Abstract
Aims:
The global rise in obesity rates has led to increased use of bariatric surgery, which can potentially exacerbate or induce gastroesophageal reflux disease. This study aimed to assess the academic impact and trends in research on gastroesophageal reflux disease in the context of obesity treatment and bariatric surgery through a comprehensive bibliometric analysis.
Materials and methods:
A bibliometric analysis was conducted using data from Web of Science and Scopus databases, covering publications from 1993 to 2024. The study utilized the Bibliometrix R package to analyze publication trends, collaborative networks, and research topics.
Results:
The analysis encompassed 257 documents from 82 sources, with 6192 total citations and an 8.2% annual growth rate in publications. The United States emerged as the leading contributor with 90 publications. Key research topics included bariatric surgery, sleeve gastrectomy, and gastroesophageal reflux disease, with increasing focus on complications and revisional bariatric surgery in recent years. Two main research clusters were identified: one focusing on general health aspects and demographics, and another on specialized bariatric procedures and outcomes. However, the analysis is constrained by its reliance on data from only two bibliographic databases, which may not encompass all pertinent studies, and by a geographic bias toward high-income countries. Moreover, our deep literature reviews highlighted that obesity is a known risk factor for gastroesophageal reflux disease, and while Roux-en-Y gastric bypass often reduces gastroesophageal reflux disease symptoms, sleeve gastrectomy may exacerbate or cause de novo gastroesophageal reflux disease postoperatively.
Conclusions:
This bibliometric study reveals a significant increase in research activity on gastroesophageal reflux disease in relation to obesity treatment and bariatric surgery, particularly since 2017. The findings highlight the growing importance of this field and the need for continued international research efforts to optimize surgical protocols and improve patient outcomes.
Keywords: Bariatric surgery, bibliometric analysis, gastroesophageal reflux diseases, obesity management, publication trends
Introduction
Global obesity rates have dramatically risen. By 2013, about 36.9% of men and 38% of women worldwide were overweight or obese, with significant increases in obesity rates among both children and adults in developed and developing countries. 1 Moreover, previous studies found that there are a significant relationship between obesity and gastroesophageal reflux disease (GERD), and the prevalence of the obese population with GERD varies globally, ranging from 18.1% to 27.8% in North America, 8.8%–25.9% in Europe, 2.5%–7.8% in East Asia, 8.7%–33.1% in the Middle East, 11.6% in Australia, and 23.0% in South America.2,3 Despite these alarming trends, no country has successfully reversed this epidemic, highlighting an urgent need for effective global intervention. When methods such as dietary changes, physical activity, behavioral therapy, and medications prove ineffective, particularly for individuals who have failed to sustain weight loss through nonsurgical means, bariatric surgery is considered. 4 The most frequently performed bariatric surgery procedures include Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG).5–7 At present, bariatric surgery is advised for people with a BMI < 40 or <35 if they have serious health conditions related to obesity. 8
SG is a procedure that stands out for its technical simplicity, low risk of postoperative complications, and long-term effectiveness in reducing body weight and alleviating related conditions. 9 Undoubtedly, preserving the pyloric mechanism and allowing for the controlled passage of food into the duodenum is a significant advantage of this procedure. 10
However, the invasive nature and significant lifestyle changes required postsurgery have led researchers to explore less-invasive alternatives that could complement or even enhance the outcomes of traditional bariatric procedures. Despite these benefits, bariatric surgery may also lead to complications, such as nutrient deficiencies, surgical risks, and the potential development or worsening of GERD. 11 The incidence of GERD following SG reported in the literature can reach up to 17%. 12 Obesity is a known risk factor for GERD, as excess weight can increase abdominal pressure, promoting acid reflux. 13
The prevalence in Kazakhstan varies by region, ranging from 40.5% to 67.6%. 14 GERD usually presents with heartburn and regurgitation, but it can also have atypical symptoms such as chest pain, dental erosions, chronic cough, laryngitis, or asthma.15–19 Therefore, the surgical treatment of patients with GERD involves performing fundoplication using various techniques, which is currently considered the gold standard. 20 Furthermore, while RYGB is often associated with reduced GERD symptoms due to its anatomical modifications, SG may exacerbate GERD or even cause de novo GERD postoperatively due to changes in the gastroesophageal junction.21,22
The association of obesity and GERD, as well as the impact of bariatric surgery on the course of GERD, are complex and multilayered issues that require careful investigation. 8 The interaction between these conditions makes it necessary to understand how different surgical approaches may impact GERD symptoms in obese patients. Several studies highlight the importance of choosing the appropriate procedure based on the presence or risk of GERD in order to minimize complications and improve patients’ quality of life.
Bibliometry, a field within library and information science, focuses on the quantitative study of bibliographic data. 23 Bibliometric analysis helps evaluate research trends and activities on specific topics, aiding in future planning and funding decisions. 24 This method helps spot emerging trends and key features of a disease. 25 Several bibliometric studies have been carried out on both bariatric surgery and botulinum toxin independently. Previous bibliometric studies have covered several distinct areas: analyzing publications and research trends related to bariatric surgery and its impact on weight gain, 26 focusing on the most frequently performed procedures in bariatric surgery, 27 and conducting trend analysis of bibliometric data in the medical literature concerning GERD. 28 However, in the available databases, we did not find any bibliometric analysis that combines topics—GERD in the context of obesity treatment and bariatric surgery. This analysis includes a wide range of analytical activities, from reviewing recent publications to analyzing collaborative networks and highlighting relevant topics. Unlike previous reviews focusing on clinical outcomes, this study uses a bibliometric approach to uncover trends, collaborations, and gaps in GERD research within the context of bariatric surgery.
This bibliometric analysis aims to offer a thorough examination of the research landscape surrounding GERD within the context of obesity treatment and bariatric surgery. By scrutinizing publication patterns, collaborative networks, and emerging themes from 1993 to 2024, we seek to shed light on the evolving comprehension of the intricate interplay between these conditions. Our study endeavors to identify key contributors, seminal publications, and research focal points in this multifaceted field. Moreover, we strive to uncover gaps in current knowledge and potential avenues for future inquiry, thereby guiding researchers, clinicians, and policymakers in addressing the challenges posed by the complex relationship between GERD, obesity, and bariatric interventions. Through this comprehensive analysis, we aspire to promote a more holistic approach to patient care and catalyze innovative research directions in this crucial area of healthcare.
Materials and methods
Search strategy
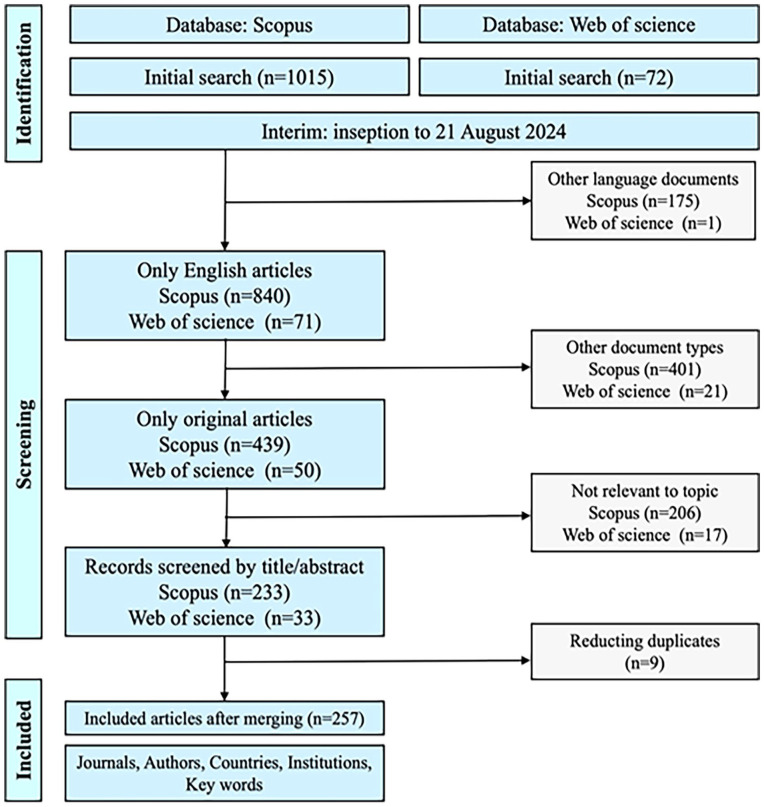
We conducted a search in the Web of Science Core Collection (WoS-CC) and Scopus databases on August 21, 2024. WoS and Scopus were chosen for their comprehensive coverage of high-impact journals and robust citation metrics. Publications from 1993 to 2024 were exported from WoS-CC in plain text and from Scopus in BibTeX format. These exports include details such as authors, title, publication year, source name, volume, issue, pages, DOI, open access status, and bibliographic information. They also contain organizational affiliations, ISSN, PubMed ID, the document’s language, funding details, conference information, and keywords. Only English-language research articles were considered for this bibliometric analysis. The search process is detailed in Figure 1, and the search formulas are presented in Supplemental Tables S1–S3. Search formulas included keywords such as “GERD,” “bariatric surgery,” and “obesity,” combined using Boolean operators to capture relevant studies. The analysis covered the annual distribution of relevant documents; the countries, institutions, and journals that published these; the authors; the keywords employed; and the trends in keyword usage over time.
Figure 1.
Search strategy in Prisma chart using Web of Science (WoS) and Scopus database.
Study selection and data extraction
A two-step process was implemented to select articles that fulfilled the inclusion criteria. Initially, two authors (AI, AY) independently reviewed the titles and abstracts of the articles identified through the search strategy. Articles that both authors agreed upon were subjected to full-text analysis. If there was any disagreement, a third author (BZ) was brought in to make the final decision.
Performance analysis
Performance analysis and the creation of scientific maps from the Scopus and WoS databases were conducted using the Bibliometrix R package (available at http://www.bibliometrix.org) within the RStudio programming environment, updated to version 2023.12.1+402. The annual scientific production and average citations per year were plotted using Biblioshiny and subsequently recreated in Flourish.studio (https://flourish.studio).
Results
Summary of the papers
Our study analyzed 257 documents from 82 sources, over the period of 1993 to 2024, including 482 references and identifying 523 unique author keywords with 6192 total citation. The annual growth rate of publications on the topic was 8.2%, the average age of documents was 5.99 years, and the average number of citations per document was 23.92.
Annual analysis of publications
The publications in this field began intermittently in the 1990s, showing limited academic activity with minimal citation impact. From 2004, there was a noticeable increase in both the number and citations of published research, showing a growing interest from scholars. The period from 2017 onwards saw a significant surge in research activity, with substantial growth in the volume of publications. By 2023, the field recorded 36 articles annually, averaging an impressive 433.68 citations per article, highlighting a strong and increasing interest among the academic community in this area of research. (Figure 2). In Table 1, the top 10 most frequently cited papers were shown which had significant impact on this field of study.
Figure 2.

Annual publication trends over time on the context of gastroesophageal reflux disease in the context of obesity treatment and bariatric surgery (1993–2024).
Table 1.
The 10 most frequently cited papers on the gastroesophageal reflux disease in the context of obesity treatment and bariatric surgery (1993–2024).
| Rank | Article | 1st Author | DOI | Total citations | Tc per year | Year of publication |
|---|---|---|---|---|---|---|
| 1 | Efficacy and safety of one anastomosis gastric bypass versus Roux-En-Y gastric bypass for obesity (YOMEGA): a multicenter, randomized, open-label, noninferiority trial 12 | Robert M | 10.1016/S0140-6736(19)30475-1 | 302 | 50.33 | 2019 |
| 2 | Symptomatic improvement in gastroesophageal reflux disease (GERD) following laparoscopic Roux-En-Y gastric bypass 29 | Rrezza EE | 10.1007/S00464-001-8313-5 | 261 | 11.35 | 2002 |
| 3 | Management of gastroesophageal reflux disease 30 | Maria G | 10.1053/J.Gastro.2017.07.049 | 213 | 30.43 | 2018 |
| 4 | Procedure incidence and in-hospital complication rates of bariatric surgery in the United States 31 | Livingston EH | 10.1016/J.Amjsurg.2004.03.001 | 176 | 8.38 | 2004 |
| 5 | Systematic endoscopy 5 years after sleeve gastrectomy results in a high rate of Barrett’s esophagus: results of a multicenter study 32 | Sebastianelli L | 10.1007/S11695-019-03704-Y | 171 | 28.50 | 2019 |
| 6 | Laparoscopic Roux-En-Y gastric bypass for BMI < 35 kg/m2: a tailored approach 33 | Cohen R | 10.1016/J.Soard.2006.02.011 | 118 | 6.21 | 2006 |
| 7 | Superior resolution of metabolic comorbidities independent of weight loss in the super-obese (BMI ⩾ 50 kg/m2) compared with gastric bypass 34 | Prachand VN | 10.1111/J.1572-0241.2007.01676.X | 103 | 6.87 | 2010 |
| 8 | Association of race with bariatric surgery outcomes 35 | Wood MH | 10.1136/Gut.46.5.597 | 100 | 16.67 | 2019 |
| 9 | Effects of Omega-loop bypass on esophagogastric junction function 36 | Tolone S | 10.1016/J.Soard.2015.03.011 | 97 | 10.78 | 2016 |
| 10 | Conversion of sleeve gastrectomy to Roux-En-Y gastric bypass is effective for gastro-esophageal reflux disease but not for further weight loss 37 | Parmar CD | 10.1007/S11695-017-2542-8 | 96 | 12.00 | 2017 |
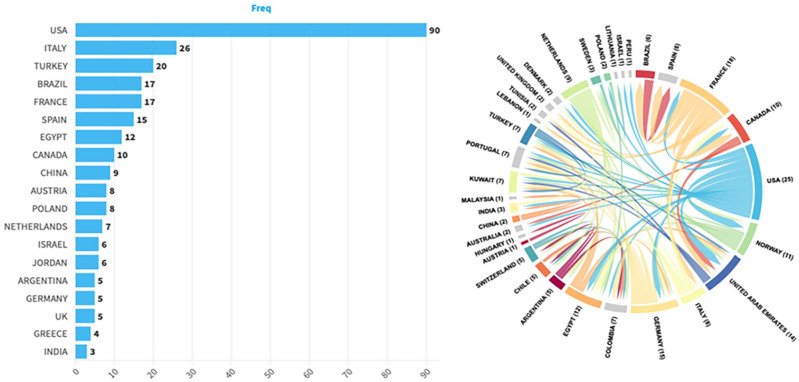
Countries and affiliations
The USA produced the most articles, leading with 90 publications and accounting for 31.14% of the total output (Figure 3). The USA also stands out as the most active nation in terms of collaborations, engaging in 18 joint projects, particularly with the United Arab Emirates (Figure 3). France, Germany, and the Netherlands also engage in international collaborations, though with fewer partner nations. Additionally, the USA and France amassed 2033 and 780 total citations, respectively. Meanwhile, Chile and France achieved the highest citation rates per article, at 71.50 and 43.30 respectively (Table 2).
Figure 3.
Top 20 countries with the highest number of articles produced and global research collaboration network. Larger nodes indicate countries with higher publication output, while thicker lines represent stronger collaboration networks.
Table 2.
Most cited countries publishing on the gastroesophageal reflux disease in the context of obesity treatment and bariatric surgery (1993–2024).
| Rank | Country | Total citations | Average article citations |
|---|---|---|---|
| 1 | USA | 2033 | 29.00 |
| 2 | France | 780 | 43.30 |
| 3 | Italy | 563 | 26.80 |
| 4 | Brazil | 244 | 30.50 |
| 5 | Germany | 172 | 28.70 |
| 6 | Austria | 155 | 31.00 |
| 7 | Chile | 143 | 71.50 |
| 8 | United Kingdom | 132 | 33.00 |
| 9 | Egypt | 99 | 9.00 |
| 10 | Spain | 90 | 12.90 |
Leading institutions contributing to this research include the University of Padova in Italy, with 10 publications, underscoring its leadership in the field. The University of Michigan in the USA closely follows with seven publications, highlighting Italy’s strong contribution to the research. Significant contributions also come from the Mayo Clinic and the University of California in the USA, which together produced a total of 19 articles. These statistics illustrate the pivotal roles that both the USA and Italy play in advancing research in this area (Table 3).
Table 3.
Most relevant affiliations on the gastroesophageal reflux disease in the context of obesity treatment and bariatric surgery (1993–2024).
| Rank | Affiliation | Articles | Country |
|---|---|---|---|
| 1 | University of Padova | 10 | Italy |
| 2 | University of Michigan | 7 | United States |
| 3 | Alexandria University | 6 | Egypt |
| 4 | Athens | 6 | Greece |
| 5 | Mayo Clinic | 6 | United States |
| 6 | Sapienza University of Rome | 6 | Italy |
| 7 | Tel Aviv University | 6 | Israel |
| 8 | University of Alberta | 6 | Canada |
| 9 | University of California | 6 | United States |
| 10 | Haukeland University Hospital | 5 | Norway |
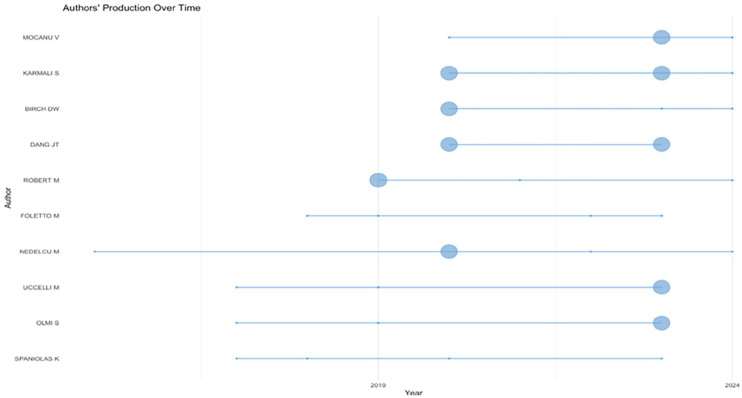
The number of publications and citations by different authors
M. Robert stands out among the authors with a significant peak in total citations, especially in 2019, when one of his publications garnered 473 citations, averaging 78,833 citations per year. Other consistently active authors, such as Birch DW, Dang JT, and Karmali S, also achieved relatively high total citations over several years. The data show variations in both publication frequency and total citations per year among different authors, reflecting the dynamic engagement in the field. For example, Foletto M achieved notable results in 2019 with 171 total citations for a single paper, averaging 28.5 citations per year. Similarly, Karmali S and Mocanu V have demonstrated increasing citation impact in recent years, especially in 2023. Nedelcu M also showed significant citation performance in certain years, indicating periods of high engagement and impact in their research fields (Figure 4). In this field, the cited authors are predominantly from Italy, in particular from the Fondazione Policlinico Universitario Agostino Gemelli Istituto di Ricerca e Cura a Carattere Scientifico (IRCCS). The leaders of this group are Brisinda G and Maria G, each with 10 articles and H-indexes of 27 and 24, respectively. Another notable author from the same institution is Gui D with 5 articles and an H-index of 15 (Table 4).
Figure 4.
Authors’ production over time on the gastroesophageal reflux disease in the context of obesity treatment and bariatric surgery (1993–2024).
Table 4.
Most cited authors on the gastroesophageal reflux disease in the context of obesity treatment and bariatric surgery (1993–2024).
| Rank | Authors | Articles | H-index | Affiliation |
|---|---|---|---|---|
| 1 | Dang J | 5 | 22 | University of Alberta, Faculty of Medicine and Dentistry |
| 2 | Karmali S | 5 | 42 | University of Alberta |
| 3 | Nedelcu M | 5 | 24 | Clinique Bouchard, Marseille, France |
| 4 | Birch D | 4 | 44 | University of Alberta, Faculty of Medicine and Dentistry |
| 5 | Foletto M | 4 | 39 | Università Degli Studi Di Padova |
| 6 | Mocanu V | 4 | 18 | University of Alberta, Faculty of Medicine and Dentistry |
| 7 | Olmi S | 4 | 29 | Università Vita-Salute San Raffaele |
| 8 | Robert M | 4 | 27 | Hospital Edouard Herriot |
| 9 | Spaniolas K | 4 | 31 | Stony Brook Medicine |
| 10 | Switzer N | 4 | 26 | University of Alberta, Faculty of Medicine and Dentistry |
Journals
The presented data on journals publishing the most prominent journals based on the volume of publications include Obesity Surgery with 71 articles, Surgery for Obesity and Related Diseases with 41 articles, and Surgical Endoscopy with 20 articles, all predominantly published in the United States and highly regarded within the medical community. Despite fewer contributions in this specific field (only 3 articles), Annals of Surgery stands out for its exceptionally high impact factor, underscoring its importance and the quality of research across broader surgical disciplines, including bariatric surgery (Table 5).
Table 5.
Rank of the highest publication rate of sources on the gastroesophageal reflux disease in the context of obesity treatment and bariatric surgery (1993–2024).
| Rank | Sources name | Articles | If | JCR category | Country |
|---|---|---|---|---|---|
| 1 | Obesity surgery | 71 | 2,9 | Surgery-Scie (Q1) | USA |
| 2 | Surgery for obesity and related diseases | 41 | 3,5 | Surgery-Scie (Q1) | USA |
| 3 | Surgical endoscopy | 20 | 2,4 | Surgery-Scie (Q2) | USA |
| 4 | Journal of gastrointestinal surgery | 11 | 2,2 | Surgery-Scie (Q2) | USA |
| 5 | Journal of laparoendoscopic and advanced surgical techniques | 8 | 1,1 | Surgery-Scie (Q3) | USA |
| 6 | Bariatric surgical practice and patient care | 4 | 0,4 | Surgery-Scie (Q4) | USA |
| 7 | Journal of clinical medicine | 4 | 3,0 | Medicine, General & Internal (Q1) | Switzerland |
| 8 | Annals of surgery | 3 | 7,5 | Surgery-Scie (Q1) | USA |
| 9 | Foregut | 3 | USA | ||
| 10 | Langenbeck’s archives of surgery | 3 | 2,1 | Surgery-Scie (Q2) | Germany |
Most relevant documents and trend topics
The highest frequency on “bariatric surgery” of 132 items, with a steady increase in publication years from 2017 to 2023. “SG” and “obesity” follow, with increasing frequencies and recent median publication years, indicating growing research interest. Terms like “GERD” and “gastric bypass” also show notable activity, particularly in the past 5 years. “GERD” and “morbid obesity” have less frequent but significant research activity, with median publication years reflecting their relevance in recent studies. “Complications” and “revisional bariatric surgery” are emerging topics with recent peaks in publications. The lower frequencies of terms like “botulinum toxin A” and “quality of life” suggest they are less central, but still relevant in the context of bariatric surgery and associated outcomes (Figure 5). As a result of our network analysis, we identified two main clusters that represent distinct subgroups within the studied theme, each containing closely interconnected nodes: Cluster 1 focuses on general health aspects, such as the relationship between obesity and GERD, while Cluster 2 delves into specific surgical procedures and their outcomes. In more details, the first cluster encompasses nodes associated with general health aspects, such as gastroesophageal reflux, obesity, and bariatric surgery, with a focus on gender aspects (female, male) and age categories (adult, middle aged). These results demonstrate a broad spectrum of common and fundamental health issues and related research. The second cluster is focused on specialized procedures and outcomes of bariatric surgery, including nodes such as gastric bypass, SG, and postoperative complications, reflecting specialized research aspects related to treatment outcome evaluation, potential complications, and surgical methods. We also identified intercluster connections that indicate interactions between general health principles and specific medical procedures (Figure 6).
Figure 5.
Trend topics on the gastroesophageal reflux disease in the context of obesity treatment and bariatric surgery (1993–2024). Larger nodes indicate higher term frequency during different times (X-axis).
Figure 6.

Co-occurrence network on the gastroesophageal reflux disease in the context of obesity treatment and bariatric surgery (1993–2024). Upper nodes with red color belongs to Cluster 1 and lower nodes with blue color belongs to Cluster 2.
Discussion
Bibliometrics evaluation of GERD and bariatric surgery
This bibliometric analysis, covering 257 publications over 3 decades, marks a significant advance in our understanding of the interactions between GERD and obesity treatment, particularly bariatric surgery. Our study not only demonstrates growing academic interest but also highlights the growing complexity of managing GERD in the context of obesity.12,38
The sustained growth in publication volume, with a marked acceleration since 2017, demonstrates that the academic community is responding decisively to the rising prevalence of obesity and its complications. This response is timely as the obesity epidemic continues to expand worldwide, bringing GERD and other related conditions to the forefront of surgical interventions and medical research. 8
The significant contributions from high-income countries, particularly the United States, highlight the cutting-edge research capabilities and substantial funding available in these regions. However, the significant role of the United States, accounting for over 30% of publications, along with emerging research centers such as the United Arab Emirates, highlights the need for a more diversified global research effort. This geographic skew highlights potential gaps in understanding how different populations respond to bariatric surgery and GERD treatment, pointing to the opportunity to conduct research in different socioeconomic settings. 39 The preponderance of research from high-income nations underscores the importance of expanding research participation to include low- and middle-income areas. This broader approach is crucial for gaining a more comprehensive understanding of how GERD and bariatric outcomes vary globally. By recognizing these disparities, funding organizations can focus on supporting underrepresented regions and foster global partnerships to address the existing gaps in GERD research. This version maintains the original message while using different wording and phrasing.
Institutions such as the University of Michigan and the University of Padova are at the forefront, likely due to their comprehensive programs that not only address surgical techniques but also include long-term follow-up and treatment of complications. The significant international collaboration evident in our study highlights the multidisciplinary nature of managing GERD in obese patients, requiring contributions from gastroenterology, surgery, endocrinology, and nutrition. 40
Authors such as Robert M, Birch DW, and Dang JT have shaped the discourse in this field and their work is frequently cited, indicating their seminal contributions. However, the field would benefit from a broader range of voices, particularly from regions that are underrepresented in the current literature. 41
Thematic shifts toward less-invasive procedures and treatment of postoperative complications such as Barrett’s esophagus demonstrate an adaptive surgical community interested in improving patient outcomes. However, the focus on complications also highlights the need for improved preoperative assessment and postoperative care protocols to reduce risks and improve quality of life for patients undergoing bariatric surgery. 42 Emerging topics such as the use of botulinum toxin to treat GERD symptoms after bariatric surgery offer innovative approaches to postoperative care but also require rigorous clinical trials to establish efficacy and safety. This area represents fertile ground for future research, particularly in developing standardized guidelines that can be applied globally.43,44
Limitations of bibliometric studies
Bibliometric studies are invaluable for understanding research trends, publication dynamics, and emerging areas of interest. These analyses offer insights into collaborative networks, influential authors, and high-impact publications, thereby aiding in strategic research planning. 45 For example, bibliometric tools can identify the frequency of keywords, co-authorship patterns, and citation metrics, enabling researchers to align their focus with impactful topics. 23
Despite their utility, these studies face critical limitations. First, citation-based analyses can be biased by factors such as self-citation and geographical disparities. Researchers from high-income countries often dominate the field, skewing results toward regions with greater research funding and publication access. 45 Additionally, bibliometric methods are quantitative and lack the depth needed to evaluate the quality or clinical applicability of individual studies. 8
To address these shortcomings, we integrated a literature review into this study. This approach allows for a richer understanding of GERD and bariatric surgery by contextualizing bibliometric trends within clinical findings, bridging gaps in the analysis.
GERD: Mechanisms, prevalence, and mortality
GERD arises from the reflux of gastric contents into the esophagus due to dysfunction of the lower esophageal sphincter (LES). 18 This dysfunction may result from transient LES relaxations, hiatal hernias, or increased intra-abdominal pressure, the latter of which is exacerbated by obesity. 2 Structural abnormalities such as a short esophagus or weakened diaphragmatic crura further impair the esophagogastric junction’s ability to prevent reflux. 38
On a cellular level, GERD leads to chronic inflammation of the esophageal mucosa, causing oxidative stress and promoting metaplastic changes. Over time, these changes can progress to Barrett’s esophagus, a precursor to esophageal adenocarcinoma. 46 This progression underscores the disease’s potential severity if untreated.
Obesity is a critical risk factor, significantly increasing GERD prevalence and severity due to increased abdominal pressure and hormonal changes that affect LES function. 14 The disease’s prevalence in Kazakhstan ranges from 40.5% to 67.6%, highlighting significant regional variability linked to dietary and genetic factors. 18
Complications of untreated GERD, including Barrett’s esophagus and esophageal adenocarcinoma, contribute to increased mortality. For instance, previous studies showed that the incidence of esophageal adenocarcinoma has risen sharply in obesity- related GERD patients.8,47
Treatment methods for GERD and their limitations
Pharmacological and conservative management
Initial management of GERD focuses on lifestyle modifications, such as weight loss, dietary changes, and head-of-bed elevation. These interventions are particularly beneficial for obese patients, as weight loss reduces intra-abdominal pressure. 30 However, adherence to lifestyle changes remains a significant challenge, limiting their efficacy in severe GERD cases. 15
Pharmacological treatments, primarily proton pump inhibitors (PPIs), offer effective acid suppression and symptomatic relief. Long-term use of PPIs, however, is associated with risks such as nutrient deficiencies (e.g., magnesium and vitamin B12), increased susceptibility to infections, and potential kidney complications.17,48 H2 receptor antagonists and antacids provide alternative options but are less effective for chronic or severe GERD cases. 38
Botulinum toxin, commonly known as Botox, has been investigated as a potential treatment for GERD. 49 Its administration involves injecting the toxin into the LES to decrease sphincter pressure, thereby aiming to alleviate GERD symptoms. 50 However, research has shown that this approach may lead to hiatal paralysis, which can result in an increase in gastroesophageal reflux episodes. 49 For instance, studies have demonstrated that Botox injections into the LES can cause significant reductions in sphincter pressure and hiatal contraction, further exacerbating reflux symptoms. 51 Therefore, while botulinum toxin injections may provide temporary relief for certain esophageal motility disorders, their long-term efficacy and safety in GERD treatment remain uncertain, necessitating further clinical research.49,50
Surgical methods for GERD treatment and their comparison
Surgical options for GERD aim to restore the physiological barrier against reflux. Nissen fundoplication, the gold standard, involves a 360-degree wrap of the gastric fundus around the lower esophagus to augment LES pressure. This procedure is highly effective, with success rates exceeding 90% in symptom control.52,53 However, it carries risks such as dysphagia and gas bloat syndrome, particularly in patients with motility disorders.
Partial fundoplications, such as Toupet (posterior 270-degree wrap) and Dor (anterior 180-degree wrap), offer comparable reflux control while reducing the risk of dysphagia. These procedures are better suited for patients with preexisting esophageal motility issues.30,52,53 Laparoscopic approaches have further reduced surgical morbidity and recovery times, making fundoplication a viable option for a broader patient population. 54
Bariatric surgery: Procedures, privileges, and effectiveness
Bariatric surgery is an effective solution for managing both obesity and GERD. The two most common procedures are RYGB and SG.
How bariatric surgery is performed
RYGB: This procedure involves creating a small gastric pouch and rerouting the small intestine to bypass a significant portion of the stomach and duodenum. The new gastric pouch reduces acid production, and the intestinal diversion prevents bile reflux, making RYGB particularly effective for GERD patients. 55 In this surgical approach, the incidence of de novo GERD is approximately 11% 5 years after the procedure. 56 Additionally, studies indicate that GERD remission rates can reach up to 99% following revisional surgery for GERD after gastric bypass. 55
SG: SG involves removing approximately 80% of the stomach, leaving a tubular gastric sleeve. While effective for weight loss, SG often exacerbates GERD due to increased intragastric pressure and alterations in LES function.57,58 Additionally, long-term follow-up studies indicate that de novo GERD occurs in 30.4% of patients.56,59 Research findings suggest that GERD remission rates reach 86.4% within 12 months following SG and improve further to 90.9% at 34 months when fundoplication is performed alongside SG. 59 Furthermore, prior studies have demonstrated that incorporating hiatal hernia repair with SG significantly alleviates postoperative GERD symptoms. 59
One-anastomosis gastric bypass (OAGB): OAGB has gained popularity in recent years due to its technical simplicity, shorter operative time, and favorable weight-loss outcomes. However, despite these advantages, concerns persist regarding the risk of bile reflux, which can lead to alkaline esophagitis and Barrett’s esophagus. 60 For this technique, de novo GERD occurs in 6% of patients, while esophagitis develops in 15%, and Barrett’s esophagus is observed in 1% of cases. 61 Furthermore, GERD remission is reported at 86.4% within the first year postoperatively, with rates improving to 90.9% during long-term follow-up. 59
Fundoplication sleeve gastrectomy (FSG): FSG is a surgical technique that combines SG with fundoplication to address GERD in patients undergoing bariatric surgery. 62 This approach aims to enhance the LES tone, thereby reducing the incidence of postoperative GERD. 63 Previous study assessing SG combined with Rossetti fundoplication reported a 330% increase in LES tone, indicating a substantial improvement in esophagogastric junction competency. 62 Furthermore, previous study showed that 1 year after LSG, 52.2% developed GERD, decreasing to 30.4% at 34 months. In the group with FSG, reflux symptoms improved in 86.4% at 12 months and 90.9% at 34 months. 59 This approach also demonstrated high GERD remission rates, with 86.4% of patients experiencing symptom resolution within 1 year, which further improved to 90.9% over extended follow-up periods. 59 However, while FSG shows promise in reducing GERD symptoms, further research is needed to evaluate its long-term efficacy and potential impact on gastric motility. 64
Privileges and effectiveness, and disadvantages of bariatric surgery
RYGB offers significant advantages for GERD resolution, with studies showing a symptom improvement rate of 80%–90%. Its anatomical alterations reduce acid exposure and bile reflux, addressing both primary and secondary causes of GERD. 54 In contrast, SG is preferred for patients who prioritize a simpler procedure with fewer nutritional deficiencies, although GERD outcomes may be suboptimal. 8 However, its association with GERD remains a subject of concern. Studies indicate that LSG can lead to de novo GERD in 20%–30% of patients postoperatively, with exacerbation of preexisting GERD symptoms observed in up to 32% of cases. 32 The mechanisms underlying these effects include alterations in the esophagogastric junction, increased intragastric pressure, and disruption of normal LES function. Notably, preoperative GERD is a predictor of postoperative symptom persistence, with some patients requiring conversion to RYGB for symptom resolution.55,65
Laparoscopic sleeve gastrectomy (LSG) is known to compromise the integrity of the antireflux barrier, a crucial anatomical mechanism preventing gastroesophageal reflux. By altering the esophagogastric junction and reducing LES pressure, LSG disrupts the valve-like mechanism that normally impedes acid reflux, thereby increasing the likelihood of de novo GERD and worsening pre-existing symptoms. 65 This disruption is primarily attributed to the resection of the gastric fundus, which plays a key role in augmenting LES function and maintaining a pressure gradient between the stomach and esophagus. 66 Additionally, LSG-induced changes in gastric anatomy, such as increased intragastric pressure and reduced gastric compliance, further contribute to pathological reflux. Given these considerations, preoperative assessment of esophagogastric junction (EGJ) integrity using endoscopic and manometric evaluation is critical for patient selection and surgical planning, particularly in those at high risk for GERD-related complications.65,66
Unlike RYGB, which diverts bile away from the esophagus, OAGB creates a direct path for biliary secretions, increasing the potential for reflux-related complications. The long-term consequences of bile reflux, including esophageal mucosal damage and potential carcinogenic risks, remain subjects of ongoing debate. 54
Moreover, hiatal hernia repair is increasingly performed in combination with bariatric surgery, particularly in patients with obesity-related GERD. Hiatal hernias contribute to reflux by weakening the antireflux barrier and disrupting the esophagogastric junction, making their correction an essential adjunct to bariatric procedures such as SG and RYGB. 67 Studies suggest that concurrent HHR with bariatric surgery can improve postoperative reflux control and reduce the likelihood of persistent GERD symptoms (Castagneto-Gissey et al., 2023). 63 However, the durability of these repairs remains a topic of debate, as some patients experience hernia recurrence and reflux symptoms over time, necessitating long-term follow-up, and potential revisional interventions.67,68
While traditional fundoplication procedures such as Nissen and Toupet fundoplication are rarely performed in patients with prior bariatric surgery, emerging techniques now integrate fundoplication with LSG to enhance reflux control. Sleeve-fundoplication hybrid procedures, such as SG with concomitant anterior or posterior fundoplication, aim to preserve the weight-loss benefits of LSG while minimizing the risk of postoperative GERD.69,70 Early studies suggest that these approaches improve LES function and reduce acid exposure without significantly altering gastric emptying. However, long-term data on durability, safety, and weight-loss efficacy remain limited, necessitating further research to validate these novel surgical strategies.67,71
Future prospects
Emerging technologies, such as magnetic sphincter augmentation and endoscopic antireflux procedures, promise to improve GERD management by minimizing complications and offering durable symptom control. 40 Personalized treatment strategies integrating surgical and pharmacological approaches are essential for optimizing outcomes in diverse patient populations.
Conclusion
While our analysis paints a comprehensive picture of the current research landscape, it also identifies a critical need for continued innovation, diversified global participation, and a holistic approach to the treatment of GERD in the context of obesity and bariatric surgery. Future research should aim to fill the identified gaps, particularly in long-term outcomes and the effectiveness of new treatments, ensuring that improvements in bariatric surgery translate into tangible benefits for patients worldwide.
Future studies should emphasize the standardization of methodologies for GERD and bariatric surgery research, alongside fostering collaborations across diverse socioeconomic contexts to enhance generalizability. By establishing consistent research protocols, the reliability of findings can be significantly improved, enabling a clearer understanding of the interplay between obesity and GERD. Additionally, addressing healthcare disparities through inclusive research efforts will better inform clinical practices and optimize patient outcomes. Ultimately, these initiatives will pave the way for innovative approaches in managing GERD within the framework of obesity treatment and bariatric interventions.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121251336304 for Assessing academic impact through a bibliometrics analysis: Gastroesophageal reflux disease in the context of obesity treatment and bariatric surgery by Akbayan Imanbayeva, Bazylbek Zhakiev, Asset Yelemessov, Kairat Adaibayev, Kymbat Tussupkaliyeva, Dulat Turebayev, Saltanat Urazova, Laura Mamesheva and Alireza Afshar in SAGE Open Medicine
Acknowledgments
Not applicable.
Footnotes
ORCID iD: Alireza Afshar  https://orcid.org/0000-0002-8618-5872
https://orcid.org/0000-0002-8618-5872
Ethical considerations: Not applicable.
Author contributions: Conceptualization: AI, KT, and AA; Methodology: AI, AY, KT, and DT; Software: BZ, AI, and DT; Validation: AY, KT, and SU; Formal analysis: BZ, KA, SU, and AA; Investigation: AY, KA, LM, and AA; Resources: AI and KT; Data curation: AY and LM; Writing – original draft preparation: AI, KT, and AA; Writing – review and editing: AI, BZ, AY, KA, KT, DT, SU, LM, and AA; Visualization: DT and AA; Supervision: AI and BZ; Project administration: KA; Funding acquisition: N/A. All authors have read and agreed to the published version of the manuscript.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Data availability Statement: The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Supplemental material: Supplemental material for this article is available online.
References
- 1. Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014; 384: 766–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. El-Serag HB, Sweet S, Winchester CC, et al. Update on the epidemiology of gastro-esophageal reflux disease: a systematic review. Gut 2014; 63: 871–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ting L, Lixin C, Jiahui C, et al. Association of obesity with coronary artery disease, erosive esophagitis and gastroesophageal reflux disease: a systematic review and meta-analysis. Iran J Public Health 2022; 51(8): 1690–1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gulinac M, Miteva DG, Peshevska-Sekulovska M, et al. Long-term effectiveness, outcomes and complications of bariatric surgery. World J Clin Cases 2023; 11: 4504–4512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dixon JB, O’Brien PE, Playfair J, et al. Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA 2008; 299: 316–323. [DOI] [PubMed] [Google Scholar]
- 6. Colquitt JL, Pickett K, Loveman E, et al. Surgery for weight loss in adults. Cochrane Database Syst Rev 2014; 2014(8): CD003641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schauer Philip R, Bhatt Deepak L, Kirwan John P, et al. Bariatric surgery versus intensive medical therapy for diabetes—5-year outcomes. N Engl J Med 2017; 376: 641–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Masood M, Low D, Deal SB, et al. Gastroesophageal reflux disease in obesity: bariatric surgery as both the cause and the cure in the morbidly obese population. J Clin Med 2023; 12; 20230825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery survey 2018: similarities and disparities among the 5 IFSO chapters. Obes Surg 2021; 31: 1937–1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bou Daher H, Sharara AI. Gastroesophageal reflux disease, obesity and laparoscopic sleeve gastrectomy: the burning questions. World J Gastroenterol 2019; 25: 4805–4813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gu L, Chen B, Du N, et al. Relationship between bariatric surgery and gastroesophageal reflux disease: a systematic review and meta-analysis. Obes Surg 2019; 29: 4105–4113. [DOI] [PubMed] [Google Scholar]
- 12. Robert M, Espalieu P, Pelascini E, et al. Efficacy and safety of one anastomosis gastric bypass versus Roux-en-Y gastric bypass for obesity (YOMEGA): a multicenter, randomized, open-label, non-inferiority trial. Lancet 2019; 393: 1299–1309. [DOI] [PubMed] [Google Scholar]
- 13. Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Internal Med 2005; 143: 199–211. [DOI] [PubMed] [Google Scholar]
- 14. Baimakhanov B, Zhurayev S, Shokebaev A, et al. Clinical outcome and recurrence of open versus laparoscopic Nissen fundoplication in the Republic of Kazakhstan during 2010–2021. Iran J Med Sci 2024; 49: 22–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wu J, Ma Y, Chen Y. GERD-related chronic cough: possible mechanism, diagnosis and treatment. Front Physiol 2022; 13: 1005404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Priyadharsini JV, Gayatridevi R. Gerd induced dental erosion. Int J Pharmac Res 2020: 24. DOI: 10.31838/ijpr/2020.SP1.004. [DOI] [Google Scholar]
- 17. Vaezi MF, Slaughter JC, Smith BS, et al. Dilated intercellular space in chronic laryngitis and gastro-esophageal reflux disease: at baseline and post-lansoprazole therapy. Aliment Pharmacol Ther 2010; 32: 916–924. [DOI] [PubMed] [Google Scholar]
- 18. Durazzo M, Lupi G, Cicerchia F, et al. Extra-esophageal presentation of gastroesophageal reflux disease: 2020 update. J Clin Med 2020; 9(8): 2559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kim SY, Min C, Oh DJ, et al. Bidirectional association between GERD and asthma: two longitudinal follow-up studies using a national sample cohort. J Allergy Clin Immunol Pract 2020; 8: 1005–1013.e9. [DOI] [PubMed] [Google Scholar]
- 20. Hakanson BS, Lundell L, Bylund A, et al. Comparison of laparoscopic 270 degrees posterior partial fundoplication versus total fundoplication for the treatment of gastroesophageal reflux disease: a randomized clinical trial. JAMA Surg 2019; 154: 479–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fass OZ, Mashimo H. The effect of bariatric surgery and endoscopic procedures on gastroesophageal reflux disease. J Neurogastroenterol Motil 2021; 27: 35–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. El-Hadi M, Birch DW, Gill RS, et al. The effect of bariatric surgery on gastroesophageal reflux disease. Can J Surg 2014; 57: 139–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Manoj Kumar L, George RJ, P SA. Bibliometric analysis for medical research. Indian J Psychol Med 2022; 45: 277–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ellili NOD. Bibliometric analysis and systematic review of environmental, social, and governance disclosure papers: current topics and recommendations for future research. Environ Res Commun 2022; 4: 092001. [Google Scholar]
- 25. Bekenova NB, Vochshenkova TA, Ablakimova N, et al. A bibliometric analysis of study of associations of certain genotypes with the cardiovascular form of diabetic neuropathy. BioMed Res Int 2024; 2024: 6761451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Seckin D, Cebeci F. Bariatric surgery and weight gain: bibliometric analysis. Obes Surg 2024; 34: 929–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ozsoy Z, Demir E. Which bariatric procedure is the most popular in the world? A bibliometric comparison. Obes Surg 2018; 28: 2339–2352. [DOI] [PubMed] [Google Scholar]
- 28. Zhang T, Zhang B, Tian W, et al. Trends in gastroesophageal reflux disease research: a bibliometric and visualized study. Front Med 2022; 9: 994534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rrezza EE, Ikramuddin S, Gourash W, et al. Symptomatic improvement in gastroesophageal reflux disease (GERD) following laparoscopic Roux-en-Y gastric bypass. Surg Endosc 2002; 16: 1027–1031. [DOI] [PubMed] [Google Scholar]
- 30. Gyawali CP, Fass R. Management of gastroesophageal reflux disease. Gastroenterology 2018; 154: 302–318. [DOI] [PubMed] [Google Scholar]
- 31. Livingston EH. Procedure incidence and in-hospital complication rates of bariatric surgery in the United States. Am J Surg 2004; 188: 105–110. [DOI] [PubMed] [Google Scholar]
- 32. Sebastianelli L, Benois M, Vanbiervliet G, et al. Systematic endoscopy 5 years after sleeve gastrectomy results in a high rate of Barrett’s esophagus: results of a multicenter study. Obes Surg 2019; 29: 1462–1469. [DOI] [PubMed] [Google Scholar]
- 33. Cohen R, Pinheiro JS, Correa JL, et al. Laparoscopic Roux-en-Y gastric bypass for BMI < 35 kg/m2: a tailored approach. Surg Obes Relat Dis 2006; 2: 401–404. [DOI] [PubMed] [Google Scholar]
- 34. Prachand VN, Ward M, Alverdy JC. Duodenal Switch provides superior resolution of metabolic comorbidities independent of weight loss in the super-obese (BMI ⩾ 50 kg/m2) compared with gastric bypass. J Gastrointest Surg 2010; 14: 211–220. [DOI] [PubMed] [Google Scholar]
- 35. Wood MH, Carlin AM, Ghaferi AA, et al. Association of race with bariatric surgery outcomes. JAMA Surg 2019; 154: e190029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tolone S, Cristiano S, Savarino E, et al. Effects of omega-loop bypass on esophagogastric junction function. Surg Obes Relat Dis 2016; 12: 62–69. [DOI] [PubMed] [Google Scholar]
- 37. Parmar CD, Mahawar KK, Boyle M, et al. Conversion of sleeve gastrectomy to Roux-en-Y gastric bypass is effective for gastro-esophageal reflux disease but not for further weight loss. Obes Surg 2017; 27: 1651–1658. [DOI] [PubMed] [Google Scholar]
- 38. Shaqran TM, Ismaeel MM, Alnuaman AA, et al. Epidemiology, causes, and management of gastro-esophageal reflux disease: a systematic review. Cureus 2023; 15: e47420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Xie M, Deng L, Fass R, et al. Obesity is associated with higher prevalence of gastroesophageal reflux disease and reflux related complications: a global healthcare database study. Neurogastroenterol Motil 2024; 36: e14750. [DOI] [PubMed] [Google Scholar]
- 40. Marabotto E, Mari A, Calabrese F, et al. Biliary reflux after bariatric surgery and after gastroesophageal surgery for gastroesophageal reflux disease. Digest Med Res 2023; 7: 2. [Google Scholar]
- 41. Okunogbe A, Nugent R, Spencer G, et al. Economic impacts of overweight and obesity: current and future estimates for eight countries. BMJ Global Health 2021; 6: e006351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Benalcazar DA, Cascella M. Obesity surgery preoperative assessment and preparation. In: StatPearls. Treasure Island, FL: StatPearls Publishing, 2024. [PubMed] [Google Scholar]
- 43. Sánchez-Torralvo FJ, Vázquez-Pedreño L, Gonzalo-Marín M, et al. Endoscopic intragastric injection of botulinum toxin A in obese patients accelerates weight loss after bariatric surgery: follow-up of a randomized controlled trial (IntraTox Study). J Clin Med 2022; 11(8): 2126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Sánchez Torralvo FJ, Vázquez Pedreño L, Gonzalo Marín M, et al. Endoscopic intragastric injection of botulinum toxin A in obese patients on bariatric surgery waiting lists: a randomized double-blind study (IntraTox study). Clin Nutr 2021; 40: 1834–1842. [DOI] [PubMed] [Google Scholar]
- 45. Mukhtar B, Shad MK, Ali K, et al. Systematic literature review and retrospective bibliometric analysis on ESG research. Int J Product Perform Manag 2024; 74(4): 1365–1399. [Google Scholar]
- 46. Kim SE, Lezama MM, Schlottmann F. Gastroesophageal reflux disease, Barrett’s esophagus and beyond. In: Schlottmann F, Herbella FAM, Patti MG. (eds) Gastroesophageal reflux disease: from pathophysiology to treatment. Cham: Springer Nature Switzerland, 2023, pp. 147–158. [Google Scholar]
- 47. Elliott JA, Reynolds JV. Visceral obesity, metabolic syndrome, and esophageal adenocarcinoma. Front Oncol 2021; 11: 627270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Zhao Y, Han H, Lu Q, et al. Characteristics of laryngopharyngeal reflux in patients with chronic cough induced by gastroesophageal reflux disease. Ear Nose Throat J 2023: 01455613231205393. DOI: 10.1177/01455613231205393. [DOI] [PubMed] [Google Scholar]
- 49. Kumar D, Zifan A, Mittal RK. Botox injection into the lower esophageal sphincter induces hiatal paralysis and gastroesophageal reflux. Am J Physiol Gastrointest Liver Physiol 2019; 318: G77–G83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Beutner C, Bartsch K, Laskawi R, et al. Botulinum toxin A in the treatment of oropharyngeal or esophageal dysphagia. Int J Otolaryngol Head Neck Surg 2013; 2: 253–258. [Google Scholar]
- 51. Thomas A, de Souza Ribeiro B, Malespin M, et al. Botulinum toxin as a treatment for refractory gastroparesis: a literature review. Curr Treat Options Gastroenterol 2018; 16: 479–488. [DOI] [PubMed] [Google Scholar]
- 52. Analatos A, Håkanson BS, Ansorge C, et al. Clinical outcomes of a laparoscopic total versus a 270° posterior partial fundoplication in chronic gastroesophageal reflux disease: a randomized clinical trial. JAMA Surg 2022; 157: 473–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Gefen R, Marom G, Brodie R, et al. Complete versus partial fundoplication: a laboratory measurement of functionality and effectiveness. Minim Invasive Ther Allied Technol 2022; 31: 635–641. [DOI] [PubMed] [Google Scholar]
- 54. Robert M, Poghosyan T, Maucort-Boulch D, et al. Efficacy and safety of one anastomosis gastric bypass versus Roux-en-Y gastric bypass at 5 years (YOMEGA): a prospective, open-label, non-inferiority, randomized extension study. Lancet Diabetes Endocrinol 2024; 12: 267–276. [DOI] [PubMed] [Google Scholar]
- 55. Chiappetta S, Lainas P, Kassir R, et al. Gastroesophageal reflux disease as an indication of revisional bariatric surgery—indication and results—a systematic review and metanalysis. Obes Surg 2022; 32: 3156–3171. [DOI] [PubMed] [Google Scholar]
- 56. Ashrafi D, Osland E, Memon MA. Bariatric surgery and gastroesophageal reflux disease. Ann Transl Med 2019; 8(Suppl 1): S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Silecchia G, Iossa A. GERD and Barrett’s esophagus as indications for revisional surgery after sleeve gastrectomy: experience of a bariatric center of excellence IFSO-EC and narrative review. Expert Rev Endocrinol Metab 2021; 16: 229–235. [DOI] [PubMed] [Google Scholar]
- 58. Qumseya BJ, Qumsiyeh Y, Ponniah SA, et al. Barrett’s esophagus after sleeve gastrectomy: a systematic review and meta-analysis. Gastrointest Endosc 2021; 93: 343–352.e342. [DOI] [PubMed] [Google Scholar]
- 59. Liu G, Wang P, Ran S, et al. Surgical treatment strategies for gastroesophageal reflux after laparoscopic sleeve gastrectomy. Front Endocrinol 2024; 15: 1463567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Csendes A. Bile reflux after one anastomosis gastric bypass. Obes Surg 2020; 30: 2802–2803. [DOI] [PubMed] [Google Scholar]
- 61. Petrucciani N, Benois M, Aurello P, et al. Analysis of factors related to gastroesophageal reflux after gastric bypass at 10-year follow-up: a retrospective single-institutional study. In Vivo 2024; 38: 982–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Di Capua F, Cesana GC, Uccelli M, et al. Sleeve gastrectomy with Rossetti fundoplication increases lower esophageal sphincter tone preventing gastroesophageal reflux disease: high-resolution manometry assessment. J Laparoendosc Adv Surg Tech A 2022; 33: 44–51. [DOI] [PubMed] [Google Scholar]
- 63. Castagneto-Gissey L, Russo MF, D’Andrea V, et al. Efficacy of sleeve gastrectomy with concomitant hiatal hernia repair versus sleeve–fundoplication on gastroesophageal reflux disease resolution: systematic review and meta-analysis. J Clin Med 2023; 12(9): 3323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Bolckmans R, Roriz-Silva R, Mazzini GS, et al. Long-term implications of GERD after sleeve gastrectomy. Curr Surg Rep 2021; 9: 7. [Google Scholar]
- 65. Ottoboni Brunaldi V, Ghanem OM, Abu Dayyeh BK. Physiological archetypes of de novo gastroesophageal reflux disease after laparoscopic sleeve gastrectomy. Foregut 2023; 4: 140–149. [Google Scholar]
- 66. Nguyen NT, Thosani NC, Canto MI, et al. The American Foregut Society white paper on the endoscopic classification of esophagogastric junction integrity. Foregut 2022; 2: 339–348. [Google Scholar]
- 67. Ehlers AP, Bonham AJ, Ghaferi AA, et al. Impact of hiatal hernia repair technique on patient-reported gastroesophageal reflux symptoms following laparoscopic sleeve gastrectomy. Surg Endosc 2022; 36: 6815–6821. [DOI] [PubMed] [Google Scholar]
- 68. Ehlers AP, Chhabra K, Thumma JR, et al. In the eye of the beholder: surgeon variation in intra-operative perceptions of hiatal hernia and reflux outcomes after sleeve gastrectomy. Surg Endosc 2021; 35: 2537–2542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Sawas T, Marya NB, Storm AC, et al. Laparoscopic hernia repair and fundoplication with endoscopic sleeve gastroplasty for complex hernia and GERD management in morbid obesity. VideoGIE 2020; 5: 555–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Gensthaler L, Schoppmann SF. New developments in anti-reflux surgery: where are we now? Visc Med 2024; 40: 250–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Aiolfi A, Micheletto G, Marin J, et al. Laparoscopic sleeve-fundoplication for morbidly obese patients with gastroesophageal reflux: systematic review and meta-analysis. Obes Surg 2021; 31: 1714–1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121251336304 for Assessing academic impact through a bibliometrics analysis: Gastroesophageal reflux disease in the context of obesity treatment and bariatric surgery by Akbayan Imanbayeva, Bazylbek Zhakiev, Asset Yelemessov, Kairat Adaibayev, Kymbat Tussupkaliyeva, Dulat Turebayev, Saltanat Urazova, Laura Mamesheva and Alireza Afshar in SAGE Open Medicine