Abstract
Background
Oral submucous fibrosis (OSMF) is a chronic, irreversible collagen metabolic disorder resulting in progressive reduction of mouth opening due to submucosal fibrosis. Currently, the benefit of interincisal mouth opening (IMO) has been attributed to physical therapy. This meta-analysis aimed to find evidence about effectiveness of physiotherapy in increasing of IMO.
Method
Literature search was conducted in Scopus, Web of Science, and PubMed databases using "Oral submucous fibrosis", "OSMF", "OSF”, “treatment”, “treatment modalities", "physiotherapy devices", “mouth opening exercise device”, “mouth opening”, “mouth opening device”, and "physiotherapy" search terms to find the relevant studies published till March 2024. Studies evaluating the effectiveness of physiotherapy alone or in combination in improvement of IMO pre-post intervention in OSMF patients were included. Random-effect analysis was carried out to obtain the pooled IMO. Heterogeneity and publication bias was assessed using the I2 and funnel plot. The main outcome variable was increase in IMO which was measured on linear scale.
Results
20 studies included in meta-analysis. Physiotherapy alone was found to be effective in improving IMO (4 studies; MD 1.19 [0.18, 2.20]). Further, addition of physiotherapy along with ultrasound (US) (3 studies; MD 3.96 [1.50, 6.42]), medicinal therapy including herbal (13 studies; MD 8.35 [5.18, 11.51]) and surgery (8 studies; MD 21.84 [18.29, 25.38]) improves the IMO.
Conclusion
There is evidence of effectiveness of physiotherapy in improving the IMO. However, evidence need to be substantiated with stringent methodology which is lacking in most of studies.
Keywords: Oral submucous fibrosis, Treatment, Physiotherapy, Interincisal mouth opening, Mouth opening exercise
1. Introduction
Oral Submucous Fibrosis (OSMF/OSF) is an insidious chronic disease associated with a juxta epithelial inflammatory reaction followed by fibro-elastic changes of the lamina propria and epithelial atrophy leading stiffness and progressive reduction in mouth opening.1 The global prevalence of OSF is 4.96 % [CI 95 % 2.28–8.62].2, 3, 4 OSMF is predominantly seen in the Indian subcontinent and Southeast Asia, with a prevalence ranging from 0.2 to 4.6 % in India.2,3 Unfortunately, the prevalence of OSMF has increased in recent years due to the prevalent habit of areca chewing, reaching 6.42 %.2 Recently literature estimated the overall malignant transformation rate [MTR] of OSMF between 4.2 % and 6 %.5,6 Therefore, clinician needed to address the OSMF condition at early stage. In addition to causing major difficulties with diet management, reduced mouth opening can also lower immunity and cause general health problems, making it difficult for these individuals to lead regular, healthy life.
Various drug treatments have been attempted for OSMF, but no single therapy has proven to be effective. Notably systematic reviews have evaluated treatment modalities in OSMF, but evidence of well-planned combination therapy or randomized controlled trials [RCTs] is lacking.7,8 Nevertheless, topical corticosteroid application, antioxidant use, and effective physiotherapy exercises have shown promise in the treatment of OSMF.9,10 Additionally, recent studies have explored the efficacy of combinations like lycopene and curcumin.8,11 Ayurvedic medicines such as Aloe Vera, Curcumin, Spirulina, Black Pepper, and Nigella sativa have also demonstrated effectiveness in the oral submucous fibrosis.9,10,12,13.
Physiotherapy has been one of treatment modalities for OSMF.1,14 It mostly involve mouth exercising (MEDs) or opening devices. These includes MED,14 Oral stent,15 Tongue spatula,16Nallan C-H appliance,17 and EZBite.18 These devices are effective in increasing the mouth opening.1,18 Two systematic reviews has highlighted the role of these MEDs in management of OSMF.1,19 Although, MEDs can increase the mouth opening, there is no clarity on minimal clinically important differences (MCID). Both systematic review did not answer this. Further, there are significant gaps in knowledge that warrant further review of literature with more emphasis on physiotherapy in managing OSMF especially mouth opening. Addressing the difficulty faced by practitioners in managing OSF may involve finding the right physiotherapy for OSMF.
2. Research question
The systematic review was conducted to addressed the following research question: “Is physiotherapy alone or in combination effective in improving the IMO in OSMF patients?”
3. Methods
The present systematic review is reported as per Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA 2020) (Table S1: PRISMA Checklist).20,21
3.1. Inclusion and exclusion criteria
Following eligibility criteria (based on PICO) was applied for searching the eligible studies for systematic review and meta-analysis.
P - OSMF patients, I - Physiotherapy and medicinal therapy (single or in combination), C – IMO pre and post treatment, O – Increase in IMO.
-
1.
Studies conducted in clinically/histopathologically diagnosed as OSMF patients.
-
2.
Studies evaluated the physiotherapy alone or in combination as intervention.
-
3.
Studies compared the pre-post treatment mouth opening.
-
4.
Studies reported the mouth opening as a continuous variable (mean and standard deviation).
-
5.
Studies that have excluded the OSMF patients with comorbidity or any other premalignant disorder or systematic illness.
3.2. Search strategy
Literature search was conducted in Scopus, Web of Science, PubMed databases using various search terms related to OSMF treatment. The search strategies were used as shown in TableS2. The following search terms were used: "Oral submucous fibrosis", "OSMF", "OSF”, “treatment”, “treatment modalities", "physiotherapy devices", “mouth opening exercise device”, “mouth opening”, “mouth opening device”, "physiotherapy". Boolean operators such as ‘AND’ and ‘OR’ were utilized to combine search terms for more specific results.
3.3. Screening and selection
Two reviewers independently screened the extracted articles by reading the title, abstract, and keywords. Those studies selected at this were further subjected to screening after obtaining the full-text. The disagreement was addressed by consulting the third author.
3.4. Risk of bias in individual studies
RCT studies were assessed using Cochrane Risk of bias 2 tool containing 5 domains which included randomization process (D1), deviations from intended intervention (D2), missing outcome data (D3), outcome measurement (D4), and selection of reported results (D5). NRCT studies were assessed for bias using Risk Of Bias In Non-randomised Studies - of Interventions (ROBINS-I) tool containing 7 domains. The bias levels for study were labelled low risk, some concerns, and high risk.
3.5. Data extraction
During the full-text screening of final eligible studies, two authors extracted following data: authors, title of publication, country, year, population, age, gender, sample, treatment modality, MEDs, duration, mouth opening values, follow-up. Any discrepancies were solved through discussion with third author.
3.6. Statistical analysis
The pre- and post-intervention means and standard deviations (SDs) in IMO in OSMF patients were used to compute mean differences (MDs) (effect sizes) and 95 % CIs. Meta-analysis was carried out using an inverse variance method and random-effect analysis. Revman 5.4 software (Review Manager (RevMan) (2014) Version 5.4. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration) was used for synthesis of results. Meta-analysis was carried out to see effectiveness of physiotherapy alone in improvement of IMO in OMSF. In order to ascertain whether combining physiotherapy with other modalities has an impact on IMO, the following group analysis was carried out: 1. Physiotherapy + US, 2. Physiotherapy and medicine, 3. Physiotherapy + surgery.
Heterogeneity and publication bias was assessed by I2 and funnel plot. Subgroups analysis was planned for OSMF stage, population, gender, age groups based on availability of data from original studies. Unfortunately, sufficient data was not available to carry out the subgroups analysis.
4. Results
4.1. Search results
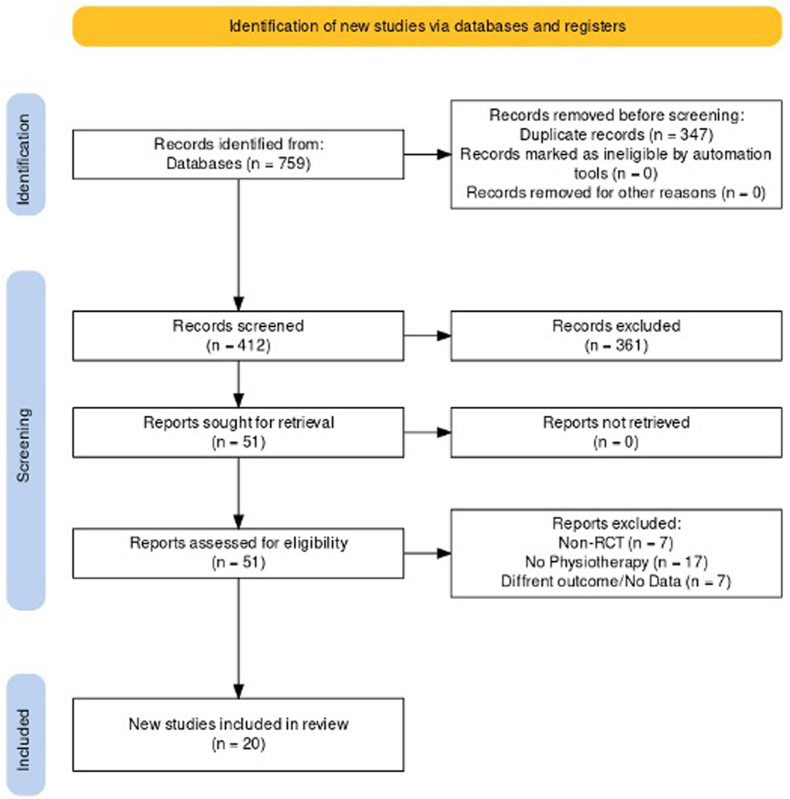
A total of 759 studies were initially identified. This screening process resulted in a total of 412 relevant studies being selected for further analysis. Out of which, 20 studies22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41 were selected for systematic review and meta-analysis on effectiveness of physiotherapy for treatment of OSMF (Fig. 1). The characteristics of included studies is given in Table S3 (Appendix I). The selected studies were published ranged from 2014 to 2024. 18 RCTs and two NRCTs were included in the systematic review and meta-analysis (Table S3). Most studies were from India (n = 16). 1235 OSMF patients were recruited in 20 included studies, 1202 analysed, and 33 were drop out or lost to follow-up or did not stick to treatment protocol. 714 were male whereas 144 were females (344 unknown). Age range was 15–59 years, however, majority were in third and fourth decade. Similarly, patients were within stage II and Stage III. Authors have used different grading and classification criteria for staging of OSMF.42, 43, 44, 45 891 OSMF patients treated with physiotherapy (either with or without device) alone or in combination whereas 311 OSMF patients were treated with drugs or surgery without physiotherapy. Ice cream stick exercise (n = 3), Wooden tongue depressors (WTDs)(n = 1), Heister jaw opener (HJO) (n = 7), threaded tapered screw device, and mouth stretching device (MSD) (n = 1) were MED employed in RCTs. Dexamethasone, hyaluronidase, triamcinolone, and placental extract were most commonly investigated medicine/drugs in OSMF treatment. The follow-up period in studies was from 15 days to 2 years. Further, measurement points were variable among the studies (days, weeks, months). Outcomes in studies were burning sensation, mouth opening, tongue protrusion, and cheek flexibility. Only one RCT study was registered in CTRI.23
Fig. 1.
Flowchart showing the screening, selection and inclusion of article in this systematic review.
4.2. Metanalysis of IMO improvement post-intervention
Meta-analysis of 20 studies evaluated the physiotherapy alone or as adjunct to drug and/or surgery. These studies evaluated the IMO at baseline (pre) and postoperatively (post). Out of these studies, only 4 studies33,35,36,40 evaluated physiotherapy alone (pre and post-operatively) (2 weeks–6 weeks). The meta-analysis of these 4 studies involving 58 OSMF patients showed that there is improvement in IMO after physiotherapy (n = 4; MD 1.19 mm [0.18, 2.20]) (Fig. 2), while combining it with US increase IMO to 3.96 mm (MD 3.96 [95 %CI, 1.5, 6.42] When physiotherapy is combined with drugs (n = 13; MD 8.35 [5.18, 11.51]) or surgery (n = 8; MD 21.84 [18.29, 25.38]), it showed better improvement in IMO (Fig. 2) than physiotherapy alone or with US. There was 5.18 mm and 21.38 mm increase in IMO when OMSF patients were treated with drugs and surgery, respectively. Visual inspection of funnel plot showed asymmetrical distribution indicating some bias in publication for physiotherapy, MOE + US, and surgery (Fig. 3). However, it was absent for drug intervention.
Fig. 2.
Forest plot of random effects meta-analysis of physiotherapy efficacy in oral submucous fibrosis.
Fig. 3.
Funnel plot assessing publication bias in included studies.
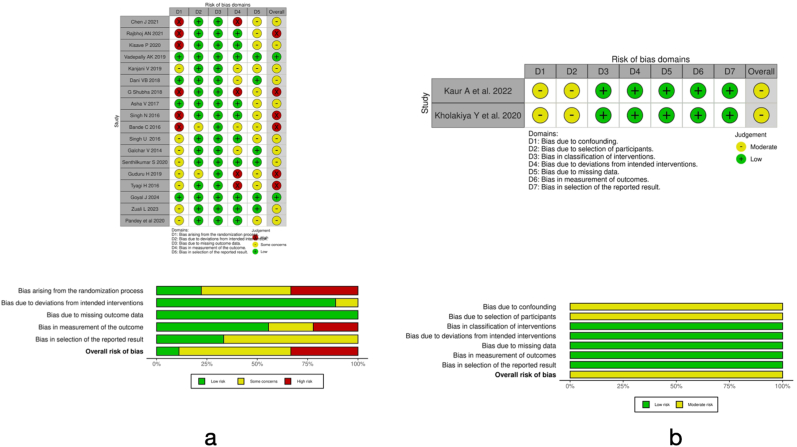
4.3. Risk of bias in included studies
Chen et al.,28 Rajbhoj et al.,13 Kisave et al.,30 and Shubha G et al.,36 exhibit a significant risk of bias, especially concerning the randomization process (D1), frequently associated with complications in outcome measurement (D4), resulting in an adverse overall assessment (Fig. 4). Conversely, Vadepally et al.,31 Dani et al.,35 Asha et al.,33 and Goyal et al.23 demonstrate uniformly low risk across all assessed domains, resulting in an overall low-risk assessment and reflecting robust methodological rigor. A significant number of studies, such as those by Kanjani et al.,32 Singh et al.,41 and Zuali et al.,24 exhibit "some concerns," particularly regarding randomization (D1) and outcome measurement (D4), as indicated by their overall bias evaluations. Kaur et al.25 and Kholakiya et al.26 presented a moderate risk due to the retrospective design of their studies.
Fig. 4.
Distribution of risk of bias across studies included in the systematic review and meta-analysis a) RoB2 for RCTs and b) ROBINS-I for NRCTs.
5. Discussion
The OSMF progression is largely defined by mouth opening and decides the efficacy of treatment modality.46 Past few decades, medicine/drug and surgery based treatment modalities have been tested.8,47, 48, 49 Unfortunately, each have their inherent advantages, disadvantage, and limitations. Clinicians and patients immediate concern is to increase mouth opening as it interferes with daily routine. Surgery is regarded the most effective approach for immediately increasing IMO; yet, surgery has its own disadvantages. Intramucosal injections frequently need strict patient compliance for consistent clinic visits, which is not always attainable. As a result, it is critical to develop a strategy for treating OSMF that can overcome the above indicated constraints.
Physiotherapy or MOE are one of the treatment modalities which does not have above mentioned limitations. It can be easily practiced by patient without much supervision and frequent clinic visits. The present meta-analysis found that physiotherapy alone can be effective treatment modality in increase the IMO, however, at present, it based on limited RCTs. Current evidence suggests that the mean change of 1.19 mm with range of 0.1 mm–2.2 mm in IMO in OSMF patients. Although, it is not highly significant (p = 0.02), still it can be better alternative to surgery and medicines. Unfortunately, it is mostly used as adjunct to previously mentioned treatment modalities rather than standalone treatment. One of the reason for this could be time required by physiotherapy to achieve same or near amount of IMO by surgery or medicine treatment.
Using one's own fingers to perform the MOE is a frequent, simple, non-invasive, and cost-effective procedure, particularly in rural settings. Furthermore, common people may easily grasp and follow the instructions. Unfortunately, exerting force to open the mouth with fingers is difficult and might create weariness. In a few studies, icestick packs were indicated as a mouth opening gag.13,37 This is also a cost-effective and simple procedure. But much like hand fingers, it has limitations as well.
Past few years, several MED were developed and experimented in RCTs. Heister jaw opener is one of routinely used MED for increasing the IMO. It used mostly as adjunct to surgery or medicine. It is effective in improving the IMO as well as preventing the relapse of treatment. However, actually efficacy of Heister jaw opener alone is not tested and validated with proper RCT. Similarly, several different MED have been developed and used for improving the IMO in OSMF. EZBite and Nallan C–H appliance are another MED.18 EZbite have limited amount of IMO capacity. However, validity and reliability of these MED has not been well-established at this moment due to lacks of RCTs.
IMO in OSMF is mostly because loss of elasticity of mucosa as result of excessive collagen deposition (fibrosis). To make the reverse the change, it is important to break fibres or increase fibres stretchability. In early stage of OSMF, there is less fibrosis, hence, MED are reported to be effective with less forces.18,28 However, this is often a difficult to achieve with just stretching with MED especially in advanced stage of OSMF. Ultrasound (US) has been used in treatment of OSMF along with MOE. US cause local vasodilation thereby increase vascular permeability and flow of blood to area.50 Further, US cause the collagen degradation51 as well as help in healing.52 Dani et al.35 when combined US with physiotherapy, found that US was effective in improving outcomes compared to physiotherapy alone. Similarly, Galchar et al.39 found similar findings when compared US and exercise with exercise alone. This suggest additional benefits of US in improving the IMO by modulating the soft tissue. Further, research into US role in OSMF treatment is warranted considering the absence of side effects.
Localized application of medicine along with physiotherapy in OSMF has been in practice for several years where dexamethasone/triamcinolone acetonide with hyaluronidase or placental extract is injected. Hyaluronidase help in absorption of medicine in interstitial spaces whereas dexamethasone basically helps in relieving the inflammation through anti-inflammatory activity. There are 13 studies in which dexamethasone and hyaluronidase was administered and patients were instructed to do the physiotherapy. Chen et al.28 established that mouth opening training, when combined with local injection treatment, can significantly increase the degree of mouth opening in patients with OSF. Overall, these studies showed the improvement in IMO over the period. This could be attributable to fact that after the hyaluronidase degrade the hyaluronic acid, decrease inflammation and oedema and increase granulation tissue formation, regular IMO prevent the fibrosis and stiffness. MOE improve the microvascular circulation thereby improve healing.53 Further, it was observed that physical exercise can decrease collagen cross linking and fibrosis.54This is one of the reasons that stage I of OSMF patients receive mild to moderate physical therapy. This will stop the composite fibres from further cross-linking. However, little is known about exact mechanism how dexamethasone and hyaluronidase help in improving IMO or it just MOE which play major role.
Surgery is only option in advanced stage of OSMF. Surgery usually involved fibrectomy or removal of fibrous tissue and placement of placental extract to avoid the post-surgical fibrosis, wound contraction, and relapse. MOE has been increasingly considered as mandatory adjunct after surgery to prevent any relapse. This is evident in Bande et al. study in which they compared the immediate and late physiotherapy in surgically treated OSMF patients.37 They found that in event of late physiotherapy, there is slight reduction of IMO compared to immediate. This highlight the importance of MOE even in after surgery in OSMF. However, there is need for well-designed RCTs with innovative methods.
The current meta-analysis has a few limitations. First, there are fewer research comparing physiotherapy to other treatment techniques. This might be attributed, as previously said, to the lack of quick improvement. Second, majority studies had included the OSMF patients which are categorized in different stages or grading based on different classification or criteria. Few of included RCTs have mentioned about Pindborg et al. criteria,43 Khanna and Andrade classification,44 and Passi et al.45 Only this, there few RCTs did not provide any specific reference or system for staging or grading the OSMF instead divided based on IMO which was also arbitrary. e.g. Shubha et al. divided OSMF patient as stage II when IMO is < 35 mm and >20 mm whereas Rajbhoj et al.13 considered stage II when IMO is > 30 mm–35 mm. Further, Rajbhoj et al.13 mentioned Lai et al.55 classification. Lai et al.55 study did not give any classification instead used the Pindborg's criteria for OSMF diagnosis and divided OSMF patients into group based on IMO. Third, duration of assessment was variable in RCTs which can have impact on IMO post-treatment. In future, RCTs should be conducted by removing these limitations. Finally, the physiotherapy can be beneficial to OSMF patients in increasing the IMO considering the irreversible nature of OSMF.
6. Conclusion
The meta-analysis found moderate levels of evidence on efficacy of physiotherapy alone in improvement of IMO in OSMF. Further, Physiotherapy can improve the IMO when combined with medicine and surgical treatment. Therefore, it is recommended to have a physiotherapy as part of treatment protocol of OSMF. However, on cautious note, several methodological limitations in past RCTs which needs to addressed to construct new evidences from well-planned, defined, longitudinal RCTs.
Patient's/Guardian's consent
It not applicable since it is systematic review and meta-analysis.
Authors Contribution
AB, AD, MY, AG, and DD contributed equally to conceptualization, data curation, formal analysis, writing – original draft, writing-review and editing, and approved final draft. AB, AD, MY, DD collected, analysed, and interpreted the data. AB, AD, MY, AG, and DD involved in drafting the manuscript or revising it critically for important intellectual content, given final approval of the version to be published.
Ethics approval and Consent
Not Applicable.
Ethical clearance
Ethical clearance is not required since it is systematic review and meta-analysis.
Data availability statement
The author confirms that all data generated or analysed during this review are included in this published article.
Sources of funding
Authors have not received any financial support or funding for this systematic review and meta-analysis.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Nil.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jobcr.2025.04.007.
Contributor Information
Ashish Bodhade, Email: ashishbodhade@gmail.com.
Alka Dive, Email: dive_alka@rediffmail.com.
Monal Yuwanati, Email: monal9817@gmail.com.
Amol Gadbail, Email: gadbail@yahoo.co.in.
Dhara Dwivedi, Email: dwivedidhara@gmail.com.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Gondivkar S.M., Gadbail A.R., Sarode S.C., et al. Clinical efficacy of mouth exercising devices in oral submucous fibrosis: a systematic review. J Oral Biol Craniofac Res. 2020;10(4):315–320. doi: 10.1016/j.jobcr.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yuwanati M., Ramadoss R., Kudo Y., Ramani P., Senthil Murugan M. Prevalence of oral submucous fibrosis among areca nut chewers: a systematic review and meta-analysis. Oral Dis. 2023;29(5):1920–1926. doi: 10.1111/odi.14235. [DOI] [PubMed] [Google Scholar]
- 3.Muller S., Tilakaratne W.M. Update from the 5th edition of the world health organization classification of head and neck tumors: tumours of the oral cavity and mobile tongue. Head Neck Pathol. 2022;16(1):54–62. doi: 10.1007/s12105-021-01402-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Poornachitra P., Maheswari U. Analysis of clinical symptoms in patients with oral submucous fibrosis. Ann Dent Spec. 2023;1(11):1–6. doi: 10.51847/iRUEgUex6m. [DOI] [Google Scholar]
- 5.Gondivkar S.M., Yuwanati M., Sarode S.C., et al. Malignant transformation in oral submucous fibrosis: tertiary level evidence: an umbrella review. Oral Dis. 2024;30(4):1818–1827. doi: 10.1111/odi.14718. [DOI] [PubMed] [Google Scholar]
- 6.Kizhakkoottu S., Ramani P., Tilakaratne W.M. Role of stem cells in the pathogenesis and malignant transformation of oral submucous fibrosis. Stem Cell Rev Rep. 2024;20(6):1512–1520. doi: 10.1007/s12015-024-10744-0. [DOI] [PubMed] [Google Scholar]
- 7.Kerr A., Warnakulasuriya S., Mighell A., et al. A systematic review of medical interventions for oral submucous fibrosis and future research opportunities. Oral Dis. 2011;17(SUPPL. 1):42–57. doi: 10.1111/j.1601-0825.2011.01791.x. [DOI] [PubMed] [Google Scholar]
- 8.Fedorowicz Z., Chan Shih-Yen E., Dorri M., Nasser M., Newton T., Shi L. Interventions for the management of oral submucous fibrosis. Cochrane Database Syst Rev. 2008;(2) doi: 10.1002/14651858.CD007156. [DOI] [PubMed] [Google Scholar]
- 9.Pérez‐Leal M., Lanciano F., Flacco N., Estornut C., Carceller M.C. Antioxidant treatments in patients with oral submucous fibrosis: a systematic review. J Oral Pathol Med. 2024;53(1):31–41. doi: 10.1111/jop.13503. [DOI] [PubMed] [Google Scholar]
- 10.Shao Y., Miao J., Wang Y. Curcumin in the treatment of oral submucous fibrosis: a systematic review and meta-analysis of randomized controlled trials. Int J Oral Maxillofac Surg. 2024;53(3):239–250. doi: 10.1016/j.ijom.2023.11.005. [DOI] [PubMed] [Google Scholar]
- 11.Pal S., Sharma D., Yadav N.P. Plant leads for mitigation of oral submucous fibrosis: current scenario and future prospect. Oral Dis. 2024;30(2):80–99. doi: 10.1111/odi.14485. [DOI] [PubMed] [Google Scholar]
- 12.Chandrashekar A., Annigeri R.G., Va U., Thimmasetty J. A clinicobiochemical evaluation of curcumin as gel and as buccal mucoadhesive patches in the management of oral submucous fibrosis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2021;131(4):428–434. doi: 10.1016/j.oooo.2020.12.020. [DOI] [PubMed] [Google Scholar]
- 13.Rajbhoj A.N., Kulkarni T.M., Shete A., Shete M., Gore R., Sapkal R. A comparative study to evaluate efficacy of curcumin and aloe vera gel along with oral physiotherapy in the management of oral submucous fibrosis: a randomized clinical trial. Asian Pac J Cancer Prev APJCP. 2021;22(Supplement 1):107–112. doi: 10.31557/APJCP.2021.22.S1.107. [DOI] [PubMed] [Google Scholar]
- 14.Patil P., Hazarey V., Chaudhari R., Nimbalkar-Patil S. Clinical efficacy of a mouth-exercising device adjunct to local ointment, intra-lesional injections and surgical treatment for oral submucous fibrosis: a randomized controlled trial. Asian Pac J Cancer Prev APJCP. 2016;17(3):1255–1259. doi: 10.7314/APJCP.2016.17.3.1255. [DOI] [PubMed] [Google Scholar]
- 15.Le P.V., Gornitsky M. Oral stent as treatment adjunct for oral submucous fibrosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81(2):148–150. doi: 10.1016/S1079-2104(96)80404-5. [DOI] [PubMed] [Google Scholar]
- 16.Cox S., Zoellner H. Physiotherapeutic treatment improves oral opening in oral submucous fibrosis. J Oral Pathol Med. 2009;38(2):220–226. doi: 10.1111/j.1600-0714.2008.00696.x. [DOI] [PubMed] [Google Scholar]
- 17.Chaitanya N.C.S.K., Krishna Prasad C.M.S., Priyanka Danam R., et al. A new intraoral appliance for trismus in oral submucous fibrosis. Case Rep Dent. 2018;2018:1–5. doi: 10.1155/2018/1039391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li Y.H., Chang W.C., Chiang T.E., Lin C.S., Chen Y.W. Mouth-opening device as a treatment modality in trismus patients with head and neck cancer and oral submucous fibrosis: a prospective study. Clin Oral Investig. 2019;23(1):469–476. doi: 10.1007/s00784-018-2456-4. [DOI] [PubMed] [Google Scholar]
- 19.Chitlange N.M., Phansopkar P. Physiotherapeutic approach in oral submucous fibrosis: a systematic review. Cureus. 2023 doi: 10.7759/cureus.48155. Published online November 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. 2021;372 doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haddaway N.R., Page M.J., Pritchard C.C., McGuinness L.A. PRISMA2020 : an R package and Shiny app for producing PRISMA 2020‐compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Systematic Rev. 2022;18(2) doi: 10.1002/cl2.1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tyagi H., Lakhanpal M., Dhillon M., Baduni A., Goel A., Banga A. Efficacy of therapeutic ultrasound with soft tissue mobilization in patients of oral submucous fibrosis. J Indian Acad Oral Med Radiol. 2018;30(4):349. doi: 10.4103/jiaomr.jiaomr_142_18. [DOI] [Google Scholar]
- 23.Goyal J., Iyer S., Palande C., Brahmankar U., John J., Patil K. Comparative assessment of the efficacy of an intralesional injection of placentrex, hyaluronidase and dexamethasone in the management of oral submucous fibrosis: a randomized controlled trial. Med Int. 2024;4(2):19. doi: 10.3892/mi.2024.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zuali L., Mohiyuddin S.M.A., A S., Mohammadi K., Paul I. Comparison between clinical outcome of intralesional human placental extract alone and topical application of placental extract gel after fibrotomy in oral submucous fibrosis. Cureus. 2023 doi: 10.7759/cureus.40105. Published online June 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaur A., Rustagi N., Ganesan A., Pm N., Kumar P., Chaudhry K. Minimal clinically important difference of mouth opening in oral submucous fibrosis patients: a retrospective study. J. Korean Assoc. Oral. Maxillofac. Surg. 2022;48(3):167–173. doi: 10.5125/jkaoms.2022.48.3.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kholakiya Y., Jose A., Rawat A., Nagori S.A., Jacob S., Roychoudhury A. Surgical management of oral submucous fibrosis with “Seagull-nasolabial flap” combined with short-term oral pentoxifylline for preventing relapse. J Stomatol Oral Maxillofac Surg. 2020;121(5):512–516. doi: 10.1016/j.jormas.2019.12.015. [DOI] [PubMed] [Google Scholar]
- 27.Pandey A., Sharma N., Dhiman N., et al. Comparative evaluation of buccal pad of fat with and without bovine collagen membrane in the management of oral submucous fibrosis: a prospective clinical study. Natl J Maxillofac Surg. 2020;11(1):57. doi: 10.4103/njms.njms_70_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen J., Wu Y., Peng J., Ma L. Oral opening training increases oral opening in patients with oral submucous fibrosis. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2021;46(7):731–735. doi: 10.11817/j.issn.1672-7347.2021.200786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rajbhoj A.N., Kulkarni T.M., Shete A., Shete M., Gore R., Sapkal R. A comparative study to evaluate efficacy of curcumin and aloe vera gel along with oral physiotherapy in the management of oral submucous fibrosis: a randomized clinical trial. Asian Pac J Cancer Prev APJCP. 2021;22(Supplement 1):107–112. doi: 10.31557/APJCP.2021.22.S1.107. [DOI] [PubMed] [Google Scholar]
- 30.Kisave P., Shekhar V., Babu P., et al. The study of placentrex and hydrocortisone as an adjunct treatment in oral submucous fibrosis. J Family Med Prim Care. 2020;9(5):2469. doi: 10.4103/jfmpc.jfmpc_268_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vadepally A.K., Salavadi R.K., Sinha R. A comparative clinical study on physiotherapy outcomes with wooden tongue depressors versus Heister jaw opener in oral submucous fibrosis patients. J Oral Biol Craniofac Res. 2019;9(3):263–267. doi: 10.1016/j.jobcr.2019.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kanjani V., Annigeri R., Revanappa M., Rani A. Efficacy of spirulina along with different physiotherapeutic modalities in the management of oral submucous fibrosis. Ann Maxillofac Surg. 2019;9(1):23. doi: 10.4103/ams.ams_3_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Asha V., Baruah Nevica. Physiotherapy in treatment of oral submucous fibrosis related restricted mouth opening. Int Healthcare Res J. 2017;1(8):252–257. doi: 10.26440/ihrj/01_08/125. [DOI] [Google Scholar]
- 34.Singh N., Hebbale M., Mhapuskar A., Nisa S.U., Thopte S., Singh S. Effectiveness of aloe vera and antioxidant along with physiotherapy in the management of oral submucous fibrosis. J Contemp Dent Pract. 2016;17(1):78–84. doi: 10.5005/jp-journals-10024-1806. [DOI] [PubMed] [Google Scholar]
- 35.Dani V.B., Patel S.H. The effectiveness of therapeutic ultrasound in patients with oral submucosal fibrosis. Indian J Cancer. 2018;55(3):248–250. doi: 10.4103/ijc.IJC_611_17. [DOI] [PubMed] [Google Scholar]
- 36.Shubha G., Sheshaprasad R., Hebbar P., Pai A., Shubhasini A.R., Keerthi G. Efficacy of conservative versus intralesional therapy in OSMF – a comparative study. J Med Radiol Pathol Sur. 2018;5(6):13–17. doi: 10.15713/ins.jmrps.149. [DOI] [Google Scholar]
- 37.Bande C., Dawane P., Gupta M.K., Gawande M., Rode V. Immediate versus delayed aggressive physical therapy following buccal fat pad interposition in oral submucous fibrosis—a prospective study in Central India. Oral Maxillofac Surg. 2016;20(4):397–403. doi: 10.1007/s10006-016-0580-3. [DOI] [PubMed] [Google Scholar]
- 38.Guduru H., Garlapati K., Solomon R., Ignatius A., Yeladandi M., Madireddy N. A comparative study of efficacy of intralesional corticosteroids and hyaluronidase therapy with and without ultrasound therapy in patients with oral submucous fibrosis. J Indian Acad Oral Med Radiol. 2019;31(1):11. doi: 10.4103/jiaomr.jiaomr_158_18. [DOI] [Google Scholar]
- 39.Galchar P, Soni N, Bhise A. A comparative study of ultrasound and exercise versus placebo ultrasound and exercise in patient with oral submucous fibrosis. Indian J Phys Ther. .
- 40.Senthilkumar S., Chitra S., Vijayaraghavan R., Hemaashree V., Subhavani P. Effectiveness of ultrasound therapy on oral submucosal fibrosis. Indian J Public Health Res Dev. 2020;11(3):320–325. [Google Scholar]
- 41.Singh U. Efficacy and safety of intralesional xantinol nicotinate in the treatment of various stages of oral submucous fibrosis. J Clin Diagn Res. 2016;10(10):ZC34–ZC37. doi: 10.7860/jcdr/2016/20138.8639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kakar P.K., Puri R.K., Venkatachalam V.P. Oral submucous fibrosis—treatment with hyalase. J Laryngol Otol. 1985;99(1):57–60. doi: 10.1017/S0022215100096286. [DOI] [PubMed] [Google Scholar]
- 43.Pindborg J.J. Oral submucous fibrosis: a review. Ann Acad Med Singapore. 1989;18(5):603–607. doi: 10.36106/gjra/0710216. [DOI] [PubMed] [Google Scholar]
- 44.Khanna J.N., Andrade N.N. Oral submucous fibrosis: a new concept in surgical management. Report of 100 cases. Int J Oral Maxillofac Surg. 1995;24(6):433–439. doi: 10.1016/S0901-5027(05)80473-4. [DOI] [PubMed] [Google Scholar]
- 45.Passi D., Bhanot P., Kacker D., Chahal D., Atri M., Panwar Y. Oral submucous fibrosis: newer proposed classification with critical updates in pathogenesis and management strategies. Natl J Maxillofac Surg. 2017;8(2):89. doi: 10.4103/njms.njms_32_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kumar V.J., Ezhilarasan D., Veeraiyan D.N. Oral submucosal fibrosis: an updated molecular mechanism on pathogenesis and treatment modalities. Oral Dis. 2024;30(7):4798–4799. doi: 10.1111/odi.14901. [DOI] [PubMed] [Google Scholar]
- 47.Kerr A.R. Efficacy of oral lycopene in the management of oral submucous fibrosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(2):214–215. doi: 10.1016/j.tripleo.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 48.Dhanvanth M., Maheswari T.N.U. Topical herbal therapeutic formulation used in the management of oral potentially malignant disorders – a systematic review. J Indian Acad Oral Med Radiol. 2022;34(2):223–227. doi: 10.4103/jiaomr.jiaomr_101_21. [DOI] [Google Scholar]
- 49.Renu K. Exosomes derived from human adipose mesenchymal stem cells act as a therapeutic target for oral submucous fibrosis. J Stomatol Oral Maxillofac Surg. Published online January 2025:102224. doi:10.1016/j.jormas.2025.102224. [DOI] [PubMed]
- 50.Morishita K., Karasuno H., Yokoi Y., et al. Effects of therapeutic ultrasound on intramuscular blood circulation and oxygen dynamics. J Jpn Phys Ther Assoc. 2014;17(1):1–7. doi: 10.1298/jjpta.Vol17_001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tu Z cai, Huang T., Wang H., et al. Physico-chemical properties of gelatin from bighead carp (Hypophthalmichthys nobilis) scales by ultrasound-assisted extraction. J Food Sci Technol. 2015;52(4):2166–2174. doi: 10.1007/s13197-013-1239-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Best T.M., Wilk K.E., Moorman C.T., Draper D.O. Low intensity ultrasound for promoting soft tissue healing: a systematic review of the literature and medical technology. Intern Med Rev (Wash D C). 2016;2(11) doi: 10.18103/imr.v2i11.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fronza M., Caetano G.F., Leite M.N., et al. Hyaluronidase modulates inflammatory response and accelerates the cutaneous wound healing. Yamamoto M., editor. PLoS One. 2014;9(11) doi: 10.1371/journal.pone.0112297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kwak H., Kim J., Joshi K., Yeh A., Martinez D.A., Lawler J.M. Exercise training reduces fibrosis and matrix metalloproteinase dysregulation in the aging rat heart. FASEB J. 2011;25(3):1106–1117. doi: 10.1096/fj.10-172924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lai D.R., Chen H.R., Lin L.M., Huang Y.L., Tsai C.C., Lai D. Clinical evaluation of different treatment methods for oral submucous fibrosis. A 10‐year experience with 150 cases. J Oral Pathol Med. 1995;24(9):402–406. doi: 10.1111/j.1600-0714.1995.tb01209.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The author confirms that all data generated or analysed during this review are included in this published article.