) and methicillin-resistant S. aureus (MRSA) USA300 LAC as model organisms to test the new peptoid library under standard laboratory conditions (Mueller Hinton Broth; MHB) and physiologically relevant conditions (tissue culture medium supplemented with fetal bovine serum and glucose, DFG) (Table 1). An inactive control peptoid lacking aromatic side chains [28], TM22 [29], was included as well.
Table 1.
MIC (μg/mL) of peptoids against multidrug-resistant P. aeruginosa LESB58 and methicillin-resistant S. aureus USA300 LAC in MHB and DFG.
| TM 11 | TM 12 | TM 13 | TM 14 | TM 15 | TM 16 | TM 17 | TM 18 | TM 19 | TM 20 | TM 22 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| P. aeruginosa LESB58 | |||||||||||
| DFG | 50 | 100 | 100 | 25 | 25 | 12.5 | >100 | 12.5 | 25 | 25 | >100 |
| MHB | 50 | >100 | 100 | 25 | 100 | 100 | >100 | 6.3 | 12.5 | 25 | >100 |
| S. aureus LAC USA300 | |||||||||||
| DFG | 1.6 | 1.6 | 3.1 | 1.6 | 1.6 | 0.6 | 12.5 | 1.6 | 3.1 | 6.3 | >100 |
| MHB | 6.3 | 6.3 | 6.3 | 6.3 | 3.1 | 0.6 | 25 | 6.3 | 12.5 | 12.5 | >100 |
The MICs against P. aeruginosa ranged from 6.25 to >100 μg/mL, with half of the peptoids showing no change in activity under host-mimicking conditions. Interestingly, TM15 and TM16 exhibited a 4- and 8-fold increase in activity, respectively, in DFG. In contrast, TM18 and TM19 showed a 2-fold decrease in activity in DFG against P. aeruginosa. Despite the decrease, TM18 exhibited the most potent activity against P. aeruginosa (12.5 μg/mL) under host-mimicking conditions. TM16 also demonstrated strong activity against P. aeruginosa in DFG and had the best activity against S. aureus (0.63 μg/mL).
On the other hand, all peptoids, except TM22, demonstrated strong activity against S. aureus with MIC values ranging from 0.63 to 12.5 μg/mL in both media. Most peptoids, except TM16, showed a 2-4-fold increase in activity against S. aureus under host-mimicking conditions compared to standard laboratory conditions.
2.2. Peptoids eradicated P. aeruginosa-S. aureus dual-species biofilms
Peptoids have emerged as promising agents with significant antibiofilm activity against both mono- and dual-species biofilms [17,23]. In our previous studies, we demonstrated that TM1-TM10 exhibited excellent antibiofilm activity, effectively killing bacteria within biofilms [17]. Here, we further investigated the efficacy of the new variants TM11-TM20 against biofilms formed by P. aeruginosa and S. aureus, both individually and in combination. Like the original peptoids [17], the new variants also did not exhibit strong activity against P. aeruginosa biomass removal as measured by crystal violet staining. However, many of the new peptoids were highly effective in reducing the biofilm mass of S. aureus by more than 50 % (Figs. S1A and S1B).
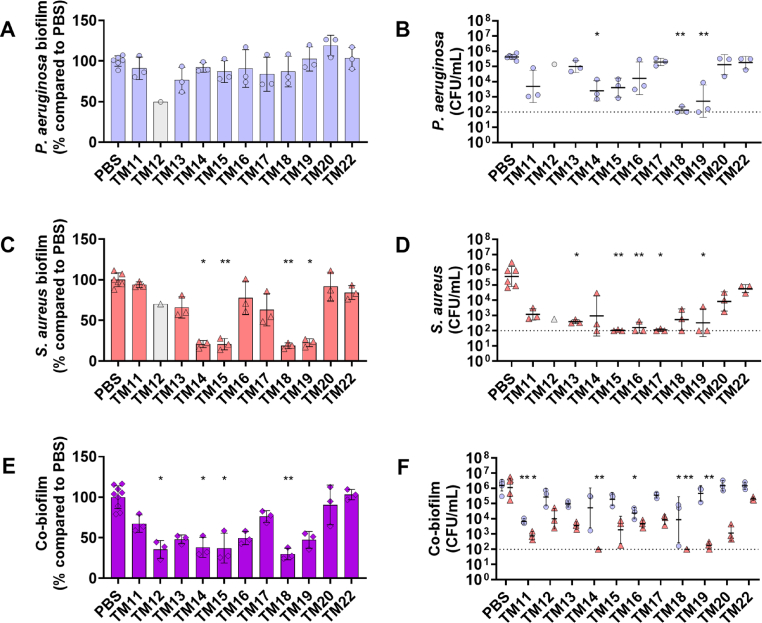
To gain further insights into their killing activity within biofilms, we used a fixed peptoid concentration of 31.25 μg/mL, determined by the overall antibiofilm activity of all peptoids and our previous studies [17]. This concentration is approximately at the P. aeruginosa MIC and 10–50 times the S. aureus MIC for most peptoids. As expected, peptoids at 31.25 μg/mL did not reduce mono-species P. aeruginosa biofilm mass (Fig. 1A). However, TM14, TM18, and TM19 significantly reduced bacterial survivors within the biofilm (Fig. 1B). In contrast, peptoids TM14, TM15, TM18, and TM19 exhibited a significant reduction of S. aureus biofilm mass (Fig. 1C), while TM15, TM16, TM17, and TM19 also significantly reduced S. aureus survivors within mono-species biofilms (Fig. 1D).
Fig. 1.
Antibiofilm activities of peptoids against mono-species and dual-species biofilms. Peptoids (31.25 μg/mL) were used to treat mono-species biofilms of (A, B) P. aeruginosa (purple circles), and (C, D) S. aureus (red triangles), as well as (E, F) dual-species biofilms of P. aeruginosa-S. aureus. Biofilms were grown for 20–24 h in DFG in 96-well plates before peptoid treatment, followed by re-incubation for 24 h. (A, C, E) Biofilm mass was quantified by staining with 0.1 % crystal violet and (B, D, F) bacterial survivors were determined on selective agar plates. TM12 data (grey circle/triangle; n = 1) was excluded from statistical analysis due to limited sample availability. Significance levels are indicated as ∗p < 0.05 and ∗∗p < 0.01 based on the Kruskal−Wallis test with Dunn's correction. Dashed line represents the limit of detection. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
We also previously used this specific peptoid concentration to treat P. aeruginosa-S. aureus dual-species biofilms [17]. Therefore, we further investigated the biofilm eradication activity against these biofilms. We found that TM12, TM14, TM15, and TM18 significantly reduced dual-species biofilm mass by more than 50% compared to untreated biofilms (Fig. 1E). Intriguingly, peptoids TM11, TM16 and TM18 displayed enhanced killing against P. aeruginosa, reducing bacterial survivors by approximately 1000-, 100-, and 100-fold, respectively. Peptoids TM12, TM13, TM15, TM16, TM17, TM20, and the control peptoid TM22 showed no significant reduction in S. aureus in dual-species biofilms (Fig. 1F). The most promising candidates, TM11, TM14, TM18 and TM19, reduced S. aureus bacterial survivors by 1000- to 10,000-fold.
Due to peptoid TM18 showing the greatest promise as an effective molecule, it was tested against additional P. aeruginosa (PAO1 and PA14) and S. aureus (HG001 and Newman) strains, showing broad-spectrum antimicrobial (Table S8) and antibiofilm activity (Fig. S2).
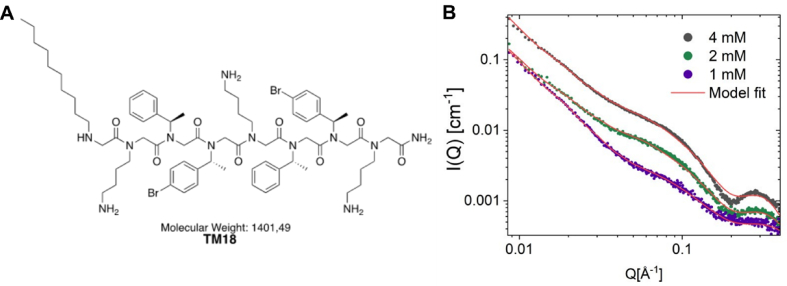
2.3. Lipo-peptoid TM18 self-assembled into core-shell ellipsoidal micelles
Among the peptoids screened for antimicrobial and anti-biofilm activity, the lipo-peptoid TM18 emerged as a particularly promising candidate due to its broad-spectrum antimicrobial activity and capability to reduce bacterial survivors within biofilms. Lipo-peptoids combine the structural features of peptides and lipids, enhancing their ability to interact with and disrupt bacterial membranes. To characterize the self-assembled structure of TM18 (H-Ndec-(NLys-Nspe-Nspe)2-NLys-NH2) in aqueous solution, we conducted synchrotron SAXS (Small-Angle X-ray Scattering) experiments and analyzed the data using theoretical modelling (Fig. 2). The results revealed that TM18 self-assembles into core-shell ellipsoidal micelles, similar to those shown for TM5 and TM8, which are well-characterized peptoids with potent broad-spectrum antimicrobial activity [17,30].
Fig. 2.
Structural and SAXS analysis of TM18. A) Chemical structure of TM18. B) SAXS data for TM18 measured at 1 mM, 2 mM, and 4 mM plotted together with the best fit (red line) using an ellipsoidal core shell-micellar model described in [17]. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
However, TM18 and TM8 have a slightly thicker shell (9 Å compared to 7 Å for TM5), which can be attributed to the two and three extra residues in the peptoid sequence. Similar to TM8, TM18 has a slightly smaller core than TM5 (10 Å compared to 13 Å for TM5), likely due to the shorter alkyl tail (Ndec rather than Ntridec). The scattering also indicated the presence of a small fraction of larger aggregates (0.08), evidenced by a sharp upturn at low Q (∼0.009−0.03), similarly as observed for TM8 [17].
2.4. TM18 induced transcriptional tolerance in P. aeruginosa and metabolic changes in S. aureus biofilms
Given the strong broad-spectrum, anti-biofilm activity of TM18 against mono- and dual-species P. aeruginosa and S. aureus biofilms, we further investigated the transcriptional regulatory responses using RNA-seq. Here, we utilized a static biofilm model on hydroxyapatite discs, which more accurately mimics biological surfaces and supports biofilm maturation [31,32]. Mono- and dual-species biofilms were grown under host-mimicking conditions and treated with TM18 for 1 h to capture an early treatment response. There was a considerable overlap (∼30 %) in the genes significantly dysregulated in response to TM18 treatment in both mono- and dual-species biofilms (Fig. S3).
For P. aeruginosa mono-species biofilms, TM18 treatment led to modest transcriptional changes with 96 genes significantly differentially expressed (FDR adjusted p-value <0.05 and fold-change >1.5 or < -1.5; 59 genes upregulated, 37 genes downregulated), likely due to the short treatment duration and its ability to tolerate the treatment, at least for a short period. Notably, TM18 treatment resulted in widespread upregulation of RND (resistance-nodulation-cell division)-type efflux systems, including mexCD-oprJ, mexEF-oprN mexJK, mexGHI-opmD and muxABC-opmB (Table 2, Table S1, Fig. S4). Additionally, the PmrAB two-component system, which modulates resistance to cationic antimicrobial peptides [33], was upregulated ∼20 fold, along with LPS aminoarabinosylation lipid A modification system, arn [34] (Table 2, Fig. S4). Interestingly, the outer membrane porin oprD was significantly dysregulated, showing a >3-fold downregulation when treated with TM18 in mono-species biofilms. Phenazine biosynthesis was also highly upregulated upon TM18 treatment (Fig. S4).
Table 2.
Differentially expressed genes for P. aeruginosa mono-species biofilms treated with 32 μg/mL TM18, compared to dual-species biofilms. Fold change (FC) relative to untreated samples, with positive values indicating increased expression when treated with TM18.
| Loci | Gene | Description | FC mono-species biofilms |
FC dual-species biofilms |
|---|---|---|---|---|
| Quorum sensing | ||||
| PALES_43251 | pqsE | Quinolone signal response protein | 4.4 | 1.5 |
| PALES_43261 | pqsD | 3-oxoacyl-(acyl carrier protein) synthase III | 4.0 | 1.4 |
| PALES_43271 | pqsC | beta-keto-acyl-acyl-carrier protein synthase | 3.0 | 1.2 |
| PALES_43281 | pqsB | Homologous to beta-keto-acyl-acyl-carrier protein synthase | 3.2 | 1.5 |
| PALES_43291 | pqsA | coenzyme A ligase | 2.7 | 1.4 |
| Efflux/uptake systems | ||||
| PALES_28031 | mexE | Resistance-Nodulation-Cell Division (RND) multidrug efflux membrane fusion protein | 1.6 | 1.2 |
| PALES_27691 | opmB | Outer membrane protein precursor | 3.6 | 2.6a |
| PALES_27681 | muxC | (RND) efflux transporter | 4.2 | 2.6a |
| PALES_27671 | muxB | (RND) efflux transporter | 4.4 | 2.3a |
| PALES_27661 | muxA | (RND) efflux membrane fusion protein | 3.1 | 2.2a |
| PALES_13081 | mexK | (RND) efflux transporter | 2.7 | 1.8a |
| PALES_13071 | mexJ | (RND) efflux membrane fusion protein | 2.7 | 1.0 |
| PALES_07201 | mexI | (RND) efflux transporter | 2.0 | 1.6 |
| PALES_49821 | oprJ | Multidrug efflux outer membrane protein | 10.8 | 24.0a |
| PALES_49831 | mexD | (RND) multidrug efflux transporter | 10.3 | 12.0a |
| PALES_49841 | mexC | (RND) multidrug efflux membrane fusion protein | 4.1 | 9.3a |
| PALES_43561 | oprD | Basic amino acid, basic peptide and imipenem outer membrane porin | −3.2 | −1.2 |
| Outer membrane/LPS | ||||
| PALES_20851 | murB | UDP-N-acetylenolpyruvoylglucosamine reductase | 1.6 | −1.0 |
| PALES_14811 | arnB | UDP-4-amino-4-deoxy-l-arabinose-oxoglutarate aminotransferase | 29.4 | 16.7a |
| PALES_14801 | arnC | Glycosyl transferase | 45.5 | 19.7a |
| PALES_14791 | arnA | Bifunctional UDP-glucuronic acid decarboxylase/UDP-4-amino-4-deoxy-l-arabinose formyltransferase | 45.1 | 16.8a |
| PALES_14781 | arnD | Olysaccharide deacetylase | 31.6 | 20.8a |
| PALES_14771 | arnT | 4-amino-4-deoxy-l-arabinose transferase | 92.1 | 8.8a |
| PALES_14761 | arnE | Inner membrane protein | 16.4 | 14.3a |
| PALES_14751 | arnF | Hypothetical protein | 92.3 | 38.3a |
| PALES_14741 | PALES_14741 | Nucleotide sugar dehydrogenase | 51.3 | 17.0a |
| PALES_50471 | pagL | Lipid A 3-O-deacylase | 2.6 | 2.3a |
| PALES_51611 | pmrA | Two-component regulator system response regulator | 21.3 | 14.3a |
| PALES_51621 | pmrB | Two-component regulator system signal sensor kinase | 17.8 | 16.2a |
| Periplasm/PMF | ||||
| PALES_41491 | napC | Cytochrome c-type protein | −2.0 | 1.3 |
| PALES_41481 | napB | Cytochrome c-type protein precursor | −1.5 | 1.3 |
| PALES_41471 | napA | Periplasmic nitrate reductase protein | −1.4 | −1.1 |
| PALES_41461 | napD | Protein of periplasmic nitrate reductase | −2.8 | 1.5 |
| PALES_41451 | napE | Periplasmic nitrate reductase protein | −1.5 | −1.2 |
| PALES_37731 | ccoP2 | Cytochrome c oxidase, cbb3-type, CcoP | −2.3 | 1.6 |
| PALES_37721 | ccoO2 | Cytochrome c oxidase, cbb3-type, CcoO | −2.6 | 1.4 |
| PALES_37711 | ccoN2 | Cytochrome c oxidase, cbb3-type, CcoN | −1.9 | 1.0 |
| PALES_49541 | PALES_49541 | Putative cytochrome c | −2.0 | −1.0 |
Denotes genes significantly differentially expressed in dual-species biofilms. All genes listed were significantly differentially expressed in mono-microbial biofilms.
When examining P. aeruginosa response to TM18 under dual-species biofilm conditions, the transcriptional response was less substantial, with only 48 genes significantly differentially expressed (Table S4, Fig. S5). Although there was a large overlap between the mono-species and dual-species response (Fig. S3), many key genes were no longer significantly differentially expressed (Table 2). Comparing the P. aeruginosa gene expression under dual-species conditions with S. aureus to mono-species conditions, it was evident that the presence of S. aureus primed P. aeruginosa by upregulating specific genes. This priming effect resulted in less pronounced dysregulation of gene expression but increased tolerance to environmental stressors and antimicrobial agents in dual-species environments. Specifically, these priming mechanisms included a strong upregulation of the aminoarabinose biosynthesis pathway, various efflux pump systems and the expression of porin proteins.
In contrast, treatment of S. aureus mono-species biofilms with TM18 caused the dysregulation of 665 genes (283 genes upregulated, 362 genes downregulated). This response reflects a more pronounced impact on S. aureus compared to P. aeruginosa, likely due to the high peptoid concentration, which may have induced cell death. The observed transcriptional changes included dysregulation in the expression of proteases and peptidases, with >2-fold downregulation of serine proteases and lysins, and >2-fold downregulation of the type VII secretion system. Additionally, genes associated with phosphate metabolism were >2-fold upregulated (Table 3). There was also a significant upregulation of genes involved in fatty acid synthesis and nicotinamide adenine dinucleotide (NAD) binding, which are crucial for redox reactions. Metabolic pathways, particularly those related to amino acid metabolism, were also significantly upregulated. Conversely, genes associated with adhesion and cell wall synthesis were predominantly downregulated (Fig. S6).
Table 3.
Differentially expressed genes for S. aureus mono-species biofilms treated with 32 μg/mL TM18, compared to dual-species biofilms. Fold change (FC) relative to untreated samples, with positive values indicating increased expression when treated with TM18.
| Loci | Gene | Description | FC mono-species biofilms |
FC dual-species biofilms |
|---|---|---|---|---|
| Protease/peptidase | ||||
| SAUSA300_1146 | hslV | ATP-dependent protease HslV | 2.0 | 1.4 |
| SAUSA300_1147 | hslU | ATP-dependent protease ATPase HslU | 1.7 | 1.3 |
| SAUSA300_1402 | SAUSA300_1402 | Clp protease ClpP | −1.6 | 1.7 |
| SAUSA300_1753 | splF | Serine protease SplF | −2.5 | 1.3 |
| SAUSA300_1754 | splE | Serine protease SplE | −2.5 | 1.1 |
| SAUSA300_1755 | splD | Serine protease SplD | −2.5 | −1.0 |
| SAUSA300_1756 | splC | Serine protease SplC | −2.5 | −2.0 |
| SAUSA300_1757 | splB | Serine protease SplB | −3.7 | −1.0 |
| SAUSA300_1758 | splA | Serine protease SplA | −3.5 | −2.3 |
| SAUSA300_1890 | scpA | Cysteine protease staphopain A | −1.9 | −1.3 |
| SAUSA300_0207 | SAUSA300_0207 | M23 family metallopeptidase | 5.7 | 4.3a |
| SAUSA300_0752 | clpP | ATP-dependent Clp endopeptidase proteolytic subunit | 1.6 | 1.4 |
| SAUSA300_1351 | SAUSA300_1351 | Zinc metallopeptidase | 1.6 | 2.1a |
| SAUSA300_1674 | SAUSA300_1674 | Trypsin-like peptidase domain-containing protein | 2.0 | 1.1 |
| SAUSA300_1691 | SAUSA300_1691 | M42 family metallopeptidase | 1.6 | 2.3a |
| SAUSA300_2381 | SAUSA300_2381 | C39 family peptidase | 2.3 | −1.4 |
| SAUSA300_2400 | SAUSA300_2400 | M42 family metallopeptidase | 1.6 | 1.1 |
| Phosphate metabolism | ||||
| SAUSA300_0145 | SAUSA300_0145 | Phosphate/phosphite/phosphonate ABC transporter substrate-binding protein | 1.5 | −1.1 |
| SAUSA300_0216 | uhpT | Hexose-6-phosphate:phosphate antiporter | −4.0 | −2.6a |
| SAUSA300_0360 | SAUSA300_0360 | Aminotransferase class I/II-fold pyridoxal phosphate-dependent enzyme | 2.0 | 1.5 |
| SAUSA300_1122 | plsX | Phosphate acyltransferase | 2.1 | −1.0 |
| SAUSA300_1279 | phoU | Phosphate signaling complex protein | 2.6 | 2.5a |
| SAUSA300_1280 | SAUSA300_1280 | Phosphate ABC transporter ATP-binding protein | 2.6 | 2.3a |
| SAUSA300_1281 | pstA | Phosphate ABC transporter permease | 2.8 | 2.3a |
| SAUSA300_1282 | pstC | Phosphate ABC transporter permease | 2.6 | 2.1a |
| SAUSA300_1283 | SAUSA300_1283 | Phosphate ABC transporter substrate-binding protein | 2.6 | 2.3a |
| Type VII secretion system | ||||
| SAUSA300_0278 | esxA | WXG100 family type VII secretion effector EsxA | −2.0 | 1.5 |
| SAUSA300_0279 | esaA | Type VII secretion protein EsaA | −3.0 | −2.6a |
| SAUSA300_0280 | essA | Type VII secretion protein EssA | −3.0 | −1.9a |
| SAUSA300_0281 | esaB | Type VII secretion protein EsaB | −1.9 | −1.7 |
| SAUSA300_0282 | essB | Type VII secretion protein EssB | −3.0 | −2.0a |
| SAUSA300_0283 | essC | Type VII secretion protein EssC | −2.5 | −1.5 |
| SAUSA300_0284 | esaC | Type VII secretion substrate EsaC | −2.5 | −1.3 |
| SAUSA300_0285 | esxB | WXG100 family type VII secretion effector EsxB | −2.0 | −1.3 |
| SAUSA300_2524 | SAUSA300_2524 | TIGR04197 family type VII secretion effector | −1.6 | −2.0a |
| Lysins | ||||
| SAUSA300_2365 | hlgA | Bi-component gamma-hemolysin HlgAB subunit A | −13.0 | −16.0a |
| SAUSA300_2366 | hlgC | Bi-component gamma-hemolysin HlgCB subunit C | −9.8 | −17.1a |
| SAUSA300_1058 | hyl | Alpha-hemolysin | −6.5 | −4.0a |
| SAUSA300_2367 | hlgB | Bi-component gamma-hemolysin HlgAB/HlgCB subunit B | −3.5 | −5.7a |
| SAUSA300_1988 | SAUSA300_1988 | Delta-lysin family phenol-soluble modulin | −3.0 | 1.0 |
| SAUSA300_0438 | aaa | Autolysin/adhesin Aaa | −2.5 | −1.7a |
| SAUSA300_2572 | aur | Zinc metalloproteinase aureolysin | −1.9 | 1.2 |
Denotes genes significantly differentially expressed in dual-species biofilms. All genes listed were significantly differentially expressed in mono-microbial biofilms.
Changes similar to those observed under mono-species conditions were found in dual-species biofilms (Table 3, Fig. S7). Interestingly, S. aureus treated with TM18 in a dual-species biofilm showed extensive dysregulation of genes, with approximately one-third of the genome significantly dysregulated (878 genes; 462 upregulated and 416 downregulated) (Table S5). Like the priming effect observed in P. aeruginosa, the dual-species environment primed S. aureus through the upregulation of various efflux pumps, including norAB, potentially increasing its tolerance to antimicrobial treatment. Notably, TM18 treatment caused downregulation of S. aureus infection-associated genes under mono- and dual-species conditions (Fig. S7).
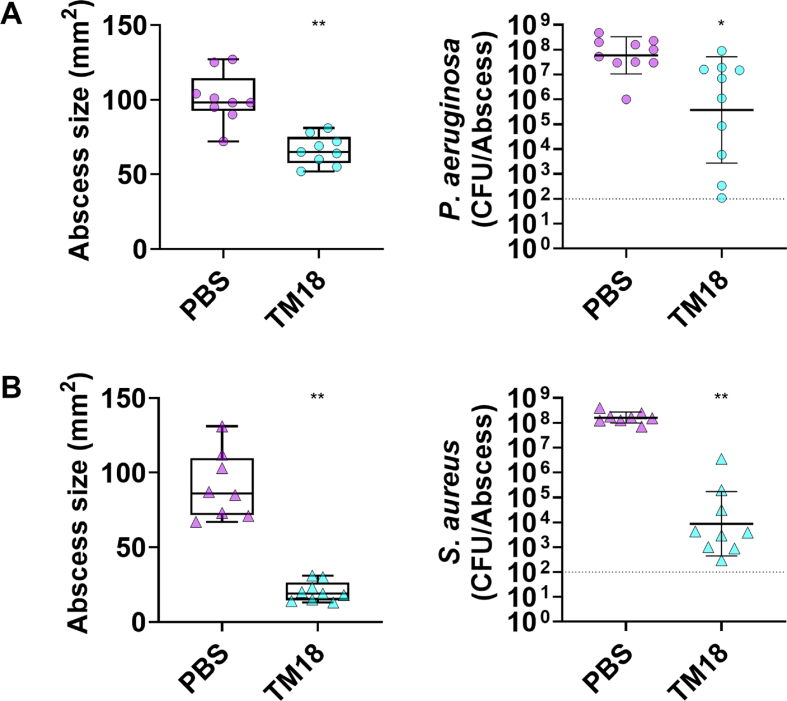
2.5. TM18 exhibited anti-abscess activity in a murine skin abscess model
Testing antimicrobial agents in vivo is crucial for understanding their efficacy in complex biological environments. While in vitro studies provide initial insights into the biological activities of compounds, they cannot fully replicate the host environment, including immune system interactions with pathogens and antimicrobial agents [35,36].
Given the remarkable in vitro activity of lipo-peptoid TM18, we explored its potential in a murine skin abscess model [37,38]. Prior to skin toxicity testing (Table S10), the cytotoxicity of each peptoid was assessed using L929 mouse fibroblast cells (Table S9). The lowest observed lethal dose 50 (LC50) was 50 μg/mL for TM11 and TM14, while all other peptoids exhibited LC50 values exceeding 100 μg/mL. Additionally, an in vivo dose of up to 5 mg/kg (equivalent to 125 μg per injection in a 25 g mouse) showed no detectable toxicity for TM14 and TM18.
Mice were infected with either P. aeruginosa or S. aureus and treated 1 h post-infection. Peptoid TM18 significantly reduced P. aeruginosa skin abscesses by 35% (Fig. 3A, left) and reduced bacterial survivors by >100-fold, although this reduction was not statistically significant (Fig. 3A, right). The activity of peptoid TM18 was compared to that of the established peptoid TM1. In comparison, peptoid TM1 reduced abscesses by 30%, but showed only minor bactericidal activity. TM14 was also tested but exhibited no anti-abscess activity in this model (Fig. S8A). Additionally, TM1 and TM18 prevented scabbing at the infection site (Fig. S9A).
Fig. 3.
In vivo activity of peptoid TM18 treatment in a high-density mono-species P. aeruginosa or S. aureus infection model. Female Swiss Webster mice were subcutaneously injected with 2.5 × 107 CFU of (A) P. aeruginosa LESB58, or (B) S. aureus USA300 LAC. One-hour post-infection, mice were treated intra-abscess with 125 μg (5 mg/kg) peptoid or PBS as a vehicle control. After three days, the mice were euthanized. Abscesses were measured, including the area of skin dermonecrosis, and collected for bacterial enumeration. Results are presented as median with whiskers indicating min and max values, or as geometric mean ± geometric SD. Statistical significance is denoted as ∗∗p < 0.01, according to Kruskal−Wallis test with Dunn's correction. Dashed line represents limit of detection.
In S. aureus infections, TM18 significantly reduced abscess sizes 78% (Fig. 3B, left), prevented scabbing (Fig. S9B), and reduced bacterial survivors by more than >10,000-fold (Fig. 3B, right). TM1 showed a significant reduction of abscesses by 45%, prevented scabbing, and significantly reduced bacterial survivors by over 100-fold. TM14 did not reduce abscesses but decreased scabbing by 50% and significantly reduced S. aureus survivors by ∼10-fold (Figure S8B, Figure S9B).
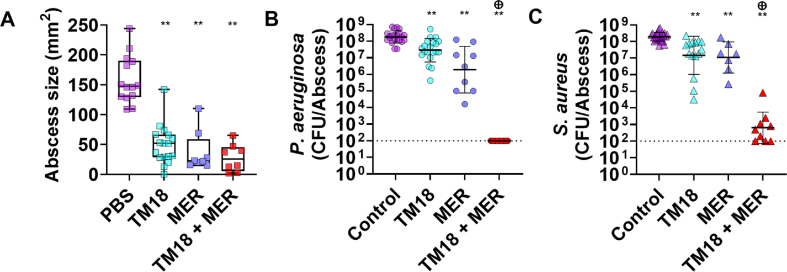
2.6. TM18 and meropenem as an effective combination therapy for treating complex skin abscess co-infections by P. aeruginosa and S. aureus
Combination therapy is critically important in the treatment of infectious diseases, particularly for combating multi-drug resistant pathogens and enhancing therapeutic efficacy [39]. The challenge of finding antibiotics effective against multiple pathogens underscores the need for combination approaches, as single-agent therapies often fail to address the diverse mechanisms of resistance and virulence exhibited by various bacterial species.
To test an effective antibiotic combination with TM18 in vivo, we first needed to identify an antibiotic that works equally well against both bacterial pathogens to avoid eradication of one bacterium over the other. Various antibiotics from different classes against P. aeruginosa LESB58 and S. aureus USA300 LAC were tested (Table S7). We found that tobramycin (MIC 1.56 μg/mL against P. aeruginosa, 0.78 μg/mL against S. aureus) and meropenem (MIC 1.56 μg/mL against P. aeruginosa, 0.78 μg/mL against S. aureus) had similar MICs against both strains (Table S6). Both antibiotics were then tested in combination with TM18 using a checkerboard synergy assay, showing additive effects against both strains (FICI 0.75–1) (Table S7).
Given the challenge of treating polymicrobial infections with conventional antibiotics [10,40,41], we further investigated meropenem and TM18 efficacy, individual and combined, using the P. aeruginosa and S. aureus dual-species in vivo infection model (Fig. 4). Individual treatments with TM18 and meropenem significantly reduced abscess sizes by 65% and 78%, respectively. The combination also reduced abscess sizes by 65% (Fig. 4A). However, in the co-infection model, TM18 lost some of its bactericidal activity against both P. aeruginosa and S. aureus, like the results obtained in the in vitro dual-species biofilm experiments (Fig. 1E and F), albeit still a significant reduction.
Fig. 4.
Peptoid TM18 synergizes with meropenem against P. aeruginosa and S. aureus co-infections in vivo. Female Swiss Webster mice were subcutaneously injected with 2.5 × 107 CFU of P. aeruginosa LESB58 and S. aureus USA300 LAC. After 1 h, mice were treated intra-abscess with 5 mg/kg of peptoid TM18, meropenem, 5 mg/kg, a combination of peptoid TM18 and meropenem, or vehicle (PBS) control. After three days, mice were euthanized, abscesses were measured and then collected for bacterial enumeration, and (A) skin dermonecrosis area was measured; (B) P. aeruginosa survivors, and (C) S. aureus survivors. Results are displayed as geometric mean ± geometric SD. ∗p < 0.05, ∗∗p < 0.01, according to Kruskal−Wallis test with Dunn's correction. Sum of CFU log reduction obtained for each single treatment and a Mann-Whitney test performed to compare PAE of the individual treatments to the CFU counts obtained by the drug combination ⊕ p =<0.05 is synergistic. Dashed line indicates limit of detection.
Meropenem alone significantly reduced abscess sizes by 85% and efficiently killed P. aeruginosa and S. aureus by ∼100- and 10-fold, respectively. Intriguingly, the combination of TM18 and meropenem not only significantly reduced abscess sizes but also reduced the bacterial burden of P. aeruginosa to the limit of detection (Fig. 4B) and reduced S. aureus bacterial burden to within 10-fold of the limit of detection (Fig. 4C). This effect was synergistic, highlighting the importance of testing for in vivo synergistic interactions. This also shows the strong potential of using peptoids in combination therapy with broad-spectrum antibiotics to effectively manage complex infections.
3. Discussion
The global burden of AMR is escalating, posing a significant threat to public health [42]. Given the urgent need for new antimicrobials, the ability to repurpose existing therapies and the development of new combination therapies to enhance efficacy and reduce resistance has become a promising approach to tackling antibiotic-resistant pathogens. Peptoids, a class of peptides resistant to proteases with increased biostability, potent antimicrobial activity, and low toxicity to human cells, have emerged as promising candidates for novel antimicrobial therapeutics [17,43].
Does the addition of a cationic NLys residue improve the antimicrobial activity of peptoids? The addition of NLys introduces a positive charge to the peptoid molecule, facilitating electrostatic interactions with the negatively charged bacterial membranes and promoting membrane disruption and subsequent bacterial lysis [44,45]. We hypothesized that the incorporation of an additional NLys molecule would enhance the bactericidal efficacy of peptoids and improve biofilm penetration. Using an iterative process to refine previously characterized antimicrobial peptoids (TM1-TM10), we found that the addition of a cationic NLys residue did not uniformly enhance the ability to combat priority pathogens. Our broad screen of ten peptoids with additional NLys residues revealed that the positive charge predominantly reduced efficacy against Gram-negative P. aeruginosa (Table 1) compared to previously published TM1-TM10 [17]. Three out of 10 peptoids exhibited a weak two-fold decrease in activity against P. aeruginosa, while the remaining peptoids displayed a two-fold increase. The activity against S. aureus remained largely unchanged, except for TM19, which showed a four-fold increase in efficacy. Hence, host-mimicking conditions in evaluating the true potential of antimicrobial agents are crucial, as they reveal nuances in efficacy that are not apparent in standard laboratory media [46].
Peptidomimetics also hold significant potential for development as an anti-biofilm drug compound [17,23,47]. To further explore the efficacy of our modified peptoids against biofilms formed by either bacterium alone or in co-culture, we conducted biofilm eradication experiments similar to those previously performed for TM1-TM10. Intriguingly, the addition of NLys enhanced anti-biofilm activity against P. aeruginosa while maintaining efficacy against S. aureus mono-species biofilms (Fig. 1). Most of the modified peptoids also retained their activity against dual-species biofilms formed by both pathogens. Notably, TM14 and TM18 demonstrated superior activity, effectively eradicating both bacteria within a dual-species biofilm. TM14 is particularly interesting because its parent compound, TM4, which features halogen substituents, did not exhibit anti-biofilm activity against P. aeruginosa in mono- or dual-species conditions. Similarly, lipo-peptoid TM18, an NLys-modified version of TM8, a lead candidate from our previous study [17], showed improved anti-biofilm activity against both mono- and dual-species biofilms of either pathogen. Remarkably, while the potential of NLys-modified peptoids was shown in previous research [45], our study is among the first to demonstrate such significant anti-biofilm efficacy in dual-species settings, underscoring the unique promise of these modifications in combating complex biofilm-associated infections.
We and others [48,49] highlight the significance of specific chemical modifications in enhancing the antimicrobial properties of peptoids, while also emphasizing the complexity of the chemical landscape and the influence of culture conditions on peptoid activity. The observed improvement in anti-biofilm activity against P. aeruginosa and the sustained efficacy against S. aureus suggest that NLys-modified peptoids could be a promising avenue for developing effective treatments against polymicrobial biofilms. This emphasizes the necessity for tailored approaches in peptoid design rather than generalizing modifications, also considering the propensity for self-assembly of peptoids with alkyl tails. We have previously shown that relatively small modifications in the chemical structure of lipo-peptoids can have dramatic effects on the self-assembly [17], including the critical aggregation concentration, aggregation number and morphology of self-assembled particles. However, in this case we observe that addition of one NLys group in TM18 has limited effect on the self-assembled particles when comparing to TM8.
Optimized peptoids as alternatives to other peptide-based antibiotics. The efficacy of TM18 in vitro and in vivo is comparable to clinically used peptide-based antibiotics like colistin and daptomycin. The MIC values of TM18 in both DFG and MHB are within two-fold range of colistin's activity against P. aeruginosa, while demonstrating strong activity against S. aureus, where colistin has no canonical activity [50]. Similarly, TM18's MIC is comparable to that of daptomycin in DFG, with the added advantage that TM18 retains activity against P. aeruginosa, unlike daptomycin [50]. These findings suggest that peptoids represent a promising class of broad-spectrum antimicrobials with potential advantages in treating complex polymicrobial infections.
The co-existence of P. aeruginosa and S. aureus primes both bacteria to become more tolerant towards antimicrobial compounds. Previous studies have shown that the presence of multiple bacterial species alters gene expression, leading to increased antibiotic tolerance [6]. Tognon et al. [51] demonstrated that co-infections under planktonic conditions result in significant metabolic changes in both organisms, specifically in nitrogen, amino acid and nucleotide metabolism. Briaud et al. [52] extended this by using RNA-Seq to show that S. aureus dysregulates 217 genes in the presence of P. aeruginosa, including genes involved in major metabolic pathways and energetic metabolism including dehydrogenases. These changes occur despite no differences in growth, suggesting a priming effect. Our biofilm studies corroborate these findings, showing similar dysregulation patterns, including dysregulation of metabolic pathways and efflux pumps (Table 2, Table 3), leading to antibiotic tolerance. In dual-species biofilms, S. aureus exhibits upregulation of efflux pumps, such as NorAB, which may protect it from P. aeruginosa-produced phenanzines that would otherwise inhibit its growth [53].
Furthermore, P. aeruginosa benefits from iron potentially released by S. aureus, thereby enhancing its survival in co-culture conditions [54]. This further supports the potential priming effect, which prepares bacteria to withstand future harsh conditions. Magalhaes et al. [55] found that P. aeruginosa in dual-species biofilms drives S. aureus into fermentation [56] and downregulates metabolic and peptidoglycan synthesis genes while upregulating membrane activity and carbon transport. Gene expression changes in P. aeruginosa were minimal, primarily affecting dehydrogenase activity. Miller et al. [57] observed that P. aeruginosa modulates only 0.3% of its genome in mixed biofilms, whereas S. aureus adjusts about 5%, leading to increased virulence and metabolic quiescence.
Our RNA-Seq analysis of bacterial biofilms grown under host-mimicking conditions revealed significant upregulation of the aminoarabinose biosynthesis pathway. This modification of the lipopolysaccharide (LPS) layer enhances resistance to cationic antimicrobial peptides and contributes to survival in hostile environments [58]. Additionally, there was a notable upregulation of efflux pump systems such as MexAB-OprM and MexXY-OprM, as well as porin proteins such as OprD that regulate membrane permeability. These changes suggest that P. aeruginosa is better equipped to survive in the presence of S. aureus by preemptively activating defense mechanisms that confer a higher level of tolerance and adaptability. Similarly, S. aureus upregulated several efflux pumps under dual-species conditions. Moreover, a widespread upregulation of oxidative stress response genes was observed in dual-species biofilms of both organisms compared to their respective mono-species biofilms. Increased ROS levels can lead to the modulation of resistance gene expression, increased mutation rates and enhanced horizontal gene transfer [59]. This further supports a priming mechanism and indicates enhanced tolerance to both host immune responses and antibiotic treatments.
Mechanisms of TM18 in the treatment of P. aeruginosa-S. aureus dual-species biofilms. We further investigated the mechanisms of TM18 at the molecular level to understand its efficacy against P. aeruginosa and S. aureus dual-species biofilms. We observed variable responses among peptoids in their ability to kill bacteria within biofilms under dual-species conditions (Fig. 1). Our RNA-seq data indicate that TM18 induces transcriptomic responses similar to those observed with conventional AMPs, demonstrating its potential as a novel AMP alternative. The similarities in bacterial responses do not necessarily indicate an identical mechanism of action, as AMP mechanisms remain diverse and not well-defined. Instead, for example, the upregulation of pmr and anr pathways aligns with general bacterial adaptations to cationic compounds rather than a specific AMP-associated mode of action.
Focusing on TM18 due to its superior activity against P. aeruginosa mono-species biofilms, we investigated its effects under both mono- and dual-species conditions. Interestingly, TM18 minimally impacted P. aeruginosa gene expression while significantly altering S. aureus gene expression. This aligns with our hypothesis that bacteria are primed under dual-species conditions, making TM18 more effective in mono-species settings but less so in dual-species ones. We observed dysregulation in efflux pumps, LPS and quorum sensing in P. aeruginosa, though expression levels were lower under dual-species conditions compared to mono-species ones. This suggests that P. aeruginosa biofilms, being three days old, were already more resistant/tolerant. Notably, TM18 treatment upregulated phenazine biosynthesis (Fig. S4), which is associated with increased antibiotic tolerance in P. aeruginosa biofilms [60]. However, this comes with a caveat: while phenazine production enhances attacks against S. aureus, it also inadvertently increases tolerance by upregulating efflux pumps. This dual effect complicates the overall impact of treating dual-species infections.
In contrast, gene expression analysis of S. aureus revealed extensive dysregulation in response to TM18 treatment, likely due to the high concentration used. We found significant dysregulation in proteases and peptidases, including an upregulation of HslV and ClpP, which are involved in stress response and protein degradation [61,62]. The downregulation of serine (Spl) proteases, which are associated with virulence and biofilm maintenance, suggests that TM18 disrupts S. aureus biofilm formation by targeting the expression of the spl operon, which warrants further investigations in the future. Additionally, there was a strong upregulation of other proteases, indicating that S. aureus senses the presence of the peptoid [63] but cannot degrade it due to its protease-resistant backbone structure. Other dysregulated pathways included phosphate metabolism, type VII secretion system as well as various lysins, indicating reduced virulence of S. aureus in the presence of TM18.
Enhanced treatment of complex biofilm-associated infections with TM18 and antibiotic combinations. Polymicrobial interactions are inherently complex [6] and are further complicated by the host immune system, which can reduce the efficacy of conventional antibiotics [25,64]. We explored the efficacy of TM18 in treating such infections, motivated by the promising mechanistic insights observed under dual-species biofilm conditions. TM18 demonstrated strong anti-abscess activity against mono-species P. aeruginosa and S. aureus infections, which was notable since TM8, lacking an additional NLys residue, was inactive against P. aeruginosa in this murine model [17]. Encouraged by these results, we tested TM18 in a dual-species infection model, where its activity was reduced, potentially due to the priming effect of the co-existence of these two bacteria. Nonetheless, TM18 showed similar activity to the carbapenem antibiotic meropenem used in this co-infection model.
Given these findings, we hypothesized that combining TM18 with an antibiotic might enhance its efficacy as previously shown for other peptides [37]. We identified meropenem, used to treat infections caused by P. aeruginosa, as a potential candidate. Meropenem is generally not the first choice for treating S. aureus infections, but it might be used in combination with other antibiotics in specific cases where mixed infections are present or when other options are limited. Meropenem is a broad-spectrum carbapenem antibiotic; a common resistance mechanism in P. aeruginosa involves the downregulation of the porin protein OprD, which facilitates meropenem entry into the cell [65]. In mono-species biofilms, TM18 treatment resulted in a downregulation of oprD, indicating that meropenem might not be effective in combinatorial treatment (consistent with our synergy experiments where we only found additive activity; Table S7). However, in dual-species biofilms, oprD downregulation was not observed, suggesting that the dual-species environment limits the ability of P. aeruginosa to modulate oprD expression. This led us to hypothesize a potential synergistic effect between TM18 and meropenem in dual-species environments, suggesting that the dual-species environment restricts the ability of P. aeruginosa to modulate oprD expression.
Remarkably, in vivo studies showed that dual-species infections were significantly reduced with the combination of TM18 and meropenem, demonstrating a strong synergistic effect against both P. aeruginosa and S. aureus (Fig. 4). Previous reports have shown that antimicrobial peptides can synergize with meropenem [66] and other antibiotics [67,68], highlighting the potential of combining peptidomimetics with conventional antibiotics to enhance efficacy. Our study is among the first to show near-complete eradication of high-density infections upon such treatment.
Our study presents promising results for the broad-spectrum activity of TM18, but there are several limitations to consider. While RNA-Seq analysis provided valuable insights into the gene expression changes induced by TM18, further studies are necessary to confirm these findings and fully elucidate the molecular mechanisms involved. Additionally, the potential for resistance development against peptides, peptoids, and lipo-peptoids has not been thoroughly investigated. Long-term studies assessing the risk of resistance emergence are crucial for evaluating the sustainability of peptoids as a treatment option. To translate our findings into clinical applications, large-scale clinical trials are required to evaluate the efficacy of TM18 in treating various types of infections, including those in different anatomical sites and patient populations. Moreover, developing effective delivery systems to target infection sites will be critical for maximizing its therapeutic benefits.
In conclusion, our study highlights the potential of NLys-modified peptoids as effective treatments against dual-species biofilms and antibiotic-resistant pathogens. TM18 showed promising activity against both P. aeruginosa and S. aureus. The addition of an NLys residue enhanced the antibiofilm properties of TM18, and the combination of TM18 with meropenem offers a potential strategy for treating complex biofilm-associated infections. Further studies are warranted to optimize the design of NLys-modified peptoids and to explore their mechanisms of action in more detail.
4. Materials and methods
4.1. Bacterial strains and growth conditions
Bacterial strains used in this study include P. aeruginosa LESB58 [69], PAO1 [70](Hancock lab; University of British Columbia), PA14 [71], and S. aureus USA300 LAC [72], Newman [73], and HG001 [74]. Strains were cultured in Lysogeny Broth (LB) or double Yeast Tryptone (dYT) for 16–24 h at 37 °C. Liquid cultures were grown with shaking at 250 rpm and growth was measured using a spectrophotometer (Eppendorf) at an absorbance OD600 (optical density 600 nm). Co-cultures were separated on selective agar plates: Pseudomonas cetrimide agar (Oxoid) to select for P. aeruginosa and 7.5 % NaCl plates to select for S. aureus as previously described [17].
4.2. Antimicrobial activity assay
Minimum inhibitory concentrations (MIC) were determined using an adapted broth microdilution method [75] in Greiner bio flat chimney polypropylene 96-well plates. P. aeruginosa was used at 1 × 106 CFU/mL and S. aureus at 5 × 106 CFU/mL in MHB (Oxoid) and DFG, respectively. A separate polypropylene plate was used to prepare two-fold peptoid dilutions in PBS pH 7.5 (Gibco). Bacterial growth was determined by visible turbidity after incubation at 37 °C for 16 h (S. aureus) or 24 h (P. aeruginosa). MIC values were determined as the lowest concentration of the drug where no bacterial growth was visible. Metabolic activity (color change from blue to pink) was further determined by adding the metabolic dye PrestoBlue™ (Invitrogen) to each well for 30 min as confirmation of visual determination. All tests were performed in triplicate.
4.3. Small angle X-ray scattering (SAXS)
SAXS experiments on peptoid TM18 was performed at ALS beamline 12.3.1 LBNL Berkeley, California, USA [76], with a detector distance of 2 m and X-ray wavelength of λ = 1.27 Å, covering a Q range of 0.009 Å−1 to 0.4 Å−1. The data set was calibrated to an absolute intensity scale using water as a primary standard. All experiments were performed at room temperature and data were processed as previously described [77]. The scattering data for TM18 was analyzed using a core-shell ellipsoidal model previously described in detail by Jensen et al. [78].
4.4. Biofilm growth conditions
Greiner bio flat chimney polypropylene 96-well plates were used to grow biofilms in host-mimicking media, consisting of Gibco Dulbecco's minimal Eagle's medium (DMEM; Thermo Fisher) supplemented with 5 % fetal bovine serum (FBS; NZ origin) and 1 % glucose (DFG). Briefly, bacteria were scraped from an overnight-grown plate, resuspended in PBS (Gibco, pH 7.4), and adjusted to a final CFU/mL in DFG broth: P. aeruginosa 1 × 107 CFU/mL and S. aureus 1 × 107 CFU/mL. For dual-species biofilms of P. aeruginosa and S. aureus a 1:1 ratio was used with 1 x 107 CFU/mL per species.
4.5. Biofilm eradication activity of peptoids
The biofilm eradication methodology was adapted from Nielsen et al. [17]. Mono-species and dual-species biofilms were grown for 20–24 h in DFG in 96-well microtiter plates as above. Biofilms were washed with PBS once and fresh DFG added to the wells. A separate polypropylene plate was used to prepare the two-fold peptoid dilutions. Subsequently, peptoids (dilutions or a 31.25 μg/mL fixed concentration) were added to the biofilm plate. A fixed concentration of 31.25 μg/mL was used as an antibiofilm concentration as it effectively reduced polymicrobial biofilms across all tested peptoids (Fig. S1) and aligns with our previous work on structurally related parent peptoids [17]. The treated plate was incubated for another 20–24 h at 37 °C. After incubation, plates were washed three times with PBS and stained with 0.1 % crystal violet (CV) (Sigma Aldrich) for 20–30 min with shaking at 150 RPM. Plates were washed with PBS three to five times to remove unbound CV. The remaining dye (i.e., biofilm mass) was dissolved in 70% EtOH for 20–30 min shaking at 150 RPM. The OD595 was measured with a plate reader (Thermo Scientific Varioskan® Flash).
For eradication experiments at a fixed concentration, biofilms were scraped from five technical replicate wells with a cotton swab, submerged in one mL of PBS, vortexed and used for serial dilutions. Dilutions were plated onto LB agar for mono-species biofilm survivors and selective agar plates for dual-species biofilms. After 24 h incubations, colonies were enumerated and presented as CFU/mL. Experiments were reproduced with at least three biological replicates.
4.6. Transcriptome sequencing (RNA-seq) of biofilms treated with peptoid TM18
To determine their transcriptomic responses to peptoid treatment, individual P. aeruginosa LESB58 or S. aureus USA300 LAC biofilms as well as dual-species biofilms using P. aeruginosa LESB58 and S. aureus USA300 (seeded at 1 × 107 CFU/mL) were grown on four hydroxyapatite (HA) [79] discs (0.5′ diameter x 0.04–0.15′ thick) (Clarkson Chromatography Products Inc.) submerged in DFG broth in a 6-well plate for 72 h. Medium was exchanged daily. Subsequently, biofilms were treated with either PBS or 32 μg/mL TM18 for 1 h. After treatment, three HA discs were submerged in RNAprotect® (QIAGEN) to extract RNA. HA discs were soaked in a lysostaphin 12.5 μg/mL (Biovendor), and lysozyme 500 μg/mL (Sigma Aldrich) TE buffer pH 8.0 (Invitrogen) solution during sonication for 5 min at 100% intensity (40 kHz, BactoSonic waterbath sonicator) and subsequently incubated at 37 °C for 1 h. RNA was isolated using the QIAGEN RNeasy kit, according to the manufacturer's protocol. A 1-h timepoint was chosen to show the early adaptive responses, as longer exposure increased bacterial killing (Fig. S10), especially for S. aureus. P. aeruginosa LESB58 and S. aureus USA300 were selected due to their co-existence in HA disc biofilms [50], while dual-species biofilms with P. aeruginosa PA14 or PAO1 led to rapid S. aureus killing (Fig. S11).
Four biological replicates were used to prepare RNAseq TruSeq stranded RNA libraries from rRNA-depleted RNA samples using a Zymo-Seq RiboFree total RNA library kit and sequenced as 100 bp single-end reads (average of 11 million reads per sample, Table S1) using an Illumina NextSeq2000 at the Otago Genomics Facility (Dunedin, New Zealand). Reads were trimmed using Trimmomatic v0.39 [80] and subsequently mapped using STAR v2.7.8a [81] to either Pseudomonas aeruginosa LESB58 (genome assembly accession ASM2664v1, GenBank assembly GCA_000026645.1 [82]) or Staphylococcus aureus USA300 FPR3757 (genome assembly accession ASM1346v1, GenBank assembly GCA_000013465.1 [83]). MultiQC v1.11 [84] was used to examine mapping statistics and read quality. Differential gene expression analyses were carried out with R version 4.3.1 [85], using DESeq2 v1.40.2 [86]. Significantly differentially expressed genes were only considered from genes with >1.5-fold change and a false discovery rate (FDR) adjusted p-value ≤0.05. Gene ontology (GO) enrichment analysis was carried out using clusterProfiler v4.8.3 [87], P. aeruginosa LESB58 gene ontology terms were obtained from pseudomonas.com [88], S. aureus USA300 LAC gene ontology terms were obtained from UniProtKB for taxonomic groups (taxonomy_id:367830) [89]. Significantly enriched terms from differentially expressed genes were plotted using gene ratio of the number of genes associated with the given ontology term, all plots were generated using ggplot2 v3.3.5 [90].
4.7. Checkerboard titration assays (in vitro synergy)
The synergy between TM18 and the antibiotics meropenem, tobramycin, ciprofloxacin, gentamicin, azithromycin, and ceftazidime (Sigma Aldrich) was determined using the checkerboard titration assay [91]. Each compound was serially diluted in PBS before transferring to a 96-well plate containing 1 × 106 CFU/mL P. aeruginosa or S. aureus, respectively, in DFG medium and incubated at 37 °C for 16–24 h. The MIC or combinatorial effect was determined as the lowest concentration with no visible growth and the fractional inhibitory concentration index (FICI) was calculated as [(MICA in combination)/MICA] + [(MICB in combination)/MICB] as previously [92]. FICIs ≤ 0.5 indicate synergy, 0.5–1 indicate additivity and values above 1 indicate indifference or antagonism.
4.8. Peptoid toxicity assay
Peptoid toxicity was determined using the Promega CytoTox® Non-Radioactive Cytotoxicity Assay Kit. Mouse fibroblast cells (L929 cells) were seeded into 96-well plates (Greiner Bio Cell) at 10,000 cells/well. Cells were grown for 24 h in Dulbecco's minimal Eagle's medium (DMEM) high glucose + 10% fetal bovine serum (Gibco) and 1% pen-strep (Gibco) at 37 °C with 5% CO2. After 24 h media was removed, and cells were treated with peptoids dissolved in PBS. LDH control wells and PBS control wells were used as 100% and 0% death controls, respectively. Lethal Concentration 50 (LC50) was determined as the lowest concentration of peptoid which induced a minimum of 50% cell death.
4.9. Study approval and animals
All animal experiments were conducted in adherence to the University of Otago Animal Ethics Committee under protocol number AUP19-125. For this study, female Swiss Webster mice, aged approximately 6–8 weeks were used. These mice were obtained from the University of Otago Biomedical Research Facility. They were housed in groups of five littermates.
4.10. Skin abscess model and treatment with peptoids
The abscess model was performed as described previously [37,38] for mono-species infections and modified as follows for dual-species infection. P. aeruginosa and S. aureus were grown individually to an OD600 of 1.0 in dYT broth. Bacterial cells were washed twice in PBS pH 7.4 (Gibco) and resuspended to an OD600 of 2.0 for S. aureus (∼2.5 × 107) and 1.0 for P. aeruginosa (∼2.5 × 107). For co-infections, P. aeruginosa and S. aureus were mixed (1:1) immediately before injecting 50 μL subcutaneously into the right side of the dorsum. TM1, TM14, TM18, or sterile PBS were injected directly into the infected area 1-h post-infection at a concentration of 5 mg/kg which was the highest concentration determined as non-toxic in our murine model (Table S10). The progression of the infection was monitored daily. A caliper was used to measure the abscess lesion size manually. The SilhouetteStar™ 3D wound camera and SilhouetteConnect™ software were used to photograph, measure, and analyze abscess lesion sizes (visible dermonecrosis). The skin abscesses (including accumulated pus) were excised and homogenized in sterile PBS using SPEX®SamplePrep 1600 MiniG™ for 5 min. Serial dilutions were plated on LB agar plates for mono-species infections and selective agar plates for co-infections. Bacterial numbers were enumerated after incubation for 16–24 h at 37 °C.
4.11. Statistical analysis
In vitro experiments were performed with at least three biological replicates. In vivo experiments were conducted with three biological replicates with at least three mice per group. Statistical analysis was performed using GraphPad Prism v9.5.0 (GraphPad Software, Boston, Massachusetts USA). A One-way ANOVA Kruskal-Wallis test with Dunn's correction was used for mono-species biofilms. A two-way ANOVA with post-hoc Dunnett's multiple correction test was utilized for dual-species biofilms. Data was considered significant when p-values were below 0.05 or 0.01 as indicated. The predicted additive effect (PAE) was determined by calculating the sum of CFU log reduction for each individual treatment. The Mann-Whitney test was then performed to compare the PAE with the CFU counts obtained from the drug combination. Synergy was defined as p ≤ 0.05 [37,93].
CRediT authorship contribution statement
Samuel J.T. Wardell: Writing – review & editing, Writing – original draft, Visualization, Software, Investigation, Formal analysis. Deborah B.Y. Yung: Visualization, Methodology, Investigation. Josefine E. Nielsen: Writing – review & editing, Investigation. Rajesh Lamichhane: Investigation. Kristian Sørensen: Resources, Investigation. Natalia Molchanova: Resources. Claudine Herlan: Resources. Jennifer S. Lin: Writing – review & editing, Resources. Stefan Bräse: Supervision. Lyn M. Wise: Writing – review & editing, Supervision, Funding acquisition. Annelise E. Barron: Writing – review & editing, Supervision, Resources. Daniel Pletzer: Writing – review & editing, Writing – original draft, Supervision, Resources, Project administration, Methodology, Funding acquisition, Conceptualization.
Data and materials availability
All data needed to evaluate the conclusions in the paper are present in the paper and/or the supplementary materials. Raw RNA-seq files are available under SRA accession number PRJNA1113372.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
-
•
Maurice Wilkins Centre for Molecular Biodiscovery MWC4064 (DP, LW)
-
•
Royal Society of New Zealand Marsden Fund MFP-UOO2203 (DP, LW, RL)
-
•
University of Otago Research Grant (DP)
-
•
Lotteries Health Postdoctoral Research fellowship, LHR-2023-215235 (SJTW)
-
•
University of Otago doctoral scholarship (DBYY)
-
•
NIH Director's Pioneer Award, 1DP1 OD029517 (AEB, KBS, JSL)
-
•
SENS Research Foundation, Stanford University's Discovery Innovation Fund, the Cisco University Research Program Fund, and the Silicon Valley Community Foundation, and Dr. James J. Truchard and the Truchard Foundation (AEB)
-
•
Novo Nordisk Foundation, and the Stanford Bio-X Program, NNF21OC0068675 (JEN)
Acknowledgments
We acknowledge Bianca Tawatao and Meg Vallabh for their initial assistance with the synergy experiments. We thank Shuying Wee for her help with the cytotoxicity assays. The SAXS experiments were conducted at the Advanced Light Source (ALS), a national user facility operated by Lawrence Berkeley National Laboratory on behalf of the Department of Energy, Office of Basic Energy Sciences, through the Integrated Diffraction Analysis Technologies (IDAT) program, supported by DOE Office of Biological and Environmental Research. Additional support comes from the National Institute of Health project ALS-ENABLE (P30 GM124169) and a High-End Instrumentation Grant S10OD018483. We thank Dr. Gregory Hura and Kathryn Burnett at ALS for support during the SAXS experiment. Work at the Molecular Foundry was supported by the Office of Science, Office of Basic Energy Sciences, of the U.S. Department of Energy under Contract No. DE-AC02-05CH11231. We gratefully acknowledge Dr. Michael Connolly and Dr. Behzad Rad at the Molecular Foundry for assistance with peptoid synthesis and sample preparation equipment.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bioflm.2025.100272.
Appendix A. Supplementary data
The following are the Supplementary data to this article.
Data availability
Raw RNAseq fastq files are available under SRA accession PRJNA1113372. A summary of mapping statistics is shown in Table S1. Pairwise comparisons of differentially expressed genes in mono-species P. aeruginosa and S. aureus biofilms treated with TM18 are shown in Tables S2 and S3. Differentially expressed genes in dual-species biofilms treated with TM18 for either P. aeruginosa or S. aureus are provided in Tables S4 and S5.
References
- 1.Jamal M., Ahmad W., Andleeb S., Jalil F., Imran M., Nawaz M.A., Hussain T., Ali M., Rafiq M., Kamil M.A. Bacterial biofilm and associated infections. J Chin Med Assoc. 2018;81:7–11. doi: 10.1016/j.jcma.2017.07.012. [DOI] [PubMed] [Google Scholar]
- 2.Donlan R.M. Biofilm formation: a clinically relevant microbiological process. Clin Infect Dis. 2001;33:1387–1392. doi: 10.1086/322972. [DOI] [PubMed] [Google Scholar]
- 3.Dayton H., Kiss J., Wei M., Chauhan S., LaMarre E., Cornell W.C., Morgan C.J., Janakiraman A., Min W., Tomer R., Price-Whelan A., Nirody J.A., Dietrich L.E.P. Cellular arrangement impacts metabolic activity and antibiotic tolerance in Pseudomonas aeruginosa biofilms. PLoS Biol. 2024;22 doi: 10.1371/journal.pbio.3002205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu H.Y., Prentice E.L., Webber M.A. Mechanisms of antimicrobial resistance in biofilms. NPJ Antimicrob Resist. 2024;2:27. doi: 10.1038/s44259-024-00046-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hall C.W., Mah T.F. Molecular mechanisms of biofilm-based antibiotic resistance and tolerance in pathogenic bacteria. FEMS Microbiol Rev. 2017;41:276–301. doi: 10.1093/femsre/fux010. [DOI] [PubMed] [Google Scholar]
- 6.Yung D.B.Y., Sircombe K.J., Pletzer D. Friends or enemies? The complicated relationship between Pseudomonas aeruginosa and Staphylococcus aureus. Mol Microbiol. 2021 doi: 10.1111/mmi.14699. [DOI] [PubMed] [Google Scholar]
- 7.Serra R., Grande R., Butrico L., Rossi A., Settimio U.F., Caroleo B., Amato B., Gallelli L., de Franciscis S. Chronic wound infections: the role of Pseudomonas aeruginosa and Staphylococcus aureus. Expert Rev Anti Infect Ther. 2015;13:605–613. doi: 10.1586/14787210.2015.1023291. [DOI] [PubMed] [Google Scholar]
- 8.Buch P.J., Chai Y., Goluch E.D. Treating polymicrobial infections in chronic diabetic wounds. Clin Microbiol Rev. 2019;32 doi: 10.1128/CMR.00091-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Magana M., Sereti C., Ioannidis A., Mitchell C.A., Ball A.R., Magiorkinis E., Chatzipanagiotou S., Hamblin M.R., Hadjifrangiskou M., Tegos G.P. Options and limitations in clinical investigation of bacterial biofilms. Clin Microbiol Rev. 2018;31 doi: 10.1128/CMR.00084-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nabb D.L., Song S., Kluthe K.E., Daubert T.A., Luedtke B.E., Nuxoll A.S. Polymicrobial interactions induce multidrug tolerance in Staphylococcus aureus through Energy depletion. Front Microbiol. 2019;10:2803. doi: 10.3389/fmicb.2019.02803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O'Brien T.J., Figueroa W., Welch M. Decreased efficacy of antimicrobial agents in a polymicrobial environment. ISME J. 2022;16:1694–1704. doi: 10.1038/s41396-022-01218-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ersoy S.C., Heithoff D.M., Barnes L.t., Tripp G.K., House J.K., Marth J.D., Smith J.W., Mahan M.J. Correcting a fundamental flaw in the paradigm for antimicrobial susceptibility testing. EBioMedicine. 2017;20:173–181. doi: 10.1016/j.ebiom.2017.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Orazi G., O'Toole G.A. "It takes a village": mechanisms underlying antimicrobial recalcitrance of polymicrobial biofilms. J Bacteriol. 2019;202 doi: 10.1128/JB.00530-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dostert M., Belanger C.R., Hancock R.E.W. Design and assessment of anti-biofilm peptides: steps toward clinical application. J Innate Immun. 2019;11:193–204. doi: 10.1159/000491497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haney E.F., Straus S.K., Hancock R.E.W. Reassessing the host defense peptide landscape. Front Chem. 2019;7:43. doi: 10.3389/fchem.2019.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huan Y., Kong Q., Mou H., Yi H. Antimicrobial peptides: classification, design, application and research progress in multiple fields. Front Microbiol. 2020;11 doi: 10.3389/fmicb.2020.582779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nielsen J.E., Alford M.A., Yung D.B.Y., Molchanova N., Fortkort J.A., Lin J.S., Diamond G., Hancock R.E.W., Jenssen H., Pletzer D., Lund R., Barron A.E. Self-assembly of antimicrobial peptoids impacts their biological effects on ESKAPE bacterial pathogens. ACS Infect Dis. 2022;8:533–545. doi: 10.1021/acsinfecdis.1c00536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li Petri G., Di Martino S., Rosa De, Peptidomimetics M. An overview of recent medicinal chemistry efforts toward the discovery of novel small molecule inhibitors. J Med Chem. 2022;65:7438–7475. doi: 10.1021/acs.jmedchem.2c00123. [DOI] [PubMed] [Google Scholar]
- 19.Lenci E., Trabocchi A. Peptidomimetic toolbox for drug discovery. Chem Soc Rev. 2020;49:3262–3277. doi: 10.1039/d0cs00102c. [DOI] [PubMed] [Google Scholar]
- 20.Park M., Jardetzky T.S., Barron A.E. NMEGylation: a novel modification to enhance the bioavailability of therapeutic peptides. Biopolymers. 2011;96:688–693. doi: 10.1002/bip.21607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sanborn T.J., Wu C.W., Zuckermann R.N., Barron A.E. Extreme stability of helices formed by water-soluble poly-N-substituted glycines (polypeptoids) with alpha-chiral side chains. Biopolymers. 2002;63:12–20. doi: 10.1002/bip.1058. [DOI] [PubMed] [Google Scholar]
- 22.Brandt W., Herberg T., Wessjohann L. Systematic conformational investigations of peptoids and peptoid-peptide chimeras. Biopolymers. 2011;96:651–668. doi: 10.1002/bip.21620. [DOI] [PubMed] [Google Scholar]
- 23.Gomes Von Borowski R., Gnoatto S.C.B., Macedo A.J., Gillet R. Promising antibiofilm activity of peptidomimetics. Front Microbiol. 2018;9:2157. doi: 10.3389/fmicb.2018.02157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kapoor R., Wadman M.W., Dohm M.T., Czyzewski A.M., Spormann A.M., Barron A.E. Antimicrobial peptoids are effective against Pseudomonas aeruginosa biofilms. Antimicrob Agents Chemother. 2011;55:3054–3057. doi: 10.1128/AAC.01516-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li J., Xie S., Ahmed S., Wang F., Gu Y., Zhang C., Chai X., Wu Y., Cai J., Cheng G. Antimicrobial activity and resistance: influencing factors. Front Pharmacol. 2017;8:364. doi: 10.3389/fphar.2017.00364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pulkkinen K., Pekkala N., Ashrafi R., Hamalainen D.M., Nkembeng A.N., Lipponen A., Hiltunen T., Valkonen J.K., Taskinen J. Effect of resource availability on evolution of virulence and competition in an environmentally transmitted pathogen. FEMS Microbiol Ecol. 2018;94 doi: 10.1093/femsec/fiy060. [DOI] [PubMed] [Google Scholar]
- 27.Lee J., Kang D., Choi J., Huang W., Wadman M., Barron A.E., Seo J. Effect of side chain hydrophobicity and cationic charge on antimicrobial activity and cytotoxicity of helical peptoids. Bioorg Med Chem Lett. 2018;28:170–173. doi: 10.1016/j.bmcl.2017.11.034. [DOI] [PubMed] [Google Scholar]
- 28.Chongsiriwatana N.P., Patch J.A., Czyzewski A.M., Dohm M.T., Ivankin A., Gidalevitz D., Zuckermann R.N., Barron A.E. Peptoids that mimic the structure, function, and mechanism of helical antimicrobial peptides. Proc Natl Acad Sci U S A. 2008;105:2794–2799. doi: 10.1073/pnas.0708254105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhao W., Lin J.S., Nielsen J.E., Sorensen K., Wadurkar A.S., Ji J., Barron A.E., Nangia S., Libera M.R. Supramolecular peptoid structure strengthens complexation with polyacrylic acid microgels. Biomacromolecules. 2024;25:1274–1281. doi: 10.1021/acs.biomac.3c01242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lin J.S., Bekale L.A., Molchanova N., Nielsen J.E., Wright M., Bacacao B., Diamond G., Jenssen H., Santa Maria P.L., Barron A.E. Anti-persister and anti-biofilm activity of self-assembled antimicrobial peptoid ellipsoidal micelles. ACS Infect Dis. 2022;8:1823–1830. doi: 10.1021/acsinfecdis.2c00288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shen Y., Qian W., Chung C., Olsen I., Haapasalo M. Evaluation of the effect of two chlorhexidine preparations on biofilm bacteria in vitro: a three-dimensional quantitative analysis. J Endod. 2009;35:981–985. doi: 10.1016/j.joen.2009.04.030. [DOI] [PubMed] [Google Scholar]
- 32.Wang D., Haapasalo M., Gao Y., Ma J., Shen Y. Antibiofilm peptides against biofilms on titanium and hydroxyapatite surfaces. Bioact Mater. 2018;3:418–425. doi: 10.1016/j.bioactmat.2018.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moskowitz S.M., Ernst R.K., Miller S.I. PmrAB, A two-component regulatory system of Pseudomonas aeruginosa that modulates resistance to cationic antimicrobial peptides and addition of aminoarabinose to lipid A. J Bacteriol. 2004;186:575–579. doi: 10.1128/JB.186.2.575-579.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Breazeale S.D., Ribeiro A.A., McClerren A.L., Raetz C.R. A formyltransferase required for polymyxin resistance in Escherichia coli and the modification of lipid A with 4-Amino-4-deoxy-L-arabinose. Identification and function oF UDP-4-deoxy-4-formamido-L-arabinose. J Biol Chem. 2005;280:14154–14167. doi: 10.1074/jbc.M414265200. [DOI] [PubMed] [Google Scholar]
- 35.Righi E., Scudeller L., Chiamenti M., Abdelraouf K., Lodise T., Carrara E., Savoldi A., Menghin D., Pellizzari G., Ellis S., Franceschi F., Piddock L., Rebuffi C., Sanguinetti M., Tacconelli E. In vivo studies on antibiotic combination for the treatment of carbapenem-resistant Gram-negative bacteria: a systematic review and meta-analysis protocol. BMJ Open Sci. 2020;4 doi: 10.1136/bmjos-2019-100055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shi D., Mi G., Wang M., Webster T.J. In vitro and ex vivo systems at the forefront of infection modeling and drug discovery. Biomaterials. 2019;198:228–249. doi: 10.1016/j.biomaterials.2018.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pletzer D., Mansour S.C., Hancock R.E.W. Synergy between conventional antibiotics and anti-biofilm peptides in a murine, sub-cutaneous abscess model caused by recalcitrant ESKAPE pathogens. PLoS Pathog. 2018;14 doi: 10.1371/journal.ppat.1007084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pletzer D., Mansour S.C., Wuerth K., Rahanjam N., Hancock R.E. New mouse model for chronic infections by gram-negative bacteria enabling the study of anti-infective efficacy and host-microbe interactions. mBio. 2017;8 doi: 10.1128/mBio.00140-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lyons N., Wu W., Jin Y., Lamont I.L., Pletzer D. Using host-mimicking conditions and a murine cutaneous abscess model to identify synergistic antibiotic combinations effective against Pseudomonas aeruginosa. Front Cell Infect Microbiol. 2024;14 doi: 10.3389/fcimb.2024.1352339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Anju V.T., Busi S., Imchen M., Kumavath R., Mohan M.S., Salim S.A., Subhaswaraj P., Dyavaiah M. Polymicrobial infections and biofilms: clinical significance and eradication strategies. Antibiotics. 2022;11 doi: 10.3390/antibiotics11121731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ghuneim L.J., Raghuvanshi R., Neugebauer K.A., Guzior D.V., Christian M.H., Schena B., Feiner J.M., Castillo-Bahena A., Mielke J., McClelland M., Conrad D., Klapper I., Zhang T., Quinn R.A. Complex and unexpected outcomes of antibiotic therapy against a polymicrobial infection. ISME J. 2022;16:2065–2075. doi: 10.1038/s41396-022-01252-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Organization W.H. Antimicrobial resistance. 2024. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
- 43.Chongsiriwatana N.P., Lin J.S., Kapoor R., Wetzler M., Rea J.A.C., Didwania M.K., Contag C.H., Barron A.E. Intracellular biomass flocculation as a key mechanism of rapid bacterial killing by cationic, amphipathic antimicrobial peptides and peptoids. Sci Rep. 2017;7 doi: 10.1038/s41598-017-16180-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nyembe P.L., Ntombela T., Makatini M.M. Review: structure-activity relationship of antimicrobial peptoids. Pharmaceutics. 2023;15 doi: 10.3390/pharmaceutics15051506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mojsoska B., Zuckermann R.N., Jenssen H. Structure-activity relationship study of novel peptoids that mimic the structure of antimicrobial peptides. Antimicrob Agents Chemother. 2015;59:4112–4120. doi: 10.1128/AAC.00237-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Diamond G., Yim S., Rigo I., McMahon L. Measuring antimicrobial peptide activity on epithelial surfaces in cell culture. Methods Mol Biol. 2010;618:371–382. doi: 10.1007/978-1-60761-594-1_23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kapoor R., Wadman M.W., Dohm M.T., Czyzewski A.M., Spormann A.M., Barron A.E. Antimicrobial peptoids are effective against Pseudomonas aeruginosa biofilms. Antimicrob Agents Chemother. 2011;55:3054–3057. doi: 10.1128/AAC.01516-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gan B.H., Gaynord J., Rowe S.M., Deingruber T., Spring D.R. The multifaceted nature of antimicrobial peptides: current synthetic chemistry approaches and future directions. Chem Soc Rev. 2021;50:7820–7880. doi: 10.1039/d0cs00729c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bicker K.L., Cobb S.L. Recent advances in the development of anti-infective peptoids. Chem Commun. 2020;56:11158–11168. doi: 10.1039/d0cc04704j. [DOI] [PubMed] [Google Scholar]
- 50.Wardell S.J.T., Yung D.B.Y., Gupta A., Bostina M., Overhage J., Hancock R.E.W., Pletzer D. DJK-5, an anti-biofilm peptide, increases Staphylococcus aureus sensitivity to colistin killing in co-biofilms with Pseudomonas aeruginosa. NPJ Biofilms Microbiomes. 2025;11:8. doi: 10.1038/s41522-024-00637-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tognon M., Kohler T., Luscher A., van Delden C. Transcriptional profiling of Pseudomonas aeruginosa and Staphylococcus aureus during in vitro co-culture. BMC Genom. 2019;20:30. doi: 10.1186/s12864-018-5398-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Briaud P., Camus L., Bastien S., Doleans-Jordheim A., Vandenesch F., Moreau K. Coexistence with Pseudomonas aeruginosa alters Staphylococcus aureus transcriptome, antibiotic resistance and internalization into epithelial cells. Sci Rep. 2019;9 doi: 10.1038/s41598-019-52975-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fu T., Cai Z., Yue Z., Yang H., Fang B., Zhang X., Fan Z., Pan X., Yang F., Jin Y., Cheng Z., Wu W., Sun B., Huigens R.W., 3rd, Yang L., Bai F. Evolution of resistance to phenazine antibiotics in Staphylococcus aureus and its role during coinfection with Pseudomonas aeruginosa. ACS Infect Dis. 2021;7:636–649. doi: 10.1021/acsinfecdis.0c00837. [DOI] [PubMed] [Google Scholar]
- 54.Mashburn L.M., Jett A.M., Akins D.R., Whiteley M. Staphylococcus aureus serves as an iron source for Pseudomonas aeruginosa during in vivo coculture. J Bacteriol. 2005;187:554–566. doi: 10.1128/JB.187.2.554-566.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Magalhaes A.P., Franca A., Pereira M.O., Cerca N. Unveiling Co-infection in cystic fibrosis airways: transcriptomic analysis of Pseudomonas aeruginosa and Staphylococcus aureus dual-species biofilms. Front Genet. 2022;13 doi: 10.3389/fgene.2022.883199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Filkins L.M., Graber J.A., Olson D.G., Dolben E.L., Lynd L.R., Bhuju S., O'Toole G.A. Coculture of Staphylococcus aureus with Pseudomonas aeruginosa drives S. aureus towards fermentative metabolism and reduced viability in a cystic fibrosis model. J Bacteriol. 2015;197:2252–2264. doi: 10.1128/JB.00059-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Miller C.L., Van Laar T.A., Chen T., Karna S.L.R., Chen P., You T., Leung K.P. Global transcriptome responses including small RNAs during mixed-species interactions with methicillin-resistant Staphylococcus aureus and Pseudomonas aeruginosa. Microbiology (Road Town, V I (Br)) 2017;6 doi: 10.1002/mbo3.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Simpson B.W., Trent M.S. Pushing the envelope: LPS modifications and their consequences. Nat Rev Microbiol. 2019;17:403–416. doi: 10.1038/s41579-019-0201-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Qi W., Jonker M.J., de Leeuw W., Brul S., Ter Kuile B.H. Reactive oxygen species accelerate de novo acquisition of antibiotic resistance in E. coli. iScience. 2023;26 doi: 10.1016/j.isci.2023.108373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schiessl K.T., Hu F., Jo J., Nazia S.Z., Wang B., Price-Whelan A., Min W., Dietrich L.E.P. Phenazine production promotes antibiotic tolerance and metabolic heterogeneity in Pseudomonas aeruginosa biofilms. Nat Commun. 2019;10:762. doi: 10.1038/s41467-019-08733-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jeong S., Ahn J., Kwon A.R., Ha N.C. Cleavage-dependent activation of ATP-dependent protease HslUV from Staphylococcus aureus. Mol Cells. 2020;43:694–704. doi: 10.14348/molcells.2020.0074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Michel A., Agerer F., Hauck C.R., Herrmann M., Ullrich J., Hacker J., Ohlsen K. Global regulatory impact of ClpP protease of Staphylococcus aureus on regulons involved in virulence, oxidative stress response, autolysis, and DNA repair. J Bacteriol. 2006;188:5783–5796. doi: 10.1128/JB.00074-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kolar S.L., Ibarra J.A., Rivera F.E., Mootz J.M., Davenport J.E., Stevens S.M., Horswill A.R., Shaw L.N. Extracellular proteases are key mediators of Staphylococcus aureus virulence via the global modulation of virulence-determinant stability. Microbiology (Road Town, V I (Br)) 2013;2:18–34. doi: 10.1002/mbo3.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pirofski L.A., Casadevall A. Antimicrobial therapy in the context of the damage-response framework: the prospect of optimizing therapy by reducing host damage. Antimicrob Agents Chemother. 2020;64 doi: 10.1128/AAC.01800-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Li H., Luo Y.F., Williams B.J., Blackwell T.S., Xie C.M. Structure and function of OprD protein in Pseudomonas aeruginosa: from antibiotic resistance to novel therapies. Int J Med Microbiol. 2012;302:63–68. doi: 10.1016/j.ijmm.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Martinez M., Goncalves S., Felicio M.R., Maturana P., Santos N.C., Semorile L., Hollmann A., Maffia P.C. Synergistic and antibiofilm activity of the antimicrobial peptide P5 against carbapenem-resistant Pseudomonas aeruginosa. Biochim Biophys Acta Biomembr. 2019;1861:1329–1337. doi: 10.1016/j.bbamem.2019.05.008. [DOI] [PubMed] [Google Scholar]
- 67.Duong L., Gross S.P., Siryaporn A. Developing antimicrobial synergy with AMPs. Front Med Technol. 2021;3 doi: 10.3389/fmedt.2021.640981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kampshoff F., Willcox M.D.P., Dutta D. A pilot study of the synergy between two antimicrobial peptides and two common antibiotics. Antibiotics. 2019;8 doi: 10.3390/antibiotics8020060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cheng K., Smyth R.L., Govan J.R., Doherty C., Winstanley C., Denning N., Heaf D.P., van Saene H., Hart C.A. Spread of beta-lactam-resistant Pseudomonas aeruginosa in a cystic fibrosis clinic. Lancet. 1996;348:639–642. doi: 10.1016/S0140-6736(96)05169-0. [DOI] [PubMed] [Google Scholar]
- 70.Hancock R.E.W., Carey A.M. Outer membrane of Pseudomonas aeruginosa: heat- 2-mercaptoethanol-modifiable proteins. J Bacteriol. 1979;140(3):902–910. doi: 10.1128/jb.140.3.902-910.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.He J., Baldini R.L., Deziel E., Saucier M., Zhang Q., Liberati N.T., Lee D., Urbach J., Goodman H.M., Rahme L.G. The broad host range pathogen Pseudomonas aeruginosa strain PA14 carries two pathogenicity islands harboring plant and animal virulence genes. Proc Natl Acad Sci U S A. 2004;101:2530–2535. doi: 10.1073/pnas.0304622101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Centers for Disease, C. & Prevention Outbreaks of community-associated methicillin-resistant Staphylococcus aureus skin infections--Los Angeles County, California, 2002-2003. MMWR Morb Mortal Wkly Rep. 2003;52:88. [PubMed] [Google Scholar]
- 73.Duthie E.S., Lorenz L.L. Staphylococcal coagulase; mode of action and antigenicity. J Gen Microbiol. 1952;6:95–107. doi: 10.1099/00221287-6-1-2-95. [DOI] [PubMed] [Google Scholar]
- 74.Herbert S., Ziebandt A.K., Ohlsen K., Schafer T., Hecker M., Albrecht D., Novick R., Gotz F. Repair of global regulators in Staphylococcus aureus 8325 and comparative analysis with other clinical isolates. Infect Immun. 2010;78:2877–2889. doi: 10.1128/IAI.00088-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wiegand I., Hilpert K., Hancock R.E. Agar and broth dilution methods to determine the minimal inhibitory concentration (MIC) of antimicrobial substances. Nat Protoc. 2008;3:163–175. doi: 10.1038/nprot.2007.521. [DOI] [PubMed] [Google Scholar]
- 76.Classen S., Hura G.L., Holton J.M., Rambo R.P., Rodic I., McGuire P.J., Dyer K., Hammel M., Meigs G., Frankel K.A., Tainer J.A. Implementation and performance of SIBYLS: a dual endstation small-angle X-ray scattering and macromolecular crystallography beamline at the Advanced Light Source. J Appl Crystallogr. 2013;46:1–13. doi: 10.1107/S0021889812048698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hura G.L., Menon A.L., Hammel M., Rambo R.P., Poole F.L., 2nd, Tsutakawa S.E., Jenney F.E., Jr., Classen S., Frankel K.A., Hopkins R.C., Yang S.J., Scott J.W., Dillard B.D., Adams M.W., Tainer J.A. Robust, high-throughput solution structural analyses by small angle X-ray scattering (SAXS) Nat Methods. 2009;6:606–612. doi: 10.1038/nmeth.1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Jensen G.V., Lund R., Gummel J., Narayanan T., Pedersen J.S. Monitoring the transition from spherical to polymer-like surfactant micelles using small-angle X-ray scattering. Angew Chem Int Ed Engl. 2014;53:11524–11528. doi: 10.1002/anie.201406489. [DOI] [PubMed] [Google Scholar]
- 79.Gonçalves da Costa Sousa M., Conceição de Almeida G., Martins Mota D.C., Andrade da Costa R., Dias S.C., Limberger S.N., Ko F., Lin L.T., Haney E.F., Etayash H., Baquir B., Trimble M.J., Shen Y., Su Z., Haapasalo M., Pletzer D., Chaves de Souza L., Schuindt Teixeira G., Silva R.M., Hancock R.E.W., Franco O.L., Berto Rezende T.M. Antibiofilm and immunomodulatory resorbable nanofibrous filing for dental pulp regenerative procedures. Bioact Mater. 2022 doi: 10.1016/j.bioactmat.2022.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bolger A.M., Lohse M., Usadel B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics. 2014;30:2114–2120. doi: 10.1093/bioinformatics/btu170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Dobin A., Davis C.A., Schlesinger F., Drenkow J., Zaleski C., Jha S., Batut P., Chaisson M., Gingeras T.R. STAR: ultrafast universal RNA-seq aligner. Bioinformatics. 2013;29:15–21. doi: 10.1093/bioinformatics/bts635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Winstanley C., Langille M.G.I., Fothergill J.L., Kukavica-Ibrulj I., Paradis-Bleau C., Sanschagrin F., Thomson N.R., Winsor G.L., Quail M.A., Lennard N., Bignell A., Clarke L., Seeger K, Saunders D., Harris D., Parkhill J., Hancock R.E.W., Brinkman F.S.L., Levesque R.C. Newly introduced genomic prophage islands are critical determinants of in vivo competitiveness in the Liverpool Epidemic Strain of Pseudomonas aeruginosa. Genome Res. 2009;19:12–23. doi: 10.1101/gr.086082.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Diep B.A., Gill S.R., Chang R.F., Phan T.H., Chen J.H., Davidson M.G., Lin F., Lin J., Carleton H.A., Mongodin E.F., Sensabaugh G.F., Perdreau-Remington F. Complete genome sequence of USA300, an epidemic clone of community-acquired meticillin-resistant Staphylococcus aureus. Lancet. 2006;367(9512):731–739. doi: 10.1016/S0140-6736(06)68231-7. [DOI] [PubMed] [Google Scholar]
- 84.Ewels P., Magnusson M., Lundin S., Kaller M. MultiQC: summarize analysis results for multiple tools and samples in a single report. Bioinformatics. 2016;32:3047–3048. doi: 10.1093/bioinformatics/btw354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.R: a language and environment for statistical computing v. 3.4.3. R Foundation for Statistical Computing; Vienna, Austria: 2017. [Google Scholar]
- 86.Love M.I., Huber W., Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014;15:550. doi: 10.1186/s13059-014-0550-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wu T., Hu E., Xu S., Chen M., Guo P., Dai Z., Feng T., Zhou L., Tang W., Zhan L., Fu X., Liu S., Bo X., Yu G. clusterProfiler 4.0: a universal enrichment tool for interpreting omics data. Innovation. 2021;2 doi: 10.1016/j.xinn.2021.100141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Winsor G.L., Griffiths E.J., Lo R., Dhillon B.K., Shay J.A., Brinkman F.S.L. Enhanced annotations and features for comparing thousands of Pseudomonas genomes in the Pseudomonas genome database. Nucleic Acids Research. 2016;44:D646–D653. doi: 10.1093/nar/gkv1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.The UniProt Consortium UniProt: the Universal Protein Knowledgebase in 2025. Nucleic Acids Research. 2025;53:D609–D617. doi: 10.1093/nar/gkae1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wickham H. Springer-Verlag; New York: 2016. ggplot2: elegant graphics for data analysis. [Google Scholar]
- 91.Berenbaum M.C. A method for testing for synergy with any number of agents. J Infect Dis. 1978;137:122–130. doi: 10.1093/infdis/137.2.122. [DOI] [PubMed] [Google Scholar]
- 92.Odds F.C. Synergy, antagonism, and what the chequerboard puts between them. J Antimicrob Chemother. 2003;52:1. doi: 10.1093/jac/dkg301. [DOI] [PubMed] [Google Scholar]
- 93.Maset R.G., Hapeshi A., Lapage J., Harrington N., Littler J., Perrier S., Harrison F. Combining SNAPs with antibiotics shows enhanced synergistic efficacy against S. aureus and P. aeruginosa biofilms. NPJ Biofilms and Microbiomes. 2023;9:36. doi: 10.1038/s41522-023-00401-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Raw RNAseq fastq files are available under SRA accession PRJNA1113372. A summary of mapping statistics is shown in Table S1. Pairwise comparisons of differentially expressed genes in mono-species P. aeruginosa and S. aureus biofilms treated with TM18 are shown in Tables S2 and S3. Differentially expressed genes in dual-species biofilms treated with TM18 for either P. aeruginosa or S. aureus are provided in Tables S4 and S5.